Contents
What is intussusception
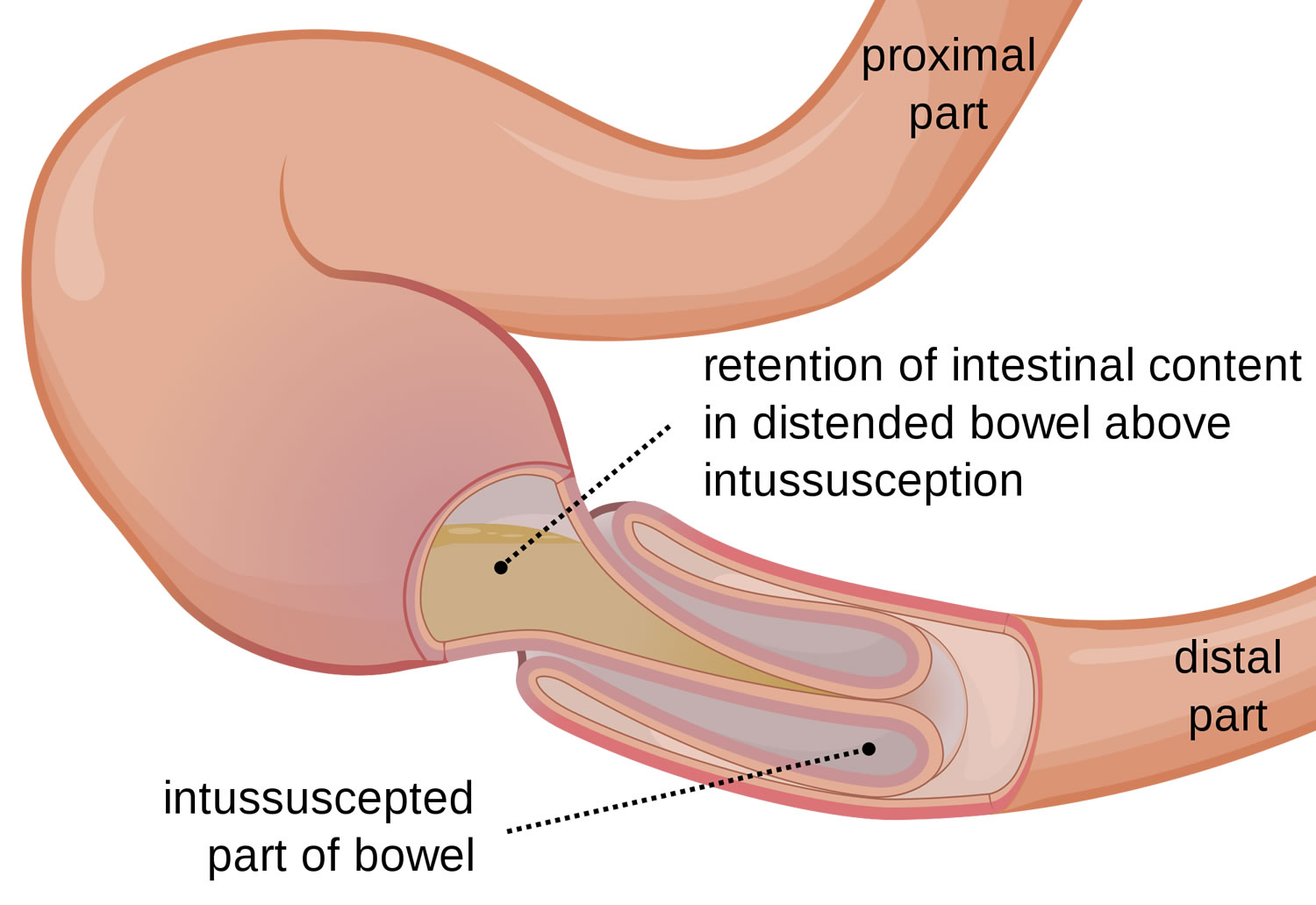
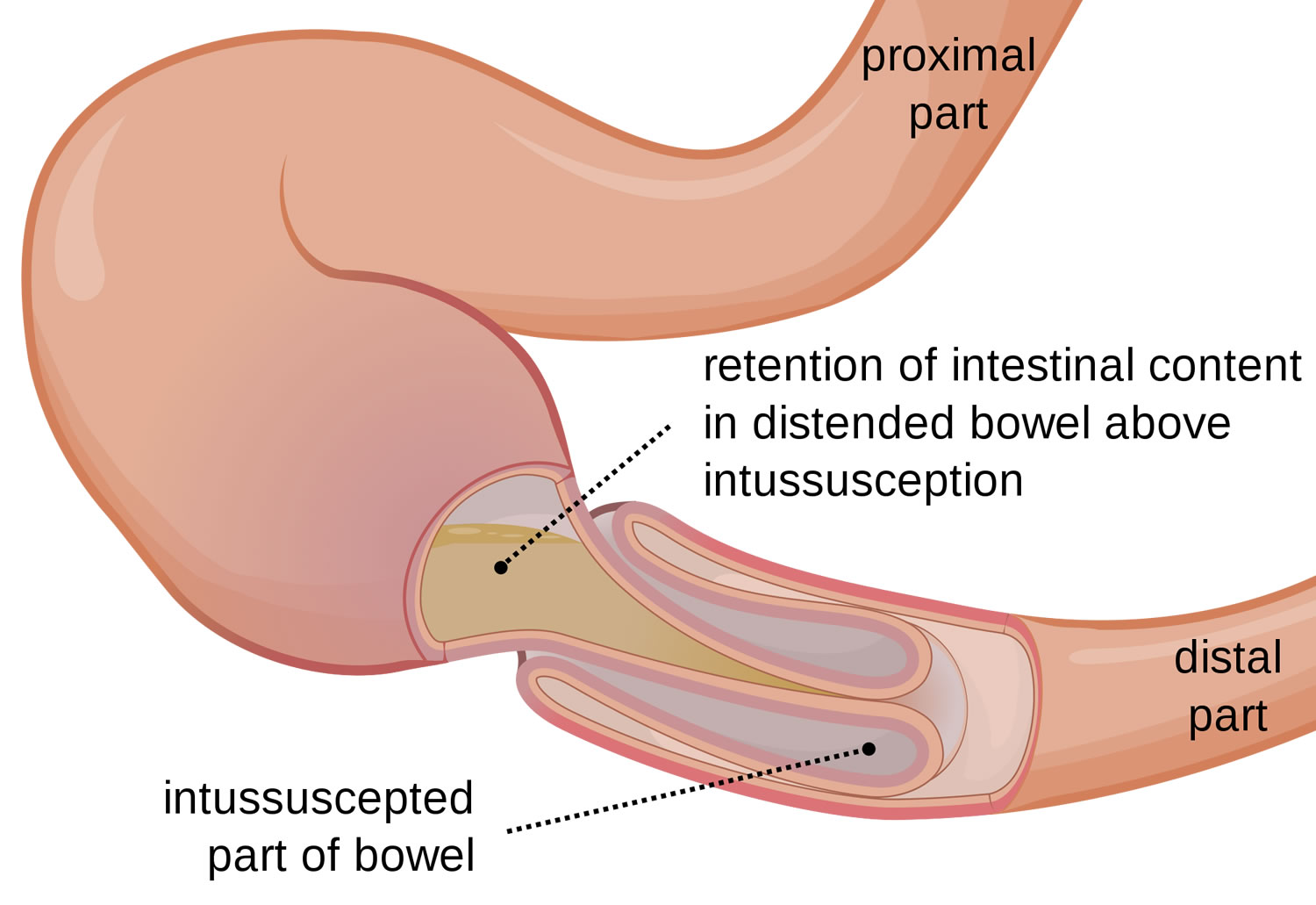
Intussusception is a medical emergency in which part of the intestine slides into an adjacent part of the intestine. This “telescoping” often blocks food or fluid from passing through. Intussusception also cuts off the blood supply to the part of the intestine that’s affected, which can lead to a tear in the bowel (perforation), infection and death of bowel tissue.
Intussusception is an important cause of an intestinal obstruction in children younger than 3 and merits timely ultrasound examination and reduction to preclude significant sequelae including bowel necrosis. The vast majority of intussusceptions occur in children (95%), usually after the first three months of life 1. The cause of most cases of intussusception in children is unknown.
