What is hyperhidrosis
This is a medical condition that causes excessive sweating. The word “hyperhidrosis” means too much (hyper) sweating (hidrosis). You may sweat so much that sweat soaks through your clothes or drips off your hands. Besides disrupting normal daily activities, hyperhidrosis can cause social anxiety and embarrassment. Social isolation may result from wet palms as patients are embarrassed. The simple act of holding hands on a date can be traumatic. Hyperhidrosis onset for the majority is before age 30, with many in early childhood.
Hyperhidrosis does not occur when patient is asleep or under general anesthesia.
It quite normal and necessary to sweat. Sweating cools the body, which prevents you from overheating. People who have hyperhidrosis, however, sweat when the body does not need cooling. People with hyperhidrosis may sweat even when the temperature is cool or when they are at rest.
Many people who have hyperhidrosis sweat from one or two areas of the body. Most often, they sweat from their palms, feet, underarms, or head at least one episode a week, during waking hours. And the sweating usually occurs on both sides of the body. While the rest of the body remains dry, one or two areas may drip with sweat. Sweating of the palms and soles can begin at birth. Sweating of the axilla begins at puberty. Palmar/plantar sweating is controlled solely by the cerebral cortex. It does not occur when patient is asleep or under general anesthesia. Axillary sweating is related to emotional issues or thermoregulation. Humans can sweat three to four liters per hour to maintain thermal homeostasis.
This excessive sweating can interfere with everyday activities. Hands can be so sweaty that it becomes difficult to turn a doorknob or use a computer. Sweat from the underarms often soaks through clothes, causing obvious sweat marks. Because the skin is often wet, skin infections can develop.
Hyperhidrosis treatment usually involves prescription-strength antiperspirants on the affected areas. Rarely, an underlying cause may be found and treated. For persistent hyperhidrosis, you may need to try different medications or other therapies. In severe cases, your doctor may suggest surgery either to remove the sweat glands or to disconnect the nerves responsible for the overproduction of sweat.
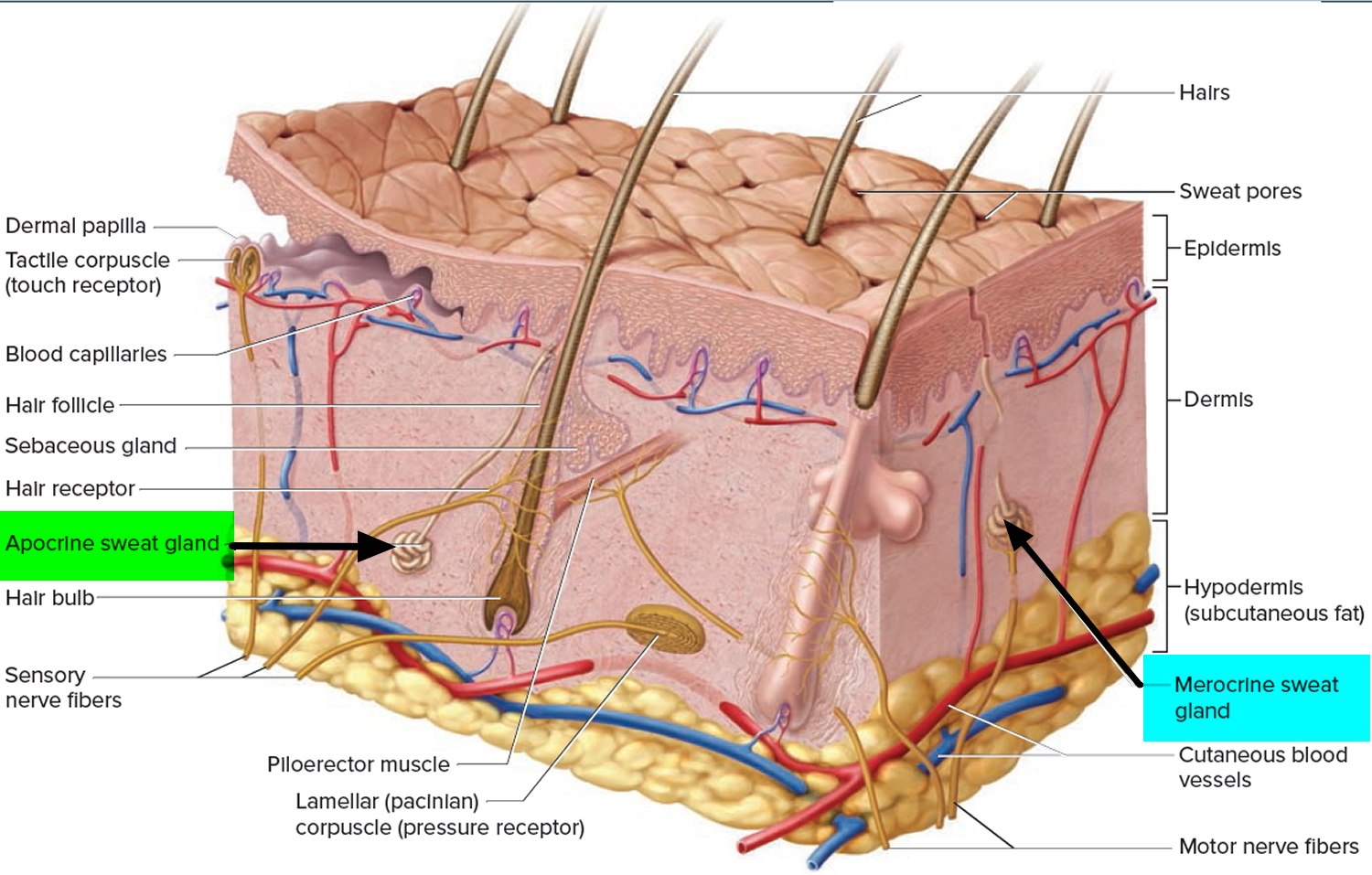
Sweat Glands
Sweating can be broadly divided into:
- Apocrine, apocrine glands accumulate their secretory product at the apical surface of the secreting cell. Then, that portion of the cell pinches off by exocytosis from the rest of the cell to release the secretion. The cell repairs itself and repeats the process.
