Contents
What is local anesthesia
Local anesthesia is used when pain control (pain relief) is required in small areas (e.g., for repair of minor lacerations, skin biopsies). An anesthetic drug (which can be given as a shot, spray, or ointment) numbs only a small, specific area of the body (for example, a foot, a single tooth, a hand, a toe or a patch of skin). With local anesthesia, a person is awake and comfortable or sedated, depending on what is needed. Local anesthesia lasts for a short period of time and is often used for minor outpatient procedures (when patients come in for surgery and can go home that same day). For someone having outpatient surgery in a clinic or doctor’s office (such as the dentist or dermatologist), this is probably the type of anesthetic used. The medicine used can numb the area during the procedure and for a short time afterwards to help control post-surgery discomfort.
Local anesthesia are often used in dentistry, for eye surgeries such as cataract removal, and to remove small skin growths including warts and moles.
Local cutaneous infiltration is the most commonly used anesthetic technique and involves direct injection into the area requiring anesthesia. The anesthetic solution is infiltrated to the deep dermis, where the sensory plexus supplying the skin begins to branch. The amount of solution used depends on the area that needs to be infiltrated.
Sometimes the local anesthetic agents are applied topically to relieve pain and itching caused by conditions such as sunburn or other minor burns, insect bites or stings, poison ivy, poison oak, poison sumac, and minor cuts and scratches.
Local and topical anesthetics deaden the nerve endings in the skin. They do not cause unconsciousness as do general anesthetics used for surgery.
Furthermore, most topical anesthetics are available without a prescription; however, your doctor may have special instructions on the proper use and dose for your medical problem.
Topical anesthetic product is available in the following dosage forms:
- Spray
- Solution
- Gel/Jelly
- Cream
- Soap
- Pad
- Ointment
- Lotion
- Liquid
- Patch, Extended Release
- Film
- Swab
- Kit
- Dressing
- Patch, Device Assisted
- Foam
- Lozenges
How does local anesthesia work
There are two classes of infiltrative anesthetics, amides and esters, which create a reversible blockade of sodium channels within the nerve fibers by inhibiting sodium influx through sodium-specific ion channels in the neuronal cell membrane, in particular the so-called voltage-gated sodium channels 1. When the influx of sodium is interrupted, an action potential cannot arise and signal conduction is inhibited. The receptor site is thought to be located at the cytoplasmic (inner) portion of the sodium channel. Local anesthetic drugs bind more readily to sodium channels in an activated state, thus onset of neuronal blockade is faster in rapidly firing neurons. This is referred to as state-dependent blockade.
Local anesthetics can block almost every nerve between the peripheral nerve endings and the central nervous system. The most peripheral technique is topical anesthesia to the skin or other body surface. Small and large peripheral nerves can be anesthetized individually (peripheral nerve block) or in anatomic nerve bundles (plexus anesthesia). Spinal anesthesia and epidural anesthesia merge into the central nervous system.
When choosing an anesthetic agent, it is important to consider the type of procedure, the length of time required for anesthesia, and the pharmacodynamics of each medication. Table 1 is an overview of commonly used infiltrative anesthetic agents 2. True allergies to local anesthetics are rare, especially with amide preparations 3. However, evidence suggests there is cross reactivity between agents within the same class 4. In patients with a possible allergy, skin testing should be considered when immunoglobulin E–mediated reactions cannot be ruled out using the history 5.
Local anesthesia drugs
Lidocaine (Xylocaine), an amide, is the most commonly used infiltrative anesthetic and is available in several concentrations 3. For most procedures, a 0.5% or 1% solution is appropriate. Higher concentrations of lidocaine do not improve onset or duration of action and may increase the risk of toxicity 6. Adding epinephrine (concentration of 1:100,000 or 1:200,000) prolongs the duration of anesthesia, increases the maximum dose, and may aid hemostasis 7. Contrary to longstanding belief, the use of lidocaine with epinephrine on the nose, ears, digits, and penis appears to be safe 8, 9. However, many physicians still choose to avoid epinephrine use in these areas. Epinephrine should not be used in patients with peripheral artery disease.
Bupivacaine (Marcaine) is a widely used amide. It has a prolonged duration of action, but this also increases the risk of toxicity (4:1 risk of toxicity compared with lidocaine) and can cause a dose-dependent widening of the QRS interval, leading to ventricular fibrillation 10. Bupivacaine is contraindicated in pregnant women because of the increased bio-availability from decreased venous return 11.
Procaine (Novocain) and tetracaine (Pontocaine) are most often used for dental, topical, spinal, and epidural anesthesia.
