Contents
- What is Hepatitis C
- What is acute hepatitis C?
- What is chronic hepatitis C?
- What is the likelihood of hepatitis C virus infection becoming chronic?
- Why do most people remain chronically infected with hepatitis C virus?
- Is it possible for someone to become infected with hepatitis C virus and then spontaneously clear the infection?
- How common is hepatitis C in the United States?
- Who is at risk for hepatitis C infection?
- Should I be screened for hepatitis C?
- Who should be tested for hepatitis C virus on a routine basis?
- How many new hepatitis C infections occur annually in the United States?
- What is the prevalence of hepatitis C among people who inject drugs?
- What is the risk of acquiring hepatitis C from transfused blood or blood products in the United States?
- Can hepatitis C be spread within a household?
- Can hepatitis C be spread during medical or dental procedures?
- Do hepatitis C outbreaks occur in health care settings?
- How can I protect myself from hepatitis C infection?
- Complications of Hepatitis C virus (HCV) Infection
- How do doctors treat the complications of hepatitis C?
- What are the chances of someone with hepatitis C virus infection developing cirrhosis or liver cancer?
- What are the chances of someone developing chronic Hepatitis C virus (HCV) infection, chronic liver disease, cirrhosis, or liver cancer or dying as a result of hepatitis C?
- Who is more likely to develop cirrhosis after becoming infected with hepatitis C virus?
- Is hepatitis C a common cause for liver transplantation?
- How many deaths can be attributed to chronic hepatitis C virus infection?
- How many different genotypes of hepatitis C virus exist?
- Which hepatitis C virus genotypes are found in the United States?
- Can superinfection with more than one hepatitis C virus genotype occur?
- Can people become infected with a different strain of hepatitis C virus after they have cleared the initial infection?
- Hepatitis C causes
- How is Hepatitis C transmitted?
- What is the prevalence of Hepatitis C virus infection among injection drug users?
- Is cocaine use associated with hepatitis C virus transmission?
- Who is at risk for Hepatitis C virus infection?
- What is the risk of acquiring hepatitis C virus infection from transfused blood or blood products in the United States ?
- Can hepatitis C virus be spread during medical or dental procedures ?
- Can hepatitis C virus be spread within a household ?
- Hepatitis C prevention
- Hepatitis C symptoms
- Hepatitis C complications
- How is hepatitis C infection diagnosed?
- Screening for Hepatitis C
- Blood tests to detect hepatitis C virus infection
- Hepatitis C virus test results interpretation
- Tests for liver damage
- How soon after exposure to hepatitis C virus can anti-HCV (hepatitis C virus antibody) be detected?
- Is an hepatitis C virus antibody (anti-HCV) test sufficient to diagnose current hepatitis C virus infection?
- Is someone with a positive anti-hepatitis C virus (anti-HCV) test still at risk for hepatitis C?
- Under what circumstances might a false-negative hepatitis C virus antibody (anti-HCV) test result occur, even when a person has been exposed to hepatitis C virus?
- How soon after exposure to hepatitis C virus can hepatitis C virus RNA be detected?
- Under what circumstances is a false-positive anti-hepatitis C virus test result likely?
- Can a patient have a normal liver enzyme (e.g., ALT) level and still have chronic hepatitis C?
- Hepatitis C Treatment
- Antiviral medications
- Liver transplantation
- Vaccinations
- Is it necessary to do viral genotyping when managing a person with chronic hepatitis C?
- Can superinfection with more than one genotype of hepatitis C virus occur?
- Should patients with acute hepatitis C receive treatment?
- What is the treatment for chronic hepatitis C?
- Does chronic hepatitis C affect only the liver?
- Are patients undergoing treatment for hepatitis C at risk for reactivation of an existing hepatitis B virus infection? How are these patients managed?
- Lifestyle and home remedies for Hepatitis C infection
- Pregnancy and Hepatitis C virus Infection
- Should pregnant women be routinely tested for anti-hepatitis C virus?
- What is the risk that an hepatitis C virus-infected mother will spread hepatitis C virus to her infant during birth?
- Should a woman with hepatitis C virus infection be advised against breastfeeding?
- Is it safe for a mother infected with hepatitis C virus to breastfeed her infant?
- Is it safe for the hepatitis C virus-positive mother to breastfeed if her nipples are cracked and bleeding?
- When should children born to hepatitis C virus-infected mothers be tested to see if they were infected at birth ?
- Hepatitis C prognosis
What is Hepatitis C
Hepatitis C is a liver infection caused by the Hepatitis C virus (HCV). Hepatitis C is a blood-borne virus – it usually spreads through contact with infected blood 1. Today, most people become infected with the Hepatitis C virus by sharing needles or other equipment to inject drugs. However, hepatitis C virus can also spread through sex with an infected person and from mother to baby during childbirth. The Centers for Disease Control and Prevention (CDC) now recommends universal hepatitis C screening for all U.S. adults and all pregnant women during every pregnancy, except in settings where the prevalence of hepatitis C virus infection is <0.1% 2.
You can’t get hepatitis C from 3:
- being coughed or sneezed on by an infected person
- drinking water or eating food
- hugging an infected person
- shaking hands or holding hands with an infected person
- sharing spoons, forks, and other eating utensils
- sitting next to an infected person
A baby can’t get hepatitis C from breast milk 4.
Hepatitis C can be acute or chronic:
- Acute hepatitis C is a short-term infection. The symptoms can last up to 6 months. Sometimes your body is able to fight off the infection and the virus goes away. But for most people, an acute infection leads to chronic infection.
- Chronic hepatitis C is a long-lasting infection. If it is not treated, it can last for a lifetime and cause serious health problems, including liver damage, cirrhosis (scarring of the liver), liver cancer, and even death.
In 2019, a total of 4,136 cases of acute hepatitis C were were reported to Centers for Disease Control and Prevention (CDC) 5. The overall incidence rate for acute hepatitis C in 2019 was 1.3 cases per 100,000 population, an increase from 2010–2012 5. After adjusting for under-ascertainment and under-reporting, an estimated 57,500 acute hepatitis C cases occurred in 2019 5. Since 2006, the number of new hepatitis C infections has been rising, especially among people younger than age 30 who inject heroin or misuse prescription opioids and inject them 6, 7.
Most people who are infected with hepatitis C don’t have any symptoms for years. Hepatitis C can cause an acute (short-term) or chronic (long-term) infection. For some people, hepatitis C is a short-term illness but for 70%–85% of people who become infected with Hepatitis C, it becomes a long-term, chronic infection 8. Chronic Hepatitis C is a serious disease than can result in long-term health problems, even death. The majority of infected persons might not be aware of their infection because they are not clinically ill. If you do get symptoms, you may feel as if you have the flu. You may also have jaundice, a yellowing of skin and eyes, dark-colored urine, and pale bowel movements. Many people with hepatitis C don’t know they have it. That’s mainly because hepatitis C symptoms can take decades to appear. So, the U.S. Preventive Services Task Force and the U.S. Centers for Disease Control and Prevention (CDC) recommend that all adults ages 18 to 79 years and all pregnant women during every pregnancy be screened for hepatitis C 9, 10. Screening is for everyone, even those who don’t have symptoms or known liver disease. The largest group at risk includes everyone born between 1945 and 1965 — a population five times more likely to be infected than those born in other years. A blood test can tell if you have Hepatitis C virus (HCV). Usually, hepatitis C does not get better by itself. The Hepatitis C virus (HCV) infection can last a lifetime and may lead to cirrhosis (scarring of the liver), liver failure or liver cancer. Medicines sometimes help, but side effects can be a problem. Serious cases may need a liver transplant.
There is no vaccine for Hepatitis C. The best way to prevent Hepatitis C is by avoiding behaviors that can spread the disease, especially injecting drugs.
- There is currently NO Hepatitis C vaccine. Development of a vaccine for hepatitis C has been challenging, because the virus has multiple genotypes and subtypes and mutates rapidly, allowing it to evade the immune system. However, research into the development of a vaccine is under way 11.
If you have hepatitis C, talk with your doctor about treatment. Today, chronic hepatitis C virus infection is usually curable with oral medications taken every day for two to six months 12, 13.
