What is hypothermia
Hypothermia is a medical emergency that occurs when your body’s temperature drops from the usual healthy 98.6° F (37° C) to below 95° F (35° C). A drop in body temperature to 89.6° F (32 °C) or less can be fatal. This can develop with prolonged exposure to temperatures under 50° F (10° C), or after prolonged immersion in cold water of less than 68° F (20° C). Left untreated, hypothermia can eventually lead to complete failure of your heart and respiratory system and eventually to death.
If you are exposed to prolonged cold conditions, whether outdoors or in an unheated house, you may get hypothermia. You are at greater risk if you are elderly, very young, underweight, or in poor health. Babies can get it from sleeping in a cold room. Temperature regulation in the elderly is impaired making the elderly more prone to hypothermia (cold temperature). Even during the heat of summer, older people and very small children are at risk if air conditioning makes their homes too cold.
For parents and carers of children
- Young children and babies are at high risk from extreme cold and can develop hypothermia very quickly as their body size is so small. It is important to cover their head if they are out in cold weather.
- Children can become colder much quicker than adults because they have less muscle mass.
- Limit exposure to prolonged or extreme cold weather.
- Babies with hypothermia may look healthy, but their skin will feel cold. They may also be limp, unusually quiet and refuse to feed.
- Keep your home at a temperature of at least 64.4° F (18° C)
- A baby’s room should be 60-68° F (16-20° C)
- Keep windows and internal doors shut
- Wear warm clothes
- Use a room thermometer
Postoperative hypothermia causes shivering, increasing work on a potentially over-worked heart, putting the patient at risk of suffering a heart attack.
- If you suspect someone has severe hypothermia, call your local emergency number for an ambulance immediately.
- A body temperature below 95° F (35° C) is a medical emergency and can lead to death if not treated promptly.
- Several hundred people in the U.S.—half of them age 65 or older—die from hypothermia each year.
Hypothermia can make you sleepy, confused, and clumsy. Because hypothermia happens gradually and affects your thinking, you may not realize you need help. That makes hypothermia especially dangerous. A body temperature below 95° F (35° C) is a medical emergency and can lead to death if not treated promptly.
The US Centers for Disease Control and Prevention (CDC) report the following statistics for deaths by excessive natural cold in the period 1999-2011 1:
- Total deaths: 16,911
- Average deaths per year: 1,301
- Highest yearly total: 1,536 (2010)
- Lowest yearly total: 1,058 (2006)
- Approximately 67% were among males
The overall mortality rate from hypothermia is similar between men and women. Because of a higher incidence of exposure among males, men account for 65% of hypothermia-related deaths.
Your body is finely tuned to operate within a narrow temperature range inside the body, despite large differences in temperature outside the body. The body’s core temperature is tightly regulated in the “thermoneutral zone” between 36.5°C and 37.5°C, outside of which thermoregulatory responses are usually activated. You have all sorts of mechanisms—like adjusting the size of our small blood vessels and shivering—to help you maintain a healthy body temperature. But older adults and young children are more susceptible to the effects of outside temperature changes. The hypothalamus controls thermoregulation via increased heat conservation (peripheral vasoconstriction and behavior responses) and heat production (shivering and increasing levels of thyroxine and epinephrine). Alterations of the central nervous system may impair these mechanisms. The threshold for shivering is 1 degree lower than that of vasoconstriction and is considered a last resort mechanism by the body to maintain temperature 2. The body maintains a stable core temperature through balancing heat production and heat loss. At rest, humans produce 40-60 kilocalories (kcal) of heat per square meter of body surface area through generation by cellular metabolism, most prominently in the liver and the heart. Heat production increases with striated muscle contraction; shivering increases the rate of heat production 2-5 times. The mechanisms for heat preservation may be overwhelmed in the face of cold stress and core temperature can drop secondary to fatigue or glycogen depletion.
When your body’s inside temperature strays beyond that narrow range, your body functions don’t operate well causing health problems, such as a heart attack, kidney problems, liver damage, or worse. Hypothermia results in decreased depolarization of cardiac pacemaker cells, causing bradycardia (slower than normal heart rate ~ less than 60 beats a minute). Atrial and ventricular arrhythmias can result from hypothermia; asystole and ventricular fibrillation have been noted to begin spontaneously at core temperatures below 25-28°C.
Hypothermia progressively depresses the central nervous system (CNS), decreasing CNS metabolism in a linear fashion as the core temperature drops. At core temperatures less than 33°C, brain electrical activity becomes abnormal; between 19°C and 20°C, an electroencephalogram (EEG) may appear consistent with brain death. Tissues have decreased oxygen consumption at lower temperatures; it is not clear whether this is due to decreases in metabolic rate at lower temperatures or a greater hemoglobin affinity for oxygen coupled with impaired oxygen extraction of hypothermic tissues.
When cold affects your body, you may have trouble thinking clearly, talking properly, or moving well. You may not realize what’s happening, or you might not be able to take steps to warm up or ask for help.
Sometimes it is hard to tell if a person has hypothermia. Look for clues. Is the house very cold? Is the person not dressed for cold weather? Is the person speaking slower than normal and having trouble keeping his or her balance?
Watch for the signs of hypothermia in yourself, too. You might become confused if your body temperature gets very low. Talk to your family and friends about the warning signs so they can look out for you.
Early signs of hypothermia:
- Cold feet and hands
- Puffy or swollen face
- Pale skin
- Shivering (in some cases the person with hypothermia does not shiver)
- Slower than normal speech or slurring words
- Acting sleepy
- Being angry or confused
Later signs of hypothermia:
- Moving slowly, trouble walking, or being clumsy
- Stiff and jerky arm or leg movements
- Slow heartbeat
- Slow, shallow breathing
- Blacking out or losing consciousness
Call your local emergency number right away if you think someone has warning signs of hypothermia.
What to do after you call your local emergency number for an ambulance to arrive:
- Try to move the person to a warmer place.
- Wrap the person in a warm blanket, towels, or coats—whatever is handy. Even your own body warmth will help. Lie close, but be gentle.
- Give the person something warm to drink, but avoid drinks with alcohol or caffeine, such as regular coffee.
- Do not rub the person’s legs or arms.
- Do not try to warm the person in a bath.
- Do not use a heating pad.
The only way to tell for sure that someone has hypothermia is to use a special thermometer that can read very low body temperatures. Most hospitals have these thermometers. In the emergency room, doctors will warm the person’s body from inside out. For example, they may give the person warm fluids directly by using an IV. Recovery depends on how long the person was exposed to the cold and his or her general health.
