Contents
- What is hantavirus pulmonary syndrome
- Hantaviruses
- Risk factors for hantavirus pulmonary syndrome
- How People Get Hantavirus Infection
- Hantavirus pulmonary syndrome prevention
- Hantavirus pulmonary syndrome symptoms
- Hantavirus pulmonary syndrome complications
- Hantavirus pulmonary syndrome diagnosis
- Hantavirus pulmonary syndrome treatment
What is hantavirus pulmonary syndrome
Hantavirus Pulmonary Syndrome is a severe, sometimes fatal, respiratory infectious disease in humans caused by infection with hantaviruses (part of the hemorrhagic fever virus). Hantavirus pulmonary syndrome is characterized by flu-like symptoms that can progress rapidly to potentially life-threatening breathing problems. Many hantaviruses are known to cause hantavirus pulmonary syndrome. Each virus has a single primary host. The most important hantavirus in the US is the Sin Nombre virus, which means “no name virus” in Spanish, hosted by the deer mouse (see Figure 1 below). You become infected primarily by breathing air infected with hantaviruses that are shed in rodent urine and droppings.
Anyone who comes into contact with rodents that carry hantaviruses is at risk of hantavirus pulmonary syndrome. Rodent infestation in and around the home remains the primary risk for hantavirus exposure. Even healthy individuals are at risk for hantavirus pulmonary syndrome infection if exposed to the virus.
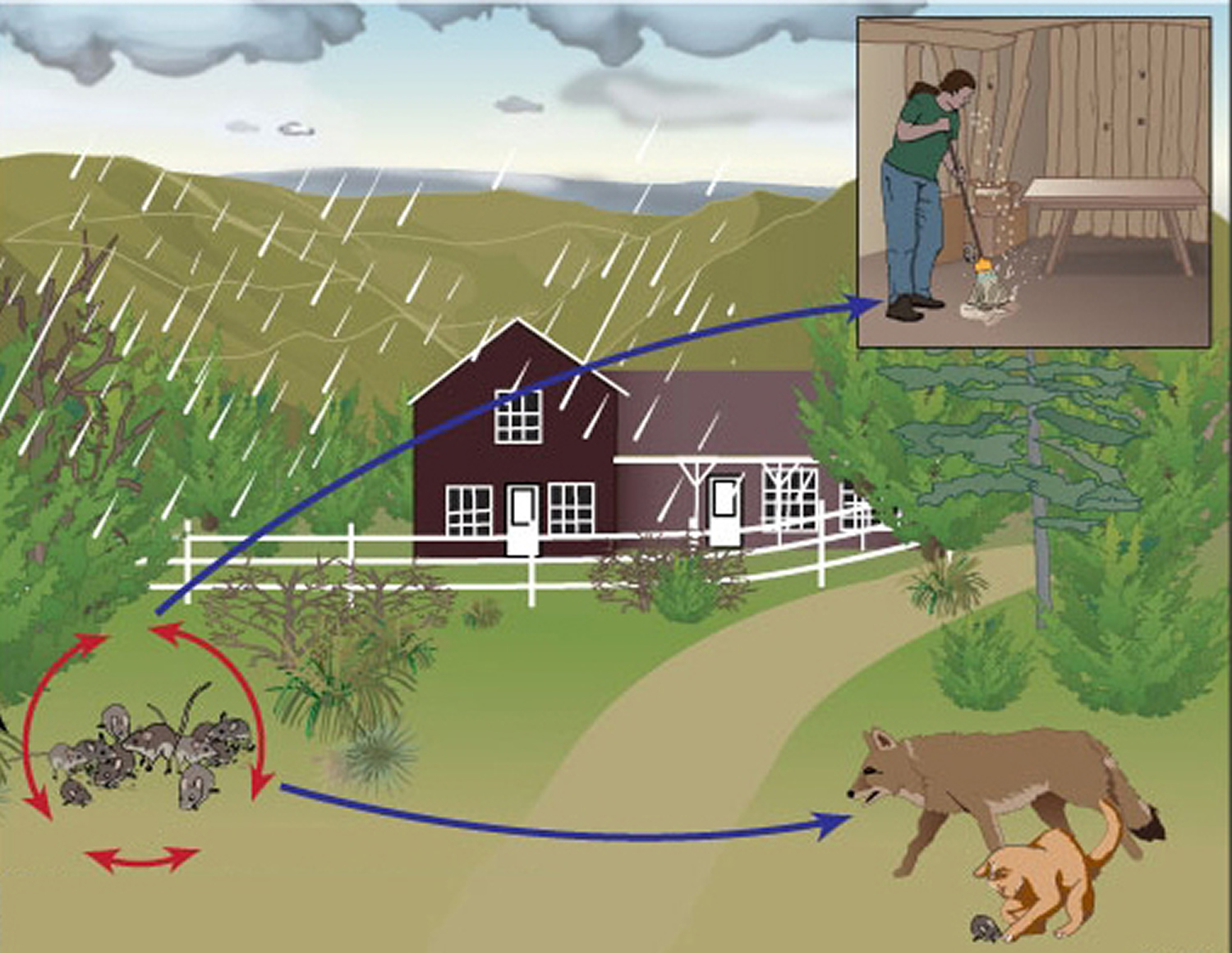
Favorable environmental conditions such as mild winters and summer rainfall may cause dramatic increases in rodent populations. More rodents become infected under crowded conditions. Deer mice may enter human structures in rural areas. Humans may become infected when they inhale airborne virus or come into direct contact with infected rodents or their urine, feces, or nests. Other mammal species (cats, dogs, coyotes) may be infected through contact with rodent hosts, but they are not known to transmit hantavirus.
