Contents
What is helicobacter pylori
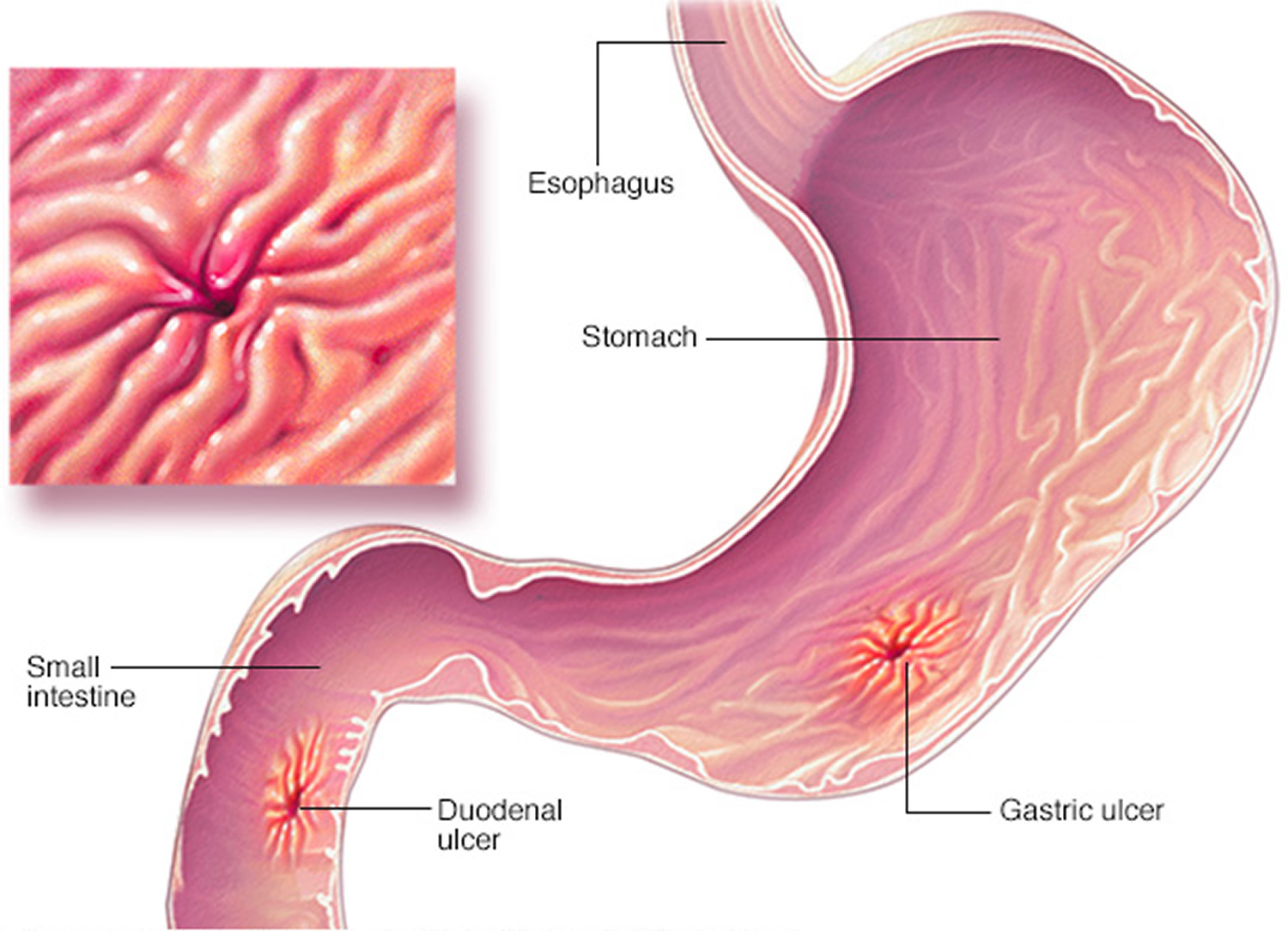
Helicobacter pylori (H. pylori) is a spiral-shaped bacterium that grows in the mucus layer that coats the inside of the human stomach, in the acidic environment of the stomach (Figure 1). The human body has no natural immune response to Helicobacter pylori, which causes inflammation and ulcers within the stomach. Helicobacter pylori is a common gastrointestinal bacterial strain closely associated with the incidence of chronic gastritis (the irritation and inflammation of the stomach lining), peptic ulcers (sores in the lining of the stomach, small intestine, or esophagus), gastric mucosa-associated lymphoid tissue lymphoma, and gastric cancer later in life.
