Contents
Iliocostal friction syndrome
Iliocostal friction syndrome also called costoiliac impingement syndrome, iliocostal impingement syndrome or rib-tip syndrome, is a rare, painful, and disabling condition in which the lowermost ribs margin comes in contact with the iliac crest as a result of a reduced costoiliac distance due to thoracic hyperkyphosis, thoracolumbar scoliosis or lumbar vertebral compression fractures that occurs with severe spinal osteoporosis, trauma, stroke or congenital deformities 1, 2, 3, 4, 5. Iliocostal friction syndrome presents as low back pain which may radiate to other surrounding areas as a result of irritated nerve, tendon, and muscle structures. Iliocostal friction syndrome may occur unilaterally due to conditions such as scoliosis, or bilaterally due to conditions such as osteoporosis and hyperkyphosis.
Diagnosis and treatment of iliocostal friction syndrome can be challenging for various reasons. The differential diagnosis of nonspecific low back and flank pain is extensive, including intrathoracic, intra-abdominal, neurologic, and musculoskeletal causes.
Iliocostal friction syndrome diagnosis is predominately clinical with tenderness to palpation of the iliac crests which are extremely tender and in contact with lower ribs 4. If the ribs arc moved away from the iliac crest by compression of the lower chest margin, pain is immediately relieved 4. If iliocostal friction syndrome is suspected following this simple examination, the doctor will usually order X-rays of the entire spine from the neck to the pelvis (back and side views). Thoracic hyperkyphosis and thoracic spine radiographs showing contact of the lowermost ribs on the ilium can aid in the diagnosis of iliocostal friction syndrome.
There is little published literature regarding management of iliocostal friction syndrome 2. Treatment of iliocostal friction syndrome is typically by addressing the underlying cause, commonly with the use of elastic belt to compress the lower chest and infiltration of the iliac crest with sclerosant solution 4. However surgical resection may be necessary if medical treatment fails to provide relief.
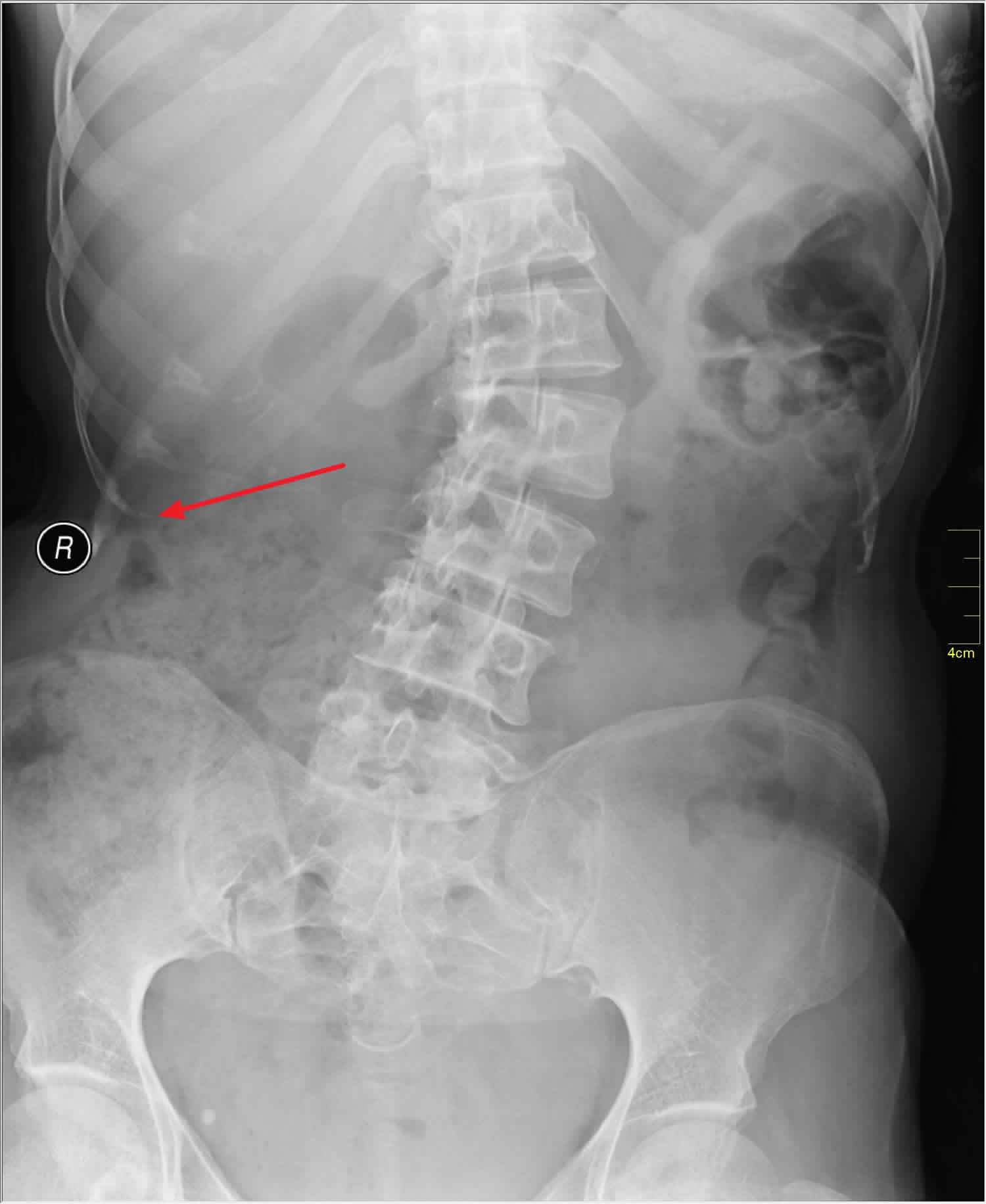
Figure 1. Iliocostal friction syndrome
Footnotes: Full spine anterior-posterior (A) view shows severe angular thoracic kyphosis, with apex at T10 resulting extension of rib cage into pelvis (left arrow, rib; right arrow, iliac crest). Lateral view (B) shows severely diminished distance between the lower edge of the rib cage (upper arrows) and iliac crest (lower arrows).
