Contents
- What are head lice
- What causes head lice ?
- How did my child get head lice ?
- What do head lice look like ?
- How is head lice infestation diagnosed ?
- How do you get head lice
- Head lice symptoms
- Head lice prevention
- Best head lice treatment
What are head lice
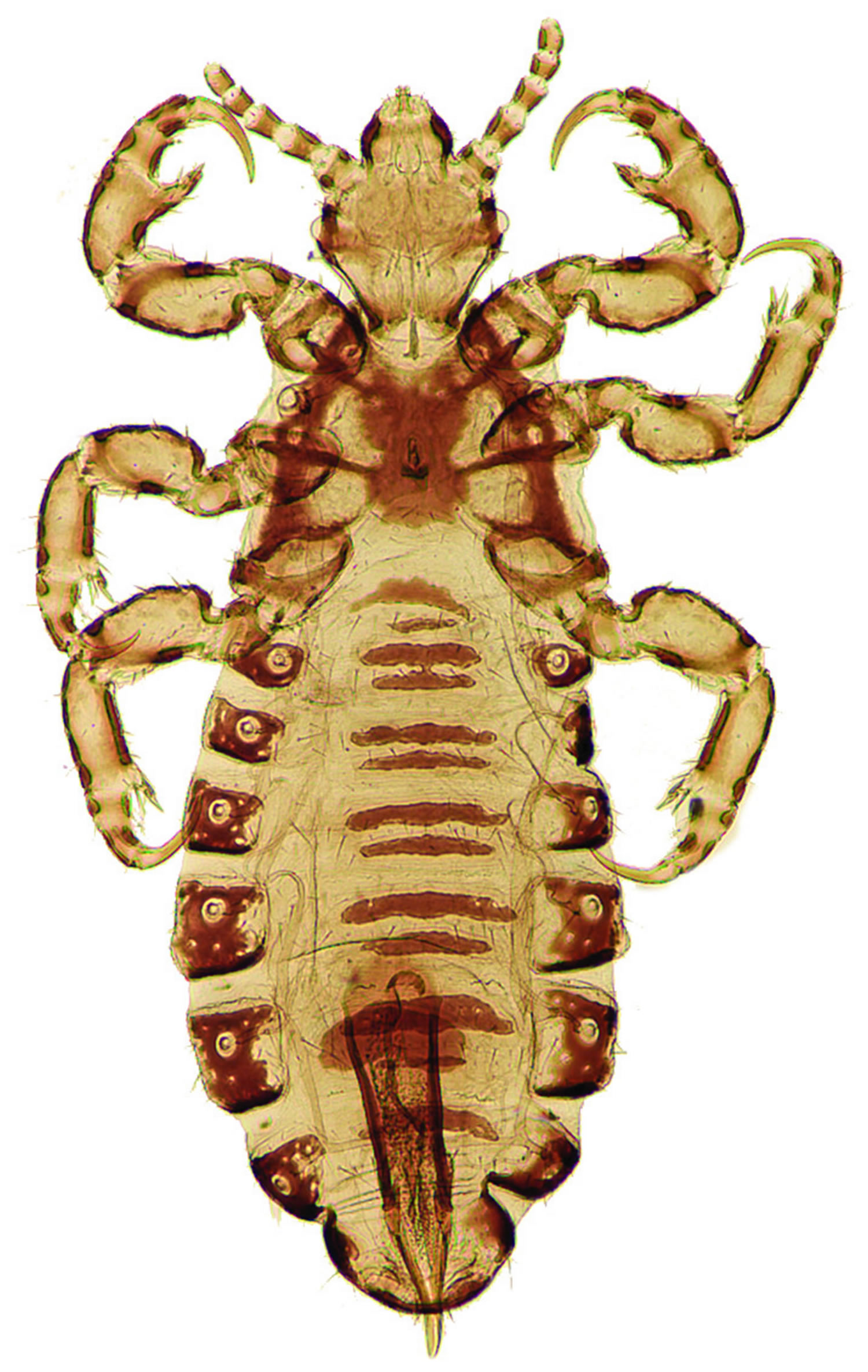
Head lice are parasitic wingless insects also called Pediculus humanus capitis 1, is an ectoparasite whose only host are humans. The head lice feed on blood several times daily and resides close to the scalp to maintain their body temperature. An adult louse is about the size of a sesame seed. The eggs, called nits, are even smaller – about the size of a knot in thread (see Figure 1 and 2). Lice and nits are found on or near the scalp, most often at the neckline and behind the ears.