- Eccrine with eccrine glands (also called merocrine glands) being distributed widely over the entire skin surface, except on the nipples and parts of the external genitalia and numbering over 2.5 million 1. Secretions of eccrine (merocrine) glands are synthesized on ribosomes attached to rough ER; processed, sorted, and packaged by the Golgi complex; and released from the cell in secretory vesicles via exocytosis.
Eccrine gland function is primarily thermoregulatory and activity may alter in response to thermal, osmotic, mental and gustatory factors 2. The hypothalamic sweat centre, which controls the palms and soles, is separate from the rest of the hypothalamic sweat centers. It is activated mainly by emotional and mental stimuli, and less so by thermoregulatory stimuli 3. Eccrine bromhidrosis may be associated with hyperhidrosis as the maceration of keratin by the sweat can lead to increased odor, especially of the soles. Pitted keratolysis of the feet is a bacterial infection of the stratum corneum due to infection with Micrococcus sedentarius. It occurs in the setting of hyperhidrosis and presents with numerous small pits over the web spaces and plantar surfaces of the feet. Fungal infections and intertrigo (inflammation of the skin folds) can also contribute to smell.
Figure 1. Sweat glands
Two types of hyperhidrosis
Both types cause excessive sweating, but there are some differences 4.
Primary hyperhidrosis
In medical terminology, the word “primary” means that the cause is not another medical condition. This type of hyperhidrosis usually begins when the person is a child or adolescent. Most people who have this type are otherwise healthy.
Primary Focal Hyperhidrosis
Focal, visible, excessive sweating of at least 6 months duration without apparent cause with at least 2 of the following characteristics:
- “Focal” means that the excessive sweating (hyperhidrosis) affects one or a few parts of the body. The areas of the body most commonly affected are the underarms, hands and/or feet, and forehead.
- On both sides of the body: If the excessive sweating occurs in the underarms, the person usually notices both underarms sweat excessively. The same holds true for the hands and feet.
- After waking up: Sweating may begin soon after the person wakes up, but the person usually does not notice damp sheets or wet clothing unless the room is hot.
- At least once a week: For many people, it occurs much more often.
- Bilateral and relatively symmetric.
- Impairs daily activities.
