Contents
What is a lumbar puncture
A lumbar puncture also called a spinal tap, is a common medical test where a spinal needle is advanced between two lumbar bones (vertebrae) into the subarachnoid space in your lower back in order to collect a small sample of cerebrospinal fluid (CSF) for examination. Lumbar puncture procedure is done to measure pressures within the CSF and to collect a sample of the cerebrospinal fluid (CSF) for further testing. Cerebral spinal fluid (CSF) is a clear, colorless liquid that delivers nutrients and “cushions” the brain and spinal cord, or central nervous system.
In a lumbar puncture, a needle is carefully inserted into the lower spine to collect the cerebrospinal fluid (CSF) sample.
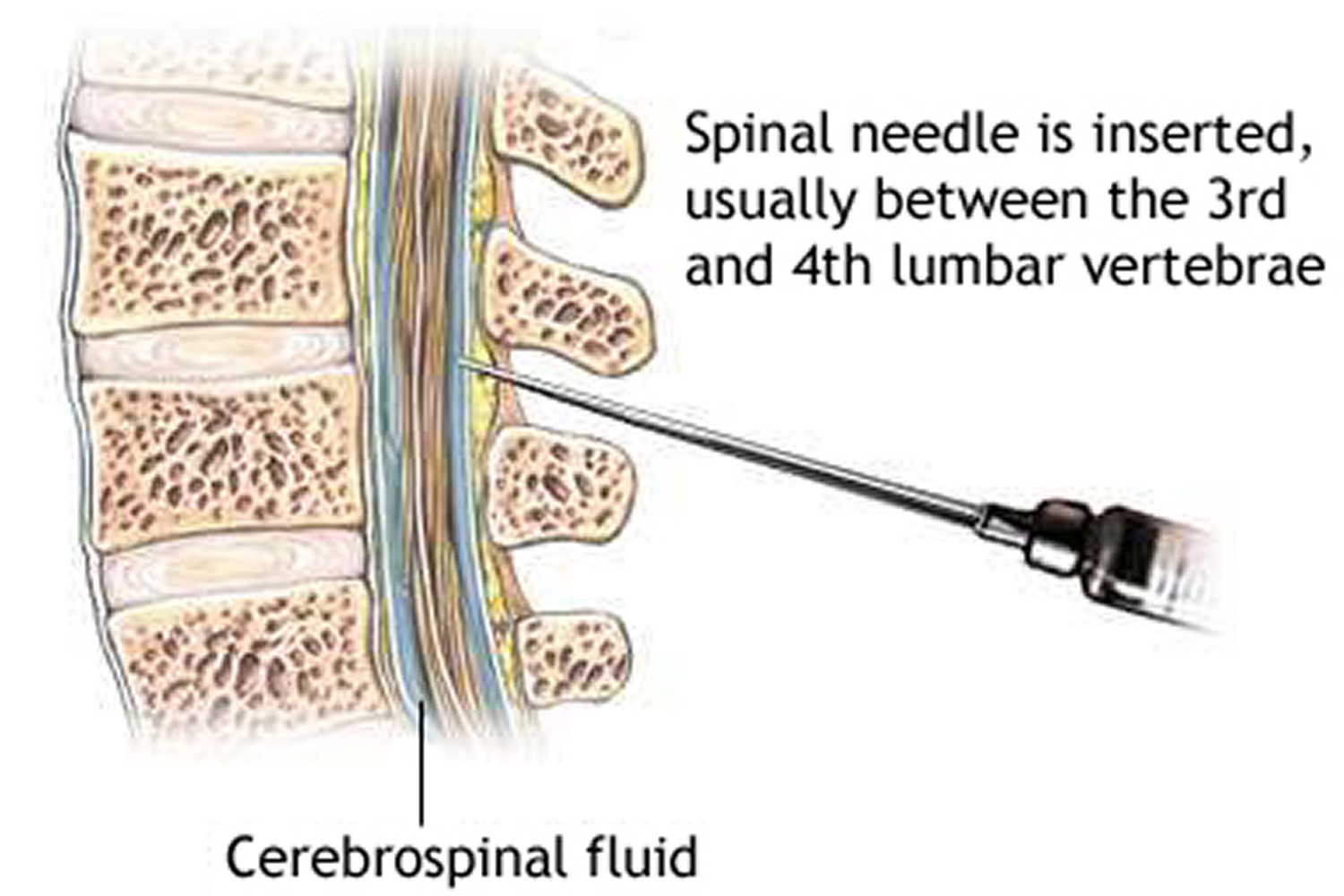
Cerebral spinal fluid (CSF) is a clear fluid that circulates in the space surrounding the spinal cord and brain. Cerebrospinal fluid (CSF) protects the brain and spinal cord from injury by acting like a liquid cushion. Cerebrospinal fluid (CSF) is usually obtained through a lumbar puncture (spinal tap). During the procedure, a needle is inserted usually between the 3rd and 4th lumbar vertebrae and the cerebrospinal fluid (CSF) is collected for testing.
Healthcare professionals perform lumbar punctures and test the CSF to detect or rule out suspected diseases or conditions through analysis of the white blood cell count, glucose levels, protein, and bacteria.
Most lumbar punctures are done to test for infections (such as meningitis), but they also can detect bleeding in the brain and certain conditions affecting the nervous system (such as Guillain-Barré syndrome and multiple sclerosis or cancers of the brain or spinal cord). Lumbar punctures also can deliver chemotherapeutic medications or to inject anesthetic medications.
Special testing can look for certain bacteria and viruses, or find the presence of abnormal cells that can help identify specific diseases in the central nervous system.
Cerebrospinal fluid (CSF) analysis can also be used to diagnose certain neurologic disorders. These may include brain or spinal cord damage. A spinal tap may also be done to establish the diagnosis of normal pressure hydrocephalus.
Depending on the doctor’s recommendations, you might have to lie on your back for a few hours after the procedure. You might feel tired and have a mild backache the day after the lumbar puncture procedure.
Up to 1 to 43 percent of people who have undergone a lumbar puncture develop a headache afterward due to a leak of CSF fluid into nearby tissues 1. Lumbar puncture headache after the test that can last a few hours or days. If headaches last more than a few days (especially when you sit, stand or walk) you might have a CSF-leak. You should talk to your physician if this occurs.
Post-dural (post-lumbar or post-spinal) puncture headache is defined as any headache after a lumbar puncture that worsens within 15 minutes of sitting or standing and that is relieved within 15 minutes of lying down 2. Ninety per cent of post-lumbar puncture headaches occur within three days of the procedure, and 66% start within the first 48 hours 3.
A lumbar puncture takes around 30 to 45 minutes but you’ll need to stay lying down at the hospital for at least another hour while the nurses monitor you.
You’ll be able to go home the same day if you feel well enough – but you won’t be able to drive yourself home.
Lumbar puncture side effects
A lumbar puncture is generally a safe procedure and serious side effects are uncommon.
The most common side effects are:
- headaches, which can last for up to a week – you’ll be given painkillers at the hospital if you need them
- swelling and lower back pain where the needle was inserted – this should get better on its own after a few days and is normally nothing to worry about
Is lumbar puncture painful?
While some people notice a brief pinch and some discomfort, most people don’t consider a lumbar puncture to be painful.
Sometimes, sedation medication may be helpful for you in order to perform the lumbar puncture procedure. If sedation is necessary, be sure to discuss the risks and benefits with your doctor.
Contact the hospital team or a doctor if:
- your headaches are severe or don’t go away
- you’re feeling or being sick
- you have a very high temperature or feel hot and shivery
- it’s painful to look at bright lights
- the swelling in your back lasts for more than a few days or keeps getting worse
- you see blood or clear fluid leaking from your back
Why is lumbar puncture done
There are many indications for lumbar puncture (Table 1), but obtaining CSF may be the only way of confirming or refuting subarachnoid haemorrhage (SAH), meningitis and neuro-inflammatory diseases. Lumbar puncture is still required to obtain indirect measurements of intracranial pressure, although non-invasive methods of intracranial pressure estimation are undergoing validation 4.