Who is at risk of hypothermia?
Hypothermia can affect anyone, those at higher risk include:
- people over 75 years.
- babies and young children – they lose heat faster than adults
- heavy alcohol and drug users – their bodies lose heat faster
- people with poor circulation or diabetes.
- people with chronic physical or mental disabilities.
- people with underlying infection.
- people who are very thin and have low body fat.
- people who work outdoors.
- people who are homeless.
- people who are wet from any cause.
Some things can make hypothermia worse:
- Don’t put the person into a hot bath.
- Don’t massage their limbs.
- Don’t use heating lamps.
- Don’t give them alcohol to drink.
These actions can cause the heart to suddenly stop beating (cardiac arrest).
Staying warm in cold weather
Before you or your children step out into cold air, remember the advice that follows with the simple acronym COLD — cover, overexertion, layers, dry:
- Cover. Wear a hat or other protective covering to prevent body heat from escaping from your head, face and neck. Cover your hands with mittens instead of gloves.
- Overexertion. Avoid activities that would cause you to sweat a lot. The combination of wet clothing and cold weather can cause you to lose body heat more quickly.
- Layers. Wear loosefitting, layered, lightweight clothing. Outer clothing made of tightly woven, water-repellent material is best for wind protection. Wool, silk or polypropylene inner layers hold body heat better than cotton does.
- Dry. Stay as dry as possible. Get out of wet clothing as soon as possible. Be especially careful to keep your hands and feet dry, as it’s easy for snow to get into mittens and boots.
Hypothermia prognosis
The risk of morbidity and mortality depends on the severity of the degree of hypothermia and the underlying cause. Recovery is usually complete for previously healthy individuals with mild or moderate hypothermia (mortality rate < 5%). The mortality rate for patients with severe hypothermia, especially with preexisting illness, may be higher than 50%.
According to one study, overall in-patient mortality in hypothermic patients was 12%. Most people tolerate mild hypothermia (32-35°C body temperature) fairly well, which is not associated with significant morbidity or mortality. In contrast, a multicenter survey found a 21% mortality rate for patients with moderate hypothermia (28-32°C body temperature). Mortality is even higher in severe hypothermia (core temperature below 28°C). Despite hospital-based treatment, mortality from moderate or severe hypothermia approaches 40%. Patients experiencing concurrent infection account for most deaths due to hypothermia. Other comorbidities associated with higher mortality rates include homelessness, alcoholism, psychiatric disease, and advanced age.
“Indoor hypothermia” is more likely to occur in patients with significant medical comorbidities (alcoholism, sepsis, hypothyroidism/hypopituitarism) and tends to carry worse outcomes than exposure hypothermia.
According to current records, approximately 700 people die in the United States from accidental primary hypothermia each year.
Hypothermia complications
People who develop hypothermia because of exposure to cold weather or cold water are also vulnerable to other cold-related injuries, including:
- Freezing of body tissues (frostbite)
- Decay and death of tissue resulting from an interruption in blood flow (gangrene)
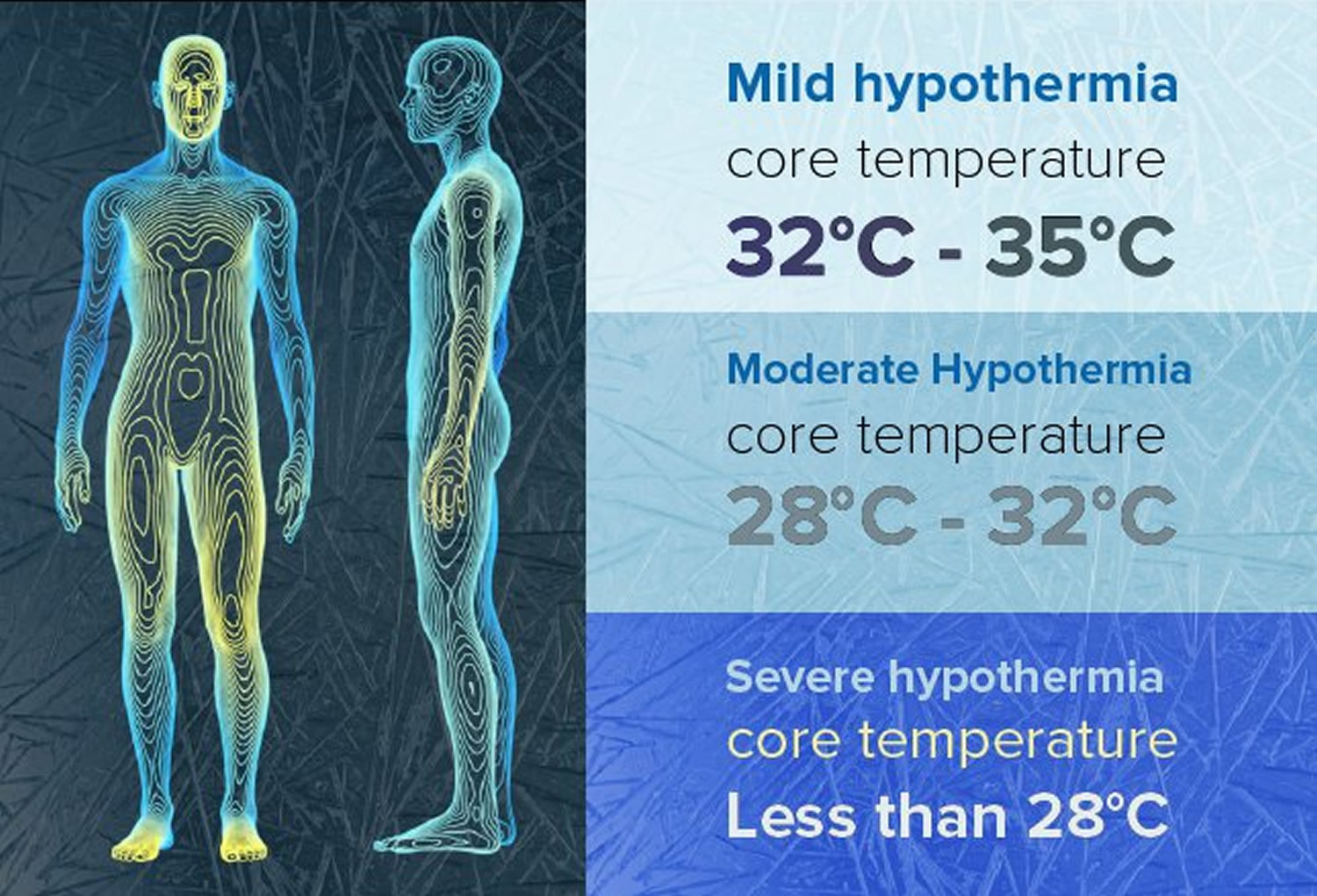
Hypothermia stages
The diagnosis is generally made based on the person’s symptoms and the condition in which the person became unwell or was found. However, if the diagnosis is not obvious, it can be made by measuring the core body temperature with a special low-reading thermometer (general medical thermometers do not measure temperatures below 32-34°C).