In 1982, two Australian scientists discovered that a certain bacterium, Helicobacter pylori, was a common cause of persistent stomach inflammation and stomach ulcers. This realization revolutionized ulcer treatment. These bacteria are found worldwide, but especially in developing countries, where up to 10% of children and 80% of adults are likely to have had an Helicobacter pylori infection — usually without any symptoms.
To survive in the harsh, acidic environment of the stomach, Helicobacter pylori secretes an enzyme called urease, which converts the chemical urea to ammonia. The production of ammonia around Helicobacter pylori neutralizes the acidity of the stomach, making it more hospitable for the bacterium. In addition, the helical shape of Helicobacter pylori allows it to burrow into the mucus layer, which is less acidic than the inside space, or lumen, of the stomach. Helicobacter pylori can also attach to the cells that line the inner surface of the stomach.
Although immune cells that normally recognize and attack invading bacteria accumulate near sites of Helicobacter pylori infection, they are unable to reach the stomach lining. In addition, Helicobacter pylori has developed ways of interfering with local immune responses, making them ineffective in eliminating this bacterium 1.
Helicobacter pylori has coexisted with humans for many thousands of years, and infection with this bacterium is common. The Centers for Disease Control and Prevention (CDC) estimates that approximately two-thirds of the world’s population harbors the bacterium, with infection rates much higher in developing countries than in developed nations.
In 1994, the International Agency for Research on Cancer classified Helicobacter pylori as a carcinogen, or cancer-causing agent, in humans. Since then, it has been increasingly accepted that colonization of the stomach with Helicobacter pylori is an important cause of gastric cancer and of gastric mucosa-associated lymphoid tissue (MALT) lymphoma. Infection with Helicobacter pylori is also associated with a reduced risk of esophageal adenocarcinoma.
While fairly common, helicobacter pylori infection usually causes no symptoms and does not cause illness in most infected people, but Helicobacter pylori can sometimes lead to ulcers in the stomach or the very first part of the small intestine (duodenum), and to certain types of stomach cancer. There is also evidence linking Helicobacter pylori infection to other conditions like iron-deficiency anemia and vitamin B12 deficiency. The Helicobacter pylori bacteria are thought to spread through contaminated water, vomit, or feces and through direct mouth-to-mouth contact. Most infections are acquired in childhood and often within families, especially in developing countries. Helicobacter pylori infection is more likely in children living in poverty, in crowded conditions, and in areas with poor sanitation.
There is no vaccine for Helicobacter pylori. Since Helicobacter pylori might spread through unclean food and water, you might be able to prevent it if you
- Wash your hands after using the bathroom and before eating
- Eat properly prepared food
- Drink water from a clean, safe source
Most people don’t realize they have Helicobacter pylori infection, because they never get sick from it. If you develop signs and symptoms of a peptic ulcer, your doctor will probably test you for Helicobacter pylori infection. If you have Helicobacter pylori infection, it can be treated with antibiotics.
Figure 1. Helicobacter pylori bacteria
Helicobacter pylori gastritis
Gastritis is inflammation or irritation of the stomach lining. It can be caused by some medicines (such as aspirin or other anti-inflammatory medicines), overuse of alcohol, stomach acid, or bacterial infection.
An infection with the bacteria Helicobacter pylori can cause gastritis. Helicobacter pylori is also the bacteria that causes ulcers.
