Contents
What is Japanese encephalitis
Japanese Encephalitis is a severe inflammation of the brain caused by the Japanese B Encephalitis virus that is transmitted by the bite of infected mosquitoes in certain areas of the world, particularly Asia and the western Pacific. This disorder most commonly affects children and tends to be more actively spread during the summer. Symptoms include high fever, headaches, weakness, nausea, vomiting, paralysis, personality changes, and coma, possibly leading to neurological damage or death.
For most travelers to Asia, the risk for Japanese encephalitis is very low but varies based on destination, duration of travel, season, and activities. Japanese encephalitis usually occurs in rural or agricultural areas, where there are pig farms and rice fields. In temperate areas of Asia, transmission is seasonal, and human disease usually peaks in the summer and fall. In the subtropics and tropics, transmission can occur year-round, often with a peak during the rainy season.
Japanese encephalitis can’t be spread from person to person.
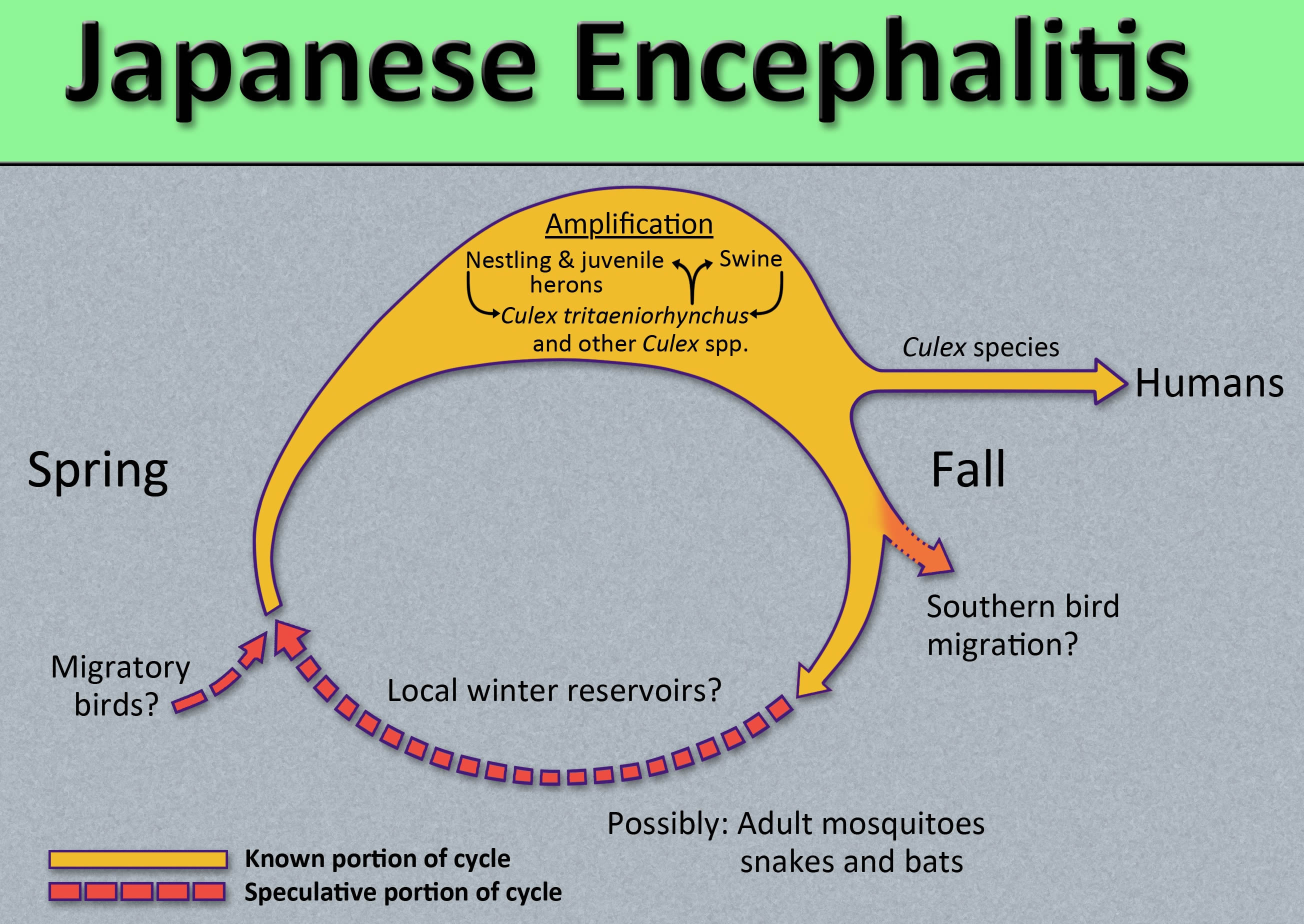
Japanese encephalitis virus is maintained in a cycle involving mosquitoes and vertebrate hosts, mainly pigs and wading birds (see Figure 2). Humans can be infected when bitten by an infected mosquito. It takes 5 to 15 days after the bite of an infected mosquito to develop