Contents
What is hypospadias
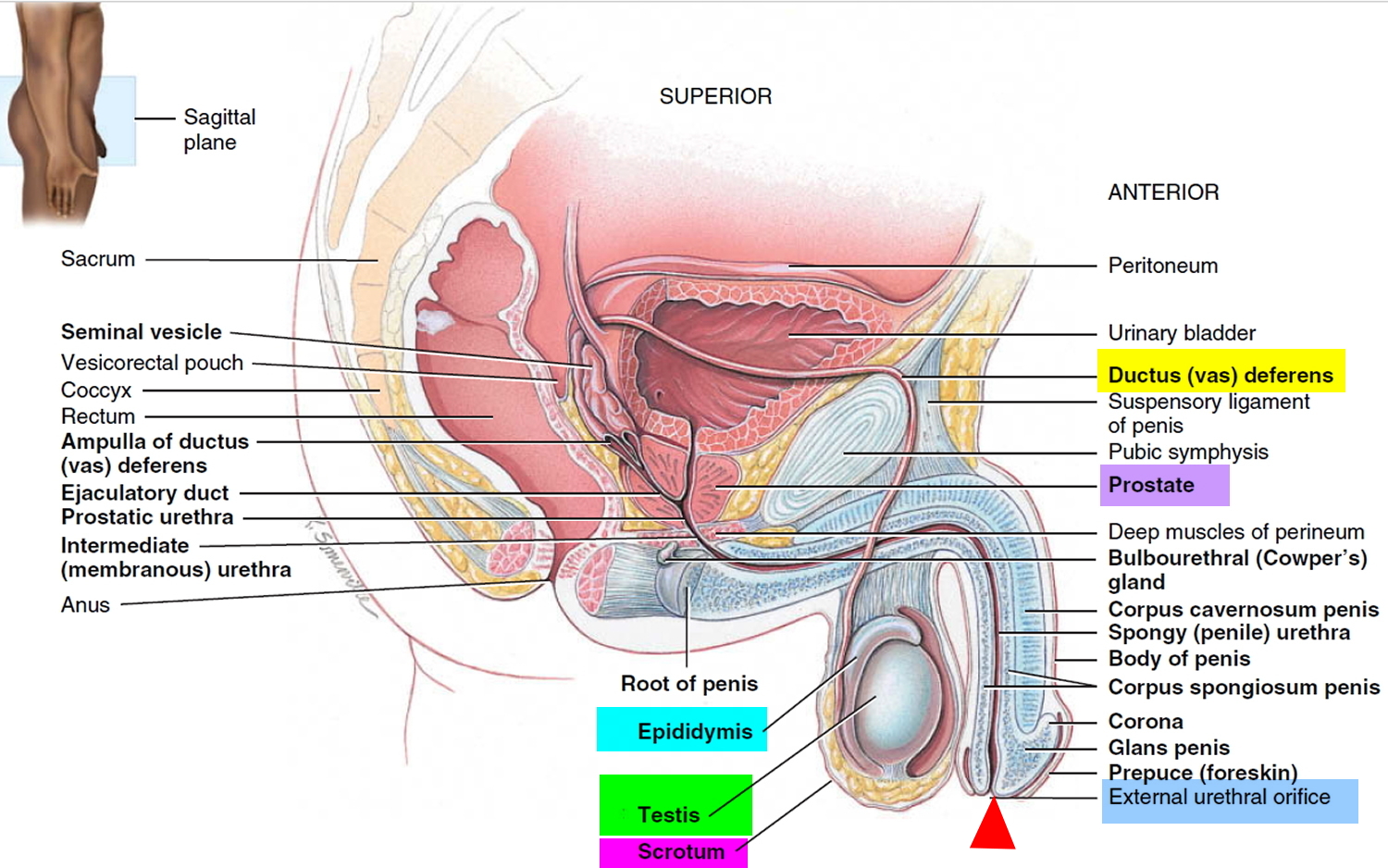
Hypospadias is a birth defect (congenital condition) in which a baby boy’s urethra is located on the under side of his penis rather than at the tip 1; you may have concerns about what this means for everything from toilet training to his future life as an adult. In boys with hypospadias, the urethra forms abnormally during weeks 8–14 of pregnancy. The abnormal opening can form anywhere from just below the end of the penis to the scrotum.