Table 1. Commonly Used Infiltrative Anesthetic Agents
| Agent | Concentration | Onset* | Duration* | Maximum dose | |
|---|---|---|---|---|---|
| mg per kg | mL | ||||
Amides | |||||
Lidocaine (Xylocaine) | 0.5%, 1%, or 2%† | Rapid: < 2 minutes | 30 to 60 minutes | 4 (up to 300 mg per dose) | 0.5%: 60 1%: 30 2%: 15 |
Lidocaine with epinephrine‡ | 1% or 2% | Rapid: < 2 minutes§ | 1 to 4 hours | 7 (up to 500 mg per dose) | 1%: 50 2%: 25 |
Bupivacaine (Marcaine) | 0.25% or 0.5% | Slow: 5 minutes | 2 to 4 hours | 2 (up to 175 mg per dose) | 0.25%: 70 0.5%: 35 |
Esters | |||||
Procaine (Novocain) | 1% or 2% | Moderate: 2 to 5 minutes | 15 to 60 minutes | 7 (up to 600 mg per dose) | 1%: 60 2%: 30 |
Tetracaine (Pontocaine) | 0.5% | Slow: 5 to 10 minutes | 2 to 3 hours | 1.4 (up to 120 mg per dose) | 24 |
*—Similar for all concentrations of each agent.
†—Higher concentrations provide no additional anesthetic effects.
‡—Epinephrine concentration may be 1:100,000 or 1:200,000.
§—May take up to 5 minutes for epinephrine to be effective.
Uses of Local anesthetics
Local anesthetics uses include:
- Surface anesthesia is the application of an local anesthetic spray, solution, or cream to the skin or a mucous membrane; the effect is short lasting and is limited to the area of contact.
- Infiltration anesthesia is infiltration of local anesthetic into the tissue to be anesthetized; surface and infiltration anesthesia are collectively topical anesthesia
- Field block is subcutaneous injection of an local anesthetic in an area bordering on the field to be anesthetized.
- Peripheral nerve block is injection of local anesthetic in the vicinity of a peripheral nerve to anesthetize that nerve’s area of innervation.
- Plexus anesthesia is injection of local anesthetic in the vicinity of a nerve plexus, often inside a tissue compartment that limits the diffusion of the drug away from the intended site of action. The anesthetic effect extends to the innervation areas of several or all nerves stemming from the plexus.
- Epidural anesthesia is an local anesthetic injected into the epidural space, where it acts primarily on the spinal nerve roots; depending on the site of injection and the volume injected, the anesthetized area varies from limited areas of the abdomen or chest to large regions of the body.
- Spinal anesthesia is an local anesthetic injected into the cerebrospinal fluid, usually at the lumbar spine (in the lower back), where it acts on spinal nerve roots and part of the spinal cord; the resulting anesthesia usually extends from the legs to the abdomen or chest.
- Intravenous regional anesthesia (Bier’s block) is when blood circulation of a limb is interrupted using a tourniquet (a device similar to a blood-pressure cuff), then a large volume of local anesthetic is injected into a peripheral vein. The drug fills the limb’s venous system and diffuses into tissues, where peripheral nerves and nerve endings are anesthetized. The anesthetic effect is limited to the area that is excluded from blood circulation and resolves quickly once circulation is restored.
- Local anesthesia of body cavities includes intrapleural anesthesia and intra-articular anesthesia.
- Transincision (or transwound) catheter anesthesia uses a multilumen catheter inserted through an insicion or wound and aligned across it on the inside as the incision or wound is closed, providing continuous administration of local anesthetic along the incision or wound.
How local anaesthetics are used
- Treating pain
Slightly painful conditions such as mouth ulcers and sore throats can sometimes be treated with over-the-counter gels and sprays that contain a local anaesthetic.
Injections of a local anaesthetic and steroid medication may be used to treat more severe conditions, such as long-term joint pain.
- Preventing pain during and after surgery
A local anaesthetic may be used along with a sedative medication to keep you relaxed while an operation or procedure is carried out.
Local anaesthetics are mainly used for relatively minor procedures, such as:
- a filling or wisdom tooth removal
- a minor skin operation, such as the removal of moles, warts and verrucas
- some types of eye surgery, such as cataract removal
- a biopsy – where a sample of tissue is removed for closer examination under a microscope
A local anaesthetic may occasionally be used for more major surgery when it’s important for you to be awake, such as during certain types of brain surgery, or to prevent pain after a major operation carried out under a general anaesthetic (see below).
