Contents
Why is my skin so itchy
Itchy skin or pruritus is an itchy feeling that makes you want to scratch your skin. It can be caused by many things. Normally, itchy skin isn’t serious, but it can make you uncomfortable. Itchy skin can become severe enough to interfere with work and restful sleep. Histamine is the primary mediator of itching in many disorders 1.
Sometimes, itchy skin is caused by a serious medical condition. Certain conditions, cancers, and blood disorders may cause itchy skin. Of the patients referred to a dermatologist for generalized itchy skin with no apparent primary skin cause, 14 to 24 percent have a systemic etiology. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Findings suggestive of less serious etiologies include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel. Chronic or generalized itchy skin, older age, and abnormal physical findings should increase concern for underlying systemic conditions. Initial evaluation for systemic disease includes complete blood count and measurement of thyroid-stimulating hormone, fasting glucose, alkaline phosphatase, bilirubin, creatinine, and blood urea nitrogen. Hodgkin lymphoma is the malignant disease most strongly associated with itchy skin, which affects up to 30 percent of patients with the disease 2.
A wheal and flare response indicates histamine-induced itchy skin in patients with urticaria or an allergic dermatitis. Antihistamines are effective in treating histamine-mediated itchy skin, but they may be less effective in patients with diseases that trigger itchy skin through mechanisms involving serotonin, leukotrienes, or neuropeptides 3. These patients benefit from continuous dosing of a long-acting antihistamine. Second-generation antihistamines, such as cetirizine, loratadine, and fexofenadine, may be more effective because of improved patient compliance.
However, most itchy skin can be treated at home with lotions, moisturizers, and over-the-counter medicines. Itchy skin may occur without a rash or skin lesions.
Itchy skin sometimes feels like pain because the signals for itching and pain travel along the same nerve pathways. Scratching may cause breaks in the skin, bleeding, and infection. If your skin feels itchy, let your doctor know so it can be treated and relieved.
The way itchy skin feels and how long it lasts is not the same in everyone.
The skin is the largest organ of the body. The most important job of skin is to protect against heat, sunlight, injury, and infection. The skin is also important to self-image and your ability to touch and be touched.
Itchy skin is a symptom of a certain condition, blood disorder, or a disease. These include:
- Cancer and conditions related to cancer.
- Liver, kidney, or thyroid disorders.
- Diabetes mellitus.
- HIV or parasite infection.
- Dry skin.
- Drug reactions.
- Conditions related to stress, anxiety, or depression.
The cause of itchy skin is not always known.
What causes itchy skin ?
Many different things can cause itchy skin. For example, it may be caused by allergies, infections, certain medicines, or skin conditions such as eczema or psoriasis (see Table 1). Many times itchy skin just happens when your skin is dry. This pattern is very common in the winter.
Or itchy skin can be a symptom of an occult underlying systemic disease (see Table 2).
Common Skin Causes of Itchy Skin
Atopic Dermatitis
Atopic dermatitis is characterized by itchy skin. It is generally defined as a chronic, relapsing inflammatory skin disease that often occurs in patients with a personal or family history of asthma or allergic rhinitis 4. In contrast to other dermatologic disorders, atopic dermatitis often lacks a primary skin lesion. Usually only the secondary cutaneous findings of excoriation, weeping, lichenification, and pigment changes are apparent 3.
Contact Dermatitis
Contact dermatitis is a rash caused by direct skin exposure to a substance. It is one of the most common skin disorders, with a lifetime prevalence of 30 percent. 12 Often intensely itchy, the dermatitis can be induced by an allergen or more commonly by an irritant. Irritant contact dermatitis represents the most common cause of occupational skin diseases in industrial countries 5.
Dermatophytes
Dermatophyte infections cause localized itchy skin and a rash characterized by peripheral scaling and central clearing. Tinea pedis (athlete’s foot) usually occurs between the toes with dry, cracking skin and white areas of maceration. Tinea infections can occur at several other sites, including the scalp, trunk, and groin.
Lice
Pediculosis is marked by itchy skin caused by a delayed hypersensitivity reaction to the saliva of the louse. A magnifying lens is often necessary to see the lice or eggs, usually at the base of hair shafts. Body lice are typically found in patients with poor hygiene, whereas pubic lice are sexually transmitted 6.
