Contents
What is kyphosis
Kyphosis (also called Roundback or Hunchback) is curvature of the spine that causes the top of the back to appear more rounded than normal – this leads to a hunchback or slouching posture.
Usually, kyphosis doesn’t lead to any problems and nothing needs to be done about it. But sometimes it can be serious enough that someone has to wear a back brace or have an operation.
Everyone has some degree of curvature in their spine. However, a curve of more than 45 degrees is considered excessive.
Kyphosis can occur at any age, although it is rare at birth. The prevalence of Kyphosis is estimated to affect 4-8% of the general population. While the prevalence of Kyphosis is generally accepted to be essentially equal in males and females, this finding is debated in literature.
Kyphosis can vary in severity. In general, the greater the curve, the more serious the condition. Milder curves may cause mild back pain or no symptoms at all. More severe curves can cause significant spinal deformity and result in a visible hump on the patient’s back.
A type of kyphosis that occurs in young teens is known as Scheuermann’s disease. It is caused by the wedging together of several bones of the spine (vertebrae) in a row. The cause of this condition is unknown.
In adults, kyphosis can be caused by:
- Degenerative diseases of the spine (such as arthritis or disk degeneration)
- Fractures caused by osteoporosis (osteoporotic compression fractures)
- Injury (trauma)
- Slipping of one vertebra forward on another (spondylolisthesis)
Sometimes kyphosis doesn’t cause any symptoms other than the back appearing abnormally curved or hunched. However, in some cases the condition causes:
- back pain and stiffness
- tenderness of the spine
- tiredness
Back pain can be particularly problematic in adults with kyphosis because the body has to compensate for the spinal abnormality.
If you have severe kyphosis, your symptoms may get worse over time. You may also have difficulty breathing and eating.
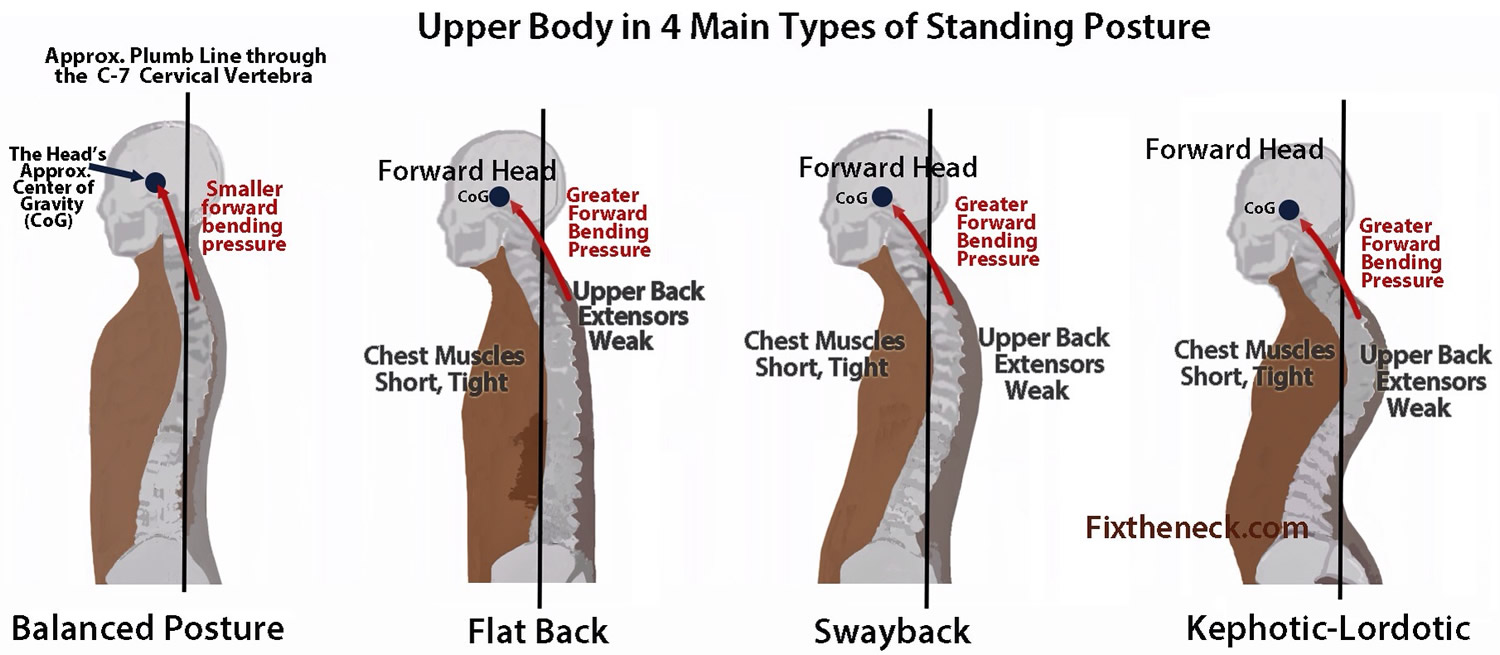
In kyphosis, the normal curve in the middle section of vertebral column (the thoracic vertebrae) is more curved than normal. There are a number of reasons why this might happen, including:
- poor posture (postural kyphosis) – slouching, leaning back in chairs and carrying heavy bags can stretch supporting muscles and ligaments, which can increase spinal curvature
- abnormally shaped vertebrae (Scheuermann’s kyphosis) – if the vertebrae don’t develop properly, they can end up being out of position
- abnormal development of the spine in the womb (congenital kyphosis) – if something disrupts the spine’s normal development, two or more vertebrae sometimes fuse together
- age – as people get older, their spinal curvature can be expected to increase. Age-related kyphosis often occurs after osteoporosis weakens spinal bones to the point that they crack and compress.
