Contents
What is hypoparathyroidism
Hypoparathyroidism is a rare condition where the parathyroid glands, which are in the neck near the thyroid gland, produce too little parathyroid hormone (PTH). Hypoparathyroidism is characterized by low levels of parathyroid hormone (PTH), which decreases the amount of calcium in your blood (hypocalcemia) and blood phosphorus levels to rise (hyperphosphatemia), which can cause a wide range of symptoms, including muscle cramps, pain and twitching. Nerve and muscles cells are unable to function properly. Causes of hypoparathyroidism include magnesium deficiency, injury to the glands, surgery on the nearby thyroid gland, genetic disorder or the congenital lack of parathyroid glands. The most common cause of hypoparathyroidism is removal of or accidental injury to the parathyroid glands during surgery to the neck.
When children have hypoparathyroidism, they might grow poorly, have tooth problems such as delayed tooth development or a lot of cavities, and have slow mental development.
In adults, hypoparathyroidism can lead to kidney problems, heart problems, and calcium deposits in the brain. Calcium in the brain can cause tremors, slowed movement, balance problems, and seizures.
Hypoparathyroidism can be linked to other health problems, such as cataracts, Addison disease (problems with your adrenal glands), and pernicious anemia (a shortage of vitamin B12).
Symptoms of hypoparathyroidism include:
- Pins and needles
- Brittle hair and nails
- Dry, roughened skin
- Muscle cramps and spasms
- Convulsions.
Treatment for hypoparathyroidism involves taking calcium and vitamin D supplements to normalize your calcium and phosphorus levels. Depending on the cause of your hypoparathyroidism, you may need to take the supplements for the rest of your life. Parathyroid hormone (PTH) replacement is also available in injectable form. Injecting parathyroid hormone (PTH) may decrease the need to take too many calcium and vitamin D supplements. Your doctor will check your blood levels regularly.
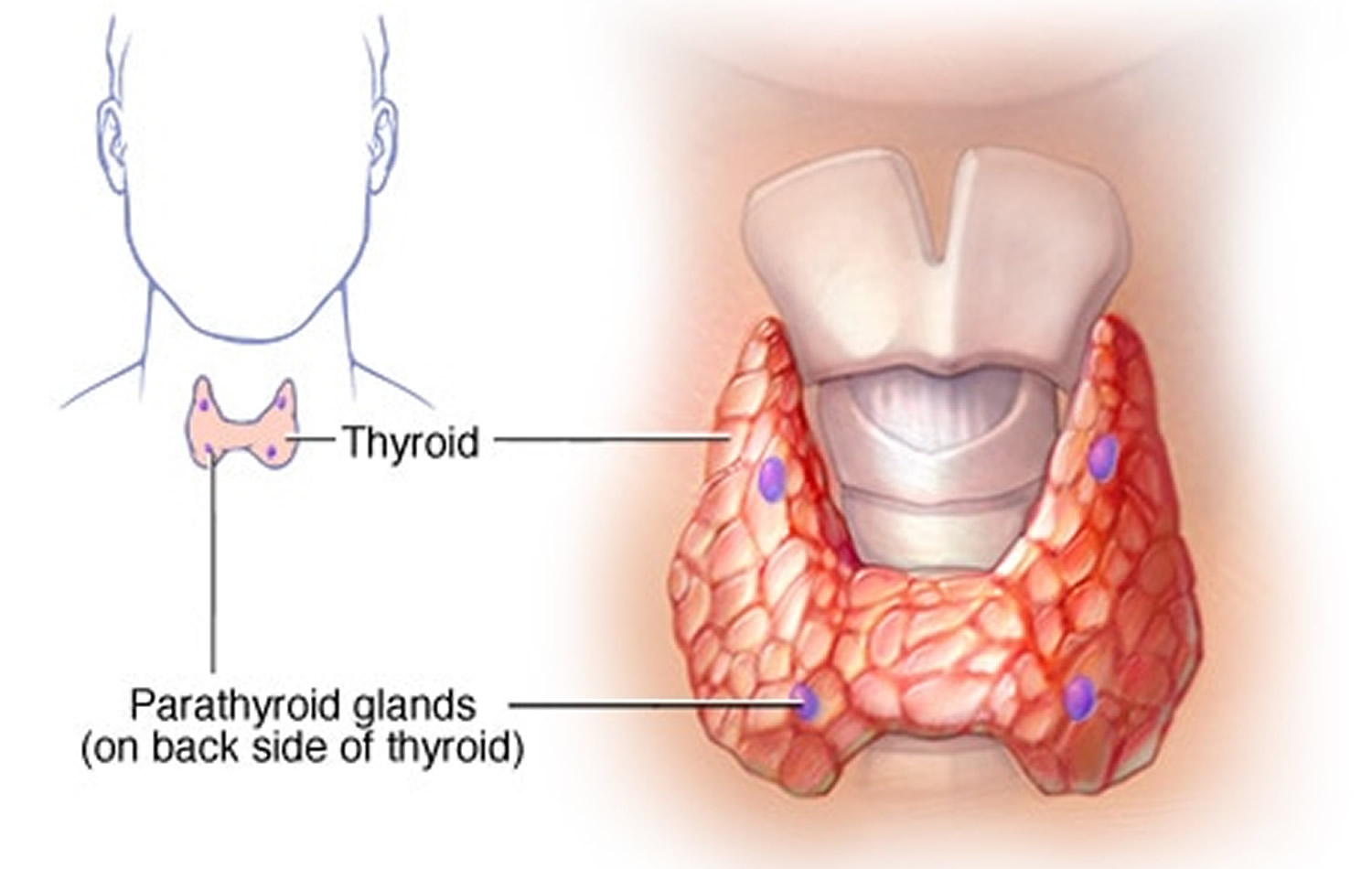
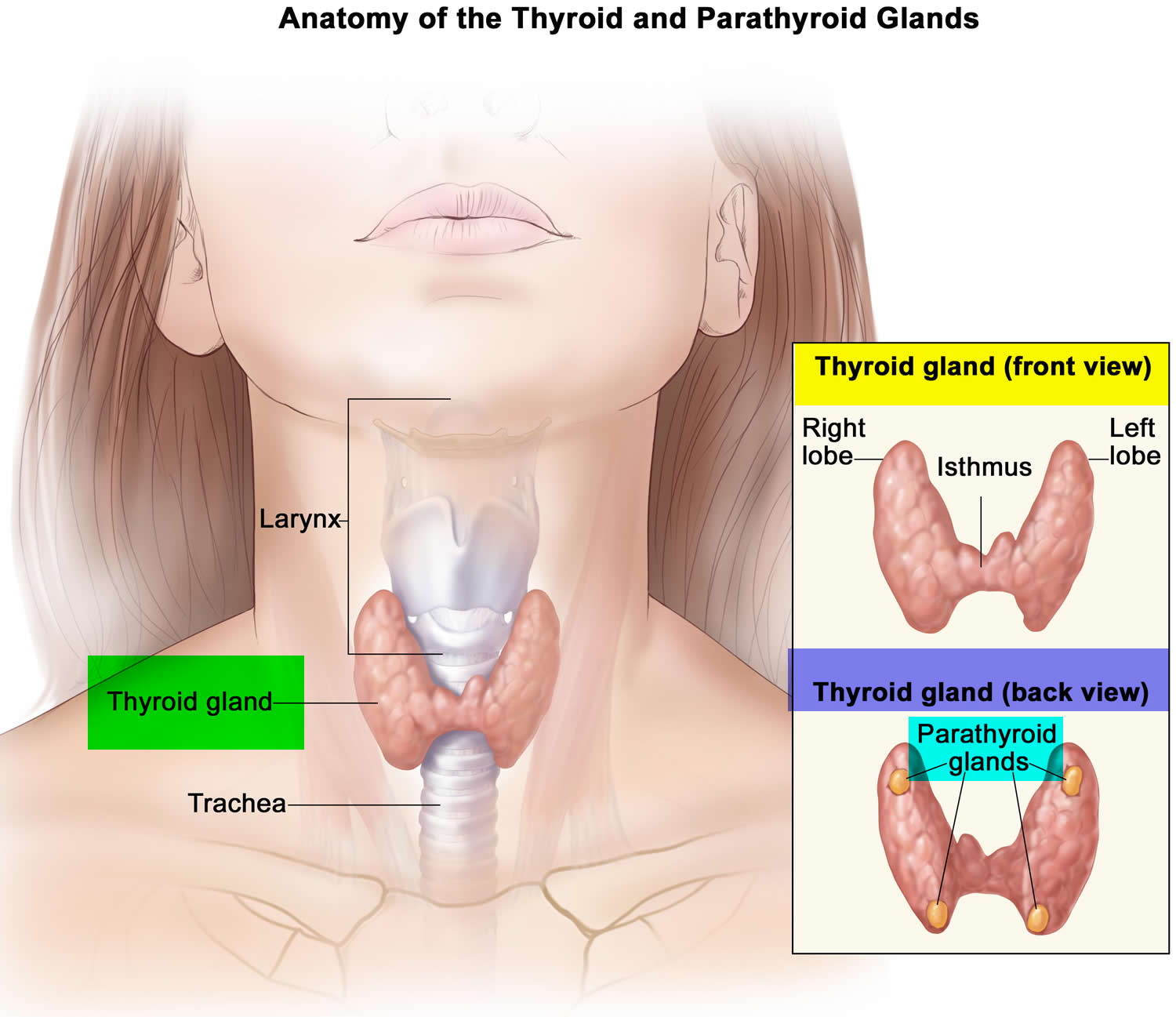
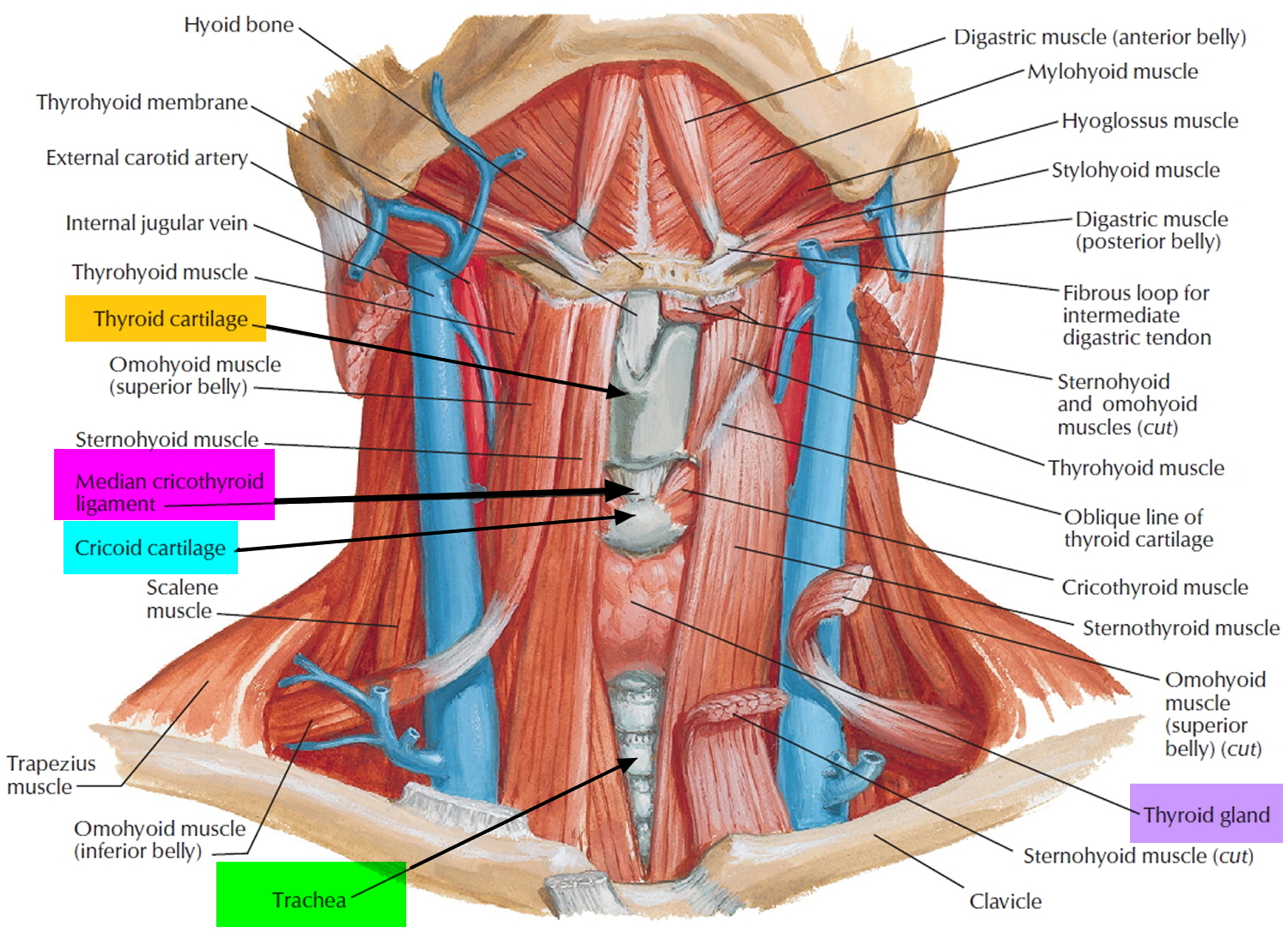
What is parathyroid gland
The parathyroid glands are ovoid glands, usually four in number, partially embedded in the posterior (behind) surface of the thyroid. Each parathyroid gland has a mass of about 40 mg and is about 3 to 8 mm long and 2 to 5 mm wide. Usually, one superior and one inferior parathyroid gland are attached to each lateral thyroid lobe, for a total of four. The parathyroid glands are separated from the thyroid follicles by a thin fibrous capsule and adipose tissue. Often, the parathyroid glands occur in other locations ranging from as high as the hyoid bone to as low as the aortic arch, and about 5% of people have more than four parathyroids.
Microscopically, the parathyroid glands contain two kinds of epithelial cells. The more numerous cells, called chief cells or principal cells, produce parathyroid hormone (PTH), also called parathormone. The function of the other kind of cell, called an oxyphil cell, is not known in a normal parathyroid gland. Oxyphil cells do not appear until after puberty, and then their numbers increase with age. However, its presence clearly helps to identify the parathyroid gland histologically due to its unique staining characteristics. Furthermore, in a cancer of the parathyroid glands, oxyphil cells secrete excess parathyroid hormone (PTH).
