Contents
- What is methylene blue
- Methylene blue contraindications
- What is methylene blue used for?
- Methemoglobinemia
- Vasoplegic syndrome
- Methylene blue in septic shock
- Methylene blue and hepatopulmonary syndrome
- Methylene blue as antimalarial
- Methylene blue and cancer
- Methylene blue and ifosfamide-induced encephalopathy
- Methylene blue as dye and stain
- Methylene blue neutralization of heparin
- Methylene blue and priapism
- Methylene blue and Alzheimer’s disease
- Methylene blue photodynamic therapy
- Methylene blue in pain treatment
- Methylene blue dose
- Methylene blue side effects
What is methylene blue
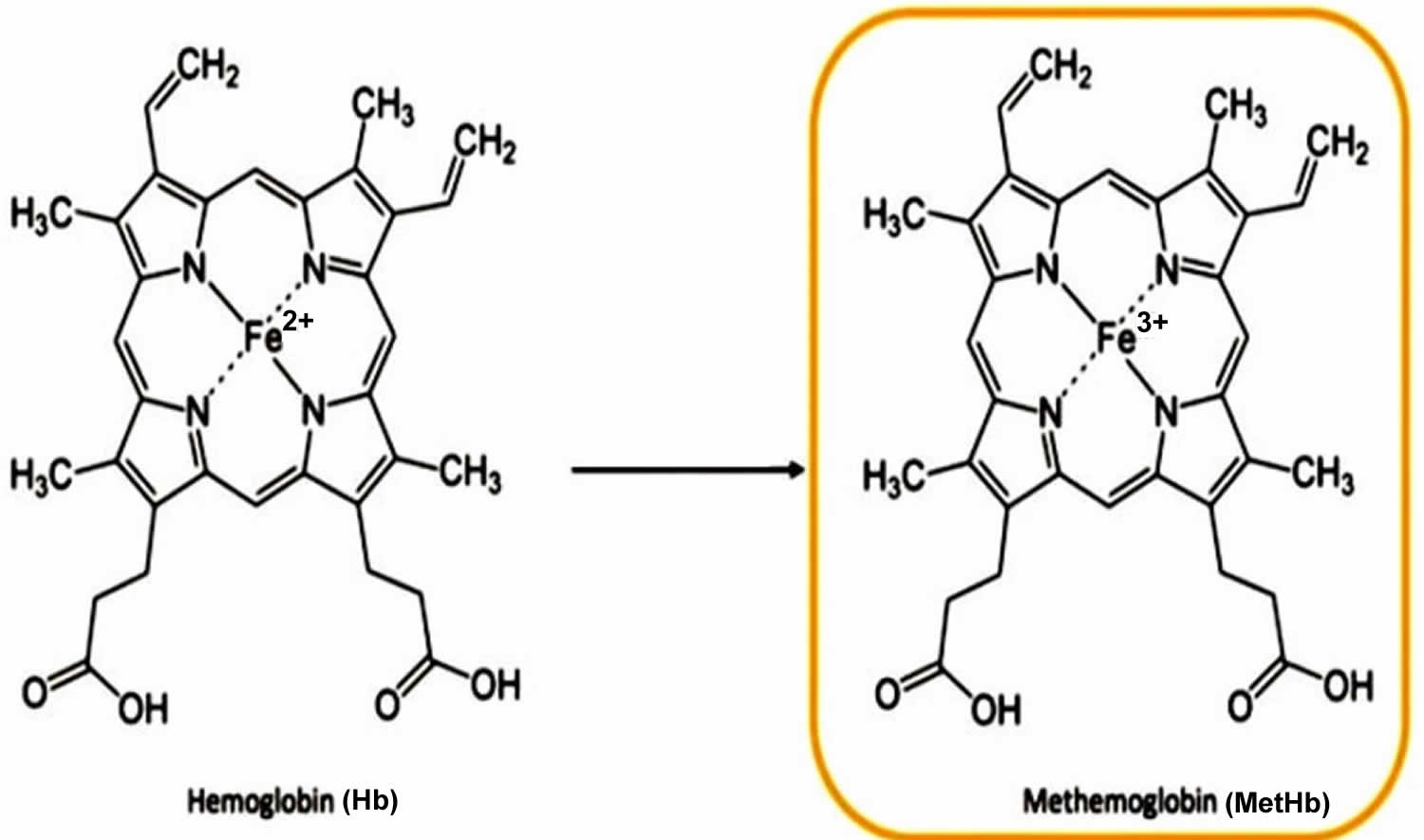
Methylene blue (C16H18ClN3S), also known as methylthioninium chloride or tetramethylthionine chloride, is a medication and an oxidation-reduction agent that is used to treat hereditary and acquired methemoglobinemia, a blood disorder where an abnormal amount of methemoglobin (MetHb), a form of hemoglobin (Hb) that cannot carry oxygen, a condition when Fe2+ of hemoglobin gets oxidized to Fe3+ reducing the oxygen-carrying capacity of hemoglobin 1, 2, 3, 4. Methemoglobinemia can lead to a reduced capacity of the blood to deliver oxygen to tissues, resulting in symptoms like bluish discoloration of the skin (cyanosis, due to poor circulation or inadequate oxygenation of the blood), shortness of breath, and fatigue 5, 6. Methemoglobinemia can be either inherited (congenital) or acquired from exposure to certain drugs or toxins 6. Methylene blue is FDA approval for treating methemoglobinemia under the brand name Provayblue. Methylene blue works by reducing the oxidized hemoglobin, converting it back to hemoglobin so that it can carry oxygen properly again. When used for methemoglobinemia, methylene blue is given as an injection by a doctor. As a medication, when administered intravenously in low doses to treat methemoglobinemia, methylene blue converts methemoglobin to hemoglobin 7. Specifically, methylene blue is used to treat methemoglobin levels that are greater than 30% or in which there are symptoms despite oxygen therapy. Methylene blue is typically given by injection into a vein. Methylene blue inhibits guanylate cyclase and has been used to treat cyanide poisoning, but this use is no longer recommended. Methylene blue should be avoided in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency, and caution should be exercised when administering serotonin-metabolizing drugs.
Methylene blue is also used as a bacteriologic stain and as an indicator during a lumpectomy or mastectomy with sentinel lymph node biopsy, as it is applied as a dye to map out which lymph nodes, if any, have any signs of cancer cells. Methylene blue stains to negatively charged cell components like nucleic acids; when administered in the lymphatic bed of a tumor during cancer surgery, methylene blue may stain lymph nodes draining from the tumor, thereby aiding in the visual localization of tumor sentinel lymph nodes. Surgeons may use methylene blue as a dye to identify sentinel lymph nodes during cancer surgeries, such as lumpectomies or mastectomies 8. Methylene blue is also used to evaluate or indicate lesions and other conditions during procedures. Another indication for the use of methylene blue is to identify the parathyroid glands during parathyroidectomy procedures 9
