Contents
What is medulla oblongata
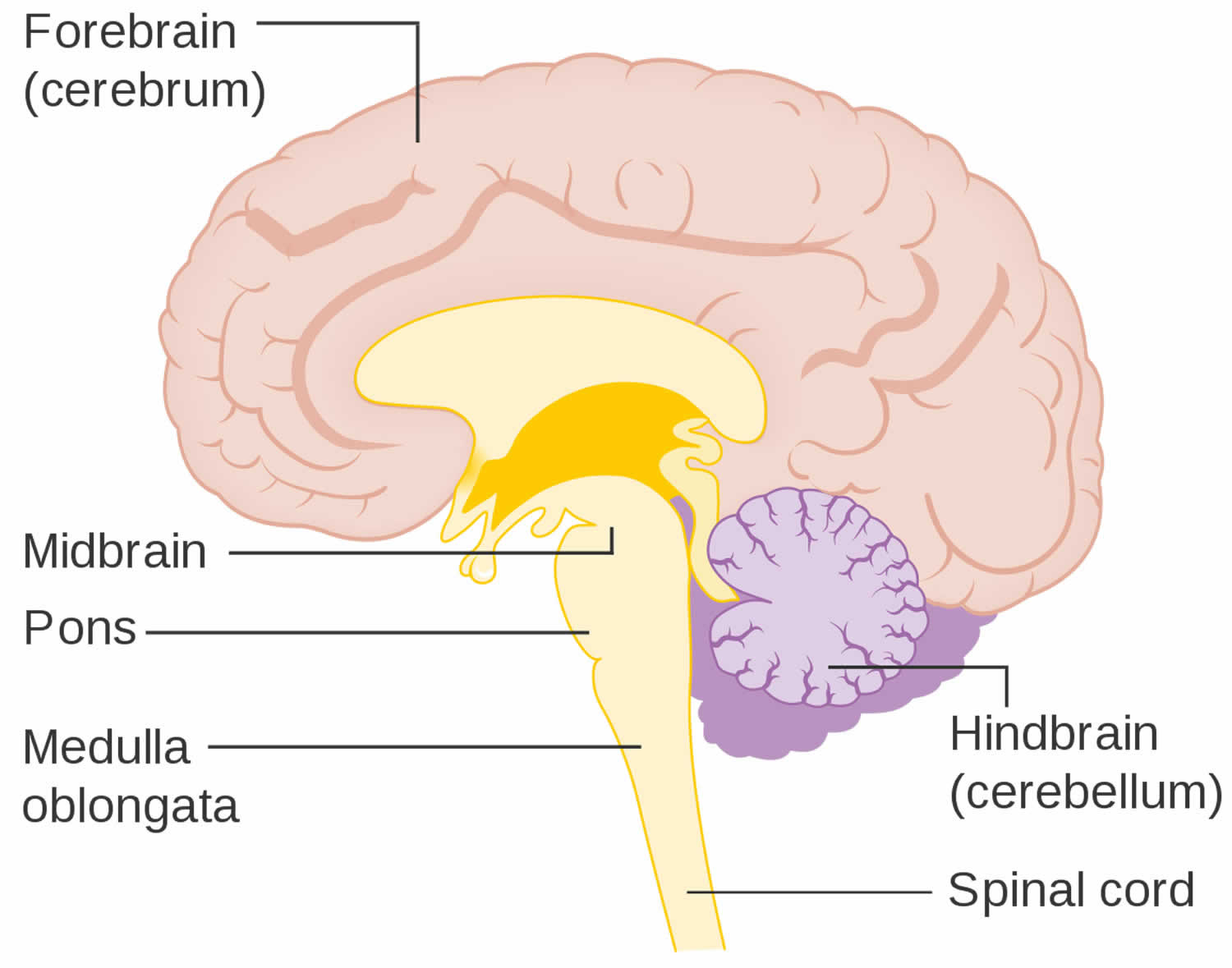
The medulla oblongata or simply the medulla is the most caudal part of the brainstem between the pons superiorly and spinal cord inferiorly. Medulla oblongata is the transition from the spinal cord to the brain, it ends at the foramen magnum or the uppermost rootlets of the first cervical nerve and to which cranial nerves VI to XII are attached. Medulla oblongata contains the vital autonomic cardiovascular and respiratory centers controlling heart rate, blood pressure, and breathing. Medulla oblongata is composed of grey matter, cranial nerve (CN) nuclei 9-12, and white matter tracts 1. White matter fiber tracts connecting the more rostral regions of the brain with the spinal cord must pass through the medulla oblongata.
The medulla oblongata is approximately 3 cm in length and 2 cm in greatest diameter 1. The caudal border of the medulla is the 1st cervical spinal nerves. The superior broad part of the medulla joins the pons 1.