Kyphosis can also develop as a result of a spinal injury.
If you have kyphosis, your treatment depends on how curved your spine is, whether you have any additional symptoms such as back pain, and the underlying causes.
Children with kyphosis may be able to be treated using non-surgical methods, such as bracing, to limit the progression of kyphosis as they grow. Treatment for mild kyphosis may not be necessary.
Kyphosis rarely requires surgical treatment. It’s only needed in some severe cases to correct the curvature of the spine.
Spine Anatomy
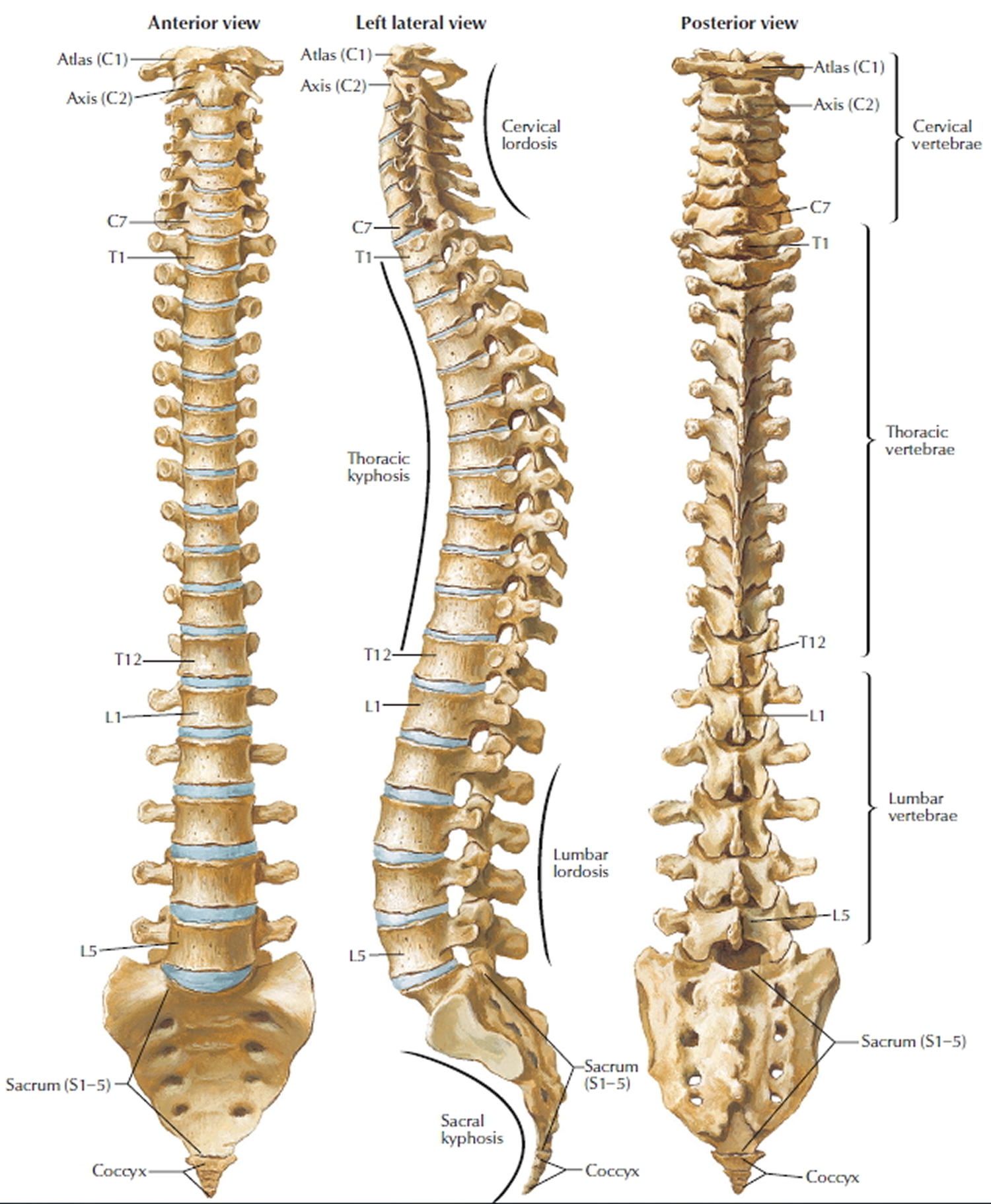
Your spine extends from your skull to your pelvis. It’s made up of 24 individual rectangular-shaped bones called vertebrae, which are stacked on top of one another.
Your spine is made up of three segments. When viewed from the side, these segments form three natural curves.
Although the thoracic spine should have a natural kyphosis between 20 to 45 degrees, postural or structural abnormalities can result in a curve that is outside this normal range.