Methylene blue can also reduce post-injection pain when used 45 seconds before the administration of propofol 10. Methylene blue has been used to treat various painful syndromes, including postoperative pain, discogenic pain, and neuropathic pain e.g., intractable idiopathic pruritus ani, pain after open diathermy hemorrhoidectomy and chronic discogenic low back pain 11, 12, 13. There is evidence in the literature to support methylene blue for use as an analgesic for discogenic low back pain 14, 15, 16.
Methylene blue has been used off-label for vasoplegic syndrome, an uncommon but life-threatening condition characterized by uncontrolled peripheral vasodilation leading to dangerously low blood pressure (hypotension) despite a normal or even elevated cardiac output that can occur during septic shock, following cardiopulmonary bypass during cardiac surgery, or after other major surgeries, burns, and trauma 17, 18, 19. Methylene blue may be used when epinephrine has not worked to stabilize blood pressure 20, 21. The mechanism of action of methylene blue involves inhibiting 2 enzymes, namely nitric oxide synthase (NOS) and guanylyl cyclase. This inhibition leads to a reduction in the vasodilatory effects of cytokines that are released in response to shock 18. Additionally, the binding affinity for the M3 receptor exerts inhibitory effects on cholinesterase activity.
In the past, methylene blue has been used to treat malaria in areas with chloroquine-resistant Plasmodium falciparum strains 22, 23. Methylene blue was the first synthetic antimalarial to be used, which occurred in a German hospital some 120 years ago 24. Methylene blue global use in malaria endemic areas is well documented for the late 19th and early 20th centuries 25, 26. However, methylene blue usage was stopped after new synthetic antimalarials were developed 2.
Cancer patients undergoing chemotherapy with ifosfamide may develop brain damage (encephalopathy), leading to confusion, hallucinations, or even coma. Methylene blue may be beneficial in treating ifosfamide-induced encephalopathy in human cancer management due to the drug’s ability to prevent the formation of neurotoxic metabolites that cause the encephalopathy, but it is ineffective when used as a preventative treatment 27, 28, 29, 30.
Methylene blue has also been considered to be effective in priapism (a prolonged, often painful, penile erection that persists for more than four hours and is unrelated to sexual stimulation), against septic shock (blocking the nitric oxide-dependant guanylate-cyclase), the prevention of urinary tract infections, the intraoperative visualisation of nerves and endocrine glands as well as of pathologic fistulae, and the sterilisation of transfusion blood and it is under investigation as an experimental drug against Alzheimer’s disease 31, 32, 33, 34, 35.