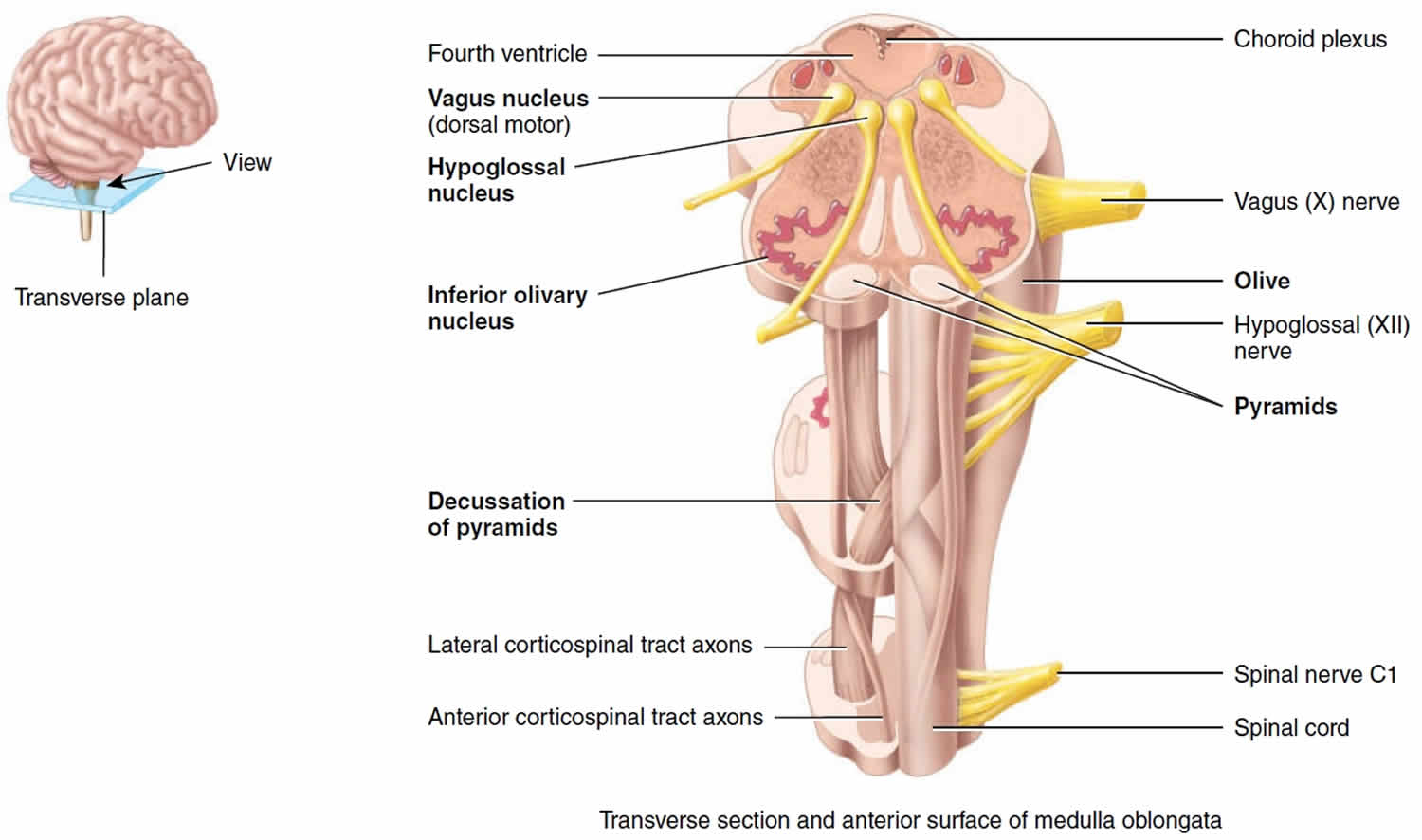
- Externally, two longitudinal ridges called pyramids (Figure 1) flank the ventral midline of the medulla oblongata. These ridges are formed by the pyramidal tracts, large fiber tracts that originate from pyramid-shaped neurons in the cerebrum and descend through the brain stem and spinal cord carrying voluntary motor output to the spinal cord. In the caudal part of the medulla oblongata, 70–90% of these pyramidal fibers cross over to the opposite side of the brain at a point called the decussation of the pyramids (“a crossing”). The result of this crossover is that each cerebral hemisphere controls the voluntary movements of the opposite side of the body (see Figure 2). Just lateral to each pyramid is the olive. This enlargement contains the inferior olivary nucleus, a large wavy fold of gray matter viewable in cross section (Figures 1 and 2). This brain nucleus is a relay station for sensory information traveling to the cerebellum, especially for proprioceptive information ascending from the spinal cord. Relay nuclei such as this process and edit information before sending it along. The inferior cerebellar peduncles are fiber tracts that connect the medulla to the cerebellum dorsally.
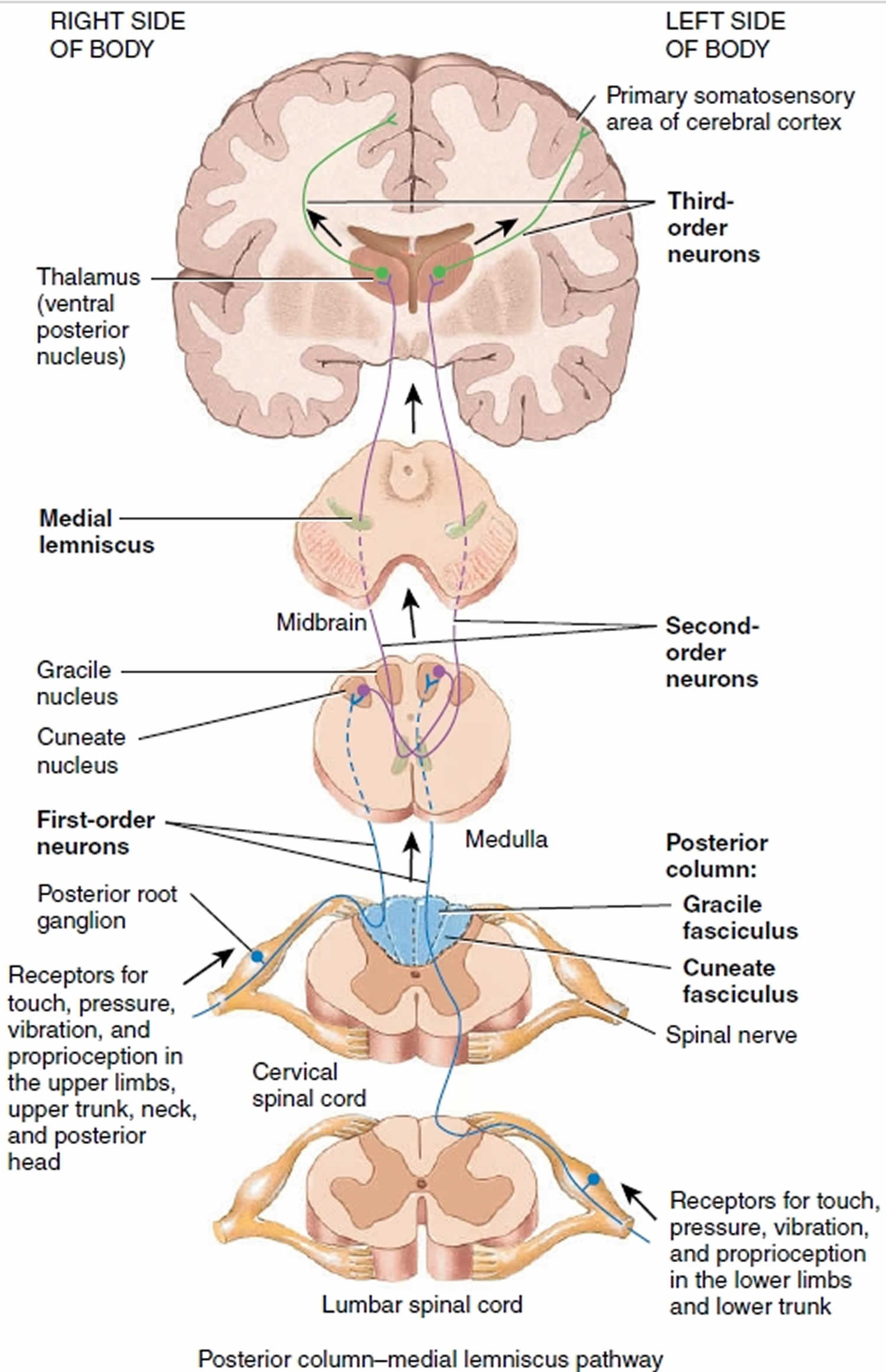
- Internally, two other important relay nuclei are located in the caudal medulla, nucleus fasiculatus and nucleus cuneatus. Ascending fibers carrying general sensation from the discriminative senses (touch, pressure, limb/joint position) from the skin and proprioceptors synapse in these medullary nuclei along their pathway to the cerebrum.
