Contents
What is oral thrush
Oral thrush (oral candidiasis), also known as oral moniliasis, “thrush” or oropharyngeal candidiasis, is a yeast infection of the mouth or throat (the oral cavity) 1. There are over 20 species of Candida yeasts that can cause infection in humans, that most commonly causes oral candidiasis is Candida albicans.
Candida (yeast) is a normal organism in your mouth, but sometimes it can overgrow and cause symptoms 2. Candida is a fungus that lives almost everywhere, including in your body 3. Usually, your immune system keeps yeast under control. If you are sick or taking antibiotics, it can multiply and cause an infection.
Oral thrush causes creamy white lesions, usually on your tongue or inner cheeks. Sometimes oral thrush may spread to the roof of your mouth, your gums or tonsils, or the back of your throat.
Although oral thrush can affect anyone, it’s more likely to occur in babies and older adults because they have reduced immunity; in other people with suppressed immune systems or certain health conditions; or people who take certain medications. Oral thrush is a minor problem if you’re healthy, but if you have a weakened immune system, symptoms may be more severe and difficult to control.
Candidiasis in the esophagus (the tube that connects the throat to the stomach) is called esophageal candidiasis or Candida esophagitis. Esophageal candidiasis is one of the most common infections in people living with HIV/AIDS 4.
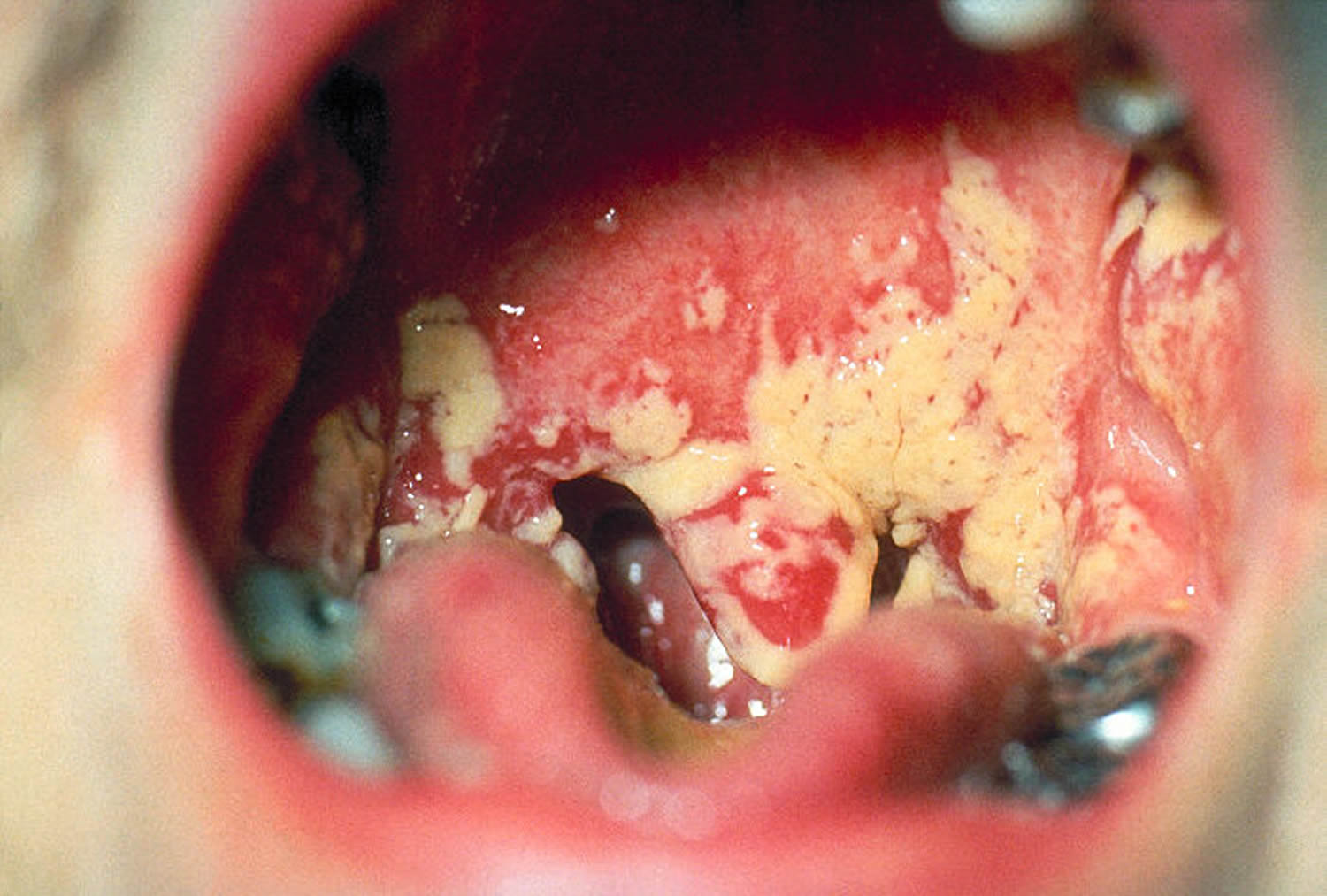
Figure 1. Oral thrush

Figure 2. Oral thrush
Symptoms of oral thrush
Candidiasis in the mouth and throat can have many different symptoms, including:
- White patches on the inner cheeks, tongue, roof of the mouth, and throat (photo showing candidiasis in the mouth)
- Redness or soreness
- Cottony feeling in the mouth
- Loss of taste
- Pain while eating or swallowing
- Cracking and redness at the corners of the mouth
Symptoms of candidiasis in the esophagus usually include pain when swallowing and difficulty swallowing. Contact your healthcare provider if you have symptoms that you think are related to candidiasis in the mouth, throat, or esophagus.