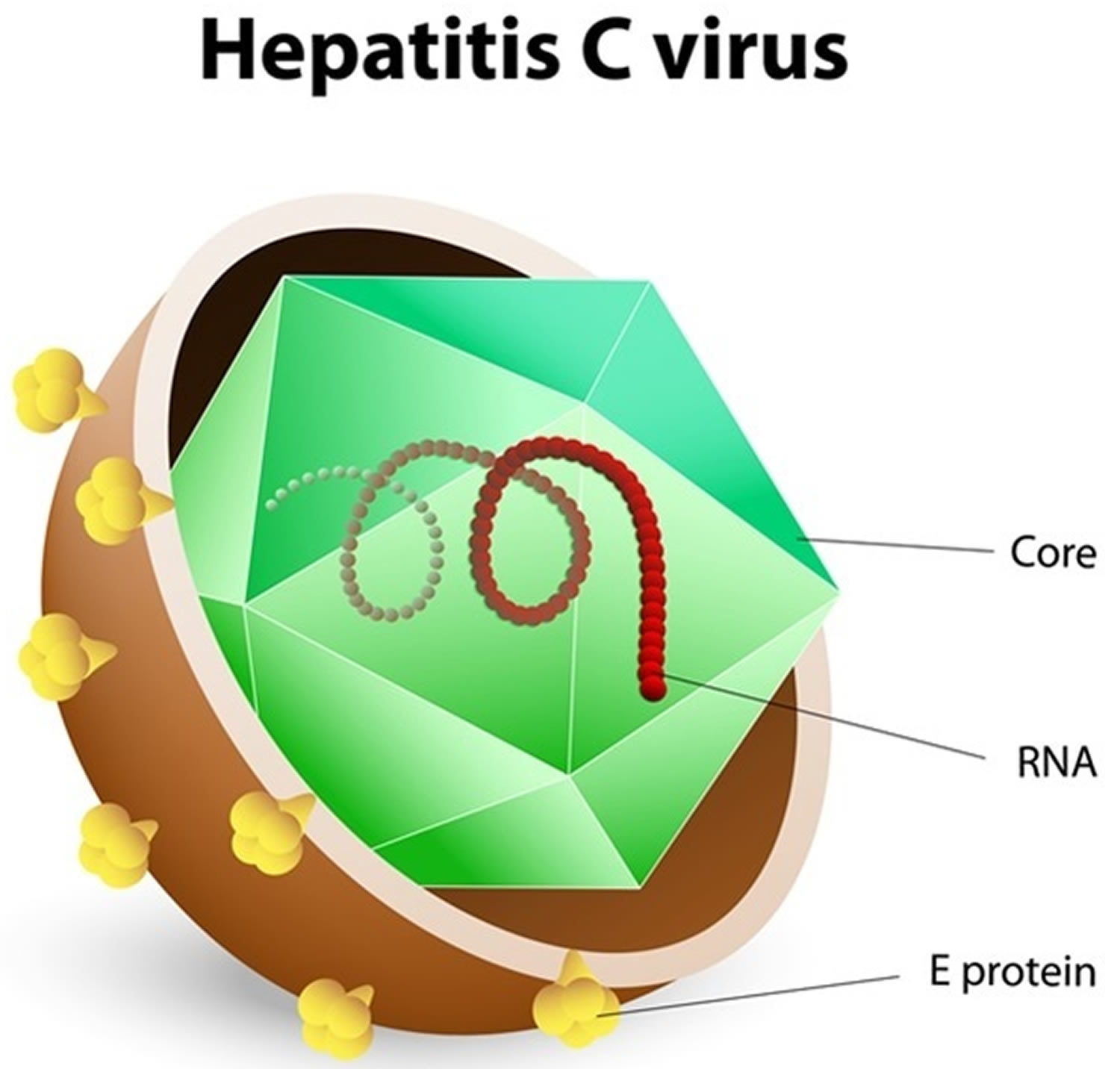
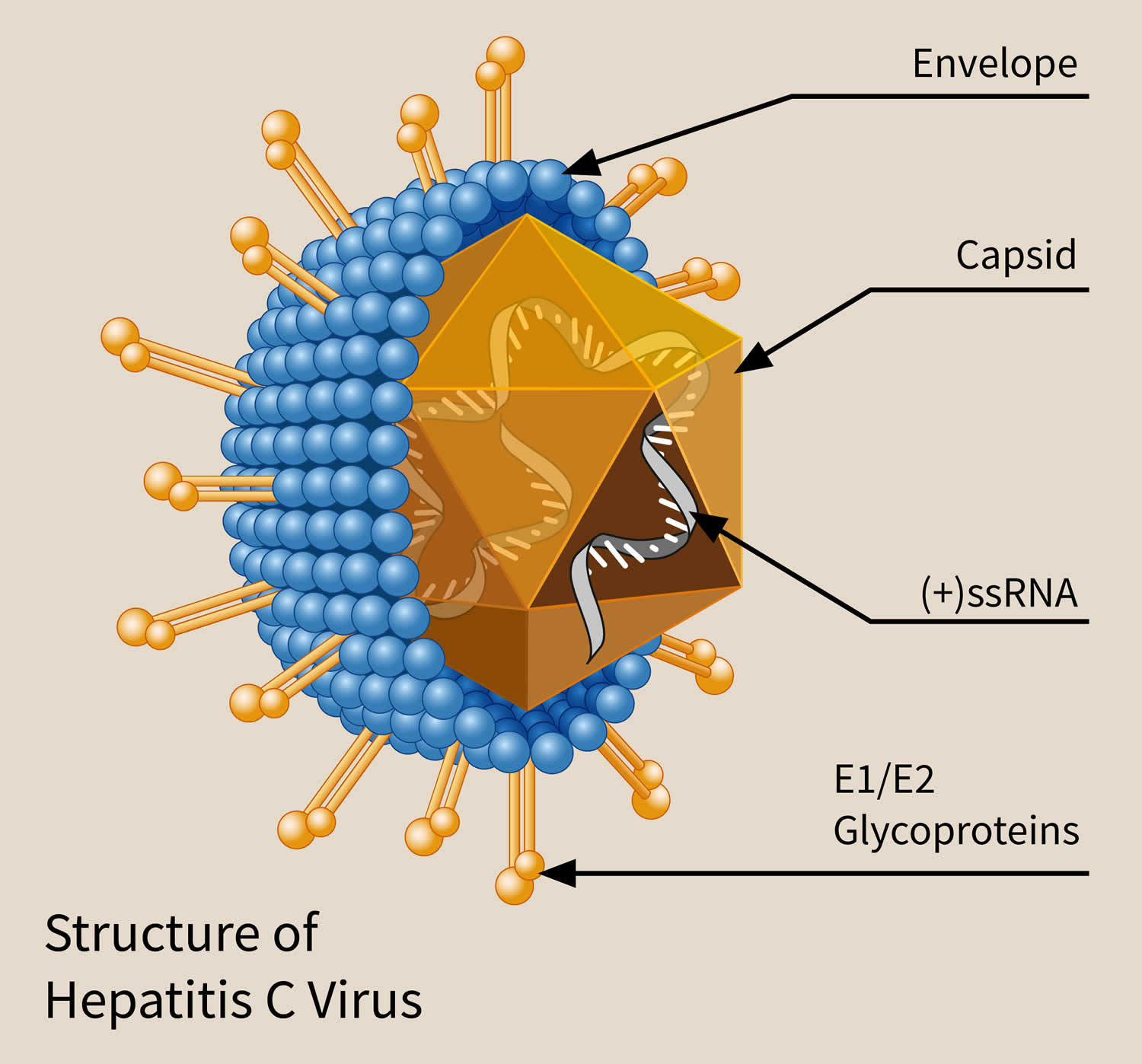
Figure 1. Hepatitis C virus
What is acute hepatitis C?
Acute hepatitis C is a short-term infection. Symptoms can last up to 6 months. Sometimes your body is able to fight off the infection and the virus goes away.
What is chronic hepatitis C?
Chronic hepatitis C is a long-lasting infection. Chronic hepatitis C occurs when your body isn’t able to fight off the virus. About 75 to 85 percent of people with acute hepatitis C will develop chronic hepatitis C 8. An estimated 2.4 million people in the United States were living with chronic hepatitis C infection during 2013–2016 14.
Early diagnosis and treatment of chronic hepatitis C can prevent liver damage. Without treatment, chronic hepatitis C can cause chronic liver disease, cirrhosis, liver failure, or liver cancer.
What is the likelihood of hepatitis C virus infection becoming chronic?
More than half of people who become infected with hepatitis C virus will develop chronic hepatitis C infection 15, 16.
Why do most people remain chronically infected with hepatitis C virus?
A person infected with hepatitis C virus mounts an immune response to the virus, but replication of the virus during infection can result in changes that evade the immune response. This may explain how the virus establishes and maintains chronic infection 15.
Is it possible for someone to become infected with hepatitis C virus and then spontaneously clear the infection?
Yes. Recent data reveal that up to approximately half of people who test anti-hepatitis C virus positive do not have current chronic infection, indicating they may have experienced spontaneous clearance after acute infection 17. Only those with current infection as evidenced by a positive hepatitis C virus (HCV) RNA test need treatment. Factors that are predictive of spontaneous clearance of hepatitis C virus (HCV) include having jaundice, elevated ALT level, and hepatitis B virus surface antigen (HBsAg) positivity; younger age, being female; being infected with hepatitis C virus genotype 1; and having certain host genetic polymorphisms, most notably those near the IL28B gene 18, 19.
How common is hepatitis C in the United States?
In the United States, hepatitis C is the most common chronic viral infection found in blood and spread through contact with blood 10.
Researchers estimate that about 2.7 million to 3.9 million people in the United States have chronic hepatitis C 8. Many people who have hepatitis C don’t have symptoms and don’t know they have this infection.
Since 2006, the number of new hepatitis C infections has been rising, especially among people younger than age 30 who inject heroin or misuse prescription opioids and inject them 6, 7.
Who is at risk for hepatitis C infection?
The following people are at increased risk for hepatitis C:
- People with HIV infection
- Current or former people who use injection drugs, including those who injected only once many years ago
- People with selected medical conditions, including those who ever received maintenance hemodialysis 20
- Prior recipients of transfusions or organ transplants, including people who received clotting factor concentrates produced before 1987, people who received a transfusion of blood or blood components before July 1992, people who received an organ transplant before July 1992, and people who were notified that they received blood from a donor who later tested positive for hepatitis C virus infection
- Health care, emergency medical, and public safety personnel after needle sticks, sharps, or mucosal exposures to hepatitis C virus-positive blood
- Children born to mothers with hepatitis C virus infection
In the United States, injecting drugs is the most common way that people get hepatitis C 8.
Should I be screened for hepatitis C?
Doctors usually recommend one-time screening of all adults ages 18 to 79 for hepatitis C 9, 10. Screening is testing for a disease in people who have no symptoms. Doctors use blood tests to screen for hepatitis C. Many people who have hepatitis C don’t have symptoms and don’t know they have hepatitis C. Screening tests can help doctors diagnose and treat hepatitis C before it causes serious health problems.