The female louse lives about three to four weeks and lays approximately 10 eggs, or nits, a day. The eggs are incubated by body heat and hatch in 10 to 14 days. Once the eggs hatch, nymphs grow for about nine to 12 days, mate, and then females lay eggs. If not treated, this cycle may repeat itself every three weeks.
The gold standard for diagnosing head lice is finding a live louse on the head, which can be difficult. The eggs may be easier to see, especially at the nape of the neck or behind the ears, within 1 cm of the scalp.
Lice spread by close person-to-person contact. It is possible, but not common, to get lice by sharing personal belongings such as hats or hairbrushes. Children ages 3-11 and their families get head lice most often. Personal hygiene has nothing to do with getting head lice. Head lice do not spread disease.
Symptoms of head lice infestation are:
- Tickling feeling in the hair
- Frequent itching
- Sores from scratching
- Irritability and difficulty sleeping. Head lice are most active in the dark.
Treatment is recommended for people who have an active infestation of head lice. All household members and other close contacts should be checked and treated if necessary. Some experts also recommend treating anyone who shares a bed with an infested person. It is important to treat everyone at the same time.
What causes head lice ?
The head louse, or Pediculus humanus capitis, is a parasitic insect that can be found on the head, eyebrows, and eyelashes of people.
Head lice are found worldwide. In the United States, infestation with head lice is most common among pre-school children attending child care, elementary schoolchildren, and the household members of infested children. Although reliable data on how many people in the United States get head lice each year are not available, an estimated 6 million to 12 million infestations occur each year in the United States among children 3 to 11 years of age. In the United States, infestation with head lice is much less common among African-Americans than among persons of other races, possibly because the claws of the of the head louse found most frequently in the United States are better adapted for grasping the shape and width of the hair shaft of other races.
Head lice move by crawling; they cannot hop or fly. Head lice are spread by direct contact with the hair of an infested person. Anyone who comes in head-to-head contact with someone who already has head lice is at greatest risk. Spread by contact with clothing (such as hats, scarves, coats) or other personal items (such as combs, brushes, or towels) used by an infested person is uncommon. Personal hygiene or cleanliness in the home or school has nothing to do with getting head lice.
Where are head lice most commonly found ?
Head lice and head lice nits are found almost exclusively on the scalp, particularly around and behind the ears and near the neckline at the back of the head. Head lice or head lice nits sometimes are found on the eyelashes or eyebrows but this is uncommon. Head lice hold tightly to hair with hook-like claws at the end of each of their six legs. Head lice nits are cemented firmly to the hair shaft and can be difficult to remove even after the nymphs hatch and empty casings remain.
How did my child get head lice ?
Head-to-head contact with an already infested person is the most common way to get head lice. Head-to-head contact is common during play at school, at home, and elsewhere (sports activities, playground, slumber parties, camp).
Although uncommon, head lice can be spread by sharing clothing or belongings. This happens when lice crawl, or nits attached to shed hair hatch, and get on the shared clothing or belongings. Examples include:
- sharing clothing (hats, scarves, coats, sports uniforms) or articles (hair ribbons, barrettes, combs, brushes, towels, stuffed animals) recently worn or used by an infested person;
- or lying on a bed, couch, pillow, or carpet that has recently been in contact with an infested person.
Dogs, cats, and other pets do not play a role in the spread of head lice.
Do head lice spread disease ?
Head lice should not be considered as a medical or public health hazard. Head lice are not known to spread disease. Head lice can be an annoyance because their presence may cause itching and loss of sleep. Sometimes the itching can lead to excessive scratching that can sometimes increase the chance of a secondary skin infection.
Can head lice be spread by sharing sports helmets or headphones ?
Head lice are spread most commonly by direct contact with the hair of an infested person. Spread by contact with inanimate objects and personal belongings may occur but is very uncommon. Head lice feet are specially adapted for holding onto human hair. Head lice would have difficulty attaching firmly to smooth or slippery surfaces like plastic, metal, polished synthetic leathers, and other similar materials.
Can wigs or hair pieces spread lice ?
Head lice and their eggs (nits) soon perish if separated from their human host. Adult head lice can live only a day or so off the human head without blood for feeding. Nymphs (young head lice) can live only for several hours without feeding on a human. Nits (head lice eggs) generally die within a week away from their human host and cannot hatch at a temperature lower than that close to the human scalp. For these reasons, the risk of transmission of head lice from a wig or other hairpiece is extremely small, particularly if the wig or hairpiece has not been worn within the preceding 48 hours by someone who is actively infested with live head lice.
Can swimming spread lice ?
