Contents
What is menorrhagia
Menorrhagia or heavy periods are hard to define, but if you feel you are using more tampons or sanitary towels than usual or blood is leaking through to your clothes and bedding, this usually means your period is heavy. Menorrhagia can also mean you need to change a pad overnight, you’re passing clots larger than a 50 cent piece, or you bleed for more than 7-8 days.
Heavy menstrual bleeding affects about one in five women 1 and is a common problem in the 30-50 year old age group.
- It’s important to note that women who have gone through menopause should not have any vaginal bleeding/spotting. If this occurs you should see your doctor.
How can heavy bleeding affect you?
You may:
- feel fatigued, exhausted, dizzy and look pale
- have low iron levels because of the blood loss
- have cramping and pain in the lower abdomen
- have to change sanitary products very frequently
- fear bleeding through to your clothes and this affects your daily activities
How much is heavy bleeding?
It’s difficult to define exactly what a menorrhagia (heavy period) is because this varies from woman to woman. What’s heavy for one woman may be normal for another.
The average amount of blood lost during a period is 30 to 40 ml, with 9 out of 10 women losing less than 80 ml. Menorrhagia or heavy menstrual bleeding is considered to be 60 ml or more in each cycle or periods lasting more than seven to eight days.
But it’s not usually necessary to measure blood loss. Most women have a good idea of how much bleeding is normal for them during their period, and can tell when this amount increases or decreases.
A good indication that your blood loss is excessive is if:
- you feel you’re using an unusually high number of tampons or pads
- you experience flooding (heavy bleeding) through to your clothes or bedding
- you need to use tampons and towels together
- bleeding or ‘flooding’ not contained within a pad/tampon (especially wearing the largest size)
- changing a pad/tampon every hour or less
- changing a pad overnight
- clots greater than a 50 cent piece in size
- bleeding for more than 7-8 days
Menorrhagia doesn’t necessarily mean there’s anything seriously wrong, but it can affect a woman physically and emotionally, and disrupt everyday life.
You should visit your doctor if menorrhagia are disrupting your everyday life. Your doctor may want to investigate the possible causes of heavy bleeding to rule out any other health conditions which may be causing it.
Blood is full of iron, which helps red blood cells carry oxygen around the body. Heavy blood loss month after month can lead to a loss of iron resulting in iron deficiency or, if the iron deficiency is prolonged or severe, iron deficiency anemia (low hemoglobin).
Menorrhagia anemia symptoms
The most common symptoms of anemia include:
- tiredness
- shortness of breath
- palpitations (irregular heart beat).
Some people also experience:
- headaches
- altered sense of taste
- ringing in their ears (tinnitus)
- a sore tongue.
If you are concerned about this, you should visit your doctor.
Here is some self-care advice for coping with menorrhagia:
- Make sure you change your tampon or sanitary towel at regular intervals. The recommended time frame is every four to eight hours for a tampon, and every four to five hours for a sanitary towel.
- You should never leave a tampon in for longer than eight hours. You could try using a higher absorbency tampon and consider using sanitary towels as well.
- You may need to use more tampons or towels on the heavier days of your period. However, if you are changing your towel every one to two hours due to heavy blood loss, you should visit your doctor for advice.
Seek medical help before your next scheduled exam if you experience:
- Vaginal bleeding so heavy it soaks at least one pad or tampon an hour for more than two hours
- Bleeding between periods or irregular vaginal bleeding
- Any vaginal bleeding after menopause
Menorrhagia causes
About 50% of women with heavy menstrual bleeding have no abnormalities in their uterus. It may be related to hormonal or chemical levels in the endometrium (the internal lining of the uterus) or conditions not yet identified in the endometrium. In some cases, the cause of menorrhagia can’t be identified.
In the other 50% of cases, there are a number of conditions and some treatments that can cause heavy menstrual bleeding.