- Epidural and spinal anaesthetics
An epidural anaesthetic, often referred to as an epidural, is where a local anaesthetic is continually injected through a tube into an area of the lower back called the epidural space.
A spinal anaesthetic is a single injection into a similar space in the back.
Both types of anaesthetic can be used to numb large areas of the body by stopping pain signals travelling along the nerves in the spine.
They’re often used during childbirth to ease the pain of labour, or if a caesarean section is needed.
They can also be used to reduce the amount of general anaesthesia needed during some operations and can provide pain relief afterwards. In some types of surgery, such as knee and hip replacements, they can be used in place of a general anaesthetic.
- Peripheral nerve blocks
A nerve block is an injection of a local anaesthetic to numb the nerves supplying a particular part of the body, such as the hand, arm or leg.
It may be used so that an operation can be carried out without needing a general anaesthetic, or to prevent pain afterwards.
An ultrasound scan is often used to pinpoint the correct nerve. The injection shouldn’t be painful and usually takes about 30 minutes to become fully effective.
When peripheral nerve blocks and epidural or spinal anaesthetics are used in place of general anaesthetics, they are often combined with sedation to make you feel drowsy and more relaxed.
Local anaesthesia risks and side effects
Local anaesthetics are generally very safe and serious problems are rare.
You may have some discomfort when the injection is given, a tingling sensation as the medication wears off, and possibly some minor bruising, bleeding or soreness where the injection was given, but you shouldn’t experience any significant side effects.
You should move carefully until the anaesthetic has worn off, as you may not notice if you injured yourself.
Some people experience temporary side effects from a local anaesthetic, such as:
- dizziness
- headaches
- blurred vision
- twitching muscles
- continuing numbness, weakness or pins and needles
These problems will usually pass, but you should tell the healthcare professional in charge of your care if you experience any.
In very rare cases, you could have an allergic reaction to the local anaesthetic or develop serious problems such as seizures (fits) or a cardiac arrest (when the heart stops pumping blood around the body).
Local anesthesia in dentistry
A nerve block is achieved by targeting a specific nerve that supplies sensation to the desired location.