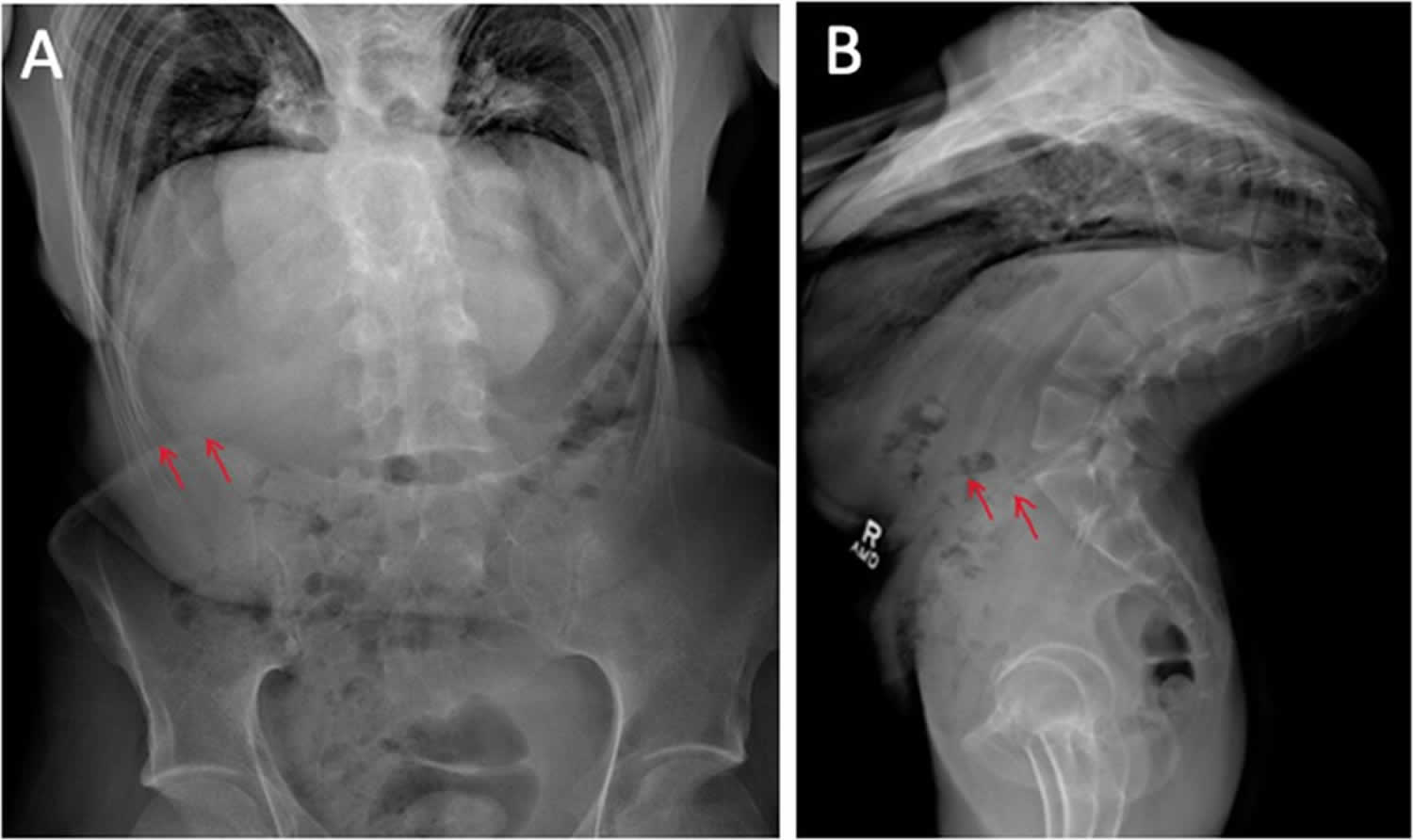
[Source 1 ]Figure 2. Scoliosis
Footnote: Instead of a straight line down the back, a spine with scoliosis curves from side-to-side. (Left) Normal spine anatomy. (Right) Scoliosis can make the spine look more like the letters “C” or “S”. Neuromuscular scoliosis curves are typically long and involve the entire spine.