Four pairs of cranial nerve attach to the medulla oblongata. The brain nuclei associated with these cranial nerves may be sensory nuclei that receive sensory input from the cranial nerve or motor nuclei that initiate a motor response which is transmitted on the cranial nerve. The sensory and motor nuclei associated with these cranial nerves lie near the fourth ventricle and can be viewed in a cross section through the medulla (Figure 1).
- The vestibulocochlear nerve (cranial nerve VIII) attaches at the junction of the medulla and the pons and is the sensory nerve of hearing and equilibrium. The vestibular and cochlear nuclei relay sensory input from each of these nerves to other regions of the brain. They are located on the dorsolateral portion of the medulla.
- The glossopharyngeal nerve (cranial nerve IX) innervates part of the tongue and pharynx. The brain nuclei associated with the glossopharyngeal nerve that are illustrated are the nucleus ambiguus, a motor nucleus, and the solitary nucleus, a sensory nucleus.
- The vagus nerve (cranial nerve X) innervates many visceral organs in the thorax and abdomen. There are three brain nuclei associated with the vagus nerve: the dorsal motor nucleus of the vagus, the solitary nucleus, and the nucleus ambiguus.
- Accessory (XI) nerves (cranial portion). These fibers are actually part of the vagus (X) nerves. Nuclei in the medulla oblongata are the origin for nerve impulses that control swallowing via the vagus nerves (cranial portion of the accessory nerves).
- The hypoglossal nerve (cranial nerve XII) innervates tongue muscles. The hypoglossal nucleus, a motor nucleus, is located dorsomedially, just deep to the fourth ventricle.
Running through the core of the brain stem is a loose cluster of brain nuclei called the reticular formation. The brain nuclei in the reticular formation form three columns on each side that extend the length of the brain stem: (1) the midline raphe nuclei, which are flanked laterally by (2) the medial nuclear group and then (3) the lateral nuclear group. Reticular formation nuclei that are clustered around the motor nuclei of the cranial nerves function to coordinate reflexes and autonomic behaviors involving the cranial nerves. The most important nuclei in the medulla’s reticular formation involved with visceral activities are the following:
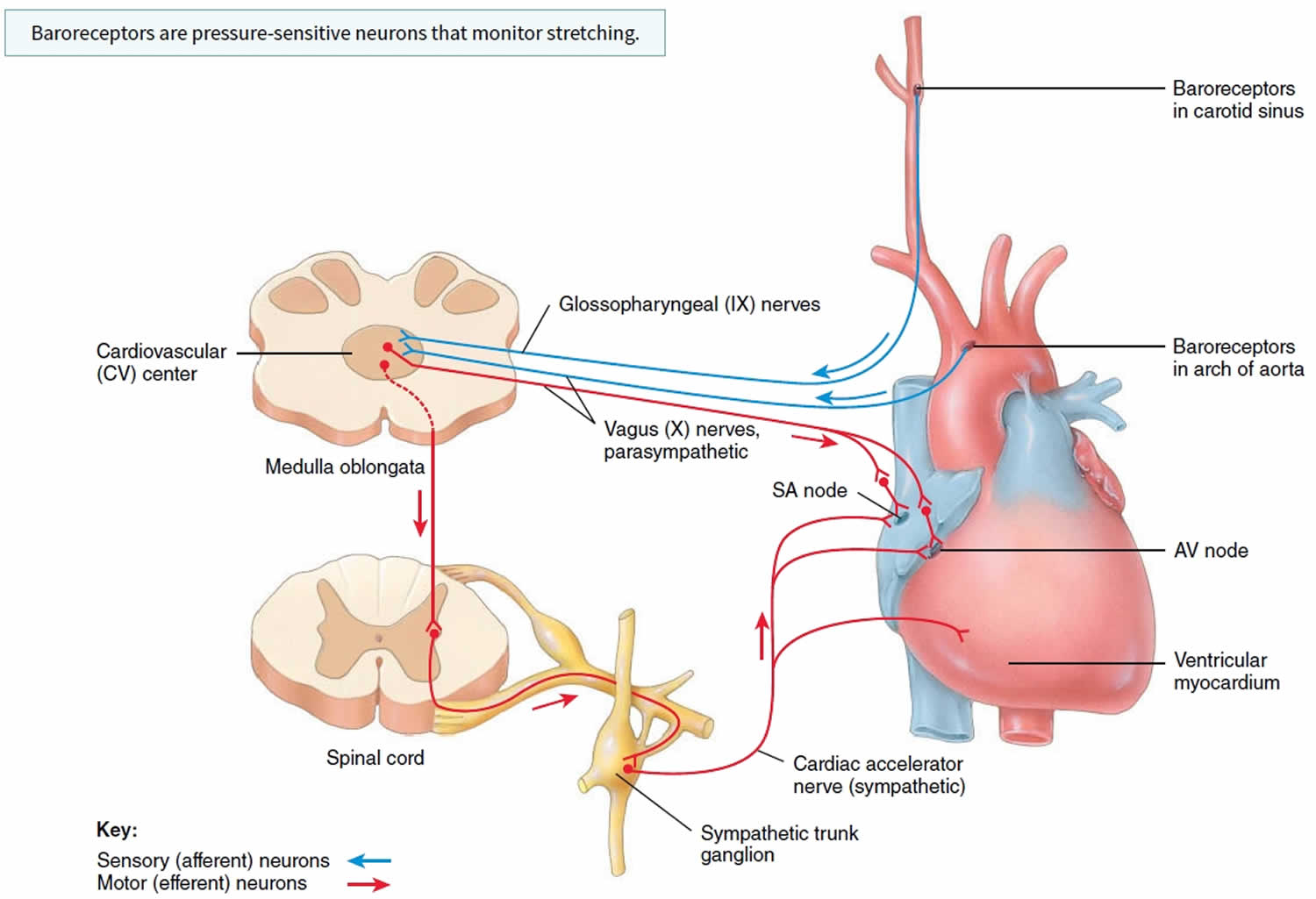
- The cardiac center adjusts the force and rate of the heartbeat.
- The vasomotor center regulates blood pressure by stimulating or inhibiting the contraction of smooth muscle in the walls of blood vessels, thereby constricting or dilating the vessels. Constriction of arteries throughout the body causes blood pressure to rise, whereas dilation reduces blood pressure.