Data show that head lice can survive under water for several hours but are unlikely to be spread by the water in a swimming pool. Head lice have been seen to hold tightly to human hair and not let go when submerged under water. Chlorine levels found in pool water do not kill head lice.
Head lice may be spread by sharing towels or other items that have been in contact with an infested person’s hair, although such spread is uncommon. Children should be taught not to share towels, hair brushes, and similar items either at poolside or in the changing room.
Swimming or washing the hair within 1–2 days after treatment with some head lice medicines might make some treatments less effective. Seek the advice of your health care provider or health department if you have questions.
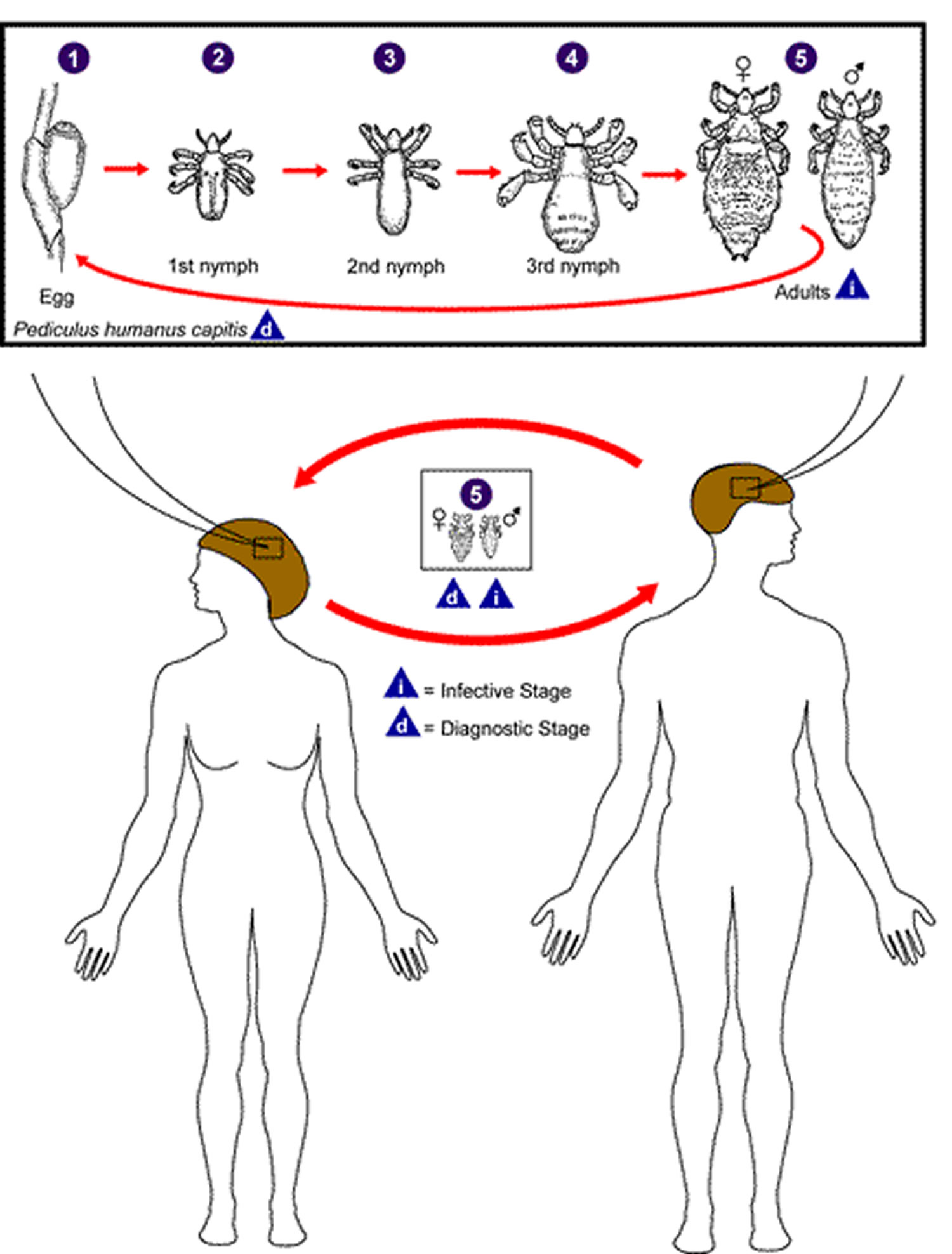
Figure 1. Head lice
What do head lice look like ?
Head lice have three forms: the egg (also called a nit), the nymph, and the adult 2.