Methylene blue is a diaminophenothiazine drug that at low doses (0.5 – 4 mg/kg body weight) has neurometabolic-enhancing properties 36. Preclinical research with rodents has shown that at low doses, methylene blue is a metabolic and cognitive enhancer that improves brain oxygen consumption, brain glucose uptake, cerebral blood flow, fMRI responses and memory consolidation by induction of cytochrome oxidase, the respiratory enzyme found within nerve cells 36. By enhancing cytochrome oxidase activity, methylene blue increases oxygen consumption and amount of ATP available in neurons during memory consolidation. Although methylene blue has the potential to enter any nerve cell, it preferentially accumulates in neurons with higher energy demand, such as those involved in memory consolidation after extinction training 37. Hence, by acting as a mitochondrial electron cycler and antioxidant, low-dose methylene blue increases cellular energy production and support enhanced memory consolidation in key brain regions associated with memory processing 36. Based on the findings of this study 38, patients who continue to show moderate to high levels of fear at the conclusion of an exposure therapy session may have their fear inadvertently strengthened by methylene blue administration, thus leading to a less favorable therapeutic outcome.
Methylene blue common side effects include headache, vomiting, confusion, shortness of breath, and high blood pressure. Other side effects include serotonin syndrome, red blood cell breakdown, and allergic reactions. Use often turns the urine, sweat, and stool blue to green in color. Methylene blue is a thiazine dye. It works by converting the ferric iron (Fe3+) in hemoglobin to ferrous iron (Fe2+). While use during pregnancy may harm the baby, not using it in methemoglobinemia is likely more dangerous.
Methylene blue may be unsafe in people who have or may be at risk for a blood disease called glucose-6-phosphate dehydrogenase (G6PD) deficiency. They should not take this medicine. If you or your child has G6PD deficiency, always tell your doctor before getting treatment.
Methylene blue is a monoamine oxidase (MAO) inhibitor and therefore can interact with Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Monoamine Oxidase Inhibitors (MAOIs), and Tricyclic Antidepressants (TCAs) to cause serious serotonin toxicity or serotonin syndrome 39. Serotonin syndrome has been found to occur when combining serotonergic agents with methylene blue at a dose of 5 mg/kg 40.
Methylene blue also interacts with dapsone and forms hydroxylamine which oxidizes hemoglobin causing hemolysis 41.
A few very rare case reports regarding methylene blue‐induced anaphylactic reactions upon injection in surgery patients were identified in the scientific literature 42. These reactions were IgE mediated and probably caused by a conjugation of methylene blue as hapten to a protein.
As no food or respiratory allergy nor skin allergy was identified in the literature search for methylene blue, and concern for anaphylactic reactions upon oral exposure is low, there are no safety concerns with respect to allergenicity of methylene blue 43.
Methylene blue is a safe drug at a therapeutic dose of less than 2 mg/kg; however, when methylene blue levels are greater than 7 mg/kg, many of the adverse effects it exhibits will occur 19. Methylene blue is usually well tolerated and accepted with mild and regularly self-limiting gastrointestinal and urogenital symptoms, which are the main side effects. To avoid vomiting, methylene blue should be given in a taste-masked formulation and/or together with food. In historical studies, nutmeg has been shown to be effective in moderating the frequent occurrence of urethritis, which should be evaluated in future studies. Whether the small effect of methylene blue on the methemoglobin (MetHb) development is of clinical significance needs to be monitored in future large-scale studies including regions with more severe forms of G6PD deficiency. Methylene blue use also requires caution in patients with kidney failure due to its ability to reduce kidney blood flow 19.