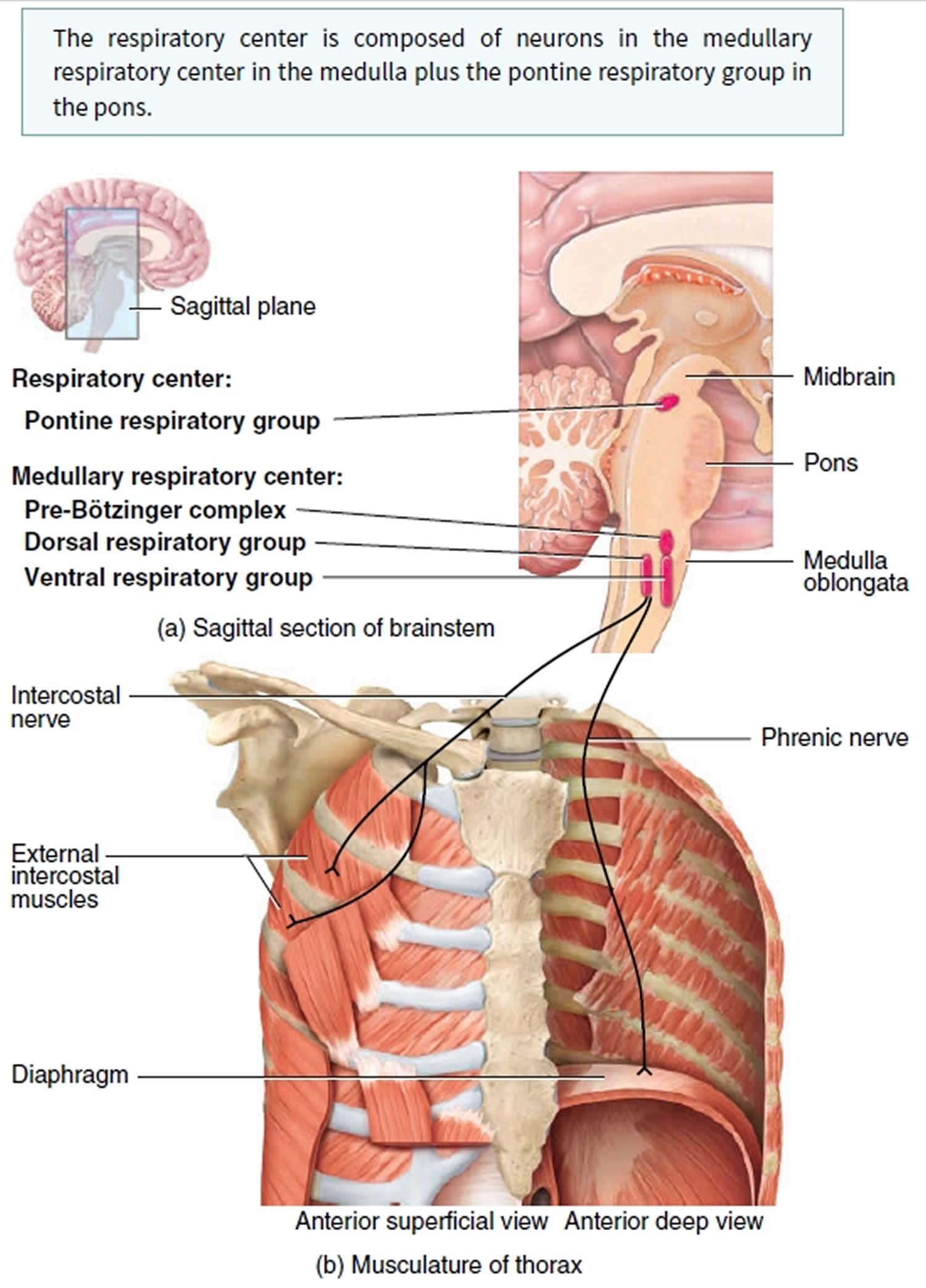
- The medullary respiratory center controls the basic rhythm and rate of breathing.
Medulla oblongata anatomy
Medulla oblongata is separated into two main parts:
- Ventral (anterior) medulla which contains the olive, pyramidal tracts, and cranial nerve 9-12 rootlets
- Tegmentum (dorsal) medulla which contain the cranial nerve nuclei and white matter tracts
Ventral medulla
Pyramids are paired structures located at the medial aspect of ventral medulla and flank the anterior median fissure. It contains the anterior and lateral corticospinal tracts. At the caudal end of pyramids the corticospinal tracts decussate.
Olivary bodies are paired structures located at lateral aspect of ventral medulla, lateral to the pyramids. They are separated from the pyramids by an anterolateral sulcus (pre-olivary sulcus). There is also a post-olivary sulcus lateral to the olivary bodies. Olivary bodies contain the superior and larger inferior olivary nuclei.
Medulla tegmentum
The dorsal aspect of the medulla contains the posterior median sulcus (most dorsal medial sulcus) and more lateral posterolateral sulcus. Between these sulci are the fasciculus gracilis and nuclei forming gracilis tubercle at the midline and fasciculus cuneatus and nuclei forming cuneate tubercle more laterally.
Superiorly the dorsal surface of the medulla is slightly depressed, forming the diamond-shaped rhomboid fossa which is the floor of the fourth ventricle. The superior dorsal aspect of medulla is occupied by the inferior cerebellar peduncle situated between the lower part of the fourth ventricle. The inferior dorsal and lateral aspect of the medulla is surrounded by the cisterna magna (posterior cerebellomedullary cistern), and lateral cerebellomedullary cistern.
The median aperture (foramen of Magendie) and the more superior lateral apertures (foramina of Luschka) open at the level of the pons, with the canals projecting to the level of the medulla region and terminating into the cisterna magna and lateral cerebellomedullary cistern respectively.
Cranial nerves
The nuclei of the cranial nerves in the medulla originate in the tegmentum, but the nerve roots exit ventrally. Cranial nerves IX and X as well as the roots of XI exit the lateral medulla at the post-olivary sulcus, posterior to olivary bodies. Cranial nerve XII emerges between the pyramid and the olive at the pre-olivary sulcus as a number of rootlets.
Blood supply
- posterior inferior cerebellar artery (PICA) supplies the lateral aspect of the medulla oblongata.
- anterior spinal artery supplies the entire medial aspect.
- direct branches of the distal vertebral artery supplies an area between the other two main arteries.
Figure 1. Medulla oblongata anatomy
Figure 2. Medulla oblongata neural pathways
Medulla oblongata location
The medulla oblongata is continuous with the superior part of the spinal cord; it forms the inferior part of the brainstem. Medulla oblongata begins at the foramen magnum and extends to the inferior border of the pons, a distance of about 3 cm (1.2 in.). A part of the fourth ventricle lies dorsal to the superior half of the medulla oblongata.