Conditions that can cause menorrhagia include:
- Polycystic ovary syndrome (PCOS) – a common condition that affects how the ovaries work; it causes irregular periods, and periods can be heavy when they start again
- Pelvic inflammatory disease (PID) – an infection in the upper genital tract (the womb, fallopian tubes or ovaries) that can cause pelvic or abdominal pain and bleeding after sex or between periods
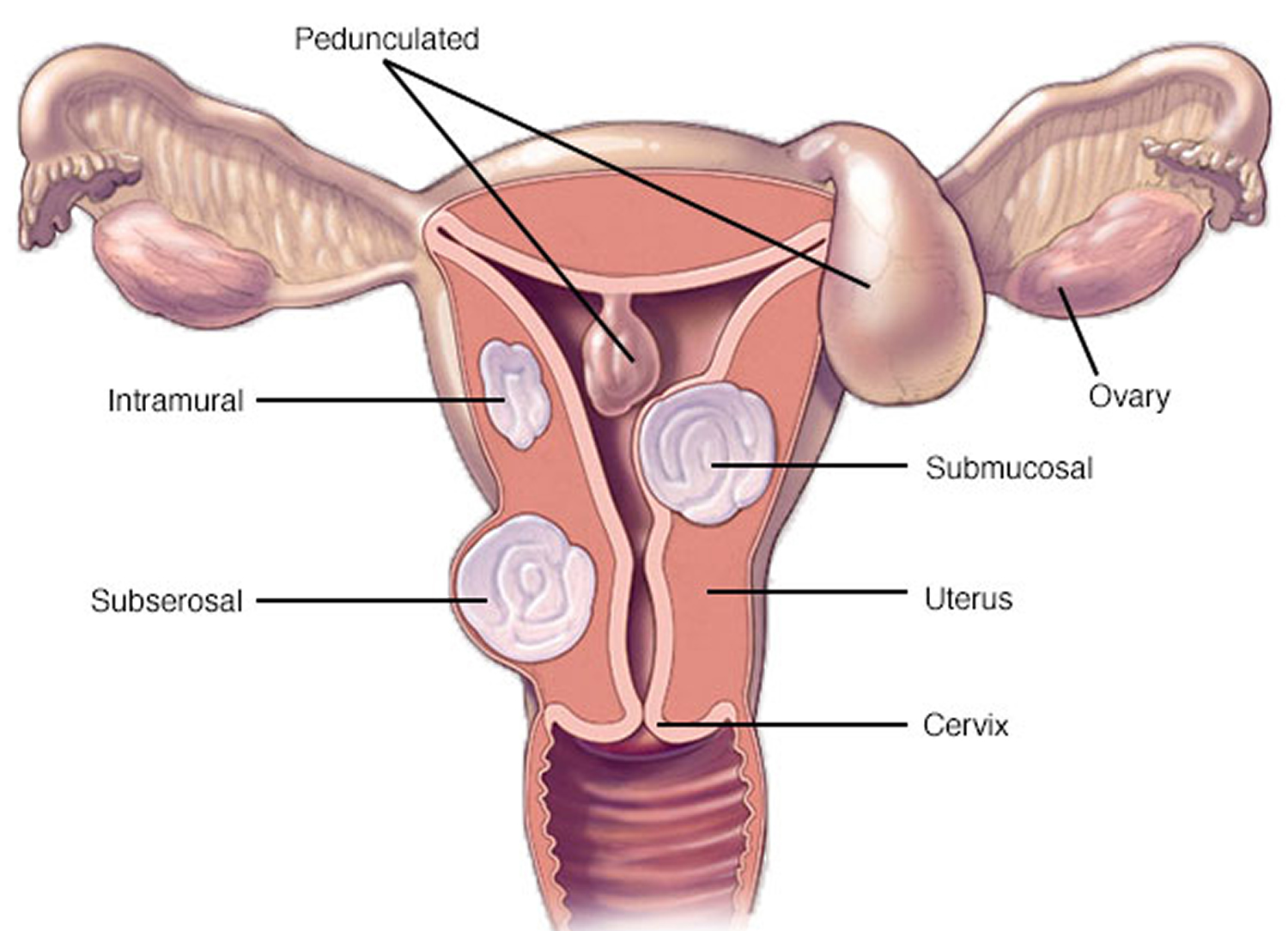
- Uterine fibroids – non-cancerous growths that develop in or around the womb and can cause heavy or painful periods
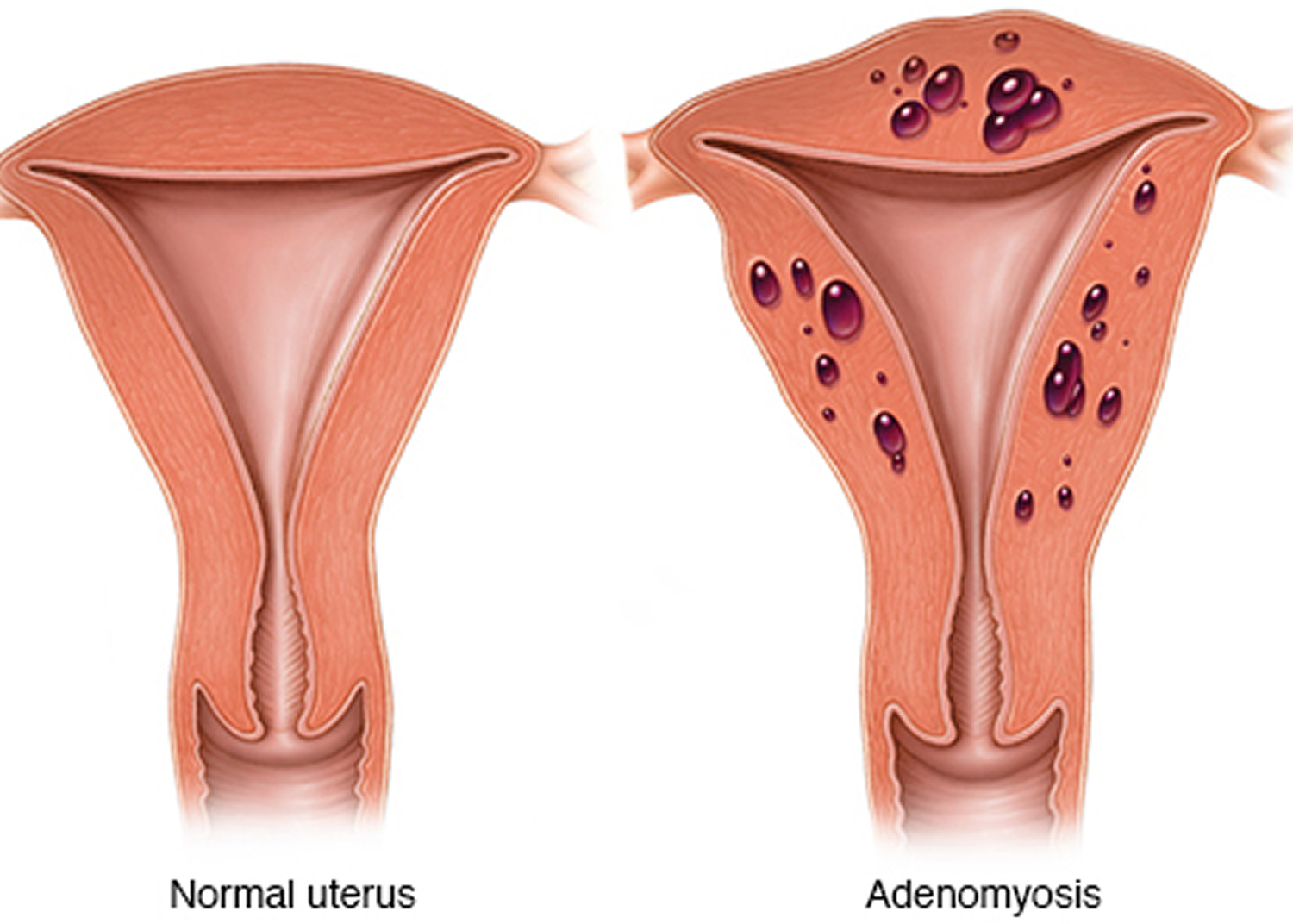
- Adenomyosis – when tissue from the womb lining becomes embedded in the wall of the womb