symptoms. Most human infections are asymptomatic or result in only mild symptoms. However, a small percentage of infected persons develop inflammation of the brain (encephalitis), with symptoms including sudden onset of headache, high fever, disorientation, coma, tremors and convulsions. Coma and paralysis occur in some cases.
About 1 in 4 cases are fatal.
There is no specific treatment for Japanese encephalitis. Treatment involves supporting the functions of the body as it tries to fight off the infection. This usually requires the person being admitted to hospital, so they can be given intravenous fluids, oxygen and medication to treat any symptoms.
Steps to prevent Japanese encephalitis include using personal protective measures to prevent mosquito bites and vaccination.
Japanese encephalitis vaccine is recommended for travelers who plan to spend at least 1 month in endemic areas during the Japanese encephalitis virus transmission season. Vaccine should also be considered for the following:
- Short-term (less than 1 month) travelers to endemic areas during the transmission season, if they plan to travel outside an urban area and their activities will increase the risk of exposure. Higher-risk activities include participating in extensive outdoor activities (such as camping, hiking, trekking, biking, fishing, hunting, or farming) and staying in accommodations without air conditioning, screens, or bed nets.
- Travelers to an area with an ongoing outbreak.
- Travelers to endemic areas who are uncertain of specific travel destinations, activities, or duration.
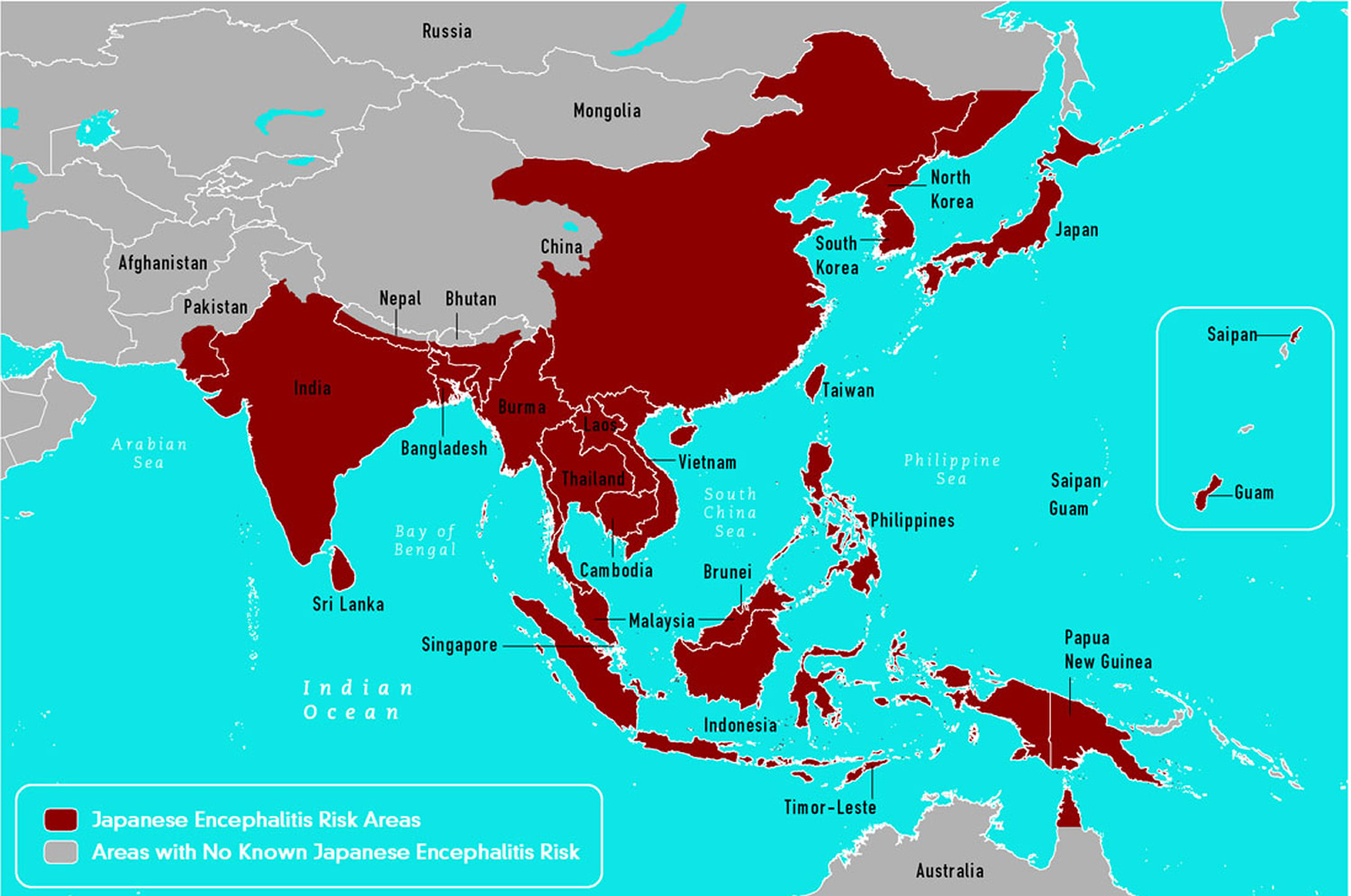
Countries in which Japanese encephalitis virus has been identified (see Japanese Encephalitis Virus Geographic Distribution map in Figure 3)
- Australia
- Bangladesh
- Brunei*
- Burma
- Cambodia
- China
- Guam
- India
- Indonesia
- Japan
- Laos
- Malaysia
- Nepal
- North Korea
- Pakistan
- Papua New Guinea
- Phillipines
- Russia
- Saipan
- Singapore
- South Korea
- Sri Lanka
- Taiwan
- Thailand
- Timor-Leste
- Vietnam
How common is Japanese encephalitis?
It’s very rare for travelers visiting risk areas to be affected by Japanese encephalitis. It’s estimated that less than one in a million travelers develop Japanese encephalitis in any given year.
The people most at risk are those who live and work in rural areas where the condition is widespread. Around 75% of cases involve children under the age of 15.
The World Health Organization (WHO) estimates there are around 68,000 cases of Japanese encephalitis worldwide each year.
Japanese encephalitis outcome
- Among patients who develop encephalitis, 20% – 30% die.
- Although some symptoms improve after the acute illness, 30%-50% of survivors continue to have neurologic, cognitive, or psychiatric symptoms.