Lichen Simplex Chronicus
Lichen simplex chronicus is a localized disorder characterized by itchy skin that leads to thickened, lichenified, violaceous patches. These patches are intensely itchy, which causes the patient to continue to scratch, perpetuating the cycle. Early lesions manifest as erythematous, well-defined plaques with excoriations. Lesions continue to thicken if the itch-scratch-itch cycle is not broken with appropriate treatment 7.
Psoriasis
Up to 80 percent of patients with psoriasis report itchy skin that is cyclical, with nigh-time exacerbations that interrupt sleep. Itchy skin is often more generalized and not restricted to areas of psoriatic plaques 8.
Scabies
The classic feature of scabies is itchy skin, which is caused by deposition of mite eggs in the epidermal layer of skin. The itchy skin is often severe and worsens at night.
The primary lesion is a small, erythematous papule that is often excoriated. A thin, reddish-brown line, or burrow, 2 to 15 mm long in intertriginous regions is more pathognomic. However, burrows are often absent or obscured by excoriation or secondary infection. 9
Urticaria
Urticaria, or hives, is a common disorder that affects up to 25 percent of the population 10. The usual lesion is an intensely pruritic, well-circumscribed, erythematous, elevated wheal. Individual lesions may coalesce and wax and wane over several hours 11. Histamine is the primary mediator for most types of urticaria, although other immunohistochemicals may play an important role in more chronic cases 10.
Xerosis
Xerosis is the most common cause of pruritus in the absence of an identifiable skin lesion. It is characterized by dry, scaly skin, usually on the lower extremities and in axillary creases, and most often occurs in the winter months. Associated factors include older age, frequent bathing, use of hot water when bathing, and exposure to high ambient temperatures with relatively low humidity 12.
Table 1. Skin Causes of Itchy Skin
| Causes | Features |
|---|---|
Allergic/irritant contact dermatitis | Sharply demarcated, erythematous lesion with overlying vesicles |
Reaction within two to seven days of exposure | |
Atopic dermatitis | Pruritic area where rash appears when scratched in patients with atopic conditions (e.g., allergic rhinitis, asthma) |
Involvement of flexor wrists and ankles, as well as antecubital and popliteal fossae | |
Bullous pemphigoid | Initially pruritic urticarial lesions, often in intertriginous areas |
Formation of tense blisters after urticaria | |
Cutaneous T-cell lymphoma (mycosis fungoides) | Oval eczematous patch on skin with no sun exposure (e.g., buttocks) |
Possible presentation of new eczematous dermatitis in older adults | |
Possible presentation of erythroderma (exfoliative dermatitis) | |
Dermatitis herpetiformis | Rare vesicular dermatitis affecting the lumbosacral spine, elbows, or knees |
Dermatophyte infection | Localized pruritus and rash characterized by peripheral scaling and central clearing |
Can occur on several sites, including the feet, scalp, trunk, and groin | |
Folliculitis | Pruritus out of proportion to appearance of dermatitis |
Papules and pustules at follicular sites on chest, back, or thigh | |
Lichen planus | Lesions often located on the flexor wrists |
Characterized by the six P’s (pruritus, polygonal, planar, purple, papules, plaques) | |
Lichen simplex chronicus | Localized, intense pruritus |
Initial erythematous, well-defined plaques with excoriations lead to thickened, lichenified, violaceous patches if scratching continues | |
Pediculosis (lice infestation) | Occiput in school-aged children; genitalia in adults (sexually transmitted) |
Psoriasis | Plaques on extensor extremities, low back, palms, soles, and scalp |
Scabies | Burrows in hand web spaces, axillae, and genitalia |
Hyperkeratotic plaques, pruritic papules or scales | |
Face and scalp affected in children but not in adults | |
Sunburn | Possible photosensitizing cause (e.g., with use of nonsteroidal anti-inflammatory drugs or cosmetics) |
Urticaria (hives) | Intensely pruritic, well-circumscribed, erythematous, and elevated wheals |
Lesions may coalesce and wax and wane over several hours | |
Xerosis | Intense pruritus, often during winter months in northern climates |
Involvement of back, flank, abdomen, waist, and lower extremities | |
More common in older persons |
Common Systemic Causes of Itchy Skin
Itchy skin in the absence of a primary dermatologic etiology may be indicative of a serious underlying systemic disease 13. Studies have shown that 14 to 24 percent of patients presenting to a dermatologist’s office with itchy skin and no primary dermatologic cause have a systemic condition 14. However, itchy skin is often overemphasized as an early manifestation of cancer 15.