Children and adults oral thrush
Initially, you may not even notice symptoms of oral thrush. Signs and symptoms may include 5:
- Creamy white lesions on your tongue, inner cheeks, and sometimes on the roof of your mouth, gums and tonsils
- Slightly raised lesions with a cottage cheese-like appearance
- Redness, burning or soreness that may be severe enough to cause difficulty eating or swallowing
- Slight bleeding if the lesions are rubbed or scraped
- Cracking and redness at the corners of your mouth
- A cottony feeling in your mouth
- Loss of taste
- Redness, irritation and pain under dentures (denture stomatitis)
- Thrush may be associated with a burning sensation in the mouth or throat.
In severe cases, usually related to cancer or a weakened immune system from HIV/AIDS, the lesions may spread downward into your esophagus — the long, muscular tube stretching from the back of your mouth to your stomach (Candida esophagitis). If this occurs, you may experience difficulty swallowing and pain or feel as if food is getting stuck in your throat.
Infants and breast-feeding mothers oral thrush
In addition to the distinctive white mouth lesions, infants may have trouble feeding or be fussy and irritable. They can pass the infection to their mothers during breast-feeding. The infection may then pass back and forth between the mother’s breasts and the baby’s mouth.
Women whose breasts are infected with candida may experience these signs and symptoms:
- Unusually red, sensitive, cracked or itchy nipples
- Shiny or flaky skin on the darker, circular area around the nipple (areola)
- Unusual pain during nursing or painful nipples between feedings
- Stabbing pains deep within the breast
When to see a doctor
If you or your child develops white lesions inside the mouth, see your doctor or dentist.
Thrush is uncommon in healthy older children, teenagers and adults, so if thrush develops, see your doctor to determine if further evaluation is needed to check for an underlying medical condition or other cause.
What causes oral thrush
Normally, your immune system works to repel harmful invading organisms, such as viruses, bacteria and fungi, while maintaining a balance between “good” and “bad” microbes that normally inhabit your body. But sometimes these protective mechanisms fail, increasing the number of candida fungus and allowing an oral thrush infection to take hold.
The most common type of candida fungus is Candida albicans. Several factors, such as a weakened immune system, can increase your risk of oral thrush.
Risk factors for oral thrush
You may have an increased risk of oral thrush infection if any of these issues apply:
- Weakened immunity. Oral thrush is more likely to occur in infants and older adults due to reduced immunity. Some medical conditions and treatments can suppress your immune system, such as cancer and its treatments, organ transplantation and required drugs that suppress the immune system, and HIV/AIDS.
- Diabetes. If you have untreated diabetes or the disease isn’t well-controlled, your saliva may contain large amounts of sugar, which encourages the growth of candida.
- Vaginal yeast infections. Vaginal yeast infections are caused by the same fungus that causes oral thrush. You can pass the infection to your baby.
- Medications. Drugs such as prednisone, inhaled corticosteroids, or antibiotics that disturb the natural balance of microorganisms in your body can increase your risk of oral thrush.
- Other oral conditions. Wearing dentures, especially upper dentures, or having conditions that cause dry mouth can increase the risk of oral thrush.
Who’s at risk of oral thrush ?
Thrush is very common in infants. Adults who develop thrush include:
- People with diabetes or other glandular (endocrine) disorders
- Denture wearers
- People taking antibiotics
- Persons undergoing chemotherapy
- Drug users
- People with poor nutrition
- Persons who have an immune deficiency, such as HIV
- People who use inhaled steroids for certain lung conditions
- Pregnant women or women on birth control pills
Complications of oral thrush
Oral thrush is seldom a problem for healthy children and adults.
For people with lowered immunity, such as from cancer treatment or HIV/AIDS, thrush can be more serious. Untreated oral thrush can lead to more-serious systemic candida infections. If you have a weakened immune system, thrush may spread to your esophagus or other parts of your body.
Prevention of oral thrush
These measures may help reduce your risk of developing candida infections:
- Rinse your mouth. If you need to use a corticosteroid inhaler, be sure to rinse your mouth with water or brush your teeth after taking your medication.
- Brush your teeth at least twice a day and floss daily or as often as your dentist recommends.