Japanese encephalitis virus transmission
Japanese encephalitis virus, a flavivirus, is closely related to West Nile and St. Louis encephalitis viruses. Japanese encephalitis virus is transmitted to humans through the bite of infected Culex species mosquitoes, particularly Culex tritaeniorhynchus.
The virus is maintained in a cycle between mosquitoes and vertebrate hosts, primarily pigs and wading birds. Humans are incidental or dead-end hosts, because they usually do not develop high enough concentrations of Japanese encephalitis virus in their bloodstreams to infect feeding mosquitoes.
Japanese encephalitis virus transmission occurs primarily in rural agricultural areas, often associated with rice production and flooding irrigation. In some areas of Asia, these conditions can occur near urban centers.
In temperate areas of Asia, Japanese encephalitis virus transmission is seasonal. Human disease usually peaks in the summer and fall. In the subtropics and tropics, transmission can occur year-round, often with a peak during the rainy season.
Figure 1. Armigeres subalbatus mosquito has been found to be naturally infected with the Japanese Encephalitis virus
Note: Armigeres subalbatus mosquito is a vector of the filarial parasite Wuchereria bancrofti, and upon examination of captured specimens in the wild, at times has also been found to be naturally infected with the Japanese Encephalitis virus. This species can be found throughout Asia, from Pakistan in the west, all the way through Southeast Asia to Indonesia, and north to Japan and Korea.
Figure 2. Culex tritaeniorhynchus mosquito (female) can transmit Japanese encephalitis virus
 Note: Culex mosquitoes appear dull in color. Complete metamorphosis from egg , larval, pupa and adult is about 6 to 8 days. Culex mosqutioes breed mainly in polluted stagnant water especially in construction areas and drains. They are night biters and will usually stay indoors after a blood meal. Female Culex tritaeniorhynchus are active at night. They prefer to feed outdoors. Large animals like cattle and pigs are their primary vertebrates of blood meals. They also feed on birds, bats, and human.
Note: Culex mosquitoes appear dull in color. Complete metamorphosis from egg , larval, pupa and adult is about 6 to 8 days. Culex mosqutioes breed mainly in polluted stagnant water especially in construction areas and drains. They are night biters and will usually stay indoors after a blood meal. Female Culex tritaeniorhynchus are active at night. They prefer to feed outdoors. Large animals like cattle and pigs are their primary vertebrates of blood meals. They also feed on birds, bats, and human.Figure 3. Japanese Encephalitis Virus Geographic Distribution
Figure 4. Japanese encephalitis virus lifecycle
Japanese encephalitis prevention
All travelers to Japanese encephalitis endemic areas should take precautions to avoid mosquito bites to reduce the risk for Japanese encephalitis and other vector-borne infectious diseases. For some travelers who will be in a high-risk setting based on season, location, duration, and activities, Japanese encephalitis vaccine can further reduce the risk for infection.
The mosquitoes that transmit Japanese encephalitis virus feed mainly outside during the cooler hours from dusk to dawn. Travelers to high risk areas should consider minimizing outdoor activities at these times if possible. To reduce the risk of Japanese encephalitis and other vector-borne diseases, travelers should stay in air-conditioned or well-screened rooms, or use a bed net and aerosol room insecticides.
Your best bet for preventing Japanese encephalitis virus and other mosquito-borne illnesses is to prevent mosquito bites and to avoid exposure to mosquitoes and eliminate standing water, where mosquitoes breed. Be aware of the Japanese encephalitis virus activity in your area and take action to protect yourself and your family.
- Unclog roof gutters.
- Empty unused swimming pools or empty standing water on pool covers.
- Change water in birdbaths and pet bowls regularly.
- Remove old tires or unused containers that might hold water and serve as a breeding place for mosquitoes.
- Install or repair screens on windows and doors.
To reduce your exposure to mosquitoes:
- Avoid unnecessary outdoor activity when mosquitoes are most prevalent, such as at dawn, dusk and early evening.
- Wear long-sleeved shirts and long pants when outdoors.