To date, no cases of hantavirus pulmonary syndrome have been reported in the United States in which the virus was transmitted from one person to another. In fact, in a study of health care workers who were exposed to either patients or specimens infected with related types of hantaviruses (which cause a different disease in humans), none of the workers showed evidence of infection or illness.
In Chile and Argentina, rare cases of person-to-person transmission have occurred among close contacts of a person who was ill with a type of hantavirus called Andes virus.
Because treatment options are limited, the best protection against hantavirus pulmonary syndrome is to avoid rodents and their habitats.
The signs and symptoms of hantavirus pulmonary syndrome can worsen suddenly and may quickly become life-threatening. If you’ve been around rodents or rodent droppings and have signs and symptoms of fever, chills, muscle aches or any difficulties breathing, seek immediate medical attention.
Hantaviruses
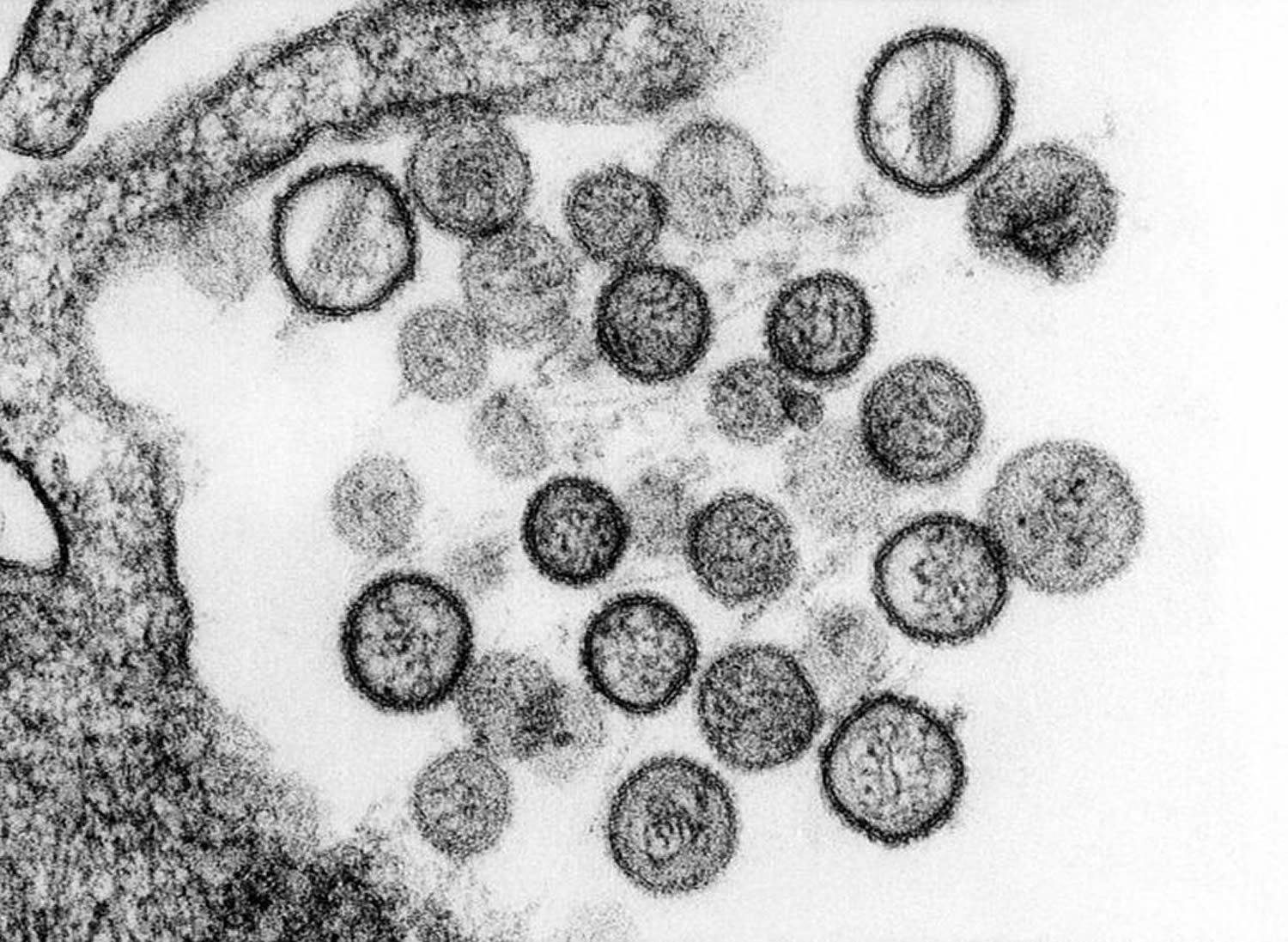
Hantaviruses belong to the bunyavirus family of viruses. There are 5 genera within the family: bunyavirus, phlebovirus, nairovirus, tospovirus, and hantavirus. Each is made up of negative-sensed, single-stranded RNA viruses. All these genera include arthropod-borne viruses, with the exception of hantavirus, which is rodent-borne.
Like other members of the bunyavirus family, hantaviruses are enveloped viruses with a genome that consists of three single-stranded RNA segments designated S (small), M (medium), and L (large). All hantaviral genes are encoded in the negative (genome complementary) sense. The S RNA encodes the nucleocapsid (N) protein. The M RNA encodes a polyprotein that is cotranslationally cleaved to yield the envelope glycoproteins G1 and G2. The L RNA encodes the L protein, which functions as the viral transcriptase/replicase. Within virions, the genomic RNAs of hantaviruses are thought to complex with the N protein to form helical nucleocapsids, which circularize due to sequence complementarity between the 5′ and 3′ terminal sequences of each genomic segment.