- Frequency of at least one episode per week.
- Age of onset less than 25 years.
- Positive family history.
- Cessation of focal sweating during sleep.
Secondary hyperhidrosis
In medical terminology, “secondary” means that the excessive sweating (hyperhidrosis) has an underlying cause. The cause could be a 4:
- Medical condition
- Side effect of taking a medicine or food supplement
Drugs
- Alcohol (chronic and acute intoxication)
- Aspirin
- Insulin
- Antidepressants (eg. fluoxetine)
- Amphetamines
Medical conditions that can cause excessive sweating include:
- Diabetes
- Frostbite
- Gout
- Injury, such as head trauma caused by an accident
- Menopause
- Obesity
- Overactive thyroid (hyperthyroidism)
- Tumor
Cardiorespiratory:
- Acute heart attack
- Heart failure
- Respiratory failure
Endocrine:
- Hyperthyroidism
- Diabetic autonomic neuropathy
- Hypoglycaemia
- Gout
- Phaeochromocytoma
- Hyperpituitarism
- Carcinoid syndrome
- Menopause
- Obesity
Infection:
- Tuberculosis
- Malaria
- Infectious endocarditis
- Brucellosis
- HIV
Cancer:
- Lymphoma
- Leukaemia
- Solid malignancies
Neurological:
- Post spinal injury
- Stroke
- Parkinson’s disease
- Peripheral neuropathies
If a person has this type of hyperhidrosis, the person may notice:
- The entire body sweats excessively: Sometimes, only parts of the body sweat.
- Sweating occurs during sleeping: If you sweat excessively while asleep, it is important to see a dermatologist to learn why this happens.
This type of sweating usually begins when the person is an adult. It also may begin after an accident or frostbite. Many medicines also can cause this type of hyperhidrosis.
Anxiety and embarrassment
Both types of hyperhidrosis can cause people to feel extremely anxious and embarrassed. Students often avoid raising their hand during class. Many teens never date. Adults may hide the sweat stains by wearing layers of clothing or changing frequently throughout the day.
When to see a doctor
Sometimes excessive sweating is a sign of a serious condition. Seek immediate medical attention if your heavy sweating is accompanied by one or more of the following:
- Chills
- Lightheadedness
- Chest pain
- Nausea
- A body temperature of 104 °F (40 °C) or higher
See your doctor if:
- Sweating disrupts your daily routine
- You suddenly begin to sweat more than usual
- You experience night sweats for no apparent reason
What causes hyperhidrosis – excessive sweating
Certain nerves tell the body when to sweat. It is possible that these nerves overreact, causing excessive sweating.
Scientists know that you cannot catch it from someone.
In hyperhidrosis, sweat glands are of normal size, density, location, and histologic appearance.
Dermatologists continue to study what causes this condition. They also continue improve treatments. If excessive sweating interferes with your life, you may want to see a dermatologist. Many effective treatments are available.
Who gets hyperhidrosis ?
It is difficult to say how many people have excessive sweating – some report hyperhidrosis affects 3% of the general population. Many people never see a doctor. Some are too embarrassed to talk with a doctor. Others do not realize that this is a treatable medical condition. Dermatologists estimate that 3% of people in the United States have excessive sweating.
Scientists know that some people are more likely to get hyperhidrosis. Researchers have learned that most people have one of the following:
- Family member who sweats excessively. Positive family history in 30%-65% of patients.
- Medical condition that causes the sweating.
- Medicine or food supplement that they take, which can cause excessive sweating.
When the excessive sweating occurs in one or two areas of the body, it is likely that a family member also has this condition.
Many medical conditions can cause excessive sweating. These include diabetes and gout. A tumor or injury also can cause excessive sweating.
Women often sweat excessively when they get hot flashes during menopause. The cause is obvious. Some women, however, develop excessive sweating after they have gone through menopause. This sweating does not have an obvious cause.
People of all races get hyperhidrosis. The excessive sweating can begin at any age. For many people, it begins when they are a child or teen. Dermatologists believe that more children and adolescents have this condition than are diagnosed.
Whether you live in a cold climate or a warm one, you can have hyperhidrosis.