Chronic Renal Disease
More than 50 percent of patients with chronic renal disease and up to 80 percent of patients on dialysis have itchy skin 3. The itchy skin is often generalized, but may be localized to the back 16.
Liver Disease
Itchy skin caused by impaired bile secretion is a common symptom in several forms of liver disease. It can be generalized, but is typically worse on the palms and soles. Associated conditions include primary biliary cirrhosis, sclerosing cholangitis, viral hepatitis, drug-induced cholestasis, and other causes of obstructive jaundice. Biliary obstruction leads to itchy skin in these disorders, but there is little correlation between serum bilirubin level and severity of itchy skin 17.
Cancer
The possibility of an underlying malignant disease should be considered in patients with generalized itchy skin of unknown cause. Among malignant diseases, Hodgkin lymphoma has the strongest association with itchy skin, which occurs in up to 30 percent of patients with the disease 18. Itchy skin can precede the clinical presentation of lymphoma by up to five years and is often the presenting symptom 19. Itchy skin has been reported as a paraneoplastic manifestation in patients with nasopharynx, prostate, stomach, breast, brain, uterine, or colon cancer 20.
Peripheral or Central Nervous System
Itchy skin can also arise from diseases or disorders of the peripheral or central nervous system, such as multiple sclerosis, neuropathy, and nerve compression or irritation (e.g., notalgia paresthetica, brachioradial itchy skin) 21.
Psychiatric Illness
Psychiatric illness can cause itchy skin and is diagnosed through exclusion. Neurotic excoriations are scattered, linear, crusted lines that may occur anywhere on the body within reach of the patient, although they are most often confined to the extremities. They are associated with obsessive-compulsive disorder, depression, and delusions of parasitosis 22.
Pregnancy-related dermatoses (see Table 3) represent a heterogeneous group of itchy inflammatory skin diseases related to pregnancy or the postpartum period. Some dermatoses cause only intense itchy skin and skin lesions (e.g., polymorphic eruption of pregnancy, atopic eruption of pregnancy), but others can cause significant fetal risks, including prematurity, growth restriction, fetal distress, and intrauterine fetal demise (e.g., intrahepatic cholestasis of pregnancy, pemphigoid gestationis) 23, 24, 25. Early recognition, precise diagnosis, and prompt treatment are essential for improving maternal and fetal prognosis.
Table 2. Systemic Causes of Itchy Skin
Autoimmune |
Dermatitis herpetiformis |
Dermatomyositis |
Linear immunoglobulin A disease |
Sjögren syndrome |
Hematologic |
Hemochromatosis |
Iron deficiency anemia |
Mastocytosis |
Plasma cell dyscrasias |
Polycythemia vera |
Hepatobiliary |
Biliary cirrhosis |
Chronic pancreatitis with obstruction of biliary tracts |
Drug-induced cholestasis |
Hepatitis, particularly hepatitis C |
Sclerosing cholangitis |
Infectious disease |
AIDS |
Infectious hepatitis |
Parasitic disease (giardiasis, onchocerciasis, schistosomiasis, ascariasis) |
Prion disease |
Malignancy |
Leukemia |
Lymphoma |
Multiple myeloma |
Solid tumors with paraneoplastic syndrome |
Metabolic and endocrine |
Carcinoid syndrome |
Chronic renal disease |
Diabetes mellitus |
Hyper/hypothyroidism |
Hyperparathyroidism |
Neurologic |
Cerebral abscess |
Cerebral tumor |
Multiple sclerosis |
Stroke |
Other |
Drug ingestion |
Eating disorders with rapid weight loss |
Neuropsychiatric disorders |
Pregnancy |
Table 3. Pregnancy-Related Dermatoses That Cause Itchy Skin
| Condition | Synonyms | Timing | Features | Important considerations | Prognosis |
|---|---|---|---|---|---|
Atopic eruption of pregnancy | Prurigo, early-onset prurigo, pruritic folliculitis, or eczema of pregnancy; prurigo gestationis | Second trimester (75 percent of patients affected before third trimester) |
|
|
|
Tends to recur in subsequent pregnancies | |||||
Intrahepatic cholestasis of pregnancy | Cholestasis of pregnancy, obstetric cholestasis, jaundice of pregnancy, pruritus gravidarum, prurigo gravidarum, icterus gravidarum | Third trimester |
|
|
|
Tends to recur in subsequent pregnancies | |||||
Pemphigoid gestationis | Herpes gestationis | Third trimester or postpartum |
|
|
|
Tends to recur in subsequent pregnancies | |||||
Polymorphic eruption of pregnancy | Pruritic urticarial papules and plaques, polymorphic eruption, toxic erythema, toxemic rash, or late-onset prurigo of pregnancy | Late third trimester and postpartum, most often in primigravida |
|
|
|
Does not tend to recur in subsequent pregnancies |
Itchy Skin Diagnosis
The initial clinical approach in patients with pruritus includes a history and physical examination to determine if the itchy skin is caused by a skin condition or is secondary to an underlying systemic disease. Figure 1 is a diagnostic algorithm for itchy skin.
