Contents
- Tacrolimus
- Tacrolimus special precautions
- Tacrolimus mechanism of action
- Tacrolimus uses
- Tacrolimus dosage
- Tacrolimus side effects
- Tacrolimus overdose
Tacrolimus
Tacrolimus also known as Prograf, Astagraf XL, Envarsus XR or FK 506 is an immunosupressant or a drug that weakens your body’s immune system in order to help keep it from “rejecting” a transplanted organ that is used along with other medications to prevent rejection (attack of a transplanted organ by the immune system of a person receiving the organ) in people who have received a heart, kidney, liver, or lung transplant 1, 2. Tacrolimus works by decreasing the activity of your immune system to prevent it from attacking the transplanted organ. Tacrolimus is also sometimes used to treat fistulizing Crohn’s disease (a condition in which the body attacks the lining of the digestive tract, causing pain, diarrhea, weight loss, fever, and the formation of abnormal tunnels connecting the digestive tract to other organs or the skin).
Tacrolimus should be used only by physicians with experience in immunosuppressive therapy and its complications.
Tacrolimus was approved for use in the United States in 1994 and rapidly became an important part of the primary regimen of immunosuppression after allogenic transplantation 3. Tacrolimus current indications are for prevention of organ rejection after transplantation. It is also used off label as therapy of active and recalcitrant forms of autoimmune diseases 3.
Tacrolimus comes as a capsule of 0.5, 1 and 5 mg, granules for oral suspension (to be mixed with liquid), an extended-release (long acting) capsule, and an extended-release tablet to take by mouth. Tacrolimus is also available as a solution for intravenous administration (5 mg/mL). Tacrolimus is also available in topical forms for ophthalmologic and dermatologic conditions, as eye drops, creams ointments and lotions. The immediate-release capsules (Prograf) and oral suspension (Prograf) are usually taken twice a day (12 hours apart). You may take the immediate-release capsules and oral suspension either with or without food, but be sure to take it the same way each time. The extended-release capsules (Astagraf XL) or extended-release tablets (Envarsus XR) are usually taken every morning on an empty stomach at least 1 hour before breakfast or at least 2 hours after breakfast. Take tacrolimus at the same time(s) every day. Because of variability in individual pharmacokinetics of tacrolimus, the maintenance dose varies greatly and proper dosing requires monitoring for drug levels, which is also important because of its many dose dependent side effects and drug-drug interactions. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take tacrolimus exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
If you are taking the granules for oral suspension, you will need to mix it with room temperature water before use. Place 1 to 2 tablespoons (15 to 30 milliliters) of water into a cup containing the granules. Mix the contents and then immediately take the mixture by mouth from the cup or with an oral syringe; do not save the mixture for a later time. The granules will not completely dissolve. If any of the mixture remains, add 1 to 2 tablespoons (15 to 30 milliliters) of water to the mixture and immediately take it.
Swallow the extended-release capsules and extended-release tablets whole with water; do not split, chew, or crush them. Do not open or crush the immediate-release capsules,
Your doctor will monitor you carefully and adjust your dose as needed. Talk to your doctor often about how you are feeling during your treatment. Ask your doctor if you have any questions about how much tacrolimus you should take.
Different tacrolimus products release the medication differently in your body and cannot be used interchangeably. Only take the tacrolimus product prescribed by your doctor and do not switch to a different tacrolimus product unless your doctor says that you should.
Tacrolimus can only prevent rejection of your transplant as long as you are taking the medication. Continue to take tacrolimus even if you feel well. Do not stop taking tacrolimus without talking to your doctor.
Oral and parenteral tacrolimus common side effects include headache, dizziness, paresthesias, neuropathy, hypertension, nephropathy, diabetes, acne, hirsutism and opportunistic infections. Less common but potentially severe adverse events include diabetes, renal failure, hyperkalemia, hypertension, severe neuropathy, blood dyscrasias, microangiopathy and anaphylactic reactions. Talk to your doctor about the risks of using tacrolimus to treat your condition.
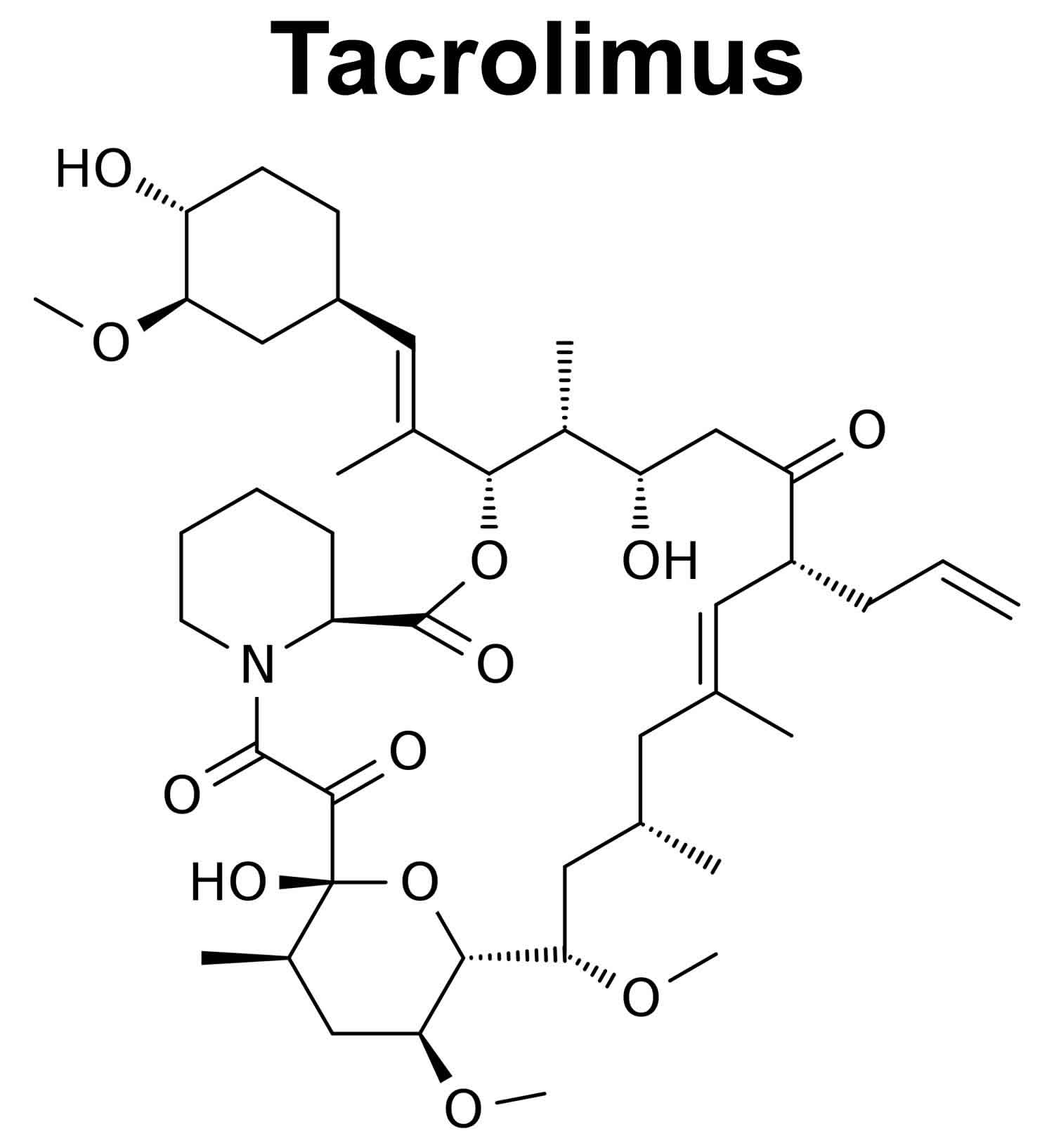
Figure 1. Tacrolimus chemical structure
Tacrolimus should only be given under the supervision of a doctor who is experienced in treating people who have had an organ transplant and in prescribing medications that decrease the activity of the immune system.