Hantaviruses replicate exclusively in the host cell cytoplasm. Entry into host cells is thought to occur by attachment of virions to cellular receptors and subsequent endocytosis. Nucleocapsids are introduced into the cytoplasm by pH-dependent fusion of the virion with the endosomal membrane. Transcription of viral genes is initiated by association of the L protein with the three nucleocapsid species. In addition to transcriptase and replicase functions, the viral L protein is also thought to have an endonuclease activity that cleaves cellular messenger RNAs (mRNAs) for the production of capped primers used to initiate transcription of viral mRNAs. As a result of this “cap snatching”, the mRNAs of hantaviruses are believed to be capped and contain nontemplated 5′ terminal extensions. The viral N and L mRNAs are thought to undergo translation at free ribosomes, whereas the M mRNA is translated in the endoplasmic reticulum. G1 and G2 glycoproteins form heterodimers and are then transported from the endoplasmic reticulum to the Golgi complex, where glycosylation is completed. The L protein produces nascent genomes by replication via a positive-sense RNA intermediate. Hantavirions are believed to form by association of nucleocapsids with glycoproteins embedded in the membranes of the Golgi, followed by budding into the Golgi cisternae. Nascent virions are then transported in secretory vesicles to the plasma membrane and released by exocytosis.
Table 1. Characteristics of Some Known Hantaviruses
| Hantaviruses | Geographic Region | Reservoir | Pathology | Mortality |
|---|---|---|---|---|
| Hantaan | Asia | Field mouse | Renal | 5-15% |
| Seoul | Worldwide | Domestic rat | Renal | 1% |
| Puumala | Northern Europe | Bank vole | Renal | 1% |
| Prospect Hill | United States | Meadow vole | No known human disease | N/A |
| Sin Nombre | North America | Deer mouse | Pulmonary | 50% |
Hantaviruses causing diseases
Hantaviruses are distributed worldwide, and are broadly split into Old World hantaviruses, which cause hemorrhagic fever with renal syndrome (hemorrhagic fever with renal syndrome), and the New World hantaviruses, which cause hantavirus pulmonary syndrome 2. Hemorrhagic fever with renal syndrome-causing hantaviruses are mainly present in Asia and Europe, and have a case fatality of 0.1–15% 2. Hantavirus pulmonary syndrome-causing hantaviruses are found throughout the Americas, and have much higher case fatality rates of 35–40% 3. Old World hantaviruses were discovered to cause hemorrhagic fever with renal syndrome around the time of the Korean War, although the first hantavirus was not isolated until 1978. However, hantaviruses were not known to cause human disease in the Americas until Sin Nombre virus—which means “no name virus” in Spanish—was first identified as the cause of an outbreak of acute respiratory distress syndrome in the southwestern United States in 1993 4. Since then, hantavirus pulmonary syndrome has been an emerging infectious disease in the Americas, and more than 20 different hantavirus pulmonary syndrome-associated hantaviruses have been identified 5. The hantavirus causing the highest burden of disease in South America is Andes virus, the only known hantavirus implicated in human-to-human transmission 6. Hantaviruses are transmitted to humans by inhalation of infectious aerosols from rodent excreta 7. Although a rare disease with a total of a few thousand cases reported, hantavirus pulmonary syndrome remains in the spotlight because of the high case fatality rates. For example, a recent hantavirus pulmonary syndrome outbreak in Yosemite park in California, in the summer of 2012, although modest in size with 10 confirmed cases and 3 deaths, caused international alarm, and hundreds of thousands of international visitors had to be notified by the National Park Services 8. Currently, no FDA-approved immunotherapeutics, antivirals, or vaccines are available for use against hantavirus pulmonary syndrome 9.
The hallmarks of both hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome are increased vascular permeability and thrombocytopenia 5. In both syndromes, patients may have pulmonary and/or renal involvement, though pulmonary involvement dominates in hantavirus pulmonary syndrome, and renal involvement in hemorrhagic fever with renal syndrome.
Table 2. Comparison of Hemorrhagic fever with renal syndrome and Hantavirus pulmonary syndrome
| Feature | Hemorrhagic fever with renal syndrome | Hantavirus pulmonary syndrome |
|---|---|---|
| Major target organ | Kidney | Lung |
| First phase | Febrile | Febrile “prodrome” |
| Second phase | Shock | Shock, pulmonary edema |
| Evolution | Oliguria, diureses, convalescence | Diureses, convalescence |
| Mortality | 1-15% | 50% |
Hantavirus pulmonary syndrome prognosis
Previous observations of patients that develop hantavirus pulmonary syndrome from New World Hantaviruses recover completely. No chronic infection has been detected in humans. Some patients have experienced longer than expected recovery times, but the virus has not been shown to leave lasting effects on the patient.
Hantavirus pulmonary syndrome can be fatal with a mortality rate of 38-50%.
Risk factors for hantavirus pulmonary syndrome
Hantavirus pulmonary syndrome is most common in rural areas of the western United States during the spring and summer months. Hantavirus pulmonary syndrome also occurs in South America and Canada. Other hantaviruses occur in Asia, where they cause kidney disorders rather than lung problems.
The chance of developing hantavirus pulmonary syndrome is greater for people who work, live or play in spaces where rodents live. Factors and activities that increase the risk include:
- Opening and cleaning long unused buildings or sheds
- Housecleaning, particularly in attics or other low-traffic areas
- Having a home or workspace infested with rodents
- Having a job that involves exposure to rodents, such as construction, utility work and pest control
- Camping, hiking or hunting
How People Get Hantavirus Infection
Where Hantavirus is Found
Cases of human hantavirus infection occur sporadically, usually in rural areas where forests, fields, and farms offer suitable habitat for the virus’s rodent hosts. Areas around the home or work where rodents may live (for example, houses, barns, outbuildings, and sheds) are potential sites where people may be exposed to the virus. In the US and Canada, the Sin Nombre hantavirus is responsible for the majority of cases of hantavirus infection. The host of the Sin Nombre virus is the deer mouse (Peromyscus maniculatus), present throughout the western and central US and Canada.