What is excessive sweating at night
Night sweats are repeated episodes of extreme perspiration that may soak your nightclothes or bedding and are related to an underlying medical condition or illness.
You may occasionally awaken after having perspired excessively, particularly if you are sleeping under too many blankets or if your bedroom is too warm. Although uncomfortable, these episodes are usually not labeled as night sweats and typically aren’t a sign of a medical problem.
In general, night sweats are also associated with fever, weight loss, localized pain, cough, diarrhea, or other symptoms of concern.
What causes excessive sweating at night
Medications that can cause night sweats
Night sweats are a common side effect of many medications, such as:
- Depression medications (antidepressants)
- Hormone-blocking drugs used to treat certain cancers (hormone therapy)
- Drugs used to treat diabetes (if the level of sugar in your blood gets too low) (hypoglycemic agents)
Medical conditions that can cause night sweats
Diseases and conditions that can cause night sweats include:
- Anxiety
- Autoimmune disorders
- Autonomic neuropathy (damage to your autonomic nerves)
- Brucellosis (a bacterial infection)
- Carcinoid syndrome (a certain type of cancerous tumor in your intestines)
- Drug addiction (alcohol, opioids, cocaine, cannabis, benzodiazepines)
- Infective endocarditis (an infection of your heart valves)
- HIV/AIDS
- Hodgkin’s lymphoma (Hodgkin’s disease) (Hodgkin’s disease)
- Hyperthyroidism (overactive thyroid)
- Leukemia
- Myelofibrosis (a bone marrow disorder)
- Non-Hodgkin’s lymphoma
- Osteomyelitis (a bone infection)
- Pheochromocytoma (a rare adrenal gland tumor)
- Pyogenic abscess (a pus-filled cavity caused by an infection)
- Sleep disorders (such as obstructive sleep apnea)
- Stroke
- Syringomyelia (a fluid-filled cyst in the spinal cord)
- Thyroid disease
- Tuberculosis
Night sweats and hot flashes are very common among women around the time of menopause. If you are around age 50 and are having irregular or absent menstrual periods, and have no other symptoms, this is likely the cause of your symptoms.
When to see a doctor
Schedule a doctor’s visit if night sweats:
- Occur on a regular basis
- Interrupt your sleep
- Are accompanied by a fever, weight loss, localized pain, cough, diarrhea, or other symptoms of concern.
- Come on after your menopause symptoms have been absent for months to years.
Signs and symptoms of hyperhidrosis
If you have this medical condition, you may notice:
Visible sweating: When you are not exerting yourself, do you often see beads of sweat on your skin or have sweat-soaked clothing? Do you sweat when you’re sitting?
Sweating interferes with everyday activities: Does sweating cause difficulty holding a pen, walking, or turning a doorknob? Does sweat drip heavily on to your papers or computer?
Skin turns soft, white, and peels in certain areas: Does your skin stay wet for long periods?
Skin infections: Do you get frequent skin infections on the parts of your body that sweat heavily? Athlete’s foot and jock itch are common skin infections.
Hyperhidrosis treatment
Before treatment begins, it is important to find out why you have excessive sweating.
To diagnose this condition, a skin doctor gives the patient a physical exam. This includes looking closely at the areas of the body that sweat excessively. A skin doctor also asks very specific questions. This helps the doctor understand why the patient has excessive sweating.
Sometimes medical testing is necessary. Some patients require a test called the sweat test. This involves coating some of their skin with a powder that turns purple when the skin gets wet.
If abnormalities of the skin are present, bacterial swabs and scrapes for fungi may be taken to identify pathogens. If any features suggestive of secondary hyperhidrosis are present, or if the presentation is not typical (eg. unilateral or asymmetric symptoms) then targeted investigations should be performed. These may include thyroid function testing for hyperthyroidism, full blood count, and relevant imaging if cancer, infectious or neurological cause is suspected. Referral for further opinion may also be warranted.
Initial management of hyperhidrosis
The first line treatment for primary palmoplantar hyperhidrosis should be with antiperspirants.