The “c-shaped” curves of the neck (cervical spine) and lower back (lumbar spine) are called lordosis. The “reverse c-shaped” curve of the chest (thoracic spine) is called kyphosis.
This natural curvature of the spine is important for balance and helps us to stand upright. If any one of the curves becomes too large or too small, it becomes difficult to stand up straight and our posture appears abnormal.
Other parts of your spine include:
- Vertebrae. The spine is made up of 24 small rectangular-shaped bones, called vertebrae, which are stacked on top of one another. These bones create the natural curves of your back and connect to create a canal that protects the spinal cord.
- Intervertebral disks. In between the vertebrae are flexible intervertebral disks. These disks are flat and round and about a half inch thick. Intervertebral disks cushion the vertebrae and act as shock absorbers when you walk or run.
Figure 1. Vertebral column
The vertebrae are separated by soft pads, or discs, which act as shock absorbers. The vertebrae are held together by tough bands of tissue called ligaments. Together with the spinal muscles, the ligaments give the back its strength.
In cases of kyphosis, the middle section of vertebrae, known as the thoracic vertebrae, are curved out of position.
Everyone has some amount of curvature in their spine to allow space inside the chest for organs such as the heart and lungs. There is a range of curvature which is considered normal. However, excessive curvature can lead to symptoms.
There are several reasons why the vertebrae can be affected in this way.
Kyphosis types
There are different types of kyphosis that affect kids, and each has its own cause:
Postural kyphosis
Postural kyphosis is the most common type of kyphosis, usually becomes noticeable during adolescence and it’s rarely a problem. It’s more common among girls than boys, and it happens when bones and muscles develop in an abnormal way as they grow, possibly because of slouching or poor posture. Kids may start to notice this kind of kyphosis as they get closer to being teenagers. The curve caused by postural kyphosis is typically round and smooth and can often be corrected by the patient when he or she is asked to “stand up straight.”
Scheuermann’s kyphosis
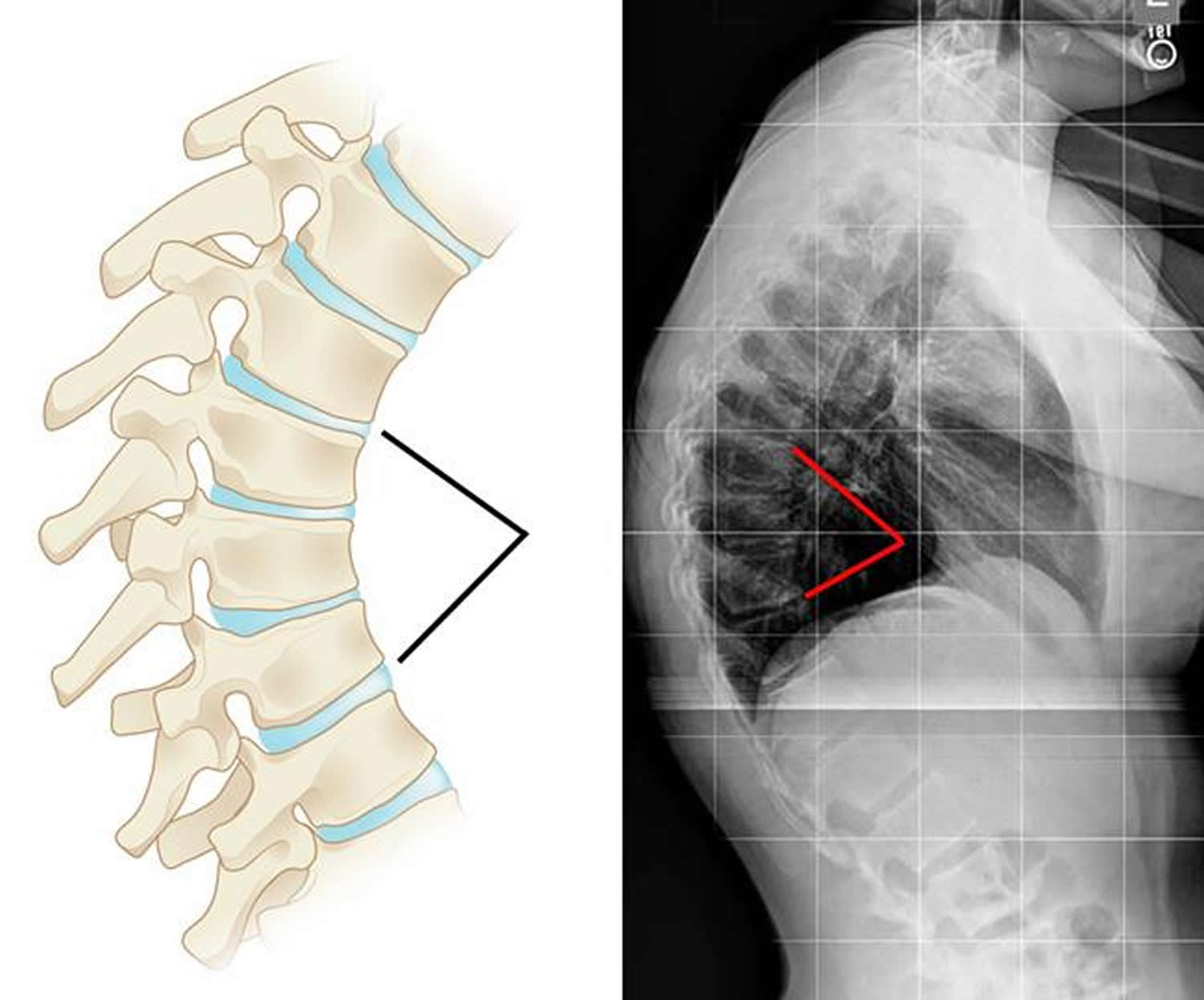
Scheuermann’s kyphosis (named for a Danish radiologist) also usually shows up as you get closer to your teen years. It causes vertebrae to look like wedges instead of rectangles when they’re viewed from the side on X-rays. Scheuermann’s kyphosis is slightly more common among boys than girls and can run in families. Like postural kyphosis, Scheuermann’s kyphosis often becomes apparent during the teen years. However, Scheuermann’s kyphosis can result in a significantly more severe deformity than postural kyphosis—particularly in thin patients.