Several other hantaviruses are capable of causing hantavirus infection in the US. The New York hantavirus, carried by the white-footed mouse, is associated with hantavirus pulmonary syndrome cases in the northeastern US. The Black Creek hantavirus, carried by the cotton rat, is found in the southeastern US. Cases of hantavirus pulmonary syndrome have been confirmed elsewhere in the Americas, including Canada, Argentina, Bolivia, Brazil, Chile, Panama, Paraguay, and Uruguay.
Can pets transmit hantavirus pulmonary syndrome to humans?
The hantaviruses that cause human illness in the United States are not known to be transmitted by any types of animals other than certain species of rodents. Dogs and cats are not known to carry hantavirus; however, they may bring infected rodents into contact with people if they catch such animals and carry them home.
How People Become Infected with Hantaviruses
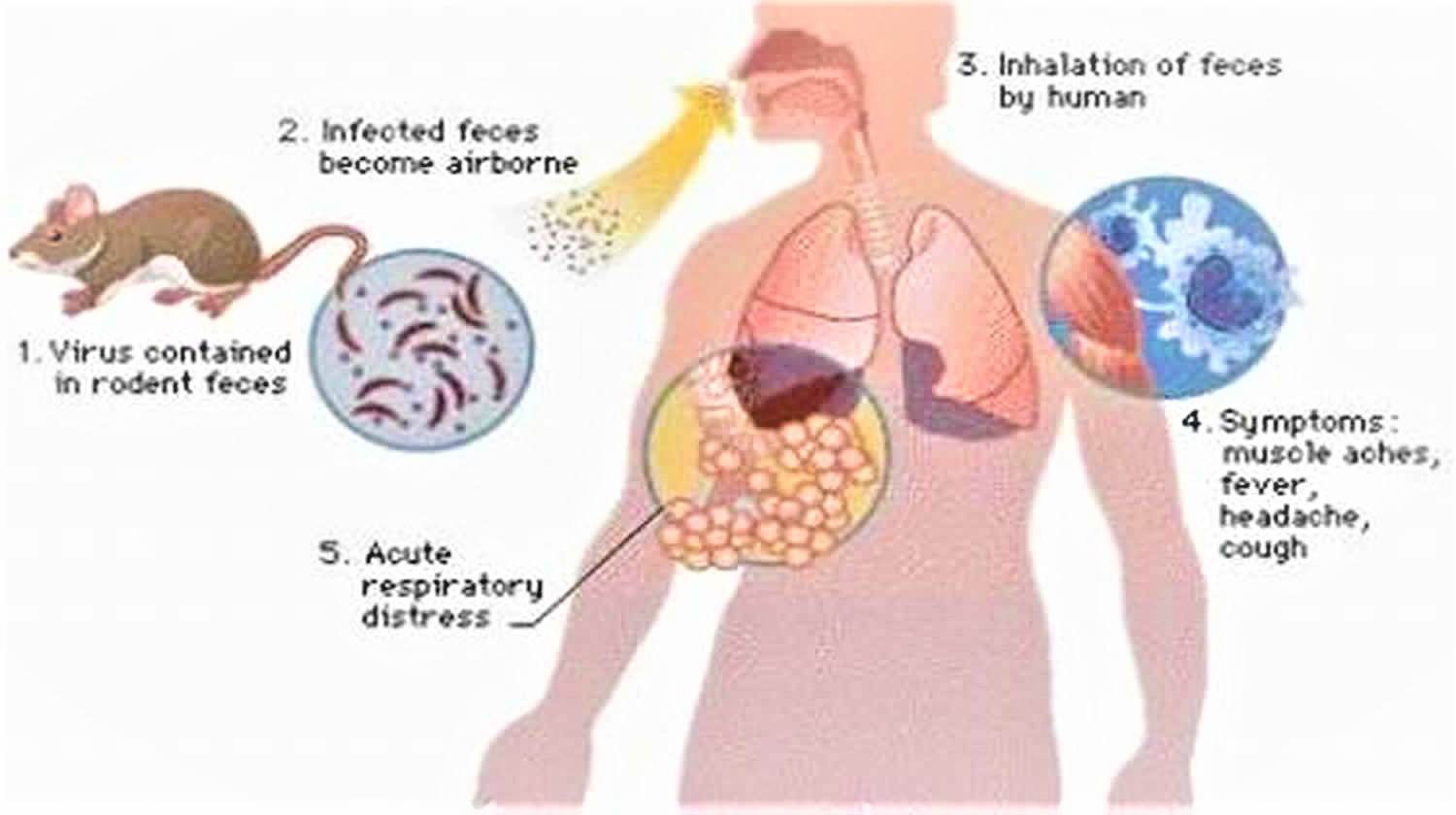
In the United States, deer mice (along with cotton rats and rice rats in the southeastern states and the white-footed mouse in the Northeast) are reservoirs of the hantaviruses. The rodents shed the virus in their urine, droppings, and saliva. The virus is mainly transmitted to people when they breathe in air contaminated with the hantavirus.
When fresh rodent urine, droppings, or nesting materials are stirred up, tiny droplets containing the virus get into the air. This process is known as “airborne transmission“.
There are several other ways rodents may spread hantavirus to people:
- If a rodent with the virus bites someone, the virus may be spread to that person, but this type of transmission is rare.
- Scientists believe that people may be able to get the virus if they touch something that has been contaminated with rodent urine, droppings, or saliva, and then touch their nose or mouth.
- Scientists also suspect people can become sick if they eat food contaminated by urine, droppings, or saliva from an infected rodent.
