Contents
What is a keloid
Keloid is a thick, irregular scar caused by excessive tissue growth at the site of an incision (a cut made in the body to perform surgery) or wound 1. After your skin is injured, both skin cells and connective tissue cells (fibroblasts) begin multiplying to repair the damage by forming a scar 2. A scar is made up of ‘connective tissue’, gristle-like fibers deposited in the skin by the fibroblasts to hold the wound closed. With keloids, the fibroblasts continue to multiply even after the wound is filled in. Thus keloids project above the surface of the skin and form large mounds of scar tissue. In some people, the scar tissue keeps forming long after the wound heals. This extra scar tissue causes a red, raised area on your skin that is called a keloid. Keloids don’t usually hurt, but they may feel itchy or sensitive to the touch.
Keloids may form on any part of the body, although the upper chest, shoulders and upper back are especially prone to keloid formation. Symptoms include pigmentation of the skin, itchiness, redness, unusual sensations and pain.
Keloids are dense, thick nodules, typically found at areas of previously injured skin (burns, lacerations), or they may arise spontaneously on normal skin. They may be single or multiple. Over weeks to months, these nodules can become painful, tender, itchy (pruritic), and grow to become very large, up to about 30 cm. They can be unsightly, and patients often seek removal.
It is estimated that keloids occur in about 10% of people. While most people never form keloids, others develop them after minor injuries, even insect bites or pimples. Darkly pigmented people seem to be more prone to forming keloids. Men and women are equally affected.
Keloids are considered a benign tumor, but they are mainly a cosmetic nuisance and never become malignant 3. Operating on a keloid usually stimulates more scar tissue to form, so people with keloids may have been told that there is nothing that can be done to get rid of them.
Figure 1. Keloid

Keloids can form after skin injuries from 4:
- Acne
- Burns
- Chickenpox
- Ear or body piercing
- Minor scratches
- Cuts from surgery or trauma
- Vaccination sites
Keloids are most common in people younger than 30. Blacks, Asians, and Hispanics are more prone to developing keloids. Keloids often run in families. Sometimes, a person may not recall what injury caused a keloid to form.
Figure 2. Keloid on face after acne

Symptoms of keloid scar
Keloids are usually seen on the neck, ear lobes, legs or arms, and on the upper trunk, especially the chest. They frequently follow the lines of injury. Spontaneous keloids are common on the mid-chest. Keloids are smooth and shiny, firm to the touch, red, hyperpigmented or skin-colored nodules with regular or irregular ridges. Keloids may develop projections that extend beyond the area of injury.
A keloid may be 5:
- Flesh-colored, red, or pink
- Located over the site of a wound or injury
- Lumpy or ridged
- Tender and itchy
- Irritated from friction such as rubbing on clothing
A keloid will tan darker than the skin around it if exposed to sun during the first year after it forms. The darker color may not go away.
Keloid diagnosis
Your doctor will look at your skin to see if you have a keloid. A skin biopsy may be done to rule out other types of skin growths (tumors).