Eggs: Nits are head lice eggs. They are hard to see and are often confused for dandruff or hair spray droplets. Nits are laid by the adult female and are cemented at the base of the hair shaft nearest the scalp The number 1. They are 0.8 mm by 0.3 mm, oval and usually yellow to white. Nits take about 1 week to hatch (range 6 to 9 days). Viable eggs are usually located within 6 mm of the scalp.
Nymphs: The egg hatches to release a nymph The number 2. The nit shell then becomes a more visible dull yellow and remains attached to the hair shaft. The nymph looks like an adult head louse, but is about the size of a pinhead. Nymphs mature after three molts (The number 3, The number 4) and become adults about 7 days after hatching.
Adults: The adult louse is about the size of a sesame seed, has 6 legs (each with claws), and is tan to grayish-white The number 5. In persons with dark hair, the adult louse will appear darker. Females are usually larger than males and can lay up to 8 nits per day. Adult lice can live up to 30 days on a person’s head. To live, adult lice need to feed on blood several times daily. Without blood meals, the louse will die within 1 to 2 days off the host.
Figure 2. Head lice life cycle
How is head lice infestation diagnosed ?
Misdiagnosis of head lice infestation is common. The diagnosis of head lice infestation is best made by finding a live nymph or adult louse on the scalp or hair of a person.
Because adult and nymph lice are very small, move quickly, and avoid light, they may be difficult to find. Use of a fine-toothed louse comb may facilitate identification of live lice.
If crawling lice are not seen, finding nits attached firmly within ¼ inch of the base of hair shafts suggests, but does not confirm, the person is infested. Nits (head lice eggs) frequently are seen on hair behind the ears and near the back of the neck. Nits that are attached more than ¼ inch from the base of the hair shaft are almost always non-viable (hatched or dead). Head lice and nits can be visible with the naked eye, although use of a magnifying lens may be necessary to find crawling lice or to identify a developing nymph inside a viable nit. Nits are often confused with other particles found in hair such as dandruff, hair spray droplets, and dirt particles.
If no nymphs or adults are seen, and the only nits (head lice eggs) found are more than ¼ inch from the scalp, then the infestation is probably old and no longer active — and does not need to be treated.
Figure 3. Head lice

How do you get head lice
In the United States, infestation with head lice (Pediculus humanus capitis) is most common among preschool- and elementary school-age children and their household members and caretakers. Head lice are not known to transmit disease; however, secondary bacterial infection of the skin resulting from scratching can occur with any lice infestation.
Getting head lice is not related to cleanliness of the person or his or her environment.
Head lice are mainly spread by direct contact with the hair of an infested person. The most common way to get head lice is by head-to-head contact with a person who already has head lice. Such contact can be common among children during play at:
- school,
- home, and
- elsewhere (e.g., sports activities, playgrounds, camp, and slumber parties).
Uncommonly, transmission may occur by:
- wearing clothing, such as hats, scarves, coats, sports uniforms, or hair ribbons worn by an infested person;
- using infested combs, brushes or towels; or
- lying on a bed, couch, pillow, carpet, or stuffed animal that has recently been in contact with an infested person.
Reliable data on how many people get head lice each year in the United States are not available; however, an estimated 6 million to 12 million infestations occur each year in the United States among children 3 to 11 years of age. Some studies suggest that girls get head lice more often than boys, probably due to more frequent head-to-head contact.
In the United States, infestation with head lice is much less common among African-Americans than among persons of other races. The head louse found most frequently in the United States may have claws that are better adapted for grasping the shape and width of some types of hair but not others.
Head lice symptoms
Head lice are not known to transmit any disease and therefore are not considered a health hazard.
Head lice infestations can be asymptomatic, particularly with a first infestation or when an infestation is light. Itching (“pruritus”) is the most common symptom of head lice infestation and is caused by an allergic reaction to louse bites. It may take 4–6 weeks for itching to appear the first time a person has head lice.
Other symptoms may include:
- a tickling feeling or a sensation of something moving in the hair;
- irritability and sleeplessness; and
- sores on the head caused by scratching. These sores caused by scratching can sometimes become infected with bacteria normally found on a person’s skin.
Head lice prevention
Head lice are spread most commonly by direct head-to-head (hair-to-hair) contact. However, much less frequently they are spread by sharing clothing or belongings onto which lice have crawled or nits attached to shed hairs may have fallen. The risk of getting infested by a louse that has fallen onto a carpet or furniture is very small. Head lice survive less than 1–2 days if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the scalp.