Tacrolimus decreases the activity of your immune system. This may increase the risk that you will get a serious infection. If you experience any of the following symptoms, call your doctor immediately: sore throat; cough; fever; extreme tiredness; flu-like symptoms; warm, red, or painful skin; or other signs of infection.
When your immune system is not working normally, there may be a greater risk that you will develop cancer, especially lymphoma (a type of cancer that begins in the cells of the immune system). The longer you take tacrolimus or other medications that decrease the activity of the immune system, and the higher your doses of these medications, the more this risk may increase. If you experience any of the following symptoms of lymphoma, call your doctor immediately: swollen lymph nodes in the neck, armpits, or groin; weight loss; fever; night sweats; excessive tiredness or weakness; cough; trouble breathing; chest pain; or pain, swelling, or fullness in the stomach area.
Studies have shown that women who received a liver transplant and were taking tacrolimus extended-release capsules (Astagraf XL) had an increased risk of death. Tacrolimus extended-release capsules (Astagraf XL) are not approved by the FDA to prevent rejection (attack of a transplanted organ by the immune system of a person receiving the organ) of a liver transplant.
Talk to your doctor about the risks of taking tacrolimus.
Tacrolimus special precautions
Before taking tacrolimus:
- Tacrolimus increases the risk of development of lymphoma and other cancers, particularly of the skin, due to immunosuppression. This may lead to hospitalization or death.
- Tacrolimus increases your risk to bacterial, viral, fungal, and protozoal infections, including opportunistic infections.
- Patients should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources.
- Only physicians experienced in immunosuppressive therapy and management of organ transplant patients should prescribe tacrolimus. The physician responsible for maintenance therapy should have complete information requisite for the follow-up of the patient.
- tell your doctor and pharmacist if you are allergic to tacrolimus, any other medications, or any of the other ingredients in tacrolimus products. Ask your pharmacist or check the Medication Guide for a list of the ingredients.
- tell your doctor and pharmacist what prescription and nonprescription medications, vitamins, and nutritional supplements you are taking or plan to take. Your doctor may need to change the doses of your medications or monitor you more carefully for side effects.
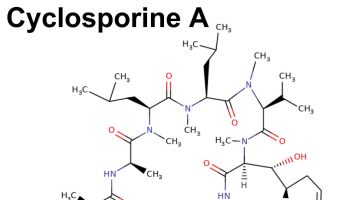
- tell your doctor if you are taking or have recently stopped taking cyclosporine (Gengraf, Neoral, Sandimmune). If you were taking cyclosporine, your doctor will probably tell you not to start taking tacrolimus until 24 hours after you took your last dose of cyclosporine. If you stop taking tacrolimus, your doctor will also tell you to wait 24 hours before starting to take cyclosporine.
The following nonprescription or herbal products may interact with tacrolimus: antacids containing magnesium and aluminum hydroxide (Maalox), cimetidine, lansoprazole (Prevacid 24 HR), omeprazole (Prilosec OTC, Zegerid OTC), St. John’s wort, or Schisandra sphenanthera extracts. Be sure to let your doctor and pharmacist know that you are taking any of these medications before you start taking tacrolimus. Do not start these medications while taking tacrolimus without discussing with your healthcare provider. - tell your doctor if you have or have ever had long QT syndrome (an inherited condition in which a person is more likely to have QT prolongation, an irregular heart rhythm that can lead to fainting, loss of consciousness, seizures, or sudden death) low or high levels of potassium or low levels of calcium or magnesium in your blood, an irregular heartbeat, high cholesterol levels, high blood pressure, cystic fibrosis (an inborn disease that causes the body to produce thick, sticky mucus that may clog the pancreas, the lungs, and other parts of the body), heart, kidney, or liver disease.
- tell your doctor if you are pregnant, plan to become pregnant, or are breast-feeding. If you or your partner are able to become pregnant, use effective birth control before and during treatment with tacrolimus. If you become pregnant while taking tacrolimus, call your doctor. Tacrolimus may harm the fetus.
- if you are having surgery, including dental surgery, tell the doctor or dentist that you are taking tacrolimus.
- you should know that taking tacrolimus may increase the risk that you will develop skin cancer. Protect yourself from skin cancer by avoiding unnecessary or prolonged exposure to sunlight or ultraviolet light (tanning beds) and wearing protective clothing, sunglasses, and sunscreen with a high skin protection factor (SPF).