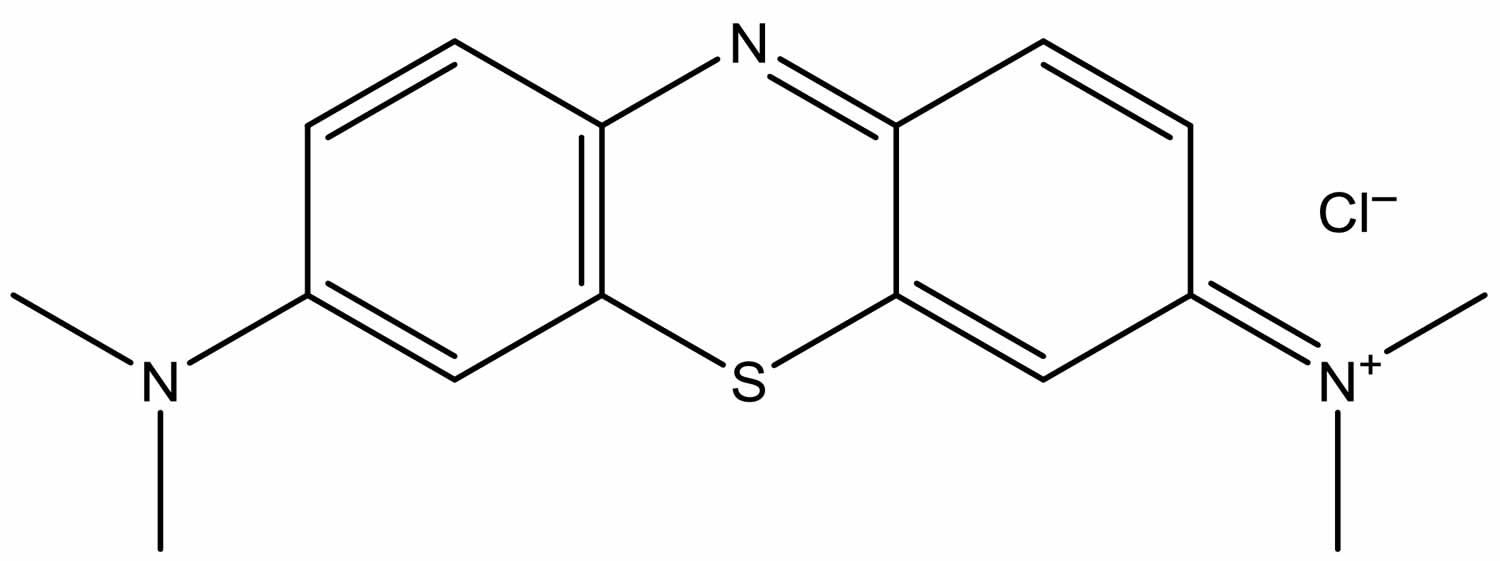
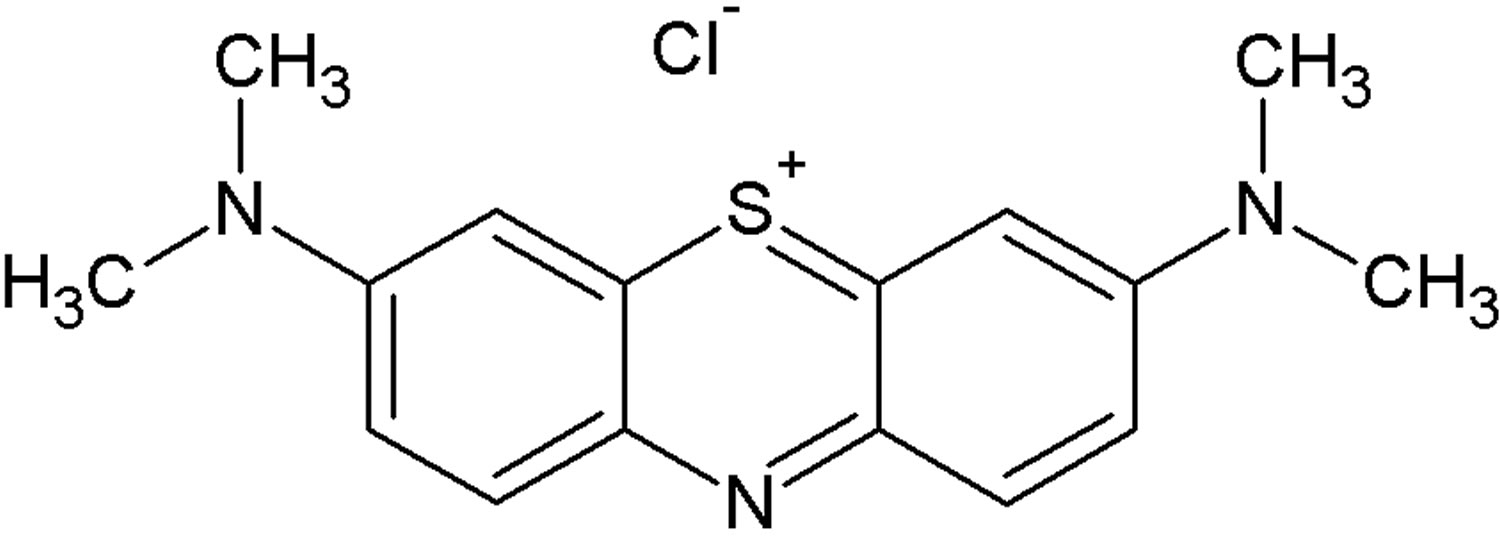
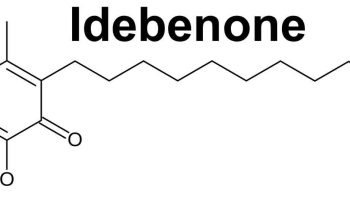
Figure 1. Methylene blue molecular structure
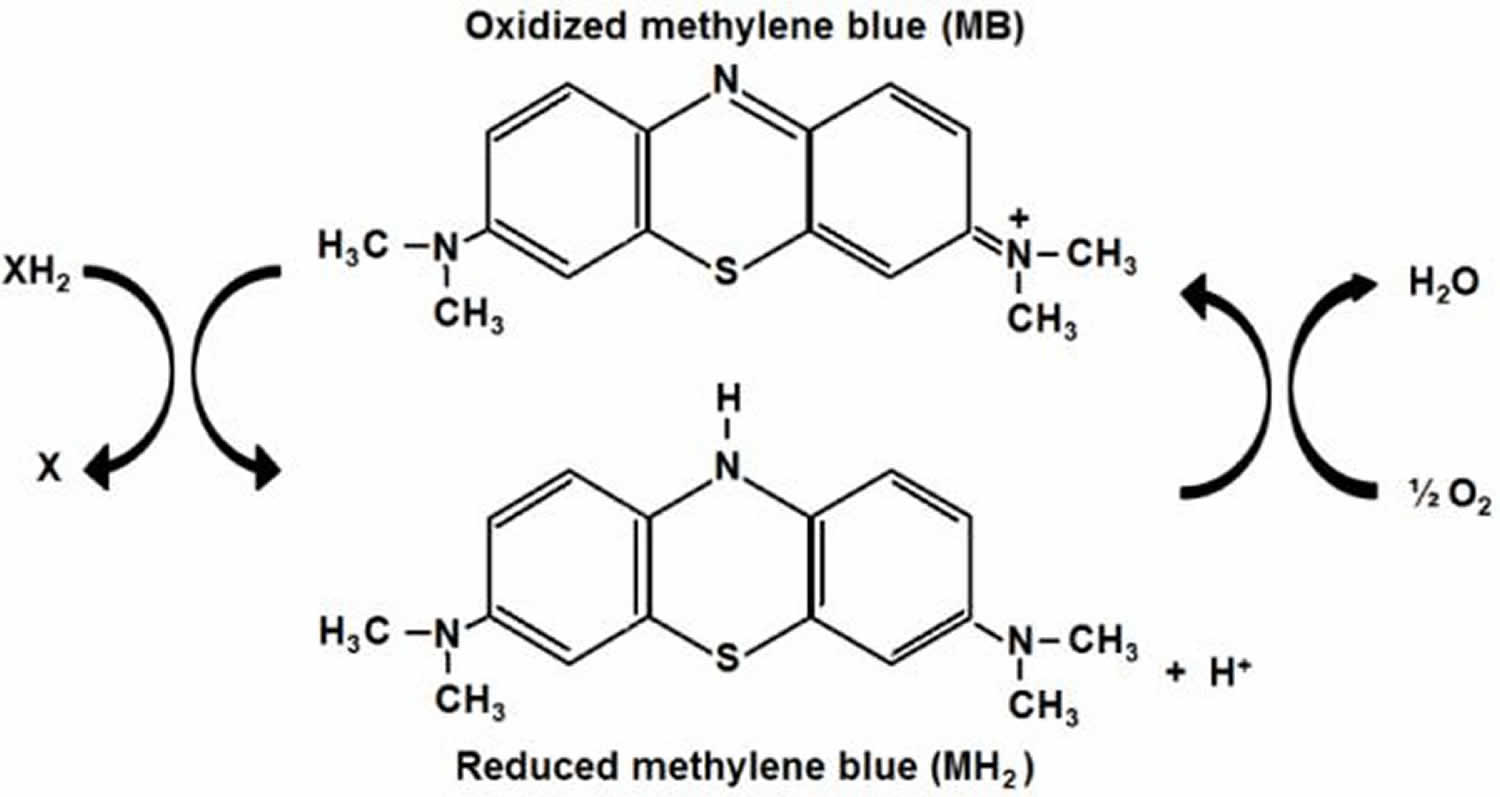
[Source 44 ]Figure 2. Oxidized and reduced methylene blue
Footnotes: Methylene blue (MB) can be reduced into leucomethylene blue (MH2), and therefore, it can be used as an antioxidant 45. Methylene blue can work as a catalytic redox cycler in mitochondria and bypass Complex I/III activity 46. The tri-heterocyclic thiazide ring of methylene blue allows the presence of a delocalized positive charge that confers a high reduction potential. At the same time, the presence of imine groups (C = N − R) confers high antioxidant activity to the methylene blue molecule. In its oxidized form, methylene blue (MB) accepts electrons from an electron donor (XH2). In its reduced form, leucomethylene blue (MH2) is colorless, acts as an electron donor, and it can transfer electrons to oxygen to form water. In vivo and at low concentrations methylene blue and leucomethylene blue (MH2) are at equilibrium, so that they form a reversible reduction-oxidation system. The auto-oxidizing capacity of methylene blue provides a mechanism for electron transfer to oxygen, which accounts for its antioxidant and metabolic-enhancing properties, as well as its hormetic dose-response effects at the biochemical, physiological and behavioral levels.