- Endometriosis – when small pieces of the womb lining are found outside the womb, such as in the fallopian tubes, ovaries, bladder or vagina (although this is more likely to cause painful periods)
- An underactive thyroid gland (hypothyroidism) – where the thyroid gland doesn’t produce enough hormones, causing tiredness, weight gain and feelings of depression
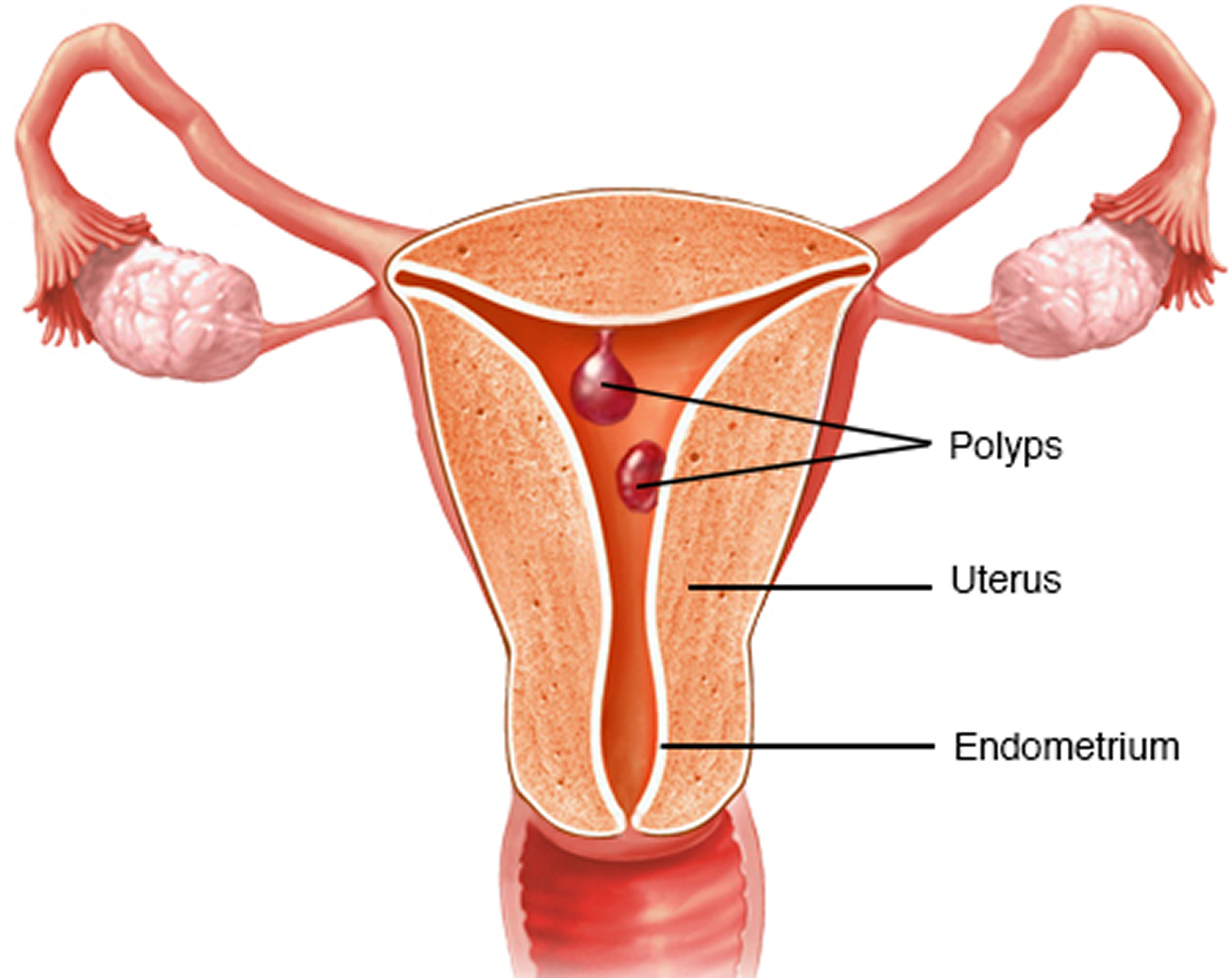
- Cervical or endometrial polyps – non-cancerous growths in the lining of the womb or cervix (neck of the womb)
- Blood clotting disorders, such as Von Willebrand disease
- Endometrial cancer or uterine cancer (although this is relatively rare).