- do not drink alcoholic beverages while you are taking tacrolimus extended-release capsules or extended-release tablets. Alcohol can make the side effects from tacrolimus worse.
you should know that tacrolimus may cause high blood pressure. Your doctor will monitor your blood pressure carefully, and may prescribe medication to treat high blood pressure if it develops. - you should know that there is a risk that you will develop diabetes during your treatment with tacrolimus. African American and Hispanic patients who have had kidney transplants have an especially high risk of developing diabetes during their treatment with tacrolimus. Tell your doctor if you or anyone in your family has or has ever had diabetes. If you experience any of the following symptoms, call your doctor immediately: excessive thirst; excessive hunger; frequent urination; blurred vision or confusion.
- do not have any vaccinations without talking to your doctor.
Breastfeeding women
Limited data indicate that amounts of systemically administered tacrolimus are low in breastmilk and probably do not adversely affect the breastfed infant 4. United States and European experts and guidelines consider tacrolimus to be probably safe to use during breastfeeding 5, 6, 7, 8, 9, 10, 11, 12, 13. Exclusively breastfed infants should be monitored if this drug is used during lactation, possibly including measurement of serum levels to rule out toxicity if there is a concern.
Topical tacrolimus presents a low risk to the nursing infant because it is poorly absorbed after topical application and peak blood concentrations are less than 2 mcg/L in most patients. Ensure that the infant’s skin does not come into direct contact with the areas of skin that have been treated. Current guidelines allow topical tacrolimus to be applied to the nipples just after nursing, with the nipples cleaned gently before nursing 14, 15. Only water-miscible cream or gel products should be applied to the breast or nipple because ointments may expose the infant to high levels of mineral paraffins via licking, so pimecrolimus cream may be preferable to tacrolimus ointment for nipple application 9.
Tacrolimus contraindications
Contraindications to tacrolimus include:
- Hypersensitivity
- Polyoxyl 60 hydrogenated castor oil (HCO-60) or other components of the formulation.
Tacrolimus drug interactions
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective. Tacrolimus can harm your kidneys, especially if you also use certain medicines for infections, cancer, osteoporosis, organ transplant rejection, bowel disorders, high blood pressure, or pain or arthritis (including Advil, Motrin, and Aleve).
Tell your doctor about all your current medicines. Many drugs can affect tacrolimus, especially:
- amiodarone
- cisplatin
- cyclosporine
- sirolimus
- antibiotic, antifungal, or antiviral medicines
- heart or blood pressure medication, such as a diuretic or “water pill.”
This list is not complete and many other drugs may affect tacrolimus.
Tacrolimus mechanism of action
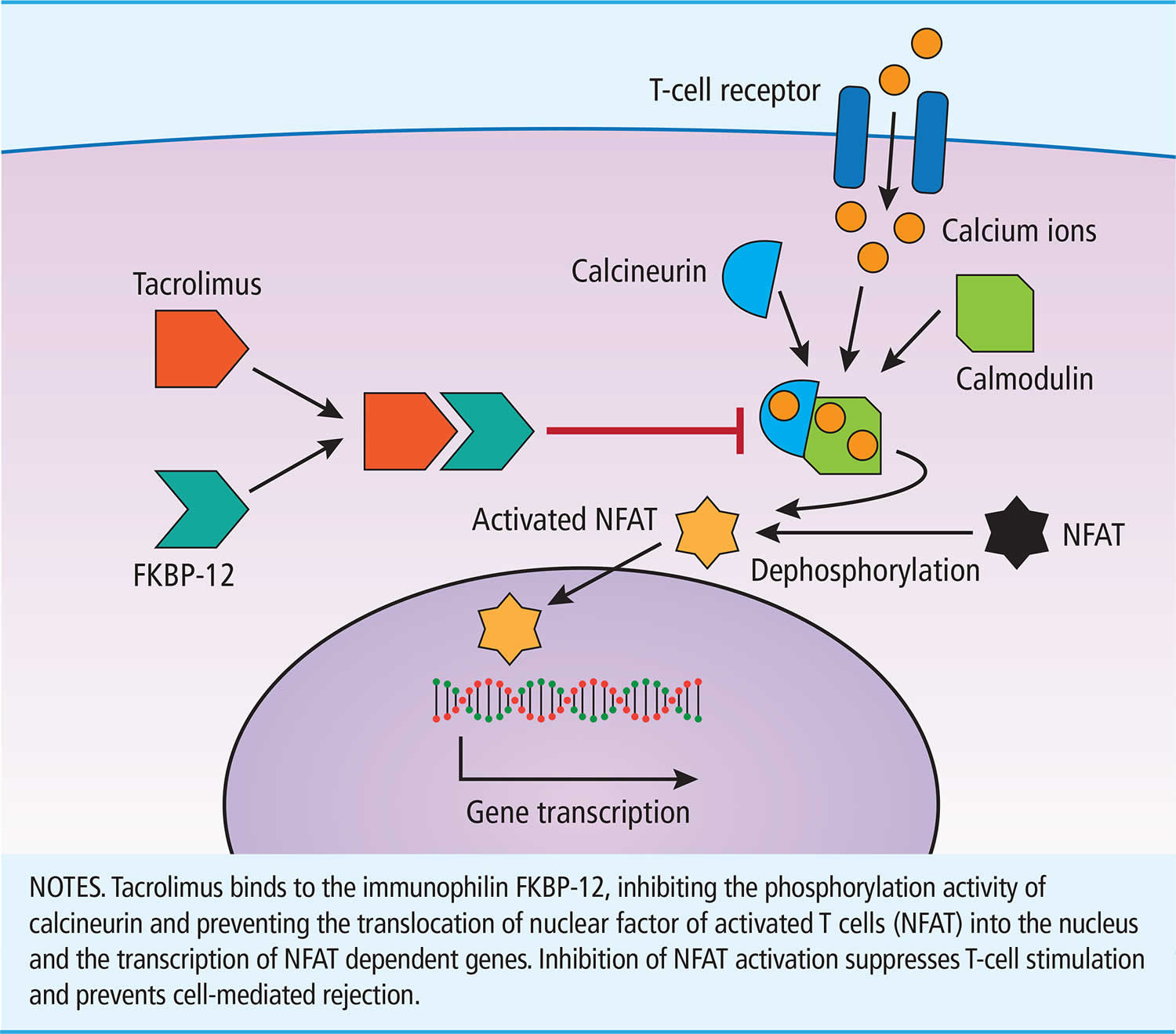
Tacrolimus is a macrolide antibiotic which also has profound immunosuppressive properties, particularly affecting T cells and the cellular immune response. Tacrolimus acts as a calcineurin inhibitor which is responsible for activating an important signal transduction molecule in the pathway of T cell activation. Inhibition of this pathway results in a decrease in maturation of T lymphocytes and reduction in lymphokine production, including interlukin-2 (IL-2) 16, 17. The molecular action of tacrolimus is depicted in Figure 2. Tacrolimus binds to the immunophilin FKBP-12. The resulting molecular complex inhibits the phosphorylation activity of calcineurin therefore preventing the translocation of nuclear factor of activated T cells (NFAT) into the nucleus and the transcription of NFAT-dependent genes. Inhibition of nuclear factor of activated T cells (NFAT) activation thereby suppresses T-cell stimulation and prevents cell-mediated rejection.