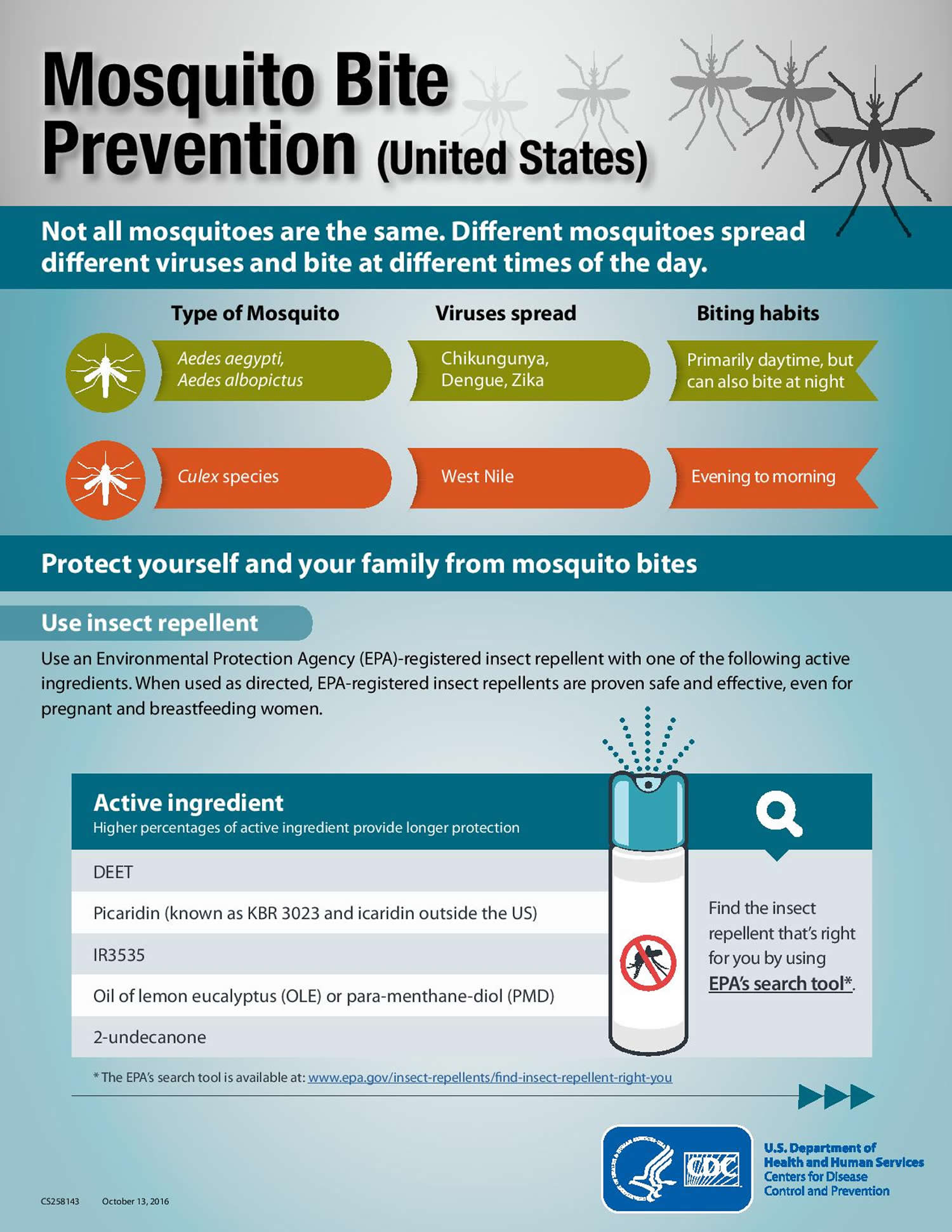
- Apply mosquito repellent containing an Environmental Protection Agency-registered insect repellent to your skin and clothing. Choose the concentration based on the hours of protection you need — the higher the percentage (concentration) of the active ingredient, the longer the repellent will work. Follow the directions on the package, paying special attention to recommendations for use on children.