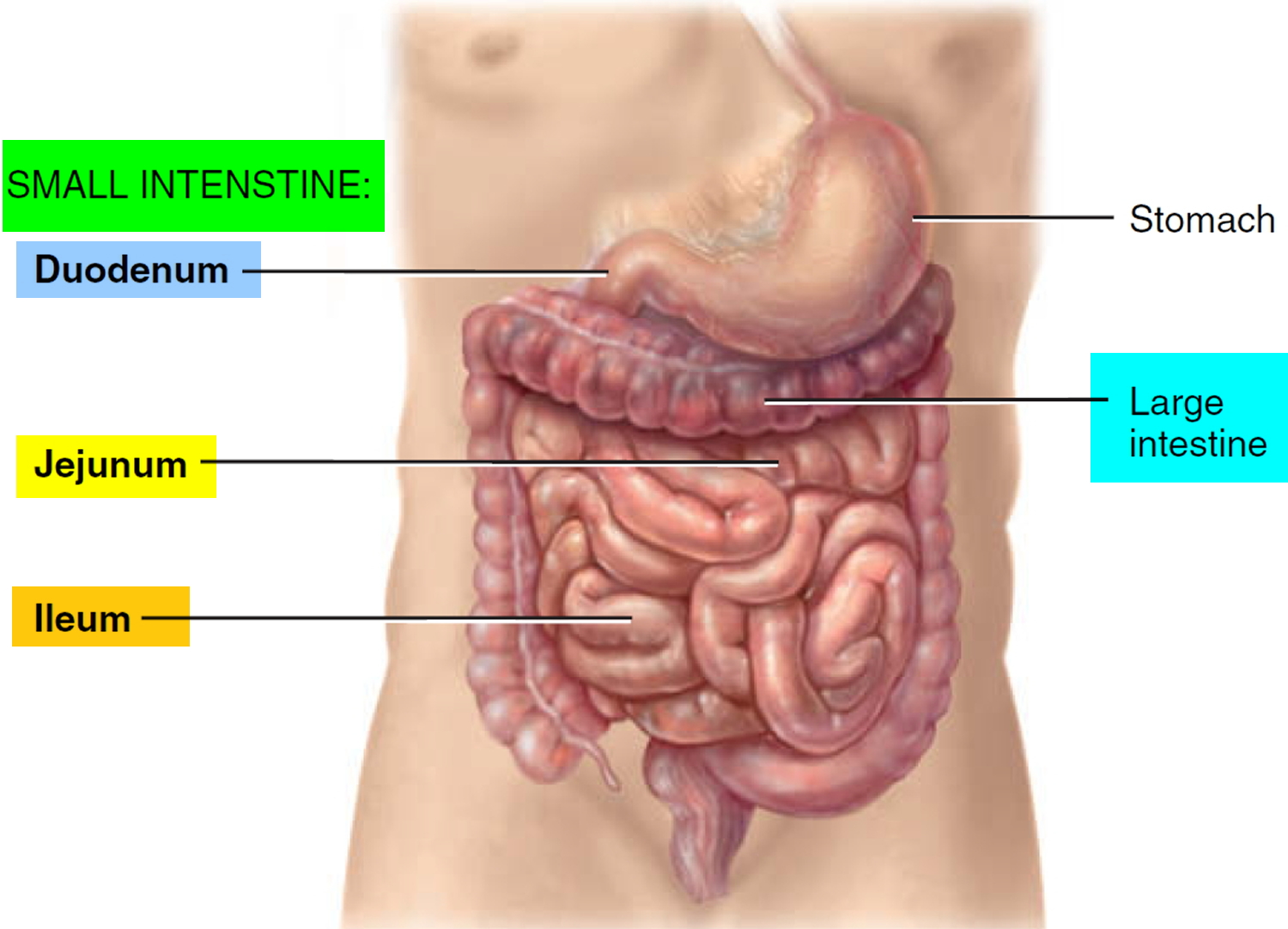
Intussusception can occur essentially anywhere. In adults no pattern of distribution is present as such as in the vast majority of cases a lead point lesion is present, and thus the location will depend on the location of that lesion. In children there is a strong predilection for the ileocolic region:
- ileocolic: most common (75-95%), presumably due to the abundance of lymphoid tissue related to the terminal ileum and the anatomy of the ileocaecal region
- ileoileocolic: second most common
- ileoileal and colocolic: uncommon
- gastric intussusception: rare, but documented 1
Though rare in adults, most cases of adult intussusception are the result of an underlying medical condition, such as a tumor, where it caused a focal lesion acting as a lead point.