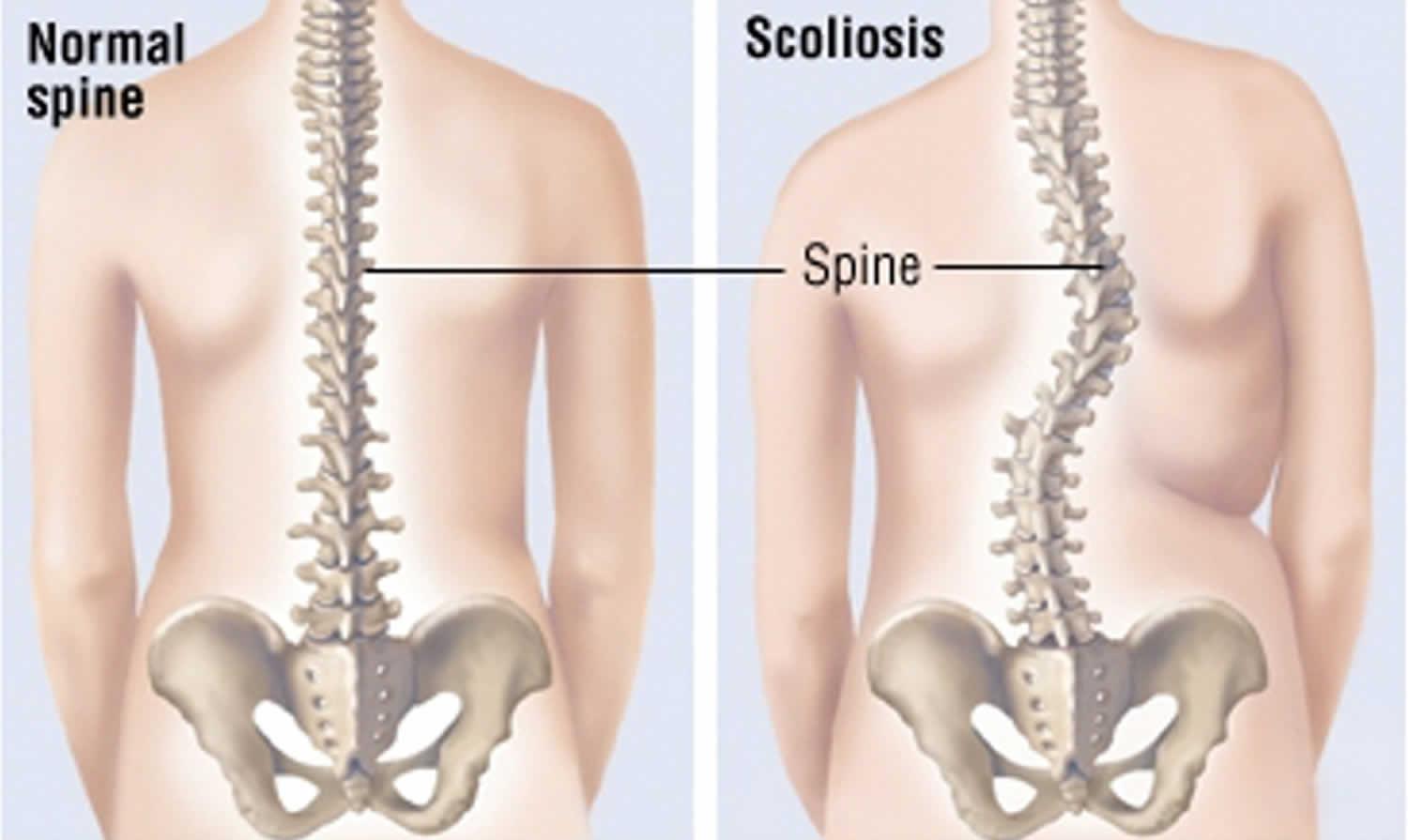
Figure 3. Kyphosis
Footnotes: 27-year-old male, who presented with a 4-month history of chronic right-sided flank and back pain (5.5 in a “0 to 10” Numerical Rating Scale). (A) Patient with severe kyphosis. Photograph shows triangular upper back protuberance of a patient with severe kyphosis. (B) CT scan revealed severe hair-pin shaped kyphotic deformity (165°); the apex of T7–T12 are fused together into one vertebral body. Spinal cord is draped over this hairpin turn without spinal canal narrowing.