Medulla oblongata function
The medulla oblongata’s white matter contains all sensory (ascending) tracts and motor (descending) tracts that extend between the spinal cord and other parts of the brain. Some of the white matter forms bulges on the anterior aspect of the medulla. These protrusions, called the pyramids are formed by the large corticospinal tracts that pass from the cerebrum to the spinal cord. The corticospinal tracts control voluntary movements of the limbs and trunk. Just superior to the junction of the medulla oblongata with the spinal cord, 90% of the axons in the left pyramid cross to the right side, and 90% of the axons in the right pyramid cross to the left side. This crossing is called the decussation of pyramids (decuss = crossing) and explains why each side of the brain controls voluntary movements on the opposite side of the body.
The medulla oblongata also contains several nuclei. A nucleus is a collection of neuronal cell bodies within the central nervous system. Some of these nuclei control vital body functions. Examples of nuclei in the medulla oblongata that regulate vital activities include the cardiovascular center and the medullary rhythmicity center. The cardiovascular center regulates the rate and force of the heartbeat and the diameter of blood vessels (see Figure 3). The medullary respiratory center adjusts the basic rhythm of breathing (see Figure 4).
Figure 3. Medulla oblongata cardiovascular center regulates heartbeat and the diameter of blood vessels
Figure 4. Medulla oblongata respiratory center adjusts the basic rhythm of breathing
Besides regulating heartbeat, blood vessel diameter, and the normal breathing rhythm, nuclei in the medulla oblongata also control reflexes for vomiting, swallowing, sneezing, coughing, and hiccupping. The vomiting center of the medulla oblongata causes vomiting, the forcible expulsion of the contents of the upper gastrointestinal (GI) tract through the mouth. The deglutition center of the medulla oblongata promotes deglutition (swallowing) of a mass of food that has moved from the oral cavity of the mouth into the pharynx (throat). Sneezing involves spasmodic contraction of breathing muscles that forcefully expel air through the nose and mouth. Coughing involves a long-drawn and deep inhalation and then a strong exhalation that suddenly sends a blast of air through the upper respiratory passages. Hiccupping is caused by spasmodic contractions of the diaphragm (a muscle of breathing) that ultimately result in the production of a sharp sound on inhalation.
Just lateral to each pyramid is an oval-shaped swelling called an olive (see Figure 1). Within the olive is the inferior olivary nucleus, which receives input from the cerebral cortex, red nucleus of the midbrain, and spinal cord. Neurons of the inferior olivary nucleus extend their axons into the cerebellum, where they regulate the activity of cerebellar neurons. By influencing cerebellar neuron activity, the inferior olivary nucleus provides instructions that the cerebellum uses to make adjustments to muscle activity as you learn new motor skills.
Nuclei associated with sensations of touch, pressure, vibration, and conscious proprioception are located in the posterior part of the medulla oblongata. These nuclei are the right and left gracile nucleus (slender) and cuneate nucleus (wedge). Ascending sensory axons of the gracile fasciculus and the cuneate fasciculus, which are two tracts in the posterior columns of the spinal cord, form synapses in these nuclei (see Figure 2). Postsynaptic neurons then relay the sensory information to the thalamus on the opposite side of the brain. The axons ascend to the thalamus in a band of white matter called the medial lemniscus (ribbon), which extends through the medulla, pons, and midbrain. The tracts of the posterior columns and the axons of the medial lemniscus are collectively known as the posterior column–medial lemniscus pathway.
The medulla oblongata also contains nuclei that are components of sensory pathways for gustation (taste), audition (hearing), and equilibrium (balance). The gustatory nucleus of the medulla oblongata is part of the gustatory pathway from the tongue to the brain; it receives gustatory input from the taste buds of the tongue. The cochlear nuclei of the medulla oblongata are part of the auditory pathway from the inner ear to the brain; they receive auditory input from the cochlea of the inner ear. The vestibular nuclei of the medulla oblongata and pons are components of the equilibrium pathway from the inner ear to the brain; they receive sensory information associated with equilibrium from proprioceptors (receptors that provide information regarding body position and movements) in the vestibular apparatus of the inner ear.
Finally, the medulla oblongata contains nuclei associated with the following five pairs of cranial nerves.
- Vestibulocochlear (VIII) nerves. Several nuclei in the medulla oblongata receive sensory input from and provide motor output to the cochlea of the internal ear via the vestibulocochlear nerves. These nerves convey impulses related to hearing.
- Glossopharyngeal (IX) nerves. Nuclei in the medulla oblongata relay sensory and motor impulses related to taste, swallowing, and salivation via
the glossopharyngeal nerves. - Vagus (X) nerves. Nuclei in the medulla oblongata receive sensory impulses from and provide motor impulses to the pharynx and larynx and many thoracic and abdominal viscera via the vagus nerves.
- Accessory (XI) nerves (cranial portion). These fibers are actually part of the vagus (X) nerves. Nuclei in the medulla oblongata are the origin for nerve impulses that control swallowing via the vagus nerves (cranial portion of the accessory nerves).
- Hypoglossal (XII) nerves. Nuclei in the medulla oblongata are the origin for nerve impulses that control tongue movements during speech and swallowing via the hypoglossal nerves.
Medulla oblongata damage
Wallenberg syndrome
Wallenberg syndrome also called lateral medullary syndrome or posterior inferior cerebellar artery (PICA) syndrome is a clinical syndrome caused by a stroke of the lateral medulla oblongata, in the region supplied by the vertebral or posterior inferior cerebellar artery (PICA) of the brain stem. Wallenberg syndrome is most commonly due to occlusion of the intracranial portion of the vertebral artery followed by posterior inferior cerebellar artery (PICA) and its branches 2.
Lateral medullary syndrome (Wallenberg syndrome) is characterized by:
- Vestibulocerebellar symptoms: vertigo, falling towards the side of lesion, diplopia, and multidirectional nystagmus (inferior cerebellar peduncle and vestibular nucleus) 2.
- Autonomic dysfunction: ipsilateral Horner syndrome, hiccups 2.
- Sensory symptoms: initially abnormal stabbing pain over the ipsilateral face then loss of pain and temperature sensation over the contralateral side of body (spinal trigeminal nucleus involvement) 2.
- Ipsilateral bulbar muscle weakness: hoarseness, dysphonia, dysphagia, and dysarthria, decreased gag reflex (nucleus ambiguus) 2.
Wallenberg syndrome signs and symptoms may include swallowing difficulties, dizziness, hoarseness, nausea and vomiting, nystagmus, and problems with balance. Some people have uncontrollable hiccups, loss of pain and temperature sensation on one side of the face, and/or weakness or numbness on one side of the body. Wallenberg syndrome is often caused by a stroke in the brain stem. Treatment addresses each symptom and may include a feeding tube for swallowing problems, speech and/or swallowing therapy, and medication for pain. While some people’s symptoms may improve within weeks or months, others may have long-term neurological problems 3.