The U.S. Preventive Services Task Force recommends that all adults ages 18 to 79 years get a blood test to screen for hepatitis C infection, even those without symptoms or known liver disease 10. Screening for hepatitis C virus is especially important if you’re at high risk of exposure, including:
- Persons who have ever injected illegal drugs, including those who injected only once many years ago or inhaled illicit drugs
- Anyone who has abnormal liver function test results with no identified cause
- Babies born to mothers with hepatitis C (to avoid detecting maternal antibody, these children should not be tested before age 18 months)
- Persons with known exposures to hepatitis C virus, such as:
- health care workers after needlesticks involving hepatitis C virus-positive blood
- recipients of blood or organs from a donor who later tested hepatitis C virus-positive
- People with hemophilia who were treated with clotting factors before 1987
- People who have ever undergone long-term hemodialysis treatments
- People who received blood transfusions or organ transplants before 1992
- Sexual partners of anyone diagnosed with hepatitis C infection
- People with HIV infection
- Anyone born from 1945 to 1965
- Anyone who has been in prison
- All pregnant women during each pregnancy
- Children born to mothers with hepatitis C virus infection
- People who were notified that they received blood from a donor who later tested positive for hepatitis C virus infection
- Health care, emergency medical, and public safety personnel after needle sticks, sharps, or mucosal exposures to hepatitis C virus‑positive blood
- Any person who requests hepatitis C testing
Who should be tested for hepatitis C virus on a routine basis?
Routine periodic testing is recommended for people with ongoing risk factors, while risk factors persist, including those who currently inject drugs and share needles, syringes, or other drug preparation equipment, along with people who have certain medical conditions (e.g., people who ever received maintenance hemodialysis). Testing of people at risk should occur regardless of setting prevalence.
How many new hepatitis C infections occur annually in the United States?
In 2018, a total of 3,621 cases of acute hepatitis C were reported to CDC 21. After adjusting for under-ascertainment and under-reporting, an estimated 50,300 acute hepatitis C cases occurred in 2018. More information on hepatitis C surveillance is available from CDC (https://www.cdc.gov/hepatitis/statistics/2019surveillance/index.htm).
What is the prevalence of hepatitis C among people who inject drugs?
No nationwide seroprevalence surveys targeting people who inject drugs have been conducted in the United States, and estimates based on smaller surveys in regional and metropolitan areas vary considerably. A 2017 review estimated an overall hepatitis C prevalence of about 53% among people who inject drugs in the United States, which varies from state to state (range: 38.1%–68.0%) 22.
What is the risk of acquiring hepatitis C from transfused blood or blood products in the United States?
Now that more advanced screening tests for hepatitis C are used in blood banks, the risk of transmission to recipients of blood or blood products is considered extremely rare, at <1 case per 2 million units transfused. Before 1992 (the year that blood screening became available), blood transfusion was a leading cause of hepatitis C virus transmission 23.
Can hepatitis C be spread within a household?
Yes; however, transmission between household members does not occur very often. If hepatitis C is spread within a household, it is most likely a result of direct (i.e., parenteral or percutaneous) exposure to the blood of an infected household member.
Can hepatitis C be spread during medical or dental procedures?
As long as Standard Precautions and other infection-control practices are consistently implemented, medical and dental procedures performed in the United States generally do not pose a risk for the spread of hepatitis C. Standard Precautions are based on a risk assessment and make use of common sense practices and personal protective equipment use that protect healthcare providers from infection and prevent the spread of infection from patient to patient 24. However, hepatitis C can be spread in health-care settings when injection equipment, such as syringes, is shared between patients or when injectable medications or intravenous solutions are mishandled and become contaminated with blood. Health-care personnel should understand and adhere to Standard Precautions, which include maintaining injection safety practices aimed at reducing bloodborne pathogen risks for patients and health-care personnel. Cases of suspected health-care-associated hepatitis C virus infection should be reported to state and local public health authorities for prompt investigation and response.
Do hepatitis C outbreaks occur in health care settings?
Yes. Hepatitis C can be spread in health-care settings when Standard Precautions and other infection-control practices are not consistently implemented 25, 26. In the United States, health-care-associated transmission of hepatitis C has been associated with inadequate infection prevention practices during inpatient care, outpatient care, and hemodialysis (kidney dialysis). These infection control breaches have included reuse of syringes and other failures of aseptic technique, contamination of multidose vials, and inadequate cleaning of equipment. Diversion of controlled substances for illicit use has also been associated with outbreaks 27. Often, health-care-associated outbreaks are first detected by astute clinicians who find new infections in people without risk factors and then report cases to public health authorities.
How can I protect myself from hepatitis C infection?
If you don’t have hepatitis C, you can help protect yourself from hepatitis C infection by:
- not sharing drug needles or other drug materials
- wearing gloves if you have to touch another person’s blood or open sores
- making sure your tattoo artist or body piercer uses sterile tools and unopened ink
- not sharing personal items such toothbrushes, razors, or nail clippers
Hepatitis C can spread from person to person during sex, but the chances are low. People who have multiple sex partners, have HIV or other sexually transmitted diseases, or who engage in rough or anal sex have a higher chance of getting hepatitis C. Talk with your doctor about your risk of getting hepatitis C through sex and about safe sex practices, such as using a latex or polyurethane condom to help prevent the spread of hepatitis C.
If you had hepatitis C in the past and your body fought off the infection or medicines cured the infection, you can get hepatitis C again. Follow the steps above, and talk with your doctor about how to protect yourself from another hepatitis C infection.
If you think you may have been exposed to the hepatitis C virus, see your doctor as soon as possible. Early diagnosis and treatment can help prevent liver damage.
Complications of Hepatitis C virus (HCV) Infection
Hepatitis C infection that continues over many years can cause significant complications, such as:
- Scarring of the liver (cirrhosis). After 20 to 30 years of hepatitis C infection, cirrhosis may occur. Scarring in your liver makes it difficult for your liver to function.
- Liver cancer. A small number of people with hepatitis C infection may develop liver cancer.
- Liver failure. Advanced cirrhosis may cause your liver to stop functioning.
How do doctors treat the complications of hepatitis C?
If hepatitis C leads to cirrhosis, you should see a doctor who specializes in liver diseases. Doctors can treat the health problems related to cirrhosis with medicines, surgery, and other medical procedures. If you have cirrhosis, you have an increased chance of liver cancer. Your doctor may order an ultrasound test to check for liver cancer.
If hepatitis C leads to liver failure or liver cancer, you may need a liver transplant.
What are the chances of someone with hepatitis C virus infection developing cirrhosis or liver cancer?
Of every 100 people infected with hepatitis C virus, approximately 5–25 will develop cirrhosis within 10–20 years. Patients who develop cirrhosis have a 1%–4% annual risk of developing hepatocellular carcinoma (liver cancer) and a 3%–6% annual risk of hepatic decompensation (liver failure); for patients with liver failure, the risk of death in the following year is 15%–20% 15.
What are the chances of someone developing chronic Hepatitis C virus (HCV) infection, chronic liver disease, cirrhosis, or liver cancer or dying as a result of hepatitis C?
Of every 100 persons infected with hepatitis C virus , approximately:
- 75–85 will go on to develop chronic infection
- 60–70 will go on to develop chronic liver disease
- 5–20 will go on to develop cirrhosis over a period of 20–30 years
- 1–5 will die from the consequences of chronic infection (liver cancer or cirrhosis)
Who is more likely to develop cirrhosis after becoming infected with hepatitis C virus?
Rates of progression to cirrhosis are increased in the presence of a variety of factors, including:
- Being male
- Being age >50 years
- Consuming alcohol
- Having nonalcoholic fatty liver disease (NAFLD), hepatitis B, or HIV coinfection
- Receiving immunosuppressive therapy 28
Is hepatitis C a common cause for liver transplantation?
Yes. Chronic hepatitis C virus infection is the leading indication for liver transplants in the United States 29.
How many deaths can be attributed to chronic hepatitis C virus infection?
The Centers for Disease Control and Prevention (CDC) estimates that there were 19,659 deaths with hepatitis C virus (HCV) as an underlying or contributing cause of death in 2014. In 2018, a total of 15,713 U.S. death certificates had hepatitis C recorded as an underlying or contributing cause of death 21. This number is considered a conservative estimate; data indicate that most people who die from hepatitis C lack documentation of hepatitis C virus infection on their death certificates 30.
How many different genotypes of hepatitis C virus exist?
Globally, hepatitis C virus exists in several distinct forms, known as genotypes. Seven hepatitis C virus genotypes and 67 subtypes have been identified 31. The most common hepatitis C virus genotype in North America and Europe is type 1. Type 2 also occurs in the United States and Europe, but is less common than type 1. Both type 1 and type 2 have also spread through much of the world, although other genotypes cause a majority of infections in the Middle East, Asia and Africa.
Which hepatitis C virus genotypes are found in the United States?
Genotypes 1a, 1b, 2, and 3 are the most common hepatitis C virus genotypes in the United States 32.
Can superinfection with more than one hepatitis C virus genotype occur?
Superinfection (a second infection superimposed on an earlier infection) is possible if risk behaviors for hepatitis C virus infection (e.g., injection-drug use) continue; however, superinfection does not appear to complicate decisions regarding treatment, because hepatitis C virus antivirals with pan-genotypic activity are available.
Can people become infected with a different strain of hepatitis C virus after they have cleared the initial infection?
Yes. Prior infection with hepatitis C virus does not protect against later infection with the same or different genotypes of the virus. This is because people infected with hepatitis C virus typically have an ineffective immune response due to changes in the virus during infection.
Although chronic hepatitis C follows a similar course regardless of the genotype of the infecting virus, treatment recommendations vary depending on viral genotype.
Hepatitis C causes
Hepatitis C infection is caused by the hepatitis C virus (HCV).Hepatitis C infection spreads when blood that has the hepatitis C virus (HCV) enters the bloodstream of a person who isn’t affected. Hepatitis C virus is a spherical, enveloped, positive-strand ribonucleic acid (RNA) virus that is approximately 55 nm in diameter (Figure 1) 33. Hepatitis C virus (HCV) is a member of the family Flaviviridae, yet distinct to be classified as a separate genus, Hepacivirus. The genome is approximately 9.6 kb in length. It encodes a polyprotein that then gets processed into at least ten proteins. These include three “structural” proteins, the nucleocapsid protein, core (C), and two envelope proteins (E1 and E2); two proteins that are essential for virion production (p7 and NS2); and five nonstructural proteins that are an essential part of the viral replication complex (NS3, NS4A, NS4B, NS5A, and NS5B) 33. A virion is a complete hepatitis C virus particle that consists of an RNA core with a protein coat sometimes with external envelopes and that is the extracellular infectious form of a virus. There is a very high level of virion turnover by the NS5B RNA polymerase with an absence of proofreading, resulting in the generation of viral mutants, also known as “quasispecies” 34.