[Source 1 ]Iliocostal friction syndrome cause
Iliocostal friction syndrome is caused by your 10th, 11th, or 12th rib coming in contact with the iliac crest 4. Typically, individuals with iliocostal friction syndrome will have an underlying condition such as scoliosis or osteoporosis 6.
There are several nerve branches surrounding the iliac crest that may be impinged or irritated upon contact. The superior cluneal nerves travel through the thoracolumbar fascia and drape over the iliac crest 7. The posterior branches of the iliohypogastric nerve can emerge on the surface above the iliac crest, with the nerve draping lower than usual in some individuals 6. Similarly, the ilioinguinal nerve runs below the iliohypogastric nerve, following just above the iliac crest 8. These nerves may be impinged or irritated as a result of the lower ribs coming in contact with the iliac crest 7.
The top of the iliac crest includes the attachments of the latissimus dorsi, the transversus abdominis, as well as the internal and external obliques. The quadratus lumborum also connects from the back tip of the iliac crest up to the 12th rib 9. These tendon and muscle structures surrounding the iliac crest are at risk for irritation due to iliocostal contact. Tendon irritation can result in referred pain, therefore affected individuals may experience pain throughout the hip, low back, the groin, chest, and thigh. This contributes towards the difficulty in diagnosis of iliocostal friction syndrome 4.
Unilateral causes
Scoliosis is a side-to-side curve of your spine (backbone or vertebrae [the bones that make up your spine]). This differs from your body’s natural front-to-back curve. Your spine naturally has a slight forward and backward curve. With scoliosis, your spine curves to the left and right into a C or S shape.
Scoliosis has been known to cause unilateral iliocostal friction syndrome 7. Scoliosis is a condition in which the lateral curvature of the spine is measured to be more than 10 degrees. Scoliosis is typically categorized into congenital, neuromuscular, idiopathic (which means that the exact cause is not known and is the most common cause of scoliosis causes [80 to 85% of scoliosis cases]), degenerative, and pathologic scoliosis 10.
- Idiopathic scoliosis. The term idiopathic means unknown cause. Idiopathic scoliosis is the most common type. Although scientists do not know for sure what causes the majority of scoliosis cases (80 to 85%), they do know that it tends to run in families and has a genetic (hereditary) link. Idiopathic scoliosis can occur in toddlers and young children, but the majority of cases occur from age 10 to the time a child is fully grown.
- Idiopathic scoliosis is grouped by age:
- In children age 3 and younger, it is called infantile scoliosis.
- In children age 4 through 10, it is called juvenile scoliosis.
- In children age 11 through 18, it is called adolescent scoliosis.
- Risk factors for idiopathic scoliosis:
- Age – Idiopathic scoliosis typically starts between the ages of 9-15 when the body is growing.
- Gender – Girls are at a higher risk of worsening scoliosis and needing treatment for it. However, there is no difference between gender in terms of who gets the disease.
- Family history – Idiopathic scoliosis has been shown to run in families at times. However, majority of children with scoliosis don’t have a family history of the disease.
- Idiopathic scoliosis is grouped by age:
- Congenital scoliosis means that you are born with scoliosis (the sideways curvature of the spine is caused by a defect that was present at birth). Congenital scoliosis occurs in only 1 in 10,000 newborns and is much less common than the idiopathic scoliosis that begins in adolescence. Congenital scoliosis starts as the spine forms before birth. Part of one vertebra (or more) does not form completely or the vertebrae do not separate properly. Some types of congenital scoliosis can change quickly with growth, while others remain unchanged. Congenital scoliosis can be associated with other health issues, such as heart and kidney problems.
- Neuromuscular scoliosis. Any medical condition that affects the nerves and muscles that support the spine can lead to scoliosis. This is most commonly due to muscle imbalance and/or weakness. Common neuromuscular conditions that can lead to scoliosis include cerebral palsy, muscular dystrophy, spina bifida and spinal cord injury.
You may also hear your doctor refer to scoliosis diagnosed during adulthood as adult-onset scoliosis or degenerative scoliosis. You may have had mild, undiagnosed scoliosis throughout your life. Symptoms can increase or appear as your body ages, which results in a late diagnosis. Specifically, adult-onset scoliosis or degenerative scoliosis happens when your disks and joints weaken or you lose bone density (osteoporosis).
In all types of scoliosis, the side-to-side curves of the spine often become larger and more noticeable during periods of rapid growth, such as adolescence. Idiopathic and congenital scoliosis curves typically affect limited sections of the spine and stop progressing when an adolescent is full-grown. On the other hand, in neuromuscular scoliosis the spinal curves often develop at a younger age than idiopathic scoliosis. These curves typically are long and involve the entire spine. In addition, the neuromuscular scoliosis curves progress more rapidly and may continue to worsen even into adulthood.