In children, the intestines can usually be pushed back into position with an X-ray procedure. In adults, surgery is often required to correct the problem.
Figure 1. Small and large intestines
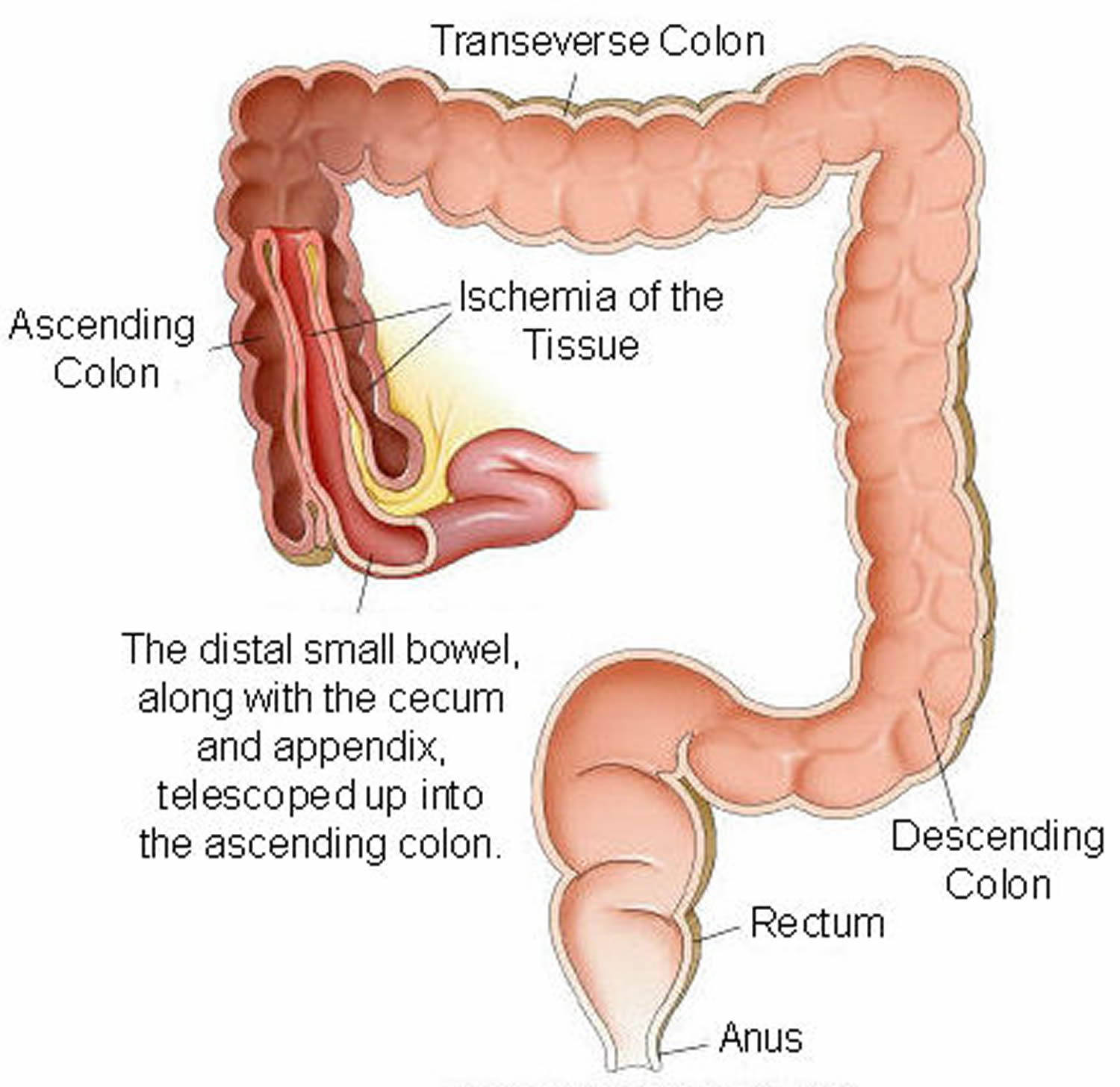
Figure 2. Intussusception
Figure 3. Intussusception of distal small intestine into the cecum (large intestine)
 Intussusception in infants
Intussusception in infants
Intussusception is the most common abdominal emergency affecting children under 2 years old. Intussusception happens when one portion of the bowel slides into the next, much like the pieces of a telescope.
When this “telescoping” happens, the flow of fluids and food through the bowel can become blocked, the intestine can swell and bleed, and the blood supply to the affected part of the intestine can get cut off. Eventually, this can cause part of the bowel to die.
Intussusception happens in 1 to 4 out of every 1,000 infants and is most common in babies 5 to 9 months old, though older children also can have it. Boys get intussusception more often than girls.
Intussusception in infants signs and symptoms
Babies and children with intussusception have intense abdominal pain, which often begins suddenly and causes the child to draw the knees up toward the chest. The pain often makes the child cry very loudly. As it eases, the child may stop crying for a while and may seem to feel better. The pain usually comes and goes like this, but can become very strong when it returns.
The pain of intussusception comes and goes, usually every 15 to 20 minutes at first. These painful episodes last longer and happen more often as time passes.
Symptoms also can include:
- abdominal swelling
- vomiting
- vomiting up bile, a bitter-tasting yellowish-green fluid
- passing stools (poop) mixed with blood and mucus, known as currant jelly stool
- grunting due to pain
- fever
Not everyone has all of the symptoms. Some infants have no obvious pain, and some children don’t pass blood or have a lump in the abdomen. Some older children have pain but no other symptoms.