- Mild hypothermia: 32-35°C.
- Moderate hypothermia (28-32°C)
- Severe hypothermia: below 28°C.
Mild hypothermia (32-35°C)
Between 34°C and 35°C, most people shiver vigorously, usually in all extremities.
As the temperature drops below 34°C, a patient may develop altered judgment, amnesia, and dysarthria. Respiratory rate may increase.
At approximately 33°C, ataxia and apathy may be seen. Patients generally are stable hemodynamically and able to compensate for the symptoms.
In this temperature range, the following may also be observed: hyperventilation, tachypnea, tachycardia, and cold diuresis as renal concentrating ability is compromised.
Moderate hypothermia (28-32°C)
Oxygen consumption decreases, and the central nervous system depresses further; hypoventilation, hyporeflexia, decreased renal flow, and paradoxical undressing may be noted.
Most patients with temperatures of 32°C or lower present in stupor.
As the core reaches temperatures of 31°C or below, the body loses its ability to generate heat by shivering.
At 30°C, patients develop a higher risk for arrhythmias. Atrial fibrillation and other atrial and ventricular rhythms become more likely. The pulse continues to slow progressively, and cardiac output is reduced. J wave may be seen on ECG in moderate hypothermia.
Between 28°C and 30°C, pupils may become markedly dilated and minimally responsive to light, a condition that can mimic brain death.
Severe hypothermia (<28°C)
At 28°C, the body becomes markedly susceptible to ventricular fibrillation and further depression of myocardial contractility.
Below 27°C, 83% of patients are comatose.
Pulmonary edema, oliguria, coma, hypotension, rigidity, apnea, pulselessness, areflexia, unresponsiveness, fixed pupils, and decreased or absent activity on EEG are all seen.
Hypothermia causes
Hypothermia occurs when your body loses heat faster than it produces it.
You may get hypothermia if you spend time in air below 50° F (10° C) or in water below 68° F (20° C). Some medical conditions can also make people susceptible to hypothermia. But prolonged exposure to any environment colder than your body can lead to hypothermia if you aren’t dressed appropriately or can’t control the conditions.
Specific conditions leading to hypothermia include:
- Wearing clothes that aren’t warm enough for weather conditions
- Staying out in the cold too long
- Being unable to get out of wet clothes or move to a warm, dry location
- Falling into the water, as in a boating accident
- Living in a house that’s too cold, either from poor heating or too much air conditioning
How your body loses heat
The mechanisms of heat loss from your body include the following:
- Radiated heat. Most heat loss is due to heat radiated from unprotected surfaces of your body.
- Direct contact. If you’re in direct contact with something very cold, such as cold water or the cold ground, heat is conducted away from your body. Because water is very good at transferring heat from your body, body heat is lost much faster in cold water than in cold air. Similarly, heat loss from your body is much faster if your clothes are wet, as when you’re caught out in the rain.
- Wind. Wind removes body heat by carrying away the thin layer of warm air at the surface of your skin. A wind chill factor is important in causing heat loss.
Risk factors for hypothermia
Risk factors for hypothermia include:
- Exhaustion. Your tolerance for cold diminishes when you are fatigued.
- Older age. The body’s ability to regulate temperature and to sense cold may lessen with age. And some older adults may not be able to communicate when they are cold or to move to a warm location if they do feel cold.
- Very young age. Children lose heat faster than adults do. Children may also ignore the cold because they’re having too much fun to think about it. And they may not have the judgment to dress properly in cold weather or to get out of the cold when they should.
- Mental problems. People with a mental illness, dementia or other conditions that interfere with judgment may not dress appropriately for the weather or understand the risk of cold weather. People with dementia may wander from home or get lost easily, making them more likely to be stranded outside in cold or wet weather.
- Alcohol and drug use. Alcohol may make your body feel warm inside, but it causes your blood vessels to expand, resulting in more rapid heat loss from the surface of your skin. The body’s natural shivering response is diminished in people who’ve been drinking alcohol. In addition, the use of alcohol or recreational drugs can affect your judgment about the need to get inside or wear warm clothes in cold weather conditions. If a person is intoxicated and passes out in cold weather, he or she is likely to develop hypothermia.
- Certain medical conditions. Some health disorders affect your body’s ability to regulate body temperature. Examples include an underactive thyroid (hypothyroidism), poor nutrition or anorexia nervosa, diabetes, stroke, severe arthritis, Parkinson’s disease, trauma, and spinal cord injuries.
- Medications. Some drugs can change the body’s ability to regulate its temperature. Examples include certain antidepressants, antipsychotics, narcotic pain medications and sedatives.
Hypothermia prevention
Follow some of the common sense advice that you’ve probably all heard. Dress in layers; cover up with blankets; and if you expect to be out in the wind, rain or snow, wear a jacket with a waterproof and windproof outer shell.
If you live or work outdoors in a cold climate, or are planning a camping or hiking trip in the cold, you can decrease the risk of hypothermia by:
- listening to the weather forecast
- limiting the amount of time you spend outdoors in the cold
- planning ‘warm-up’ breaks if you work outside
- dressing warmly, including wearing a wind resistant jacket, gloves and a hat
- avoiding alcohol, caffeine and cigarettes, which can make you more sensitive to cold
- asking your doctor if your medication can make you susceptible to cold
- making sure your home is adequately heated.
Make sure you cover your children’s heads when they are out in the cold – kids can lose body heat more quickly than adults.
To keep warm at home, wear socks, slippers, and a cap or hat. Set your heat at 68° F (20° C) or higher when it’s cold outside. To save on heating bills, close off rooms you’re not using. If you need help paying your home heating bills, you may qualify for an energy assistance program.
- Get Help With Your Energy Bills https://liheapch.acf.hhs.gov/help
Here are some tips for keeping warm while you’re inside:
- Set your heat at 68° F (20° C) or higher. To save on heating bills, close off rooms you are not using. Close the vents and shut the doors in these rooms, and keep the basement door closed. Place a rolled towel in front of all doors to keep out drafts.