- Cervical cancer can cause excessive menstrual bleeding, especially if you are postmenopausal or have had an abnormal Pap test in the past.
- Pregnancy or complications of pregnancy. A single, heavy, late period may be due to a miscarriage. Another cause of heavy bleeding during pregnancy includes an unusual location of the placenta, such as a low-lying placenta or placenta previa.
- Endometrial hyperplasia – an overgrowth of the endometrium which can progress to cancer.
- Chronic kidney or liver disease
- Dysfunction of the ovaries. If your ovaries don’t release an egg (ovulate) during a menstrual cycle (anovulation), your body doesn’t produce the hormone progesterone, as it would during a normal menstrual cycle. This leads to hormone imbalance and may result in menorrhagia.
Figure 1. Uterine fibroids
Medical treatments that can sometimes cause heavy periods include:
- an IUD (intrauterine contraceptive device, or “the coil”) – this can make your periods heavier for the first three to six months after insertion
- anticoagulant medication (taken to prevent blood clots)
- some medicines used for chemotherapy
- certain medications, including anti-inflammatory medications, hormonal medications such as estrogen and progestins, and anticoagulants such as warfarin (Coumadin, Jantoven) or enoxaparin (Lovenox), can contribute to heavy or prolonged menstrual bleeding.
Bleeding after childbirth
After having a baby, heavy vaginal bleeding, known as lochia, is very common and completely normal. It’s your body’s way of getting rid of the womb lining after you’ve given birth.
The bleeding can last from two to six weeks, and the blood may come out quickly, or slowly and evenly.
The amount of blood loss varies between women. If you’ve had a caesarean section, you’ll also have some bleeding as the womb lining sheds, although it may be lighter than if you’d had a vaginal birth.
You’ll need to use thick sanitary pads to start with while the bleeding is at its heaviest.
Once the flow settles down, you can switch to using normal sanitary pads. Always wash your hands before and after changing your pad.
Don’t use tampons for the first six weeks after the birth as it increases the risk of your womb becoming infected.
The color of the blood will also change in the days and weeks after childbirth. It’ll be bright red for the first few days and may contain small clots.
As the bleeding becomes less heavy, the color of the blood will lighten, becoming pinkish and more watery.
It’s important to make sure you get plenty of rest and don’t overdo it during this time.
You should seek medical advice from your doctor if:
- the bleeding smells unpleasant
- you get a fever or chills
- you still have heavy, bright red bleeding after the first week
- you have lower tummy pain on one or both sides
Call your local emergency number to ask for an ambulance if you experience very heavy bleeding (bleeding that soaks through more than one pad an hour) after having a baby.
It could be a postpartum hemorrhage caused by a piece of placenta still inside your womb. You may need antibiotics or an operation to remove the piece of placenta.
Risk factors for menorrhagia
Risk factors vary with age and whether you have other medical conditions that may explain your menorrhagia. In a normal cycle, the release of an egg from the ovaries stimulates the body’s production of progesterone, the female hormone most responsible for keeping periods regular. When no egg is released, insufficient progesterone can cause heavy menstrual bleeding.
Menorrhagia in adolescent girls is typically due to anovulation. Adolescent girls are especially prone to anovulatory cycles in the first year after their first menstrual period (menarche).
Menorrhagia in older reproductive-age women is typically due to uterine pathology, including fibroids, polyps and adenomyosis. However, other problems, such as uterine cancer, bleeding disorders, medication side effects and liver or kidney disease must be ruled out.
Menorrhagia symptoms
Signs and symptoms of menorrhagia may include:
- Soaking through one or more sanitary pads or tampons every hour for several consecutive hours
- Needing to use double sanitary protection to control your menstrual flow
- Needing to wake up to change sanitary protection during the night
- Bleeding for longer than a week
- Passing blood clots larger than a quarter
- Restricting daily activities due to heavy menstrual flow
- Symptoms of anemia, such as tiredness, fatigue or shortness of breath.
Menorrhagia complications
Excessive or prolonged menstrual bleeding can lead to other medical conditions, including:
Anemia. Menorrhagia can cause blood loss anemia by reducing the number of circulating red blood cells. The number of circulating red blood cells is measured by hemoglobin, a protein that enables red blood cells to carry oxygen to tissues.