Attached to the chief cells of these parathyroid glands is a newly discovered molecule called the Calcium Sensing Receptor (CaSR). This Calcium Sensing Receptor (CaSR) responds to very small changes in the blood level of calcium to turn the parathyroid glands on and off when needed. The Calcium Sensing Receptor (CaSR) is working as the thermostat. If the body is not getting enough calcium from the diet, for example, the Calcium Sensing Receptor (CaSR) senses a need to get calcium from somewhere. The immediate response is for the parathyroid glands to make and secrete more of their active hormone – parathyroid hormone (PTH). This sets off a chain of events that get more calcium into the bloodstream. First, parathyroid hormone (PTH) goes to the calcium bank – namely your bones, where 98% of the body’s store of calcium is warehoused. This is good for the blood calcium and for the cells that need calcium, but not good for the bones themselves. The second line of defense against a need for more calcium is the kidneys. Here parathyroid hormone (PTH) does two things. First, it limits the kidneys from excreting too much calcium, thereby keeping the blood levels up. Next, it works on the kidneys to produce another hormone called calcitriol or “active vitamin D.”
Figure 1. Parathyroid gland location (hidden behind the thyroid gland)
Figure 2. Thyroid gland location
Parathyroid gland function
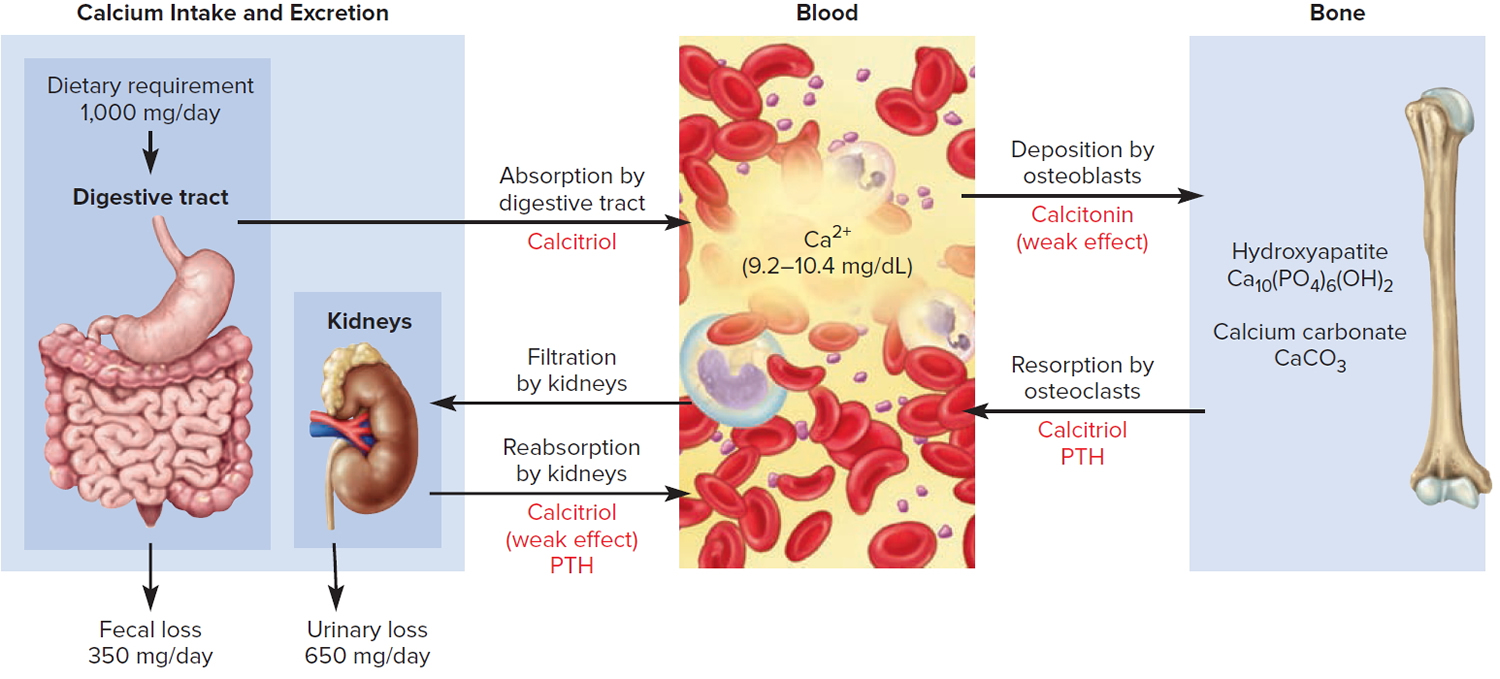
Parathyroid hormone (PTH) is secreted by the parathyroid glands, which regulates blood calcium levels (Ca 2+).
Furthermore, the parathyroid hormone (PTH) is also the major regulator of the levels of magnesium (Mg 2+), and phosphate (HPO4 2−) ions in the blood. The specific action of parathyroid hormone (PTH) is to increase the number and activity of osteoclasts. The result is elevated bone resorption, which releases ionic calcium (Ca 2+) and phosphates (HPO4 2−) into the blood.
Parathyroid hormone (PTH) also acts on the kidneys. First, it slows the rate at which Ca 2+ and magnesium (Mg 2+) are lost from blood into the urine. Second, it increases loss of phosphate (HPO4 2−) from blood into the urine. Because more phosphate (HPO4 2−) is lost in the urine than is gained from the bones, PTH decreases blood phosphate (HPO4 2−) level and increases blood Ca2+ and magnesium (Mg 2+) levels.