- Make sure your house isn’t losing heat through windows. Keep your blinds and curtains closed. If you have gaps around the windows, try using weather stripping or caulk to keep the cold air out.
- Dress warmly on cold days even if you are staying in the house. Throw a blanket over your legs. Wear socks and slippers.
- When you go to sleep, wear long underwear under your pajamas, and use extra covers. Wear a cap or hat.
- Make sure you eat enough food to keep up your weight. If you don’t eat well, you might have less fat under your skin. Body fat helps you to stay warm.
- Drink alcohol moderately, if at all. Alcoholic drinks can make you lose body heat.
- Ask family or friends to check on you during cold weather. If a power outage leaves you without heat, try to stay with a relative or friend.
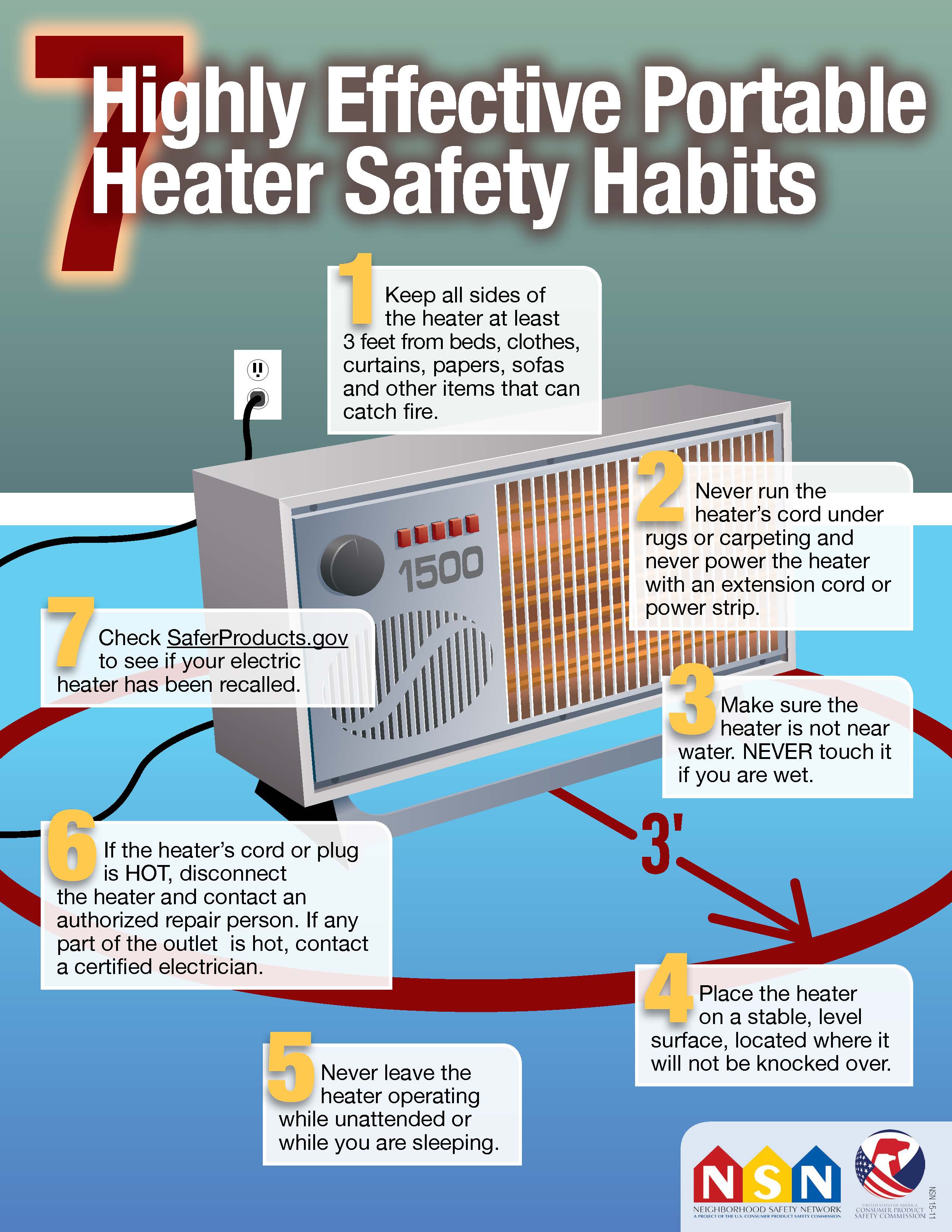
You may be tempted to warm your room with a space heater. But, some space heaters are fire hazards, and others can cause carbon monoxide poisoning. The Consumer Product Safety Commission 3 has information on the use of space heaters.
Bundle Up on Windy, Cold Days
A heavy wind can quickly lower your body temperature. Check the weather forecast for windy and cold days. On those days, try to stay inside or in a warm place. If you have to go out, wear warm clothes, and don’t stay out in the cold and wind for a long time.
Here are some other tips:
- Dress for the weather if you have to go out on chilly, cold, or damp days.
- Wear loose layers of clothing. The air between the layers helps to keep you warm.
- Put on a hat and scarf. You lose a lot of body heat when your head and neck are uncovered.
- Wear a waterproof coat or jacket if it’s snowy.
Illness, Medicines, and Cold Weather
Some illnesses may make it harder for your body to stay warm. Diabetes, thyroid problems, Parkinson’s disease, memory loss, and arthritis are problems that can make it harder for older adults to stay warm. Talk with your doctor about your health problems and how to prevent hypothermia.
Taking some medicines and not being active also can affect body heat. These include medicines you get from your doctor and those you buy over-the-counter. Ask your doctor if the medicines you take may affect body heat. Always talk with your doctor before you stop taking any medication.
Here are some topics to talk about with your doctor to stay safe in cold weather:
- Ask your doctor about signs of hypothermia.
- Talk to your doctor about any health problems and medicines that can make hypothermia a special problem for you. Your doctor can help you find ways to prevent hypothermia.
- Ask about safe ways to stay active even when it’s cold outside.
Keeping children safe from the cold
To help prevent hypothermia when children are outside in the winter:
- Dress infants and young children in one more layer than an adult would wear in the same conditions.
- Bring children indoors if they start shivering — that’s the first sign that hypothermia is starting.
- Have children come inside frequently to warm themselves when they’re playing outside.
- Don’t let babies sleep in a cold room.