As the illness continues, the child may gradually become weaker. He or she may develop a fever and appear to go into shock, a life-threatening medical problem in which lack of blood flow to the body’s organs causes the heart to beat quickly and blood pressure to drop.
Some babies with intussusception may just appear drowsy without vomiting, have stool changes, or have abdominal swelling.
Intussusception in infants causes
Most of the time, doctors don’t know what causes intussusception. In some cases, it might follow a recent attack of gastroenteritis (or “stomach flu”). Bacterial or viral gastrointestinal infections may cause swelling of the infection-fighting lymph tissue that lines the intestine, which may result in one part of the intestine being pulled into the other.
In kids younger than 3 months of age or older than 5, intussusception is more likely to be caused by an underlying condition like enlarged lymph nodes, a tumor, or a blood vessel abnormality in the intestines.
Intussusception in infants diagnosis and treatment
Doctors usually check for intussusception if a child is having repeat episodes of pain, drawing up the legs, vomiting, feeling drowsy, or passing stools with blood and mucous.
During the visit, the doctor will ask about the child’s overall health, family health, any medications the child is taking, and any allergies the child may have. Next, the doctor will examine the child, paying special attention to the abdomen, which may be swollen or tender to the touch. Sometimes the doctor can feel the part of the intestine that’s involved.
If the doctor suspects intussusception, the child may be sent to an emergency room (ER). Usually, doctors there will ask a pediatric surgeon to see the child right away. The ER doctor might order an abdominal ultrasound or X-ray, which can sometimes show a blockage in the intestines. If the child looks very sick, suggesting damage to the intestine, the surgeon may take the child to the operating room right away to correct the bowel obstruction.
Two kinds of enemas (an air enema or a barium enema) often can diagnose and treat intussusception at the same time.
For an air enema, a small soft tube is placed in the rectum and air is passed through the tube. The air travels into the intestines and outlines the bowels on the X-rays. If intussusception is present it shows the doctors the telescoping piece in the intestine. At the same time, the pressure of the air unfolds the bowel that has been turned inside out and cures the blockage. Barium, a liquid mixture, is sometimes used in place of air to fix the blockage in the same way.
Both types of enema are very safe, and children usually do very well. However, it’s important to remember that the intussusception can return in 1 out of 10 cases. This usually happens within 72 hours following the procedure.
If the intestine is torn, an enema doesn’t work, or the child is too sick to try an enema, the child will need surgery. This is often the case in older children. Surgeons will try to fix the obstruction, but if too much damage has been done, that part of the bowel will be removed.
After treatment, the child will stay in the hospital and get intravenous (IV) feedings through a vein until he or she can eat and normal bowel function returns. Doctors will watch the child closely to make sure that the intussusception does not return. Some babies may also need antibiotics to prevent infection.
Intussusception in children
Intussusception is the sliding of one part of the intestine into another.
Intussusception in children causes
Intussusception is caused by part of the intestine being pulled inward into itself.
The pressure created by the walls of the intestine pressing together causes:
- Decreased blood flow
- Irritation
- Swelling
Intussusception can block the passage of food through the intestine. If the blood supply is cut off, the segment of intestine pulled inside can die. Heavy bleeding may also occur. If a hole develops, infection, shock, and dehydration can take place very rapidly.
The cause of intussusception is not known. Conditions that may lead to the problem include:
- Viral infection
- Englarged lymph node in the intestine
- Polyp or tumor
The reason for the problem is more likely to be found in older children.
Intussusception can affect both children and adults. However, most cases occur in children ages 6 months to 2 years. It affects boys four times as often as girls.
Intussusception in children prognosis
The outcome is good with early treatment. There is a risk this problem will come back.
When a hole or tear in the bowel occurs, it must be treated right away. If not treated, intussusception is almost always fatal for infants and young children.
Intussusception in children symptoms
The first sign of intussusception is very often sudden, loud crying caused by abdominal pain. The pain is colicky and not continuous (intermittent), but it comes back often. The pain will get stronger and last longer each time it returns.
An infant with severe abdominal pain may draw the knees to the chest while crying.
Other symptoms include:
- Bloody, mucus-like bowel movement, sometimes called a “currant jelly” stool
- Fever
- Shock (pale color, lethargy, sweating)
- Stool mixed with blood and mucus
- Vomiting
Intussusception in children diagnosis
Your doctor will perform a thorough exam, which may reveal a mass in the abdomen. There may also be signs of dehydration or shock.
Tests may include:
- Abdominal ultrasound
- Abdominal x-ray
- Air or contrast enema
Intussusception in children treatment
The child will first be stabilized. A tube will be passed into the stomach through the nose (nasogastric tube). An intravenous (IV) line will be placed in the arm, and fluids will be given to prevent dehydration.
In some cases, the bowel blockage can be treated with an air or contrast enema. This is done by a radiologist skilled with the procedure. There is a risk of bowel tearing (perforation) with this procedure.
The child will need surgery if these treatments do not work. The bowel tissue can very often be saved. Dead tissue will be removed.
Antibiotics may be needed to treat any infection.
Intravenous feeding and fluids will be continued until the child has a normal bowel movement.
Intussusception in adults
Bowel intussusception in adults is considered a rare condition, accounting for 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction 2. Eight to twenty percent of cases are idiopathic, without a lead point lesion. Secondary intussusception is caused by organic lesions, such as inflammatory bowel disease, postoperative adhesions, Meckel’s diverticulum, benign and malignant lesions, metastatic neoplasms or even iatrogenically, due to the presence of intestinal tubes, jejunostomy feeding tubes or after gastric surgery. Computed tomography is the most sensitive diagnostic modality and can distinguish between intussusceptions with and without a lead point. Surgery is the definitive treatment of adult intussusceptions.