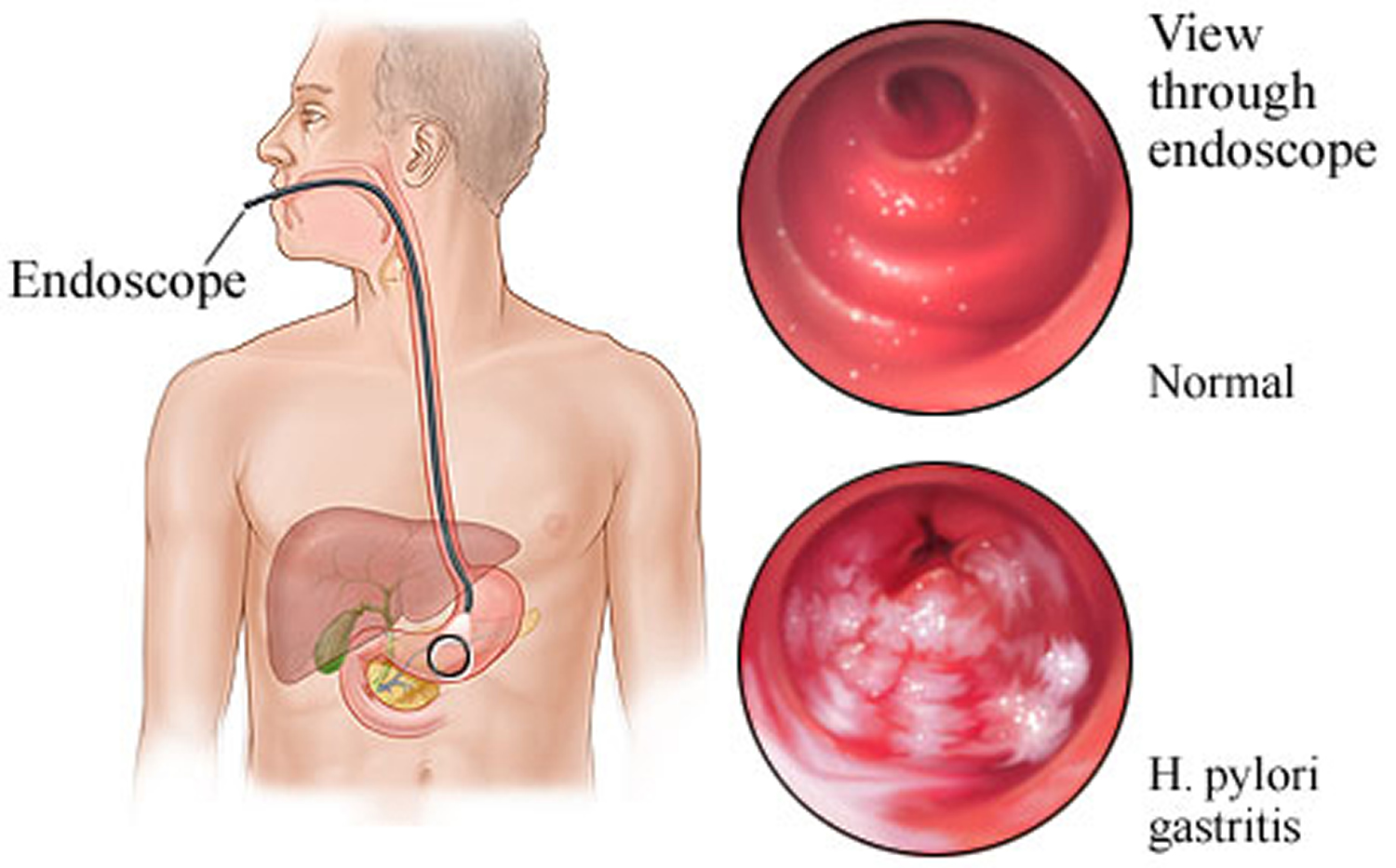
One way to test for Helicobacter pylori is to take a tissue sample from the stomach. The doctor uses a thin, flexible, lighted viewing instrument (endoscope) to look down your throat and into your stomach. Looking through the endoscope, your doctor may also see irritation or inflammation in the lining of your stomach. This irritation is gastritis. And a tissue sample will tell the doctor if the cause is Helicobacter pylori.
Figure 2. Helicobacter pylori gastritis
Helicobacter pylori infection causes
The exact way Helicobacter pylori infects someone is still unknown. Helicobacter pylori bacteria may be passed from person to person through direct contact with saliva, vomit or fecal matter. Helicobacter pylori may also be spread through contaminated food or water.
Risk factors for Helicobacter pylori infection
Helicobacter pylori is often contracted in childhood. Risk factors for Helicobacter pylori infection are related to living conditions in your childhood, such as:
- Living in crowded conditions. You have a greater risk of Helicobacter pylori infection if you live in a home with many other people.
- Living without a reliable supply of clean water. Having a reliable supply of clean, running water helps reduce the risk of Helicobacter pylori.
- Living in a developing country. People living in developing countries, where crowded and unsanitary living conditions may be more common, have a higher risk of Helicobacter pylori infection.
- Living with someone who has an Helicobacter pylori infection. If someone you live with has Helicobacter pylori, you’re more likely to also have Helicobacter pylori.
Helicobacter pylori prevention
In areas of the world where Helicobacter pylori infection and its complications are common, doctors sometimes test healthy people for Helicobacter pylori. Whether there is a benefit to treating Helicobacter pylori when you have no signs or symptoms of infection is controversial among doctors.
If you’re concerned about Helicobacter pylori infection or think you may have a high risk of stomach cancer, talk to your doctor. Together you can decide whether you may benefit from Helicobacter pylori screening.
Helicobacter pylori symptoms
Most people with Helicobacter pylori infection will never have any signs or symptoms. It’s not clear why this is, but some people may be born with more resistance to the harmful effects of Helicobacter pylori.