- Topical aluminium chloride hexahydrate 20% (aluminum chloride 20% in alcohol [Drysol in the US] – available over-the-counter at chemists) should be trialed at night until normal sweating is achieved. Apply to dry skin. May blow dry first. Or apply at night. Use for at least 10 days to see effect. The frequency can then be decreased to 1-3 times per week. This approach is usually quite effective in the armpit, but often fails on the palms and soles. The effect is thought to be due to an occlusive action of aluminium containing particles in the upper epidermis and change in ionic transport within secretory cells 5. However, this is generally effective in only the mildest cases. Irritation, which can occur when the preparation is applied to other sites, is much less of a problem when used on the thicker acral (palms and soles) skin.
- Oral anticholinergics, such as propantheline bromide 15 mg every 4-6 hours or glycopyrrolate 1 mg one daily to three times per day, may be tried, but these usually require doses that cause intolerable side effects, including dry eyes, dry mouth and throat, and urinary retention, before they have any real benefit on the sweating 6, 7. 30% get dry mouth or dry eyes. It is very easy to carry around a water bottle. Patients must be counseled that this approach can stop sweating all over and caution must be taken not to get overheated (risk of heat stroke) if outside on warm days. Typically one starts glycopyrrolate 1 mg oral daily x 7 days, then if control is not achieved, twice daily x 7 days, and three times daily if needed. The patient should stop escalating the dose once control is achieved. Oral anticholinergic agents are effective for hyperhidrosis, especially in teenage boys. Patients are often very compliant because when it works, it works. 90% of patients experience improvement (within 1-3 days) at 2 mg/day. Hyperhidrosis recurs quickly if stopped. For children, glycopyrrolate is FDA-approved for 3-16 year olds for severe chronic drooling caused by neurologic disorders. Treatment is off-label for hyperhidrosis. It comes as Cuvposa, a cherry-flavored solution at 1 mg/5 cc. Make sure to discuss with parents the potential side effects, including dry eyes and mouth. In one study of 31 children with hyperhidrosis (mean age 15 years), the average age of onset was 10.3 years and at a mean dosage of 2 mg daily, 90% of patients experienced improvement 8. Topical glyocpyrrolate 2% in clinical studies has been effective 9.
- Oxybutynin (comes as 5 mg/5 cc) has been found to be a good treatment option for children 10. In that study, children weighing more than 40 kg received 2.5 mg of oxybutynin once daily in the evening for 7 days, then 2.5 mg twice daily from day 7–21 and then 5 mg twice daily. Patients weighing < 40 kg received the same treatment for the first 3 weeks, but their dose was not increased after day 21. The most common side effect was dry mouth. In one study of adults with generalized hyperhidrosis 11, the oxybutynin was started at 2.5 mg per day and increased gradually until it reached an effective dose, without exceeding 7.5 mg per day. Sixty percent of patients experienced some improvement, compared with 27% of patients receiving placebo.
- Oxybutynin:
- Oral therapy that is relatively effective.
- It may be used for both focal and generalized hyperhidrosis.
- Use caution if patient lives in a hot environment. Decreased sweating poses risk of heat stroke.
- Dry mouth is a common side effect.
- Ongoing therapy
- The presence of a fungal infection requires treatment. Topical creams may be tried initially (terbinafine, the azole group) but if extensive, a short course of an oral preparation may be required. The identification of the pathogen is useful in helping to decide between terbinafine and the cheaper preparation, griseofulvin. The presence of pitted keratolysis similarly requires treatment.
- An antibacterial wash in the shower, such as benzoyl peroxide 5% 12, is an important first step; but make sure this is washed away well as it has bleaching properties. Otherwise, topical antibiotics such as clindamycin 1% or erythromycin 2%, or a combination product containing benzoyl peroxide 5% and clindamycin 1%, could be used. The azole antifungals may also give good results 12. If unsuccessful, a course of oral antibiotics such as erythromycin for 7–10 days may be required.
It is also important to pay attention to your footwear. Occlusive and rubber shoes often exacerbate the problem by increasing sweating. You should change your (cotton) socks frequently and alternate the shoes you wear each day to allow the shoes to dry out, use Zeasorb powder, and remove shoes when at home. Fungi can survive for 30 days off the body, so shoes and socks can be a reservoir for re-infection. Avoid boots if possible.