Adult intussusception is distinct from pediatric intussusception in various aspects. In children, it is usually primary and benign, and pneumatic or hydrostatic (air contrast enemas) reduction of the intussusception is sufficient to treat the condition in 80% of the patients. In contrast, almost 90% of the cases of intussusception in adults are secondary to a pathologic condition that serves as a lead point, such as carcinomas, polyps, Meckel’s diverticulum, colonic diverticulum, strictures or benign neoplasms, which are usually discovered intraoperatively 3. Due to a significant risk of associated malignancy, which approximates 65% 4, radiologic decompression is not addressed preoperatively in adults. Therefore, 70 to 90% of adult cases of intussusception require definite treatment, of which surgical resection is, most often, the treatment of choice 5.
Intussusceptions have been classified according to their locations into four categories 6:
- Entero-enteric, confined to the small bowel,
- Colo-colic, involving the large bowel only,
- Ileo-colic, defined as the prolapse of the terminal ileum within the ascending colon and
- Ileo-cecal, where the ileo-cecal valve is the leading point of the intussusception and that is distinguished with some difficulty from the ileo-colic variant.
Intussusceptions have also been classified according to cause (benign, malignant or idiopathic). In the small intestine, an intussusception can be secondary either to the presence of intra- or extra-luminal lesions (inflammatory lesions, Meckel’s diverticulum, postoperative adhesions, lipoma, adenomatous polyps, lymphoma and metastases) or iatrogenic, e.g. due to the presence of an intestinal tube 7 or even in patients with a gastrojejunostomy 8. Malignancy (adenocarcinoma) accounts for up to 30% of cases of intussusception occurring in the small intestine 5.
Adult bowel intussusception is a rare but challenging condition for the surgeon. Preoperative diagnosis is usually missed or delayed because of nonspecific and often subacute symptoms, without the pathognomonic clinical picture associated with intussusception in children. Abdominal CT is considered as the most sensitive imaging modality in the diagnosis of intussusception and distinguishes the presence or absence of a lead point. Due to the fact that adult intussusception is often frequently associated with malignant organic lesions, surgical intervention is necessary. Treatment usually requires formal resection of the involved bowel segment. Reduction can be attempted in small bowel intussusceptions provided that the segment involved is viable or a malignancy is not suspected.
Intussusception in adults causes
Intussusception in adults up to 90% of cases having a lead point, which is usually malignant in the large bowel and benign in the small bowel 1.
Intussusception in adults symptoms
The clinical presentation of adult intussusception varies considerably. The presenting symptoms are nonspecific and the majority of cases in adults have been reported as chronic, consistent with partial obstruction 9. The classic pediatric presentation of acute intussusception (a triad of cramping abdominal pain, bloody diarrhea and a palpable tender mass) is rare in adults. Nausea, vomiting, gastrointestinal bleeding, change in bowel habits, constipation or abdominal distension are the nonspecific symptoms and signs of intussusception 10.
Intussusception in adults can be further classified according to the presence of a lead point or not 11: transient non-obstructing intussusception without a lead point has been described in patients with celiac 12 or Crohn’s disease 13, but is more frequently idiopathic and resolves spontaneously without any specific treatment. On the other hand, intussusception with an organic lesion as the lead point usually presents as a bowel obstruction, persistent or relapsing, necessitating, however, a definite surgical therapy.
Intussusception in adults diagnosis
Variability in clinical presentation and imaging features often make the preoperative diagnosis of intussusception a challenging and difficult task. Reijnen et al 14 reported a preoperative diagnostic rate of 50%, while Eisen et al 15 reported a lower rate of 40.7%.
Plain abdominal films are typically the first diagnostic tool, since in most cases the obstructive symptoms dominate the clinical picture. Such films usually demonstrate signs of intestinal obstruction and may provide information regarding the site of obstruction 15. Upper gastrointestinal contrast series may show a “stacked coin” or “coil-spring” appearance, while a barium enema examination may be useful in patients with colo-colic or ileo-colic intussusception, during which a “cup-shaped” filling defect or “spiral” or “coil-spring” appearances are characteristically demonstrated 15.
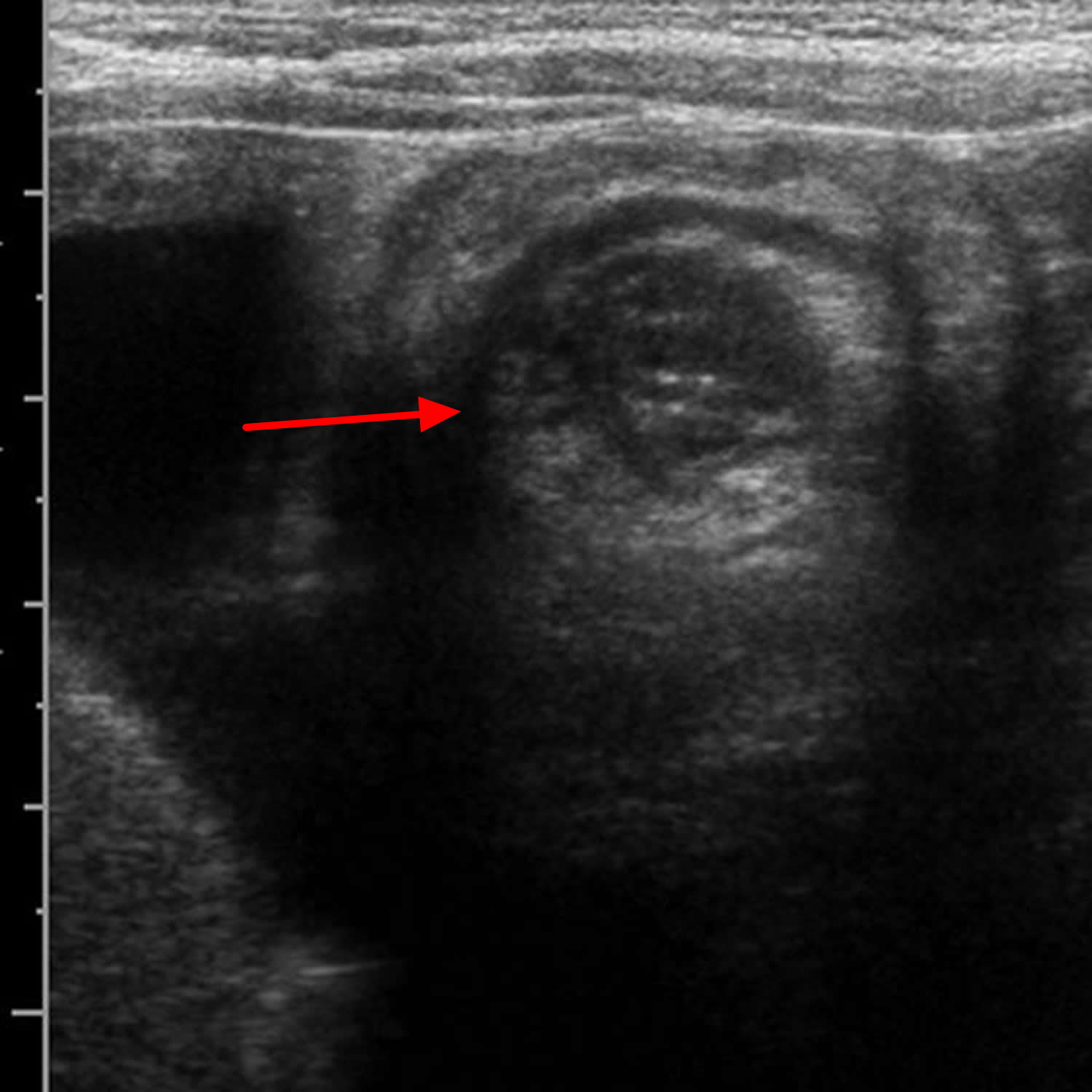
Ultrasonography is considered a useful tool for the diagnosis of intussusception, both in children and in adults 16. The classical imaging features include the “target” or “doughnut” signs on the transverse view and the “pseudo-kidney” sign or “hay-fork” sign in the longitudinal view 17. Undoubtedly, this procedure requires handling and interpretation by an experienced radiologist, in order to confirm the diagnosis. However, obesity and the presence of massive air in the distended bowel loops limit the image quality and the subsequent diagnostic accuracy.