A lumbar puncture may be done to:
- Collect cerebrospinal fluid for laboratory analysis
- Measure the pressure of your cerebrospinal fluid
- Remove some fluid to reduce pressure in the skull or spine
- Inject spinal anesthetics, chemotherapy drugs or other medications
- Inject dye (myelography) or radioactive substances (cisternography) into cerebrospinal fluid to make diagnostic images of the fluid’s flow
Table 1. Indications for Lumbar Puncture
| To exclude subarachnoid haemorrhage in acute severe headache |
|---|
To investigate or exclude meningitis
|
To investigate neurological disorders
|
To demonstrate and manage disorders of Intracranial Pressure
|
To administer therapeutic or diagnostic agents
|
A lumbar puncture procedure may be helpful in diagnosing many diseases and disorders, including:
- Meningitis. An inflammation of the membrane covering the brain and spinal cord. The inflammation is usually the result of a viral, bacterial, or fungal infection.
- Encephalitis. An inflammation of the brain that is usually caused by a virus.
- Certain cancers involving the brain and spinal cord
- Bleeding in the area between the brain and the tissues that cover it (subarachnoid space)
- Reye syndrome. A sometimes fatal disease that causes severe problems with the brain and other organs. Although the exact cause of the disease is not known, it has been linked to giving aspirin to children. It is now advised not to give aspirin to children during illnesses, unless prescribed by your child’s healthcare provider.
- Myelitis. An inflammation of the spinal cord or bone marrow.
- Neurosyphilis. A stage of syphilis during which the bacteria invades the central nervous system.
- Guillain-Barré syndrome. A disorder in which the body’s immune system attacks part of the nervous system.
- Demyelinating diseases. Diseases that attack the protective coating that surrounds certain nerve fibers – for example, multiple sclerosis or acute demyelination polyneuropathy.
- Headaches of unknown cause. After evaluation and head imaging if necessary, a lumbar puncture may be done to diagnose certain inflammatory conditions that can result in a headache.