The hantaviruses that cause human illness in the United States cannot be transmitted from one person to another. For example, you cannot get these viruses from touching or kissing a person who has hantavirus pulmonary syndrome or from a health care worker who has treated someone with the disease.
In Chile and Argentina, rare cases of person-to-person transmission have occurred among close contacts of a person who was ill with a type of hantavirus called Andes virus.
Figure 1. North American deer mouse (Peromyscus maniculatus) has been determined to be one of the reservoirs and transmitters of the hantavirus.
Note: North American deer mouse (Peromyscus maniculatus) is a deceptively cute animal, with big eyes and big ears. Its head and body are normally about 2 – 3 inches long, and its tail adds another 2 – 3 inches in length. Depending on its age, you may see it in a variety of colors, from gray, to reddish brown. The underbelly is always white, and the tail has sharply defined white sides. The deer mouse is found almost everywhere in North America. Though this mouse prefers woodlands, it also turns up in desert areas.
Figure 2. Cotton rat (Sigmodon hispidus) is a known hantavirus carrier
Note: A cotton rat, Sigmodon hispidus, whose habitat includes the southeastern United States, and way down into Central and South America. Its body is larger than the North American deer mouse, Peromyscus maniculatus, and measures about 5 – 7 inches, which includes the head and body; the tail measures an additional 3 – 4 inches. Its hair is longer, and coarser than Peromyscus maniculatus, and is a grayish-brown color, sometimes grayish-black. The cotton rat prefers overgrown areas with shrubs and tall grasses. Sigmodon hispidus is a known hantavirus carrier.
Figure 3. Hantavirus transmission
Figure 4. Hantavirus – Sin Nombre virus particles/virions
[Source 10]People at Risk for Hantavirus Infection
Anyone who comes into contact with rodents that carry hantavirus is at risk of hantavirus pulmonary syndrome. Rodent infestation in and around the home remains the primary risk for hantavirus exposure. Even healthy individuals are at risk for hantavirus pulmonary syndrome infection if exposed to the virus.
Any activity that puts you in contact with rodent droppings, urine, saliva, or nesting materials can place you at risk for infection. Hantavirus is spread when virus-containing particles from rodent urine, droppings, or saliva are stirred into the air. It is important to avoid actions that raise dust, such as sweeping or vacuuming. Infection occurs when you breathe in virus particles.
Potential Risk Activities for Hantavirus Infection
Opening and Cleaning Previously Unused Buildings
Opening or cleaning cabins, sheds, and outbuildings, including barns, garages and storage facilities, that have been closed during the winter is a potential risk for hantavirus infections, especially in rural settings.
Housecleaning Activities
Cleaning in and around your own home can put you at risk if rodents have made it their home too. Many homes can expect to shelter rodents, especially as the weather turns cold. Please see our prevention information on how to properly clean rodent-infested areas.
Work-related Exposure
Construction, utility and pest control workers can be exposed when they work in crawl spaces, under houses, or in vacant buildings that may have a rodent population.
Campers and Hikers
Campers and hikers can also be exposed when they use infested trail shelters or camp in other rodent habitats.
The chance of being exposed to hantavirus is greatest when people work, play, or live in closed spaces where rodents are actively living. However, recent research results show that many people who have become ill with hantavirus pulmonary syndrome were infected with the disease after continued contact with rodents and/or their droppings. In addition, many people who have contracted hantavirus pulmonary syndrome reported that they had not seen rodents or their droppings before becoming ill. Therefore, if you live in an area where the carrier rodents, such as the deer mouse, are known to live, take sensible precautions-even if you do not see rodents or their droppings.
Hantavirus pulmonary syndrome prevention
Eliminate or minimize contact with rodents in your home, workplace, or campsite. If rodents don’t find that where you are is a good place for them to be, then you’re less likely to come into contact with them. Seal up holes and gaps in your home or garage. Place traps in and around your home to decrease rodent infestation. Clean up any easy-to-get food.
Recent research results show that many people who became ill with hantavirus pulmonary syndrome developed the disease after having been in frequent contact with rodents and/or their droppings around a home or a workplace. On the other hand, many people who became ill reported that they had not seen rodents or rodent droppings at all. Therefore, if you live in an area where the carrier rodents are known to live, try to keep your home, vacation place, workplace, or campsite clean.
Helpful suggestions on rodent control during and after a rodent infestation
The primary strategy for preventing human exposure to rodent diseases is effective rodent control in and around the home. This is achieved by eliminating any food sources, sealing even the smallest entries into homes, and successfully trapping rodents in and around the home.
Seal up holes inside and outside the home to prevent entry by rodents
Mice can squeeze through a hole the size of a nickel, and rats can squeeze through a hole the size of a half dollar! Prevent rodents from entering the home by checking inside and outside the house for gaps or holes.
Where to look for gaps or holes inside your home:
- Inside, under, and behind kitchen cabinets, refrigerators and stoves.
- Inside closets near the floor corners.
- Around the fireplace.
- Around doors.
- Around the pipes under sinks and washing machines.
- Around the pipes going to hot water heaters and furnaces.
- Around floor vents and dryer vents.
- Inside the attic.
- In the basement or crawl space.
- In the basement and laundry room floor drains.
- Between the floor and wall juncture.
Where to look for gaps or holes outside your home:
- In the roof among the rafters, gables, and eaves.
- Around windows.
- Around doors.
- Around the foundation
- Attic vents and crawl space vents.
- Under doors.
- Around holes for electrical, plumbing, cable, and gas lines.
Fill small holes with steel wool. Put caulk around the steel wool to keep it in place. Use lath screen or lath metal, cement, hardware cloth, or metal sheeting to fix large holes. These materials can be found at your local hardware store. Fix gaps in trailer skirtings and use flashing around the base of the house. If you do not remember to seal up entry holes in your home, rodents will continue to get inside. Outbuildings and garages should also be sealed to prevent the entrance of rodents.