A third effect of PTH on the kidneys is to promote formation of the hormone calcitriol, the active form of vitamin D. Calcitriol, also known as 1,25-dihydroxyvitamin D3, increases the rate of calcium (Ca 2+), phosphate (HPO4 2−) and magnesium (Mg 2+) absorption from the gastrointestinal tract into the blood.
Figure 3. Hormonal control of calcium balance
Note: The central panel represents the blood reservoir of calcium and shows its normal (safe) range. Calcitriol and Parathyroid Hormone (PTH) regulate calcium exchanges between the blood and the small intestine and kidneys (left). Calcitonin, calcitriol, and Parathyroid Hormone (PTH) regulate calcium exchanges between blood and bone (right).
Control of Secretion of Calcitonin and Parathyroid Hormone
The blood calcium (Ca 2+) level directly controls the secretion of both calcitonin and parathyroid hormone (PTH) via negative feedback loops that do not involve the pituitary gland.
These parathyroid glands release PTH when blood calcium is low. A mere 1% drop in the blood calcium level doubles the secretion of PTH.
A lower-than-normal level of calcium ions (Ca 2+) in the blood stimulates chief cells of the parathyroid gland to release more parathyroid hormone (PTH).
PTH raises the blood calcium level by four mechanisms:
- PTH binds to receptors on the osteoblasts, stimulating them to secrete RANKL, which in turn raises the osteoclast population and promotes bone resorption of bone extracellular matrix, which releases Ca 2+ into the blood and slows loss of Ca 2+ in the urine, raising the blood level of Ca 2+.
- PTH promotes Ca 2+ reabsorption by the kidneys, so less calcium is lost in the urine.
- PTH promotes the final step of calcitriol synthesis in the kidneys, thus enhancing the calcium-raising effect of calcitriol. Calcitriol stimulates increased absorption of Ca 2+ from foods in the gastrointestinal tract, which helps increase the blood level of Ca 2+.
- TH inhibits collagen synthesis by osteoblasts, thus inhibiting bone deposition.
Once the levels of calcium have been brought back to normal, the system slows down and waits for the next call. Interestingly, and perhaps surprising to most, this chain of events happens without you knowing about or feeling anything wrong. Even the changes in blood calcium that set the whole system in motion are too small to be measured most of the time. The need to keep the blood calcium constant is so great that, when everything is working properly, even the minutest change triggers a response from the parathyroid glands. Yes, vitamin D is actually a hormone, not a vitamin. The vitamin D you get from your multi-vitamins, your diet or that is made by the action of sunlight on your skin is not very active at all. First, it has to go to the liver where it is turned into calcediol, which is more active than vitamin D but still not good enough. This calcediol is then carried in the blood to the kidneys where it is converted to calcitriol. This change from calcediol to calcitriol is controlled by PTH.
Figure 4. Correction of hypocalcemia (low blood calcium)
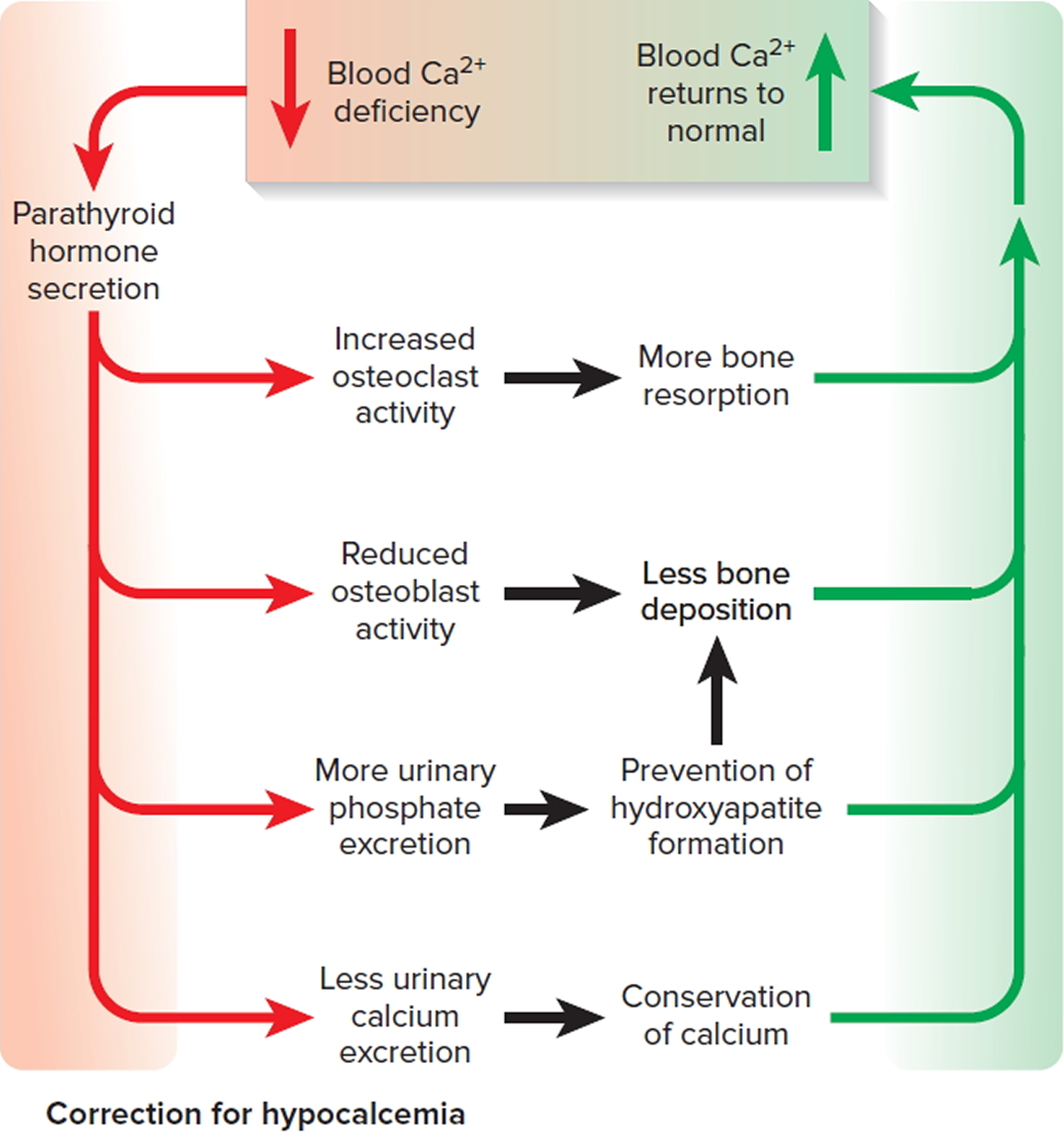
Note: The correction of hypocalcemia by parathyroid hormone (PTH).
- A higher-than-normal level of calcium ions (Ca 2+) in the blood stimulates parafollicular cells of the thyroid gland to release more calcitonin.