Physical examination should include an evaluation of the liver, spleen, and lymph nodes. Organomegaly increases the likelihood of an underlying systemic disease, such as lymphoma. The skin should also be examined. Finger webs, intertriginous regions, and the genitals should be evaluated for the presence of scabies or lice.
Historical and physical findings that suggest a less serious etiology include younger age, localized symptoms, acute onset, involvement limited to exposed areas, and a clear association with a sick contact or recent travel.3–5 Chronic or generalized pruritus, age older than 65 years, and abnormal physical findings should increase concern for an underlying systemic condition.3–8
If the diagnosis is unclear after the history and physical examination or if initial empiric treatment is ineffective, a limited laboratory evaluation should be performed, including complete blood count and measurement of 19:
- thyroid-stimulating hormone,
- fasting glucose,
- alkaline phosphatase (ALP),
- bilirubin, creatinine, and
- blood urea nitrogen.
If immune suppression or lymphoma is possible, a human immunodeficiency virus (HIV) antibody assay and chest radiography should also be performed 27, 29. Further diagnostic tests may include biopsy, scraping, or culture of the skin or lesions.
Figure 1. Diagnostic algorithm for itchy skin
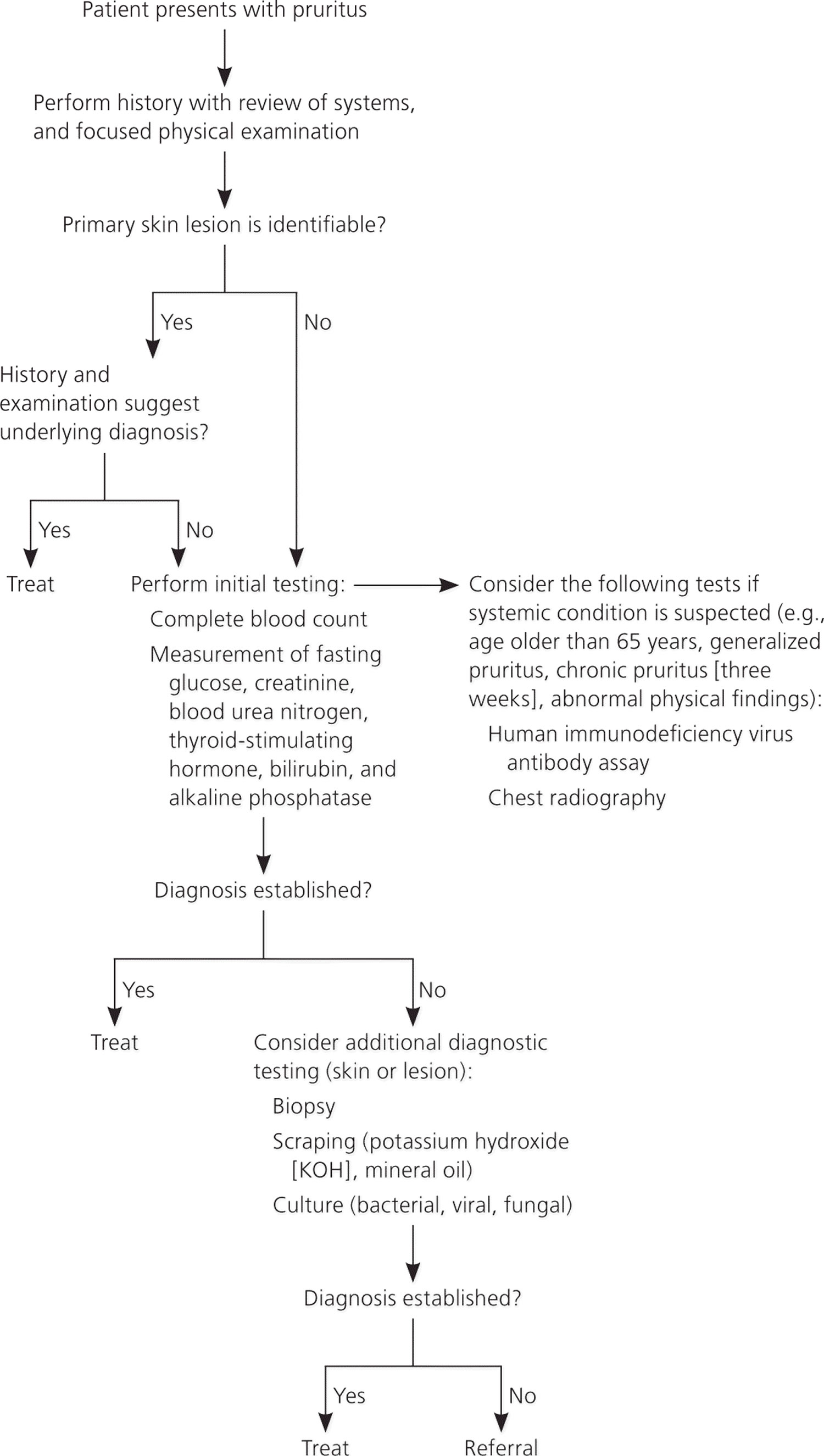
The presence of a primary skin lesion may aim the evaluation toward a dermatologic cause. The history should focus on recent exposures to new topical, oral, or airborne substances that can cause skin lesions. New cosmetics and creams can trigger allergic contact dermatitis, urticaria, and photodermatitis. New drugs (medications, nutritional supplements, illicit drugs) can lead to urticaria or fixed drug eruptions. Travel can expose a person to new foods that can trigger urticaria and to sunlight that can trigger photodermatitis. Travelers are also susceptible to infestations, such as with scabies or lice. Hobbies may expose the skin to solvents and topical agents that can trigger contact dermatitis. Chronic occupational exposure to solvents can dry the skin, causing xerosis and atopic dermatitis or eczema. New animal exposures can lead to flea infestations, allergic cutaneous reactions to dander, and urticaria. Another important finding in the evaluation of patients with pruritus is a recent exposure to sick contacts who have febrile diseases, such as rubeola, mumps, or varicella, or exposure to infectious organisms that can cause rashes, such as parvovirus, Staphylococcus aureus, or Streptococcus species. In the absence of a primary skin lesion, the review of systems should include evaluation for thyroid disorders, lymphoma, kidney and liver diseases, and diabetes mellitus. Table 3 includes historical findings that suggest etiologies for itchy skin.