- Pseudotumor cerebri (also called idiopathic intracranial hypertension, or IIH). In this condition,pressure within the subarachnoid space is elevated for reasons that are not clear. A lumbar puncture is only done in this condition after evaluation and head imaging.
- Normal pressure hydrocephalus. A rare condition affecting mainly older people in which there is a triad of loss of urinary control, memory problems, and an unsteady gait. A lumbar puncture is done to see if the pressure of the CSF is elevated or not.
In addition, a lumbar puncture may be used to measure the pressure of the CSF. The healthcare provider uses a special tube (called a manometer) to measures the pressure during a lumbar puncture.
Finally, a lumbar puncture may be done to inject medicine directly into the spinal cord. These include:
- Spinal anesthetics before a surgical procedure
- Contrast dye for X-ray studies – for example, myelography
- Chemotherapy drugs used to treat cancer
Your healthcare provider may have other reasons to recommend a lumbar puncture.
Information gathered from a lumbar puncture can help diagnose:
- Serious bacterial, fungal and viral infections, including meningitis, encephalitis and syphilis
- Bleeding around the brain (subarachnoid hemorrhage)
- Certain cancers involving the brain or spinal cord
- Certain inflammatory conditions of the nervous system, such as multiple sclerosis and Guillain-Barre syndrome
Getting the results
Some results from a lumbar puncture are available within 45 to 60 minutes. However, to look for specific bacteria growing in the sample, a bacterial culture is sent to the lab and these results are usually available in 48 hours. If it’s determined there might be an infection, the doctor will start antibiotic treatment while waiting for the results of the culture.
Lumbar puncture can allow the physician to determine:
- the cause of meningitis
- if the patient has a subarachnoid hemorrhage in the setting of a normal non-contrast head CT scan