The curve caused by Scheuermann’s kyphosis is usually sharp and angular. It is also stiff and rigid; unlike a patient with postural kyphosis, a patient with Scheuermann’s kyphosis is not able to correct the curve by standing up straight.
Scheuermann’s kyphosis usually affects the thoracic spine, but occasionally develops in the lumbar (lower) spine. The condition is more common in boys than girls and stops progressing once growing is complete.
Scheuermann’s kyphosis can sometimes be painful. If pain is present, it is commonly felt at the highest part or “apex” of the curve. Pain may also be felt in the lower back. This results when the spine tries to compensate for the rounded upper back by increasing the natural inward curve of the lower back. Activity can make the pain worse, as can long periods of standing or sitting.
Figure 2. Scheuermann’s kyphosis (x-ray show the vertebral wedging that occurs in patients with Scheuermann’s kyphosis)
Congenital kyphosis
Congenital kyphosis happens when the spine develops abnormally while a baby is still in its mother’s womb – congenital kyphosis is present at birth. Several vertebrae can be fused together, or the bones can form improperly.
It occurs when the spinal column fails to develop normally while the baby is in utero. The bones may not form as they should or several vertebrae may be fused together. Congenital kyphosis typically worsens as the child ages.
Patients with congenital kyphosis often need surgical treatment at a very young age to stop progression of the curve. Many times, these patients will have additional birth defects that impact other parts of the body such as the heart and kidneys.
Kyphosis complications
Complications of kyphosis usually only occur in more severe cases. They include:
- Persistent pain that can’t be controlled with medication. In some cases, the misalignment of the spine can lead to pain, which can become severe and disabling.
- Breathing difficulties caused by the spine compressing the lungs and airways
- Decreased appetite. In severe cases, the curve may cause the abdomen to be compressed and lead to decreased appetite.
Occasionally, people with kyphosis can have difficulties when the nerves running through the spine become compressed or pinched. This can disrupt nerve signals and cause symptoms such as:
- numbness or weakness in the arms and legs
- problems with sense of balance
- loss of normal bladder or bowel control
These serious complications require urgent medical attention and surgery would usually be recommended.
Emotional issues
Older children with kyphosis may become concerned or embarrassed about the effect the condition has on their appearance, or having to wear a back brace.
These concerns can affect different children in different ways. Some children can become socially withdrawn and they may be reluctant to take part in activities, such as physical activities, where their condition may be exposed.
There are no easy answers to these problems, but it can sometimes help to reassure your child that their feelings will improve with time.
Kyphosis prognosis (outlook)
Young teens with Scheuermann disease tend to do well, even if they need surgery. The disease stops once they stop growing. If the kyphosis is due to degenerative joint disease or multiple compression fractures, correction of the defect is not possible without surgery, and improvement of pain is less reliable.
If the kyphosis is due to degenerative joint disease or multiple compression fractures, surgery is needed to correct the defect and improve pain.
If kyphosis is diagnosed early, the majority of patients can be treated successfully without surgery and go on to lead active, healthy lives. If left untreated, however, curve progression could potentially lead to problems during adulthood. For patients with kyphosis, regular check-ups are necessary to monitor the condition and check progression of the curve.
Kyphosis causes
Kyphosis may be caused by poor posture during childhood or be the result of abnormally shaped vertebrae or developmental problems with the spine.
Poor posture
Poor posture in childhood, such as slouching, leaning back in chairs and carrying heavy schoolbags, can cause the ligaments and muscles that support the vertebrae to stretch. This can pull the thoracic vertebrae out of their normal position, resulting in kyphosis.
Kyphosis caused by poor posture is known as postural kyphosis.
Abnormally shaped vertebrae
Kyphosis can also be caused when the vertebrae don’t develop correctly. They can take on a wedged, triangular shape, rather than the normal rectangular, box-like shape. This leads to the vertebrae being out of position and is known as Scheuermann’s kyphosis. Scheuermann’s kyphosis typically begins during the growth spurt that occurs before puberty. Boys are affected more often than are girls.
In people with Scheuermann’s kyphosis, the ligaments surrounding the veterbrae can also be thicker than normal, which may contribute further to the condition.
It’s not known what disrupts the normal formation of the spine. One idea is that the blood supply to the vertebrae becomes disrupted, affecting the growth of the vertebrae. There also appears to be a genetic link, as the condition occasionally runs in families.