What causes keloids
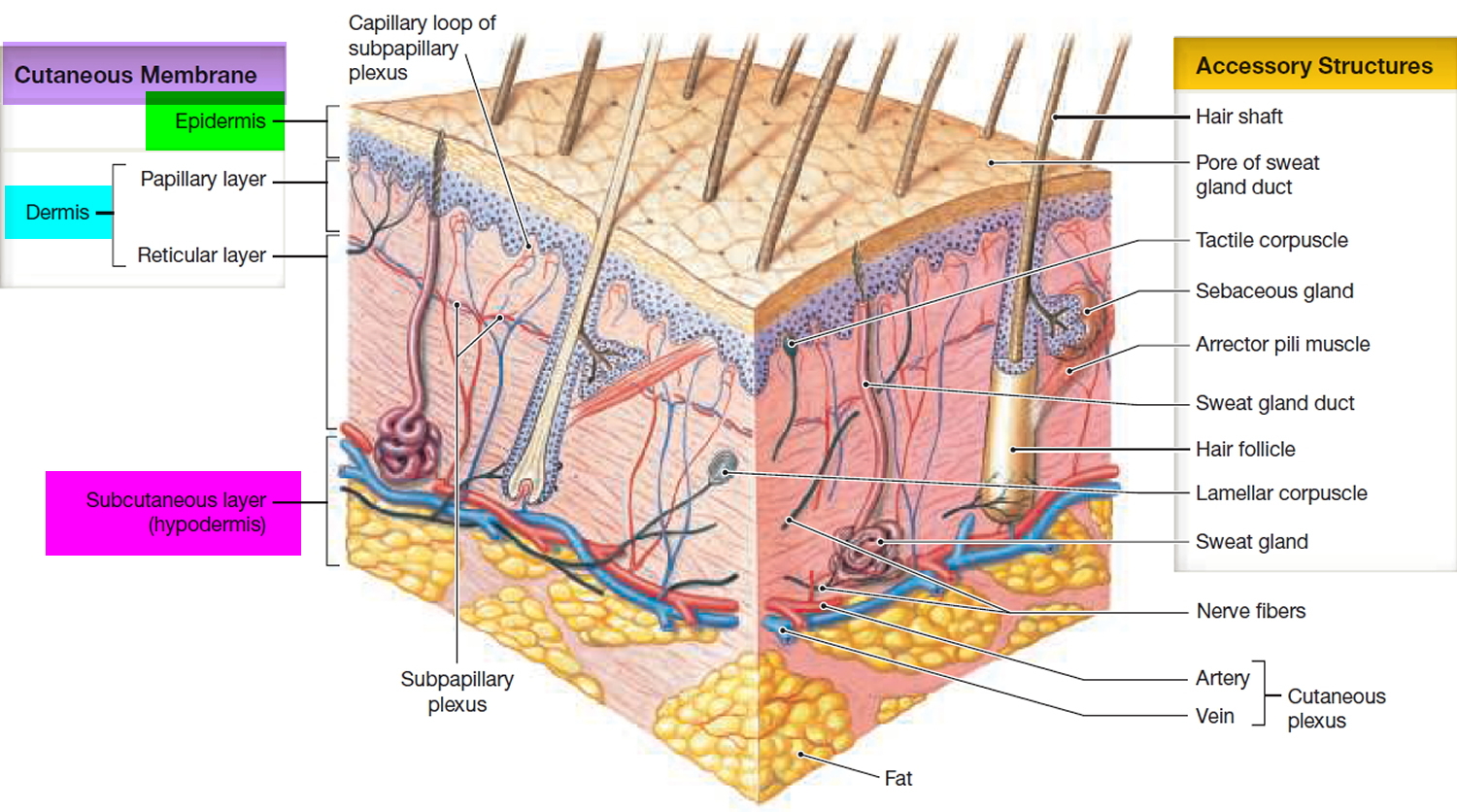
The skin is the largest organ on your body and it protects you against dangerous environmental factors and water loss. Skin is composed of two main layers: the dermis and the epidermis. The dermis contains a variable amount of fat, collagen, and elastic fibers that provide strength and flexibility to the skin.
Keloids are benign hyperproliferative growths of dermal fibroblasts characterized by the excessive deposition of extracellular matrix components, especially collagen, fibronectin, elastin, proteoglycans, and growth factors such as transforming growth factor (TGF) β 6. The mechanisms of keloid formation include alterations in growth factors, collagen turnover and tension alignment, as well as genetic and immunological contributions. Trauma, foreign-body reactions, infections, and endocrine dysfunctions have all been proposed as risk factors for the development of keloids after surgery in genetically susceptible people 7. Keloid disease affects both sexes equally 8 and can occur at every age but is more prevalent between the ages of 10 and 30 9.
Genetic basis for keloid disease
The incidence of keloids is different among populations that reflect different etiologic factors. The worldwide keloid disease prevalence varies according to ethnicity. Patients with darker skin, however, have a higher prevalence than those with lighter pigmentation 10. It is the fifth most common skin disease in adult black patients in the United Kingdom 11 and the most common skin disease among ethnic Chinese patients in Asia 12. In addition, many reports have been published on familial keloid cases 9, 13, 14, reflecting the importance of genetic factors among these families. Finally, the high frequency of identical twins both developing keloids also strongly supports a role for genetics in keloid etiology 15.