Winter car safety
Whenever you’re traveling during bad weather, be sure someone knows where you’re headed and at what time you’re expected to arrive. That way, if you get into trouble on your way, emergency responders will know where to look for your car.
It’s also a good idea to keep emergency supplies in your car in case you get stranded. Supplies may include several blankets, matches, candles, a clean can where you can melt snow into drinking water, a first-aid kit, dry or canned food, a can opener, tow rope, booster cables, compass, and a bag of sand or kitty litter to spread for traction if you’re stuck in the snow. If possible, travel with a cellphone.
If you’re stranded, put everything you need in the car with you, huddle together and stay covered. Run the car for 10 minutes each hour to warm it up. Make sure a window is slightly open and the exhaust pipe isn’t covered with snow while the engine is running.
To avoid alcohol-related risks of hypothermia, don’t drink alcohol:
- If you’re going to be outside in cold weather
- If you’re boating
- Before going to bed on cold nights
Cold-water safety
Water doesn’t have to be extremely cold to cause hypothermia. Any water that’s colder than normal body temperature causes heat loss. (8, p2) The following tips may increase your survival time in cold water if you accidentally fall in:
- Wear a life jacket. If you plan to ride in a watercraft, wear a life jacket. A life jacket can help you stay alive longer in cold water by enabling you to float without using energy and by providing some insulation. Keep a whistle attached to your life jacket to signal for help.
- Get out of the water if possible. Get out of the water as much as possible, such as climbing onto a capsized boat or grabbing onto a floating object.
- Don’t attempt to swim unless you’re close to safety. Unless a boat, another person or a life jacket is close by, stay put. Swimming will use up energy and may shorten survival time.
- Position your body to minimize heat loss. Use a body position known as the heat escape lessening position (HELP) to reduce heat loss while you wait for assistance. Hold your knees to your chest to protect the trunk of your body. If you’re wearing a life jacket that turns your face down in this position, bring your legs tightly together, your arms to your sides and your head back.
- Huddle with others. If you’ve fallen into cold water with other people, keep warm by facing each other in a tight circle.
- Don’t remove your clothing. While you’re in the water, don’t remove clothing because it helps to insulate you from the water. Buckle, button and zip up your clothes. Cover your head if possible. Remove clothing only after you’re safely out of the water and can take measures to get dry and warm.
Help for at-risk people
For people most at risk of hypothermia — infants, older adults, people who have mental or physical problems, and people who are homeless — community outreach programs and social support services can be of great help. If you’re at risk or know someone at risk, contact your local public health office for available services, such as the following:
- Assistance for paying heating bills. Get Help With Your Energy Bills https://liheapch.acf.hhs.gov/help
- Check-in services to see if you and your home are warm enough during cold weather
- Homeless shelters
- Community warming centers, safe and warm daytime locations where you can go during cold weather
Hypothermia signs and symptoms
Shivering is likely the first thing you’ll notice as the temperature starts to drop because it’s your body’s automatic defense against cold temperature — an attempt to warm itself.
Someone with hypothermia usually isn’t aware of his or her condition because the symptoms often begin gradually. Also, the confused thinking associated with hypothermia prevents self-awareness. The confused thinking can also lead to risk-taking behavior.
People with mild hypothermia feel cold. They may also:
- Be shivering uncontrollably
- Have slurred speech or mumbling
- Have slow, shallow breathing
- Have a weak pulse
- Have clumsiness or lack of coordination
- Have drowsiness or very low energy
- Have confusion or memory loss
- Have loss of consciousness
- Be bright red, cold skin (in infants)
- Have cool, pale skin
- Be clumsy and walk unsteadily
- Be confused and drowsy.
People with severe hypothermia might have stopped shivering. They might:
- breathe slowly
- have a slow heart rate
- have dilated pupils
- be in a coma.
They might even look like they are dead.
- If you suspect someone has severe hypothermia, call your local emergency number for an ambulance immediately.
Hypothermia diagnosis
The diagnosis of hypothermia is usually apparent based on a person’s physical signs and the conditions in which the person with hypothermia became ill or was found. Blood tests also can help confirm hypothermia and its severity.
A diagnosis may not be readily apparent, however, if the symptoms are mild, as when an older person who is indoors has symptoms of confusion, lack of coordination and speech problems.
Hypothermia treatment
Seek immediate medical attention for anyone who appears to have hypothermia. Until medical help is available, follow these first-aid guidelines for hypothermia.
If you suspect someone has hypothermia:
First get the person out of the cold or wet environment if possible, remove any wet clothes, and cover the person with dry blankets or whatever’s handy.
Hypothermia first aid treatment
- Move them to somewhere warm.
- Take off any wet clothes.
- Warm their head, neck, chest and groin with blankets or wrapped hot water bottles, or get someone warm to cuddle them.
- Cover the person with blankets. Use layers of dry blankets or coats to warm the person. Cover the person’s head, leaving only the face exposed.
- Insulate the person’s body from the cold ground. If you’re outside, lay the person on his or her back on a blanket or other warm surface.
- Don’t apply direct heat. Avoid things like a hot-water bath or a heating pad. External heat sources for hypothermia can be risky because of the potential for things like burns, low blood pressure, or irregular heart rhythms.
- Keep them still.
- Give them warm drinks, but avoid alcohol or caffeinated beverages like coffee.
- Monitor breathing. A person with severe hypothermia may appear unconscious, with no apparent signs of a pulse or breathing. If the person’s breathing has stopped or appears dangerously low or shallow, begin CPR (cardiopulmonary resuscitation) immediately if you’re trained.
If they look like they’re dead, call your local emergency number for an ambulance and give CPR (cardiopulmonary resuscitation).
Don’t make them exert themselves and don’t rub them vigorously.
Active rewarming techniques are best used in settings where doctors can closely monitor a patient’s vital signs, so getting professional help is important.
Medical treatment
Depending on the severity of hypothermia, emergency medical care for hypothermia may include one of the following interventions to raise the body temperature:
- Passive rewarming. For someone with mild hypothermia, it is enough to cover them with heated blankets and offer warm fluids to drink.
- Blood rewarming. Blood may be drawn, warmed and recirculated in the body. A common method of warming blood is the use of a hemodialysis machine, which is normally used to filter blood in people with poor kidney function. Heart bypass machines also may need to be used.
- Warm intravenous fluids. A warmed intravenous solution of salt water may be put into a vein to help warm the blood.
- Airway rewarming. The use of humidified oxygen administered with a mask or nasal tube can warm the airways and help raise the temperature of the body.