Data from in vitro studies suggest that calcineurin is activated by the influx of calcium ions secondary to T-cell receptor binding at the cell surface 16. Calmodulin activity is also essential for calcineurin action. Once activated, calcineurin dephosphorylates nuclear factor of activated T cells (NFAT) triggering its translocation into the nucleus and the transcription of NFAT-dependent genes including cytokines which promote T-cell proliferation.
Following oral administration, tacrolimus acts systemically to inhibit the signaling phosphatase calcineurin 18. By complexing calcineurin with the FK506-binding protein (FKBP12), tacrolimus prevents calcineurin from binding to activated calmodulin and enables the translocation of nuclear factor of activated T cells (NFAT) transcription factors from the cytoplasm to the nucleus 19. The lack of NFAT translocation prevents the transcription of NFAT-regulated proinflammatory cytokine genes in T-cells 20, subsequently blocking T-cell function. Interestingly, the use of calcineurin inhibitors does not appear to affect T-cell production, differentiation, or migration to patient skin, as T cells can be readily detected in the skin of kidney transplant recipients receiving ciclosporine and tacrolimus-based immunosuppression regimens 21.
Studies comparing the action of calcineurin inhibitors have found that tacrolimus has a 100-fold greater in vitro inhibitory activity against T lymphocytes when compared to cyclosporine 16. Furthermore, tacrolimus has been shown to inhibit the transformation of precursor T-helper cells into antigen-conditioned T cells in animal models whereas cyclosporine failed to exert this effect 16.
Figure 2. Tacrolimus mechanism of action
[Source 16 ]Tacrolimus uses
Tacrolimus use is in combination with one or, most commonly, two other immunosuppressive medications. Tacrolimus has an application as an agent for the prevention or treatment of certain autoimmune diseases.
In solid organ transplantation, Tacrolimus serves as the treatment of organ rejection in kidney, liver, and heart allogeneic transplants. There is also an off-label indication for the prevention of rejection in lung transplant patients.
Other off-label indications include:
- Crohn disease
- Graft-versus-host disease (GVHD)
- Myasthenia gravis
- Rheumatoid arthritis
Tacrolimus indications also include topical use in moderate to severe atopic dermatitis, as well as other off-label dermatologic disease states 22.
Tacrolimus administration advice
- Tacrolimus should not be used simultaneously with cyclosporine. Tacrolimus may be initiated at least 24 hours after stopping cyclosporine; however, dosing should be delayed if cyclosporine blood levels are elevated.
- Dosing should be titrated based on clinical assessments of rejection and tolerability, and to maintain recommended trough concentration ranges.
- Patients should not eat grapefruit or drink grapefruit juice with Tacrolimus.
Extended release (ER):
- Should be taken once daily in the morning, preferably on an empty stomach at least 1 hour before or 2 hours after a meal; do not take with an alcoholic beverage; do not chew, divide, or crush.
- Take a missed dose as soon as possible but not more than 14 hours after the scheduled time. Beyond the 14-hour timeframe, the patient should wait until the usual scheduled time the following morning to take the next scheduled dose. Do not take 2 doses at the same time.
General advice:
- The capsule formulation and the oral suspension of Tacrolimus are not interchangeable or substitutable with other tacrolimus extended-release products because the rate of absorption following the administration of an extended-release product is not equivalent to that of an immediate-release product. Under-or overexposure to Tacrolimus may result in graft rejection or other serious adverse reactions.
- The capsule formulation should not be used without supervision of a physician with experience in immunosuppressive therapy.
- Therapeutic drug monitoring is recommended for all patients receiving Tacrolimus.
Tacrolimus dosage
Tacrolimus can administration can be by oral, sublingual, topical, or intravenous (IV) route. Oral tacrolimus is available in immediate-release (IR) and extended-release (ER: XR and XL) formulations. The various formulations have different pharmacokinetic parameters and are not interchangeable 23. Doses should be titrated to target trough concentrations.
Adult Dosing of Post-Organ Transplant Rejection Prevention
Liver Transplant:
- Oral Tacrolimus 24:
- Immediate-release (IR): Initially 0.1 to 0.15 mg/kg/day in two divided doses in combination
- Extended-release (ER: XR and XL): 0.1 to 0.2 mg/kg once daily in combination with corticosteroid. Please note that the XL formulation is not approved for liver transplants in the US due to increased mortality in female liver transplants receiving the XL formulation.
- Intravenous (IV) Tacrolimus: Initially 0.03 to 0.05 mg/kg/day as a continuous infusion
Heart Transplant: In combination with an antimetabolite
- Oral Tacrolimus: Immediate-release (IR) Initially 0.075 mg/kg/day in two divided doses, given every 12 hours
- Intravenous (IV) Tacrolimus: Initially 0.01 mg/kg/day as a continuous infusion
Kidney Transplant: Use in combination with an antimetabolite agent
- Oral Tacrolimus:
- Immediate-release (IR): Initially, 0.2 mg/kg/day in combination with azathioprine or 0.1 mg/kg/day combined with mycophenolate mofetil.