Hypospadias is common and doesn’t cause difficulty in caring for your infant. The urethra is the tube through which urine drains from your bladder and exits your body.
Hypospadias is fairly common birth defect affecting about 1 in 200 to 1 in 300 male newborns 2. Hypospadias is often readily corrected through outpatient surgery. Hypospadias also occurs in girls, but it’s extremely rare (affecting an estimated one in 500,000 babies) and a vastly different condition. If your daughter is born with hypospadias, your child’s specialist will be your best source of information and support.
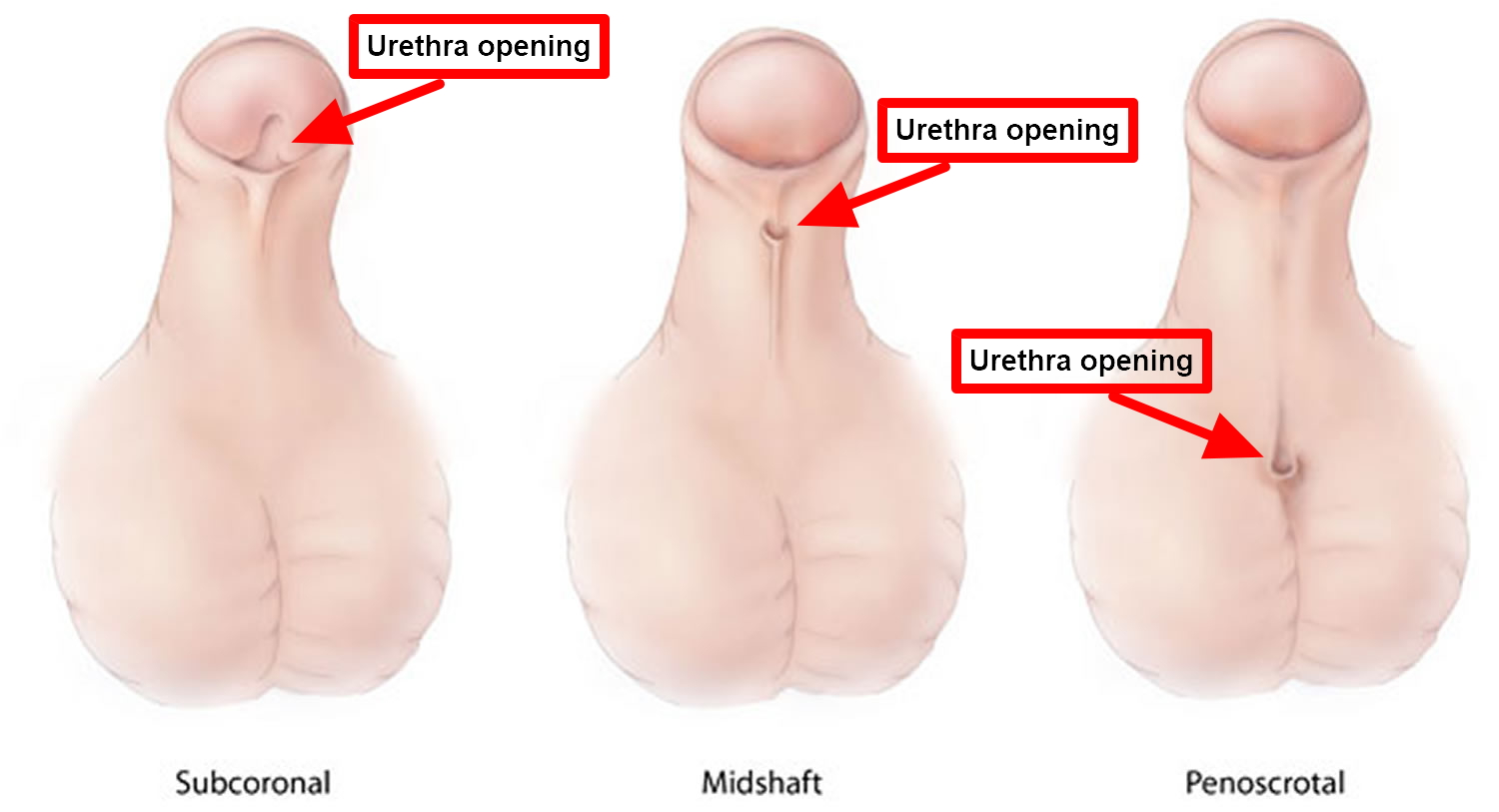
In hypospadias, the urethral opening can be located at any point along the underside of the penis (also called the “ventral aspect”) (see Figure 1). Where the opening falls will determine how severe the condition is, and how your child’s medical team will approach repairing it.