Wallenberg syndrome cause
The most common underlying cause of Wallenberg syndrome is a brain stem stroke in the vertebral or posterior inferior cerebellar arteries of the brain stem 4. However, several other disorders or conditions reportedly have been associated with Wallenberg syndrome, including 5:
- mechanical trauma to the vertebral artery in the neck
- vertebral arteritis (inflammation of the wall of the artery)
- metastatic cancer
- hematoma
- aneurysm of the vertebral artery
- herpetic brainstem encephalitis (relating to herpes)
- head injury
- arteriovenous malformations (AVMs)
- multiple sclerosis
- varicella infection
- brainstem tuberculoma (a rare form of tuberculosis)
Wallenberg syndrome signs and symptom
Wallenberg syndrome may cause a variety of symptoms depending on the specific cause and the exact location of the damage to the brain. Symptoms may include 6:
- pain and temperature sensory loss on one side of the face as well as on the opposite side of the body
- rapid involuntary movements of the eyes (nystagmus)
- problems with balance and gait (walking) coordination
- vomiting
- vertigo
- nystagmus
- dysphagia
- hoarseness
- uncontrollable hiccups
- Horner syndrome (decreased pupil size, a drooping eyelid and decreased sweating on the affected side of the face) with visual deficits
Symptoms include difficulties with swallowing, hoarseness, dizziness, nausea and vomiting, rapid involuntary movements of the eyes (nystagmus), and problems with balance and gait coordination. Some individuals will experience a lack of pain and temperature sensation on only one side of the face, or a pattern of symptoms on opposite sides of the body – such as paralysis or numbness in the right side of the face, with weak or numb limbs on the left side. Uncontrollable hiccups may also occur, and some individuals will lose their sense of taste on one side of the tongue, while preserving taste sensations on the other side. Some people with Wallenberg’s syndrome report that the world seems to be tilted in an unsettling way, which makes it difficult to keep their balance when they walk.
Wallenberg syndrome treatment
Treatment for Wallenberg’s syndrome focuses primarily on relieving symptoms and rehabilitation. A feeding tube may be necessary if swallowing is very difficult. Speech/swallowing therapy may be beneficial. In some cases, medication may be used to reduce or eliminate pain. Some doctors report that the anti-epileptic drug gabapentin appears to be an effective medication for individuals with chronic pain. Treatment may also depend on the underlying cause and/or how quickly it is identified.
Wallenberg syndrome prognosis
The prognosis for someone with Wallenberg’s syndrome depends upon the size and location of the area of the brain stem damaged by the stroke. Some individuals may see a decrease in their symptoms within weeks or months. Others may be left with significant neurological disabilities for years after the initial symptoms appeared.
Medial medullary syndrome
Medial medullary syndrome also known as Déjerine syndrome, is secondary to thrombotic or embolic occlusion of small perforating branches from vertebral or proximal basilar artery supplying the medial aspect of medulla oblongata 7. Represents less than 1% of brainstem stroke syndromes 8.
Medial medullary syndrome is characterized by contralateral hemiplegia/hemiparesis as well as hemisensory loss with ipsilateral hypoglossal palsy (ipsilateral tongue weakness and atrophy) from involvement of CN XII nucleus 7. Other manifestations such as vertigo, nausea, or contralateral limb ataxia are also reported 7.
Wallerian degeneration
Wallerian degeneration is the process of antegrade degeneration of the axons and their accompanying myelin sheaths following proximal axonal or neuronal cell body lesions. It may result following neuronal loss due to cerebral infarction, trauma, necrosis, focal demyelination, or hemorrhage.
In cases of cerebral infarction, Wallerian degeneration appears in the chronic phase (>30 days).
Wallerian degeneration is usually classified into four stages:
- Degeneration of the axons and myelin sheaths with mild chemical changes (0-4 weeks)
- Rapid destruction of myelin protein fragments that were already degenerated, lipids remain intact (4-14 weeks)
- Gliosis replaces the degenerated axons and myelin sheaths, myelin lipid breakdown (>14 weeks)
- Atrophy of the white matter tracts (months to years)
Brainstem glioma
Brainstem gliomas consist of a heterogeneous group which vary greatly in histology and prognosis.
It should be noted that if not otherwise specified the term brainstem glioma usually refers to the most common histology, the diffuse brainstem glioma, and in children is most likely a diffuse midline glioma H3 K27M–mutant.
Brainstem gliomas account for ~25% of all posterior fossa tumors and are most common in children between 7 and 9 years of age 9. There is no recognized gender or racial predilection. Childhood brain stem glioma is a rare condition in which abnormal cells develop in the tissues of the brain stem (the part of the brain connected to the spinal cord). Childhood brain stem glioma can be benign (noncancerous) or malignant (cancerous). The severity of the condition and the associated signs and symptoms vary based on the size and location of the tumor and how quickly the tumor is growing. Common features include difficulty walking; loss of the ability to move one side of the body or face; vision or hearing problems; headaches (particularly in the morning); nausea and vomiting; unusual sleepiness; and behavioral changes. In most cases, the underlying cause of childhood brain stem glioma is unknown. Certain genetic conditions, such as neurofibromatosis type I, are associated with an increased risk of childhood brainstem glioma. Treatment varies but may include surgery, radiation therapy, chemotherapy, cerebrospinal fluid diversion, observation, and targeted therapy 10.
Brainstem gliomas are also recognized in adults, although they are rare accounting for only 2% of adult brain tumors 11. They typically occur in younger adults (third and fourth decade) and tend to be of low grade (WHO I or II) 11.
Although the exact clinical presentation will vary according to location and size of the brain stem glioma, in general patients will exhibit a combination of 12:
- ataxia
- cranial nerve palsies
- long tract signs
- hydrocephalus
The duration of symptoms is usually much shorter in diffuse gliomas, in which the history is typically very short (a few days) 12. Additionally, diffuse gliomas more frequently have multiple cranial nerve palsies.
Brainstem glioma classification
The most frequently used classification system is to divide these tumors into four types 9:
- Diffuse brainstem glioma: most are diffuse midline glioma H3 K27M–mutant
- Focal brainstem glioma: tectal plate glioma and other focal gliomas
- Dorsally exophytic
- Cervicomedullary: probably an artificial group made up of the downward extension of true brainstem gliomas or upward extension of upper cervical cord intramedullary spinal cord tumors 9
Brainstem glioma location
As a general rule mesencephalic tumors tend to be of a lower grade than those in the pons and medulla 13.