The following are steps that can be taken to help prevent and control the spread of head lice:
- Avoid head-to-head (hair-to-hair) contact during play and other activities at home, school, and elsewhere (sports activities, playground, slumber parties, camp).
- Do not share clothing such as hats, scarves, coats, sports uniforms, hair ribbons, or barrettes.
- Do not share combs, brushes, or towels. Disinfest combs and brushes used by an infested person by soaking them in hot water (at least 130°F) for 5–10 minutes.
- Do not lie on beds, couches, pillows, carpets, or stuffed animals that have recently been in contact with an infested person.
- Machine wash and dry clothing, bed linens, and other items that an infested person wore or used during the 2 days before treatment using the hot water (130°F) laundry cycle and the high heat drying cycle. Clothing and items that are not washable can be dry-cleaned OR sealed in a plastic bag and stored for 2 weeks.
- Vacuum the floor and furniture, particularly where the infested person sat or lay. However, spending much time and money on housecleaning activities is not necessary to avoid reinfestation by lice or nits that may have fallen off the head or crawled onto furniture or clothing.
- Do not use fumigant sprays or fogs; they are not necessary to control head lice and can be toxic if inhaled or absorbed through the skin.
To help control a head lice outbreak in a community, school, or camp, children can be taught to avoid activities that may spread head lice.
Best head lice treatment
Treatment for head lice is recommended for persons diagnosed with an active infestation. All household members and other close contacts should be checked; those persons with evidence of an active infestation should be treated. Some experts believe prophylactic treatment is prudent for persons who share the same bed with actively-infested individuals. All infested persons (household members and close contacts) and their bedmates should be treated at the same time.
Pediculicides (medicines that kill lice) are the most effective treatment for head lice infestation, according to the American Academy of Pediatrics. Instructions on proper use of these products should be given carefully. Safety and efficacy should be taken into account.
For pediculicides that are only weakly ovicidal (kill eggs) or not ovicidal, routine retreatment is recommended. For those that are more strongly ovicidal, retreatment is recommended only if live (crawling) lice are still present several days after treatment (see recommendation for each medication). To be most effective, retreatment should occur after all eggs have hatched but before new eggs are produced.
When treating head lice, supplemental measures can be combined with recommended medicine; however, such additional (non-pharmacologic) measures generally are not required to eliminate a head lice infestation. For example, hats, scarves, pillow cases, bedding, clothing, and towels worn or used by the infested person in the 2-day period just before treatment is started can be machine washed and dried using the hot water and hot air cycles because lice and eggs are killed by exposure for 5 minutes to temperatures greater than 53.5°C (128.3°F). Items that cannot be laundered may be dry-cleaned or sealed in a plastic bag for two weeks. Items such as hats, grooming aids, and towels that come in contact with the hair of an infested person should not be shared. Vacuuming furniture and floors can remove an infested person’s hairs that might have viable nits attached.
Topical corticosteroids and oral antihistamines may be beneficial for relieving inflammation of the skin in response to topical therapeutic agents.
The oral agents sulfamethoxazole-trimethoprim and ivermectin are sometimes used to treat head lice, but they are not currently approved by the U.S. Food and Drug Administration for use as a pediculicide.
Treat the infested person(s): Requires using an Over-the-counter (OTC) or prescription medication.
Follow these treatment steps:
- Before applying treatment, it may be helpful to remove clothing that can become wet or stained during treatment.
- Apply lice medicine, also called pediculicide, according to the instructions contained in the box or printed on the label. If the infested person has very long hair (longer than shoulder length), it may be necessary to use a second bottle. Pay special attention to instructions on the label or in the box regarding how long the medication should be left on the hair and how it should be washed out.
- Have the infested person put on clean clothing after treatment.
- If a few live lice are still found 8–12 hours after treatment, but are moving more slowly than before, do not retreat. The medicine may take longer to kill all the lice. Comb dead and any remaining live lice out of the hair using a fine–toothed nit comb.
- If after 8–12 hours of treatment, no dead lice are found and lice seem as active as before, the medicine may not be working. Do not retreat until speaking with your health care provider; a different pediculicide may be necessary. If your health care provider recommends a different pediculicide, carefully follow the treatment instructions contained in the box or printed on the label.
- Nit (head lice egg) combs, often found in lice medicine packages, should be used to comb nits and lice from the hair shaft. Many flea combs made for cats and dogs are also effective.
- After each treatment, checking the hair and combing with a nit comb to remove nits and lice every 2–3 days may decrease the chance of self–reinfestation.
- Continue to check for 2–3 weeks to be sure all lice and nits are gone. Nit removal is not needed when treating with spinosad topical suspension.