Table 4. Clinical History – Causes of Itchy Skin
| Historical finding | Possible etiologies |
|---|---|
New cosmetics or creams | Allergic contact dermatitis, urticaria, photodermatitis |
New medications, supplements, or illicit drugs | Urticaria, fixed drug eruptions |
Recent travel | Pediculosis, scabies infestation, photodermatitis, urticaria |
Hobby or occupational exposure to solvents, adhesives, cleaners | Irritant contact dermatitis, xerosis, atopic dermatitis, eczema |
New animal exposures | Flea infestation, allergic contact dermatitis, urticaria |
Sick contacts, especially those with febrile diseases and rashes | Rubeola, mumps, varicella, scarlet fever, cellulitis, fifth disease, folliculitis |
Unexplained weight changes, menstrual irregularity, heat/cold intolerance | Thyroid disease with secondary urticaria or xerosis |
Unexplained weight loss, night sweats, unexplained fevers, fatigue | Lymphoma with secondary generalized pruritus |
Malaise, nausea, decreased urine output | Renal failure with generalized pruritus |
Itchy skin treatment
A wheal and flare response is a marker of histamine-induced itchy skin in patients with urticaria or an allergic dermatitis. These patients benefit from continuous dosing of long-acting antihistamines. First-and second-generation antihistamines are equally effective for resolution of pruritus 30. However, second-generation antihistamines (e.g., cetirizine [Zyrtec], loratadine [Claritin], fexofenadine [Allegra]) cause fewer adverse effects, leading to improved patient compliance 31. Concurrent administration of histamine H1 and H2 blockers increases therapeutic effectiveness 3.
Most patients with itchy skin benefit from several basic measures to lessen drying of skin, which can increase symptoms. Bathing should be limited to short, cool showers with soap applied only to intertriginous or oily skin areas. A mild moisturizing cream should be applied immediately after bathing. The patient’s home should be humidified to at least 40 percent, especially during dry, cold winter months. Contact irritants, such as wool, fiberglass, and detergents, irritate most skin and can exacerbate symptoms, particularly in persons with sensitivity to these agents 32.