Home remedies to treat hyperhidrosis
The following suggestions may help you cope with sweating and body odor:
- Use antiperspirant. Nonprescription antiperspirants contain aluminum-based compounds that temporarily block the sweat pore. This reduces the amount of sweat that reaches your skin. This type of product may help with minor hyperhidrosis.
- Bathe daily. Regular bathing helps keep the number of bacteria on your skin in check. Dry yourself thoroughly, especially between the toes and under the arms.
- Choose shoes and socks made of natural materials. Shoes made of natural materials, such as leather, can help prevent sweaty feet by allowing your feet to breathe. When you’re active, moisture-wicking athletic socks are a good choice.
- Rotate your shoes. Shoes won’t completely dry overnight, so try not to wear the same pair two days in a row.
- Change your socks often. Change socks or hose once or twice a day, drying your feet thoroughly each time. You may want to try pantyhose with cotton soles.
- Use over-the-counter foot powders to help absorb sweat.
- Air your feet. Go barefoot when you can, or at least slip out of your shoes now and then.
- Choose clothing to suit your activity. Generally, wear natural fabrics, such as cotton, wool and silk, which allow your skin to breathe. When you exercise, you might prefer fabrics designed to wick moisture away from your skin.
- Try relaxation techniques. Consider relaxation techniques such as yoga, meditation and biofeedback. These can help you learn to control the stress that triggers sweating.
For the feet, application of a creamy “clinical strength” antiperspirant and/or aluminum chloride 20% (Drysol) at night is recommended. Some benefit from wearing two pairs of socks–the one in contact with the skin 100% polyester and the outer sock 100% cotton.
Iontophoresis (the no-sweat machine)
If excessive sweating affects your hands, feet, or both areas, this may be an option. You will use this treatment at home. It requires you to immerse your hands or feet in a shallow pan of tap water. As you do this, this medical device sends a low-voltage current through the water. This can be done with tap water alone 7 or with anticholinergic drugs.
Iontophoresis using an anticholinergic solution, such as glycopyrrolate is superior to tap water 13. Some systemic absorption of the drug occurs, resulting in anticholinergic side effects for a day or so after treatment. This is generally limited to a dry throat, although it may also include blurred vision and dry eyes. The treatment is available only in specialized centers as the use of the drug in this manner is ‘off label’.
Many people obtain relief. Some people dislike that this treatment and it can be time-consuming.
Uses: Hands and feet. Best for palmar hyperhidrosis but may help for plantar hyperhidrosis.
How it works: The electric current shuts down the treated sweat glands temporarily. Iontophoresis uses electric current to introduce ions into your body through acrosyringium.
Iontophoresis (low level electric current) is very effective but requires time and money. Patients usually need to rent or buy the machine. Device instructions vary, but in general, patients immerse the affected hands or feet in a shallow tray filled with tap water for a short period of time (20 to 40 minutes) while the device sends a mild electrical current through the water. Treatment is home-based and performed 2-3 times per week until control is achieved, then tapered as able.
Most people need about 6 to 10 treatments to shut down the sweat glands. To get improvement, you begin by using the device as often your skin doctor recommends. At first, you may need 2 or 3 treatments per week. A treatment session usually takes 20 to 40 minutes.
Once you see results, you can repeat the treatment as needed to maintain results. This can range from once a week to once a month.
If this treatment is right for you, your skin doctor will teach you how to use the device and give you a prescription so that you can buy one. Some patients also receive a prescription for a medicine that they add to the tap water.
Contraindications: Pregnancy and a history of metallic implants such as orthopedic prostheses and cardiac pacemakers are contraindications to this treatment.
Side effects: Some people develop:
- Dry skin
- Irritated skin
- Discomfort during treatment
If you experience any side effects, tell your skin doctor. Making some changes often eliminates these side effects.
Prescription medicine
Some patients receive a prescription for a medicine that temporarily prevents them from sweating. These medicines work throughout the body.
Oral anticholinergics, such as propantheline, may be tried, but these usually require doses that cause intolerable side effects, including dry eyes, dry mouth and throat, and urinary retention, before they have any real benefit on the sweating 6, 7.
How it works: These medicines prevent the sweat glands from working. Athletes, people who work in a hot place, and anyone who lives in a warm climate should use extreme caution when using this treatment. The body may not be able to cool itself.