- When outside, cover your infant’s stroller or playpen with mosquito netting.
Prevent Mosquito Bites
Use Insect Repellent
Use Environmental Protection Agency (EPA)-registered insect repellents with one of the active ingredients below 1. When used as directed, EPA-registered insect repellents are proven safe and effective, even for pregnant and breastfeeding women.
- DEET
- Picaridin (known as KBR 3023 and icaridin outside the US)
- IR3535
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
Find the insect repellent that’s right for you by using EPA’s search tool (https://www.epa.gov/insect-repellents/find-repellent-right-you).
Tips for Everyone
- Always follow the product label instructions.
- Reapply insect repellent as directed.
- Do not spray repellent on the skin under clothing.
- If you are also using sunscreen, apply sunscreen first and insect repellent second.
Tips for Babies & Children
- Always follow instructions when applying insect repellent to children.
- Do NOT use insect repellent on babies younger than 2 months old.
- Do NOT apply insect repellent onto a child’s hands, eyes, mouth, and cut or irritated skin.
- Adults: Spray insect repellent onto your hands and then apply to a child’s face.
- Do NOT use products containing oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD) on children under 3 years old.
Natural insect repellents (repellents not registered with EPA)
- Scientists do not know the effectiveness of non-EPA registered insect repellents, including some natural repellents.
- To protect yourself against diseases spread by mosquitoes, CDC and EPA recommend using an EPA-registered insect repellent.
- Choosing an EPA-registered repellent ensures the EPA has evaluated the product for effectiveness.
Protect your baby or child
- Dress your child in clothing that covers arms and legs.
- Cover crib, stroller, and baby carrier with mosquito netting.
Wear long-sleeved shirts and long pants
- Treat items, such as boots, pants, socks, and tents, with permethrin* or buy permethrin-treated clothing and gear.
- Permethrin-treated clothing will protect you after multiple washings. See product information to find out how long the protection will last.
- If treating items yourself, follow the product instructions.
- Do NOT use permethrin products directly on skin.
*In some places, such as Puerto Rico, where permethrin products have been used for years in mosquito control efforts, mosquitoes have become resistant to it. In areas with high levels of resistance, use of permethrin is not likely to be effective.
Take steps to control mosquitoes inside and outside your home
- Use screens on windows and doors. Repair holes in screens to keep mosquitoes outside.
- Use air conditioning when available.
- Sleep under a mosquito bed net if air conditioned or screened rooms are not available or if sleeping outdoors.
- Once a week, empty and scrub, turn over, cover, or throw out items that hold water, such as tires, buckets, planters, toys, pools, birdbaths, flowerpots, or trash containers. Check inside and outside your home. Mosquitoes lay eggs near water.
Figure 5. Japanese encephalitis virus prevention
Japanese encephalitis vaccine
The best way to prevent Japanese encephalitis is to be vaccinated against the infection before you visit a part of the world where there’s a risk of catching it. The risk is greater if you’re planning to visit rural areas or go hiking or camping.
Japanese encephalitis vaccine, gives protection against Japanese encephalitis in more than 9 out of 10 people who receive it.
Even if you’ve been vaccinated, you should still take precautions to reduce your risk of being bitten by an infected mosquito, such as:
- sleeping in rooms with close-fitting gauze over the windows and doors – if you’re sleeping outside, use mosquito nets that have been impregnated with an insecticide
- covering up with long-sleeved tops, trousers and socks
- applying a good-quality insect repellent to exposed areas of skin
Inactivated Vero cell culture-derived Japanese encephalitis vaccine (manufactured as IXIARO) is the only Japanese encephalitis vaccine licensed and available in the United States. This vaccine was approved in March 2009 for use in people aged 17 years and older and in May 2013 for use in children 2 months through 16 years of age. Other Japanese encephalitis vaccines are manufactured and used in other countries but are not licensed for use in the United States.