Hepatitis C virus transmission requires that infectious virions contact susceptible cells that allow replication. Hepatitis C virus RNA can be detected in blood (including serum and plasma), saliva, tears, seminal fluid, ascitic fluid, and cerebrospinal fluid within days of exposure, often 1 to 4 weeks 35. Viremia peaks in the first 8 to 12 weeks of infection, and then plateaus or drops to undetectable levels (viral clearance); in the majority, 50% to 85% it persists. Persistent infection appears to be due to weak CD4+ and CD8+ T-cell responses, which fail to control viral replication. When a chronic infection is established, hepatitis C virus does not appear to be cytopathic; it is the local inflammatory response that triggers fibrogenesis. Multiple external factors, including alcohol consumption, HIV or hepatitis B virus coinfections, Genotype 3 infection, insulin resistance, obesity, and non-alcoholic fatty liver disease (NAFLD), have links with accelerated fibrosis progression and cirrhosis. The severity of liver fibrosis tightly correlates with the increased risk of hepatocellular carcinoma via facilitating genetic aberrations and promoting neoplastic clones36.
The hepatitis C virus spreads through contact with an infected person’s blood. Contact can occur by:
- sharing drug needles or other drug materials with an infected person
- getting an accidental stick with a needle that was used on an infected person
- being tattooed or pierced with tools or inks that were not kept sterile—free from all viruses and other microorganisms—and were used on an infected person before they were used on you
- having contact with the blood or open sores of an infected person
- using an infected person’s razor, toothbrush, or nail clippers
- being born to a mother with hepatitis C
- having unprotected sex with an infected person
Available data suggest that hepatitis C virus may get transmitted during sexual intercourse, but this rarely occurs. Perinatal transmission frequency ranges from 0% to 4% in more extensive studies. But for most patients with hepatitis C virus in the United States and Europe, hepatitis C infection is acquired via intravenous drug abuse or poor medical practices in resource-limited areas of the world 37.
Around the world, hepatitis C infection exists in several forms, called genotypes. There are seven genotypes and 67 subtypes of hepatitis C virus based on their nucleotide variability in hepatitis C virus sequences recovered from multiple geographic regions 38:
- Genotype 1: the most widely dispersed worldwide, 60% to 70% of isolates from the United States are subtype 1a or 1b
- Genotype 2: widely dispersed but most diverse in central and west Africa.
- Genotype 3: widely distributed but most diverse in Asia, linked to illicit drug use.
- Genotype 4: Northern Africa and the Middle East.
- Genotype 5: South Africa
- Genotype 6: Southeast Asia.
- Genotype 7: Central Africa (Congo).
The dominant genotype globally is genotype 1, which is also associated with more severe liver disease and a much greater risk of developing liver cancer. The most common hepatitis C genotype in the United States is type 1, accounting for about 60% of cases of hepatitis C virus. Genotypes 2a, 3b, and 2c account for about 10% of cases in the USA and are most responsive to antiviral medications.
Risk factors for hepatitis C infection
Your risk of hepatitis C infection is increased if you:
- Are a health care worker who has been exposed to infected blood, which may happen if an infected needle pierces your skin
- Have ever injected, snorted or inhaled illicit drugs
- Men who have sex with men.
- Have HIV
- Sexually active people about to start taking medicine to prevent HIV, called pre-exposure prophylaxis or PrEP.
- Sexual partners of anyone diagnosed with hepatitis C infection.
- Received a piercing or tattoo in an unclean environment using unsterile equipment
- Received a blood transfusion or organ transplant before 1992
- Received clotting factor concentrates before 1987
- Received hemodialysis treatments for a long period of time
- Were born to a woman with a hepatitis C infection
- Pregnant women during the pregnancy
- Has abnormal liver function test results in which the cause wasn’t found.
- Were ever in prison
- Were born between 1945 and 1965, the age group with the highest incidence of hepatitis C infection.
How is Hepatitis C transmitted?
Hepatitis C virus (HCV) is transmitted primarily through large or repeated percutaneous (i.e., passage through the skin) exposures to infectious blood, such as:
- Injection drug use (currently the most common means of hepatitis C virus transmission in the United States)
- Receipt of donated blood, blood products, and organs (once a common means of transmission but now rare in the United States since blood screening became available in 1992)
- Needlestick injuries in health care settings
- Birth to an hepatitis C virus-infected mother
Hepatitis C virus (HCV) can also be spread infrequently through:
- Sex with an hepatitis C virus-infected person (an inefficient means of transmission)
- Sharing personal items contaminated with infectious blood, such as razors or toothbrushes (also inefficient vectors of transmission)
- Other health care procedures that involve invasive procedures, such as injections (usually recognized in the context of outbreaks).
What is the prevalence of Hepatitis C virus infection among injection drug users?
The most recent surveys of active injection drug users indicate that approximately one third of young (aged 18–30 years) injection drug users are hepatitis C virus-infected. Older and former injection drug users typically have a much higher prevalence (approximately 70%–90%) of hepatitis C virus infection, reflecting the increased risk of continued injection drug use. The high hepatitis C virus prevalence among former injection drug users is largely attributable to needle sharing during the 1970s and 1980s, before the risks of bloodborne viruses were widely known and before educational initiatives were implemented.
Is cocaine use associated with hepatitis C virus transmission?
There are very limited epidemiologic data to suggest an additional risk from non-injection (snorted or smoked) cocaine use, but this risk is difficult to differentiate from associated injection drug use and sex with hepatitis C virus-infected partners.
Who is at risk for Hepatitis C virus infection?
The following persons are at known to be at increased risk for hepatitis C virus infection:
- Current or former injection drug users, including those who injected only once many years ago
- Recipients of clotting factor concentrates made before 1987, before more advanced methods for manufacturing those products were developed
- Recipients of blood transfusions or solid organ transplants before July 1992, before better testing of blood donors became available (it’s now rare in the United States since blood screening became available in 1992). Now that more advanced screening tests for hepatitis C are used in blood banks, the risk of transmission to recipients of blood or blood products is considered extremely rare, at <1 case per 2 million units transfused 23.
- Chronic hemodialysis patients (kidney dialysis)
- Persons with known exposures to hepatitis C virus, such as:
- health care workers after needlesticks involving hepatitis C virus-positive blood
- recipients of blood or organs from a donor who tested hepatitis C virus-positive
- Persons with HIV infection
- Children born to hepatitis C virus-positive mothers
- Have had tattoos or body piercings
- Have worked or lived in a prison
- Have had more than one sex partner in the last 6 months or have a history of sexually transmitted disease (STD)
- Are men who have or had sex with men
In the United States, injecting drugs is the most common way that people get hepatitis C 8.
What is the risk of acquiring hepatitis C virus infection from transfused blood or blood products in the United States ?
Now that more advanced screening tests for hepatitis C virus are used in blood banks, the risk is considered to be less than 1 chance per 2 million units transfused. Before 1992, when blood screening for hepatitis C virus became available, blood transfusion was a leading means of hepatitis C virus transmission.
Can hepatitis C virus be spread during medical or dental procedures ?
As long as Standard Precautions and other infection control practices are used consistently, medical and dental procedures performed in the United States generally do not pose a risk for the spread of hepatitis C virus. However, hepatitis C virus has been spread in health care settings when injection equipment, such as syringes, was shared between patients or when injectable medications or intravenous solutions were mishandled and became contaminated with blood. Health care personnel should understand and adhere to Standard Precautions, which includes Injection Safety practices aimed at reducing bloodborne pathogen risks for patients and health care personnel. If health care-associated hepatitis C virus infection is suspected, this should be reported to state and local public health authorities.
Can hepatitis C virus be spread within a household ?
Yes, but this does not occur very often. If hepatitis C virus is spread within a household, it is most likely a result of direct, through-the-skin exposure to the blood of an infected household member.
Hepatitis C prevention
Protect yourself from hepatitis C infection by taking the following precautions:
- Stop using illicit drugs, particularly if you inject them. If you use illicit drugs, seek help.
- Be cautious about body piercing and tattooing. If you choose to undergo piercing or tattooing, look for a reputable shop. Ask questions beforehand about how the equipment is cleaned. Make sure the employees use sterile needles. If employees won’t answer your questions, look for another shop.
- Practice safer sex. Don’t engage in unprotected sex with multiple partners or with any partner whose health status is uncertain. Sexual transmission between monogamous couples may occur, but the risk is low.
Hepatitis C can spread from person to person during sex, but the chances are low. People who have multiple sex partners, have HIV or other sexually transmitted diseases, or who engage in rough or anal sex have a higher chance of getting hepatitis C. Talk with your doctor about your risk of getting hepatitis C through sex and about safe sex practices, such as using a latex or polyurethane condom to help prevent the spread of hepatitis C.
If you had hepatitis C in the past and your body fought off the infection or medicines cured the infection, you can get hepatitis C again. Follow the steps above, and talk with your doctor about how to protect yourself from another hepatitis C infection.
If you think you may have been exposed to the hepatitis C virus, see your doctor as soon as possible. Early diagnosis and treatment can help prevent liver damage.
How can I prevent spreading hepatitis C to others?
If you have hepatitis C, follow the steps above to avoid spreading the infection. Tell your sex partner you have hepatitis C, and talk with your doctor about safe sex practices. In addition, you can protect others from infection by telling your doctor, dentist, and other health care providers that you have hepatitis C. Don’t donate blood or blood products, semen, organs, or tissue.
Is a hepatitis C vaccine available?
No. Researchers are still working on a hepatitis C vaccine. If you have hepatitis C, talk with your doctor about vaccines for hepatitis A and hepatitis B. Hepatitis A and hepatitis B vaccines can protect you from hepatitis A and hepatitis B infections, which could further damage your liver.