- Retreatment is meant to kill any surviving hatched lice before they produce new eggs. For some drugs, retreatment is recommended routinely about a week after the first treatment (7–9 days, depending on the drug) and for others only if crawling lice are seen during this period. Retreatment with lindane shampoo is not recommended.
- Retreatment of head lice usually is recommended because no approved pediculicide is completely ovicidal. To be most effective, retreatment should occur after all eggs have hatched but before before new eggs are produced. The retreatment schedule can vary depending on the pediculicide used.
- Removal of all nits after successful treatment with a pediculicide is not necessary to prevent further spread. Removal of nits after treatment with a pediculicide may be done for aesthetic reasons, or to reduce diagnostic confusion and the chance of unnecessary retreatment. Because pediculicides are not 100% ovicidal (i.e. do not kill all the egg stages), some experts recommend the manual removal of nits that are attached within ¼ inch of the base of the hair shaft.
Supplemental Measures:
Head lice do not survive long if they fall off a person and cannot feed. You don’t need to spend a lot of time or money on housecleaning activities. Follow these steps to help avoid re–infestation by lice that have recently fallen off the hair or crawled onto clothing or furniture.
- Machine wash and dry clothing, bed linens, and other items that the infested person wore or used during the 2 days before treatment using the hot water (130°F) laundry cycle and the high heat drying cycle. Clothing and items that are not washable can be dry–cleaned ORsealed in a plastic bag and stored for 2 weeks.
- Soak combs and brushes in hot water (at least 130°F) for 5–10 minutes.
- Vacuum the floor and furniture, particularly where the infested person sat or lay. However, the risk of getting infested by a louse that has fallen onto a rug
- or carpet or furniture is very small. Head lice survive less than 1–2 days if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the human scalp. Spending much time and money on housecleaning activities is not necessary to avoid reinfestation by lice or nits that may have fallen off the head or crawled onto furniture or clothing.
- Do not use fumigant sprays; they can be toxic if inhaled or absorbed through the skin.
Permethrin (1%)
Currently, permethrin is the recommended treatment for head lice. It has low mammalian toxicity and does not cause an allergic reaction in patients with plant allergies. It is a cream rinse applied to hair that is first shampooed with a nonconditioning shampoo and towel dried. After 10 minutes, it is rinsed off, but leaves a residue that is designed to kill nymphs emerging from the eggs not killed with the first application. If live lice are seen seven to 10 days later, application should be repeated. Resistance to 1 percent permethrin has been reported, but the prevalence of this is not known.
Pyrethrins Plus Piperonyl Butoxide
Pyrethrins plus piperonyl butoxide are neurotoxic to lice and have extremely low mammalian toxicity. This treatment should be avoided in patients allergic to chrysanthemums. It is a shampoo that is applied to dry hair and rinsed out after 10 minutes. Twenty to 30 percent of the eggs remain viable after treatment. A second treatment is needed seven to 10 days later to kill newly emerged nymphs. Resistance of adult lice to these products has been reported.
Lindane (1%)
Lindane is a shampoo that should be left on for no more than 10 minutes with a second application in seven to 10 days. Resistance has been reported worldwide, and it has low ovicidal activity. It is only available by prescription and should be used cautiously because several cases of seizures in children have been reported.
Malathion (0.5%)
Malathion (Ovide lotion) is a prescription lotion approved by the U.S. Food and Drug Administration (FDA) for the treatment of head lice infestation. Malathion is applied to the hair, left to air dry, then washed off after eight to 12 hours. Malathion lotion is both pediculicidal (kills live lice) and partially ovicidal (kills some lice eggs), but should be reapplied if live lice are seen in seven to 10 days. Because of its high alcohol content, it is highly flammable, and there is a risk of severe respiratory depression if it is ingested. Malathion should be used only in cases resistant to other treatments.
The safety and effectiveness of malathion lotion (Ovide*) has not been established by well controlled trials in children less than 6 years old. Malathion is contraindicated in children younger than 2 years of age.
What steps to follow when using malathion to treat head lice
Step 1: Treat the person(s) infested with head lice:
- Always follow your physician’s and pharmacist’s instructions and those contained inside the package or written on the label.
- Carefully apply the malathion lotion to dry hair until the scalp and hair are wet and thoroughly coated, especially behind the ears and on the back of the head and neck.
- The manufacturer recommends leaving the medication on the hair, uncovered, for 8–12 hours. Allow the hair to dry naturally; do not use an electrical heat source, including a hair dryer or curling iron while the hair is wet. Have the person being treated put on clean clothing once the medication has been applied. Consider treating just before bedtime. Cover any pillow(s) with a towel to keep the medication from staining the pillow.