IXIARO is given as a two-dose series, with the doses spaced 28 days apart. The last dose should be given at least 1 week before travel. For persons aged 17 years and older, a booster dose may be given if a person has received the two-dose primary vaccination series one year or more previously and there is a continued risk for Japanese encephalitis virus infection or potential for re-exposure. Although studies are being conducted on the need for a booster dose for children, data are not yet available. More information about Japanese encephalitis vaccine – IXIARO product information available at the FDA IXIARO webpage: https://www.fda.gov/biologicsbloodvaccines/vaccines/approvedproducts/ucm179132.htm
Japanese encephalitis Vaccine Recommendations
- Japanese encephalitis vaccine is recommended for travelers who plan to spend 1 month or more in endemic areas during the Japanese encephalitis virus transmission season. This includes long-term travelers, recurrent travelers, or expatriates who will be based in urban areas but are likely to visit endemic rural or agricultural areas during a high-risk period of Japanese encephalitis virus transmission.
- Vaccine should also be considered for the following:
- Short-term (less than1 month) travelers to endemic areas during the transmission season, if they plan to travel outside an urban area and their activities will increase the risk of Japanese encephalitis virus exposure. Examples of higher-risk activities or itineraries include: 1) spending substantial time outdoors in rural or agricultural areas, especially during the evening or night; 2) participating in extensive outdoor activities (such as camping, hiking, trekking, biking, fishing, hunting, or farming); and 3) staying in accommodations without air conditioning, screens, or bed nets.
- Travelers to an area with an ongoing Japanese encephalitis outbreak.
- Travelers to endemic areas who are uncertain of specific destinations, activities, or duration of travel.
- Japanese encephalitis vaccine is not recommended for short-term travelers whose visits will be restricted to urban areas or times outside a well-defined Japanese encephalitis virus transmission season.
Precautions and Contraindications
- A serious allergic reaction after a previous dose of IXIARO is a contraindication to further doses. The vaccine contains protamine sulfate, a compound known to cause allergic reactions in some people.
- No studies of IXIARO in pregnant women have been conducted. Therefore, administration of IXIARO to pregnant women usually should be deferred. However, pregnant women who must travel to an area where risk for infection is high should be vaccinated when the theoretical risk of immunization is outweighed by the risk of infection.
Japanese encephalitis vaccine administration
The primary series for IXIARO is 2 doses administered 28 days apart:
- For adults and children aged ≥3 years, each dose is 0.5 mL.
- For children aged 2 months through 2 years, each dose is 0.25 mL. To administer a 0.25-mL dose, health care providers must expel and discard half of the volume from the 0.5-mL prefilled syringe before injection. To enable this, the manufacturer has developed a prefilled syringe with a red line on the barrel to indicate the 0.25-mL point.
Studies are being conducted on the need for a booster dose for children following a primary series of IXIARO, but data are not yet available.
Japanese encephalitis vaccine side effects
Reactions to Japanese encephalitis vaccine – IXIARO – are generally mild and include pain and tenderness, mild headaches, myalgia (muscle aches), and low-grade fevers.
How long does the Japanese encephalitis vaccination last?
The duration of protection is unknown. For persons aged 17 years and older, a booster dose may be given if the primary two-dose vaccination series was given one year or more previously and there is continued risk of exposure. Although studies are being conducted on the need for a booster dose for children, data are not yet available.
Japanese encephalitis symptoms
Most human infections with Japanese encephalitis virus are asymptomatic; <1% of people infected develop clinical disease. Acute encephalitis is the most commonly recognized clinical manifestation. Milder forms of disease, such as aseptic meningitis or undifferentiated febrile illness, can also occur. Illness usually begins with sudden onset of fever, headache, and vomiting. Mental status changes, focal neurologic deficits, generalized weakness, and movement disorders may develop over the next few days.