The conditions that can lead to itchy skin are extensive. Distinguishing between itchy skin with a specific dermatologic cause and itchy skin that is a manifestation of a systemic disease can facilitate efficient diagnosis and treatment, leading to a rapid resolution of symptoms for most patients.
Moisturizers work well to treat dry, itchy skin. Choose a moisturizer that is hypoallergenic (it should say so on the label). This means that this type of moisturizer is less likely to cause an allergic reaction on your skin. The best moisturizers are also the most “greasy.” Ointments (or oils) are best, followed by creams, and then lotions.
Put a moisturizer on your skin 3 or 4 times during the day. A moisturizer might be all you need to relieve itching. Put moisturizer on right after you wash or bathe. This will hold in the moisture from the water. If you have very dry hands, put petroleum jelly (one brand name: Vaseline) on them before you go to bed at night and sleep with your hands in cotton-lined gloves. If a moisturizer does not help enough, you could try using 1% hydrocortisone steroid skin cream for a week. If this is not helpful, your doctor may prescribe stronger steroids or antihistamine pills.
Changing your bathing habits can also help. If you bathe too often, it may dry out your skin. Try to take short, lukewarm baths or showers. Oatmeal baths (one brand name: Aveeno) may be soothing to dry skin. Use a mild soap every day to clean your genital area and under your arms. Use soap on other parts of your body 2 or 3 times a week only.
Some people use bath oils to help make their skin less dry. However, these oils can make your tub slippery. To avoid slipping and falling, put the oil on your skin after you get out of the bathtub.
Be sure to talk with your doctor if you are using a steroid cream or ointment to treat your itching. Do not use steroid creams to treat itching for longer than 1 to 2 weeks unless your doctor recommends it. Do not put a steroid cream on your face or genital area. Steroid creams may make your skin get very thin and may cause other skin problems.
Home remedies for itchy skin
Home remedies include avoiding itchy skin triggers and taking good care of your skin.
Itchy skin triggers include:
- Dehydration caused by fever, diarrhea, nausea and vomiting, or low fluid intake.
- Hot baths or bathing more than once a day, or for longer than 30 minutes.
- Bubble baths or soaps with detergents.
- Reusable scrubbing sponges for the face or loofahs for the body.
- Scents, fragrances, and perfumes.
- Adding oil at the beginning of the bath.
- Dry indoor air.
- Laundry detergent with scents, dyes, or preservatives.
- Fabric softener sheets.
- Tight clothes or clothes made of wool, synthetics, or other harsh/scratchy fabric.
- Underarm deodorants or antiperspirants.
- Skin care or cosmetics with scents, dyes, or preservatives.
- Emotional stress.
Ways to help lessen itching include:
- Using unscented, soothing creams or ointments.
- Bathing in slightly warm water no more than 30 minutes daily or every other day.
- Using mild skin cleansers (non-soap) or soaps made for sensitive skin (such as Cetaphil cleanser, Dove for Sensitive Skin, Oilatum, Basis).
- Adding oil and soap at the end of a bath or adding a colloidal oatmeal treatment early to the bath.
- Using soap only for dirty areas; otherwise water is good enough.
- Gently washing, if needed, with a clean, fresh, soft cotton washcloth.
- Rinsing all soap or other residue from bathing with fresh, slightly warm water.
- Drying off by patting skin instead of rubbing.
- Keeping home air cool and humid (including use of a humidifier).
- Washing sheets, clothes, and underwear in mild soap or baby soap that contains no scents, dyes, or preservatives (such as Dreft, All Free Clear, Tide Free and Gentle). Adding vinegar (one teaspoon per quart of water) to rinse water removes traces of detergent.
- Using liquid fabric softener that gets rinsed out in the wash (such as All Free Clear Fabric Softener) or avoiding fabric softener altogether.
- Using blankets that are soft, such as cotton flannel.
- Wearing loose-fitting clothes and clothes made of cotton or other soft fabrics.
- Using distraction, music therapy, relaxation, or positive imagery.
Over-the-counter treatments
Some over-the-counter treatments (medicines that can be bought without a prescription) help prevent or relieve pruritus. However, you should read labels carefully to look for ingredients that may trigger skin reactions, including alcohol, topical antibiotics, and topical anesthetics.