- Extended-release (ER):
- XL tacrolimus: 0.15 to 0.2 mg/kg/day with basiliximab induction; 0.2mg/kg/day without basiliximab induction.
- XR tacrolimus: Initially 0.14 mg/kg/day
- Intravenous (IV) Tacrolimus: 0.03 to 0.05 mg/kg/day as a continuous infusion
IV tacrolimus use is not common due to increased kidney injury adverse effects 25, 26.
Tacrolimus can be administered with or without food but may occur with food in the presence of gastrointestinal intolerance. Immediate-release (IR) doses should be 12 hours apart. Dose rounding should be to a whole number that is feasible with the available strengths. For example, immediate-release (IR) tacrolimus comes in 0.5 mg, 1mg, and 5 mg strengths 27.
When converting from Immediate-release (IR) to Extended-release (ER) formulations, use the following factors 24, 28:
- Immediate-release (IR) to XL: 1 to 1
- Immediate-release (IR) to XR: 1 to 0.8
Sublingual to oral conversion rates have varied from 1 to 1 to 1 to 3, but 1 to 2 has recently been the most commonly suggested in studies. There has been no optimally established dosing 29, 30.
Adult dose Kidney Transplant
Immediate-release (IR) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Immediate-release (IR) in combination with azathioprine: Initial dose: 0.1 mg/kg orally every 12 hours; initiate within 24 hours of surgery but delay until renal function has recovered
- Immediate-release (IR) in combination with mycophenolate mofetil (MMF)/interleukin-2 (IL-2) receptor antagonist: Initial dose: 0.05 mg/kg orally every 12 hours; initiate within 24 hours of surgery, but delay until renal function has recovered
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Extended-release (ER) Tacrolimus
Use: Prevention of organ rejection in patients receiving a kidney transplant with mycophenolate mofetil (MMF) and corticosteroids, with or without basiliximab induction
- Extended-release (ER) with Basiliximab Induction, mycophenolate mofetil (MMF) and Corticosteroids: Initial dose: 0.15 to 0.2 mg/kg/day orally as a single dose. Give first dose prior to or within 48 hours of transplant completion. May delay initiation until renal function has recovered.
- Extended-release (ER) with mycophenolate mofetil (MMF) and Corticosteroids, but Without Basiliximab Induction: Pre-operative dose: 0.1 mg/kg/day orally as a single dose within 12 hours prior to reperfusion; Post-operative dose: 0.2 mg/kg/day orally as a single dose. Give first post-operative dose within 12 hours after reperfusion but not less than 4 hours after the pre-operative dose.
Comments:
- Extended-release capsules are not interchangeable or substitutable with immediate-release capsules.
- Concomitant use with cyclosporine is not recommended.
- If switching from tacrolimus infusion, administer 8 to 12 hours after discontinuing infusion.
Intravenous (IV) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
Intravenous (IV) Tacrolimus initial dose: 0.03 to 0.05 mg/kg/day as a continuous IV infusion
Comments:
- Adult patients should receive doses at the lower end of the dosing range.
- IV administration should be reserved only for initiation in patients unable to take oral therapy.
- Convert to oral therapy as soon as it can be tolerated, usually within 2 to 3 days.
Adult dose Liver Transplant
Immediate-release (IR) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Immediate-release (IR) initial dose: 0.05 to 0.075 mg/kg orally every 12 hours. Initiate no sooner than 6 hours after surgery.
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Intravenous (IV) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Intravenous (IV) Tacrolimus initial dose: 0.03 to 0.05 mg/kg/day as a continuous IV infusion
Comments:
- Adult patients should receive doses at the lower end of the dosing range.
- IV administration should be reserved only for initiation in patients unable to take oral therapy.
- Convert to oral therapy as soon as it can be tolerated, usually within 2 to 3 days.
Adult dose Heart Transplant
Immediate-release (IR) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Immediate-release (IR) initial dose: 0.0375 mg/kg orally every 12 hours. Initiate no sooner than 6 hours after surgery.
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Intravenous (IV) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Intravenous (IV) Tacrolimus initial dose: 0.01 mg/kg/day as a continuous IV infusion
Comments:
- Adult patients should receive doses at the lower end of the dosing range.
- IV administration should be reserved only for initiation in patients unable to take oral therapy.
- Convert to oral therapy as soon as it can be tolerated, usually within 2 to 3 days.
Children dose Liver Transplant
Immediate-release (IR) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Immediate-release (IR) initial dose: 0.075 to 0.1 mg/kg orally every 12 hours
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Intravenous (IV) Tacrolimus
Use: Prevention of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Intravenous (IV) Tacrolimus initial dose: 0.03 to 0.05 mg/kg/day as a continuous IV infusion
Comments:
- Children without pre-existing renal or hepatic dysfunction have required and tolerated higher doses than adults to achieve similar blood concentrations.
- IV administration should be reserved only for initiation in patients unable to take oral therapy.
- Convert to oral therapy as soon as it can be tolerated, usually within 2 to 3 days.
Liver impairment Dose Adjustments
Severe liver impairment (Child-Pugh 10 or greater): May require lower tacrolimus doses.
Liver transplant:
- Patients experiencing post-transplant liver impairment may be associated with an increased risk of developing renal insufficiency related to high blood levels of this drug. Monitor closely and consider dose adjustments.
Kidney impairment Dose Adjustments
Kidney transplant
- Immediate-release (IR) initial dose: 0.15 mg/kg orally every 12 hours; initiate within 24 hours of surgery but delay until renal function has recovered
- Immediate-release (IR) in combination with mycophenolate mofetil (MMF)/interleukin-2 (IL-2) receptor antagonist: Initial dose 0.05 mg/kg orally every 12 hours; initiate within 24 hours of surgery, but delay until renal function has recovered
Liver transplant
- Immediate-release (IR) initial dose: 0.075 to 0.1 mg/kg orally every 12 hours
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Use:
Prophylaxis of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
Heart transplant
- Immediate-release (IR) initial dose: 0.15 mg/kg orally every 12 hours
Comments:
Should be taken consistently either with or without food because the presence and composition of food decreases the bioavailability.