- the presence of a malignancy affecting the central nervous system (e.g., leptomeningeal carcinomatosis)
- the presence of a demyelinating disease (e.g., multiple sclerosis)
- if the patient has symptoms concerning for Guillain-Barre syndrome
Caution should be taken in performing the lumbar puncture in patients with:
- increased intracranial pressure
- the patient runs the risk of brain herniation
- thrombocytopenia (low platelets count) or other bleeeding diathesis
- signs and symptoms concerning for a spinal epidural abscess
Lumbar puncture complications
- post-lumbar puncture headache
- infection
- bleeding
- cerebral herniation
Spinal Cord Anatomy
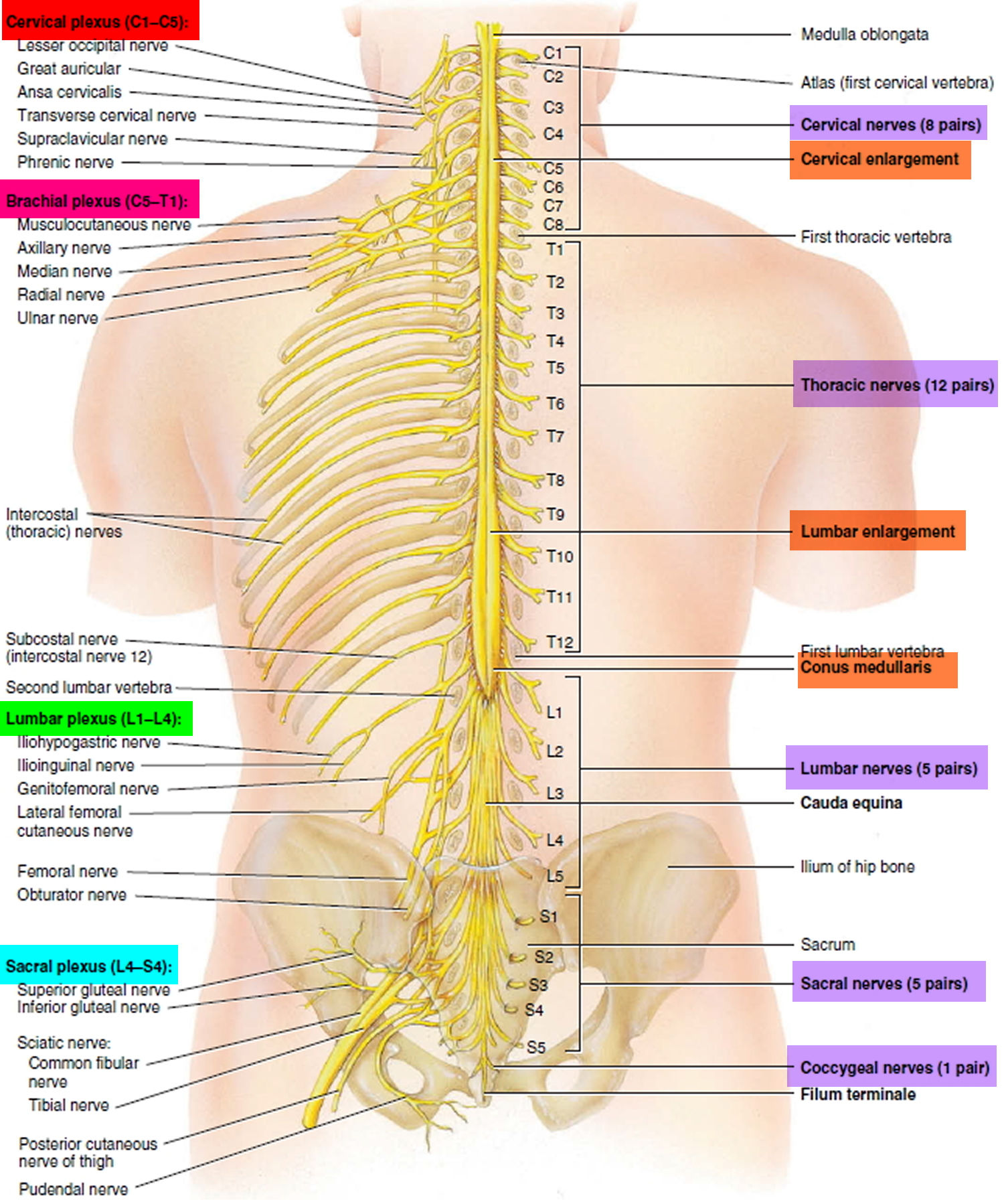
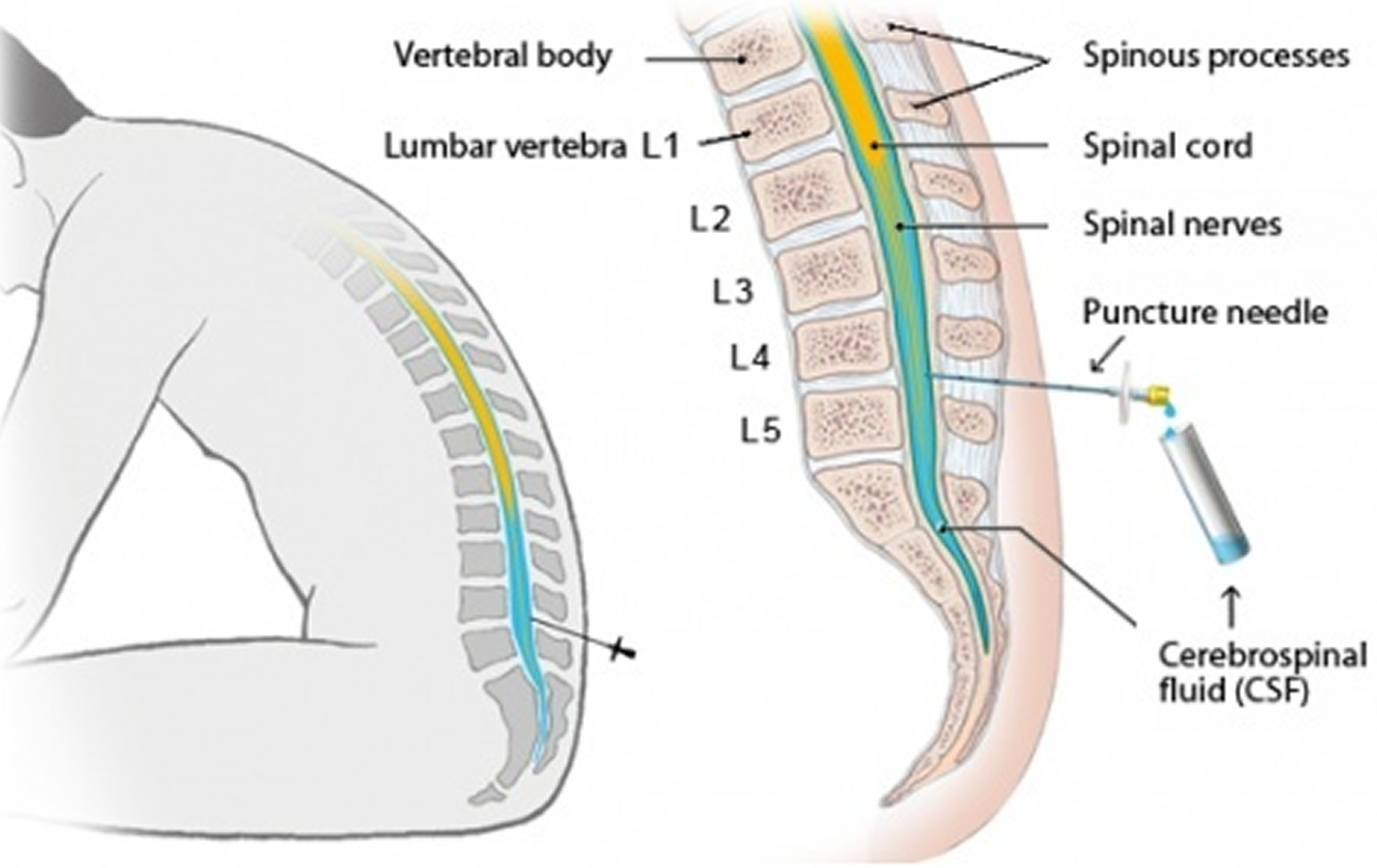
Knowledge of the anatomy of the lumbar spine 6 is essential for anyone performing lumbar puncture. The lumbar puncture needle pierces in order: skin, subcutaneous tissue, supraspinous ligament, interspinous ligament, ligamentum flavum, epidural space containing the internal vertebral venous plexus, dura, arachnoid, and finally the subarachnoid space (Figure 4).
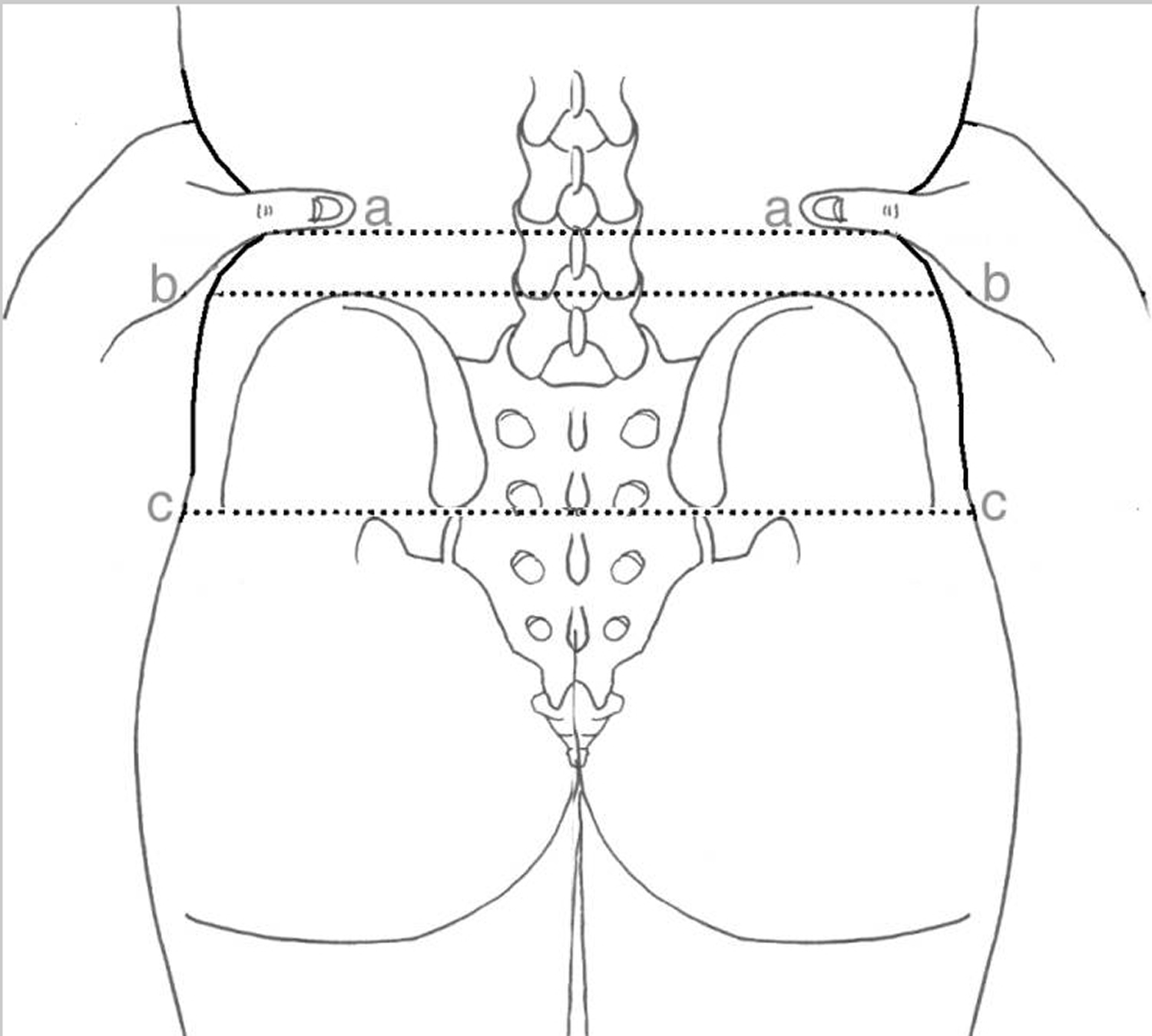
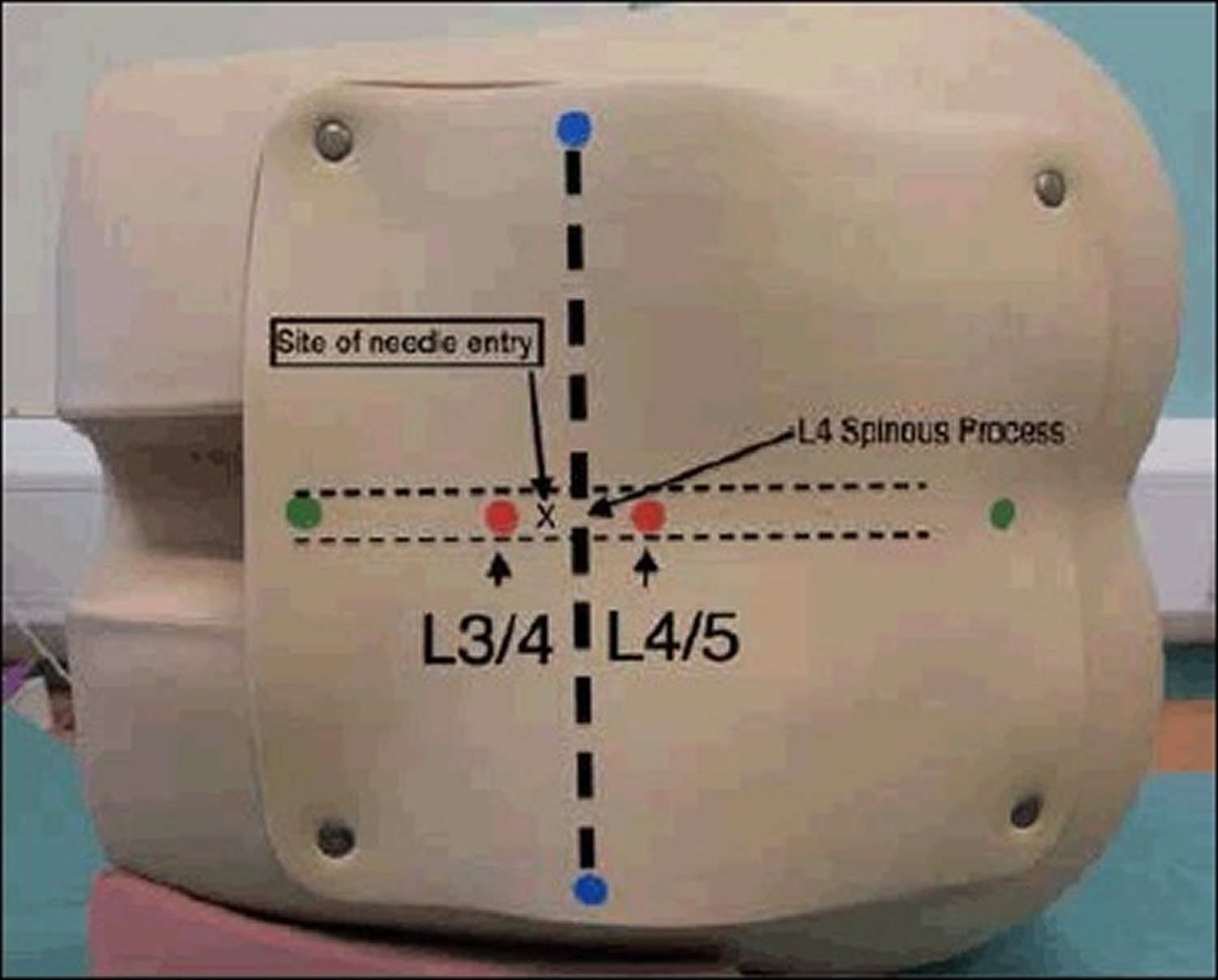
The most important bony landmark is the L4 spinous process, which is located at the intersection of the ‘intercristal’ or ‘Tuffier’s’ line (the line between the top of the iliac crests) and the lumbar spine midline (Figure 2). Radiological studies have shown that this clinical landmark is accurate in over 95% of the population 7, although in females or obese people Tuffier’s Line tends to be found at a higher level than L4 8. Note the conus medullaris can extend as low as to the upper aspect of the L3 vertebral segment 9.
Figure 1. Spinal cord
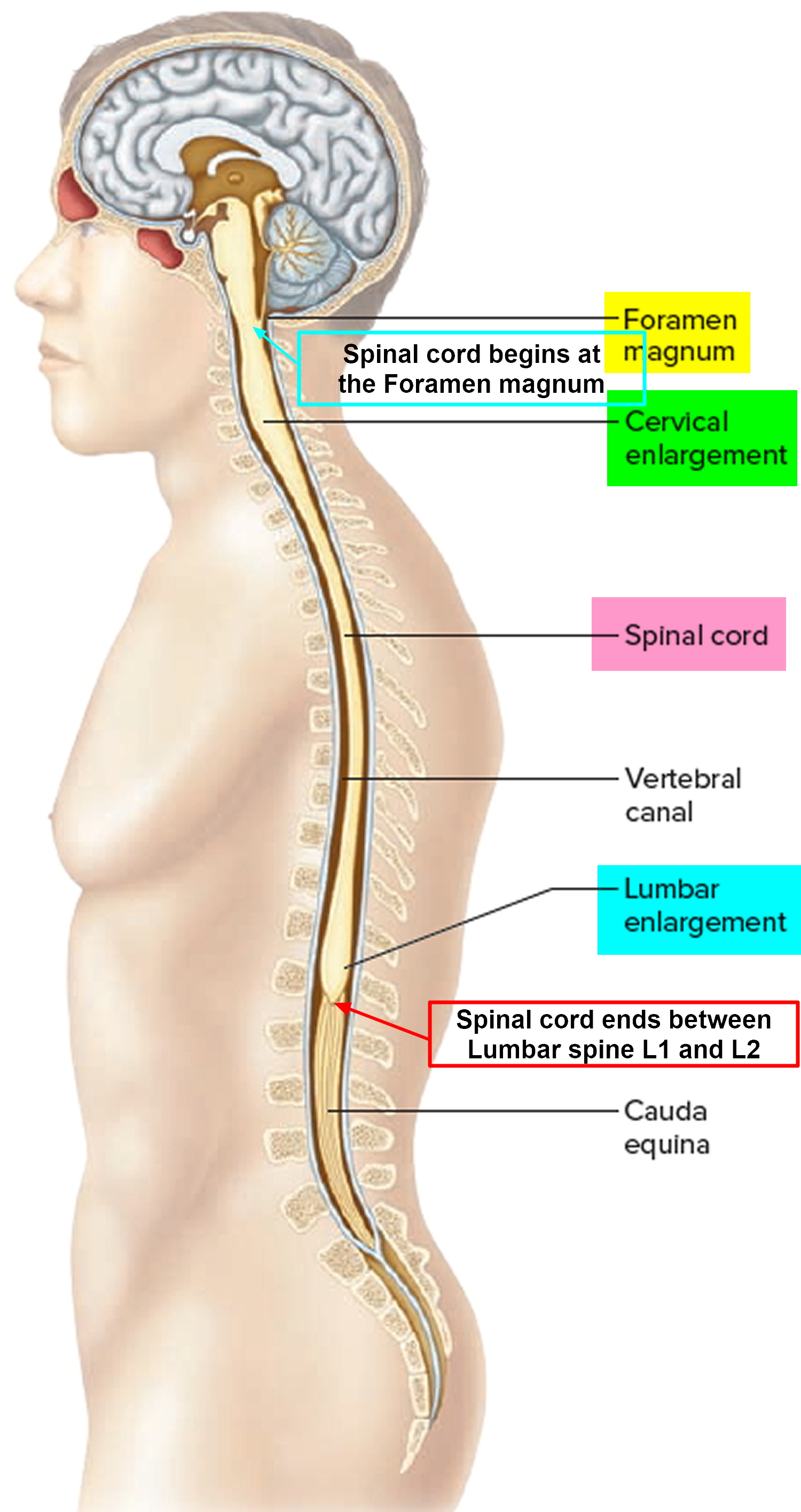
Figure 2. Spinal cord segments
Figure 3. Lumbar puncture site L3-L4 (a spinal needle is inserted, usually between the third and fourth lumbar vertebrae in the lower spine. Once the needle is properly positioned in the subarachnoid space [the space between the spinal cord and its covering, the meninges], pressures can be measured and fluid can be collected for testing.)