Clean up rodent food sources and nesting sites
Prevent contact with rodents by cleaning up your home, workplace, or campsite.
Eliminate possible rodent food sources:
- Keep food in thick plastic or metal containers with tight lids.
- Clean up spilled food right away and wash dishes and cooking utensils soon after use.
- Keep outside cooking areas and grills clean.
- Always put pet food away after use and do not leave pet-food or water bowls out overnight.
- Keep bird feeders away from the house and utilize squirrel guards to limit access to the feeder by squirrels and other rodents.
- Use a thick plastic or metal garbage can with a tight lid.
- Keep compost bins as far away from the house as possible (100 feet or more is best).
- Keep grains and animal feed in thick plastic or metal containers with tight lids. In the evening, uneaten animal feed should be returned to containers with lids.
If storing trash and food waste inside the home, do so in rodent-proof containers, and frequently clean the containers with soap and water. Dispose of trash and garbage on a frequent and regular basis, and pick up or eliminate clutter.
Eliminate possible nesting sites outside the home. Elevate hay, woodpiles, and garbage cans at least 1 foot off the ground. Move woodpiles far away from the house (100 feet or more is best). Get rid of old trucks, cars, and old tires that mice and rats could use as homes. Keep grass cut short and shrubbery within 100 feet of the home well trimmed.
Trap rodents around the home to help reduce the rodent population
Choose an appropriate snap trap. Traps for catching mice are different from those for catching rats. Carefully read the instructions before setting the trap.
When setting the trap, place a small amount of peanut butter (approximately the size of a pea) on the bait pan of the snap trap. Position the bait end of the trap next to the wall so it forms a “T” with the wall. Rodents prefer to run next to walls or other objects for safety and do not like being out in the open.
In attics, basements, and crawlspaces and other areas that do not have regular human traffic, set traps in any area where there is evidence of frequent rodent activity. Some rodents, particularly rats, are very cautious and several days may pass before they approach the traps. Other rodents, such as house mice and deer mice, are less cautious and may be trapped more quickly.
Centers for Disease Control and Prevention (CDC) do not recommend using glue traps or live traps. These traps can scare mice that are caught live and cause them to urinate. Since their urine may contain germs, this may increase your risk of being exposed to diseases.
Also place traps in outbuildings and in areas that might likely serve as rodent shelters. Natural rodent predators, such as non-poisonous snakes, owls, and hawks, may also help control and reduce the number of rodents outside the home.
If you trap inside your home, but do not seal up rodent entry holes, new rodents will enter the dwelling.
Cleaning Up After Rodents
Urine and Droppings
Take precautions before and during clean up of rodent-infested areas. Before cleaning, trap the rodents and seal up any entryways to ensure that no rodents can get in. Continue trapping for a week. If no rodents are captured, the active infestation has been eliminated and enough time has passed so that any infectious virus in the rodent’s urine/droppings or nesting material is no longer infectious.
Before starting clean up of the space, ventilate the space by opening the doors and windows for at least 30 minutes to allow fresh air to enter the area. Use cross-ventilation and leave the area during the airing-out period.
First, clean up any urine and droppings
When you begin cleaning, it is important that you DO NOT stir up dust by sweeping or vacuuming up droppings, urine, or nesting materials.
- Wear rubber, latex, or vinyl gloves when cleaning urine and droppings.
- Spray the urine and droppings with a disinfectant or a mixture of bleach and water and let soak 5 minutes. The recommended concentration of bleach solution is 1 part bleach to 10 parts water. When using a commercial disinfectant, following the manufacturer’s instructions on the label for dilution and disinfection time.
- Use a paper towel to pick up the urine and droppings, and dispose of the waste in the garbage.
- After the rodent droppings and urine have been removed, disinfect items that might have been contaminated by rodents or their urine and droppings.
Next, clean and disinfect the whole area
- Mop floors and clean countertops with disinfectant or bleach solution.
- Steam clean or shampoo upholstered furniture and carpets with evidence of rodent exposure.
- Wash any bedding and clothing with laundry detergent in hot water if exposed to rodent urine or droppings.
Lastly, remove gloves, and thoroughly wash hands with soap and water (or use a waterless alcohol-based hand rub when soap is not available and hands are not visibly soiled).
Dead Rodents or Nests
Wear rubber, latex, or vinyl gloves when cleaning up dead rodents or nests.
- Spray the dead rodent or nest and the surrounding area with a disinfectant or a mixture of bleach and water.
- Soak rodent, nesting materials or droppings in solution for 5 minutes before wiping up with a paper towel or rag.
- Place the dead rodent or nesting materials in a plastic bag and seal tightly. Place the full bag in a second plastic bag and seal.
- Throw the bag into a covered trash can that is regularly emptied.
Remove gloves, and thoroughly wash hands with soap and water (or use a waterless alcohol-based hand rub when soap is not available and hands are not visibly soiled).
Recommended methods of textile decontamination
Clothing, Bedding, Stuffed Animals
Launder potentially contaminated bedding, clothing, or stuffed animals with hot water and detergent. Use rubber, latex, vinyl, or nitrile gloves when handling contaminated laundry. Machine-dry laundry on a high setting or hang it to air dry in the sun.
Laundry detergent breaks down the virus’s lipid envelope, rendering it harmless. Additionally, heat generated by the clothes dryer will also ensure that the virus is noninfectious. However, the use of a clothes dryer alone is not recommended as the sole treatment because not all dryers reach the necessary temperature. A temperature of 45 ° Celsius, or about 115 ° Fahrenheit, is required to inactivate hantaviruses.