- Calcitonin inhibits the activity of osteoclasts, thereby decreasing the blood calcium ions (Ca 2+) level.
Hypoparathyroidism causes
Hypoparathyroidism occurs when your parathyroid glands don’t secrete enough parathyroid hormone. You have four small parathyroid glands situated in your neck, behind your thyroid gland.
Factors that can cause hypoparathyroidism include:
- Post-surgical hypoparathyroidism. This most common cause of hypoparathyroidism develops after accidental damage to or removal of the parathyroid glands during surgery. This surgery might be a treatment for diseases of the thyroid gland, or for throat or neck cancer.
- Autoimmune disease. Your immune system creates antibodies against the parathyroid tissues, trying to reject them as if they were foreign bodies. In the process, the parathyroid glands stop manufacturing their hormone.
- Hereditary hypoparathyroidism. In this form, either you’re born without parathyroid glands or with glands that don’t work properly – for example, people with the inherited genetic disorder DiGeorge syndrome are born without parathyroid glands. Some types of hereditary hypoparathyroidism are associated with deficiencies of other hormone-producing glands.
- Extensive cancer radiation treatment of your face or neck. Radiation can result in destruction of your parathyroid glands, as can radioactive iodine treatment for hyperthyroidism, occasionally.
- Low levels of magnesium in your blood – for example, because of alcohol misuse, which can affect the function of your parathyroid glands. Normal magnesium levels are required for optimum secretion of parathyroid hormone.
Risk factors for hypoparathyroidism
Factors that can increase your risk of developing hypoparathyroidism include:
- Recent neck surgery, particularly if the thyroid was involved
- A family history of hypoparathyroidism
- Having certain autoimmune or endocrine conditions, such as Addison’s disease — which causes your adrenal glands to produce too little of its hormones
Hypoparathyroidism prevention
There are no specific actions to prevent hypoparathyroidism. However, if you’re scheduled to have thyroid or neck surgery, talk to your surgeon about the risk of damage to your parathyroid glands during the procedure.
If you’ve had surgery involving your thyroid or neck, watch for signs and symptoms that could indicate hypoparathyroidism, such as a tingling or burning sensation in your fingers, toes or lips, or muscle twitching or cramping. If they occur, your doctor might recommend prompt treatment with calcium and vitamin D to minimize the effects of the disorder.
Hypoparathyroidism signs and symptoms
Signs and symptoms of hypoparathyroidism can include:
- Tingling or burning (paresthesia) in your fingertips, toes and lips
- Muscle aches or cramps in your legs, feet, abdomen or face
- Twitching or spasms of your muscles, particularly around your mouth, but also in your hands, arms and throat
- Fatigue or weakness
- Painful menstruation
- Patchy hair loss
- Dry, coarse skin
- Brittle nails
- Mood changes, such as feeling irritable, anxious or depressed
- Memory problems
Hypoparathyroidism can also cause teeth to fail to form or slow to emerge, impaired mental development, Addison’s disease and dysmenorrhea (painful menstrual periods).
Hypoparathyroidism complications
Hypoparathyroidism can result in various complications.