Figure 4. Lumbar puncture site L4-L5. Note: Sagittal section of lumbar vertebrae illustrating the course of the lumbar puncture needle through skin, subcutaneous tissue, supraspinous ligament, interspinous ligament between the spinous processes, ligamentum flavum, dura mater, into the subarachnoid space and between the nerve roots of the cauda equina. Lumbar vertebral bodies, intervertebral disc , and lumbar puncture needle.
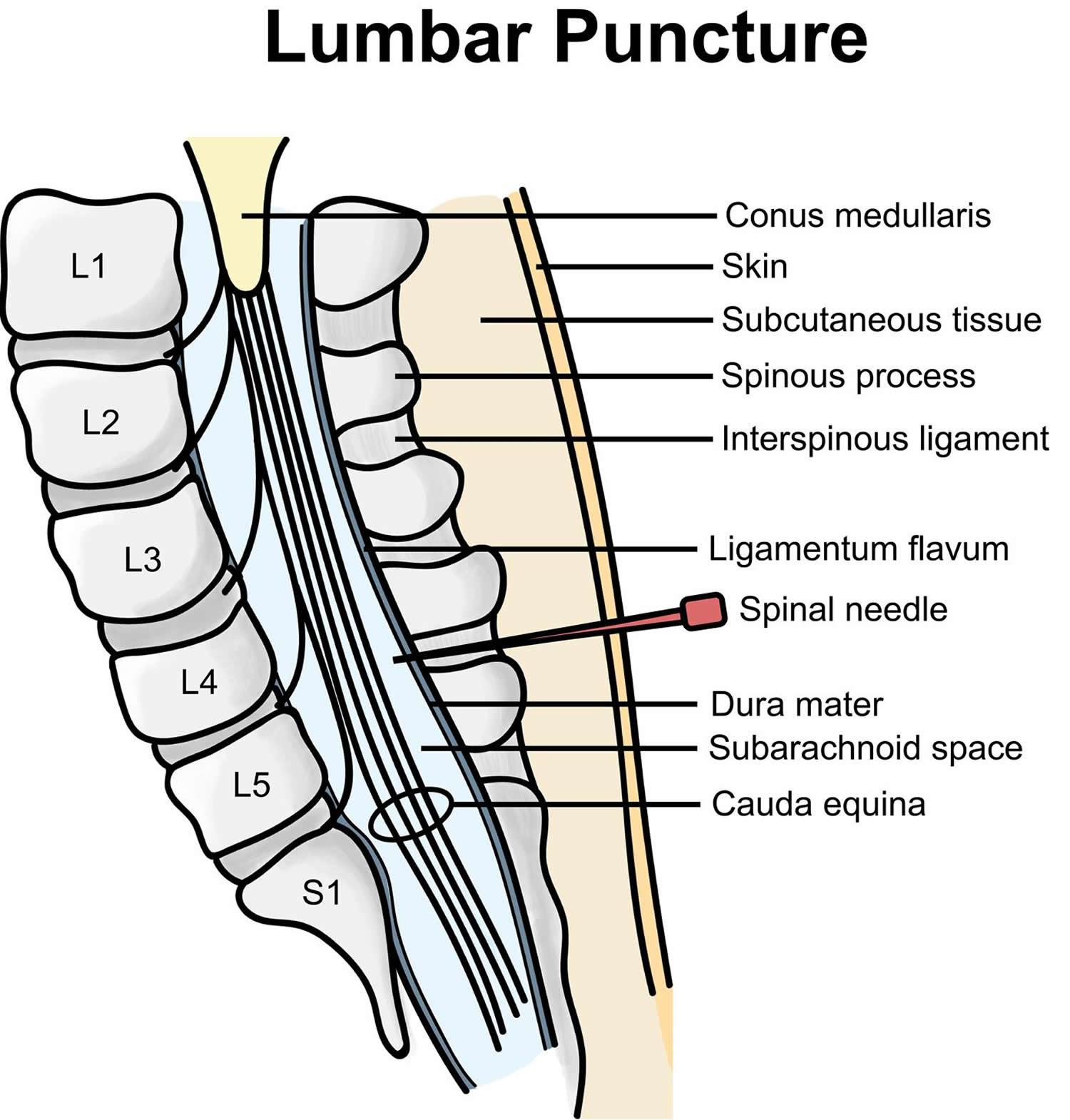 Figure 5. Lumbar puncture anatomical landmarks – the lines referred to in the study: the palpated intercristal line (a), the imaged Intercristal Line (eponymously Tuffier’s Line) (b) and the palpated posterior superior iliac spine line (c).
Figure 5. Lumbar puncture anatomical landmarks – the lines referred to in the study: the palpated intercristal line (a), the imaged Intercristal Line (eponymously Tuffier’s Line) (b) and the palpated posterior superior iliac spine line (c).Figure 6. Lumbar puncture locations – Blue dots-Iliac crests, and the line connecting them is the Intercristal Line (eponymously Tuffier’s Line). Red Dots are either side of the palpated L4 spinous process, the right hand one is in the L4/5 interspinal space and the left hand one in the L3/4 interspinal space. A diagnostic Lumbar Puncture should be performed at the L3/4 interspinal space, marked ‘x’.
Lumbar puncture contraindications
Severe thrombocytopenia, bleeding diathesis or anticoagulant therapy are contraindications to lumbar puncture, although it can be performed safely at platelet counts of 50 x 109/l or above 10.
Aspirin therapy is not associated with a high risk of bleeding in spinal anaesthetic interventions 11, but data on clopidogrel and other GP IIa/IIIb receptor antagonists are lacking. GP IIb/IIIa–Receptor Antagonists affect platelet-fibrinogen and platelet–von Willebrand factor binding to inhibit platelet aggregation. This class of antiplatelet drugs includes abciximab (ReoPro), eptifibatide (Integrilin), and tirofiban (Aggrastat) 12. Guidance on spinal anaesthetic procedures suggest that procedures should be avoided until platelet function has recovered 13. Warfarin should be stopped 5-7 days in advance of procedures and the INR should be less than 1.2. Low molecular weight heparin can be used in the interim but treatment dose heparin should be stopped for twenty-four hours prior to spinal procedures. Prophylactic doses should be avoided within twelve hours 13.
Lumbar puncture procedure
There are different ways to get a sample of cerebrospinal fluid (CSF). Lumbar puncture (spinal tap) is the most common method.
A lumbar puncture is usually done in an outpatient facility or a hospital. Your doctor will talk to you about the potential risks, and any discomfort you might feel during the procedure.
If a child is having a lumbar puncture, a parent is usually allowed to stay in the room. Talk to your child’s doctor about whether this will be possible.
Afterward, you should plan to rest for several hours, even if you feel fine. This is to prevent fluid from leaking around the site of the puncture. You will not need to lie flat on your back the entire time.
How to prepare for the lumbar puncture procedure
Before your lumbar puncture, your doctor asks questions about your medical history, does a physical exam, and orders blood tests to check if you have any bleeding or clotting disorders. You will need to give the health care team your consent before the test. Tell your doctor if you are on any blood-thinning medicines such as warfarin (Coumadin), Lovenox, aspirin, or Plavix.
Your doctor may also recommend a CT scan or MRI to determine if you have any abnormal swelling in or around your brain.
PRECAUTIONS: If you are pregnant or think you might be pregnant, please check with your doctor before scheduling the exam. Other options will be discussed with you and your doctor.
Food and medications
Your doctor will give you specific instructions about food, drink and medications. You’ll likely be asked not to eat or drink anything after midnight before your procedure.
Tell your doctor if you’re taking blood-thinning or other anticoagulant medications. Examples include warfarin (Coumadin, Jantoven), clopidogrel (Plavix), and some over-the-counter pain relievers such as aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve). Also, tell your doctor if you’re allergic to any medications, such as numbing medications (local anesthetics).
How the lumbar puncture procedure will feel
It may be uncomfortable to stay in position for the test. Staying still is important because movement may lead to injury of the spinal cord.
You may be told to straighten your position slightly after the needle is in place. This is to help measure the CSF pressure.
The anesthetic will sting or burn when first injected. There will be a hard pressure sensation when the needle is inserted. Often, there is some brief pain when the needle goes through the tissue surrounding the spinal cord. This pain should stop in a few seconds.