There are different degrees of hypospadias; some can be minor and some more severe.
- Subcoronal hypospadias – anterior or distal (near the tip of the penis): The opening of the urethra is located somewhere near the head of the penis. This is the mildest form of hypospadias, occurring in about 50 percent of cases.
- Midshaft hypospadias – middle (midway up the penis): The opening of the urethra is located along the shaft of the penis. Considered moderate hypospadias, this accounts for about 30 percent of cases.
- Penoscrotal hypospadias – posterior or proximal (at the scrotum or perineum): The opening of the urethra is located where the penis and scrotum meet. This is the most severe kind of hypospadias, and occurs in 20 percent of cases.
Some parents may confuse hypospadias with epispadias, in which the urethra opens along the top of the penis, but these are two separate and distinct conditions with very different treatments.
Boys with hypospadias can sometimes have a curved penis. They could have problems with abnormal spraying of urine and might have to sit to urinate. In some boys with hypospadias, the testicle has not fully descended into the scrotum (cryptorchidism).
While some children with very mild forms of this condition may not require surgery, if your son has hypospadias you should seek an evaluation from a pediatric urologic surgeon.
Surgery usually restores the normal appearance of your child’s penis. The outlook for infants who undergo this operation is extremely good: In most instances, they make a full recovery and have a normal-looking, fully functional penis within about six months. With successful treatment of hypospadias, most males can have normal urination and reproduction.
If left untreated, more severe forms of hypospadias can interfere with sexual intercourse when your child is an adult.
Figure 1. Hypospadias types
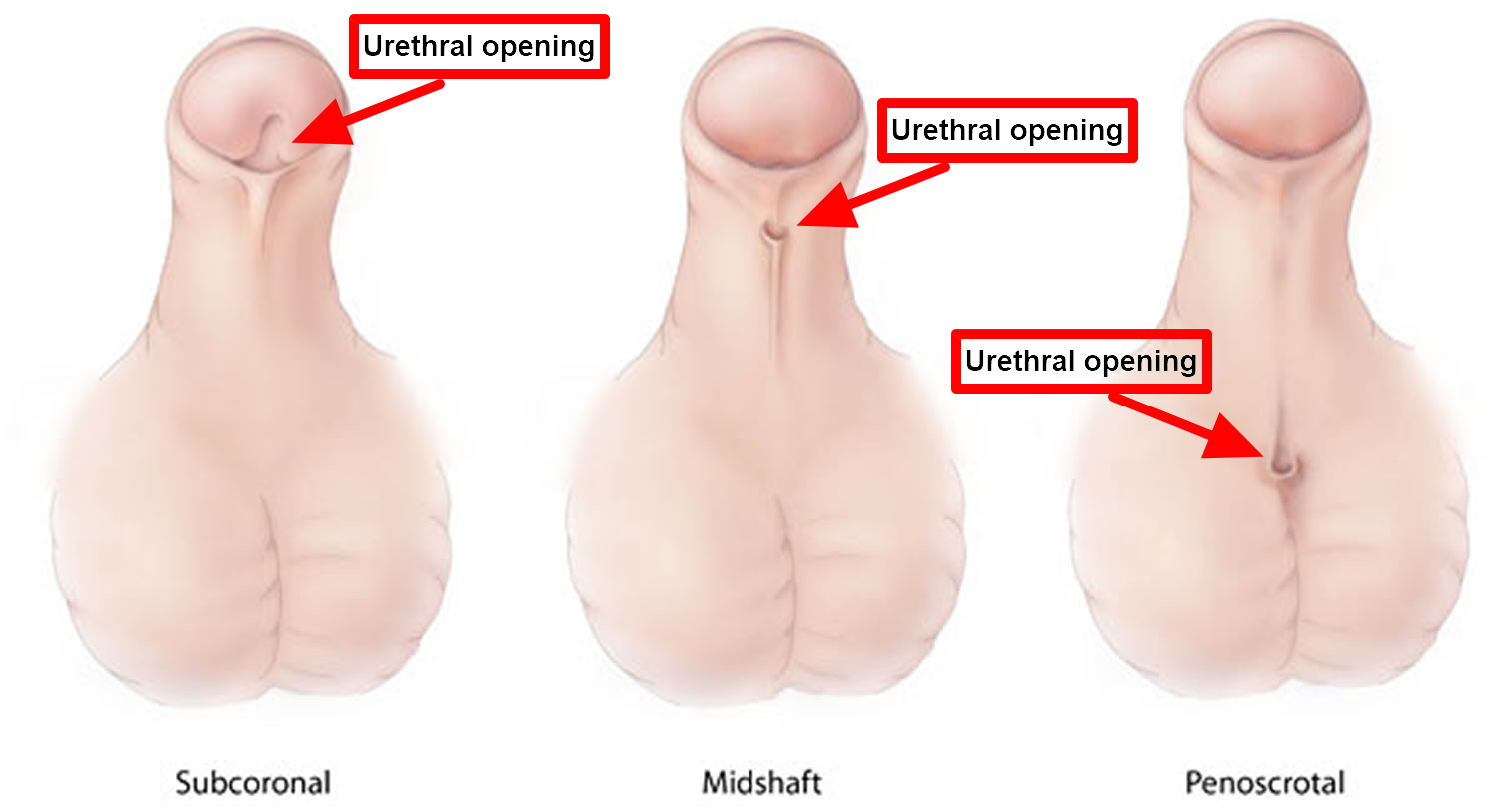
Figure 2. Normal penis with normal urethral opening
 Epispadias
Epispadias