Carpets/Furniture
Shampoo rugs and upholstered furniture with a commercial disinfectant or with a commercial-grade steam cleaner or shampoo.
Books, Papers and other Non-washable items
You may leave books, papers, and other items that cannot be cleaned with a liquid disinfectant or thrown away, outdoors in the sunlight for several hours, or in an indoor area free of rodents for approximately 1 week before cleanup. After that time, the virus should no longer be infectious. Wear rubber, latex, vinyl, or nitrile gloves and wipe the items with a cloth moistened with disinfectant.
Once excreted into the environment by the rodent, hantaviruses can survive in the environment and remain infectious for a period of 2-3 days. Ultraviolet rays in sunlight inactivate hantaviruses.
Cabins, Sheds, Barns, or Other Outbuildings
Before attempting to clean cabins, sheds, barns, or other outbuildings, open all doors and windows for 30 minutes. This will allow fresh air to enter the work area.
- Wear rubber, latex, or vinyl gloves and clean up all rodent urine, droppings, nests, and dead rodents using disinfectant or mixture of bleach and water.
- Mop floors or spray dirt floors with a disinfectant or mixture of bleach and water.
- Clean countertops, cabinets, and drawers with a disinfectant or a mixture of bleach and water.
Attics, Basements, Crawlspaces, and Other Storage Areas
Before cleaning attics, basements, crawlspaces and other storage areas, it is necessary to completely remove the existing rodent infestation by trapping. When there is no evidence of infestation, wait about 5 days before beginning to clean these areas. Before cleaning the space, ventilate the area by opening the doors and windows for at least 30 minutes to allow fresh air to enter the area and to remove potentially contaminated air from the area. Use cross-ventilation and leave the area during the airing-out period.
When cleaning attics, basements, crawlspaces and other storage areas:
- Wear rubber, latex, or vinyl gloves when cleaning up urine, droppings, or nesting materials. Note that a dust mask may provide some protection against dust, molds, and insulation fibers, but does not protect against viruses.
- Spray any urine, droppings, and nesting materials with either a bleach and water solution (1 parts bleach to 9 parts water) or a household disinfectant prepared according to the label instructions for dilution and disinfection time. Soak well. This will inactivate any virus. Use a paper towel or rag to pick up the materials and dispose of them.
- Mop floors after spraying them using bleach/water solution or a disinfectant. Dirt floors can be sprayed with either bleach and water solution or a disinfectant.
- If exposed insulation has become contaminated with urine and droppings, it should be placed into plastic bags for removal.
- To remove any potentially contaminated materials from storage vessels/boxes:
- First, move the storage vessels/boxes outside and place them in an area that is well-ventilated and exposed to direct sunlight. The outside of the storage vessels/boxes can be disinfected using bleach and water solution or disinfectant solution;
- Next, remove the potentially contaminated materials while in the sunlit, ventilated area. Remain upwind so that any dust or debris is not blown toward your face. Some contaminated stored materials, such as clothing, books, etc. can be decontaminated by following the recommended methods of disinfection provided in the table below; items that are no longer needed can be discarded.
- Dispose of any cardboard boxes contaminated with urine or droppings. Plastic, glass, or metal containers can be disinfected by spraying with the bleach and water solution or disinfectant. Then, using a rag or paper towel, wipe up the urine or droppings and dispose of the waste.
- Clean countertops, cabinets, and drawers with disinfectant or bleach and water solution.
- Decontaminate gloves with disinfectant or bleach and water solution. Wash hands well with soap and warm water.
Cleaning and Disinfection of Vehicles with Rodent Infestations
Rodents, including squirrels, mice, and rats, may construct their nests in cars, trucks, campers, and other vehicles, especially if such vehicles are used infrequently. Rodent nesting materials can be found in many areas of a vehicle:
- the engine compartment, including in engine compartment insulation
- the ducting and air filtration components of a vehicle’s heating and air conditioning system
- the trunk of a car, including the spare tire compartment
- the passenger compartment, including the headliner, glovebox, and in or under the seats
- tool compartments
- taillight and headlight access areas and enclosures
Heavy Rodent Infestation
Special precautions should be used for cleaning homes or buildings with heavy rodent infestation. The special precautions may also apply to vacant dwellings that have attracted large numbers of rodents and to dwellings and other structures where hantavirus has been confirmed in the rodent population.
Workers who are either hired specifically to perform a clean-up or are asked to do so as part of their work activities should contact their local or state health department, local or state occupational health and safety authority (OSHA) or CDC for information about preventing rodent-borne diseases.
Persons involved in the clean-up of heavy rodent infestations should wear the protective equipment listed here:
- coveralls (disposable, if possible);
- rubber boots or disposable shoe covers;
- rubber, latex, or vinyl gloves;
- protective goggles;
- and an appropriate respiratory protection device, such as a half-mask air-purifying (or negative-pressure) respirator with a high-efficiency particulate air (HEPA) filter or a powered air-purifying respirator (PAPR) with HEPA filters. Follow local and state requirement regarding pulmonary function and fit testing before beginning any work requiring the use of a respirator.
- Personal protective gear should be decontaminated upon removal at the end of the day. All potentially infective waste material (including respirator filters) from clean-up operations that cannot be burned or deep-buried on site should be double-bagged in appropriate plastic bags. The bagged material should then be labeled as infectious (if it is to be transported) and disposed of in accordance with local requirements for infectious waste.
Air Ducts (heating and cooling ventilation systems)
When there is evidence that rodents have access to heating and cooling ventilation systems, it is best to contact a professional rodent exterminating service to remove them. Companies specializing in duct cleaning are familiar with the particular problems and risks associated with rodent infestation in ventilation systems.