The decreased distance between the ribcage and the iliac crest can come in contact depending on the severity of the scoliosis curve 6. There has also been reported instances where individuals experience iliocostal friction syndrome due to an abnormally long twelfth rib. This can be presented both bilaterally or unilaterally, depending on the individual 6, 11.
Bilateral causes
Iliocostal friction syndrome most commonly occurs bilaterally as a result of spinal osteoporosis 2. Osteoporosis is a condition in which your bones become weak and are likely to fracture (break). Osteoporosis can develop when your bone mineral density and bone mass decrease. It can also happen if the structure and strength of your bones change. Osteoporosis is called a “silent” disease because it doesn’t usually cause symptoms. You may not even know you have the disease until you break a bone. This could happen with any bone, but it’s most common in the bones of your hip, vertebrae in the spine, and wrist.
Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause, are at highest risk.
Your bones are in a constant state of renewal where new bone is made and old bone is broken down. When you’re young, your body makes new bone faster than it breaks down old bone and your bone mass increases. After the early 20s this process slows, and most people reach their peak bone mass by age 30. As people age, bone mass is lost faster than it’s created. How likely you are to develop osteoporosis depends partly on how much bone mass you attained in your youth.
A number of factors can increase the likelihood that you’ll develop osteoporosis — including your age, race, lifestyle choices, and medical conditions and treatments.
Risk factors for osteoporosis:
- Your sex. Women are much more likely to develop osteoporosis than are men.
- Age. The older you get, the greater your risk of osteoporosis.
- Race. You’re at greatest risk of osteoporosis if you’re white or of Asian descent.
- Family history. Having a parent or sibling with osteoporosis puts you at greater risk, especially if your mother or father fractured a hip.
- Body frame size. Men and women who have small body frames tend to have a higher risk because they might have less bone mass to draw from as they age.
- Low calcium intake. A lifelong lack of calcium plays a role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss and an increased risk of fractures.
- Eating disorders. Severely restricting food intake and being underweight weakens bone in both men and women.
- Lifestyle factors. Some bad habits can increase your risk of osteoporosis. Examples include:
- Sedentary lifestyle. People who spend a lot of time sitting have a higher risk of osteoporosis than do those who are more active. Any weight-bearing exercise and activities that promote balance and good posture are good for your bones, but walking, running, jumping, dancing and weightlifting seem particularly helpful.
- Excessive alcohol consumption. Regular consumption of more than two alcoholic drinks a day increases the risk of osteoporosis.
- Tobacco use. The exact role tobacco plays in osteoporosis isn’t clear, but it has been shown that tobacco use contributes to weak bones.
- Gastrointestinal surgery. Surgery to reduce the size of your stomach or to remove part of the intestine limits the amount of surface area available to absorb nutrients, including calcium. These surgeries include those to help you lose weight and for other gastrointestinal disorders.
- Steroids and other medicines. Long-term use of oral or injected corticosteroid medicines, such as prednisone and cortisone, interferes with the bone-rebuilding process. Osteoporosis has also been associated with medications used to treat or prevent:
- Seizures.
- Gastric reflux.
- Cancer.
- Transplant rejection.
- Sex hormones. Lowered sex hormone levels tend to weaken bone. The fall in estrogen levels in women at menopause is one of the strongest risk factors for developing osteoporosis. Treatments for prostate cancer that reduce testosterone levels in men and treatments for breast cancer that reduce estrogen levels in women are likely to accelerate bone loss.
- Thyroid problems. Too much thyroid hormone can cause bone loss. This can occur if your thyroid is overactive or if you take too much thyroid hormone medicine to treat an underactive thyroid.
- Osteoporosis has also been associated with overactive parathyroid and adrenal glands.
- Medical problems. The risk of osteoporosis is higher in people who have certain medical problems, including:
- Celiac disease.
- Inflammatory bowel disease (IBD).
- Kidney or liver disease.
- Cancer.
- Multiple myeloma.
- Rheumatoid arthritis.
The most common fractures that occur due to osteoporosis is in the hip or vertebrae 12, resulting in a loss of space between the ribs and the iliac crest. Osteoporosis affects more women than men. Of the estimated 10 million Americans with osteoporosis, more than 8 million (or 80%) are women 13. More than 2 million fractures occur annually in the United States due to osteoporosis 14.
Women are more likely to get osteoporosis because 15, 16:
- Women usually have smaller, thinner, less dense bones than men.
- Women often live longer than men. Bone loss happens naturally as we age.
- Women also lose more bone mass after menopause with very low levels of the hormone estrogen. Higher estrogen levels before menopause helps protect bone density.
Osteoporosis is most common in older women. In the United States, osteoporosis affects 25% of women 65 or older 17. But younger women can get osteoporosis. And girls and women of all ages need to take steps to protect their bones.