When signs or symptoms do occur with Helicobacter pylori infection, they may include:
- An ache or burning pain in your abdomen
- Abdominal pain that’s worse when your stomach is empty
- Nausea
- Loss of appetite
- Frequent burping
- Bloating
- Unintentional weight loss
Helicobacter pylori complications
Complications associated with Helicobacter pylori infection include:
- Ulcers. Helicobacter pylori can damage the protective lining of your stomach and small intestine. This can allow stomach acid to create an open sore (ulcer). About 10 percent of people with Helicobacter pylori will develop an ulcer.
- Helicobacter pylori gastritis (inflammation of the stomach lining). Helicobacter pylori infection can irritate your stomach, causing inflammation (gastritis).
- Stomach cancer. Helicobacter pylori infection is a strong risk factor for certain types of stomach cancer.
Helicobacter pylori diagnosis
Tests and procedures used to determine whether you have an Helicobacter pylori infection include:
Helicobacter pylori test
The Helicobacter pylori infection can be detected by submitting a stool sample (stool antigen test) or by using a device to measure breath samples after swallowing a urea pill (urea breath test). For both of these tests to be reliable, it is important to stop taking acid-reducing medications called proton pump inhibitors (like Prilosec, Nexium, Protonix) for two weeks, and to avoid any bismuth products (like Pepto-Bismol) or antibiotics for four weeks before the test. Blood tests (serology or antibody test) are no longer recommended for most people because there are more false positives (abnormal test result when you may not have the infection), and this blood test can’t help tell whether you’ve had the infection in the past or have a current active infection. If you have specific risk factors for stomach cancer, your doctor may recommend starting with an upper endoscopy. For this test, a flexible tube with a camera is passed through the mouth and into the digestive tract. During an endoscopy the doctor can take tissue samples (biopsies) if necessary, as well as do Helicobacter pylori testing.
Helicobacter pylori breath test
During a breath test, you swallow a pill, liquid or pudding that contains tagged carbon molecules. If you have an Helicobacter pylori infection, carbon is released when the solution is broken down in your stomach.
Your body absorbs the carbon and expels it when you exhale. You exhale into a bag, and your doctor uses a special device to detect the carbon molecules.
Acid-suppressing drugs known as proton pump inhibitors (PPIs), bismuth subsalicylate (Pepto-Bismol) and antibiotics can interfere with the accuracy of this test. Your doctor will ask you to stop taking those medications for a week or two weeks before you have the test. This test is available for adults and children.
Helicobacter pylori stool antigen test
In this test, a stool (feces) sample is used to determine if Helicobacter pylori antigens are present in your gastrointestinal (GI) system. Antigens are substances that trigger the immune system to fight infection.
A doctor may request an Helicobacter pylori antigen stool test if you have symptoms that could indicate the presence of a peptic ulcer, such as indigestion, abdominal pain, a full or bloated feeling, nausea, frequent belching, or vomiting. A test also might be ordered after you complete a course of antibiotics for Helicobacter pylori to determine whether it eradicated the infection.
Preparation
Unlike most other lab tests, a stool sample is often collected by patients at home, not by health care professionals at a hospital or clinic. For 2 weeks before the test, you may be asked to avoid certain medications such as antibiotics, antacids, bismuth, and peptic ulcer medicines such as proton pump inhibitors (PPIs) and H2 blockers.
Procedure
The doctor or hospital laboratory usually will provide written instructions on how to collect a stool sample. If instructions aren’t provided, here are tips for collecting a stool sample:
- Be sure to wear protective gloves and wash your hands afterward.
- A hat-shaped plastic lid is used to collect the stool specimen. This catching device can be quickly placed over a toilet bowl, to collect the sample. Using a catching device can prevent contamination of the stool by water and dirt. Another way to collect a stool sample is to loosely place plastic wrap over the seat of the toilet. Then place the stool sample in a clean, sealable container before taking it to the lab.
- Your shouldn’t urinate into the container. If possible, empty your bladder before a bowel movement.
- The stool should be collected into clean, dry plastic jars with screw-cap lids. For best results, the stool should be brought to the lab right away. If this isn’t possible, the stool should be refrigerated and then taken to the lab as soon as possible.
What to Expect
When the sample arrives at the laboratory, a small amount of stool is placed in tiny vials. Specific chemicals and a color developer are added. At the end of the test, the presence of a blue color indicates the presence of Helicobacter pylori antigens.
Getting the Results
In general, the result of the Helicobacter pylori stool test is reported in 1-4 days.