Reversible complications
The following are due to low calcium levels, most of which are likely to improve with treatment:
- Tetany. These cramplike spasms of your hands and fingers can be prolonged and painful. Tetany might also include muscle discomfort and twitches or spasms of the muscles of your face, throat or arms. When these spasms occur in your throat, they can interfere with breathing, creating a possible emergency.
- Paresthesias. These are characterized by odd, tingling sensations or pins and needles feelings in your lips, tongue, fingers and toes.
- Loss of consciousness with convulsions (grand mal seizures).
- Malformed teeth, affecting dental enamel and roots.
- Impaired kidney function.
- Heart arrhythmias and fainting, even heart failure.
Irreversible complications
Accurate diagnosis and treatment might prevent these complications associated with hypoparathyroidism. But once they occur, calcium and vitamin D won’t improve them:
- Stunted growth (short stature)
- Slow mental development in children
- Calcium deposits in the brain, which can cause balance problems and seizures
- Cataracts
Hypoparathyroidism diagnosis
A doctor who suspects hypoparathyroidism will take a medical history and conduct a physical exam.
Blood tests
These findings on blood tests might indicate hypoparathyroidism:
- A low blood-calcium level
- A low parathyroid hormone level
- A high blood-phosphorus level
- A low blood-magnesium level
Your doctor might also order a urine test to determine whether your body is excreting too much calcium.
Hypoparathyroidism treatment
The goal of treatment is to relieve symptoms and to normalize levels of calcium and phosphorus in your body. A treatment regimen typically includes:
- Oral calcium carbonate tablets. Oral calcium supplements can increase calcium levels in your blood. However, at high doses, calcium supplements can cause gastrointestinal side effects, such as constipation, in some people.
- Vitamin D. High doses of vitamin D, generally in the form of calcitriol, can help your body absorb calcium and eliminate phosphorus.
- Parathyroid hormone (Natpara). The Food and Drug Administration has approved this once-daily injection for treatment of low blood calcium due to hyperparathyroidism. Because of the potential risk of bone cancer (osteosarcoma), at least in animal studies, this drug is available only through a restricted program to people whose calcium levels can’t be controlled with calcium and vitamin D supplements and who understand the risks.
If your blood calcium level becomes extremely low, it can be dangerous for your health. Then you will be given calcium through a vein (IV) and your heart will be checked to make sure it’s OK. Once your calcium level is normal, you can go back to taking oral supplements.
You might need to follow a diet high in calcium and low in phosphorus. A registered dietitian can help you plan a special diet.
- Good Sources of Calcium: Milk, yogurt, cheese, collard greens, and foods with added calcium, such as cereal and soy drinks.
- Good Sources of Vitamin D: Salmon, shrimp, and milk with vitamin D. Vitamin D is also made in your skin when you spend time in the sun.
- AVOID foods high in Phosphorus: Limit protein foods such as meat, milk, and hard cheeses; also whole grains, dried peas and beans, nuts, and chocolate.
The normal calcium range is around 2.2 to 2.6 millimoles per liter (mmol/L). You’ll be advised to keep your calcium levels in a slightly lower range – for example, 1.8 to 2.25mmol/L. Your recommended range will depend on your circumstances.
Calcium carbonate and vitamin D supplements – usually calcitriol (Rocaltrol) or alfacalcidol (One-Alpha) – can be taken to restore your blood calcium to these levels. They usually have to be taken for life.
You’ll also need to have regular blood tests to monitor your parathyroid hormone, calcium and phosphorus levels.
If your blood calcium levels fall to a dangerously low level or you keep having muscle spasms, you may need to be given calcium through a drip directly into your vein.
Intravenous infusion
If you need immediate symptom relief, your doctor might recommend hospitalization so that you can receive calcium by intravenous (IV) infusion, as well as oral calcium tablets. After hospital discharge, you’ll continue to take calcium and vitamin D orally.
Monitoring
Your doctor will regularly check your blood to monitor levels of calcium and phosphorus. Initially, these tests will probably be weekly to monthly. Eventually, you’ll need blood tests just twice a year.
Because hypoparathyroidism is usually a long-lasting (chronic) disorder, treatment generally is lifelong, as are regular blood tests to determine whether calcium in particular is at normal levels. Your doctor will adjust your dose of supplemental calcium if your blood-calcium levels rise or fall.
Hypoparathyroidism diet
Your doctor might recommend that you consult a dietitian, who is likely to advise a diet that’s:
- Rich in calcium. This includes dairy products, green leafy vegetables, broccoli and foods with added calcium, such as some orange juice and breakfast cereals.
- Low in phosphorus. This means avoiding carbonated soft drinks, which contain phosphorus in the form of phosphoric acid, and limiting red meat, dairy, fish, poultry, bread, rice, oats, hard cheeses and whole grains.
What foods provide calcium ?
Calcium is found in many foods. You can get recommended amounts of calcium by eating a variety of foods, including the following:
- Milk, yogurt, and cheese are the main food sources of calcium for the majority of people in the United States.
- Kale, broccoli, and Chinese cabbage are fine vegetable sources of calcium.