Congenital kyphosis
Congenital kyphosis is caused when something disrupts the normal development of the spine before birth. In many cases, two or more of the vertebrae fuse together.
It’s often unclear why certain children are affected in this way. However, some cases of congenital kyphosis run in families, so it seems genetics also play a role in this type of kyphosis.
Conditions that cause kyphosis
Conditions that can cause kyphosis include:
- Osteoporosis – where the bones become weak and fragile and more likely to break (fracture)
- Spondylosis – a term that describes the general ‘wear and tear’ that occurs in the bones, discs and ligaments of the spine as a person gets older
- Spina bifida – a birth defect in which the backbone and spinal canal don’t close before birth
- Paget’s disease – a condition in which the development of new bone cells is disrupted, resulting in the bones becoming weak
- Neurofibromatosis – a genetic disorder that affects the nervous system
- Muscular dystrophy – a genetic condition that causes progressive weakening of the muscles
- Tuberculosis – a bacterial infection that mainly affects the lungs
- Cancer that develops inside the spine or spreads to the spine from another part of the body
- Cancer treatments – chemotherapy and radiation cancer treatments
- Connective tissue disorders
- Scoliosis (curving of the spine often looks like a C or S)
- Syndromes. Kyphosis in children can also be associated with certain syndromes, such as Marfan syndrome or Prader-Willi disease.
Kyphosis can also sometimes develop as a result of an injury to the spine.
Risk Factors for kyphosis
In adults, kyphosis can be a result of osteoporotic compression fractures (fractures caused by osteoporosis), degenerative disease (such as arthritis), or spondylolisthesis (slipping of one vertebra forward on another).
Other causes of kyphosis include the following:
- Infection (such as tuberculosis)
- Neurofibromatosis (disorder in which nerve tissue tumors form)
- Connective tissue disorders
- Muscular dystrophy (group of inherited disorders that cause muscle weakness and loss of muscle tissue)
- Spina bifida (a birth defect involving incomplete formation of part of the spine)
- Disk degeneration
- Certain endocrine diseases
- Paget’s disease (disorder that involves abnormal bone destruction and regrowth)
- Polio
- Tumors Kyphosis can also be seen in association with scoliosis (an abnormal sideways curvature of the spine seen in children and adolescents). Risk factors are related to the cause of the Kyphosis.
Kyphosis be prevention
Postural kyphosis can be prevented by being aware of your posture and by taking care of your back. You should encourage your child to:
- avoid slouching
- sit correctly – sit upright, ensuring that the small of the back is supported
- avoid carrying heavy schoolbags that can pull on the back muscles and ligaments; the best schoolbags are well-designed backpacks
- take regular exercise (see below) to help strengthen the back and keep it flexible; activities such as swimming, running, walking, yoga and pilates are ideal for helping to prevent back problems
Treating and preventing osteoporosis can prevent many cases of kyphosis in older adults. Early diagnosis and bracing for Scheuermann disease can reduce the need for surgery, but there is no way to prevent the disease.
Kyphosis symptoms
The signs and symptoms of kyphosis vary, depending upon the cause and severity of the curve. In addition to an abnormally curved spine, kyphosis can also cause back pain and stiffness in some people. Mild cases of kyphosis may produce no noticeable signs or symptoms.
Pain in the middle or lower back is the most common symptom.
Other symptoms may include any of the following:
- Difficulty breathing (in severe cases)
- Fatigue
- Round back appearance
- Tenderness and stiffness in the spine
- Rounded shoulders
- A visible hump on the back
- Mild back pain
- Tight hamstrings (the muscles in the back of the thigh)
Rarely, over time, progressive curves may lead to:
- Weakness, numbness, or tingling in the legs
- Loss of sensation
- Shortness of breath or other breathing difficulties
Kyphosis diagnosis
Kyphosis can usually be diagnosed by examining your spine and taking a spine x-ray. A spine x-ray will be done to document the severity of the curve and allow serial measurements to be performed.
The provider will also look for any nervous system (neurological) changes. These include weakness, paralysis, or changes in sensation below the curve.
Occasionally, pulmonary function tests may be used to assess whether the kyphosis is affecting breathing. And bone density test (if there may be osteoporosis).
Nerve tests: If you are experiencing any numbness or muscle weakness, your doctor may recommend several tests that can determine how well nerve impulses are traveling between your spinal cord and your extremities.
Examination
During the examination, your doctor may ask you to do a number of exercises to assess whether your balance and range of movement are affected.