Hantavirus pulmonary syndrome symptoms
Due to the small number of hantavirus pulmonary syndrome cases, the “incubation time” is not positively known. However, on the basis of limited information, it appears that symptoms may develop between 1 and 8 weeks after exposure to fresh urine, droppings, or saliva of infected rodents.
Hantavirus pulmonary syndrome advances through two distinct stages.
Early Symptoms
Early symptoms include fatigue, fever and muscle aches, especially in the large muscle groups—thighs, hips, back, and sometimes shoulders. These symptoms are universal.
There may also be headaches, dizziness, chills, and abdominal problems, such as nausea, vomiting, diarrhea, and abdominal pain. About half of all hantavirus pulmonary syndrome patients experience these symptoms.
Early symptoms:
- Fever
- Headaches
- Muscle Aches
- Stomach Problems
- Dizziness
- Chills
In its early stages, hantavirus infection is difficult to distinguish from influenza, pneumonia or other viral conditions. After four to 10 days, more-serious signs and symptoms begin.
Late Symptoms
Four to 10 days after the initial phase of illness, the late symptoms of hantavirus pulmonary syndrome appear. These include coughing and shortness of breath, with the sensation of, as one survivor put it, a “tight band around my chest and a pillow over my face” as the lungs fill with fluid.
Late symptoms:
- A cough that produces secretions
- Shortness of breath
- Fluid accumulating within the lungs
- Low blood pressure
- Reduced heart efficiency
Hantavirus pulmonary syndrome complications
Hantavirus pulmonary syndrome can quickly become life-threatening. As the lungs fill with fluid, it becomes more and more difficult to breathe. Blood pressure drops and organs begin to fail, particularly the heart. Depending on the hantavirus strain, the mortality rate for the North American variety of hantavirus pulmonary syndrome can be more than 30 percent.
Hantavirus pulmonary syndrome diagnosis
Diagnosing hantavirus pulmonary syndrome in an individual who has only been infected a few days is difficult, because early symptoms such as fever, muscle aches, and fatigue are easily confused with influenza. However, if the individual is experiencing fever and fatigue and has a history of potential rural rodent exposure, together with shortness of breath, would be strongly suggestive of hantavirus pulmonary syndrome. If the individual is experiencing these symptoms they should see their physician immediately and mention their potential rodent exposure.
Hantavirus pulmonary syndrome treatment
There is no specific treatment, cure, or vaccine for hantavirus infection. However, doctors do know that if infected individuals are recognized early and receive medical care in an intensive care unit, they may do better. In intensive care, patients are intubated and given oxygen therapy to help them through the period of severe respiratory distress.
The earlier the patient is brought in to intensive care, the better. If a patient is experiencing full distress, it is less likely the treatment will be effective.
Therefore, if you have been around rodents and have symptoms of fever, deep muscle aches, and severe shortness of breath, see your doctor immediately. Be sure to tell your doctor that you have been around rodents—this will alert your physician to look closely for any rodent-carried disease, such as hantavirus pulmonary syndrome.
Supportive therapy
People with severe cases need immediate treatment in an intensive care unit. Intubation and mechanical ventilation may be needed to support breathing and to help manage fluid in the lungs (pulmonary edema). Intubation involves placing a breathing tube through your nose or mouth into the windpipe (trachea) to help keep your airways open and functioning.
Blood oxygenation
In extremely severe cases of pulmonary distress, you’ll need a method called extracorporeal membrane oxygenation to help ensure you retain a sufficient supply of oxygen. This involves continuously pumping your blood through a machine that removes carbon dioxide and adds oxygen. The oxygenated blood is then returned to your body.
- https://www.cdc.gov/hantavirus/technical/hanta/virology.html[↩][↩]
- Spiropoulou CF, Srikiatkhachorn A. The role of endothelial activation in dengue hemorrhagic fever and hantavirus pulmonary syndrome. Virulence. 2013;4(6):525-536. doi:10.4161/viru.25569. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5359750/[↩][↩]
- Schmaljohn CS, Nichol ST. Bunyaviridae. In: Knipe DM, Howley PM, eds. Fields Virology. 5th ed. Philadelphia, Pa: Lippincott-Raven, 2007:1741-89.[↩]
- Nichol ST, Spiropoulou CF, Morzunov S, Rollin PE, Ksiazek TG, Feldmann H, et al. . Genetic identification of a hantavirus associated with an outbreak of acute respiratory illness. Science 1993; 262:914 – 7; http://dx.doi.org/10.1126/science.8235615 https://www.ncbi.nlm.nih.gov/pubmed/8235615[↩]
- Hjelle B, Torres-Pérez F. Hantaviruses in the americas and their role as emerging pathogens. Viruses 2010; 2:2559 – 86; http://dx.doi.org/10.3390/v2122559 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185593/[↩][↩]
- Jonsson CB, Hooper J, Mertz G. Treatment of hantavirus pulmonary syndrome. Antiviral Res 2008; 78:162 – 9; http://dx.doi.org/10.1016/j.antiviral.2007.10.012 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2810485/[↩]
- Schmaljohn C, Hjelle B. Hantaviruses: a global disease problem. Emerg Infect Dis 1997; 3:95 – 104; http://dx.doi.org/10.3201/eid0302.970202 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627612/[↩]
- Centers for Disease Control and Prevention (CDC). Hantavirus pulmonary syndrome in visitors to a national park–Yosemite Valley, California, 2012. MMWR Morb Mortal Wkly Rep 2012; 61:952 https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a5.htm[↩]
- Dolgin E. Hantavirus treatments advance amidst outbreak in US park. Nat Med 2012; 18:1448; http://dx.doi.org/10.1038/nm1012-1448a https://www.ncbi.nlm.nih.gov/pubmed/23042337[↩]
- https://phil.cdc.gov/Details.aspx?pid=12734[↩]