Epispadias is a congenital condition in which the urethra most often opens on the top or side of the penis instead of the tip. Moreover, the urethra may also be open along the whole length of the penis. This birth defect is most commonly observed as a part of the exstrophy epispadias complex, which is a spectrum of failures of midline fusion affecting the pelvis, abdominal wall and urinary bladder. Characteristics of epispadias include a very short and wide penis often classified as complete epispadias when the entire urethra is exposed from the abdominal wall to the tip of the penis. There is usually an upward bending of the penis (chordee) associated with epispadias.
Epispadias can also occur in females, where it is manifested as a split clitoris and displacement of the urethral opening.
Epispadias is always part of the exstrophy epispadias complex, but can also occur as an isolated birth defect in a child with an otherwise normal bladder, pelvis and abdominal wall. In isolated epispadias, the bladder is closed and covered by the lower abdominal wall muscles and skin. In some children with epispadias, there may be bony- pelvis abnormalities similar to, but not as severe as, that seen with bladder exstrophy.
Isolated male epispadias in the absence of bladder-exstrophy-epispadias complex is a rare malformation, with an estimated incidence of around 1 per 117,000 live male births and only one of every 484,000 female births 3. Like hypospadias, epispadias covers a wide spectrum in which the urethral opening can be located anywhere from the distal penile shaft to the pubic area. Unlike in hypospadias, the severity of the condition is related not only to the urethral opening but also to the degree of incontinence associated with the urethral opening position, as the bladder neck might be involved in more proximal variants of isolated male epispadias 4.
Bladder exstrophy is a rare, complex birth defect involving the urinary, reproductive and intestinal tracts, as well as the musculoskeletal system. During a baby’s development in the womb, the abdominal wall and underlying organs sometimes do not fuse properly, and the infant is born with the bladder inside out and exposed on the outside of the body.