Abdominal computed tomography (CT) is currently considered as the most sensitive radiologic method to confirm intussusception, with a reported diagnostic accuracy of 58%-100% 18. The characteristic features of CT scan include an unhomogeneous “target” or “sausage”- shaped soft- tissue mass with a layering effect (see Figures 4 and 5 below); mesenteric vessels within the bowel lumen are also typical 5. A CT scan may define the location, the nature of the mass, its relationship to surrounding tissues and, additionally, it may help staging the patient with suspected malignancy causing the intussusception 15. In a recent interesting report by Kim et al 19, abdominal CT was able to distinguish between intussusception without a lead point (features: no signs of proximal bowel obstruction, target-like or sausage-shaped mass, layering effect) from that with a lead point (features: signs of bowel obstruction, bowel wall edema with loss of the classic three-layer appearance due to impaired mesenteric circulation and demonstration of the lead mass), and this may help reducing the number of unnecessary surgical interventions.
Intussusception in adults treatment
Due to the fact that adults present with acute, subacute, or chronic nonspecific symptoms 20, the initial diagnosis is missed or delayed and is established only when the patient is on the operating table. Most surgeons accept that adult intussusception requires surgical intervention because of the large proportion of structural anomalies and the high incidence of occurring malignancy. However, the extent of bowel resection and the manipulation of the intussuscepted bowel during reduction remain controversial 5. In contrast to pediatric patients, where intussusception is primary and benign, preoperative reduction with barium or air is not suggested as a definite treatment for adults 5.
The theoretical risks of preliminary manipulation and reduction of an intussuscepted bowel include:
- (1) intraluminal seeding and venous tumor dissemination,
- (2) perforation and seeding of microorganisms and tumor cells to the peritoneal cavity and
- (3) increased risk of anastomotic complications of the manipulated friable and edematous bowel tissue 21.
Moreover, reduction should not be attempted if there are signs of inflammation or ischemia of the bowel wall 22. Therefore, in patients with ileo-colic, ileo-cecal and colo-colic intussusceptions, especially those more than 60 years of age, due to the high incidence of bowel malignancy as the underlying etiologic factor, formal resections using appropriate oncologic techniques are recommended, with the construction of a primary anastomosis between healthy and viable tissue 23. Azar et al 18 report that, for right-sided colonic intussusceptions, resection and primary anastomosis can be carried out even in unprepared bowels, while for left-sided or rectosigmoid cases resection with construction of a colostomy and a Hartmann’s pouch with re-anastomosis at a second stage is considered safer, especially in the emergency setting.
However, when a preoperative diagnosis of a benign lesion is safely established, the surgeon may reduce the intussusception by milking it out in a distal to proximal direction 24, allowing for a limited resection. Wang et al 25 report that for enteric intussusceptions due to benign lesions, reduction and limited resection resulted in non-recurrence of intussusception. In patients with a risk of a short bowel syndrome due to multiple small intestinal polyps causing intussusception, such as Peutz-Jeghers syndrome, a combined approach with limited intestinal resections and multiple snare polypectomies should be mandatory 26. Moreover, in patients complicated with postoperative bowel obstruction due to an intussusception, reduction is also recommended, provided that the bowel appears non-ischemic and viable 18.
Finally, several reports have been published regarding the laparoscopic approach of adult intussusception, due to benign and malignant lesions of the small and large bowel 27. Laparoscopy has been used successfully in selected cases, depending on patients’ general status and availability of surgeons with sufficient laparoscopic expertise. After establishing the diagnosis of intussusception and the underlying disease laparoscopically, reduction and/or en bloc resection can be performed with the same method.
Intussusception requires emergency medical care. If you or your child develops the signs or symptoms listed above, seek medical help right away.
In infants, remember that signs of abdominal pain may include recurrent bouts of pulling the knees to the chest and crying.
Intussusception complications
Intussusception can cut off the blood supply to the affected portion of the intestine. If left untreated, lack of blood causes tissue of the intestinal wall to die. Tissue death can lead to a tear (perforation) in the intestinal wall, which can cause an infection of the lining of the abdominal cavity (peritonitis).