Helicobacter pylori scope test
You’ll be sedated for this test, known as an upper endoscopy exam. During the exam, your doctor threads a long flexible tube equipped with a tiny camera (endoscope) down your throat and esophagus and into your stomach and duodenum. This instrument allows your doctor to view any irregularities in your upper digestive tract and remove tissue samples (biopsy).
These samples are analyzed for Helicobacter pylori infection. This test isn’t generally recommended solely to diagnose an Helicobacter pylori infection because it’s more invasive than a breath or stool test, but it may be used to diagnose Helicobacter pylori ulcers or if it’s needed to rule out other digestive conditions.
Should everyone be tested for Helicobacter pylori?
No, not everyone. You should be tested if you have ongoing dyspepsia (discomfort or pain in the upper abdomen) or if you have an associated condition like peptic ulcers or stomach cancer. Testing for H. pylori is not needed for typical symptoms of acid reflux (heartburn).
In a recent guideline update, the American College of Gastroenterology also suggests Helicobacter pylori testing if you are on long-term aspirin therapy or starting long-term NSAID therapy (e.g., ibuprofen, naproxen) to help reduce the risk of developing ulcers and gastrointestinal bleeding. A Chinese study showed that patients with a history of bleeding ulcers and Helicobacter pylori infection who were also on low-dose aspirin were less likely to experience a recurrence of stomach bleeding when the infection was treated. Studies on patients taking NSAIDs have had mixed results. An analysis of the combined results of several of these studies showed that treating Helicobacter pylori infection reduced the number of ulcers in patients starting NSAID therapy, but not for patients already taking these medications. It’s important to keep in mind that these studies don’t provide the most definitive data. Scientists don’t know that testing everyone taking aspirin or NSAIDs long-term is cost-effective, so it’s best to talk with your doctor. Together you can determine your personal risk of ulcer bleeding against the cost and inconvenience of testing and risks of taking antibiotics.
Helicobacter pylori treatment
Treatment for Helicobacter pylori infection is challenging. Helicobacter pylori infections are usually treated with at least two different antibiotics at once, to help prevent the bacteria from developing a resistance to one particular antibiotic. Your doctor also will prescribe or recommend an acid-suppressing drug, to help your stomach lining heal.
Drugs that can suppress acid include:
- Proton pump inhibitors (PPIs). These drugs stop acid from being produced in the stomach. Some examples of PPIs are omeprazole (Prilosec, others), esomeprazole (Nexium, others), lansoprazole (Prevacid, others) and pantoprazole (Protonix, others).
- Histamine (H-2) blockers. These medications block a substance called histamine, which triggers acid production. Examples include cimetidine (Tagamet) and ranitidine (Zantac).
- Bismuth subsalicylate. More commonly known as Pepto-Bismol, this drug works by coating the ulcer and protecting it from stomach acid.
Your doctor may recommend that you undergo testing for Helicobacter pylori at least four weeks after your treatment. If the tests show the treatment was unsuccessful, you may undergo another round of treatment with a different combination of antibiotic medications.
Helicobacter pylori treatment usually involves taking a combination of three or four medications multiple times a day for 14 days. And rising antibiotic resistance has made it increasingly difficult to cure the infection.
The treatment is roughly 80% effective in getting rid of the infection, but the cure rate depends on picking the right combination of medications, taking them correctly, and finishing the full course of treatment. Your doctor will factor in what the antibiotic resistance pattern is like in your region, as well as any drug allergies you might have and other medications you take, to avoid a drug interaction. Another important consideration is what antibiotics you have taken in the past for other infections. It is best to avoid ones you have already used often, as it is more likely the Helicobacter pylori will be resistant to these.
Most experts recommend testing four or more weeks after treatment ends to confirm the infection is cured. If it isn’t, this means trying another therapy with a different combination of antibiotics. After one or more treatment failures, it may be time to have an endoscopy to obtain a culture and identify exactly which antibiotics will kill the bacteria.
If you have a condition associated with Helicobacter pylori infection or are at risk for stomach ulcers, talk to your doctor about whether testing is right for you. Testing correctly is important to reliably diagnose the infection and avoid unnecessary treatment.
Helicobacter pylori diet
Researchers have not found that diet and nutrition play an important role in causing or preventing peptic ulcers. Before acid blocking drugs became available, milk was used to treat ulcers. However, milk is not an effective way to prevent or relieve a peptic ulcer.
Alcohol and smoking do contribute to ulcers and should be avoided.
- Atherton JC. The pathogenesis of Helicobacter pylori-induced gastro-duodenal diseases. Annual Review of Pathology 2006; 1:63–96. https://www.ncbi.nlm.nih.gov/pubmed/18039108[↩]