Hepatitis C symptoms
Every chronic (long-term) hepatitis C infection starts with an acute phase. Acute hepatitis C usually goes undiagnosed because it rarely causes symptoms (asymptomatic). Some people with an acute hepatitis C infection may have symptoms within 1 to 3 months after they are exposed to hepatitis C virus and last two weeks to three months. In those people who do develop symptoms, the average period from exposure to symptom onset is 2–12 weeks (range: 2–26 weeks) 2. These symptoms may include:
- dark yellow urine
- feeling tired or fatigue
- muscle aches
- fever
- gray- or clay-colored stools
- joint pain
- loss of appetite
- nausea
- pain in your abdomen
- vomiting
- yellowish eyes and skin, called jaundice
If you have long-term hepatitis C infection also known as chronic hepatitis C, you most likely will have no symptoms until complications develop, which could be decades after you were infected, after the hepatitis C virus damages the liver enough to cause symptoms. For this reason, hepatitis C screening is important, even if you have no symptoms.
- Approximately 20%–30% of those newly infected with hepatitis C virus experience fatigue, abdominal pain, poor appetite, or jaundice.
- In those persons who do develop symptoms, the average time period from exposure to symptom onset is 4–12 weeks (range: 2–24 weeks).
Acute hepatitis C infection doesn’t always become chronic. Some people clear hepatitis C virus from their bodies after the acute phase, an outcome known as spontaneous viral clearance. In studies of people diagnosed with acute hepatitis C virus, rates of spontaneous viral clearance have varied from 15 to 25 percent without treatment and do not develop chronic infection; the reasons for this are not well known. Acute hepatitis C also responds well to antiviral therapy.
Long-term infection with the hepatitis C virus is known as chronic hepatitis C. Chronic hepatitis C is usually a “silent” infection for many years, until the virus damages the liver enough to cause the signs and symptoms of liver disease. Most people with chronic hepatitis C virus infection are asymptomatic or have non-specific symptoms such as chronic fatigue and depression. Many eventually develop chronic liver disease, which can range from mild to severe, including cirrhosis and liver cancer. Chronic liver disease in hepatitis C virus-infected people is usually insidious, progressing slowly without any signs or symptoms for several decades. In fact, hepatitis C virus infection is often not recognized until asymptomatic people are identified as hepatitis C virus-positive when screened for blood donation or when elevated alanine aminotransferase (ALT, a liver enzyme) levels are detected during routine examinations.
Signs and symptoms of chronic hepatitis C virus infection:
- Bleeding easily
- Bruising easily
- Fatigue
- Poor appetite
- Yellow discoloration of the skin and eyes called jaundice. This might show up more in white people. Also, yellowing of the whites of the eyes in white, Black and brown people.
- Dark-colored urine
- Itchy skin
- Fluid buildup in your abdomen called ascites.
- Swelling in your legs
- Weight loss
- Confusion, drowsiness and slurred speech, called hepatic encephalopathy.
- Spider-like blood vessels on your skin, called spider angiomas.
Some people with chronic hepatitis C virus infection develop medical conditions due to hepatitis C that are not limited to the liver. Such conditions can include:
- Diabetes mellitus
- Glomerulonephritis
- Essential mixed cryoglobulinemia
- Porphyria cutanea tarda
- Non-Hodgkin’s lymphoma
Hepatitis C complications
Without treatment, hepatitis C may lead to cirrhosis, liver failure, and liver cancer. Early diagnosis and treatment of hepatitis C can prevent these complications.
Cirrhosis
Cirrhosis is a condition in which the liver slowly breaks down and is unable to function normally. Scar tissue replaces healthy liver tissue and partially blocks the flow of blood through the liver. In the early stages of cirrhosis, the liver continues to function. However, as cirrhosis gets worse, the liver begins to fail.
Liver failure
Also called end-stage liver disease, liver failure progresses over months, years, or even decades. With end-stage liver disease, the liver can no longer perform important functions or replace damaged cells.
Liver cancer
Having chronic hepatitis C increases your chance of developing liver cancer. If chronic hepatitis C causes severe liver damage or cirrhosis before you receive hepatitis C treatment, you will continue to have an increased chance of liver cancer even after treatment. Your doctor may suggest blood tests and an ultrasound or another type of imaging test to check for liver cancer. Finding cancer at an early stage improves the chance of curing the cancer.
Extrahepatic complications of chronic chronic hepatitis C infection
Some people with chronic hepatitis C infection develop medical conditions due to hepatitis C that are not limited to the liver. Such conditions can include:
- Diabetes mellitus
- Glomerulonephritis
- Essential mixed cryoglobulinemia
- Porphyria cutanea tarda
- Non-Hodgkin’s lymphoma
How is hepatitis C infection diagnosed?
Doctors diagnose hepatitis C based on your medical history, a physical exam, and blood tests. If you have hepatitis C, your doctor may perform additional tests to check your liver.
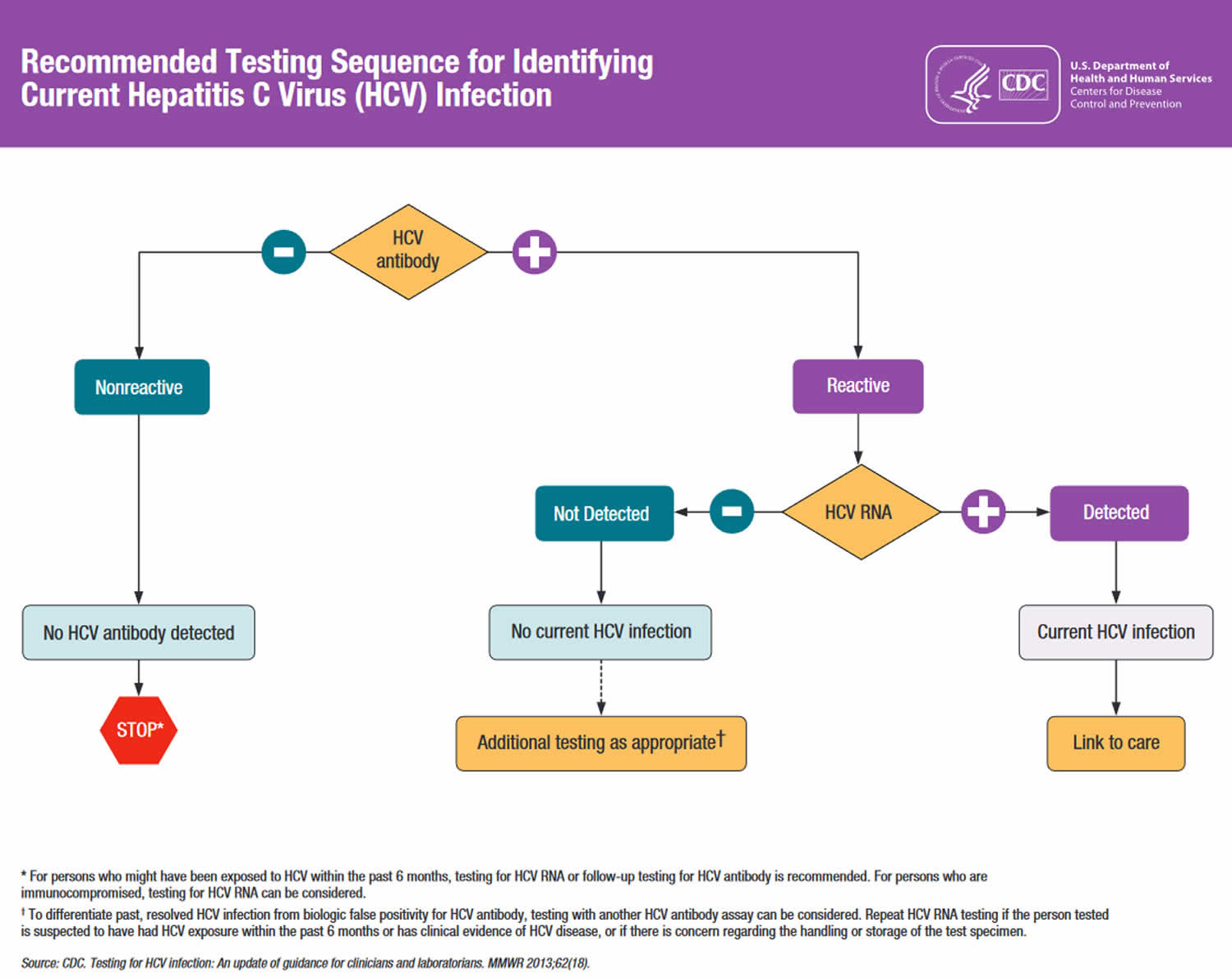
Figure 2. Hepatitis C diagnostic algorithm
[Source 39 ]Screening for Hepatitis C
A screening blood test will show whether you have developed antibodies to the hepatitis C virus. A positive antibody test means you were exposed to the hepatitis C virus at some point. However, the virus may no longer be present in your blood if your body fought off the infection on its own or if you received treatment that cured the infection.