Use:
Prophylaxis of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
- Intravenous (IV) Tacrolimus initial dose: 0.03 to 0.05 mg/kg/day as a continuous IV infusion
Comments:
- Children in general need higher doses compared to adults; the higher dose requirements may decrease as the child grows older.
- Children without pre-existing renal or hepatic dysfunction have required and tolerated higher doses than adults to achieve similar blood concentrations.
- IV administration should be reserved only for initiation in patients unable to take oral therapy.
- Convert to oral therapy as soon as it can be tolerated, usually within 2 to 3 days.
Use:
Prophylaxis of organ rejection in patients receiving allogeneic liver, kidney or heart transplants; use concomitantly with adrenal corticosteroids; in kidney and heart transplant, use in conjunction with azathioprine or mycophenolate mofetil (MMF).
Tacrolimus monitoring
Tacrolimus is a narrow therapeutic index drug. Therapeutic monitoring of tacrolimus in transplant patients is a valuable tool in adjusting drug levels 1, 31. Since tacrolimus use is typically in combination with other immunosuppressants, target levels usually decrease as post-transplant time increases to minimize calcineurin inhibitor-mediated nephrotoxicity and adverse effects 32. Whole blood concentrations should be used, drawn typically within 30 minutes before the next dose. Therapeutic levels range from 5 to 20 mcg/mL, though 5 to 15 mcg/mL is often employed to alleviate toxicity while preventing rejection.
Additional monitoring parameters include renal function, hepatic function, serum electrolytes (magnesium, phosphorus, potassium), glucose, and blood pressure. Parameters should initially be measured two to three times a week post-operatively, gradually decreasing as time passes, achieving target levels, and patient stabilization.
The following are recommendations for tacrolimus level ranges per British Columbia Transplant Guidelines (http://www.transplant.bc.ca/health-professionals/transplant-resources/transplant-clinical-guidelines). However, target levels vary by institution, induction protocols, and patient needs.
Adult and Children Kidney/Pancreas Transplant
- Less than 1 month: 8 to 12 ng/mL
- From 1 to 3 months: 6 to 9 ng/mL
- Greater than 3 months: 4 to 8 ng/mL
Adult Liver Transplant
- Less than 1 month: 6 to 9 ng/mL
- From 1 to 3 months: 4 to 8 ng/mL
- Greater than 3 months: 4 to 6 ng/mL
- More than 12 months: 3 to 5 ng/mL
Adult Heart Transplant
- Less than 3 months: 9 to 12 ng/mL
- From 3 to 6 months: 8 to 9 ng/mL
- From 6 to 12 months: 6 to 8 ng/mL
- Over 12 months: 4 to 8 ng/mL
Adult Lung Transplant
- From 0 to 3 months: 10 to 12 ng/mL
- From 4 to 12 months: 8 to 10 ng/mL
- More than 12 months: 6 to 8 ng/mL
- Due to the metabolism pathway of tacrolimus, many drug-drug interactions exist. If starting medications that inhibit or induce the metabolism of tacrolimus, added monitoring is suggested to prevent a supra or sub-therapeutic level.
What should I do if I forget a dose?
If the immediate-release capsule or oral suspension dose is missed, take it as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
If the extended-release capsule dose is missed, take the dose if it is within 14 hours after missing the dose. However, if it is more than 14 hours, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
If the extended-release tablet dose is missed, take the dose it if it is within 15 hours after missing the dose. However, if it is more than 15 hours, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
Tacrolimus side effects
Tacrolimus may cause side effects. See your doctor if any of these symptoms are severe or do not go away:
- headache
- diarrhea
- constipation
- nausea
- vomiting
- heartburn
- stomach pain
- difficulty falling asleep or staying asleep
- dizziness
- weakness
- back or joint pain
- burning, numbness, pain, or tingling in the hands or feet
Some side effects can be serious. If you experience any of the following symptoms, or those mentioned in the IMPORTANT WARNING section, see your doctor immediately:
- decreased urination
- pain or burning on urination
- shortness of breath, hives, rash, or itching
- pale skin, shortness of breath, or fast heartbeat
- tiredness; weight gain; swelling of the arms, hands, feet, ankles, or lower legs; or shortness of breath
- unusual bleeding or bruising
- seizures, vision changes, headache, confusion, or uncontrollable shaking of a part of the body
- coma (loss of consciousness for a period of time)
- pinpoint-sized purple dots under the skin, bruising, fever, tiredness, sleepiness, confusion, yellowing of skin or eyes (jaundice), or decreased urination
Additional serious adverse effects include, but are not limited to 33, 34:
- Cardiovascular: Angina pectoris, cardiac arrhythmias, hypertension
- Central nervous system: Abnormal dreams, headaches, insomnia, tremors
- Dermatologic: Acne vulgaris, alopecia, pruritis, rash
- Endocrine and metabolic: Decreased serum bicarbonate, decreased serum iron, new-onset diabetes mellitus after transplant (NODAT), hypercalcemia, hyperkalemia, hyperlipidemia, hyperphosphatemia, hypertriglyceridemia, hyperuricemia, hypervolemia, hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia, hypophosphatemia, metabolic acidosis, weight gain
- Gastrointestinal: Abdominal pain, nausea, vomiting, diarrhea
- Genitourinary: Urinary tract infection
- Liver: Abnormal hepatic function tests
- Infection: Bacterial infection, BK virus, candidiasis, cytomegalovirus, Epstein-Barr infection, herpes simplex infection, herpes zoster infection, other opportunistic infection
- Neuromuscular and skeletal: Arthralgia, muscle cramps
- Ophthalmic: Blurred vision, visual disturbance
- Otic: Otalgia, otitis media, tinnitus
- Kidney: Acute renal failure, increased blood urea nitrogen (BUN), increase serum creatinine (SCr), renal failure syndrome, renal tubular necrosis, decreased GFR, nephrotoxicity
Tacrolimus may cause other side effects. Call your doctor if you have any unusual problems while you are taking tacrolimus.