Another cause for iliocostal friction syndrome is kyphosis of the spine. Kyphosis is the abnormal curvature of the spine, from front to back. Kyphosis causes your upper back around the thoracic region (the part of your spine between your neck and ribs) to bend forward. The curvature can make it look like you’re hunched over or slouching. People sometimes call it “hunchback” or “roundback” 18. The thoracic spine is slightly curved due to the shape of the vertebral bodies and intervertebral discs, with a normal Cobb angle measurement between 20 and 40 degrees. In younger adults, the “normal” range falls between 20 and 40° of curvature using the Cobb angle measurement of kyphosis. After the fourth decade of life, the kyphosis angle begins to worsen and increase above 40°, leading to an excessive kyphosis curvature, known as “age-related hyperkyphosis” 19. Hyperkyphosis is a condition in which the curve of the kyphosis angle measures over 50 degrees. The kyphosis angle can be influenced by age, muscle tone, vertebral fractures, and intervertebral degenerative disc disease 18, 20. The curvature of hyperkyphosis may result in a decrease of space between the ribs and the iliac crest, causing iliocostal friction syndrome.
There are several types of kyphosis. Some of the most common include 21:
- Hyperkyphosis (severe kyphosis): Hyperkyphosis is a severe forward curvature of the spine. The curve measures more than 50 degrees. This type is common after age 40. Hyperkyphosis (severe kyphosis) affects an estimated 20% to 40% of adults over age 60. On average, the forward angle of your upper spine increases about 3 degrees each decade (10 years).
- Postural kyphosis: This is the most common type of kyphosis. It usually happens during your teenage years. Slouching or poor posture stretches the ligaments and muscles holding your vertebrae (spinal bones) in place. Stretching pulls your vertebrae out of their normal position, causing a rounded shape in your spine. It affects more children assigned female at birth than children assigned male at birth. It doesn’t usually cause pain.
- Scheuermann’s kyphosis (Juvenile kyphosis): Scheuermann’s kyphosis happens when vertebrae have a different shape than expected. Instead of being rectangular, your vertebrae have a wedge shape. The wedge-shaped bones curve forward, making your spine look rounded. The cause and pathogenesis of Scheuermann’s kyphosis are not exactly
known. Scheuermann kyphosis was reported to be caused by the disturbances in the vertebral epiphyseal growth 22. A mosaic structure in the endplate of the vertebrae and growth cartilage was mentioned 23. It occurs more often in boys than in girls by 2/1-7/1. In general, Scheuermann’s kyphosis occurs predominantly in children between 13 and 16 years of age. Patients are usually taller than their peers. Its incidence in the USA is 0.4% to 8%. Scheuermann’s kyphosis can be painful, especially during activity or when standing or sitting for a long time. Changing your position or posture doesn’t change the curve, as your vertebrae aren’t flexible. - Congenital kyphosis: Congenital means a condition present at birth. Congenital kyphosis occurs when your spine doesn’t properly develop or develop completely in the uterus. It can increase in severity as you grow. Surgery can correct the spine curvature during childhood to prevent it from worsening. It can happen in addition to other congenital growth defects like those that affect your heart and kidneys.
- Cervical kyphosis (military neck): This type occurs when your cervical spine, or the part of your spine at the bottom of your head to your upper back), curves toward your front instead of its natural curve to your back.
Hyperkyphosis can also result from tumors, trauma, neuro-muscular disease, postlaminectomy syndrome, dwarfism, and spinal tuberculosis also known as Pott’s disease 21.
Iliocostal friction syndrome signs and symptoms
Iliocostal friction syndrome main symptom is low back pain, which may radiate to the lower rib cage, flank, groin, buttock, and thigh 2. Iliocostal friction syndrome other symptom may include experience intermittent aches along with a ‘grating sensation’ in the hip 11. The pain may be aggravated by moving, twisting, bending, or by changing positions 4. Iliocostal friction syndrome may be bilateral as seen in individuals with hyperkyphosis or osteoporosis, but is more commonly unilateral as seen in individuals with scoliosis 7.
There typically are no symptoms in the early stages of bone loss (osteopenia). But once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a broken or collapsed bone in the spine.
- Loss of height over time.
- A stooped posture.
- A bone that breaks much more easily than expected.
Iliocostal friction syndrome diagnosis
Your doctor will perform a physical exam. Your doctor will observe you in different positions (standing, bending over, walking) and from many perspectives. You will be asked to bend forward. This makes your spine easier to see. Iliocostal friction syndrome diagnosis is predominately clinical with tenderness to palpation of the iliac crests which are extremely tender and in contact with lower ribs 4. If the ribs arc moved away from the iliac crest by compression of the lower chest margin, pain is immediately relieved 4. If iliocostal friction syndrome is suspected following this simple examination, the doctor will usually order X-rays of the entire spine from the neck to the pelvis (back and side views). Thoracic hyperkyphosis and thoracic spine radiographs showing contact of the lowermost ribs on the ilium can aid in the diagnosis of iliocostal friction syndrome.