The U.S. Preventive Services Task Force recommends that all adults ages 18 to 79 years get a blood test to screen for hepatitis C infection, even those without symptoms or known liver disease. Screening for hepatitis C virus is especially important if you’re at high risk of exposure, including:
- Persons who have ever injected illegal drugs, including those who injected only once many years ago or inhaled illicit drugs
- Anyone who has abnormal liver function test results with no identified cause
- Babies born to mothers with hepatitis C (to avoid detecting maternal antibody, these children should not be tested before age 18 months)
- Persons with known exposures to hepatitis C virus, such as:
- health care workers after needlesticks involving hepatitis C virus-positive blood
- recipients of blood or organs from a donor who later tested hepatitis C virus-positive
- People with hemophilia who were treated with clotting factors before 1987
- People who have ever undergone long-term hemodialysis treatments
- People who received blood transfusions or organ transplants before 1992
- Sexual partners of anyone diagnosed with hepatitis C infection
- People with HIV infection
- Anyone born from 1945 to 1965
- Anyone who has been in prison
- All pregnant women during each pregnancy
- Children born to mothers with hepatitis C virus infection
- People who were notified that they received blood from a donor who later tested positive for hepatitis C virus infection
- Health care, emergency medical, and public safety personnel after needle sticks, sharps, or mucosal exposures to hepatitis C virus‑positive blood
- Any person who requests hepatitis C testing
Blood tests to detect hepatitis C virus infection
If an initial blood test shows that you have hepatitis C, additional blood tests will:
- Measure the quantity of the hepatitis C virus in your blood (viral load)
- Identify the genotype of hepatitis C virus
Several blood tests are performed to test for hepatitis C virus infection, including:
- Screening tests for antibodies to the hepatitis C virus (anti-HCV). A screening blood test will show whether you have developed antibodies to the hepatitis C virus (anti-HCV). A positive antibody test(anti-HCV positive) means you were exposed to the hepatitis C virus at some point. However, the virus may no longer be present in your blood if your body fought off the infection on its own or if you received treatment that cured the infection.
- Enzyme immunoassay (EIA)
- Enhanced chemiluminescence immunoassay (CLIA)
- Chemiluminescence microparticle immunoassay (CMIA)
- Microparticle immunoassay (MEIA)
- Electrochemiluminescence immunoassay (ECLIA)
- Immunochromatographic assay (rapid test)
- Hepatitis C RNA test: If your antibody to the hepatitis C virus (anti-HCV) test is positive, your doctor will use a hepatitis C RNA test to detect RNA—a type of genetic material—from the hepatitis C virus. The hepatitis C RNA test can show whether you still have the hepatitis C virus and how much virus is in your blood. This information can help your doctor treat the infection. To see if you are responding to treatment, your doctor may order this test while you are undergoing treatment to find out if the amount of virus in your blood is changing.
- Qualitative tests to detect presence or absence of virus (hepatitis C virus RNA polymerase chain reaction [PCR])
- Quantitative tests to detect amount (titer) of virus (hepatitis C virus RNA PCR)
- Identify the genotype of the virus (Genotype test). Your doctor can use this test to find out what strain, or form, of hepatitis C virus you have. At least seven specific strains called genotypes of hepatitis C exist. Genotype 1 is the most common hepatitis C genotype in the United States 8. Your doctor will recommend treatment based on which hepatitis C genotype you have.
Hepatitis C virus test results interpretation
Table 1. Interpretation of results of tests for hepatitis C virus (HCV) infection and further Actions
| Test Outcome | Interpretation | Further Actions |
|---|---|---|
| Hepatitis C virus antibody (anti-HCV) nonreactive | No hepatitis C virus antibody detected | Sample can be reported as nonreactive for hepatitis C virus antibody. No further action required. If recent exposure in person tested is suspected, test for hepatitis C virus RNA.* |
| Hepatitis C virus antibody (anti-HCV) reactive | Presumptive hepatitis C virus infection | A repeatedly reactive result is consistent with current hepatitis C virus infection, or past hepatitis C virus infection that has resolved, or biologic false positivity for hepatitis C virus antibody. Test for hepatitis C virus RNA to identify current infection. |
| Hepatitis C virus antibody (anti-HCV) reactive, hepatitis C virus RNA detected | Current hepatitis C virus infection | Provide person tested with appropriate counseling and link person tested to care and treatment.† |
| Hepatitis C virus antibody (anti-HCV) reactive, hepatitis C virus RNA not detected | No current hepatitis C virus infection | No further action required in most cases. If distinction between true positivity and biologic false positivity for hepatitis C virus antibody is desired and if sample is repeatedly reactive in the initial test, test with another hepatitis C virus antibody assay. In certain situations,§ follow up with hepatitis C virus RNA testing and appropriate counseling. |
Footnotes:
* If hepatitis C virus RNA testing is not feasible and person tested is not immunocompromised, do follow-up testing for hepatitis C virus antibody (anti-HCV) to demonstrate seroconversion. If the person tested is immunocompromised, consider testing for hepatitis C virus RNA.
† It is recommended before initiating antiviral therapy to retest for hepatitis C virus RNA in a subsequent blood sample to confirm hepatitis C virus RNA positivity.
§ If the person tested is suspected of having hepatitis C virus exposure within the past 6 months, or has clinical evidence of hepatitis C virus disease, or if there is concern regarding the handling or storage of the test specimen.
Tests for liver damage
If you’ve had chronic hepatitis C for a long time, you could have liver damage. Doctors typically use one or more of the following tests to assess liver damage in chronic hepatitis C.
- Magnetic resonance elastography (MRE). A noninvasive alternative to a liver biopsy, magnetic resonance elastography (MRE) combines magnetic resonance imaging technology with patterns formed by sound waves bouncing off the liver to create a visual map showing gradients of stiffness throughout the liver. Stiff liver tissue indicates the presence of fibrosis, or scarring of the liver, as a result of chronic hepatitis C.
- Transient elastography. Another noninvasive test, transient elastography is a type of ultrasound that transmits vibrations into the liver and measures the speed of their dispersal through liver tissue to estimate its stiffness.
- Liver biopsy. Typically done using ultrasound guidance, this test involves inserting a thin needle through the abdominal wall to remove a small sample of liver tissue for laboratory testing.
- Blood tests. A series of blood tests can indicate the extent of fibrosis in your liver.
Doctors typically use liver biopsy only if other tests don’t provide enough information about a person’s liver damage or disease. Talk with your doctor about which tests are best for you.
How soon after exposure to hepatitis C virus can anti-HCV (hepatitis C virus antibody) be detected?
Hepatitis C virus infection can be detected by hepatitis C virus antibody (anti-HCV) screening tests (enzyme immunoassay) 4–10 weeks after infection. Anti-hepatitis C virus seroconversion occurs an average of 8–11 weeks after exposure 41, 42, 43, although cases of delayed seroconversion have been documented in people who are immunosuppressed (e.g., those with HIV infection) 44. Anti-hepatitis C virus can be detected in >97% of persons by 6 months after exposure.
Is an hepatitis C virus antibody (anti-HCV) test sufficient to diagnose current hepatitis C virus infection?
No. The anti-hepatitis C virus (anti-HCV) test only provides information about past exposure to hepatitis C virus. A negative anti-hepatitis C virus (anti-HCV) result indicates that a patient has never been exposed to the virus, and therefore the anti-hepatitis C virus (anti-HCV) test is only used to rule out hepatitis C virus infection. If a person tests positive for hepatitis C virus antibodies, hepatitis C testing is not considered complete unless the initial positive anti-hepatitis C virus (anti-HCV) test is followed by a test for hepatitis C virus RNA as per CDC guidelines. A positive test for hepatitis C virus RNA is needed before a patient can be diagnosed with current hepatitis C virus and begin receiving treatment. Ideally, positive hepatitis C virus antibody (anti-HCV) tests are “reflexed” to an hepatitis C virus RNA test automatically from the same blood sample. However, reflex testing is not possible in every laboratory or clinical setting.
Is someone with a positive anti-hepatitis C virus (anti-HCV) test still at risk for hepatitis C?
Yes. A person with a positive anti-hepatitis C virus (anti-HCV) test is susceptible to future hepatitis C virus infections. People with ongoing risk factors, such as those who currently inject drugs and those who have previously tested anti-hepatitis C virus (anti-HCV) positive and hepatitis C virus RNA negative, should receive periodic hepatitis C virus RNA testing.
Under what circumstances might a false-negative hepatitis C virus antibody (anti-HCV) test result occur, even when a person has been exposed to hepatitis C virus?
People who have been very recently infected with hepatitis C virus might not yet have developed antibody levels high enough to be detected by the anti-hepatitis C virus (anti-HCV) test. The window period for acute hepatitis C virus infection before the detection of antibodies averages 8 to 11 weeks, with a reported range of 2 weeks to 6 months. In addition, some people might lack the immune response necessary to develop detectable antibodies within this time range 44. In these people, virologic testing (e.g., PCR for hepatitis C virus RNA) can be considered.
How soon after exposure to hepatitis C virus can hepatitis C virus RNA be detected?
People with recently acquired acute infection typically have detectable hepatitis C virus RNA levels as early as 1–2 weeks after exposure to the virus 41.
Under what circumstances is a false-positive anti-hepatitis C virus test result likely?
False-positive anti-hepatitis C virus tests appear more often when persons at low risk for hepatitis C virus infection (e.g., blood donors) are tested. Therefore, it is important to follow-up all positive anti-hepatitis C virus tests with a RNA test to establish current infection.
Can a patient have a normal liver enzyme (e.g., ALT) level and still have chronic hepatitis C?
Yes. It is common for patients with chronic hepatitis C to have liver enzyme levels that go up and down, with periodic returns to normal or near normal levels. Liver enzyme levels can remain normal for over a year despite chronic liver disease 45.
Hepatitis C Treatment
Hepatitis C virus (HCV)-positive persons should be evaluated (by referral or consultation, if appropriate) for presence of chronic liver disease, including assessment of liver function tests, evaluation for severity of liver disease and possible treatment, and determination of the need for Hepatitis A and Hepatitis B vaccination.
Doctors treat hepatitis C with antiviral medicines that attack the virus and can cure the disease in most cases. Several newer medicines, called direct-acting antiviral medicines, have been approved to treat hepatitis C since 2013. Studies show that these medicines can cure chronic hepatitis C in most people with this disease. These medicines can also cure acute hepatitis C. In some cases, doctors recommend waiting to see if an acute infection becomes chronic before starting treatment. Hepatitis C medicines may cause side effects. Talk with your doctor about the side effects of treatment. For safety reasons, check with your doctor before taking any other prescription or over-the-counter medicines.
Hepatitis C infection is treated with antiviral medications intended to clear the virus from your body 12. The goal of treatment is to have no hepatitis C virus detected in your body at least 12 weeks after you complete treatment.