Iron deficiency anemia occurs as your body attempts to make up for the lost red blood cells by using your iron stores to make more hemoglobin, which can then carry oxygen on red blood cells. Menorrhagia may decrease iron levels enough to increase the risk of iron deficiency anemia.
Signs and symptoms include pale skin, weakness and fatigue. Although diet plays a role in iron deficiency anemia, the problem is complicated by heavy menstrual periods.
Severe pain. Along with heavy menstrual bleeding, you might have painful menstrual cramps (dysmenorrhea). Sometimes the cramps associated with menorrhagia are severe enough to require medical evaluation.
Menorrhagia diagnosis
Visit your doctor if you feel your periods are unusually heavy. They’ll investigate the problem and may offer treatments to help.
Doctor consultation
To try to find out what’s causing your heavy periods, your doctor will ask about:
- your medical history
- the nature of your bleeding
- any related symptoms you have
They’ll also ask some questions about your periods, including:
- how many days your periods usually last
- how much bleeding you have
- how often you have to change your tampons or sanitary pads
- whether you experience flooding (heavy bleeding through to your clothes or bedding)
- what impact your heavy periods are having on your everyday life
- whether you bleed between periods or after sex
- whether you also have pelvic pain
To help determine the cause of your heavy bleeding, you may have a physical examination, particularly if you have pelvic pain or bleeding between periods or after sex.
Your doctor may also want to know what type of contraception you’re currently using and whether you plan to have a baby in the future. The last time you had a cervical screening test will also be noted.
You’ll also be asked about your family history to rule out inherited conditions that may be responsible, such as Von Willebrand disease, which runs in families and affects the blood’s ability to clot.
Further testing
Depending on your medical history and the results of your physical examination (including a pap smear and swabs), the cause of your heavy bleeding may need to be investigated further.
For example, if you have pelvic pain and experience bleeding between periods or during or after sex, you’ll need further tests to rule out serious illness, such as womb cancer (a rare cause of heavy menstrual bleeding).
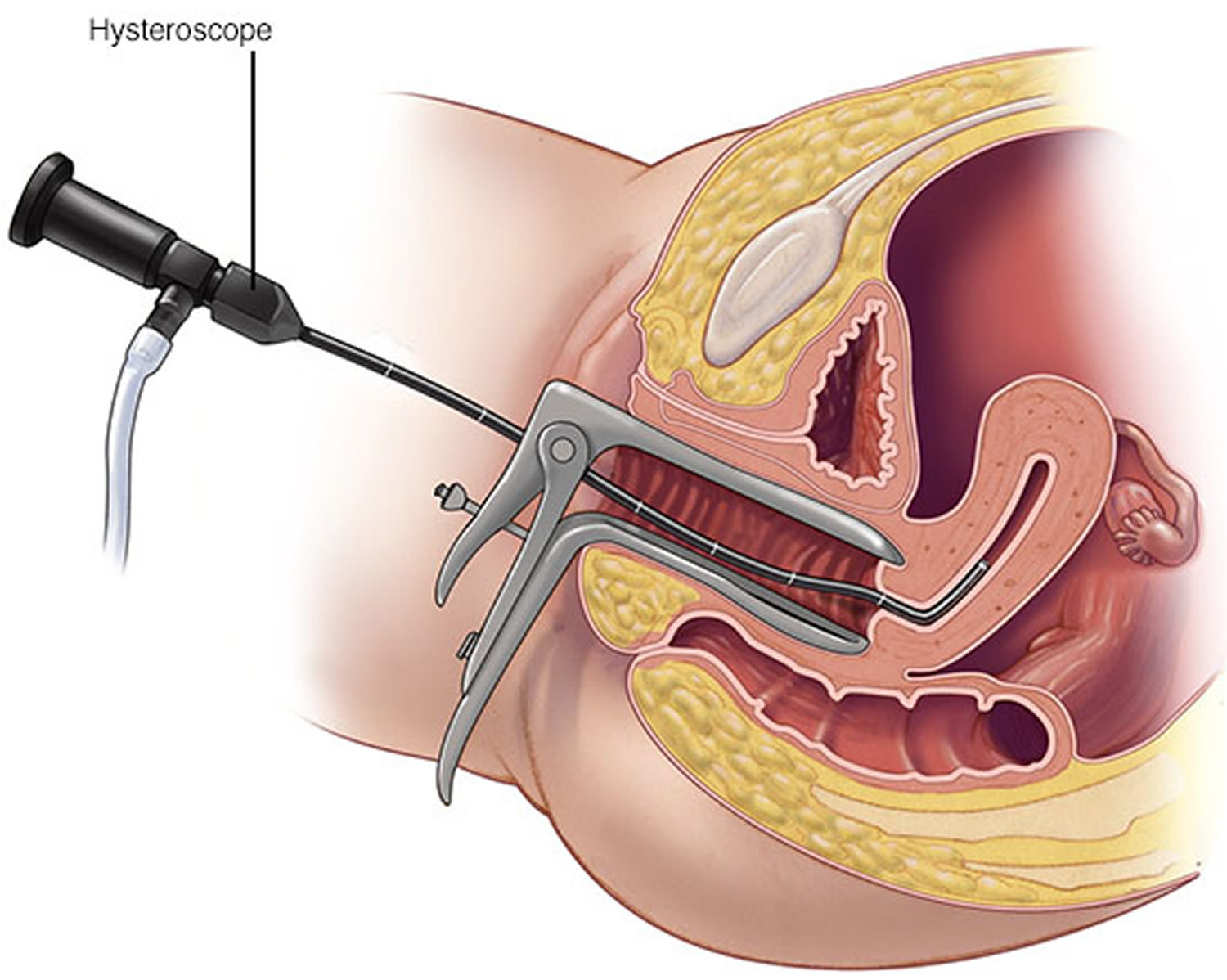
The gold standard is to perform a hysteroscopy and curette in all women over 35 years of age who have heavy menstrual bleeding to rule out endometrial hyperplasia or cancer 2. This is where the lining of the womb is looked at with a telescope, the hysteroscope and is then lightly scraped away and a biopsy (a sample of cells) is taken for examination.