Peritonitis is a life-threatening condition that requires immediate medical attention. Signs and symptoms of peritonitis include:
- Abdominal pain
- Abdominal swelling
- Fever
Peritonitis may cause your child to go into shock. Signs and symptoms of shock include:
- Cool, clammy skin that may be pale or gray
- A weak and rapid pulse
- Abnormal breathing that may be either slow and shallow or very rapid
- Anxiety or agitation
- Profound listlessness
A child who is in shock may be conscious or unconscious. If you suspect your child is in shock, seek emergency medical care right away.
Intussusception causes
Your intestine is shaped like a long tube. In intussusception, one part of your intestine — usually the small intestine — slides inside an adjacent part. This is sometimes called telescoping because it’s similar to the way a collapsible telescope folds together.
In some cases, the telescoping is caused by an abnormal growth in the intestine, such as a polyp or a tumor (called a lead point). The normal wave-like contractions of the intestine grab this lead point and pull it and the lining of the intestine into the bowel ahead of it. In most cases, however, no cause can be identified for intussusception.
In children, a lead point is not identified in 90% of cases, and this is most frequently thought to relate to hypertrophic lymphoid tissue following an infection. This potentially explains the relative rarity of the condition in the first three months of life, when passive immunity is still paramount.
In infants and adults, a lead point is more frequently identified with up to 90% of adult cases having a lead point (which is usually malignant in the large bowel and benign in the small bowel).
Lead points are numerous and include 28, 29, 1:
- gastrointestinal malignancy (most common cause in adults, accounting for 65% of cases) 1
- colorectal carcinoma (most common)
- metastases, e.g. malignant melanoma, breast cancer, lung cancer
- small bowel lymphoma/Burkitt lymphoma
- benign neoplasms
- gastrointestinal stromal tumor (GIST)
- intestinal polyps
- intestinal lipoma
- polypoid haemangioma
- congenital
- Meckel diverticulum
- duplication cyst
- ectopic pancreas
- inflammatory
- periappendicitis
- trauma
- mural hematoma
Children
In the vast majority of cases of intussusception in children, the cause is unknown. Because intussusception seems to occur more often in the fall and winter and because many children with the problem also have flu-like symptoms, some suspect a virus may play a role in the condition. Sometimes, a lead point can be identified as the cause of the condition — most frequently the lead point is a Meckel’s diverticulum (a pouch in the lining of the small intestine).
Adults
In adults, intussusception is usually the result of a medical condition or procedure, including:
- A polyp or tumor
- Scar-like tissue in the intestine (adhesions)
- Weight-loss surgery (gastric bypass) or other surgery on the intestinal tract
- Inflammation due to diseases such as Crohn’s disease
Risk factors for intussusception
Risk factors for intussusception include:
- Age. Children — especially young children — are much more likely to develop intussusception than adults are. It’s the most common cause of bowel obstruction in children between the ages of 6 months and 3 years.
- Sex. Intussusception more often affects boys.
- Abnormal intestinal formation at birth. Intestinal malrotation is a condition in which the intestine doesn’t develop or rotate correctly, and it increases the risk for intussusception.
- A prior history of intussusception. Once you’ve had intussusception, you’re at increased risk of developing it again.
- A family history. Siblings of someone who’s had an intussusception are at a much higher risk of the disorder.
Intussusception symptoms
Symptoms in infants and children
Babies and children with intussusception have intense abdominal pain, which often begins suddenly and causes the child to draw the knees up toward the chest. The pain often makes the child cry very loudly. As it eases, the child may stop crying for a while and may seem to feel better. The pain usually comes and goes like this, but can become very strong when it returns.
The pain of intussusception comes and goes, usually every 15 to 20 minutes at first. These painful episodes last longer and happen more often as time passes.
Symptoms also can include:
- abdominal swelling
- vomiting
- vomiting up bile, a bitter-tasting yellowish-green fluid
- passing stools (poop) mixed with blood and mucus, known as currant jelly stool
- grunting due to pain
- fever
Not everyone has all of the symptoms. Some infants have no obvious pain, and some children don’t pass blood or have a lump in the abdomen. Some older children have pain but no other symptoms.
As the illness continues, the child may gradually become weaker. He or she may develop a fever and appear to go into shock, a life-threatening medical problem in which lack of blood flow to the body’s organs causes the heart to beat quickly and blood pressure to drop.
Some babies with intussusception may just appear drowsy without vomiting, have stool changes, or have abdominal swelling.
Symptoms in adults
Because intussusception is rare in adults and symptoms of the disorder often overlap with the symptoms of other disorders, it’s more challenging to identify. The most common symptom is abdominal pain that comes and goes. Nausea and vomiting may also occur. Adults sometimes have symptoms for weeks before seeking medical attention.
Intussusception diagnosis
Your or your child’s doctor will start by getting a history of the symptoms of the problem. He or she may be able to feel a sausage-shaped lump in the abdomen. To confirm the diagnosis, your doctor may order:
- Ultrasound or other abdominal imaging. An ultrasound, X-ray or computerized tomography (CT) scan may reveal intestinal obstruction caused by intussusception. Imaging will typically show a “bull’s-eye,” representing the intestine coiled within the intestine. Abdominal imaging also can show if the intestine has been torn (perforated).
- Air or barium enema. An air or barium enema is basically enhanced imaging of the colon. During the procedure, the doctor will insert air or liquid barium into the colon through the rectum. In addition, an air or barium enema can actually fix intussusception 90 percent of the time in children, and no further treatment is needed. A barium enema can’t be used if the intestine is torn.
Figure 4. Intussusception ultrasound
Figure 5. Intussusception ultrasound (target sign)
Intussusception treatment
Treatment of intussusception typically happens as a medical emergency. Emergency medical care is required to avoid severe dehydration and shock, as well as prevent infection that can occur when a portion of intestine dies due to lack of blood.
Initial care
When your child arrives at the hospital, the doctors will first stabilize his or her medical condition. This includes:
- Giving your child fluids through an intravenous (IV) line
- Helping the intestines decompress by putting a tube through the child’s nose and into the stomach (nasogastric tube)
Correcting the intussusception
To treat the problem, your doctor may recommend:
- A barium or air enema. This is both a diagnostic procedure and a treatment. If an enema works, further treatment is usually not necessary. This treatment is highly effective in children, but rarely used in adults. Intussusception recurs as often as 10 percent of the time and the treatment will have to be repeated.