Bladder exstrophy usually involves several systems within the body, including the urinary tract, reproductive tract (external genitalia) and pelvic skeletal muscles and bones. In rare cases, intestinal tracts are involved.
Bladder exstrophy can result in weakened abdominal muscles and a shorter than average urethra and vagina or penis. It can cause a variety of complications and problems, including incontinence, catheterization, reflux, infertility and the need for repeated reconstructive surgery. It may be associated with urinary incontinence and back up of urine from the bladder to the kidneys, called vesicoureteral reflux.
What causes exstrophy of the bladder and epispadias?
The cause of bladder exstrophy is unknown. Some studies show a clustering of the condition in families, suggesting that there’s an inherited factor. Popular theories suggest overdevelopment of a normal structure known as the cloacal membrane. Overdevelopment or prolonged presence of the cloacal membrane may prevent appropriate tissue development, ingrowth and the joining together of the supportive lower abdominal wall structure. However, the chance for parents to have another child with exstrophy of the bladder is less than one percent.
Risk factors for exstrophy-epispadias complex include Caucasian race, young maternal age, and maternal multiparity 5. Furthermore, exstrophy-epispadias complex is increased among children conceived with assisted-reproductive technologies such as in vitro fertilization 6.
Patients who have more than a mild case of epispadias will need surgery.
Leakage of urine (incontinence) can often be repaired at the same time. Seventy-five percent of male epispadias patients are incontinent, but 80% are continent postoperatively 7. Those who are still incontinent may require later bladder neck reconstruction 8. Although there is a paucity of literature on isolated female epispadias, reports suggest 87% to 100% continence after repair 9.
How is bladder exstrophy treated?
Treatment for bladder exstrophy begins at birth. Your care team should be readily available to help you in the immediate post-natal period. The primary goal when caring for a child with bladder exstrophy is to:
- preserve normal kidney function
- develop adequate bladder function and promote urinary continence
- provide acceptable appearance and function of the external genitalia
- ensure that your child has a typical and normal childhood
There are two main approaches to the repair of bladder exstrophy:
Complete primary repair of exstrophy
Complete primary repair of exstrophy is a procedure in which both the bladder is closed and the epispadias is repaired (entire urethra is closed into a tube) at the same time. Children who undergo complete primary repair of exstrophy will likely require additional surgery during later years to manage urinary incontinence and vesicoureteral reflux. This procedure is usually performed at approximately six-to-eight weeks of life. Delaying complete primary repair of exstrophy beyond the first, 2-to-3 days of life may have several advantages for the child. The delay presents an opportunity for normal bonding between the baby and parents before the initial reconstructive surgery and lengthy recovery period that follows.
The time between birth and initial repair allows for growth, development and additional maturation of some organs and systems prior to the complex surgery and makes the anesthesia and surgery safer.
Modern staged repair of exstrophy
Modern staged repair of exstrophy involves three surgeries for reconstruction of the bladder:
- The initial repair: The bladder and abdominal wall are closed, the belly button is reconstructed and an osteotomy is sometimes performed (the pelvic bones are reformed to aid in the repair). The initial repair is usually performed in the first 2-to-3 days of life.
- The second stage: In boys, the proximal part of the urethra close to the bladder is closed along with the bladder. In girls, the urethra is usually closed along its entire length, extending all the way from the bladder to the surface of the skin between the labia as it normally should be. The second stage repair occurs around 6-to-12 months of age.
- The third stage: This stage involves bladder neck reconstruction with bilateral ureteral reimplantation. This stage is performed when the bladder has grown sufficiently to hold an appropriate volume of urine. This procedure is usually performed between the ages of 6-to-10 years of age.
Possible complications of surgery
Some people with this condition may continue to have urinary incontinence, even after surgery.
Ureter and kidney damage and infertility may occur.
What is the long-term outlook for bladder exstrophy?