Both autosomal dominant with incomplete penetrance and variable expression modes 16 as well as autosomal recessive modes of inheritance 17 have been seen among families with keloid disease. Clinical and genetic heterogeneity with a variable clinical expressivity between families and within the affected members of same family has been noted 9, 13, 14. While the autosomal dominant mode of inheritance with incomplete penetrance is the most common reported model for keloid disease, it remains unclear whether keloid disease is a simple Mendelian or a complex oligogenic disorder. As reviewed more recently, it is well known that environmental factors can trigger the formation of keloids in genetically susceptibility individuals 18. In addition, studies on people of different ethnicities have discovered non-overlapping associated genes and genomic regions. Taken together, these investigations indicate that a complex inheritance model with contributions from multiple genetic factors along with triggering environmental influences could be the best model for keloid disease. More specifically, it seems plausible that an autosomal gene may play a major role in combination with more moderate recessive gene effects.
Figure 3. Skin structure
Who’s at risk of keloid scar ?
Keloids affect people of all ages, but most patients start developing keloids in their 20s. Keloids are most frequent in individuals of African and Mediterranean ancestries, but they can appear in people of any race.
You are more likely to develop a keloid if:
- You are black, Latino or Asian
- You are younger than 30 years of age
- You are pregnant
- You are a teenager going through puberty
- You have a history of keloids in your family
People who have darker skin are 15% to 20% more likely to develop keloids. Certain areas of the body are more likely to scar than others. Keloids usually develop on the chest, shoulders, earlobes and cheeks.
How to prevent keloids
Avoid unnecessary skin injury, such as multiple piercing.
Keloids may be often be prevented by using a pressure dressing, silicone gel pad or paper tape over the injury site. These are left on for 23 of 24 hours each day. This treatment is after healing of the wound or injury, usually within a month.
When you are in the sun:
- Cover a keloid that is forming with a patch or adhesive bandage.
- Use sunblock.
Continue to follow these steps for at least 6 months after injury or surgery for an adults. Children may need up to 18 months of prevention.
Imiquimod (immunomodulators) cream may help prevent keloids from forming after surgery. The cream also prevents keloids from returning from after they are removed.
How to treat keloids
Keloids often DO NOT need treatment. If the keloid bothers you, these things can be done to reduce the size 19, 20, 21:
- Corticosteroid injections. The best initial treatment is to inject long-acting cortisone (steroid) into the keloid once a month. Inflamed keloids often respond to steroid injections near the site. Monthly corticosteroid injections (eg, triamcinolone acetonide 5 to 40 mg/mL) into the lesion sometimes flatten the keloid. There is a risk of thinning of the skin (atrophy) with steroid injections.
- Freezing (cryotherapy) and/or freezing (cryosurgery) plus steroid injections. Cryosurgery is an excellent treatment for keloids that are small and occur on lightly pigmented skin. It is often combined with monthly cortisone injections.
- Laser therapy with a pulsed-dye laser to actively expanding lesions. Laser treatment is very good at improving skin texture and color, but doesn’t always flatten out the keloid.
- Radiation. For severe cases, the keloid can surgically excised and given x-ray treatments to the site immediately afterwards, usually the on the same day. This works in about 85% of the most severe cases. Electron beam radiation can be used, which will not go deep enough to affect internal organs. Orthovoltage radiation is more penetrating and slightly more effective. There have not been any reports of this causing any form of cancer in many years of use, but it is very expensive.
- Surgical removal. Surgery plus radiation therapy to the affected area. Surgical removal (excision) of keloids may lead to the keloid coming back (recurring) larger than it was before the excision. Surgical excision is more successful if preceded and followed by a series of intralesional corticosteroid injections.
- Gel sheeting (applying a soft, semiocclusive dressing made of cross-linked polymethylsiloxane polymer, or silicone) or pressure garments are other adjuncts to prevent recurrence.
- There has been some success in treating small earlobe keloids with pressure or “clip-on” earrings.
- Other injectable agents, such as interferon alpha and gamma.