Cornstarch and talc
Cornstarch can help prevent itching of dry skin caused by radiation therapy but should not be used where skin is moist. When cornstarch becomes moist, fungus may grow. Avoid using it on areas close to mucous membranes, such as the vagina or rectum, in skin folds, and on areas that have hair or sweat glands.
Some powders and antiperspirants, such as those that contain talc and aluminum, cause skin irritation during radiation therapy and should be avoided when you’re receiving radiation treatment.
For itching not related to radiation therapy, talc-based treatments may be better than cornstarch-based treatments, especially where two skin surfaces touch or rub together (such as the underarm or between fingers or toes).
Creams and lotions
If itchy skin is related to dry skin, emollient creams or lotions may be used. Emollients help soothe and soften the skin and increase moisture levels in the skin. It is important to know the ingredients in these creams and lotions because some may cause skin reactions. Such ingredients include:
- Petrolatum, which is not well absorbed in skin treated with radiation therapy and may build up too much or be hard to remove.
- Lanolin, which may cause allergic reactions in some people.
- Mineral oil, which may be combined with petrolatum and lanolin in creams and lotions and may be an ingredient in bath oils.
Other ingredients added to emollients, such as thickeners, preservatives, fragrances, and colorings, may also cause allergic skin reactions.
Emollient creams or lotions are applied at least two or three times a day and after bathing. Gels with a local anesthetic (0.5%–5% lidocaine) can be used on some small areas as often as every 2 hours if you aren’t sensitive to alcohol ingredients.
To soothe or cool areas of severe pruritus, over-the-counter products containing menthol, camphor, pramoxine, or capsaicin can be used. These products soothe, cool, and decrease the urge to scratch. Capsaicin-based therapies may work best in pruritus related to nerve signals.
Prescription drugs applied to the skin
Your doctor may prescribe topical steroids (steroids applied to the skin) to reduce itching, but they cause thinning of the skin and make it more sensitive. They should be used only for pruritus related to inflammation. Topical steroids should not be used on skin being treated with radiation therapy, but may be used to relieve inflamed skin after radiation treatment ends.
For xerosis (abnormally dry skin) or keratoderma (a horn-like skin condition), moisturizer creams may be used to seal in moisture and peel off scaly layers of skin. Humectants with ingredients like salicylic acid, ammonium lactate, or urea may improve skin smoothness but can cause stinging if applied to broken skin.
Systemic therapies
Systemic therapies travel through the bloodstream and reach and affect cells all over the body. They may help treat the condition causing your pruritus or help control your symptoms.
Your doctor may prescribe an antibiotic if your pruritus is caused by an infection. You may also be given an oral antihistamine to relieve itching. A larger dose may sometimes be used at bedtime to help you sleep.
Other drug therapies
If other drug treatments do not work to control pruritus, sedatives and antidepressants are sometimes used.
Aspirin may relieve pruritus in some patients with polycythemia vera but may increase pruritus in others. Cimetidine alone or combined with aspirin may help control pruritus in patients with Hodgkin lymphoma and polycythemia vera.
Comfort measures
Other steps may be taken to help you keep from scratching and stop the itch-scratch-itch cycle. These may include:
- Applying emollients to help prevent skin breakdown.
- A cool washcloth or ice held over the itchy area.
- Firm pressure on the itchy area, on the same area on the opposite side of the body, and at acupressure points.
- Rubbing or vibration on the itchy area.
- Transcutaneous electrical nerve stimulation (TENS) or acupuncture.