After initial treatment for bladder exstrophy, lifelong follow-up care is necessary. Care is ongoing and can involve a range of surgical procedures and tests. Every child is different, and our doctors and nurses will work with you to develop the best plan for your baby. In many cases, additional surgery is required during childhood, adolescence and young adulthood. To ensure that your child’s kidneys and bladder are functioning properly, follow-up testing, such as a renal ultrasound, may be necessary.
Hypospadias causes
Hypospadias is present at birth (congenital). As the penis develops in a male fetus, certain hormones stimulate the formation of the urethra and foreskin. Hypospadias results when a malfunction occurs in the action of these hormones, causing the urethra to develop abnormally. As the fetus develops, the tissue on the underside of the penis that forms the urethra doesn’t completely close, shortening the passageway. In many cases, the foreskin—the fold of skin covering the penis tip, or glans—also doesn’t develop properly, resulting in extra foreskin on the top side of the penis and none on the underside.
In most cases, the exact cause of hypospadias is unknown. Sometimes, hypospadias is genetic, but environment also may play a role. Hypospadias is slightly more common in boys whose father or brother also had the condition.
Risk factors for hypospadias
Although the cause of hypospadias is usually unknown, these factors may be associated with the condition:
- Family history. This condition is more common in infants with a family history of hypospadias.
- Genetics. Certain gene variations may play a role in disruption of the hormones that stimulate formation of the male genitals.
- Maternal age over 35 and weight. Some research suggests that there may be an increased risk of hypospadias in infant males born to women older than 35 years and who were considered obese had a higher risk of having a baby with hypospadias 10.
- Fertility treatments: Women who used assisted reproductive technology to help with pregnancy had a higher risk of having a baby with hypospadias 11.
- Exposure to certain substances during pregnancy. There is some speculation about an association between hypospadias and a mother’s exposure to certain hormones 12 or certain compounds such as pesticides or industrial chemicals, but further studies are needed to confirm this.
Hypospadias symptoms
In hypospadias, the opening of the urethra is located on the underside of the penis instead of at the tip. In most cases, the opening of the urethra is within the head of the penis. Less often, the opening is at the middle or the base of the penis. Rarely, the opening is in or beneath the scrotum.
Signs and symptoms of hypospadias may include:
- Opening of the urethra at a location other than the tip of the penis
- Downward curve of the penis (chordee)
- Hooded appearance of the penis because only the top half of the penis is covered by foreskin
- Abnormal spraying during urination or a downward urinary spray (in older children with more severe hypospadias, this may mean he has to sit down to urinate)
- An abnormal appearance of the tip of the penis (the glans)
- In some cases, boys born with hypospadias may also have undescended testicles and/or inguinal hernias (that is, hernias of the groin).
Hypospadias won’t cause your son physical pain or block his urination (though if it goes untreated it can make it difficult for him to direct his urine spray).
Hypospadias complications
If hypospadias is not treated, it can result in:
- Abnormal appearance of the penis
- Problems learning to use a toilet
- Abnormal curvature of the penis with erection
- Problems with impaired ejaculation
Hypospadias diagnosis
Your child’s pediatrician can diagnose hypospadias based on a physical exam. He or she will likely refer you to a surgeon who specializes in genital and urinary conditions (pediatric urologist) for further evaluation. Medical centers with specialty teams can help you evaluate options and can provide expert treatment.
When the opening of the urethra is abnormal and the testicles cannot be felt on exam, the genitals may be difficult to identify as clearly male or female (ambiguous genitalia). In this case, further evaluation with a multidisciplinary team is recommended.
Hypospadias treatment
If your son has a very mild case, he may not require surgery because his condition will not have a large impact on his life. However, sometimes parents of boys born with minor abnormalities still opt for surgery for cosmetic reasons, like straightening the penis and removing excess foreskin. However, treatment usually involves surgery to reposition the urethral opening and, if necessary, straighten the shaft of the penis. Surgery is usually done between the ages of 6 and 12 months.
If the penis looks abnormal, circumcision should not be done. If hypospadias is found during circumcision, the procedure should be completed. In either case, referral to a pediatric urologist is recommended.
Are there any medical alternatives to surgery?
No, surgery remains the best and only way to resolve your son’s urinary difficulties; to straighten and repair his penis so it will look more normal; and to help ensure that he will have full sexual function as an adult.