Other tests will vary depending on your condition. These may include:
- Spinal curve measurement (scoliometer screening). Your doctor will use a device called a scoliometer to measure the spine curve by placing the tool on your back. This is similar to how you measure angles with a protractor in geometry class. Your X-rays will be evaluated and any curves in your spine will be measured in degrees using the Cobb method.
- No scoliosis diagnosis: Less than 10 degrees.
- A curve greater than 10º is considered scoliosis.
- Mild scoliosis: Between 10 to 24 degrees.
- Moderate scoliosis: Between 25 to 39 degrees.
- Severe scoliosis: More than 40 degrees.
- X-rays of the spine to see how flexible the curvature is
- Lung function test – a pulmonary function test to measure how well your lungs are working.
- CT scan of the spine to look at the bony changes
- Magnetic resonance imaging (MRI) scans. An MRI scan provides clear images of soft tissues and helps your child’s doctor evaluate the health of the spinal cord.
Iliocostal friction syndrome differential diagnosis
Iliocostal friction syndrome differential diagnosis can be extensive due to the presentation of the condition. Since iliocostal friction syndrome can present as pain in many areas surrounding the back, flank, and abdomen, the differential diagnosis for the condition can be extensive. Some of the diagnosis include but not limited to neuropathic pain of the intercostal nerves, conditions of the hip, pinched nerves within the spine, myofascial pain, and visceral causes 5. Iliocostal friction syndrome differential diagnosis may also include an investigation into the pathology which caused the iliocostal contact if it is not previously known, such as undiagnosed scoliosis, back strain, osteoporosis, or a compression fracture 4.
Iliocostal friction syndrome should also be differentiated from other conditions affecting the lower ribs such as slipping rib syndrome, which is a condition that involves the increased mobility of the 8th to 10th ribs at their interchondral joints. Additionally, hypermobile 11th and 12th ribs may cause twelfth rib syndrome due to the floating ribs impinging on the intercostal nerves (intercostal neuralgia). Neither of these conditions involve the iliac crest 11.
Iliocostal friction syndrome treatment
Treatment will depend on the cause of your iliocostal friction syndrome. To date, treatment of iliocostal friction syndrome has included rib-compression belts, injections, and surgical resection of the lowermost ribs 2. For most people with iliocostal friction syndrome, the most conservative and mechanically based treatment includes the use of a 3-inch wide lower rib-compression belt 2. This is fitted directly above the iliac crests and adjusted tightly to provide adequate pressure on the lower ribs, shifting them away from the iliac crests. Another approach using the weighted kypho-orthosis in combination with the home back strengthening exercise program that targets the underlying treatable causes of poor posture 2.
Injections have also been used under the assumption that the inserting tendons on the iliac crests or ribs are the primary pain generators. Hypertonic dextrose and lidocaine are injected at the osseotendinous junctions near the iliac crest and lower rib margins 24.
You may need surgery if the spine curve is severe or getting worse very quickly. The most invasive procedure is surgical resection of the 11th or 12th rib 25, 11, 24. The most common indications for surgery include:
- Curves greater than 50 degrees (in patients who are still growing)
- Curves greater than 50 degrees that have progressed more than 10 degrees (in patients who have reached skeletal maturity)
- Difficulty sitting and functional deterioration
- Pain
- Problems with heart or lung function.
Hirschberg et al. 24 evaluated the pain-relieving effects of the rib-compression belt and injections in 19 patients with iliocostal impingement syndrome. After compression belt use for 3–6 weeks, 6 of 19 patients (32%) reported adequate pain relief. The remaining 13 patients underwent injection, resulting in pain relief for all but two patients over an unknown period. Of the two patients without relief following injection, one reported ongoing pain relief with use of the compression belt and one did not experience pain relief with either of the measures.
Wynne et al. 11 described six patients with iliocostal friction syndrome who underwent surgical resection of the outermost two-thirds of the 12th rib. All patients had pain relief without recurrence at 5 to 34 month follow-up. Although these methods have been shown to provide pain relief, none have consistent long-term follow-up or aim to correct the underlying cause of poor posture, and reduced back strength.