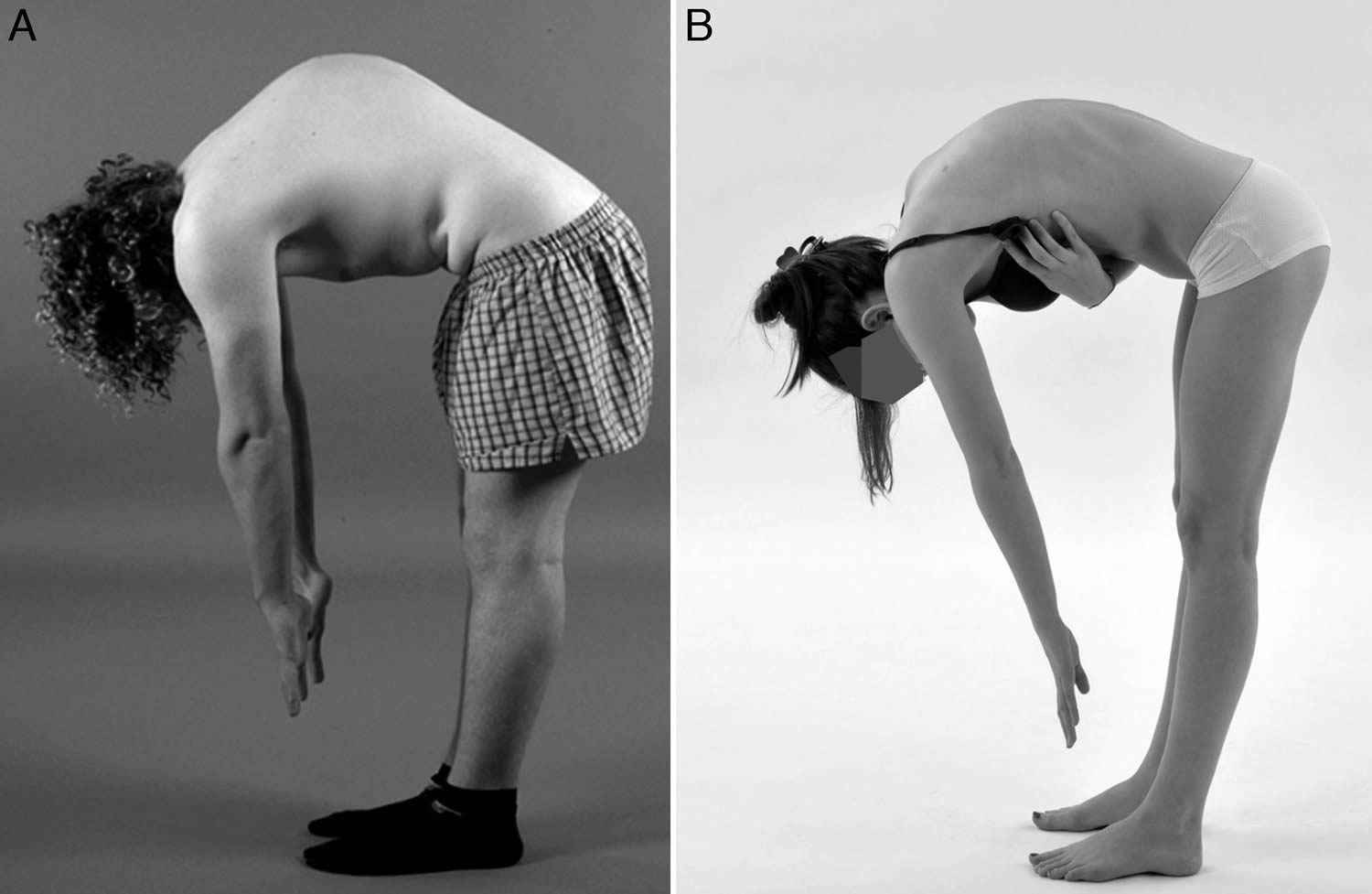
To check for kyphosis, a doctor will examine your spine and might ask you to do an easy test called the forward-bending test. It doesn’t hurt, and all you have to do is bend forward at the waist. Often, kyphosis is easier to see when the back is bent this way.
Figure 3. Forward-bending test
Your doctor may also ask you to lie down so they can see whether the curvature of your spine is caused by bad posture or a structural problem.
Although it’s not always the case, if your spine straightens when you lie down, it’s likely that your kyphosis is caused by poor posture (postural kyphosis).
However, if your spine stills curves while you’re lying down, it’s likely that kyphosis is caused by a problem with the structure of your spine, as found in the Scheuermann’s or congenital types of kyphosis.
X-ray and scans
An X-ray can usually confirm the diagnosis and determine the cause of the kyphosis.
Further scans are usually only required if complex treatment, such as surgery, is being planned, or if you have additional symptoms that suggest your nervous system has been affected, such as numbness in your arms or legs.
If you need additional scans you’ll probably have a:
- computerized tomography (CT) scan – where a series of X-rays are taken to build-up a detailed three-dimensional image of your spine
- magnetic resonance imaging (MRI) scan – where strong, fluctuating magnetic fields are used to produce a detailed image of the inside of your spine
Adults
If you develop kyphosis in adulthood, you’ll usually need some additional tests to determine the underlying cause.
The tests you’ll be referred for depend on any additional symptoms you have. They may include:
- blood tests – which can check for infections such as tuberculosis
- a bone density scan – a type of X-ray to assess how strong your bones are; this can be useful for diagnosing conditions that cause weakening of the bones, such as osteoporosis or Paget’s disease
- CT and MRI scans.
Kyphosis treatment
Most cases of kyphosis don’t require treatment.
Kyphosis caused by poor posture (postural kyphosis) can usually be corrected by improving your posture.
Treatment depends on the cause of the disorder:
- Congenital kyphosis requires corrective surgery at an early age.
- Scheuermann’s disease is initially treated with a brace and physical therapy.
- Occasionally surgery is needed for large (greater than 60 degrees), painful curves.