Uses: These medicines can effectively treat sweating that involves entire body. This medicine also can be an effective treatment for post-menopausal women who sweat excessively only from their head.
Side effects: The medicines that prevent the sweat glands from working can cause:
- Dry mouth
- Dry eyes
- Blurry vision
- Heart palpations (abnormal heartbeat)
The risk of side effects increases with higher doses. Before taking this medicine, you should talk with your skin doctor about your individual risks and benefits.
Botulinum toxin injection for hyperhidrosis
Botulinum toxin for the management of palmoplantar hyperhidrosis is well reported 14, 15, 16. The Botulinum toxin inhibits the release of acetylcholine from presynaptic nerve endings. When successful, this treatment has the advantage of long duration of symptom relief, often for at least 6 months in most patients 16, although a longer period of time has been reported 15. Botulinum toxin injections do not cure hyperhidrosis; your symptoms will go away gradually (usually in about a week) and return gradually. Follow-up injections are required to maintain dryness. Side effects include pain from the multiple injections required (the toxin diffuses approximately 1 cm from the point of injection and some form of analgesia is usually required, eg. methoxyflurane inhalation, nerve block, or in some cases, general anaesthesia), weakness of the intrinsic muscles of the hands 15, 16 and cost. When Botulinum toxin is used for plantar hyperhidrosis (excessive sweating of the feet), patients often report more pain during plantar injections and statistics indicate the treatment is less effective than when used for other body sites; indeed, some data suggests that 50% patients are dissatisfied with the results 17.
Neutralizing antibodies were once thought to limit the long term use of this treatment. However, Gordon et al 18 report this is not a clinical issue for most patients undergoing long term treatment with botulinum toxin type A. Botulinum toxin contains the blood product human albumin and it’s use may be unacceptable to some patients. Botulinum toxin may interact with medications that affect neuromuscular transmission including aminoglycosides and curare like compounds, and this may last 3–6 months after administration 19. A limited number of dermatologists offer this service, often in specialised clinics.
Botulinum Toxin
- Injections are painful but only need to be given every 3-6 months.
- Works for axillary and palmar sweating. Less so for the soles.
- For hands, there is a risk of decreased grip strength.
- For axillae, there is not necessarily a reduction in body odor.
- Use ice to minimize pain.
Subcutaneous injections of botulinum A toxin can give benefits for 3-6 months. The main downside however is the pain of injection. Ice has been enthusiastically recommended to reduce the pain 20. Additionally, up to 1/3 of patients whose hands are treated may experience decreased grip strength. Ulnar and median nerve blocks at the wrist level may be performed to reduce the pain of palmar injection. Patients should understand that the axillary injections may not reduce body odor as the eccrine glands (not apocrine) are targeted. Duration of efficacy seems to increase with repeated injections 21.
Surgery for hyperhidrosis
If other treatments fail to bring relief, surgery may be considered. Surgery is permanent and carries risks. The following surgeries can stop excessive sweating:
- Surgically remove sweat glands
- Sympathectomy
How it works: A dermatologist can surgically remove sweat glands from the underarms. This surgery can be performed in a dermatologist’s office. Only the area to be treated is numbed, so the patient remains awake during the surgery.
A dermatologist may use one or more of the following surgical techniques to remove sweat glands from the underarms:
- Excision (cut out sweat glands)
- Liposuction (remove with suction)
- Curettage (scrape out)
- Laser surgery (vaporize)
Sympathectomy is another surgery used to treat hyperhidrosis. This is major surgery, which a surgeon performs in an operating room.
During sympathectomy, the surgeon tries to stop the nerve signals that your body sends to the sweat glands. To do this, the surgeon will cut or destroy certain nerves. To find these nerves, the surgeon inserts a mini surgical camera into the patient’s chest just beneath the underarm. The patient’s lung must be temporarily collapsed so that the surgeon can cut or destroy nerves.
Uses:
- Surgical removal of sweat glands is used to treat the underarms
- Sympathectomy is mainly used to treat the palms
Side effects: All surgeries carry some risk. When sweat glands are removed from the underarm, there is risk of developing an infection. Patients may have soreness and bruising. These will go away.
- Permanent side effects also can occur. Loss of feeling in the underarm and scarring are possible.