[Source 47 ]Methylene blue contraindications
Methylene blue is contraindicated in patients who have developed hypersensitivity reactions to it or anaphylaxis after past administration and in severe renal insufficiency. Methylene blue is relatively contraindicated in people with glucose-6-phosphate dehydrogenase (G6PD) deficiency as it can cause severe hemolysis (hemolytic anemia) and also in patients with Heinz body anemia 48. Those experiencing hemolytic anemia in this situation will have jaundice and characteristic Heinz bodies on a peripheral blood smear 49. Methylene blue is also contraindicated in pregnant women. The FDA has assigned a pregnancy class X rating for methylene blue due to intestinal atresia and fetal death following an intra-amniotic injection, specifically in the second trimester 50.
What is methylene blue used for?
In 1876 a German chemist Heinrich Caro synthesized methylthionine chloride (methylene blue) for textile dyeing using the reaction of a mixture of N, N-dimethyl-p-phenylenediamine (C8 H12 N2) and hydrogen sulfide (H2S) with iron chloride (FeCl3) 51, 52. In 1882 methylene blue entered the field of medicine when Robert Koch and Paul Ehrlich used methylene blue to stain tuberculosis microorganisms as well as to differentiate the variant types of white blood cells 53. Since the 1890s, methylene blue has been used as a local anesthetic agent due to its sensory nerve-ending blocking property 54, 55. In 1891, methylene blue’s ability to target the malaria organisms was identified by Paul Ehrlich; that was the beginning of its therapeutic application for malaria 56, 57, 2, but its use was stopped due to its unavoidable side effects (reversible bluish coloration of urine, sclera, and skin) 58, 23. In 1897 methylene blue was used to treat gonorrhea 59 and in 1908 to treat fever 60.
Methylene blue is an inhibitor of the enzymes endothelial nitric oxide synthase (eNOS), inducible nitric oxide synthase (iNOS), and guanylate cyclase decreasing the amount of cyclic guanosine monophosphate (cGMP) needed for nitric oxide (NO) to be released which is responsible for relaxing blood vessels smooth muscle, therefore causing constriction of blood vessels (vasoconstriction) via inhibition of vascular smooth muscle relaxation, which increases blood pressure 61, 62, 63, 1, 19, 64. Methylene blue has been found to improve the low blood pressure (hypotension) associated with various clinical states 65. Methylene blue also improves hypoxia (low levels of oxygen in your blood and body tissues) and hyper dynamic circulation in cirrhosis of liver and severe hepatopulmonary syndrome (a lung complication of liver disease, characterized by abnormally low oxygen levels in the blood (hypoxemia) due to dilated blood vessels in the lungs) 66. Methylene blue also results in transient and reproducible improvement in blood pressure and heart function in septic shock 67.
Methylene blue is used or explored off label for a variety of indications, including for vasoplegic syndrome or septic shock, as methylene blue may help to increase blood pressure; for a neurotoxic side effect of a chemotherapeutic agent called ifosfamide, known as ifosfamide-induced encephalopathy; for certain infections such as malaria, given its antimicrobial properties; and as a dye for intraoperative tissue visualization 1.
Methylene blue has been investigated for treatment of pain 68, as a combination antimicrobial therapy such as for periodontal infections 69 or superficial fungal infection 70 and for hypoxemia 71. Methylene blue has also been suggested as a treatment for COVID-19 52.