Researchers have recently made significant advances in treatment for hepatitis C using new, “direct-acting” anti-viral medications, sometimes in combination with existing ones. As a result, people experience better outcomes, fewer side effects and shorter treatment times — some as short as eight weeks. The choice of medications and length of treatment depend on the hepatitis C genotype, presence of existing liver damage, other medical conditions and prior treatments.
For a complete list of currently approved FDA therapies to treat hepatitis C, please visit: https://www.hepatitisc.uw.edu/page/treatment/drugs
Due to the pace of research, recommendations for medications and treatment regimens are changing rapidly. It is therefore best to discuss your treatment options with a specialist.
Throughout treatment your care team will monitor your response to medications.
Your doctor may prescribe one or more of these newer, direct-acting antiviral medicines to treat hepatitis C:
- daclatasvir (Daklinza)
- elbasvir/grazoprevir (Zepatier)
- glecaprevir and pibrentasvir (Mavyret)
- ledipasvir/sofosbuvir (Harvoni)
- ombitasvir/paritaprevir/ritonavir (Technivie)
- ombitasvir/paritaprevir/ritonavir/dasabuvir (Viekira Pak, Viekira XR)
- simeprevir (Olysio)
- sofosbuvir (Sovaldi)
- sofosbuvir/velpatasvir (Epclusa)
- sofosbuvir/velpatasvir/voxilaprevir (Vosevi)
Newer medicines are sometimes used along with these older hepatitis C medicines:
- ribavirin
- peginterferon alfa-2a (Pegasys) or peginterferon alfa-2b (PEG-Intron)
You may need to take medicines for 8 to 24 weeks to cure hepatitis C. Your doctor will prescribe medicines and recommend a length of treatment based on 3:
- which hepatitis C genotype you have
- how much liver damage you have
- whether you have been treated for hepatitis C in the past
Your doctor may order blood tests during and after your treatment. Blood tests can show whether the treatment is working. Hepatitis C medicines cure the infection in most people who complete treatment.
Liver transplantation
If you have developed serious complications from chronic hepatitis C infection, liver transplantation may be an option. During liver transplantation, the surgeon removes your damaged liver and replaces it with a healthy liver. Most transplanted livers come from deceased donors, though a small number come from living donors who donate a portion of their livers.
In most cases, a liver transplant alone doesn’t cure hepatitis C. The infection is likely to return, requiring treatment with antiviral medication to prevent damage to the transplanted liver. Several studies have demonstrated that new, direct-acting antiviral medication regimens are effective at curing post-transplant hepatitis C. Treatment with direct-acting antivirals can also be effective in appropriately selected patients before liver transplantation.
Vaccinations
Although there is no vaccine for hepatitis C, your doctor will likely recommend that you receive vaccines against the hepatitis A and B viruses. These are separate viruses that also can cause liver damage and complicate the course of chronic hepatitis C.
Yes. Because there are at least seven known genotypes and more than 67 subtypes of hepatitis C virus, genotype information is helpful in defining the epidemiology of hepatitis C and in making recommendations regarding appropriate treatment regimen. In the United States, hepatitis C virus genotype 1 is most common, accounting for 74% of prevalent cases. Once the genotype is identified, it need not be tested again; genotypes do not change during the course of infection.
Can superinfection with more than one genotype of hepatitis C virus occur?
Superinfection is possible if risk behaviors (e.g., injection drug use) for hepatitis C virus infection continue, but it is believed to be very uncommon.
Should patients with acute hepatitis C receive treatment?
With the exception of pregnant women and children under 3 years of age, people with acute hepatitis C (i.e., those with measurable hepatitis C virus RNA) should be treated for their infection. There is no need to wait for potential spontaneous viral resolution 46.
What is the treatment for chronic hepatitis C?
Over 90% of people infected with hepatitis C virus (HCV) can be cured of their infection, regardless of hepatitis C virus genotype, with 8–12 weeks of oral therapy 47. To provide health-care professionals with timely guidance as new therapies are available and integrated into hepatitis C treatment regimens, the Infectious Diseases Society of America (IDSA) and American Association for the Study of Liver Diseases (AASLD), in collaboration with the International Antiviral Society–USA (IAS–USA), developed evidence-based, expert-developed recommendations for hepatitis C management. These recommendations are available at https://www.hcvguidelines.org
Does chronic hepatitis C affect only the liver?
A small percentage of persons with chronic hepatitis C virus infection develop medical conditions due to hepatitis C that are not limited to the liver. These conditions are thought to be attributable to the body’s immune response to hepatitis C virus infection. Such conditions can include:
- Diabetes mellitus, which occurs three times more frequently in HCV-infected persons
- Glomerulonephritis, a type of kidney disease caused by inflammation of the kidney
- Essential mixed cryoglobulinemia, a condition involving the presence of abnormal proteins in the blood
- Porphyria cutanea tarda, an abnormality in heme production that causes skin fragility and blistering
- Non-Hodgkins lymphoma, which might occur somewhat more frequently in hepatitis C virus-infected persons
Are patients undergoing treatment for hepatitis C at risk for reactivation of an existing hepatitis B virus infection? How are these patients managed?
Yes. Hepatitis B virus (HBV) reactivation has recently been reported in co-infected patients receiving direct acting antiviral (DAA) therapy for hepatitis C virus (HCV) infection. Therefore, all patients initiating hepatitis C virus direct acting antiviral therapy should be tested for hepatitis B virus (HBV) with HBsAg, anti-HBs, and anti-HBc. People testing positive for HBsAg and/or anti-HBc should be monitored while receiving hepatitis C treatment. More information about treating hepatitis B virus/hepatitis C virus co-infected patients can be found on these sites: https://www.hcvguidelines.org and https://liverlearning.aasld.org
Lifestyle and home remedies for Hepatitis C infection
If you receive a diagnosis of hepatitis C, your doctor will likely recommend certain lifestyle changes. These measures will help keep you healthy longer and protect the health of others as well:
- Stop drinking alcohol. Alcohol speeds the progression of liver disease.
- Avoid medications that may cause liver damage. Review your medications with your doctor, including over-the-counter medications you take as well as herbal preparations and dietary supplements. Your doctor may recommend avoiding certain medications.
- Help prevent others from coming in contact with your blood. Cover any wounds you have and don’t share razors or toothbrushes. Don’t donate blood, body organs or semen, and advise health care workers that you have the virus. Also tell your partner about your infection before you have sex, and always use condoms during intercourse.
What should I eat and drink if I have hepatitis C?
If you have hepatitis C, you should eat a balanced, healthy diet. Talk with your doctor about healthy eating. You should also avoid alcohol because it can cause more liver damage.
Pregnancy and Hepatitis C virus Infection
Should pregnant women be routinely tested for anti-hepatitis C virus?
No. Since pregnant women have no greater risk of being infected with hepatitis C virus than non-pregnant women and interventions to prevent mother-to-child transmission are lacking, routine anti-hepatitis C virus testing of pregnant women is not recommended. Pregnant women should be tested for anti-hepatitis C virus only if they have risk factors for hepatitis C virus infection.
What is the risk that an hepatitis C virus-infected mother will spread hepatitis C virus to her infant during birth?
Approximately 6 of every 100 infants born to hepatitis C virus-infected mothers become infected with the virus. Transmission occurs at the time of birth, and no prophylaxis is available to prevent it. The risk is increased by the presence of maternal hepatitis C virus viremia at delivery and also is 2–3 times greater if the woman is coinfected with HIV. Most infants infected with hepatitis C virus at birth have no symptoms and do well during childhood. More research is needed to find out the long-term effects of perinatal hepatitis C virus infection.
Should a woman with hepatitis C virus infection be advised against breastfeeding?
No. There is no evidence that breastfeeding spreads hepatitis C virus. However, hepatitis C virus-positive mothers should consider abstaining from breastfeeding if their nipples are cracked or bleeding.
Is it safe for a mother infected with hepatitis C virus to breastfeed her infant?
Yes. There is no documented evidence that breastfeeding spreads hepatitis C virus. Therefore, having hepatitis C virus-infection is not a contraindication to breastfeed. 4.
Is it safe for the hepatitis C virus-positive mother to breastfeed if her nipples are cracked and bleeding?
Data are insufficient to say yes or no 4. However, hepatitis C virus is spread by infected blood. Therefore, if the hepatitis C virus-positive mother’s nipples and/or surrounding areola are cracked and bleeding, she should stop nursing temporarily. To maintain her milk supply while not breastfeeding, she can express and discard her breast milk until her nipples are healed. Once her nipples are no longer cracked or bleeding, the hepatitis C virus-positive mother may fully resume breastfeeding. Healthcare providers may need to refer mothers for lactation support to learn how to maintain milk production and how to supplement with donor human milk or formula while temporarily not breastfeeding.
When should children born to hepatitis C virus-infected mothers be tested to see if they were infected at birth ?
According to guidelines from the Infectious Diseases Society of America (IDSA) and the American Association for the Study of Liver Disease (AASLD), children should be tested for anti-hepatitis C virus (anti-HCV) no sooner than age 18 months because anti-hepatitis C (anti-HCV) from the mother might last until this age. If diagnosis is desired before the child turns 18 months, testing for hepatitis C virus RNA (HCV RNA) could be performed at or after the infant’s first well-child visit at age 1–2 months. Hepatitis C virus RNA (HCV RNA) testing should then be repeated at a subsequent visit, independent of the initial hepatitis C virus RNA test result 48.
Hepatitis C prognosis
Only 10-15% of patients infected with hepatitis C virus (HCV) have a self-limited infection; in all others, the infection is progressive 33. About 20% will develop cirrhosis within two decades, and another 1 to 5% will develop liver cancer within three decades 33. The progression of hepatitis C is more common in alcoholic, cirrhotics, and those with a coexisting hepatitis B virus infection. Individuals who have an undetectable viral load generally have a decreased risk of developing cirrhosis and death.