- Multiple compression fractures from osteoporosis can be left alone if there is no neurologic problems or pain, but the osteoporosis needs to be treated to help prevent future fractures. For debilitating deformity or pain, surgery is an option.
- Kyphosis secondary to infection or tumor needs to be treated more aggressively, often with surgery and medications. Treatment for other types of kyphosis depends on the cause. Surgery may be necessary if neurological symptoms develop.
Compression fractures from osteoporosis can be left alone if there are no nervous system problems or pain. But the osteoporosis needs to be treated to help prevent future fractures. For severe deformity or pain from osteoporosis, surgery is an option.
Kyphosis caused by infection or tumor needs prompt treatment, often with surgery and medicines.
In many older people, kyphosis is the first clue that they have osteoporosis. Bone-strengthening drugs (osteoporosis drugs) may help prevent additional spinal fractures that would cause your kyphosis to worsen.
Treatment for other types of kyphosis depends on the cause. Surgery is needed if nervous system symptoms or constant pain develop.
If a child has kyphosis as a result of abnormally shaped vertebrae (Scheuermann’s kyphosis), treatment depends on factors such as:
- the person’s age
- their sex
- the severity of the curve
- how flexible the curve is
The condition usually stops progressing once a child is older and has stopped growing.
Scheuermann’s disease is treated with a brace and physical therapy. Sometimes surgery is needed for large (greater than 60 degrees), painful curves.
Surgery is often required for children born with congenital kyphosis.
Nonsurgical Treatment
Nonsurgical treatment is recommended for patients with postural kyphosis. It is also recommended for patients with Scheuermann’s kyphosis who have curves of less than 75 degrees.
Nonsurgical treatment may include:
- Observation. Your doctor may recommend simply monitoring the curve to make sure it does not get worse. Your child may be asked to return for periodic visits and x-rays until he or she is fully grown. Unless the curve gets worse or becomes painful, no other treatment may be needed.
- Physical therapy. Specific exercises can help relieve back pain and improve posture by strengthening muscles in the abdomen and back. Certain exercises can also help stretch tight hamstrings and strengthen areas of the body that may be impacted by misalignment of the spine.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs, including aspirin, ibuprofen and naproxen, can help relieve back pain.
- Bracing. Bracing may be recommended for patients with Scheuermann’s kyphosis who are still growing. The specific type of brace and the number of hours per day it should be worn will depend upon the severity of the curve. Your doctor will adjust the brace regularly as the curve improves. Typically, the brace is worn until the child reaches skeletal maturity and growing is complete.
Mild kyphosis
If you have mild to moderate kyphosis, it may be possible to control your symptoms using painkillers and exercise.
Painkillers and exercise
Over-the-counter painkillers, such as ibuprofen or paracetamol, can help relieve any back pain.
Regular exercise and a course of physiotherapy may be recommended to help strengthen the muscles in your back.
Back pain can also be helped by maintaining a healthy weight and activities which strengthen core muscles. For example, yoga, pilates or some martial arts.
Therapy
Some types of kyphosis can be helped by:
- Exercises. Stretching exercises can improve spinal flexibility and relieve back pain. Exercises that strengthen the abdominal muscles may help improve posture.
- Bracing. Children who have Scheuermann’s disease may be able to stop the progression of kyphosis by wearing a body brace while their bones are still growing.
- Healthy lifestyle. Maintaining a healthy body weight and regular physical activity will help prevent back pain and relieve back symptoms from kyphosis.