Methemoglobinemia
Methemoglobinemia (MetHb) is a potentially life-threatening blood disorder in which an abnormal amount of methemoglobin (MetHb) is produced 72, 73, 74, 75. Hemoglobin (hb) is the protein in red blood cells that carries and distributes oxygen to your body. Oxygen is essential to life, and your body need a certain amount of oxygen to function properly. Oxygen enters your body through your nose or mouth when you breathe (inhale) and passes through your lungs into your bloodstream. Once in your bloodstream, oxygen is carried by the hemoglobin (hb) in red blood cells to cells all over your body. All of your cells need oxygen to create energy efficiently, and your body needs energy to fulfill all of its processes, such as digestion and even thinking. Your body tightly regulates the amount of oxygen saturation in your blood, because low blood oxygen levels (hypoxemia) can lead to many serious conditions and damage to individual organ systems, especially your brain and heart. Methemoglobin (MetHb) is a form of hemoglobin (Hb) where some or all of the four iron (Fe) within the hemoglobin molecule has been oxidized from the reduced ferrous (Fe2+) state to the oxidized ferric (Fe3+) state 5. Ferric iron (Fe3+) is unable to bind and transport oxygen. This change in the iron molecule from the reduced ferrous (Fe2+) state to the oxidized ferric (Fe3+) state prevents the hemoglobin from effectively carrying oxygen to your body’s tissues, potentially leading to a condition called methemoglobinemia 76. Normally, red blood cells contain less than 2 percent methemoglobin as a naturally occurring oxidized metabolite of hemoglobin. However, when methemoglobin (MetHb) levels increase with methemoglobinemia, the blood is not able to release oxygen effectively to body tissues resulting in functional anemia. The end result of these changes is decreased oxygen delivery leading to tissue hypoxia. The resulting lack of oxygen throughout the body can cause symptoms such as pale or blue-colored skin or cyanosis.
Normal red blood cells contain molecules of iron-containing hemoglobin, which deliver oxygen to the body’s tissues. The iron in hemoglobin is the reduced ferrous (Fe2+), but it can spontaneously become the oxidized ferric (Fe3+). Hemoglobin that contains the oxidized ferric (Fe3+) iron is called methemoglobin (MetHb), and it cannot deliver oxygen.
Methemoglobinemia condition can be:
- Passed down through families (inherited or congenital) also known as autosomal recessive methemoglobinemia, congenital methemoglobinemia or hereditary methemoglobinemia. Congenital methemoglobinemia or hereditary methemoglobinemia are caused by biallelic mutations in the CYB5R3 gene that codes the NADH cytochrome b5 reductase enzyme, which is very rare and the actual incidence is not known 77. To date, more than 80 different disease‐causing gene variants in the CYB5R3 gene have been reported 78, 79, 77. Increased frequency of hereditary methemoglobinemia has been found in Siberian Yakuts, Athabaskans, Eskimos, and Navajo 80. Cytochrome-b5 reductase enzyme utilizes NADH formed during glycolysis to reduce methemoglobin back to functional hemoglobin 81. In addition to the autosomal recessive methemoglobinemia subtypes, a rare methemoglobin group called hemoglobin M disease (M group variants of hemoglobin), results from autosomal dominant mutations (variants) in the genes encoding alpha or beta globin proteins of hemoglobin due to substitution of an amino acid with tyrosine in the alpha‐globin (HBA1, HBA2), beta‐globin (HBB), or gamma‐globin (HBG1, HBG2) 72. Multiple variants of hemoglobin M have been described (Boston, Fort Ripley, Hyde Park, Iwate, Kankakee, Osaka, Saskatoon) 82, 83. In very rare cases, inherited methemoglobinemia is caused by deficiency of the electron acceptor cytochrome b5 84. This causes methemoglobinemia associated with ambiguous genitalia due to a homozygous variant in the CYB5A gene, encoding the microsomal cytochrome b5 85. This condition is due to isolated 17,20‐lyase deficiency since the cofactor cytochrome b5 is required for optimal 17,20‐lyase activity 86.
- Acquired methemoglobinemia caused by exposure to certain drugs, chemicals, or foods (acquired). The most common drugs are benzocaine and lidocaine 87, 88, 89.
Acquired methemoglobinemia is much more common than the inherited methemoglobinemia and, is the result of exposure to substances that cause oxidation of the hemoglobin either directly or indirectly. This exposure results in the production of methemoglobin (hemoglobin with oxidized ferric (Fe3+) iron) that exceeds the body’s capacity to convert the ferric (Fe3+) iron within the hemoglobin back to its ferrous (Fe2+) state. Acquired methemoglobinemia may be due to exposure to direct oxidizing agents (e.g. benzocaine and prilocaine), indirect oxidation (e.g. nitrates), or metabolic activation (e.g. aniline and dapsone) 90. Classic examples include patient exposure to benzocaine in endoscopy suite and infantile exposure to nitrites from groundwater and wells in rural areas 91.
Most cases of acquired methemoglobinemia are due to accidental exposure to a chemical or through the use of topical or local anesthetics 5. A single center review of 28,478 transesophageal echocardiograms found the incidence of methemoglobinemia to be 0.067% 88. A systematic review of cases of local anesthetic-related methemoglobinemia found that benzocaine was an agent in two-thirds of cases 92. This higher association with benzocaine-containing products has led the United States Food and Drug Administration (FDA) to release multiple advisories regarding the use of benzocaine-containing oral products 93.