Figure 4. Hysteroscopy
Pelvic examination
If you need to have a pelvic examination, your doctor will ask if you’d like a female assistant to be present.
A pelvic examination will include:
- a vulval examination – an examination of your genitals for evidence of external bleeding and signs of infection, such as a vaginal discharge
- a speculum examination – a speculum is a medical instrument inserted into your vagina to allow your vagina and cervix to be examined
- bimanual palpation – fingers are used to examine the inside of your vagina to identify whether your womb or ovaries are tender or enlarged
Before carrying out a pelvic examination, your doctor or gynecologist will explain the procedure to you and why it’s necessary.
You should ask about anything you’re unsure about. A pelvic examination shouldn’t be carried out without your consent.
Endometrial biopsy
In some cases of heavy bleeding, a biopsy may be needed to establish a cause. This will be carried out by a specialist and involves removing a small sample of womb lining for closer examination under a microscope.
Blood tests
A full blood test is usually carried out for all women with heavy periods. This can detect iron deficiency anemia, which is often caused by a loss of iron following prolonged heavy periods.
If you have iron deficiency anemia, you’ll usually be prescribed a course of medication.
Your doctor will be able to advise you about the type of medication most suitable for you and how long you need to take it for.
Ultrasound scan
If the cause of your heavy menstrual bleeding is still unknown after you’ve had the above tests, you may need an ultrasound scan of your womb.
This looks for abnormalities such as non-cancerous growths (uterine fibroids) or harmless growths (polyps). It can also be used to detect some types of cancer.
A transvaginal ultrasound scan is often used. A small probe is inserted into your vagina to get a close-up image of your womb.
Menorrhagia treatment
You may not need treatment for heavy periods if there isn’t a serious cause or if the bleeding doesn’t bother you.
Bleeding can vary over time for some women, so it may simply be that your bleeding is currently heavier than usual.
If you do need treatment, the aim is to:
- reduce or stop excessive menstrual bleeding
- treat or prevent iron deficiency anemia caused by heavy bleeding
The various treatments for heavy periods are outlined on this page.
| Anti-inflammatory drugs | Can reduce inflammation, pain and blood flow. |
|---|---|
| Tranexamic acid | Can reduce blood loss by about 50%. Non hormonal and is taken only on the heavy days of the period. |
| Insertion of a Mirena intrauterine device (IUD) | Releases a hormone that thins the endometrium and can reduce bleeding by up to 95% after 12 months 3. |
| The oral contraceptive pill | Can reduce blood flow by up to 50%. |
| Progestins (synthetic forms of progesterone) | Can reduce blood loss by about 30%. |
Your doctor may recommend endometrial ablation (removal of the endometrium) or a hysterectomy if:
- medications fail to reduce bleeding
- there are other symptoms such as pain
- you discuss the options with your doctor and you both feel it is the most appropriate treatment
Sometimes with heavy menstrual bleeding, iron levels can get low. Your doctor may get you to take a blood test and recommend iron therapy if levels are low. This usually involves taking an iron supplement daily.
Medication
Medication is usually tried first. If a particular medication isn’t effective or suitable for you, another type may be recommended.
Some medications make your periods lighter and others may stop bleeding completely. Some are also contraceptives.
Your doctor will explain how each type of medication works and any possible side effects. This will help you decide which treatment is most suitable.
The different types of medication used to treat heavy periods are outlined below.
Levonorgestrel-releasing intrauterine system
The levonorgestrel-releasing intrauterine system (LNG-IUS) is a small plastic device inserted into your womb. It slowly releases a hormone called progestogen.
It prevents the lining of your womb growing quickly and is also a form of contraceptive. Levonorgestrel-releasing intrauterine system (LNG-IUS) doesn’t affect your chances of getting pregnant after you stop using it.
Possible side effects of using levonorgestrel-releasing intrauterine system include:
- irregular bleeding that may last more than six months
- breast tenderness
- acne
- stopped or missed periods
Levonorgestrel-releasing intrauterine system (LNG-IUS) has been shown to reduce bleeding by more than 90% and it’s usually the preferred treatment to try first for women with heavy menstrual bleeding.
Tranexamic acid
If levonorgestrel-releasing intrauterine system is unsuitable – for example, if contraception isn’t wanted – tranexamic acid tablets may be considered.