Tacrolimus overdose
Tacrolimus overdose symptoms may include:
- hives
- sleepiness
- nausea, vomiting, and diarrhea
- uncontrollable shaking of a part of the body, headache, confusion, imbalance, and extreme tiredness
- swelling of arms or legs
- fever or other signs of infection
Tacrolimus overdose and toxicity commonly presents as acute renal failure. Close monitoring of serum creatinine, GFR, and urine output is necessary for patients on tacrolimus.
Tacrolimus toxicity may also present as the development of adverse effects such as tremors, electrolyte disturbances, headaches, and increased SCr.
No antidote exists currently to counter Tacrolimus toxicity 23. Hemodialysis does not remove tacrolimus 23.
- Brunet M., Van Gelder T., Åsberg A., Haufroid V., Hesselink D.A., Langman L., Lemaitre F., Marquet P., Seger C., Shipkova M., et al. Therapeutic Drug Monitoring of Tacrolimus-Personalized Therapy: Second Consensus Report. Ther. Drug Monit. 2019;41:261–307. doi: 10.1097/FTD.0000000000000640[↩][↩]
- Brunet M, Pastor-Anglada M. Insights into the Pharmacogenetics of Tacrolimus Pharmacokinetics and Pharmacodynamics. Pharmaceutics. 2022 Aug 23;14(9):1755. doi: 10.3390/pharmaceutics14091755[↩]
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Tacrolimus. [Updated 2020 Feb 17]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548545[↩][↩]
- Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-. Tacrolimus. [Updated 2023 Nov 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK501104[↩]
- van der Woude CJ, Ardizzone S, Bengtson MB, Fiorino G, Fraser G, Katsanos K, Kolacek S, Juillerat P, Mulders AG, Pedersen N, Selinger C, Sebastian S, Sturm A, Zelinkova Z, Magro F; European Crohn’s and Colitis Organization. The second European evidenced-based consensus on reproduction and pregnancy in inflammatory bowel disease. J Crohns Colitis. 2015 Feb;9(2):107-24. doi: 10.1093/ecco-jcc/jju006[↩]
- Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse MEB, Lockshin MD, Marder W, Guyatt G, Branch DW, Buyon J, Christopher-Stine L, Crow-Hercher R, Cush J, Druzin M, Kavanaugh A, Laskin CA, Plante L, Salmon J, Simard J, Somers EC, Steen V, Tedeschi SK, Vinet E, White CW, Yazdany J, Barbhaiya M, Bettendorf B, Eudy A, Jayatilleke A, Shah AA, Sullivan N, Tarter LL, Birru Talabi M, Turgunbaev M, Turner A, D’Anci KE. 2020 American College of Rheumatology Guideline for the Management of Reproductive Health in Rheumatic and Musculoskeletal Diseases. Arthritis Rheumatol. 2020 Apr;72(4):529-556. doi: 10.1002/art.41191[↩]
- Zheng S, Easterling TR, Hays K, Umans JG, Miodovnik M, Clark S, Calamia JC, Thummel KE, Shen DD, Davis CL, Hebert MF. Tacrolimus placental transfer at delivery and neonatal exposure through breast milk. Br J Clin Pharmacol. 2013 Dec;76(6):988-96. doi: 10.1111/bcp.12122[↩]
- Armenti VT, Moritz MJ, Davison JM. Breastfeeding and tacrolimus: is it a reasonable approach? Expert Rev Clin Immunol. 2013 Jul;9(7):623-6. doi: 10.1586/1744666X.2013.811042[↩]
- Thiagarajan KM, Arakali SR, Mealey KJ, Cardonick EH, Gaughan WJ, Davison JM, Moritz MJ, Armenti VT. Safety considerations: breastfeeding after transplant. Prog Transplant. 2013 Jun;23(2):137-46. doi: 10.7182/pit2013803[↩][↩]
- Constantinescu S, Pai A, Coscia LA, Davison JM, Moritz MJ, Armenti VT. Breast-feeding after transplantation. Best Pract Res Clin Obstet Gynaecol. 2014 Nov;28(8):1163-73. doi: 10.1016/j.bpobgyn.2014.09.001[↩]
- Flint J, Panchal S, Hurrell A, van de Venne M, Gayed M, Schreiber K, Arthanari S, Cunningham J, Flanders L, Moore L, Crossley A, Purushotham N, Desai A, Piper M, Nisar M, Khamashta M, Williams D, Gordon C, Giles I; BSR and BHPR Standards, Guidelines and Audit Working Group. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding-Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford). 2016 Sep;55(9):1693-7. doi: 10.1093/rheumatology/kev404[↩]
- Götestam Skorpen C, Hoeltzenbein M, Tincani A, Fischer-Betz R, Elefant E, Chambers C, da Silva J, Nelson-Piercy C, Cetin I, Costedoat-Chalumeau N, Dolhain R, Förger F, Khamashta M, Ruiz-Irastorza G, Zink A, Vencovsky J, Cutolo M, Caeyers N, Zumbühl C, Østensen M. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis. 2016 May;75(5):795-810. doi: 10.1136/annrheumdis-2015-208840[↩]
- Russell MD, Dey M, Flint J, Davie P, Allen A, Crossley A, Frishman M, Gayed M, Hodson K, Khamashta M, Moore L, Panchal S, Piper M, Reid C, Saxby K, Schreiber K, Senvar N, Tosounidou S, van de Venne M, Warburton L, Williams D, Yee CS, Gordon C, Giles I; BSR Standards, Audit and Guidelines Working Group. British Society for Rheumatology guideline on prescribing drugs in pregnancy and breastfeeding: immunomodulatory anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford). 2023 Apr 3;62(4):e48-e88. doi: 10.1093/rheumatology/keac551. Erratum in: Rheumatology (Oxford). 2022 Dec 13[↩]