- Irrigation. A warm saltwater solution may be used to warm certain areas of the body, such as the area around the lungs (pleura) or the abdominal cavity (peritoneal cavity). The warm liquid is introduced into the affected area with catheters.
How to perform a Cardiopulmonary Resuscitation (CPR)
If the person’s breathing or heart stops, cardiopulmonary resuscitation (CPR) should be performed immediately.
Hands-only CPR
- Ensure the area is safe
- Check for hazards, such as electrical equipment or traffic.
To carry out a chest compression:
- Place the heel of your hand on the breastbone at the center of the person’s chest. Place your other hand on top of your first hand and interlock your fingers.
- Position yourself with your shoulders above your hands.
- Using your body weight (not just your arms), press straight down by 5-6cm (2-2.5 inches) on their chest.
- Keeping your hands on their chest, release the compression and allow the chest to return to its original position.
- Repeat these compressions at a rate of 100 to 120 times per minute until an ambulance arrives or you become exhausted.
When you call for an ambulance, telephone systems now exist that can give basic life-saving instructions, including advice about CPR. These are now common and are easily accessible with mobile phones.
Cardiopulmonary Resuscitation (CPR) with rescue breaths
If you’ve been trained in CPR, including rescue breaths, and feel confident using your skills, you should give chest compressions with rescue breaths. If you’re not completely confident, attempt hands-only CPR instead (see above).
Adults
- Place the heel of your hand on the centre of the person’s chest, then place the other hand on top and press down by 5-6cm (2-2.5 inches) at a steady rate of 100 to 120 compressions per minute.
- After every 30 chest compressions, give two rescue breaths.
- Tilt the casualty’s head gently and lift the chin up with two fingers. Pinch the person’s nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth for about one second. Check that their chest rises. Give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Children over one year old
- Open the child’s airway by placing one hand on the child’s forehead and gently tilting their head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Pinch their nose. Seal your mouth over their mouth and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place the heel of one hand on the center of their chest and push down by 5cm (about two inches), which is approximately one-third of the chest diameter.
- The quality (depth) of chest compressions is very important. Use two hands if you can’t achieve a depth of 5cm using one hand.
- After every 30 chest compressions at a rate of 100 to 120 per minute, give two breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Infants under one year old
- Open the infant’s airway by placing one hand on their forehead and gently tilting the head back and lifting the chin. Remove any visible obstructions from the mouth and nose.
- Place your mouth over the mouth and nose of the infant and blow steadily and firmly into their mouth, checking that their chest rises. Give five initial rescue breaths.
- Place two fingers in the middle of the chest and push down by 4cm (about 1.5 inches), which is approximately one-third of the chest diameter. The quality (depth) of chest compressions is very important. Use the heel of one hand if you can’t achieve a depth of 4cm using the tips of two fingers.
- After 30 chest compressions at a rate of 100 to 120 per minute, give two rescue breaths.
- Continue with cycles of 30 chest compressions and two rescue breaths until they begin to recover or emergency help arrives.
Therapeutic hypothermia
Intentional hypothermia also known as therapeutic hypothermia is an induced state generally directed at neuroprotection after an at-risk situation (usually after cardiac arrest). Targeted temperature management, previously known as mild therapeutic hypothermia, in selected patients surviving out-of-hospital sudden cardiac arrest can significantly improve rates of long-term neurologically intact survival and may prove to be one of the most important clinical advancements in the science of resuscitation.
Despite nearly 40 years of prehospital advanced life support, the survival rate of out-of-hospital cardiac arrest is very poor 4. Less than half of victims who develop return of spontaneous circulation survive to leave the hospital alive, and the cause of death is anoxic brain injury in most patients with return of spontaneous circulation who die within one month of the cardiac arrest. Inducing mild therapeutic hypothermia in selected patients surviving out-of-hospital sudden cardiac arrest has a major impact on long-term neurologically intact survival and may prove to be one of the most important clinical advancements in the science of resuscitation.
A 2011 meta-analysis of randomized controlled trials found that therapeutic hypothermia with conventional cooling methods improves both survival and neurologic outcomes at hospital discharge for patients who experienced cardiac arrest 5.
In a retrospective cohort study covering 7 years that assessed the impact of therapeutic hypothermia on early repolarization in survivors of cardiac arrest attributed to idiopathic ventricular fibrillation compared with a control group who experienced coronary artery disease-related ventricular fibrillation, Williams et al 6 found that hypothermia increased the prevalence and mean amplitude of early repolarization in cardiac arrest survivors. Early repolarization occurred in all survivors of idiopathic ventricular fibrillation (100%) compared with over two third of survivors of coronary artery disease-related ventricular fibrillation (67%); therapeutic hypothermia increased early repolarization amplitude only in coronary artery disease-related ventricular fibrillation survivors 6.
Two early studies demonstrated improved survival and neurological outcomes with induction of mild therapeutic hypothermia for comatose survivors of out-of-hospital cardiac arrest. The Hypothermia after Cardiac Arrest Study Group showed that, when applied to unconscious out-of-hospital cardiac arrest patients with return of spontaneous circulation (n=274), mild hypothermia (cooling to 32ºC-34ºC) provided significant improvement in functional recovery at hospital discharge (55% vs 39%; number needed to treat = 6) and lower 6-month mortality rate when compared with patients who were not cooled (41% vs 55%) (number needed to treat = 7) 7.
The needed to treat is very low and comparable to other important emergent treatments such as cardiac catheterization for acute coronary syndrome 8. Bernard examined endpoint of survival to hospital discharge to home or a rehabilitation facility (good outcome) in 77 patients and demonstrated 49% in the hypothermia group compared with 26% in the normothermic group, finding an needed to treat of 4.5 for death and severe disability 9.
After studying 133 comatose patients who experienced after out-of-hospital cardiac arrest and were treated with therapeutic hypothermia, Kragholm et al 10 found that one year later, most patients who were able to work prior to cardiac arrest were able to return to work.
Literature primarily evaluating different durations of therapeutic hypothermia are lacking, as most studies maintain temperatures for at least 24 hours, with some longer (36 hours), followed by slow return to normothermia. Temperature sensitivity of the central nervous system following cardiac arrest can last as long as coma is present, and the duration of the therapeutic hypothermia upper limit is unknown 11.