- After 8–12 hours, thoroughly shampoo the hair; rinse and use a fine-toothed nit comb, usually included in the package, to remove dead lice and nits from the hair.
- After treatment, use a fine-toothed nit comb to check the hair for live lice every 2–3 days for 2–3 weeks until sure that all lice are gone.
- If live lice are found 7 to 9 days after treatment, retreat with a second application of the same medication.
Warnings and Precautions:
- Malathion may cause stinging, especially if the scalp has open sores from scratching.
- Keep medication out of the eyes.
- Malathion is flammable; keep medication and wet hair away from heat sources such as hair dryers, electric curlers, cigarettes, or open flames.
- Pregnant and nursing mothers should use malathion only after consulting their physician.
Step 2: Consider additional household measures:
Head lice do not live long (less than 1–2 days) if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the human scalp. You do not need to spend a lot of time or money on housecleaning activities. Follow these steps to help avoid re-infestation by live lice or nits that may have recently fallen off the head or crawled onto clothing or furniture.
- To kill lice and nits that may have fallen or crawled off the head onto clothing or other articles, machine wash clothing, bed linens, and other items (e.g. towels, stuffed animals, comforters, blankets, etc.) that the infested person wore, slept on, or used during the 2 days before treatment. Use the hot water (at least 130°F) cycle. Dry the laundry using the high heat setting for at least 20 minutes. Items that are not washable can be dry-cleaned.
OR
stored in a sealed plastic bag for 2 weeks.
- Soak combs and brushes in hot water (at least 130°F) for 5–10 minutes.
- Vacuum the floor and furniture, particularly where the infested person sat or lay. However, the risk of getting infested by a louse or a nit that was attached to a shed hair that has fallen onto a carpet or furniture is very small. Head lice survive less than 1–2 days if they fall off a person and cannot feed; nits cannot hatch and usually die within a week if they are not kept at the same temperature as that found close to the human scalp. Spending much time and money on housecleaning activities is not necessary to avoid reinfestation by lice that have crawled or nits on shed hairs that may have fallen off the head.
- Do not use fumigant sprays; they can be toxic if inhaled or absorbed through the skin.
Step 3: Prevent Reinfestation:
Lice are spread most commonly by direct head-to-head (hair-to-hair) contact and much less frequently by sharing clothing or belongings onto which lice or nits may have crawled or fallen. Teach children to avoid types of play and other activities that may spread lice.
- Avoid head-to-head (hair-to-hair) contact during play and other activities at home, school, and elsewhere (slumber parties, sports activities, camp, playground).
- Do not share clothing such as hats, scarves, coats, sports uniforms, hair ribbons, or barrettes.
- Do not share combs, brushes, or towels.
- Do not lie on beds, couches, pillows, carpets, or stuffed animals that have recently been in contact with an infested person.
Is a second treatment with Malathion needed ?
Maybe. If live lice still are found after 7–9 days, a second treatment with malathion lotion may be given. Other family members should be checked for signs of infestation.
Are treatment failures with malathion common ?
No, however reinfestation can occur.
Spinosad (Natroba)
Spinosad (Natroba) is a prescription topical pediculicide labeled for the treatment of head lice in patients four years and older 3. In addition to its pediculicidal activity, spinosad has also been shown to have ovicidal activity 4. Unrelated to other insecticides, spinosad is produced by a bacterium, Saccharopolyspora spinosa 4. Although it is neurotoxic to lice, it does not seem to have a similar effect on humans or animals. Spinosad is generally well tolerated. The most common adverse effects are erythema at the site of application (3.1%), ocular hyperemia (2.2%), and irritation at the site of application (0.9%) 4. One treatment (a 120-mL bottle) of spinosad will cost patients approximately $147.
Published data regarding the effectiveness of spinosad are limited. In a study involving 120 children two years and older, 86.1% of patients in the spinosad treatment group were free of live lice 14 days after a single treatment vs. 25.6% of patients who were given placebo (number needed to treat = 2) 5. The authors of two studies with a total of 1,038 participants six months and older randomized patients to receive one treatment of spinosad 0.9% crème rinse without nit combing or permethrin 1% crème rinse (Nix) with combing at baseline. If live lice were present at day 7, patients received an additional application 4. Those treated with spinosad were more likely to be lice-free two weeks after the final dose than patients treated with permethrin (86% vs. 44%, respectively 4. A single treatment was adequate for most patients treated with spinosad (74%), but not for those treated with permethrin (38%) 4. Spinosad has not been compared with pyrethrins 0.33%/piperonyl butoxide 4% shampoo or mousse (Rid), malathion, lindane, benzyl alcohol, or ivermectin.