Pontine
- most common location
- classic location for the childhood ‘brainstem glioma’ which tends to refer to a diffuse pontine glioma, the majority of which are diffuse midline gliomas, H3 K27M–mutant
- focal dorsally exophytic brainstem glioma is an uncommon variant accounting for only 10% of pontine tumors, and has a much better prognosis, as it usually represents a pilocytic astrocytoma
- overall survival of pontine gliomas is 10% at 5 years
Mesencephalic
- includes diffuse, focal, exophytic and tectal variants.
- focal brainstem gliomas are more common here than elsewhere in the brainstem
- tectal plate gliomas are typically indolent
Medulla oblongata
- least common location
- includes focal dorsally exophytic, focal, diffuse and cervicomedullary junction variants
- cervicomedullary junction tumors usually represent upper cervical tumors extending superiorly
- most common location for NF1 associated tumors
Brainstem glioma treatment
Again, both treatment and prognosis are significantly influenced by tumor type, morphology and location. Radiation is a key part of treatment.
As a general rule, dorsal exophytic tumors and cervicomedullary tumors tend to do best with surgery, whereas surgery has no role in the management of diffuse brainstem gliomas.
Brainstem glioma prognosis
- diffuse
- terrible prognosis
- 90-100% patients die within 2 years of diagnosis 14
- focal (tectal glioma): excellent long-term survival with CSF shunting (essentially benign lesions)
- focal (other): good long-term prognosis with surgery
- (dorsally) exophytic tumors: good long-term prognosis with surgery
Syringobulbia
Syringobulbia is a rare entity and refers to a syrinx that extends into the medulla oblongata 15. Some authors use syringobulbia to refer to a syrinx present in any portion of the brainstem rather than specifically involving the medulla oblongata, and therefore encompassing syringopontia and syringomesencephaly as well.
Patients with syringobulbia demonstrate a wide variety of bulbar neurological symptoms as well as symptoms relating to syringomyelia, depending on where exactly the syrinx is located 15.
When present, it is seen in continuity with a long syrinx that demonstrates syringomyelia 16. Syringobulbia is pathologically identical to a syringomyelia, as simply an extension of the collection of cerebrospinal fluid within the cord with dissection through the ependymal lining of the central canal of the spinal cord.
Syringobulbia signs and symptoms
Dissociated sensory loss – pain and temperature are disrupted whereas light touch, proprioception, and vibratory sensation are often unaffected. Sensory disturbance is almost always asymmetric in a cape-like over the shoulders and back. Pain is frequently felt in the neck and shoulders.
Central Cord Syndrome: Centrally located syrinx, that injures the fibers located centrally (cervical) before the fibers located laterally (thoracic, lumbar, and sacral, in this order) in the spinal cord. A cervical syrinx often results in early symptoms (sensory loss and motor weakness) of the more distal muscles of the fingers and hands followed by late signs in the proximal muscles of the shoulders, trunk, and later the legs. A thoracic syrinx may cause motor weakness and sensory disturbance of the trunks followed by the legs.
Brainstem symptoms and signs: When the syrinx extends into the brainstem (syringobulbia), symptoms are common early on in the process. These usually consist of dysfunction of the lower cranial nerves with coughing, aspiration, and dysphagia.
Scoliosis: May result from unequal weakness of the spinal muscles. Young age, atypical curve, rapid curve progression, and back pain associated with scoliosis should alert one to the possible role of syringomyelia.9
Chronic pain: is associated with a variety of chronic pain syndromes, particularly in posttraumatic syringomyelia, in which there is an initial traumatic injury followed by later spinal cord injury secondary to syrinx distention; however, while it is nearly impossible to determine if the pain is caused by the syrinx or the primary pathology, it appears that treatment of the syrinx rarely results in resolution of the pain, which suggests that the pain may be related to the initial spinal cord injury.
Syringobulbia diagnosis
Spinal MRI shows a dilated cavity with the same intensity of CSF on T2-weighted imaging. A complete brain and spinal MRI with and without Gadolinium is needed to determine the primary pathology. Cine MRI may also help in diagnosing abnormal CSF flow patterns. So far, results have been conflicting. Rarely, myelography may help to sort some of the more difficult cases.
Syringobulbia treatment
Asymptomatic syringobulbia patients with small syrinx cavities and no obvious etiology are best managed with watchful waiting and serial imaging exams. The management of symptomatic or large syringobulbia is focused on identifying and treating the associated condition, which is the underlying cause of the syrinx 17. These etiologies include: Chiari I malformation; congenital tethered cord (spina bifida occulta); acquired tethered cord from previous surgery (such as myelomeningocele repair); spinal arachnoiditis (old viral or bacterial meningitis, etc.); spinal trauma; spinal cord tumor; VP shunt malfunction or Chiari II in spina bifida; idiopathic (unknown cause).
Chiari I malformation: Diagnosis made on MRI. Syrinx associated with Chiari I malformation is usually treated with posterior fossa decompression. If the syrinx does not resolve, one would consider (re-explore the posterior fossa and expand the decompression; consideration of subtle craniocervical instability; consideration of benign intracranial hypertension; consideration of shunting the syrinx directly; others).
Spina bifida: The syrinx may be the result of tethered spinal cord from the myelomenigocele repair, the Chiari II malformation, or ventricular shunt malfunction. The location of the syrinx within the spinal cord may help to dictate the treatment (i.e. lumbar syrinx may respond to tethered cord release and cervical syrinx to VP shunt revision or Chiari II decompression). Most surgeons agree to check the shunt first.
Spina bifida occulta (tethered cord): Diagnosis made on MRI. Patients with congenital tethered spinal cord should undergo exploration and tethered cord release in order to prevent future neurological and urological deficits. If the syrinx is large in cross-sectional diameter, it is often drained at the same surgery 18.
Arachnoiditis (spinal inflammation): Diagnosis made on MRI. Spinal cord decompression with dissection of the arachnoid scar is performed. Reestablish normal CSF flow. If the arachnoiditis is so diffuse that it becomes impossible to achieve a good dissection, shunt the syrinx to the pleural or peritoneal cavities.
Spinal trauma: Post-traumatic syrinx is difficult to treat successfully. The syrinx can be a result of arachnoiditis and blockage of flow causing expansion of the cord or may represent an atrophic change secondary to the long-term consequence of a cord contusion 19. If a true syrinx is suspected, the treatment would consist of either arachnoidal dissection as above, or a syrinx shunt into the pleura or peritoneum.
Spinal cord tumor: Diagnosis made on MRI. syringobulbia associated with an intrinsic spinal cord tumor often have high protein content and may represent a secretory process from the tumor cells, or an obstructive process similar to other etiologies. Patients with tumor related cysts should be treated with tumor resection 20. It is rare to have to shunt the syrinx in these situations.