In most cases, the procedure takes about 30 minutes. The actual pressure measurements and CSF collection only take a few minutes.
Before the lumbar puncture procedure
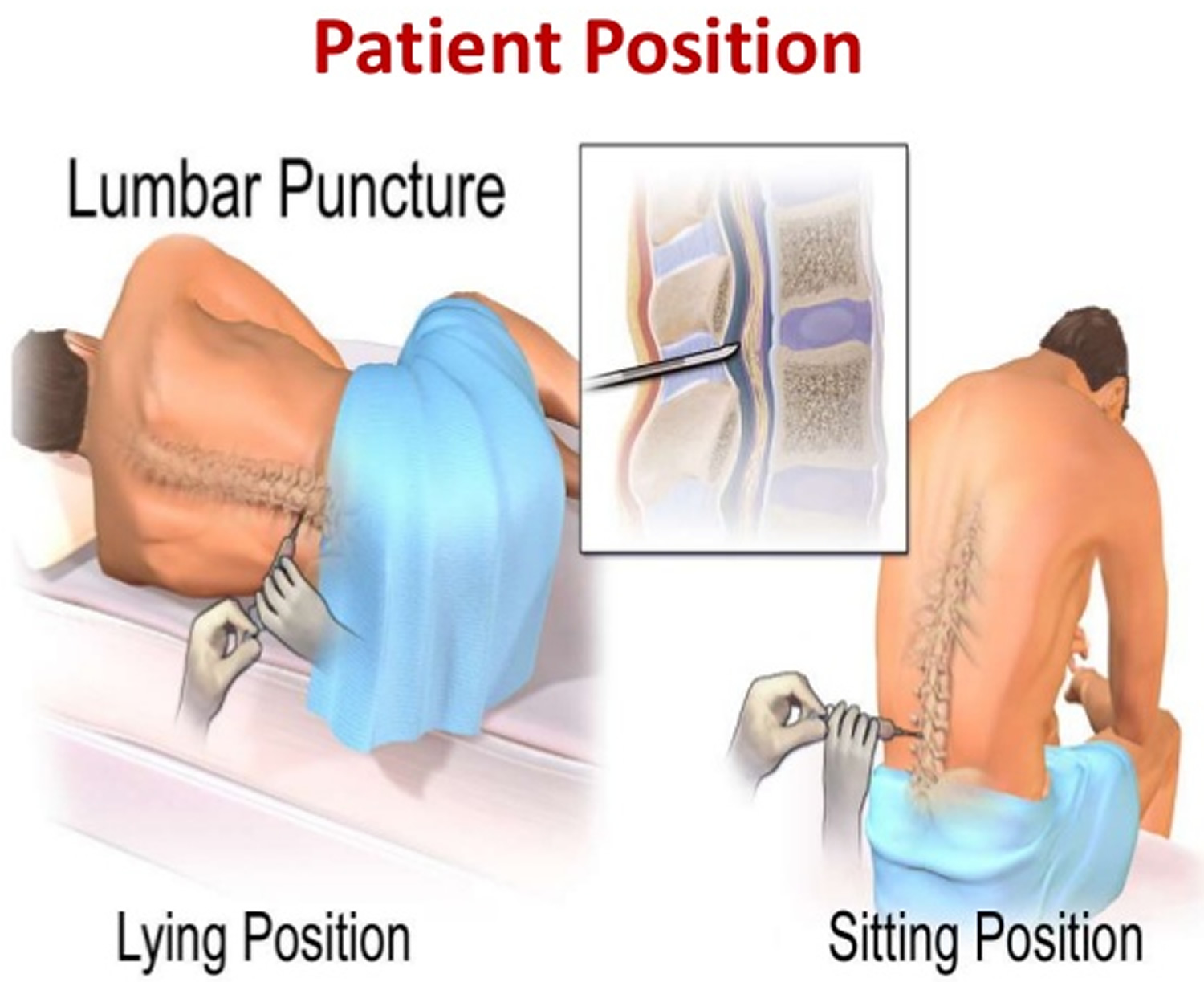
You’re asked to change into a hospital gown. There are a few possible positions for this test. Usually, you lie on your side with your knees drawn up to your chest, or you sit and lean forward on a stable surface. These positions flex your back, widening the spaces between your vertebrae and making it easier for your doctor to insert the needle.
For an infant or young child, someone will hold the child in position during the procedure.
Your back is washed with antiseptic soap or iodine and covered with a sterile sheet.
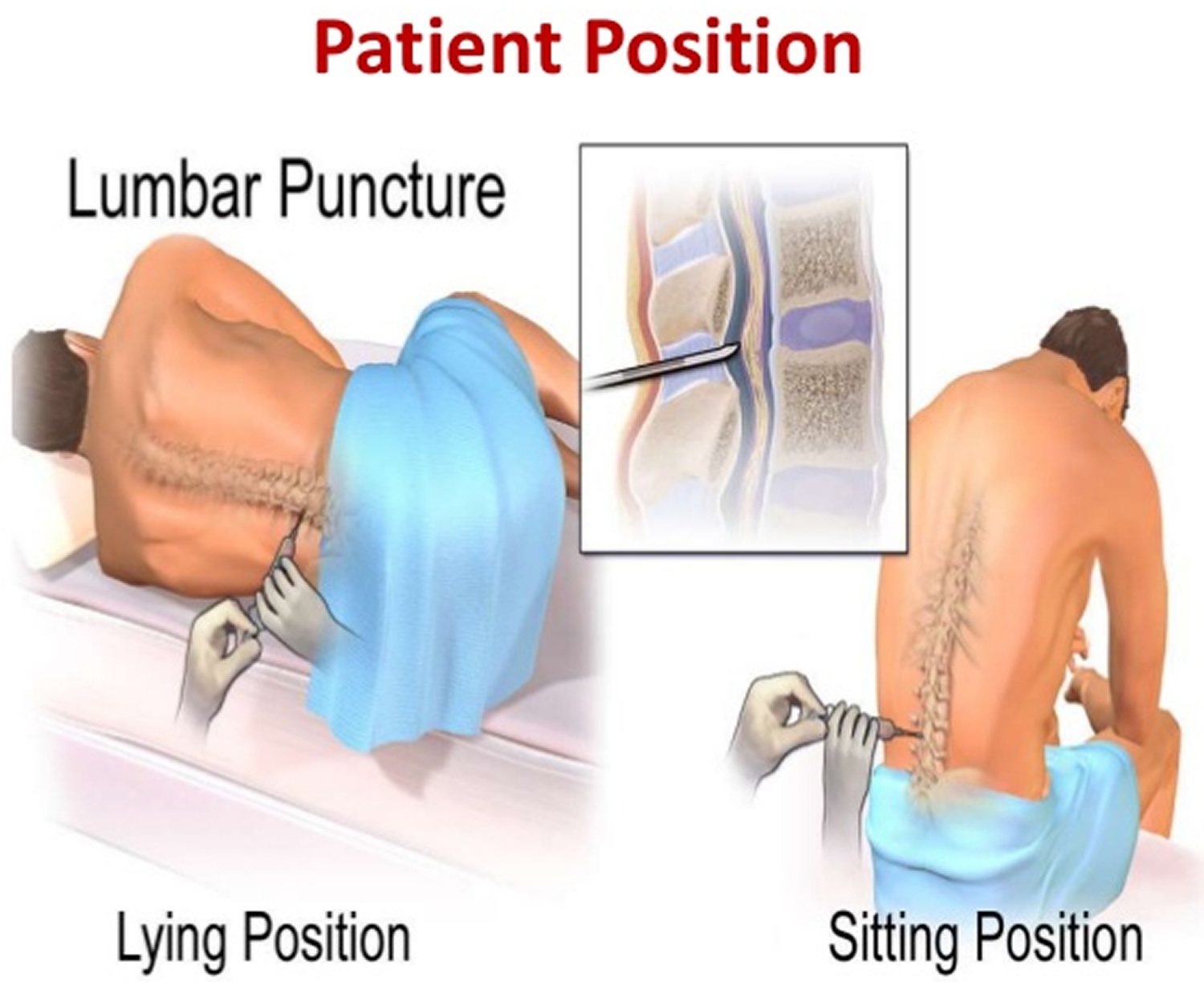
Lumbar puncture position
Patient position
- Lateral recumbent position
- preferred for accurate opening pressure measurement, so the spaces between the vertebrae are as wide as possible. This makes it easier for the doctor to insert the needle.