- Vestergaard C, Wollenberg A, Barbarot S, Christen-Zaech S, Deleuran M, Spuls P, Flohr C, Trzeciak M, von Kobyletzki L, Seneschal J, Paul C, Bieber T, Werfel T, Fölster-Holst R, Darsow U, Gieler U, Svensson Å, Cork M, Stalder JF, De Raeve L, Kunz B, Simon D, Chernyshov P, Hijnen D, Gelmetti C, Ring J, Taieb A, de Bruin-Weller M, Thyssen JP. European task force on atopic dermatitis position paper: treatment of parental atopic dermatitis during preconception, pregnancy and lactation period. J Eur Acad Dermatol Venereol. 2019 Sep;33(9):1644-1659. doi: 10.1111/jdv.15709[↩]
- Deleuran M, Dézfoulian B, Elberling J, Knutar I, Lapeere H, Lossius AH, Schuttelaar MLA, Stockman A, Wikström E, Bradley M, de Bruin-Weller M, Gutermuth J, Mandelin JM, Schmidt MC, Thyssen JP, Vestergaard C. Systemic anti-inflammatory treatment of atopic dermatitis during conception, pregnancy and breastfeeding: Interdisciplinary expert consensus in Northern Europe. J Eur Acad Dermatol Venereol. 2024 Jan;38(1):31-41. doi: 10.1111/jdv.19512[↩]
- Biddle, K. and Ahmed, S.H. (2019), Tacrolimus. Pract Diab, 36: 33-35. https://doi.org/10.1002/pdi.2209[↩][↩][↩][↩][↩]
- Thomson AW, Bonham CA, Zeevi A. Mode of action of tacrolimus (FK506): molecular and cellular mechanisms. Ther Drug Monit. 1995 Dec;17(6):584-91. doi: 10.1097/00007691-199512000-00007[↩]
- Veitch M, Beaumont K, Pouwer R, Chew HY, Frazer IH, Soyer HP, Campbell S, Dymock BW, Harvey A, Cock TA, Wells JW. Local blockade of tacrolimus promotes T-cell-mediated tumor regression in systemically immunosuppressed hosts. J Immunother Cancer. 2023 Sep;11(9):e006783. doi: 10.1136/jitc-2023-006783[↩]
- Vaeth M, Feske S. NFAT control of immune function: New Frontiers for an Abiding Trooper. F1000Res. 2018 Mar 2;7:260. doi: 10.12688/f1000research.13426.1[↩]
- Bremer S, Vethe NT, Skauby M, et al.. NFAT-regulated cytokine gene expression during tacrolimus therapy early after renal transplantation. Br J Clin Pharmacol 2017;83:2494–502. 10.1111/bcp.13367[↩]
- Burke MT, Sambira Nahum LC, Isbel NM, et al.. Sirolimus increases T-cell abundance in the sun exposed skin of kidney transplant recipients. Transplant Direct 2017;3:e171. 10.1097/TXD.0000000000000694[↩]
- Ruzicka T, Assmann T, Lebwohl M. Potential future dermatological indications for tacrolimus ointment. Eur J Dermatol. 2003 Jul-Aug;13(4):331-42.[↩]
- Araya AA, Tasnif Y. Tacrolimus. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544318[↩][↩][↩]
- Patel N, Cook A, Greenhalgh E, Rech MA, Rusinak J, Heinrich L. Overview of extended release tacrolimus in solid organ transplantation. World J Transplant. 2016 Mar 24;6(1):144-54. doi: 10.5500/wjt.v6.i1.144[↩][↩]
- Nicolai S, Bunyavanich S. Hypersensitivity reaction to intravenous but not oral tacrolimus. Transplantation. 2012 Nov 15;94(9):e61-3. doi: 10.1097/TP.0b013e31826e5995[↩]
- Takamatsu Y, Ishizu M, Ichinose I, Ogata K, Onoue M, Kumagawa M, Suzumiya J, Tamura K. Intravenous cyclosporine and tacrolimus caused anaphylaxis but oral cyclosporine capsules were tolerated in an allogeneic bone marrow transplant recipient. Bone Marrow Transplant. 2001 Aug;28(4):421-3. doi: 10.1038/sj.bmt.1703161[↩]
- Bekersky I, Dressler D, Mekki Q. Effect of time of meal consumption on bioavailability of a single oral 5 mg tacrolimus dose. J Clin Pharmacol. 2001 Mar;41(3):289-97. doi: 10.1177/00912700122010104[↩]
- Philosophe B, Leca N, West-Thielke PM, Horwedel T, Culkin-Gemmell C, Kistler K, Stevens DR. Evaluation of Flexible Tacrolimus Drug Concentration Monitoring Approach in Patients Receiving Extended-Release Once-Daily Tacrolimus Tablets. J Clin Pharmacol. 2018 Jul;58(7):891-896. doi: 10.1002/jcph.1082[↩]
- Doligalski CT, Liu EC, Sammons CM, Silverman A, Logan AT. Sublingual administration of tacrolimus: current trends and available evidence. Pharmacotherapy. 2014 Nov;34(11):1209-19. doi: 10.1002/phar.1492[↩]
- Romero I, Jiménez C, Gil F, Escuin F, Ramirez E, Fudio S, Borobia A, Carcas A. Sublingual administration of tacrolimus in a renal transplant patient. J Clin Pharm Ther. 2008 Feb;33(1):87-9. doi: 10.1111/j.1365-2710.2008.00884.x[↩]
- Degraeve A.L., Moudio S., Haufroid V., Chaib Eddour D., Mourad M., Bindels L.B., Elens L. Predictors of tacrolimus pharmacokinetic variability: Current evidences and future perspectives. Expert Opin. Drug Metab. Toxicol. 2020;16:769–782. doi: 10.1080/17425255.2020.1803277[↩]
- Nankivell BJ, PʼNg CH, OʼConnell PJ, Chapman JR. Calcineurin Inhibitor Nephrotoxicity Through the Lens of Longitudinal Histology: Comparison of Cyclosporine and Tacrolimus Eras. Transplantation. 2016 Aug;100(8):1723-31. doi: 10.1097/TP.0000000000001243[↩]
- Randomised trial comparing tacrolimus (FK506) and cyclosporin in prevention of liver allograft rejection. European FK506 Multicentre Liver Study Group. Lancet. 1994 Aug 13;344(8920):423-8. https://doi.org/10.1016/S0140-6736(94)91766-3[↩]
- Pham PT, Pham PM, Pham SV, Pham PA, Pham PC. New onset diabetes after transplantation (NODAT): an overview. Diabetes Metab Syndr Obes. 2011;4:175-86. doi: 10.2147/DMSO.S19027[↩]