Spinosad does not have any major adverse effects because topical application does not result in systemic exposure 3. Unlike lindane, spinosad has not been shown to cause neurologic toxicities, such as seizures and death. Additionally, spinosad does not have the potential to cause cholinergic symptoms or adverse effects from systemic alcohol absorption that are associated with malathion (Ovide) therapy.
However, spinosad does contain benzyl alcohol in its formulation. Benzyl alcohol has been linked to serious adverse effects and death when used as a bacteriostatic preservative in intravenous fluids administered to newborns. For this reason, the manufacturer recommends avoiding spinosad in children younger than six months. Furthermore, breastfeeding mothers who are being treated with spinosad should not use breast milk that is produced during the eight hours following treatment. Spinosad is a U.S. Food and Drug Administration pregnancy category B drug 3.
Nit Removal
After treatment with a pediculicide, removal of the eggs is not necessary to prevent spreading the infestation. Because none of the pediculicides is 100 percent ovicidal, removal of the eggs after treatment is recommended for aesthetic reasons or to decrease diagnostic confusion. Nit combs and other products are available to ease the process. Vinegar or vinegar-based products that are applied to the hair for three minutes before combing help loosen the nits attached to the hair shaft.
The actual prevalence of resistance is not known. Family physicians must consider several explanations when facing a persistent case of head lice, including misdiagnosis, noncompliance with treatment protocol, reinfestation, lack of ovicidal properties of the treatment product, or resistance to the pediculicide.
According to the American Academy of Pediatrics, if a case of head lice is identified, all household members should be checked, and only those with live lice or eggs within 1 cm of the scalp should be treated. It is prudent to treat family members who share a bed with the person who is infected and to clean hair care items and bedding belonging to that person.
A child with active head lice has likely had the infestation for a month or more by the time it is discovered and poses little risk to others. The child does not have a resulting health problem and should stay in class but be discouraged from close, direct head contact with others. The child’s parents should be notified immediately, and confidentiality should be maintained so the child is not embarrassed. A child should be allowed to return to school after proper treatment and should not miss valuable school time because of head lice.
Head lice screening programs have not had a significant effect on the incidence of head lice in the school setting over time and are not cost effective.
If the treatment for head lice doesn’t seem to be working, does this mean the lice are resistant and I need a different treatment ?
The following are several common reasons why treatment for head lice may fail sometimes:
- Misdiagnosis. The symptoms are not caused by an active head lice infestation.
- Applying the treatment to hair that has been washed with conditioning shampoo or rinsed with hair conditioner. Conditioners can act as a barrier that keeps the head lice medicine from adhering to the hair shafts; this can reduce the effectiveness of the treatment.
- Not following carefully the instructions for the treatment that is used. Some examples of this include not applying a second treatment if instructed to do so, or retreating too soon after the first treatment before all the nits are hatched and the newly hatched head lice can be killed. Another reason is retreating too late after new eggs have already been deposited.
- Resistance of the head lice to the treatment used. The head lice may have become resistant to the treatment. If the treatment used does not kill the head lice, your health care provider and pharmacist can help you be sure the treatment was used correctly and may recommend a completely different product if they think the head lice are resistant to the first treatment.
- Reinfestation. The person was treated successfully and the lice were eliminated, but then the person becomes infested again by lice spread from another infested person. Sometimes reshampooing the hair too soon (less than 2 days) after correctly applying and removing permethin can reduce or eliminate any residual (continued) killing effect on the lice.
- Parasites – Lice – Head Lice. https://www.cdc.gov/parasites/lice/head/biology.html[↩]
- Parasites – Lice – Head Lice. Centers for Disease Control and Prevention. https://www.cdc.gov/parasites/lice/head/biology.html[↩]
- Highlights of prescribing information. Natroba (spinosad) topical suspension packet insert. Carmel, Ind.: ParaPRO, LLC. www.natroba.com/full prescribing information.pdf[↩][↩][↩]
- Stough D, Shellabarger S, Quiring J, Gabrielsen AA Jr. Efficacy and safety of spinosad and permethrin creme rinses for pediculosis capitus (head lice). Pediatrics. 2009;124(3):e389–e395.[↩][↩][↩][↩][↩][↩]
- Villegas SC, Breitzka RL. Head lice and the use of spinosad. Clin Ther. 2012;34(1):14–23.[↩]