Intussusception surgery
If the intestine is torn, if an enema is unsuccessful in correcting the problem or if a lead point is the cause, surgery is necessary. The surgeon will free the portion of the intestine that is trapped, clear the obstruction and, if necessary, remove any of the intestinal tissue that has died. Surgery is the main treatment for adults and for people who are acutely ill.
In some cases, intussusception may be temporary and go away without treatment.
- Choi SH, Han JK, Kim SH et-al. Intussusception in adults: from stomach to rectum. AJR Am J Roentgenol. 2004;183 (3): 691-8. AJR Am J Roentgenol. https://www.ajronline.org/doi/full/10.2214/ajr.183.3.1830691[↩][↩][↩][↩][↩]
- Adult intussusception. Azar T, Berger DL. Ann Surg. 1997 Aug; 226(2):134-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190946/pdf/annsurg00018-0024.pdf[↩]
- Akcay MN, Polat M, Cadirci M, Gencer B. Tumor-induced ileo-ileal invagination in adults. Am Surg. 1994;60:980–981 https://www.ncbi.nlm.nih.gov/pubmed/7992979[↩]
- Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg. 2003;186:75–76. https://www.ncbi.nlm.nih.gov/pubmed/12842754[↩]
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88–94 https://www.ncbi.nlm.nih.gov/pubmed/9074370[↩][↩][↩][↩][↩]
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230–236 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1345048/pdf/annsurg00216-0114.pdf[↩]
- Ishii M, Teramoto S, Yakabe M, Yamamato H, Yamaguchi Y, Hanaoka Y, Ouchi Y. Small intestinal intussusceptions caused by percutaneous endoscopic jejunostomy tube placement. J Am Geriatr Soc. 2007;55:2093–2094 https://www.ncbi.nlm.nih.gov/pubmed/18081681[↩]
- Archimandritis AJ, Hatzopoulos N, Hatzinikolaou P, Sougioultzis S, Kourtesas D, Papastratis G, Tzivras M. Jejunogastric intussusception presented with hematemesis: a case presentation and review of the literature. BMC Gastroenterol. 2001;1:1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC29076/[↩]
- Martin-Lorenzo JG, Torralba-Martinez A, Liron-Ruiz R, Flores-Pastor B, Miguel-Perello J, Aguilar-Jimenez J, Aguayo-Albasini JL. Intestinal invagination in adults: preoperative diagnosis and management. Int J Colorectal Dis. 2004;19:68–72 https://www.ncbi.nlm.nih.gov/pubmed/12838363[↩]
- Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussu-sception in adults. Review of 160 cases. Am J Surg. 1971;121:531–535 https://www.ncbi.nlm.nih.gov/pubmed/5557762[↩]
- Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006;26:733–744 https://www.ncbi.nlm.nih.gov/pubmed/16702451[↩]
- Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146:527–531 https://www.ncbi.nlm.nih.gov/pubmed/3484870[↩]
- Knowles MC, Fishman EK, Kuhlman JE, Bayless TM. Transient intussusception in Crohn disease: CT evaluation. Radiology. 1989;170:814 https://www.ncbi.nlm.nih.gov/pubmed/2916035[↩]
- Reijnen HA, Joosten HJ, de Boer HH. Diagnosis and treatment of adult intussusception. Am J Surg. 1989;158:25–28. https://www.ncbi.nlm.nih.gov/pubmed/2662787[↩]
- Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390–395 https://www.ncbi.nlm.nih.gov/pubmed/10195723[↩][↩][↩][↩]
- Fujii Y, Taniguchi N, Itoh K. Intussusception induced by villous tumor of the colon: sonographic findings. J Clin Ultrasound. 2002;30:48–51 https://www.ncbi.nlm.nih.gov/pubmed/11807856[↩]
- Boyle MJ, Arkell LJ, Williams JT. Ultrasonic diagnosis of adult intussusception. Am J Gastroenterol. 1993;88:617–618. https://www.ncbi.nlm.nih.gov/pubmed/8470658[↩]
- Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190946/pdf/annsurg00018-0024.pdf[↩][↩][↩]
- Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006;26:733–744. https://www.ncbi.nlm.nih.gov/pubmed/16702451[↩]
- Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg. 2003;186:75–76 https://www.ncbi.nlm.nih.gov/pubmed/12842754[↩]
- Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1190946/[↩]
- Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, Hoe MN. Adult intussusception: experience in Singapore. ANZ J Surg. 2003;73:1044–1047 https://www.ncbi.nlm.nih.gov/pubmed/14632903[↩]
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230–236 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1345048/[↩]
- Wolff BC, Boller AM. Large bowel obstruction. In: JL Cameron., editor. Current surgical therapy. Mosby Elsevier: Philadelphia; 2008. pp. 189–192.[↩]
- Wang LT, Wu CC, Yu JC, Hsiao CW, Hsu CC, Jao SW. Clinical entity and treatment strategies for adult intussu-sceptions: 20 years’ experience. Dis Colon Rectum. 2007;50:1941–1949 https://www.ncbi.nlm.nih.gov/pubmed/17846839[↩]
- Lin BC, Lien JM, Chen RJ, Fang JF, Wong YC. Combined endoscopic and surgical treatment for the polyposis of Peutz-Jeghers syndrome. Surg Endosc. 2000;14:1185–1187 https://www.ncbi.nlm.nih.gov/pubmed/11148795[↩]
- Gonzalez AM, Clapp B. Laparoscopic management of small bowel intussusception in a 16-year-old with Peutz-Jeghers syndrome. JSLS. 2008;12:332–334 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3015883/[↩]
- Sparnon AL, Little KE, Morris LL. Intussusception in childhood: a review of 139 cases. Aust N Z J Surg. 1984;54 (4): 353-6 https://www.ncbi.nlm.nih.gov/pubmed/6593028[↩]
- del-Pozo G, Albillos JC, Tejedor D. Intussusception: US findings with pathologic correlation–the crescent-in-doughnut sign. Radiology. 1996;199 (3): 688-92 https://www.ncbi.nlm.nih.gov/pubmed/8637988[↩]