Therapeutic hypothermia may also confer benefits to patients experiencing cardiac arrest in other clinical environments 12, patients with hemorrhagic shock 13 and patients with other forms of severe brain injury 14. Currently, at least 19 clinical trials are underway and focus principally on return of spontaneous circulation, traumatic brain injury, stroke, neonatal hypoxic-ischemic encephalopathy, and medical device safety 15. Currently, no evidence supports using this modality for stroke 16.
Figure 1. Hypothermia protocol
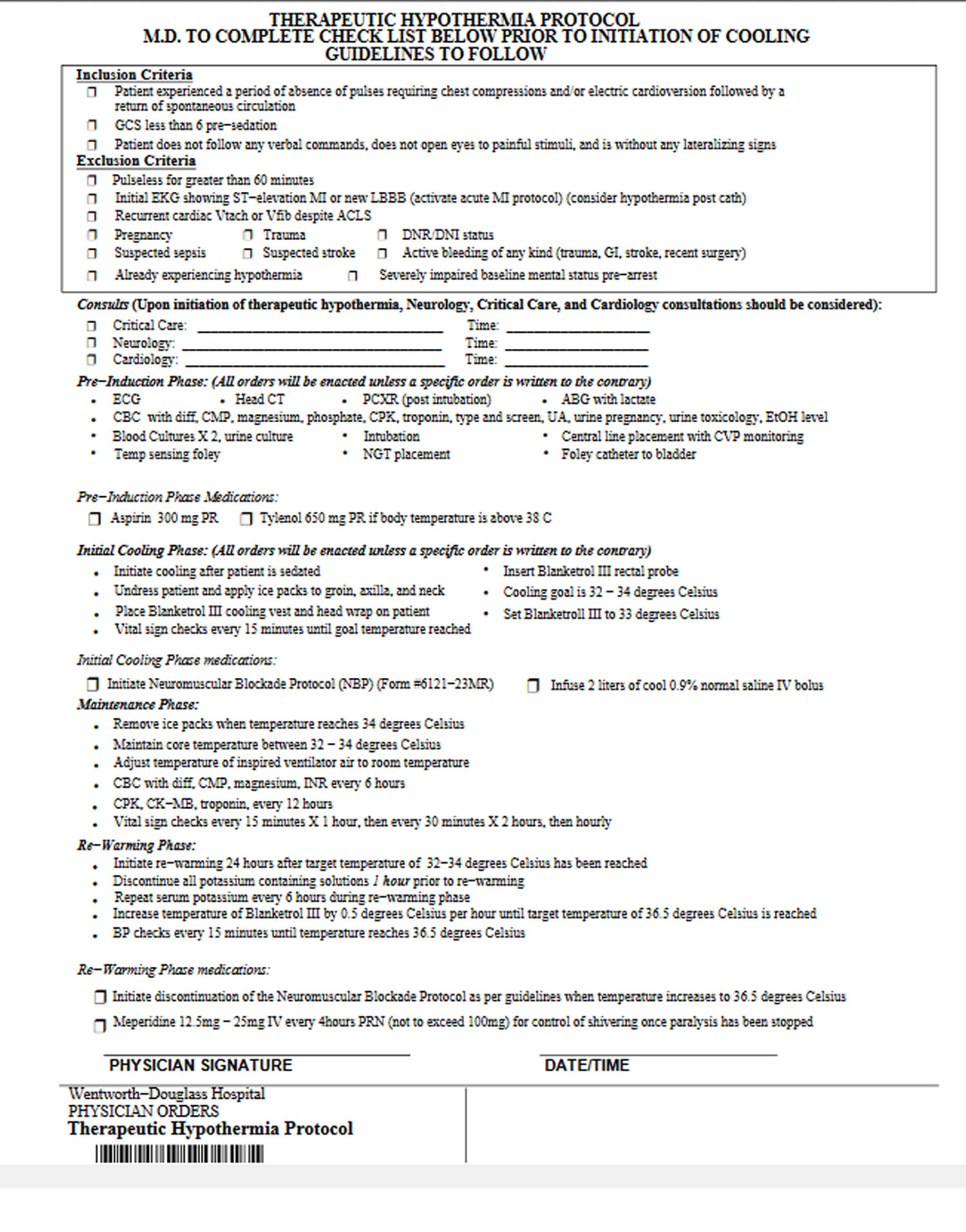 [Source 17]
[Source 17]
The 2015 American Heart Association guidelines on therapeutic hypothermia can be summarized as follows 18:
- Induce hypothermia for unconscious adult patients with return of spontaneous circulation after out-of-hospital cardiac arrest when the initial rhythm was ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT)
- Similar therapy may be beneficial for patients with non-ventricular fibrillation/non-pulseless ventricular tachycardia (nonshockable) arrest out-of-hospital or with in-hospital arrest
- The temperature should be maintained between 32ºC and 36ºC
- It is reasonable to maintain therapeutic hypothermia for at least 24 hours
- Routine prehospital cooling of patients with return of spontaneous circulation with intravenous (IV) rapid infusion is not advised
- It is reasonable to prevent fever in comatose patients after therapeutic hypothermia
- Hemodynamically stable patients with spontaneous mild hypothermia (>33°C) after resuscitation from cardiac arrest should not be actively rewarmed
Inclusion criteria
- Patients who have been shown to benefit from induced hypothermia include the following (however, strict inclusion criteria vary by institution):
- Intubated patients with treatment initiated within 6 hours after cardiac arrest (nonperfusing ventricular tachycardia or ventricular fibrillation)
- Patients able to maintain a systolic blood pressure above 90 mm Hg, with or without pressors, after cardiopulmonary resuscitation (CPR)
- Patients in a coma at the time of cooling
Exclusion criteria
- Patients for whom hypothermia may theoretically carry increased risk include those with the following conditions:
- Recent major surgery within 14 days – Possible risk for infection and bleeding
- Systemic infection/sepsis – Small increase in risk of infection
- Coma from other causes (drug intoxication, preexisting coma prior to arrest)
- Known bleeding diathesis or with active ongoing bleeding – Hypothermia may impair the clotting system (however, patients may receive chemical thrombolysis, antiplatelet agents, or anticoagulants if deemed necessary in the treatment of the primary cardiac condition)
In addition, hypothermia is inappropriate in patients with a valid do not resuscitate order (DNR).
Cooling methods
Cooling methods include the following:
- Surface cooling with ice packs
- Surface cooling with blankets or surface heat-exchange device and ice
- Surface cooling helmet
- Internal cooling methods using catheter-based technologies
- Internal cooling methods using infusion of cold fluids
Treatment protocols
The goals of treatment include achieving the target temperature as quickly as possible; in most cases, this can be reached within 3-4 hours of initiating cooling. Three phases of therapeutic hypothermia include induction, maintenance, and rewarming. Rewarming can be begun 24 hours after the time of initiation of cooling, with avoidance of hyperthermia 18.