- Fish with soft bones that you eat, such as canned sardines and salmon, are fine animal sources of calcium.
- Most grains (such as breads, pastas, and unfortified cereals), while not rich in calcium, add significant amounts of calcium to the diet because people eat them often or in large amounts.
- Calcium is added to some breakfast cereals, fruit juices, soy and rice beverages, and tofu. To find out whether these foods have calcium, check the product labels.
The U.S. Department of Agriculture’s (USDA’s) Nutrient Database website 1 lists the nutrient content of many foods with Calcium arranged by nutrient content 2 and by food name 3.
Calcium Rich Foods
Milk, yogurt, and cheese are rich natural sources of calcium and are the major food contributors of this nutrient to people in the United States 4. Nondairy sources include vegetables, such as Chinese cabbage, kale, and broccoli. Spinach provides calcium, but its bioavailability is poor. Most grains do not have high amounts of calcium unless they are fortified; however, they contribute calcium to the diet because they contain small amounts of calcium and people consume them frequently. Foods fortified with calcium include many fruit juices and drinks, tofu, and cereals. Selected food sources of calcium are listed in Table 1.
Table 1: Selected Food Sources of Calcium
| Food | Milligrams (mg) per serving | Percent DV* |
|---|---|---|
| Yogurt, plain, low fat, 8 ounces | 415 | 42 |
| Mozzarella, part skim, 1.5 ounces | 333 | 33 |
| Sardines, canned in oil, with bones, 3 ounces | 325 | 33 |
| Yogurt, fruit, low fat, 8 ounces | 313–384 | 31–38 |
| Cheddar cheese, 1.5 ounces | 307 | 31 |
| Milk, nonfat, 8 ounces** | 299 | 30 |
| Soymilk, calcium-fortified, 8 ounces | 299 | 30 |
| Milk, reduced-fat (2% milk fat), 8 ounces | 293 | 29 |
| Milk, buttermilk, lowfat, 8 ounces | 284 | 28 |
| Milk, whole (3.25% milk fat), 8 ounces | 276 | 28 |
| Orange juice, calcium-fortified, 6 ounces | 261 | 26 |
| Tofu, firm, made with calcium sulfate, ½ cup*** | 253 | 25 |
| Salmon, pink, canned, solids with bone, 3 ounces | 181 | 18 |
| Cottage cheese, 1% milk fat, 1 cup | 138 | 14 |
| Tofu, soft, made with calcium sulfate, ½ cup*** | 138 | 14 |
| Ready-to-eat cereal, calcium-fortified, 1 cup | 100–1,000 | 10–100 |
| Frozen yogurt, vanilla, soft serve, ½ cup | 103 | 10 |
| Turnip greens, fresh, boiled, ½ cup | 99 | 10 |
| Kale, fresh, cooked, 1 cup | 94 | 9 |
| Ice cream, vanilla, ½ cup | 84 | 8 |
| Chinese cabbage, bok choi, raw, shredded, 1 cup | 74 | 7 |
| Bread, white, 1 slice | 73 | 7 |
| Pudding, chocolate, ready to eat, refrigerated, 4 ounces | 55 | 6 |
| Tortilla, corn, ready-to-bake/fry, one 6” diameter | 46 | 5 |
| Tortilla, flour, ready-to-bake/fry, one 6” diameter | 32 | 3 |
| Sour cream, reduced fat, cultured, 2 tablespoons | 31 | 3 |
| Bread, whole-wheat, 1 slice | 30 | 3 |
| Kale, raw, chopped, 1 cup | 24 | 2 |
| Broccoli, raw, ½ cup | 21 | 2 |
| Cheese, cream, regular, 1 tablespoon | 14 | 1 |
* DV = Daily Value. DVs were developed by the U.S. Food and Drug Administration to help consumers compare the nutrient contents among products within the context of a total daily diet. The DV for calcium is 1,000 mg for adults and children aged 4 years and older. Foods providing 20% of more of the DV are considered to be high sources of a nutrient, but foods providing lower percentages of the DV also contribute to a healthful diet.
[Source 1]In its food guidance system, MyPlate, the U.S. Department of Agriculture recommends that persons aged 9 years and older eat 3 cups of foods from the milk group per day 5. A cup is equal to 1 cup (8 ounces) of milk, 1 cup of yogurt, 1.5 ounces of natural cheese (such as Cheddar), or 2 ounces of processed cheese (such as American).
- The USDA Food Composition Databases. https://ndb.nal.usda.gov/ndb/[↩][↩]
- The USDA Food Composition Databases. Calcium Content. https://ods.od.nih.gov/pubs/usdandb/Calcium-Content.pdf[↩]
- The USDA Food Composition Databases. Foods Calcium Content. https://ods.od.nih.gov/pubs/usdandb/Calcium-Food.pdf[↩]
- Committee to Review Dietary Reference Intakes for Vitamin D and Calcium, Food and Nutrition Board, Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press, 2010.[↩]
- U.S. Department of Agriculture, Center for Nutrition Policy and Promotion. ChooseMyPlate.gov 2011. https://www.choosemyplate.gov/[↩]