Hypospadias surgery
Most forms of hypospadias can be corrected in a single surgery that’s done on an outpatient basis. Some forms of hypospadias will require more than one surgery to correct the defect.
When the urethral opening is near the base of the penis, the surgeon may need to use tissue grafts from the foreskin or from the inside of the mouth to reconstruct the urinary channel in the proper position, correcting the hypospadias.
After surgery
Depending on the extent of surgery, your child may either go home the same day or stay in the hospital overnight. Your child’s surgeon/nurse will talk with you how to care for him at home and will provide detailed instruction sheets (how to manage his dressing, what activities should be avoided, etc.).
Also, your son’s surgeon will likely have inserted a soft drainage catheter, or stent, into the new urethra during the procedure. The stent will remain in your child’s urethra (you will be able to see the tip) to hold it open while it heals and to allow urine to drain from the bladder.
What to Expect at Home
Your child may feel sleepy when first at home. He may not feel like eating or drinking. He may also feel sick to his stomach or throw up the same day he had surgery.
Your child’s penis will be swollen and bruised. This will get better after a few weeks. Full healing will take up to 6 months.
Your child may need a urinary catheter for 5 to 14 days after the surgery.
- The catheter may be held in place with small stitches. The health care provider will remove the stitches when your child does not need the catheter anymore.
- The catheter will drain into your child’s diaper or a bag taped to his leg. Some urine may leak around the catheter when he urinates. There may also be a spot or two of blood. This is normal.
If your child has a catheter, he may have bladder spasms. These may hurt, but they are not harmful. If a catheter has not been put in, urinating be uncomfortable the first day or 2 after surgery.
Your child’s provider may write a prescription for some medicines:
- Oral antibiotics to prevent infection.
- Antibiotic ointment, to be applied to the penis several times a day
- Antispasmodic medication to relax the bladder and stop bladder spasms. These may cause your child’s mouth to feel dry.
- Prescription pain medicine, if needed. You can also give your child acetaminophen (Tylenol) for pain and soreness in the first few days after surgery
Taking Care of Your Child
Your child may eat a normal diet. Make sure he drinks plenty of fluids. Fluids help keep the urine clean.
A dressing with a clear plastic covering will be wrapped around the penis.
- If stool gets on the outside of the dressing, clean it gently with soapy water. Be sure to wipe away from the penis. DO NOT scrub.
- Give your child sponge baths until the dressing is off. When you do start bathing your son, use only warm water. DO NOT scrub. Gently pat him dry afterwards.
Some oozing from the penis is normal. You may see some spotting on the dressings, diaper, or underpants. If your child is still in diapers, ask your provider about how to use two diapers instead of one.
DO NOT use powders or ointments anywhere in the area before asking your child’s provider if it is ok.
Your child’s provider will probably ask you to take off the dressing after 2 or 3 days and leave it off. You may do this during a bath. Be very careful not to pull on the urine catheter. You will need to change the dressing before this if:
- The dressing rolls down and is tight around the penis.
- No urine has passed through the catheter for 4 hours.
- Stool gets underneath the dressing (not just on top of it).
Infants may do most of their normal activities except for swimming or playing in a sandbox. It is fine to take your baby for walks in the stroller.
Older boys should avoid contact sports, riding bicycles, straddling any toys, or wrestling for 3 weeks. It is a good idea to keep your child home from preschool or daycare the first week after his surgery.
When to Call the Doctor
Call the health care provider if your child has:
- Persistent low-grade fever or fever over 101°F (38.3°C) in the week after surgery.
- Increased swelling, pain, drainage, or bleeding from the wound.
- Trouble urinating.
- A lot of urine leakage around the catheter. This means the tube is blocked.
Also call if:
- Your child has thrown up more than 3 times and cannot keep fluid down.
- The stitches holding the catheter come out.
- The diaper is dry when it is time to change it.
- You have any concerns about your child’s condition.
Results of surgery
In most cases, surgery is highly successful. Most of the time the penis looks normal after surgery, and boys have normal urination and reproduction.