- Check your dentures. Remove your dentures at night. Make sure dentures fit properly and don’t cause irritation. Clean your dentures daily. Ask your dentist for the best way to clean your type of dentures.
- See your dentist regularly, especially if you have diabetes or wear dentures. Ask your dentist how often you need to be seen.
- Watch what you eat. Try limiting the amount of sugar-containing foods you eat. These may encourage the growth of candida.
- Maintain good blood sugar control if you have diabetes. Well-controlled blood sugar can reduce the amount of sugar in your saliva, discouraging the growth of candida.
- Treat a vaginal yeast infection as soon as possible.
- Treat dry mouth. Ask your doctor about ways to avoid or treat your dry mouth.
How is oral thrush diagnosed ?
Diagnosis of thrush depends on the location and identifying whether there is an underlying cause.
If thrush is limited to your mouth
To diagnose oral thrush, your doctor or dentist may:
- Examine your mouth to look at the lesions
- Take a small scraping of the lesions to examine under a microscope
- If needed, do a physical exam and certain blood tests to identify any possible underlying medical condition that may be the cause of oral thrush
If thrush is in your esophagus
To help diagnose thrush in your esophagus, your doctor may recommend any or all of these:
- Biopsy. The tissue sample is cultured on a special medium to help determine which bacteria or fungi, if any, are causing your symptoms.
- Endoscopic exam. In this procedure, your doctor examines your esophagus, stomach and upper part of your small intestine (duodenum) using a lighted, flexible tube with a camera on the tip (endoscope).
- Physical exam. If needed, a physical exam and certain blood tests may be done to try to identify any possible underlying medical condition that could cause thrush in the esophagus.
Treatment of oral thrush
The goal of any oral thrush treatment is to stop the rapid spread of the fungus, but the best approach may depend on your age, your overall health and the cause of the infection. Eliminating underlying causes, when possible, can prevent recurrence.
Oral thrush treatments center on killing the overgrown yeast with anti-fungal medications 6:
- Nystatin – This medicine must come into contact with the yeast in order to kill it. Nystatin comes in a suspension, or liquid, and in a lozenge, also called a troche. The suspension is swished around the mouth and then swallowed. The lozenge dissolves in the mouth. Both the suspension and the lozenges are used several times a day until the lesions are completely gone.
- Amphotericin B suspension – The suspension is swished and swallowed several times a day until complete resolution of the lesions.
- Clotrimazole lozenge – The lozenge is dissolved in the mouth several times a day until the lesions have disappeared entirely.
- Fluconazole pill – This medication is swallowed once daily for 5–10 days.
Healthy adults and children. Your doctor may recommend antifungal medication. This comes in several forms, including lozenges, tablets, or a liquid that you swish in your mouth and then swallow. If these topical medications are not effective, medication may be given that works throughout your body.
Infants and nursing mothers. If you’re breast-feeding and your infant has oral thrush, you and your baby could pass the infection back and forth. Your doctor may prescribe a mild antifungal medication for your baby and an antifungal cream for your breasts.
Adults with weakened immune systems. Most often your doctor will recommend antifungal medication.
Thrush may return even after it’s been treated if the underlying cause, such as poorly disinfected dentures or inhaled steroid use, isn’t addressed.
Home remedies for oral thrush
These suggestions may help during an outbreak of oral thrush:
- Practice good oral hygiene. Brush and floss regularly. Replace your toothbrush often until your infection clears up. Don’t share toothbrushes.
- Disinfect dentures. Ask your dentist for the best way to disinfect your dentures to avoid reinfection.
- Try warm saltwater rinses. Dissolve about 1/2 teaspoon (2.5 milliliters) of salt in 1 cup (237 milliliters) of warm water. Swish the rinse and then spit it out, but don’t swallow.
- Use nursing pads. If you’re breast-feeding and develop a fungal infection, use pads to help prevent the fungus from spreading to your clothes. Look for pads that don’t have a plastic barrier, which can encourage the growth of candida. Wear a clean bra every day. Ask your doctor about the best way to clean your breast nipples, bottle nipples, pacifiers and any detachable parts of a breast pump if you use one.
- Thrush (Oral Candidiasis). http://www.skinsight.com/skin-conditions/adult/oral-candidiasis-thrush[↩]
- Oral thrush. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/oral-thrush/symptoms-causes/syc-20353533[↩]
- Nucci M, Anaissie E. Revisiting the source of candidemia: skin or gut? Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 2001;33:1959-67.[↩]
- Buchacz K, Lau B, Jing Y, et al. Incidence of AIDS-Defining Opportunistic Infections in a Multicohort Analysis of HIV-infected Persons in the United States and Canada, 2000-2010. The Journal of infectious diseases 2016;214:862-72.[↩]
- Bolognia, Jean L., ed. Dermatology, pp.837, 1095, 1096, 1185. New York: Mosby, 2003.[↩]
- Freedberg, Irwin M., ed. Fitzpatrick’s Dermatology in General Medicine. 6th ed, pp. 2013. New York: McGraw-Hill, 2003.[↩]