- Maintaining good bone density. Proper diet with calcium and vitamin D and screening for low bone density, particularly if there is a family history of osteoporosis or history of previous fracture, may help older adults avoid weak bones, compression fractures and subsequent kyphosis.
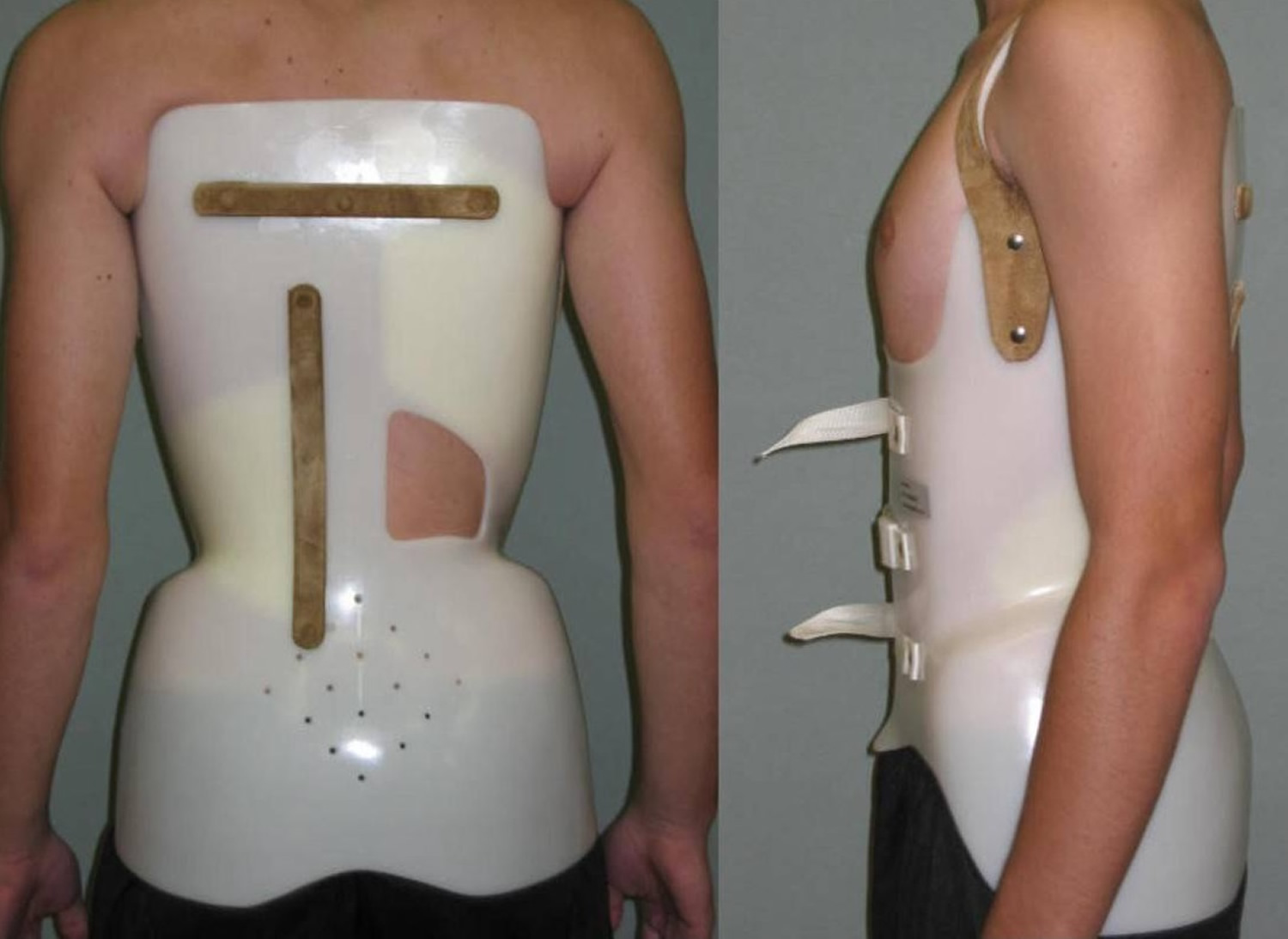
Kyphosis brace
Teenagers with mild to moderate kyphosis may need to wear a back brace. The brace is worn while the bones are still growing and prevents the curve getting worse.
Wearing a brace may feel restrictive at first. However, most people get used to them after a while. Modern braces are designed to be convenient, so it should still be possible to take part in a wide range of physical activities.
You’ll need to wear the brace until the spine stops growing, which is usually around 14 or 15 years old.
Bracing isn’t usually recommended for adults who have stopped growing because it won’t correct the position of the spine.
Figure 4. Kyphosis brace (Lapadula brace)
Surgical Treatment
Surgery is often recommended for patients with congenital kyphosis.
Surgery may also be recommended for:
- Patients with Scheuermann’s kyphosis who have curves greater than 75 degrees
- Patients with severe back pain that does not improve with nonsurgical treatment
Spinal fusion is the surgical procedure most commonly used to treat kyphosis.
The goals of spinal fusion are to:
- Reduce the degree of the curve
- Prevent any further progression
- Maintain the improvement over time
- Alleviate significant back pain, if it is present
Surgery
Surgery can usually correct the appearance of the back and may help to relieve pain but it carries quite a high risk of complications.
Surgery is only recommended for more severe cases of kyphosis, where it’s felt the potential benefits of surgery outweigh the risks.
Surgery for kyphosis would usually be recommended if:
- the curve of your spine is very pronounced
- the curve is causing persistent pain that can’t be controlled with medication
- the curve is disrupting your body’s other important functions, such as breathing and the nervous system
- without surgery it’s likely that the structure of your spine would deteriorate further
Surgical Procedure
Spinal fusion is essentially a “welding” process. The basic idea is to fuse together the affected vertebrae so that they heal into a single, solid bone. Fusing the vertebrae will reduce the degree of the curve and, because it eliminates motion between the affected vertebrae, may also help alleviate back pain.
A technique called spinal fusion is usually used to treat kyphosis. It involves joining together the vertebrae responsible for the curve of the spine.
During the operation, an incision is made in your back. The curve in your spine is straightened using metal rods, screws and hooks, and your spine is fused into place using bone grafts. Bone grafts usually use donated bone but it may taken from another place in your body, such as the pelvis.
Exactly how much of the spine is fused depends upon the size of your child’s curve. Only the curved vertebrae are fused together. The other bones in the spine can still move and assist with bending, straightening, and rotation.
The procedure takes four to eight hours and is carried out under general anesthetic.
You may need to stay in hospital for up to a week after the operation, and you may have to wear a back brace for up to nine months to support your spine while it heals.
You should be able to return to school, college or work after four to six weeks, and be able to play sports about a year after surgery.
Complications
Complications of spinal fusion surgery can include:
- infection after the operation
- excessive bleeding at the site of the surgery
- accidental damage to the nerves that run through the spine, which could result in a paralysis with loss of bladder and bowel function
Before deciding whether to have spinal surgery, you should discuss the benefits and risks with the doctor in charge of your care.