The tablets work by helping the blood in your womb to clot. They’ve been shown to reduce blood loss by around 50%.
Two or three tranexamic acid tablets are taken three times a day for a maximum of three to four days.
Treatment should be stopped if your symptoms haven’t improved within three months.
Tranexamic acid tablets aren’t a form of contraception and won’t affect your chances of becoming pregnant. If necessary, tranexamic acid can be combined with a non-steroidal anti-inflammatory drug (NSAID).
Possible side effects of tranexamic acid include indigestion and diarrhea.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs (NSAIDs) may also be used to treat heavy periods if levonorgestrel-releasing intrauterine system isn’t appropriate.
NSAIDs have been shown to reduce blood flow by 20-50%. They’re taken in tablet form from the start of your period or just before until heavy bleeding has stopped.
The NSAIDs recommended for treating menorrhagia are:
- mefenamic acid
- naproxen
- ibuprofen
Naproxen is usually taken twice a day, and ibuprofen and mefenamic acid are usually taken three times a day.
NSAIDs work by reducing your body’s production of a hormone-like substance called prostaglandin, which is linked to heavy periods. NSAIDs can also help relieve period pain. They’re not a form of contraceptive.
You can keep taking NSAIDs for as long as you need to if they’re reducing blood loss and not causing significant side effects. But treatment should be stopped after three months if NSAIDs are not effective.
Combined oral contraceptive pill
The combined contraceptive pill, often referred to as “the pill”, can be used to treat heavy periods. It contains the hormones estrogen and progestogen.
You take one pill every day for 21 days before stopping for seven days. During this seven-day break you get your period. This cycle is then repeated.
The benefit of using combined oral contraceptives as a treatment for heavy periods is they offer a more readily reversible form of contraception than levonorgestrel-releasing intrauterine system.
They reduce heavy bleeding by around 40% and have the benefit of regulating your menstrual cycle and reducing period pain.
The pill works by preventing your ovaries releasing an egg each month. As long as you’re taking it correctly, it should prevent pregnancy.
Common side effects of the combined oral contraceptive pill include:
- mood changes
- nausea (feeling sick)
- fluid retention
- breast tenderness
Oral norethisterone
Norethisterone is a type of man-made progestogen (one of the female sex hormones).
It can be used to treat heavy periods, and is taken in tablet form two to three times a day from days 5 to 26 of your menstrual cycle, counting the first day of your period as day one.
Oral norethisterone works by preventing your womb lining growing quickly. It isn’t suitable if you’re trying to conceive because it’s likely to inhibit ovulation.
It can reduce heavy bleeding by more than 80%, but isn’t an effective form of contraception and can have unpleasant side effects, including:
- weight gain
- breast tenderness
- short-term acne
Oral progestogens, such as norethisterone, aren’t as effective as tranexamic acid and may not always be able to control heavy bleeding.
Injected progestogen
A type of progestogen called medroxyprogesterone acetate is also available as an injection and is sometimes used to treat heavy periods.
It prevents the lining of your womb growing quickly and reduces bleeding by up to 50%. It’s also a form of contraception.
Injected progestogen doesn’t prevent you becoming pregnant after you stop using it, although there may be a delay of 6 to 12 months after stopping before you’re able to get pregnant.
Common side effects of injected progestogen include:
- weight gain
- irregular bleeding
- stopped or missed periods
- premenstrual symptoms, such as bloating, fluid retention and breast tenderness
You’ll need to have progestogen injected once every 12 weeks for as long as treatment is required.
Gonadotropin releasing hormone analogue
Gonadotropin releasing hormone analogue (GnRH-a) is a hormone sometimes given as an injection to treat fibroids (non-cancerous growths in the womb).
Studies have shown GnRH-a is effective in reducing blood loss during periods by almost 90%.
But it can be expensive and may cause hormone abnormalities (hypogonadism) similar to the menopause, with effects including hot flushes, increased sweating and vaginal dryness.
This means GnRH-a isn’t a routine treatment, but may be used while you await surgery.
Surgery
Your specialist may suggest surgery if medication isn’t effective in treating your heavy periods.
Surgical Procedures
You may need surgical treatment for menorrhagia if medical therapy is unsuccessful. Treatment options include:
- Dilation and curettage (D&C). In this procedure, your doctor opens (dilates) your cervix and then scrapes or suctions tissue from the lining of your uterus to reduce menstrual bleeding. Although this procedure is common and often treats acute or active bleeding successfully, you may need additional D&C procedures if menorrhagia recurs.
- Uterine artery embolization. For women whose menorrhagia is caused by fibroids, the goal of this procedure is to shrink any fibroids in the uterus by blocking the uterine arteries and cutting off their blood supply. During uterine artery embolization, the surgeon passes a catheter through the large artery in the thigh (femoral artery) and guides it to your uterine arteries, where the blood vessel is injected with materials that decrease blood flow to the fibroid.
- Focused ultrasound surgery. Similar to uterine artery embolization, focused ultrasound surgery treats bleeding caused by fibroids by shrinking the fibroids. This procedure uses ultrasound waves to destroy the fibroid tissue. There are no incisions required for this procedure.