- Prone position, better for fluoroscopy guided lumbar puncture
- Sitting upright: If the procedure is to be performed in the upright position, seated with the chin down and the feet supported, a table and pillow will improve comfort and optimise positioning. This position widens the interspinous distance 14.
- Needle entry
- into the subarachnoid space at L3-4 or L4-5 interspace
- remember that the spinal cord ends in L1-2
- thus there should not be any trauma to the spinal cord if properly performed
- In cases where there are unsuccessful attempts in obtaining CSF, imaging guidance can be used such as
- fluoroscopy
- ultrasound
Figure 5. Lumbar puncture position
During the lumbar puncture procedure
To have the lumbar puncture test:
- You will lie on your side with your knees pulled up toward the chest, and chin tucked downward. Sometimes the test is done sitting up, but bent forward.
- After the back is cleaned, the health care provider will inject a local numbing medicine (local anesthetic) into the lower spine. The local anesthetic will sting briefly as it’s injected.
- A spinal needle will be inserted between the two lower vertebrae (lumbar region), through the spinal membrane (dura) and into the spinal canal. You may feel pressure in your back during this part of the procedure. Once the needle is properly positioned in the subarachnoid space (the space between the spinal cord and its covering, the meninges), pressures can be measured and fluid can be collected for testing.
- The spinal needle is thin and the length varies according to the size of the patient. It has a hollow core, and inside the hollow core is a “stylet,” another type of thin needle that acts kind of like a plug. When the spinal needle is inserted into the lower lumbar area, the stylet is carefully removed, which allows the cerebrospinal fluid to drip out into the collection tubes.
- Once the needle is in position, the CSF pressure is measured and a sample of 1 to 10 milliliters (mL) of CSF is collected in 4 vials.
- An opening pressure is sometimes taken. An abnormal pressure can suggest an infection or other problem.
- After the CSF sample is collected (this usually takes about 2-5 minutes), the needle is withdrawn, the area is cleaned, and a small bandage is placed on the needle site. Collected samples are sent to a lab for analysis and testing.
- If the provider needs to inject medicine into the spinal canal, it will be given through the same needle after the CSF is collected.
- The lumbar puncture procedure usually lasts about 30 to 45 minutes. Your doctor may suggest lying down after the procedure for a short time after the test.
Tell the healthcare provider if you feel any numbness, tingling, headache, or lightheadedness during the procedure.
Occasionally, special x-rays are used to help guide the needle into position. This is called fluoroscopy.
Sometimes, an ultrasound may be used as a guide during the procedure on infants and young children. The ultrasound can help prevent inserting the needle too far.
Lumbar puncture with fluid collection may also be part of other procedures such as an x-ray or CT scan after dye has been inserted into the CSF.
Rarely, other methods of cerebrospinal fluid (CSF) collection may be used.
- Cisternal puncture uses a needle placed below the occipital bone (back of the skull). It can be dangerous because it is so close to the brain stem. It is always done with fluoroscopy.
- Ventricular puncture may be recommended in people with possible brain herniation. This is a very rarely used method. It is most often done in the operating room. A hole is drilled in the skull, and a needle is inserted directly into one of the brain’s ventricles.
CSF may also be collected from a tube that’s already placed in the fluid, such as a shunt or a ventricular drain.
Lumbar puncture recovery
You must have an adult driver accompany you so they can drive you home after the procedure. This is for your safety and comfort.
Please note: You will be unable to drive for 24 hours after the procedure. If you are taking a cab or using public transportation, you need to bring a friend or family member to accompany you after the procedure to your home or hotel. A cab or public transportation driver is not considered an escort.
If your ride home is longer than 30 minutes, doctors advise that on your ride home you be in a reclined position with one or two pillows supporting your head.
After the lumbar puncture procedure
You usually will be asked to lie flat for about one hour after the lumbar puncture is completed. This helps reduce the incidence of a headache. You will be allowed to roll from side to side as long as your head is not elevated. If you need to urinate, you may need to do so in a bedpan or urinal during the time that you need to stay flat.
You will be asked to drink extra fluids to rehydrate after the procedure. This replaces the CSF that was withdrawn during the spinal tap and reduces the chance of developing a headache. However, a recent 2016 Cochrane Review 15 concluded that in general, there was no evidence suggesting that routine bed rest after lumbar puncture is beneficial for the prevention of post-dural puncture headache onset. The role of fluid supplementation in the prevention of post-dural lumbar puncture headache remains unclear 15. The review authors believe that these practices should no longer be routinely recommended to patients for the prevention of headaches after lumbar puncture since there is no evidence supporting them 15.
After recovery, you may be taken to your hospital room or discharged to your home. If you go home, usually your healthcare provider will advise you to only engage in very light activity the rest of the day.
- Plan to rest. Don’t participate in strenuous activities the day of your procedure. You may return to work if your job doesn’t require you to be physically active. Discuss your activities with your doctor if you have questions.
- Take a pain medication. A nonprescription pain-relieving medication that contains acetaminophen can help reduce a headache or back pain.
While you’re recovering from a lumbar puncture:
DO
- drink plenty of fluids
- take painkillers, such as paracetamol
- lie down instead of sitting upright
- try drinks containing caffeine, such as coffee, tea or cola – some people find this helps to relieve the headaches
- remove the dressing or plaster yourself the next day
DON’T
- drive or operate machinery for at least 24 hours
- play sport or do any strenuous activities for at least a week
Once you are at home, notify your provider of any abnormalities, such as:
- Numbness and tingling of the legs
- Drainage of blood or pain at the injection site
- Inability to urinate
- Headaches
If the headaches persist for more than a few hours after the procedure, or when you change positions, contact your provider.
You may be instructed to limit your activity for 24 hours following the procedure. Generally, if no complications occur, you may return to your normal diet and activities.
Your healthcare provider may give you other specific instructions about what you should do after a lumbar puncture.
Lumbar puncture results
The spinal fluid samples are sent to a laboratory for analysis. Lab technicians check for a number of things when examining spinal fluid, including:
- General appearance. Spinal fluid is normally clear and colorless. If it’s cloudy, yellow or pink in color, it might indicate abnormal bleeding. Spinal fluid that is green might indicate an infection or the presence of bilirubin.
- Protein (total protein and the presence of certain proteins). Elevated levels of total protein — greater than 45 milligrams per deciliter (mg/dL) — may indicate an infection or another inflammatory condition. Specific lab values may vary from medical facility to medical facility.
- White blood cells. Spinal fluid normally contains up to 5 mononuclear leukocytes (white blood cells) per microliter. Increased numbers may indicate an infection. Specific lab values may vary from medical facility to medical facility.
- Sugar (glucose). A low glucose level in spinal fluid may indicate infection or another condition.
- Microorganisms. The presence of bacteria, viruses, fungi or other microorganisms can indicate an infection.
- Cancer cells. The presence of abnormal cells in spinal fluid — such as tumor or immature blood cells — can indicate certain types of cancer.
Lab results are combined with information obtained during the test, such as spinal fluid pressure, to help establish a possible diagnosis.
Your health care provider generally gives you the results within a few days, but it could take longer. Ask your doctor when he or she expects to receive the results of your test.
Write down questions that you want to ask your doctor. Don’t hesitate to ask questions during your visit. Questions you may want to ask include:
- Based on the results, what are my next steps?
- What kind of follow-up, if any, should I expect?
- Are there any factors that might have affected the results of this test and, therefore, may have altered the results?
- Will I need to repeat the test at some point?
Normal Results
Normal values typically range as follows:
- CSF Pressure: 70 to 180 mm H2O
- CSF Appearance: clear, colorless
- CSF Total protein: 15 to 60 mg/100 mL
- Gamma globulin: 3% to 12% of the total protein
- CSF glucose: 50 to 80 mg/100 mL (or greater than two thirds of blood sugar level)
- CSF cell count: 0 to 5 white blood cells (all mononuclear), and no red blood cells
- Chloride: 110 to 125 mEq/L
Normal value ranges may vary slightly among different laboratories. Talk to your provider about the meaning of your specific test results.