External cooling with cooling blankets or surface heat-exchange device and ice.
Before initiating cooling, confirm eligibility and gather materials.
- Obtain 2 cooling blankets and cables (one machine) to “sandwich” the patient; each blanket should have a sheet covering it to protect the patient’s skin
- Alternatively, place heat-exchange pads on the patient per the manufacturer’s recommendation
- Pack the patient in ice (groin, chest, axillae, and sides of neck); use additional measures as needed to bring the patient to a temperature between 32°C and 36°C; avoid packing ice on top of the chest, which may impair chest wall motion
- Monitor vital signs and oxygen saturation and place the patient on a continuous cardiac monitor, with particular attention to arrhythmia detection and hypotension
- Once a temperature below the goal temperature is reached, remove ice bags and use the cooling blanket or heat-exchange device to maintain temperature between 32°C and 36°C 18
Supportive therapy
- A mean arterial pressure (MAP) goal of more than 80 mm Hg is preferred; hypertension is potentially additive to the neuroprotection of hypothermia
- Norepinephrine can be used, starting at 0.01 mcg/kg/min and titrated to a MAP above 80 mm Hg
- Practice standard neuroprotective strategies such as placing the head of the bed at 30° 19
- Obtain a 12-lead electrocardiogram (ECG) after ROSC to evaluate for the presence of ST-elevation 18
- Monitor for dysrhythmia (most commonly bradycardia) associated with hypothermia
- If life-threatening dysrhythmia arises and persists, or hemodynamic instability or bleeding develops, discontinue active cooling and rewarm the patient
- During cooling, an ECG Osbourne or camel wave may be present; heart rate less than 40 bpm is common and is not a cause for concern in the absence of other evidence of hemodynamic instability
- Check skin every 2-6 hours for thermal injury caused by cold blankets
- Regularly check the patient’s temperature with a secondary temperature monitoring device when cooling
- After therapeutic hypothermia, fever should be avoided
- Maintain oxygen saturation above 94%
- Do not provide nutrition to the patient during the initiation, maintenance, or rewarming phases of the therapy
Controlled rewarming
- Begin rewarming of the patient 24 hours after the initiation of cooling.
- Rewarm slowly at a rate of 0.3-0.5°C every hour
- Rewarming will take approximately 8-12 hours
- Remove cooling blankets (and ice if still in use)
- One method is to set the water temperature in the cooling device to 35°C and then increase the water temperature by 0.5°C every 1-2 hours until a stable core body temperature of 36°C has been reached for 1 hour
- Maintain the paralytic agent and sedation until the patient’s temperature reaches 36°C; if infusing, discontinue the paralytic agent first; the sedation may be discontinued at the practitioner’s discretion
- Monitor the patient for hypotension secondary to vasodilation related to rewarming
- Discontinue potassium infusions
- Avoid hyperthermia
- Centers for Disease Control and Prevention. Number of Hypothermia-Related Deaths, by Sex – National Vital Statistics System, United States, 1999–2011. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6151a6.htm[↩]
- Becker LB, Smith DW, Rhodes KV. Incidence of cardiac arrest: a neglected factor in evaluating survival rates. Ann Emerg Med. 1993 Jan. 22 (1):86-91.[↩]
- Reducing Fire Hazards for Portable Electric Heaters. https://www.cpsc.gov/s3fs-public/heaters.pdf[↩]
- Cobb LA. Variability in resuscitation rates for out-of-hospital cardiac arrest. Arch Intern Med. 1993 May 24. 153 (10):1165-6.[↩]
- Seupaul RA, Wilbur LG. Evidence-based emergency medicine. Does therapeutic hypothermia benefit survivors of cardiac arrest?. Ann Emerg Med. 2011 Sep. 58 (3):282-3.[↩]
- Williams SE, Sabir I, Nimmo C, et al. Quantitative assessment of the effects of therapeutic hypothermia on early repolarization in idiopathic ventricular fibrillation survivors: a 7-year cohort study. Circ Arrhythm Electrophysiol. 2014 Feb. 7 (1):120-6.[↩][↩]
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002 Feb 21. 346 (8):549-56.[↩]
- Wright WL, Geocadin RG. Postresuscitative intensive care: neuroprotective strategies after cardiac arrest. Semin Neurol. 2006 Sep. 26(4):396-402.[↩]
- Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002 Feb 21. 346 (8):557-63.[↩]
- Kragholm K, Skovmoeller M, Christensen AL, et al. Employment status 1 year after out-of-hospital cardiac arrest in comatose patients treated with therapeutic hypothermia. Acta Anaesthesiol Scand. 2013 Aug. 57 (7):936-43.[↩]
- [Guideline] Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015 Nov 3. 132(18 suppl 2):S465-82.[↩]
- Abella BS, Rhee JW, Huang KN, Vanden Hoek TL, Becker LB. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation. 2005 Feb. 64 (2):181-6. [↩]
- Merchant RM, Soar J, Skrifvars MB, et al. Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit Care Med. 2006 Jul. 34 (7):1935-40. [↩]
- Cooper WA, Duarte IG, Thourani VH, et al. Hypothermic circulatory arrest causes multisystem vascular endothelial dysfunction and apoptosis. Ann Thorac Surg. 2000 Mar. 69 (3):696-702; discussion 703.[↩]
- Hammer MD, Krieger DW. Hypothermia for acute ischemic stroke: not just another neuroprotectant. Neurologist. 2003 Nov. 9 (6):280-9.[↩]
- Den Hertog HM, van der Worp HB, Tseng MC, Dippel DW. Cooling therapy for acute stroke. Cochrane Database Syst Rev. 2009 Jan 21. CD001247.[↩]
- Hypothermia Protocols. http://www.med.upenn.edu/resuscitation/docs/protocols/wentworthdouglassthprotocol.pdf[↩]
- [Guideline] Callaway CW, Donnino MW, Fink EL, et al. Part 8: Post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015 Nov 3. 132(18 suppl 2):S465-82[↩][↩][↩][↩]
- Rajek A, Greif R, Sessler DI, Baumgardner J, Laciny S, Bastanmehr H. Core cooling by central venous infusion of ice-cold (4 degrees C and 20 degrees C) fluid: isolation of core and peripheral thermal compartments. Anesthesiology. 2000 Sep. 93 (3):629-37.[↩]