- Hepatitis C FAQs for Health Professionals. https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm[↩]
- Hepatitis C Questions and Answers for Health Professionals. https://www.cdc.gov/hepatitis/hcv/hcvfaq.htm[↩][↩]
- Hepatitis C. https://www.niddk.nih.gov/health-information/liver-disease/viral-hepatitis/hepatitis-c[↩][↩]
- Hepatitis B or C Infections. https://www.cdc.gov/breastfeeding/breastfeeding-special-circumstances/maternal-or-infant-illnesses/hepatitis.html[↩][↩][↩]
- Viral Hepatitis Surveillance 2019. https://www.cdc.gov/hepatitis/statistics/2019surveillance/HepC.htm[↩][↩][↩]
- Suryaprasad AG, White JZ, Xu F, Eichler BA, Hamilton J, Patel A, Hamdounia SB, Church DR, Barton K, Fisher C, Macomber K, Stanley M, Guilfoyle SM, Sweet K, Liu S, Iqbal K, Tohme R, Sharapov U, Kupronis BA, Ward JW, Holmberg SD. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014 Nov 15;59(10):1411-9. doi: 10.1093/cid/ciu643[↩][↩]
- Increase in hepatitis C infections linked to worsening opioid crisis. https://www.cdc.gov/nchhstp/newsroom/2017/hepatitis-c-and-opioid-injection-press-release.html[↩][↩]
- Hepatitis C Questions and Answers for Health Professionals. https://www.cdc.gov/hepatitis/HCV/HCVfaq.htm[↩][↩][↩][↩][↩][↩]
- Schillie S, Wester C, Osborne M, Wesolowski L, Ryerson AB. CDC Recommendations for Hepatitis C Screening Among Adults — United States, 2020. MMWR Recomm Rep 2020;69(No. RR-2):1–17. DOI: http://dx.doi.org/10.15585/mmwr.rr6902a1[↩][↩]
- Hepatitis C Virus Infection in Adolescents and Adults: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/document/RecommendationStatementFinal/hepatitis-c-screening[↩][↩][↩][↩]
- Bailey JR, Barnes E, Cox AL. Approaches, Progress, and Challenges to Hepatitis C Vaccine Development. Gastroenterology. 2019;156(2):418-30.[↩]
- FDA-Approved of treatments for hepatitis C. https://www.hepatitisc.uw.edu/page/treatment/drugs[↩][↩]
- Hepatitis C. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/hepatitis-c/symptoms-causes/syc-20354278[↩]
- Hofmeister MG, Rosenthal EM, Barker LK, Rosenberg ES, Barranco MA, Hall EW, Edlin BR, Mermin J, Ward JW, Ryerson AB. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019 Mar;69(3):1020-1031. doi: 10.1002/hep.30297[↩]
- Thomas DL, Seeff LB. Natural history of hepatitis C. Clin Liver Dis. 2005;9(3):383-98.[↩][↩][↩]
- Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000;132(4):296-305.[↩]
- Seo, S., Silverberg, M. J., Hurley, L. B., Ready, J., Saxena, V., Witt, D., Hare, C. B., Champsi, J. H., Korn, D. G., Pauly, M. P., Chamberland, S., Lai, J. B., & Marcus, J. L. (2020). Prevalence of Spontaneous Clearance of Hepatitis C Virus Infection Doubled From 1998 to 2017. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association, 18(2), 511–513. https://doi.org/10.1016/j.cgh.2019.04.035[↩]
- Liang TJ, Rehermann B, Seeff LB, Hoofnagle JH. Pathogenesis, natural history, treatment, and prevention of hepatitis C. Ann Intern Med. 2000 Feb 15;132(4):296-305. doi: 10.7326/0003-4819-132-4-200002150-00008[↩]
- Thomas DL, Seeff LB. Natural history of hepatitis C. Clin Liver Dis. 2005 Aug;9(3):383-98, vi. doi: 10.1016/j.cld.2005.05.003[↩]
- Perz, J.F., Grytdal, S., Beck, S., Fireteanu, A.M., Poissant, T., Rizzo, E., Bornschlegel, K., Thomas, A., Balter, S., Miller, J., Klevens, R.M. and Finelli, L. (2013), Case-control study of hepatitis B and hepatitis C in older adults: Do healthcare exposures contribute to burden of new infections?. Hepatology, 57: 917-924. https://doi.org/10.1002/hep.25688[↩]
- Centers for Disease Control and Prevention. Viral Hepatitis Surveillance—United States, 2018. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2020.[↩][↩]
- Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, Stone J, Cunningham EB, Trickey A, Dumchev K, Lynskey M, Griffiths P, Mattick RP, Hickman M, Larney S. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Global Health. 2017;5(12):e1192-1207.[↩]
- Crowder L, Steele W, Notari E, Haynes J, Dodd R, Stramer SL. Epidemiology of Hepatitis B Virus, Hepatitis C Virus and Human Immunodeficiency Virus in United States Blood Donors. Abstract accepted for AABB Conference 2017.[↩][↩]
- Standard Precautions for All Patient Care. https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html[↩]
- World Health Organization. Consolidated strategic information guidelines for viral hepatitis: planning and tracking progress towards elimination Geneva: World Health Organization; 2018.[↩]
- Hepatitis C. Chapter 4 Travel-Related Infectious Diseases. https://wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/hepatitis-c[↩]
- Injection Safety. https://www.cdc.gov/injectionsafety/drugdiversion/index.html[↩]
- Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol. 2014;61(1 Suppl):S58-68.[↩]
- Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/data/view-data-reports/build-advanced[↩]
- Mahajan R, Xing J, Liu SJ, Ly KN, Moorman AC, Rupp L, Xu F, Holmberg SD; Chronic Hepatitis Cohort Study (CHeCs) Investigators. Mortality among persons in care with hepatitis C virus infection: The Chronic Hepatitis Cohort Study (CHeCS), 2006-2010. Clinical Infectious Diseases. 2014;58(8):1055-61.[↩]
- Smith DB, Bukh J, Kuiken C, Muerhoff AS, Rice CM, Stapleton JT, Simmonds P. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology. 2014;59(1):318-27.[↩]
- Gordon SC, Trudeau S, Li J, et al. Race, age, and geography impact hepatitis C genotype distribution in the United States. J Clin Gastroenterol 2019;53(1):40–50.[↩]
- Basit H, Tyagi I, Koirala J. Hepatitis C. [Updated 2023 Mar 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430897[↩][↩][↩][↩]
- Parigi, T. L., Torres, M., & Aghemo, A. (2019). Upcoming direct acting antivirals for hepatitis C patients with a prior treatment failure. Clinical and molecular hepatology, 25(4), 360–365. https://doi.org/10.3350/cmh.2019.0022[↩]
- Basit H, Tyagi I, Koirala J. Hepatitis C. [Updated 2021 Jul 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430897[↩]
- Soi V, Daifi C, Yee J, Adams E. Pathophysiology and Treatment of Hepatitis B and C Infections in Patients With End-Stage Renal Disease. Adv Chronic Kidney Dis. 2019 Jan;26(1):41-50. doi: 10.1053/j.ackd.2018.10.004[↩]
- Mukhtar NA, Ness EM, Jhaveri M, Fix OK, Hart M, Dale C, Pratt C, Kowdley KV. Epidemiologic features of a large hepatitis C cohort evaluated in a major health system in the western United States. Ann Hepatol. 2019 Mar-Apr;18(2):360-365. doi: 10.1016/j.aohep.2018.12.003[↩]
- Smith DB, Bukh J, Kuiken C, Muerhoff AS, Rice CM, Stapleton JT, Simmonds P. Expanded classification of hepatitis C virus into 7 genotypes and 67 subtypes: updated criteria and genotype assignment web resource. Hepatology. 2014 Jan;59(1):318-27. doi: 10.1002/hep.26744[↩]
- Recommended Testing Sequence for Identifying Current Hepatitis C Virus (HCV) Infection. https://www.cdc.gov/hepatitis/HCV/PDFs/hcv_flow.pdf[↩]
- CDC. Testing for HCV infection: An update of guidance for clinicians and laboratorians. MMWR 2013;62(18). https://www.cdc.gov/hepatitis/HCV/PDFs/hcv_graph.pdf[↩]
- Association of Public Health Laboratories (APHL). Infectious Diseases, January 2019. Interpretation of Hepatitis C Virus Test Results: Guidance for Laboratories. https://www.aphl.org/aboutAPHL/publications/Documents/ID-2019Jan-HCV-Test-Result-Interpretation-Guide.pdf[↩][↩]
- Centers for Disease Control and Prevention (CDC), Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR 2001.50:1-42.[↩]
- Orland JR, Wright TL, Cooper S. Acute hepatitis C. Hepatology. 2001;33(2):321–7.[↩]
- Vanhommerig, J.W., et al., Hepatitis C virus (HCV) antibody dynamics following acute HCV infection and reinfection among HIV-infected men who have sex with men. Clin Infect Dis, 2014. 59(12): p. 1678-85.[↩][↩]
- Alter MJ, Margolis HS, Krawczynski K, Judson FN, Mares A, Alexander WJ, Hu PY, Miller JK, Gerber MA, Sampliner RE, et al. The natural history of community-acquired hepatitis C in the United States. The Sentinel Counties Chronic non-A, non-B Hepatitis Study Team. N Engl J Med. 1992;327(27):1899-1905.[↩]
- Initial Treatment of Adults with HCV Infection. https://www.hcvguidelines.org/treatment-naive[↩]
- American Association for the Study of Liver Diseases (AASLD) and the Infectious Diseases Society of America (IDSA). Recommendations for testing, management, and treating hepatitis C: HCV testing and linkage to care. https://www.hcvguidelines.org[↩]
- Mast EE, Hwang LY, Seto DS, Nolte FS, Nainan OV, Wurtzel H, Alter MJ. Risk factors for perinatal transmission of hepatitis C virus (HCV) and the natural history of HCV infection acquired in infancy. J Infect Dis. 2005;192(11):1880-9.[↩]