- Paus R, Schmelz M, Bíró T, et al. Frontiers in pruritus research: scratching the brain for more effective itch therapy. J Clin Invest. 2006;116(5):1174–1186.[↩]
- A Diagnostic Approach to Pruritus. Am Fam Physician. 2011 Jul 15;84(2):195-202. http://www.aafp.org/afp/2011/0715/p195.html[↩][↩][↩]
- Charlesworth EN, Beltrani VS. Pruritic dermatoses: overview of etiology and therapy. Am J Med. 2002;113(suppl 9A):25S–33S.[↩][↩][↩][↩][↩]
- Charlesworth EN. Practical approaches to the treatment of atopic dermatitis. Allergy Proc. 1994;15(6):269–274.[↩]
- Clark SC, Zirwas MJ. Management of occupational dermatitis Dermatol Clin. 2009;27(3):365–383, vii–viii.[↩]
- Greco PJ, Ende J. Pruritus: a practical approach. J Gen Intern Med. 1992;7(3):340–349.[↩]
- Lichon V, Khachemoune A. Lichen simplex chronicus. Dermatol Nurs. 2007;19(3):276.[↩]
- Krueger G, Koo J, Lebwohl M, et al. The impact of psoriasis on quality of life: results of a 1998 National Psoriasis Foundation patient-membership survey. Arch Dermatol. 2001;137(3):280–284.[↩]
- Andrews RM, McCarthy J, Carapetis JR, et al. Skin disorders, including pyoderma, scabies, and tinea infections. Pediatr Clin North Am. 2009;56(6):1421–1440.[↩]
- Gratten CEH, Charlesworth EN. Urticaria. In: Holgate ST, Lichtenstein LM, Church MK, eds. Allergy. 2nd ed. London, United Kingdom: Mosby; 2001: 93–104.[↩][↩]
- Charlesworth EN. The spectrum of urticaria. All that urticates may not be urticaria. Immunol Allergy Clin North Am. 1995;15(4):641–657.[↩]
- Millikan LE. Treating pruritus. What’s new in safe relief of symptoms? Postgrad Med. 1996;99(1):173–176.[↩]
- Zirwas MJ, Seraly MP. Pruritus of unknown origin: a retrospective study. J Am Acad Dermatol. 2001;45(6):892–896.[↩]
- Rajka G. Investigation of patients suffering from generalized pruritus, with special references to systemic diseases. Acta Derm Venereol. 1966;46(2):190–194.[↩]
- Greaves MW. Itching—research has barely scratched the surface. N Engl J Med. 1992;326(15):1016–1017.[↩]
- Ponticelli C, Bencini PL. Pruritus in dialysis patients: a neglected problem. Nephrol Dial Transplant. 1995;10(12):2174–2176.[↩]
- Jones EA, Bergasa NV. The pruritus of cholestasis and the opioid system. JAMA. 1992;268(23):3359–3362.[↩]
- Lober CW. Should the patient with generalized pruritus be evaluated for malignancy? J Am Acad Dermatol. 1988;19(2 pt 1):350–352.[↩][↩]
- Etter L, Myers SA. Pruritus in systemic disease: mechanisms and management Dermatol Clin. 2002;20(3):459–472, vi–vii.[↩][↩][↩]
- Fleischer AB Jr. Pruritus in the elderly. Adv Dermatol. 1995;10:41–59.[↩]
- Bernhard JD. Itch and pruritus: what are they, and how should itches be classified? Dermatol Ther. 2005;18(4):288–291.[↩]
- Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther. 2008;21(1):32–41.[↩]
- Vaughan Jones SA, Hern S, Nelson-Piercy C, et al. A prospective study of 200 women with dermatoses of pregnancy correlating clinical findings with hormonal and immunopathological profiles. Br J Dermatol. 1999;141(1):71–81.[↩]
- Shornick JK. Pregnancy dermatoses. In: Bolognia JL, Jorizzo JL, Rapini RP, eds. Dermatology. London, United Kingdom: Mosby; 2003: 425–432.[↩]
- Cohen LM, Kroumpouzos G. Pruritic dermatoses of pregnancy: to lump or to split? J Am Acad Dermatol. 2007;56(4):708–709.[↩]
- Yosipovitch G, David M. The diagnostic and therapeutic approach to idiopathic generalized pruritus. Int J Dermatol. 1999;38(12):881–887.[↩]
- Moses S. Pruritus. Am Fam Physician. 2003;68(6):1135–1142.[↩][↩]
- Kantor GR, Lookingbill DP. Generalized pruritus and systemic disease. J Am Acad Dermatol. 1983;9(3):375–382.[↩]
- Krajnik M, Zylicz Z. Understanding pruritus in systemic disease. J Pain Symptom Manage. 2001;21(2):151–168.[↩]
- Crownover BK, Jamieson B, Mott TF. First- or second-generation antihistamines: which are more effective at controlling pruritus? J Fam Pract. 2004;53(9):742–744.[↩]
- Finn AF Jr, Kaplan AP, Fretwell R, et al. A double-blind, placebo-controlled trial of fexofenadine HCl in the treatment of chronic idiopathic urticaria. J Allergy Clin Immunol. 1999;104(5):1071–1078.[↩]
- Koblenzer CS. Itching and the atopic skin. J Allergy Clin Immunol. 1999;104(3 pt 2):S109–S113.[↩]