The inferior alveolar nerve, a branch of the mandibular nerve, supplies all of the teeth in one half of the mandible; it is often anesthetized in dental procedures. The same procedure will anesthetize the lower lip because the mental nerve is a branch of the inferior alveolar nerve. Because the lingual nerve runs very close to the inferior alveolar nerve near the mental foramen, it too is often anesthetized at the same time. For anesthesia to the upper teeth, the superior alveolar nerve endings, which are branches of the maxillary nerve, are blocked by inserting the needle beneath the mucous membrane. The anesthetic solution is then infiltrated slowly throughout the area of the roots of the teeth to be treated.
Figure 1. Mandibular nerve (branch of Trigeminal nerve or cranial nerve #5)
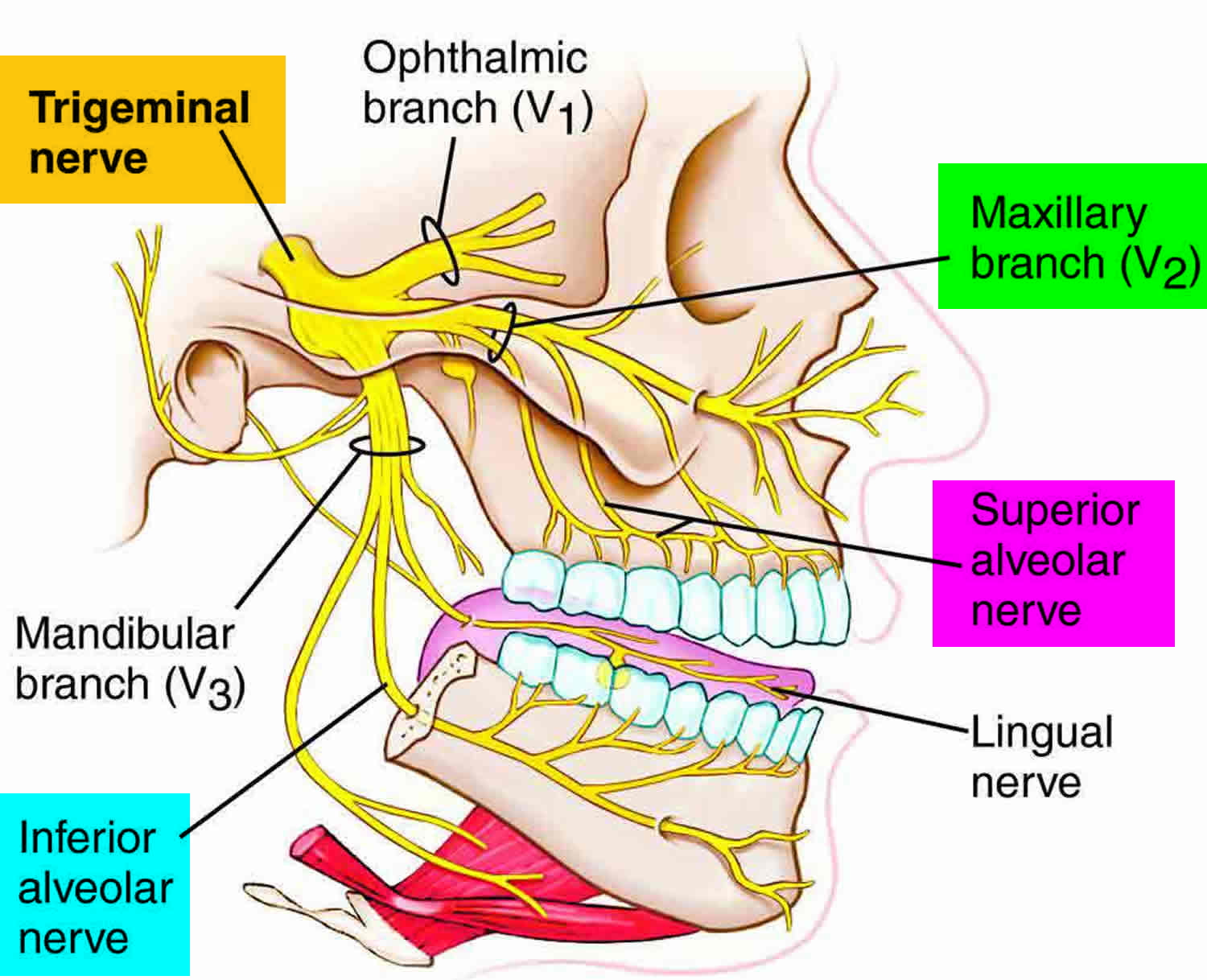
Figure 2. Inferior alveolar nerve block

Figure 3. Superior alveolar nerve block

- Becker DE, Reed KL. Essentials of local anesthetic pharmacology. Anesth Prog. 2006;53(3):98–108.[↩]
- Salam GA. Regional anesthesia for office procedures: part I. Head and neck surgeries. Am Fam Physician. 2004;69(3):585–590.[↩]
- Liu W, Yang X, Li C, Mo A. Adverse drug reactions to local anesthetics: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115(3):319–327.[↩][↩]
- Berkun Y, Ben-Zvi A, Levy Y, Galili D, Shalit M. Evaluation of adverse reactions to local anesthetics: experience with 236 patients. Ann Allergy Asthma Immunol. 2003;91(4):342–345.[↩]
- González-Delgado P, Antón R, Soriano V, Zapater P, Niveiro E. Cross-reactivity among amide-type local anesthetics in a case of allergy to mepivacaine. J Investig Allergol Clin Immunol. 2006;16(5):311–313.[↩]
- Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency Medicine. 5th ed. Philadelphia, Pa.: Saunders/ Elsevier; 2010:490–493.[↩]
- Sinnott CJ, Cogswell LP III, Johnson A, Strichartz GR. On the mechanism by which epinephrine potentiates lidocaine’s peripheral nerve block. Anesthesiology. 2003;98(1):181–188.[↩]
- Lalonde DH, Lalonde JF. Discussion. Do not use epinephrine in digital blocks: myth or truth? Part II. A retrospective review of 1111 cases. Plast Reconstr Surg. 2010;126(6):2035–2036.[↩]
- Muck AE, Bebarta VS, Borys DJ, Morgan DL. Six years of epinephrine digital injections: absence of significant local or systemic effects. Ann Emerg Med. 2010;56(3):270–274.[↩]
- Nath S, Häggmark S, Johansson G, Reiz S. Differential depressant and electrophysiologic cardiotoxicity of local anesthetics: an experimental study with special reference to lidocaine and bupivacaine. Anesth Analg. 1986;65(12):1263–1270.[↩]
- Santos AC, Pedersen H, Harmon TW, et al. Does pregnancy alter the systemic toxicity of local anesthetics? Anesthesiology. 1989;70(6):991–995.[↩]
- Infiltrative Anesthesia in Office Practice. Am Fam Physician. 2014 Jun 15;89(12):956-962. http://www.aafp.org/afp/2014/0615/p956.html[↩]