These treatments, especially surgery, sometimes cause the keloid scar to become larger.
Outlook (Prognosis) of keloid
Keloids usually are not harmful to your health, but they may affect how you look.
When to Contact a Medical Professional
See your health care provider if:
- You develop keloids and want to have them removed or reduced
- You develop new symptoms.
- Keloid. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0022137/[↩]
- Keloids. American Academy of Family Physicians. https://familydoctor.org/condition/keloids[↩]
- Keloids And Hypertrophic Scars. http://www.aocd.org/?page=KeloidsAndHypertroph[↩]
- Keloids. Medline Plus. https://medlineplus.gov/ency/article/000849.htm[↩]
- Patterson JW. Disorders of collagen. In: Patterson JW, ed. Weedon’s Skin Pathology. 4th ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2016:chap 11.[↩]
- Medical and surgical therapies for keloids. Kelly AP. Dermatol Ther. 2004; 17(2):212-8. https://www.ncbi.nlm.nih.gov/pubmed/15113289/[↩]
- Kelly AP. Keloids. Dermatol Clin. 1988;6:413–424. https://www.ncbi.nlm.nih.gov/pubmed/3048824[↩]
- Shaffer JJ, Taylor SC, Cook-Bolden F. Keloidal scars: a review with a critical look at therapeutic options. J Am Acad Dermatol. 2002;46:S63–S97. https://www.ncbi.nlm.nih.gov/pubmed/11807470[↩]
- Marneros AG, Norris JE, Olsen BR, et al. Clinical genetics of familial keloids. Arch Dermatol. 2001;137:1429–1434. https://www.ncbi.nlm.nih.gov/pubmed/11708945[↩][↩][↩]
- LeFlore IC. Misconceptions regarding elective plastic surgery in the black patient. Journal of the National Medical Association. 1980;72(10):947-948. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2552534/pdf/jnma00042-0027.pdf[↩]
- Child FJ, Fuller LC, Higgins EM, et al. A study of the spectrum of skin disease occurring in a black population in south-east London. Br J Dermatol. 1999;141:512–517. https://www.ncbi.nlm.nih.gov/pubmed/10583057[↩]
- Alhady SM, Sivanantharajah K. Keloids in various races: a review of 175 cases. Plast Reconstr Surg. 1969;44:564–566. https://www.ncbi.nlm.nih.gov/pubmed/5352921[↩]
- Bayat A, Arscott G, Ollier WER, Ferguson MWJ, McGrouther DA. “Aggressive keloid”: a severe variant of familial keloid scarring. Journal of the Royal Society of Medicine. 2003;96(11):554-555. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC539632/[↩][↩]
- Bella H, Heise M, Yagi KI, et al. A clinical characterization of familial keloid disease in unique African tribes reveals distinct keloid phenotypes. Plast Reconstr Surg. 2011;127:689–702.[↩][↩]
- Ramakrishnan KM, Thomas KP, Sundararajan CR. Study of 1,000 patients with keloids in South India. Plast Reconstr Surg. 1974;53:276–280.[↩]
- Marneros AG, Norris JE, Watanabe S, et al. Genome scans provide evidence for keloid susceptibility loci on chromosomes 2q23 and 7p11. J Invest Dermatol. 2004;122:1126–1132. https://www.ncbi.nlm.nih.gov/pubmed/15140214[↩]
- Omo-Dare P. Genetic studies on keloid. Journal of the National Medical Association. 1975;67(6):428-432. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2609462/pdf/jnma00484-0018.pdf[↩]
- Shih B, Bayat A. Genetics of keloid scarring. Arch Dermatol Res. 2010;302:319–339. https://www.ncbi.nlm.nih.gov/pubmed/20130896[↩]
- Berman B, Huo R, Viera M. Keloids. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulson I, eds. Treatment of Skin Disease: Comprehensive Therapeutic Strategies. 4th ed. Philadelphia, PA: Elsevier; 2014:chap 116.[↩]
- Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp.991-992, 2475. New York: McGraw-Hill, 2003.[↩]
- Bolognia, Jean L., ed. Dermatology, pp.1531-1535. New York: Mosby, 2003.[↩]