Occasionally, a hole (fistula) develops along the underside of the penis where the new urinary channel was created and results in urine leakage. Rarely, there is a problem with wound healing or scarring. These complications may require an additional surgery for repair.
Follow-up care
Your child’s doctor will remove the stent during a follow-up appointment 7 to 10 days after the surgery.
Your child will need a couple of visits to the surgeon after surgery. You typically can expect to see the full results of successful surgery within six months.
After that, regular follow-up with your child’s pediatric urologist is recommended after toilet training and at puberty to check for healing and possible complications.
When should the operation be scheduled?
This depends on what kind of hypospadias your child has, and whether he was diagnosed at birth (most boys are). Typically, if he requires surgery, we recommend that it be scheduled when he is between 4 and 6 months old.
Will this affect when and whether my son will be circumcised?
Babies who have hypospadias that requires surgery shouldn’t be circumcised, because the foreskin may be needed for tissue grafts during the operation.
How soon after surgery will my son’s penis looks like other little boys’?
It varies from patient to patient, but typically you’ll be able to see the full results of your son’s surgery after six months.
- Hypospadias: anatomy, etiology, and technique. Baskin LS, Ebbers MB. J Pediatr Surg. 2006 Mar; 41(3):463-72. https://www.ncbi.nlm.nih.gov/pubmed/16516617/[↩]
- Perovic S, editor. Atlas of Congenital Anomalies of the External Genitalia. Refot-Arka: Belgrad, Yugoslavia; 1999[↩]
- Management of epispadias. Grady RW, Mitchell ME. Urol Clin North Am. 2002 May; 29(2):349-60, vi. https://www.ncbi.nlm.nih.gov/pubmed/12371226/[↩]
- Kaefer M., Andler R., Bauer S. B., Hendren W. H., Diamond D. A., Retik A. B. Urodynamic findings in children with isolated epispadias. The Journal of Urology. 1999;162(3, part 2):1172–1175. doi: 10.1016/s0022-5347(01)68118-7 https://www.ncbi.nlm.nih.gov/pubmed/10458459[↩]
- Nelson CP, Dunn RL, Wei JT. Contemporary epidemiology of bladder exstrophy in the United States. Journal of Urology. 2005;173(5):1728–1731 https://www.ncbi.nlm.nih.gov/pubmed/15821570[↩]
- Wood HM, Babineau D, Gearhart JP. In vitro fertilization and the cloacal/bladder exstrophy-epispadias complex: a continuing association. Journal of Pediatric Urology. 2007;3(4):305–310. https://www.ncbi.nlm.nih.gov/pubmed/18947761[↩]
- Grady RW, Mitchell ME. Management of epispadias. Urologic Clinics of North America. 2002;29(2):349–360 https://www.ncbi.nlm.nih.gov/pubmed/12371226[↩]
- Ebert A-K, Reutter H, Ludwig M, Rösch WH. The exstrophy-epispadias complex. Orphanet Journal of Rare Diseases. 2009;4(article 23) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2777855/[↩]
- Suson KD, Preece J, Baradaran N, Di Carlo HN, Gearhart JP. The fate of the complete female epispadias and female exstrophy bladder—is there a difference? Journal of Urology. 2013;190(4):1583–1589. https://www.ncbi.nlm.nih.gov/pubmed/23376706[↩]
- Carmichael SL, Shaw GM, Laurent C, Olney RS, Lammer EJ, and the National Birth Defects Prevention Study. Maternal reproductive and demographic characteristics as risk factors for hypospadias. Paediatr Perinat Epidemiol. 2007; 21: 210–218.[↩]
- Reefhuis J, Honein MA, Schieve LA, Correa A, Hobbs CA, Rasmussen SA, and the National Birth Defects Prevention Study. Assisted reproductive technology and major structural birth defects in the United States. Human Rep. 2009; 24:360–366[↩]
- Carmichael SL, Shaw GM, Laurent C, Croughan MS, Olney RS, Lammer EJ. Maternal progestin intake and risk of hypospadias. Arch Pediatr Adolesc Med. 2005;159: 957–962[↩]