- Less than 1% of people infected with Japanese encephalitis virus develop clinical illness.
- In persons who develop symptoms, the incubation period (time from infection until illness) is typically 5-15 days.
- Initial symptoms often include fever, headache, and vomiting.
- Mental status changes, neurologic symptoms, weakness, and movement disorders might develop over the next few days.
- Stiff neck
- Confusion
- Inability to speak
- Uncontrollable shaking of body parts (tremor)
- Muscle weakness or paralysis
- Seizures are common, especially among children.
The classical description of Japanese encephalitis includes a Parkinsonian syndrome with masklike facies, tremor, cogwheel rigidity, and choreoathetoid movements. Acute flaccid paralysis, with clinical and pathological features similar to those of poliomyelitis, has also been associated with Japanese encephalitis. Seizures are common, especially among children. Up to 20%–30% of people who develop these more serious symptoms will die as a result of the infection. Among survivors, 30%–50% have permanent brain damage, significant neurologic or psychiatric sequelae. This can lead to long-term problems such as tremors and muscle twitches, personality changes, muscle weakness, learning difficulties and paralysis in one or more limbs.
Japanese encephalitis diagnosis
Diagnosis is based on a combination of clinical signs and symptoms and specialized laboratory tests of blood or spinal fluid. These tests typically detect antibodies that the immune system makes against the viral infection.
Clinical laboratory findings might include a moderate leukocytosis, mild anemia, and hyponatremia. Cerebrospinal fluid (CSF) typically has a mild to moderate pleocytosis with a lymphocytic predominance, slightly elevated protein, and normal ratio of cerebrospinal fluid (CSF) to plasma glucose. Magnetic resonance imaging (MRI) of the brain is better than computed tomography (CT) for detecting Japanese encephalitis virus-associated abnormalities such as changes in the thalamus, basal ganglia, midbrain, pons, and medulla. Thalamic lesions are the most commonly described abnormality; although these can be highly specific for Japanese encephalitis in the appropriate clinical context, they are not a very sensitive marker of Japanese encephalitis. EEG abnormalities may include theta and delta coma, burst suppression, epileptiform activity, and occasionally alpha coma.
Japanese encephalitis virus infections are confirmed most frequently by detection of virus-specific antibody in cerebrospinal fluid (CSF) or serum. Because humans have low or undetectable levels of viremia by the time distinctive clinical symptoms are recognized, virus isolation and nucleic acid amplification tests are insensitive and should not be used for ruling out a diagnosis of Japanese encephalitis.
Laboratory diagnosis of Japanese encephalitis is generally accomplished by testing of serum or cerebrospinal fluid (CSF) to detect virus-specific IgM antibodies. Japanese encephalitis virus IgM antibodies are usually detectable 3 to 8 days after onset of illness and persist for 30 to 90 days, but longer persistence has been documented. Therefore, positive IgM antibodies occasionally may reflect a past infection or vaccination. Serum collected within 10 days of illness onset may not have detectable IgM, and the test should be repeated on a convalescent sample. For patients with Japanese encephalitis virus IgM antibodies, confirmatory neutralizing antibody testing should be performed. In fatal cases, nucleic acid amplification, histopathology with immunohistochemistry, and virus culture of autopsy tissues can also be useful.
Diagnostic testing for Japanese encephalitis virus IgM antibodies is commercially-available. Confirmatory testing is only available at CDC and a few specialized reference laboratories.
Japanese encephalitis treatment
No specific treatments have been found to benefit patients with Japanese encephalitis, but hospitalization for supportive care and close observation is generally required.
Treatment is symptomatic. Rest, fluids, and use of pain relievers and medication to reduce fever may relieve some symptoms.
- Repellents: Protection against Mosquitoes, Ticks and Other Arthropods. https://www.epa.gov/insect-repellents[↩]