- Myomectomy. This procedure involves surgical removal of uterine fibroids. Depending on the size, number and location of the fibroids, your surgeon may choose to perform the myomectomy using open abdominal surgery, through several small incisions (laparoscopically), or through the vagina and cervix (hysteroscopically).
- Endometrial ablation. This procedure involves destroying (ablating) the lining of your uterus (endometrium). The procedure uses a laser, radiofrequency or heat applied to the endometrium to destroy the tissue. After endometrial ablation, most women have much lighter periods. Pregnancy after endometrial ablation has many associated complications. If you have endometrial ablation, the use of reliable or permanent contraception until menopause is recommended.
- Endometrial resection. This surgical procedure uses an electrosurgical wire loop to remove the lining of the uterus. Both endometrial ablation and endometrial resection benefit women who have very heavy menstrual bleeding. Pregnancy isn’t recommended after this procedure.
Hysterectomy. Hysterectomy — surgery to remove your uterus and cervix — is a permanent procedure that causes sterility and ends menstrual periods. Hysterectomy is performed under anesthesia and requires hospitalization. Additional removal of the ovaries (bilateral oophorectomy) may cause premature menopause.
Many of these surgical procedures are done on an outpatient basis. Although you may need a general anesthetic, it’s likely that you can go home later on the same day. An abdominal myomectomy or a hysterectomy usually requires a hospital stay.
When menorrhagia is a sign of another condition, such as thyroid disease, treating that condition usually results in lighter periods.
If the cause is fibroids, you may be recommended either:
- uterine artery embolization
- myomectomy
If your heavy periods aren’t caused by fibroids, your options include:
- endometrial ablation – where the womb lining is destroyed
- hysterectomy – surgical removal of the womb
Your specialist can discuss these procedures with you, including the benefits and any associated risks.
Uterine artery embolisation (UAE)
Uterine artery embolisation (UAE) involves inserting a small tube into your groin.
Small plastic beads are injected through the tube into the arteries supplying blood to the fibroid. This blocks the arteries and causes the fibroid to shrink over the following six months.
Advantages of uterine artery embolisation (UAE) include:
- it’s usually effective in treating heavy periods caused by fibroids
- serious complications are rare
- you only need to spend one night in hospital
But having uterine artery embolisation may cause some pain after the blood supply is removed, and strong painkillers are needed for about eight hours. There are also other complications your specialist will be able to discuss with you.
If you plan to get pregnant in the future, you may choose not to have uterine artery embolisation, as there are potential risks to your fertility.
In around 10-20% of cases, uterine artery embolisation may be required again later on. Your specialist will discuss this with you.
Myomectomy
Sometimes fibroids can be removed using a surgical procedure called a myomectomy. But it isn’t suitable for every type of fibroid.
Your specialist will be able to tell you whether a myomectomy is possible and what the possible complications are.
When they’re appropriate, myomectomies are effective. But in some cases the fibroids grow back.
Endometrial ablation
Different techniques can be used for endometrial ablation.
These include:
- microwave endometrial ablation – a probe that uses microwave energy (a type of radiation) is inserted into the womb to heat and destroy the womb lining
- thermal balloon ablation – a balloon is inserted into your womb and inflated and heated to destroy the womb lining
These procedures can be carried out either under local anesthetic or general anesthetic. They’re fairly quick procedures, taking around 20 minutes, and you can often go home on the same day.
You may experience some vaginal bleeding for a few days after endometrial ablation, similar to a light period.
Use sanitary towels rather than tampons. Some women can have bloody discharge for three or four weeks.
You may also experience tummy cramps, similar to period pains, for a day or two after the procedure. These can be treated with painkillers, such as paracetamol or ibuprofen.
Some women have reported experiencing more severe or prolonged pain after having endometrial ablation.
In this case, you should speak to your doctor or a member of your hospital care team who may be able to prescribe a stronger painkiller.
It’s usually recommended that you don’t get pregnant after having endometrial ablation because the risk of problems, such as miscarriage, is high.
The failure rate for endometrial ablation is about 25-35%. If it fails, you may be offered a repeat treatment.
Hysterectomy
A hysterectomy (removal of the womb) will stop any future periods, but should only be considered after other options have been tried or discussed.
The operation and recovery time are longer than for other surgical techniques for treating heavy periods.
A hysterectomy is only used to treat heavy periods after a thorough discussion with your specialist to outline the benefits and disadvantages of the procedure.
You won’t be able to get pregnant after having a hysterectomy.
- Cox SM, Cromwell D, Mahmood T, Templeton A et al. The delivery of heavy menstrual bleeding services in England and Wales after publication of national guidelines: a survey of hospitals. BMC Health Serv Res. 2013 Nov 25;13(1):491. Hallberg et al. Menstrual blood loss – a population study. Variation at different ages and attempts to define normality. Acta Obste Gynaecol Scand 1966; 45:320.[↩]
- Dijkhuizen FP, MolBW, Brolmann HA, Heintz AP. The accuracy of endometrial sampling in the diagnosis of patients with endometrial carcinoma and hyperplasia: a meta-analysis. Cancer 2000; 89:1765[↩]
- Stewart A, Cummins C, Gold L, Jordan R, Phillips W The effectiveness of the levonorgestrel-releasing intrauterine system in menorrhagia: a systematic review. BJOG. 2001;108(1):74[↩]