- Ratan K Banik, Eric McDaniel, Jacob C DeWeerth, Jonathan N Sembrano, Iliocostal Friction Syndrome Due to Hair-Pin Shaped Thoracic Kyphosis, Pain Medicine, Volume 22, Issue 5, May 2021, Pages 1223–1224, https://doi.org/10.1093/pm/pnab027[↩][↩][↩]
- Brubaker ML, Sinaki M. Successful management of iliocostal impingement syndrome: A case series. Prosthet Orthot Int. 2016 Jun;40(3):384-7. https://journals.sagepub.com/doi/pdf/10.1177/0309364615605394[↩][↩][↩][↩][↩][↩][↩]
- Wynne AT, Nelson MA, Nordin BEC (1985) Costo-iliac impingement syndrome J of Bone & Joint Surg 67B:1 124-125[↩]
- Hirschberg, G. G., Williams, K. A., & Byrd, J. G. (1992). Diagnosis and Treatment of Iliocostal Friction Syndromes. Journal of Orthopaedic Medicine, 14(2), 35–39. https://doi.org/10.1080/1355297X.1992.11719682[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Patel SI, Jayaram P, Portugal S, Stitik TP. Iliocostal friction syndrome causing flank pain in a patient with a history of stroke with scoliosis and compensated Trendelenburg gait. Am J Phys Med Rehabil. 2014 Jul;93(7):632-3. doi: 10.1097/PHM.0b013e318282e939[↩][↩]
- Huber, P., Arroyo, J. Syndrome algique ilio-costal. Doul. et Analg. 8, 25–27 (1995). https://doi.org/10.1007/BF03005024[↩][↩][↩][↩]
- Superior Cluneal Neuralgia from Iliocostal Impingement Treated with Phenol Neurolysis: A Case Report. Pain Management Case Reports. 4 (3): 77–84. https://painmedicine-casereports.com/current/pdf?article=NDE0&journal=21[↩][↩][↩][↩]
- Elsakka KM, Das JM, Leslie SW, et al. Ilioinguinal Neuralgia. [Updated 2024 Feb 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538256[↩]
- Myers TW (2020). Anatomy Trains E-Book: Myofascial Meridians for Manual Therapists and Movement Professionals. United Kingdom: Elsevier Health Sciences. pp. 79, 85. ISBN 9780702078149[↩]
- Blevins K, Battenberg A, Beck A. Management of Scoliosis. Adv Pediatr. 2018 Aug;65(1):249-266. doi: 10.1016/j.yapd.2018.04.013[↩]
- Wynne AT, Nelson MA, Nordin BE. Costo-iliac impingement syndrome. J Bone Joint Surg Br. 1985 Jan;67(1):124-5. doi: 10.1302/0301-620X.67B1.3155743[↩][↩][↩][↩][↩]
- Ensrud KE, Crandall CJ. Osteoporosis. Ann Intern Med. 2017 Aug 1;167(3):ITC17-ITC32. doi: 10.7326/AITC201708010. Erratum in: Ann Intern Med. 2017 Oct 3;167(7):528. doi: 10.7326/L17-0539[↩]
- Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014 Nov;29(11):2520-6. doi: 10.1002/jbmr.2269[↩]
- Anthamatten A, Parish A. Clinical Update on Osteoporosis. J Midwifery Womens Health. 2019 May;64(3):265-275. doi: 10.1111/jmwh.12954[↩]
- Cawthon PM. Gender differences in osteoporosis and fractures. Clin Orthop Relat Res. 2011 Jul;469(7):1900-5. doi: 10.1007/s11999-011-1780-7[↩]
- Schutte, H.E. (1995). Social and economic impact of osteoporosis. European Journal of Radiology; 20(3): 165-169. https://doi.org/10.1016/0720-048X(95)00628-4[↩]
- Looker, A.C., Frenk, S.M. (2015). Percentage of Adults Aged 65 and Over with Osteoporosis or Low Bone Mass at the Femur Neck or Lumbar Spine: United States, 2005-2010. https://www.cdc.gov/nchs/data/hestat/osteoporsis/osteoporosis2005_2010.htm[↩]
- Roghani T, Zavieh MK, Manshadi FD, King N, Katzman W. Age-related hyperkyphosis: update of its potential causes and clinical impacts-narrative review. Aging Clin Exp Res. 2017 Aug;29(4):567-577. doi: 10.1007/s40520-016-0617-3[↩][↩]
- Fon GT, Pitt MJ, Thies AC Jr. Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol. 1980 May;134(5):979-83. doi: 10.2214/ajr.134.5.979[↩]
- Koelé MC, Lems WF, Willems HC. The Clinical Relevance of Hyperkyphosis: A Narrative Review. Front Endocrinol (Lausanne). 2020 Jan 24;11:5. doi: 10.3389/fendo.2020.00005[↩]
- Yaman O, Dalbayrak S. Kyphosis and review of the literature. Turk Neurosurg. 2014;24(4):455-65. https://www.turkishneurosurgery.org.tr/pdf/pdf_JTN_1354.pdf[↩][↩]
- Scheuermann HW: Kyphosis dorsalis juvenilis. Ugeskr Laeger 82:385–393, 1920[↩]
- Edgren W, Vainio S. Osteochondrosis juvenilis lumbalis. Acta Chir Scand Suppl. 1957;227:1-47.[↩]
- Hirschberg GG, Williams KA, Byrd JG. Medical management of iliocostal pain. Geriatrics. 1992 Sep;47(9):62-3, 66-7.[↩][↩][↩]
- Fakundiny B, Kehrer KS, Popov A, Busk H, Walles T. Osteo-cartilaginous pain syndromes at the chest wall: results of costal cartilage excision. J Thorac Dis. 2023 Jun 30;15(6):3158-3165. doi: 10.21037/jtd-22-1479[↩]