The examples above show the common measurements for results for these tests. Some laboratories use different measurements or may test different specimens.
Abnormal Results
What abnormal results mean
If the CSF looks cloudy, it could mean there is an infection or a buildup of white blood cells or protein.
If the CSF looks bloody or red, it may be a sign of bleeding or spinal cord obstruction. If it is brown, orange, or yellow, it may be a sign of increased CSF protein or previous bleeding (more than 3 days ago). There may be blood in the sample that came from the spinal tap itself. This makes it harder to interpret the test results.
CSF pressure
- Increased CSF pressure may be due to increased intracranial pressure (pressure within the skull).
- Decreased CSF pressure may be due to spinal cord tumor, shock, fainting, or diabetic coma.
CSF protein
- Increased CSF protein may be due to blood in the CSF, diabetes, polyneuritis, tumor, injury, or any inflammatory or infectious condition.
- Decreased protein is a sign of rapid CSF production.
CSF glucose
- Increased CSF glucose is a sign of high blood sugar.
- Decreased CSF glucose may be due to hypoglycemia (low blood sugar), bacterial or fungal infection (such as meningitis), tuberculosis, or certain other types of meningitis.
Blood cells in CSF
- Increased white blood cells in the CSF may be a sign of meningitis, acute infection, beginning of a long-term (chronic) illness, tumor, abscess, stroke, or demyelinating disease (such as multiple sclerosis).
- Red blood cells in the CSF sample may be a sign of bleeding into the spinal fluid or the result of a traumatic lumbar puncture.
Other CSF results
Increased CSF gamma globulin levels may be due to diseases such as multiple sclerosis, neurosyphilis, or Guillain-Barré syndrome.
Additional conditions under which the test may be performed:
- Chronic inflammatory polyneuropathy
- Dementia due to metabolic causes
- Encephalitis
- Epilepsy
- Febrile seizure (children)
- Generalized tonic-clonic seizure
- Hydrocephalus
- Inhalation anthrax
- Normal pressure hydrocephalus
- Pituitary tumor
- Reye syndrome
Lumbar puncture risks
A lumbar puncture is considered a safe procedure with minimal risks. Most of the time, there are no complications. In some instances, a patient may get a headache. It’s recommended that patients lie down for a few hours after the lumbar puncture test and drink plenty of fluids to help prevent headaches, which usually resolve with rest, pain medications, and fluids. In rare cases, infection or bleeding can occur.
Risks of lumbar puncture include:
- Bleeding. Bleeding may occur near the puncture site or, rarely, into the epidural space. Bleeding into the spinal canal or around the brain (subdural hematomas). There is an increased risk of bleeding in people who take blood thinners.
- Discomfort during the test
- Post-lumbar puncture headache. Up to 25 percent of people who have undergone a lumbar puncture develop a headache afterward due to a leak of CSF fluid into nearby tissues. The headache typically starts several hours up to two days after the procedure and may be accompanied by nausea, vomiting and dizziness. The headaches are usually present when sitting or standing and resolve after lying down. Post-lumbar puncture headaches can last from a few hours to a week or more.
- Hypersensitivity (allergic) reaction to the anesthetic
- Infection introduced by the needle going through the skin
- Back discomfort or pain. You may feel pain or tenderness in your lower back after the procedure. The pain might radiate down the back of your legs.
- Brainstem herniation. Increased pressure within the skull (intracranial), due to a brain tumor or other space-occupying lesion, can lead to compression of the brainstem after a sample of cerebrospinal fluid is removed. A computerized tomography (CT) scan or MRI prior to a lumbar puncture can be obtained to determine if there is evidence of a space-occupying lesion that results in increased intracranial pressure. This complication is rare.
Brain herniation may occur if this test is done on a person with a mass in the brain (such as a tumor or abscess). This can result in brain damage or death. This test is not done if an exam or test reveals signs of a brain mass.
Damage to the nerves in the spinal cord may occur, particularly if the person moves during the test.
Cisternal puncture or ventricular puncture carries additional risks of brain or spinal cord damage and bleeding within the brain.
Lumbar puncture complications
Lumbar puncture is more dangerous for people with:
- A tumor in the back of the brain that is pressing down on the brainstem
- Blood clotting problems
- Low platelet count (thrombocytopenia)
- Individuals taking blood thinners, aspirin, clopidogrel, or other similar drugs to decrease the formation of blood clots.
- Grande PO. Mechanisms behind postspinal headache and brain stem compression following lumbar dural puncture – a physiological approach. Acta Anaesthesiologica Scandinavica 2005;49(5):619-26. https://www.ncbi.nlm.nih.gov/pubmed/15836674[↩]
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24 Suppl 1:9-160. https://www.ncbi.nlm.nih.gov/pubmed/14979299[↩]
- Turnbull DK, Shepherd DB. Post-dural puncture headache: pathogenesis, prevention and treatment. British Journal of Anaesthesia 2003;91(5):718-29. https://www.ncbi.nlm.nih.gov/pubmed/14570796[↩]
- Clinical assessment of noninvasive intracranial pressure absolute value measurement method. Ragauskas A, Matijosaitis V, Zakelis R, Petrikonis K, Rastenyte D, Piper I, Daubaris G. Neurology. 2012 May 22; 78(21):1684-91. https://www.ncbi.nlm.nih.gov/pubmed/22573638/[↩]
- Doherty CM, Forbes RB. Diagnostic Lumbar Puncture. The Ulster Medical Journal. 2014;83(2):93-102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4113153/[↩]
- Lumbar puncture: anatomical review of a clinical skill. Boon JM, Abrahams PH, Meiring JH, Welch T. Clin Anat. 2004 Oct; 17(7):544-53. https://www.ncbi.nlm.nih.gov/pubmed/15376294/[↩]
- Accuracy of placement of extradural needles in the L3-4 interspace: comparison of two methods of identifying L4. Ievins FA. Br J Anaesth. 1991 Mar; 66(3):381-2. https://bjanaesthesia.org/article/S0007-0912(17)48180-3/pdf[↩]
- Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? Chakraverty R, Pynsent P, Isaacs K. J Anat. 2007 Feb; 210(2):232-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2100271/[↩]
- Influence of age and sex on the position of the conus medullaris and Tuffier’s line in adults. Kim JT, Bahk JH, Sung J. Anesthesiology. 2003 Dec; 99(6):1359-63. https://www.ncbi.nlm.nih.gov/pubmed/14639149/[↩]
- Guidelines for the use of platelet transfusions. British Committee for Standards in Haematology, Blood Transfusion Task Force. Br J Haematol. 2003 Jul; 122(1):10-23. https://www.ncbi.nlm.nih.gov/pubmed/12823341/[↩]
- Horlocker TT, Wedel DJ, Schroeder DR, Rose SH, Elliott BA, McGregor DG, et al. Preoperative antiplatelet therapy does not increase the risk of spinal hematoma associated with regional anesthesia. Anesth Analg. 1995;80(2):303–9. https://www.ncbi.nlm.nih.gov/pubmed/7818117[↩]
- Recommendations for Anticoagulated Patients Undergoing Image-Guided Spinal Procedures. American Journal of Neuroradiology March 2006, 27 (3) 468-470; http://www.ajnr.org/content/27/3/468.long[↩]
- Layton KF, Kallmes DF, Horlocker TT. Recommendations for anticoagulated patients undergoing image-guided spinal procedures. AJNR Am J Neuroradiol. 2006;27(3):468–70. http://www.ajnr.org/content/27/3/468.long[↩][↩]
- Optimal patient position for lumbar puncture, measured by ultrasonography. Sandoval M, Shestak W, Stürmann K, Hsu C. Emerg Radiol. 2004 Feb; 10(4):179-81. https://www.ncbi.nlm.nih.gov/pubmed/15290485/[↩]
- Arevalo-Rodriguez I, Ciapponi A, Roqué i Figuls M, Muñoz L, Bonfill Cosp X. Posture and fluids for preventing post-dural puncture headache. Cochrane Database of Systematic Reviews 2016, Issue 3. Art. No.: CD009199. DOI: 10.1002/14651858.CD009199.pub3. http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD009199.pub3/full[↩][↩][↩]