- In some cases, this procedure triggers excessive sweating in other areas of your body.
Advances in endoscopic surgery have reduced some risks from sympathectomy. Serious side effects can still occur. Some patients develop a condition known as compensatory sweating. For some people, this causes them to sweat more heavily than did the hyperhidrosis.
Other possible side effects from sympathectomy include damage to the nerves that run between the brain and eyes, extremely low blood pressure, irregular heartbeat, and inability to tolerate heat. Patients have died during this surgery.
Hand-held medical device destroys sweat glands: This is a newer treatment approved by the FDA. A medical doctor such as a dermatologist must give these treatments.
If this is an option, the dermatologist uses a machine that emits electromagnetic energy. This energy destroys the sweat glands. In one or two office visits, the glands can be destroyed. Once destroyed, the sweat glands are gone forever.
This device can only treat the underarms because this area of the body has enough underlying fat to protect itself. This device cannot be used to treat the hands and feet because these areas do not have enough fat.
This is a newer treatment option. Unlike other treatments, there is not a lot of information about this treatment for hyperhidrosis. Scientists do not know how long the results last. Long-term side effects are not known.
- Roberts H, Dolianitis C, Sinclair R. Overview of hyperhidrosis. Medicine Today 2007;8:47–52.[↩]
- Coulson IH. Disorders of sweat glands. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook’s textbook of dermatology. 7th edn. Vol 3; Chp 45. Blackwell Science Ltd, 2004;1–23.[↩]
- Goldsmith LA. Fitzpatrick’s dermatology in general medicine. 6th edn. New York: McGraw-Hill, 2003;699–704.[↩]
- Walling H. “Clinical differentiation of primary from secondary hyperhidrosis.” J Am Acad Dermatol. 2011;64:690-5.[↩][↩]
- McWilliams SA, Montgomery I, McEwan Jenkinson D, Elder HY, Wilson SM, Sutton AM. Effects of topically-applied antiperspirant on sweat gland function. Br J Dermatol 1987;117:617–26.[↩]
- Hornberger J, Grimes K, Naumann M, et al. Recognition, diagnosis and treatment of primary focal hyperhidrosis. J Am Acad Dermatol 2004;51:274–86.[↩][↩]
- Stolman LP. Treatment of excess sweating of the palms by iontophoresis. Arch Dermatol 1987;123:893–6.[↩][↩][↩]
- JAAD 2012;67:918-23[↩]
- JEADV 2016; 30;2131[↩]
- Pediatric Dermatology 2014;31:48–53[↩]
- BJD 2015;173;1163–1168[↩]
- Lee PK, Zipoli MT, Weinberg AN, Swartz MN, Johnson RA. Fitzpatrick’s dermatology in general medicine. 6th edn. New York: McGraw-Hill, 2003;1875–6.[↩][↩]
- Dolianitis C, Scarff CE, Kelly J, Sinclair R. Iontophoresis with glycopyrrolate for the treatment of palmoplantar hyperhidrosis. Australas J Dermatol 2004;45:208–12.[↩]
- Naumann M, Flachenecker P, Brocker E-B, Toyka KV, Reiners K. Botulinum toxin for palmar hyperhidrosis. Lancet 1997;349:252.[↩]
- Shelley WB, Talanin NY, Shelley ED. Botulinum toxin therapy for palmar hyperhidrosis. J Am Acad Dermatol 1998;38:227–9.[↩][↩][↩]
- Saadia D, Voustianiouk A, Wang AK, Kaufmann H. Botulinum toxin type A in primary palmar hyperhidrosis: Randomized, single-blind, two-dose study. Neurology 2001;57:2095–9.[↩][↩][↩]
- OnabotulinumtoxinA Injections (Botox®). International Hyperhidrosis Society. https://www.sweathelp.org/hyperhidrosis-treatments/botox.html[↩]
- Gordon MF, Barron R. Effectiveness of repeated treatment with botulinum toxin type A across different conditions. South Med J 2006;99:853–61.[↩]
- Scheinberg A. Clinical use of botulinum toxin. Aust Prescr 2009;32:39–42. [↩]
- Dermatol Surg 2007;33;588[↩]
- JAAD 2014;70;1083[↩]