Idiopathic (unknown cause): In a large percentage of patients, the syrinx has no identifiable cause. Those are difficult to treat. Most large and/or symptomatic syrinxes are treated with syrinx shunting. Rarely, a posterior fossa decompression is found to be successful in the absence of a Chiari malformation. Such patients who respond to decompression are thought to have a Chiari zero. It is so far impossible to predict which patient with idiopathic syringobulbia would respond to posterior fossa decompression. The strict definition of Chiari zero 21 is “idiopathic syringobulbia that responds to posterior fossa decompression.”
Residual central canal: Many patients are referred for evaluation of a thin, fluid-filled structure within the spinal cord with no associated pathologies. This structure usually tapers at each end and likely represents a normal variant: a remnant of a central canal normally present in embryos. These are usually incidental findings on scans obtained for unrelated issues. The patients are usually neurologically normal. In patients with back pain, other causes of the pain should be investigated.
Syringobulbia prognosis
It is generally accepted that if the causative pathology is identified and treated, the long-term improvement and resolution of the syrinx is good 22. Prognosis is also largely dependent on the prognosis of the primary pathologic that resulted in the syrinx. The syrinx in Chiari I patients generally responds well over time to posterior fossa decompression. In spina bifida, the symptoms must be separated into those related to the syrinx, the tethered cord, shunt malfunction, or less commonly, the Chiari II malformation. The results are often good when the etiology is found8 In spina bifida occulta, a large syrinx has best prognosis with drainage of the syrinx at the time of tethered cord release. A small cavity is likely to remain stable over time and may even regress obviating the need for any treatment other than tethered cord release 18. The diagnosis of tethered spinal cord is made by MRI. In patients with spinal inflammation or arachnoiditis, stabilization of the syrinx can be achieved with decompression and arachnoid dissection in 83% of patients with focal scarring but only 17% of patients with scarring over multiple levels 23. Syrinx shunting alone results in very high recurrence rates. In post-traumatic patients, outcome is largely dependent on the pathology. If pain is secondary to atrophy from chronic damage to the spinal cord, it is not surprising that it will not resolve with shunting of the cavity. Long-term recurrence rates with shunting alone have been in excess of 80% 23. When considering surgical treatment, it should be noted that patients who have undergone previous surgery and failed, may have even worse outcomes. Patients with tumor related syringobulbia generally have good outcomes with tumor resection, assuming the tumor itself is curable. It appears that preoperative neurologic status is the main factor determining neurological outcome 20.
- DSc SSP. Gray’s Anatomy. Churchill Livingstone. (2011) ISBN:0443066841[↩][↩][↩]
- Kim JS. Pure lateral medullary infarction: clinical-radiological correlation of 130 acute, consecutive patients. Brain. 2003;126 (8): 1864-72. doi:10.1093/brain/awg169[↩][↩][↩][↩][↩]
- Wallenberg’s Syndrome Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Wallenbergs-Syndrome-Information-Page[↩]
- Qiu W, Wu JS, Carroll WM, Mastaglia FL, Kermode AG. Wallenberg syndrome caused by multiple sclerosis mimicking stroke. J Clin Neurosci. December 2009; 16(12):1700-1702. https://www.ncbi.nlm.nih.gov/pubmed/19800798[↩]
- Verma R, Sharma P. Lateral medullary syndrome due to brain stem tuberculoma. J Assoc Physicians India. June 2011; 59:382-384. https://www.ncbi.nlm.nih.gov/pubmed/21751596[↩]
- Louis DW, Dholakia N, Raymond MJ. Wallenberg Syndrome with Associated Motor Weakness in a Two-Week-Postpartum Female. Case Rep Neurol. September 23, 2015; 7(3):186-190. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4611068[↩]
- Ropper AH, Samuels MA, Klein JP. Adams and Victor’s principles of neurology 10th ed. New York: McGraw-Hill Medical Pub. Division; 2014.[↩][↩][↩]
- Bassetti C, Bogousslavsky J, Mattle H et-al. Medial medullary stroke: report of seven patients and review of the literature. Neurology. 1997;48 (4): 882-90[↩]
- McLone DG, Neurosurgeons AS, Neurosurgery AA. Pediatric neurosurgery, surgery of the developing nervous system. W B Saunders Co. (2001) ISBN:072168209X[↩][↩][↩]
- Brain and Spinal Cord Tumors in Children. https://www.cancer.org/cancer/brain-spinal-cord-tumors-children.html[↩]
- Mehta MP. Principles and Practice of Neuro-Oncology, A Multidisciplinary Approach. Demos Medical Pub. (2010) ISBN:1933864788[↩][↩]
- Albright AL, Adelson PD, Pollack IF. Principles and practice of pediatric neurosurgery. Thieme Medical Pub. (2007) ISBN:1588903958[↩][↩]
- Greenberg MS. Handbook of neurosurgery. George Thieme Verlag. (2006) ISBN:313110886X.[↩]
- Keating RF, Goodrich JT, Packer RJ. Tumors of the pediatric central nervous system. George Thieme Verlag. (2001) ISBN:0865778485[↩]
- Williams B. Syringobulbia: a surgical review. Acta neurochirurgica. 123 (3-4): 190[↩][↩]
- Menezes AH, Greenlee JD, Longmuir RA, Hansen DR, Abode-Iyamah K. Syringohydromyelia in association with syringobulbia and syringocephaly: case report. Journal of neurosurgery. Pediatrics. 15 (6): 657-61. doi:10.3171/2014.11.PEDS14189[↩]
- Hida K, Iwasaki Y, Koyanagi I, Sawamura Y, Abe H. Surgical indication and results of foramen magnum decompression versus syringosubarachnoid shunting for syringomyelia associated with Chiari I malformation. Neurosurgery 1995;37:673-678; discussion 678-679[↩]
- Iskandar BJ, Oakes WJ, McLaughlin C, Osumi AK, Tien RD. Terminal syringohydromyelia and occult spinal dysraphism. J Neurosurg 1994;81:513-519[↩][↩]
- Potter K, Saifuddin A. Pictorial review: MRI of chronic spinal cord injury. Br J Radiol 2003;76:347-352[↩]
- Samii M, Klekamp J. Surgical results of 100 intramedullary tumors in relation to accompanying syringomyelia. Neurosurgery 1994;35:865-873; discussion 873[↩][↩]
- Iskandar BJ, Hedlund GL, Grabb PA, Oakes WJ. The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression. J Neurosurg 1998;89:212-216[↩]
- Tubbs RS, McGirt MJ, Oakes WJ. Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg 2003;99:291-296.[↩]
- Klekamp J, Batzdorf U, Samii M, Bothe HW. Treatment of syringomyelia associated with arachnoid scarring caused by arachnoiditis or trauma. J Neurosurg 1997;86:233-240[↩][↩]