Under normal physiologic circumstances, NADPH (nicotinamide adenine dinucleotide phosphate)-MetHb reductase contributes very little to the reduction of methemoglobin, but under oxidative stress, the function of this alternative reduction pathway (NADPH-MetHb reductase) can be enhanced by the presence of exogenous electron donors, such as methylene blue. Methemoglobinemia secondary to accidental exposure to a chemical or through the use of topical or local anesthetics occurs when cytochrome-b5 reductase (CYB5R) ability to reduce ferric (Fe3+) hemoglobin, or methemoglobin, is overwhelmed by the induced oxidant stress. The result is increasing concentrations of methemoglobin leading to methemoglobinemia.
Percentage of methemoglobin is calculated by dividing the concentration of methemoglobin by the concentration of total hemoglobin. Percentage of methemoglobin is likely a better indicator of illness severity than overall concentration, as underlying medical conditions play an important role 5. For example, a methemoglobin concentration of 1.5 g/dL may represent a percentage of 10% in an otherwise healthy patient with a baseline hemoglobin of 15 mg/dL, whereas the presence of the same concentration of 1.5 g/dL of methemoglobin in an anemic patient with a baseline hemoglobin of 8 g/dL would represent a percentage of 18.75% 5. The healthy patient will be left with a functional hemoglobin concentration of 13.5 g/dL and potentially remain asymptomatic while the anemic patient with a functional hemoglobin concentration 6.5 g/dL may be severely symptomatic with a methemoglobin of less than 20%. This may be further compounded by the “functional hemoglobin’s” decreased ability to release oxygen in the presence of methemoglobin. Anemia, congestive heart failure, chronic obstructive pulmonary disease (COPD), and essentially any pathology that impairs the ability to deliver oxygen may worsen the symptoms of methemoglobinemia 5.
In the otherwise healthy person, cyanosis may be clinically evident with a methemoglobin as low as 10% 76. The classic appearance of “chocolate brown blood” can be present at as low as 15% methemoglobin. As the percentage of methemoglobinemia approaches 20%, the patient may experience anxiety, light-headedness, and headaches 5. At methemoglobin levels of 30% to 50%, there may be abnormally rapid breathing (tachypnea), confusion, and loss of consciousness 5. Approaching 50% methemoglobinemia, the patient is at risk for seizures, dysrhythmias, metabolic acidosis, and coma 5. Levels above 70% methemoglobinemia are often fatal 94.
Figure 3. Methemoglobin (MetHb)
Methemoglobinemia causes
Methemoglobinemia can result from either inherited (passed down through families or congenital) or acquired processes 5.
Inherited methemoglobinemia are caused biallelic mutations in the CYB5R3 gene that codes the NADH cytochrome b5 reductase enzyme 77. To date, more than 80 different disease‐causing gene variants in the CYB5R3 gene have been reported 78, 79, 77. Increased frequency of hereditary methemoglobinemia has been found in Siberian Yakuts, Athabaskans, Eskimos, and Navajo 80. Cytochrome-b5 reductase enzyme utilizes NADH formed during glycolysis to reduce methemoglobin back to functional hemoglobin 81.
There are 2 forms of inherited methemoglobinemia. Inherited forms of methemoglobinemia are due to autosomal recessive inheritence in the CYB5R3 genes that code the cytochrome b5 reductase enzyme (CYB5R) 5. The first form of inherited methemoglobinemia is passed on by both parents is also called autosomal recessive congenital methemoglobinemia. The parents usually do not have the condition themselves (autosomal recessive inheritance pattern). They carry the gene that causes the methemoglobinemia. The CYB5R3 gene provides instruction for making an enzyme called cytochrome b5 reductase 3. This enzyme is involved in transferring negatively charged particles called electrons from one molecule to another. Two versions (isoforms) of cytochrome b5 reductase 3 enzyme are produced from the CYB5R3 gene. The soluble isoform is present only in red blood cells, and the membrane-bound isoform is found in all other cell types. The membrane-bound cytochrome b5 reductase 3 isoform is embedded in the membranes of various cellular compartments and is widely used in the body. This cytochrome b5 reductase 3 isoform is necessary for many chemical reactions, including the breakdown and formation of fatty acids, the formation of cholesterol, and the breakdown of various molecules and drugs 95.
There are two types of inherited methemoglobinemia:
- Congenital methemoglobinemia type 1 also called erythrocyte cytochrome B5 reductase deficiency occurs when only the red blood cells lack the cytochrome B5 reductase enzyme. Congenital methemoglobinemia type 1 is mainly due to missense mutations (variants) in the CYB5R3 gene that cause a production of an unstable cytochrome B5 reductase enzyme purely in the red blood cells, associated with methemoglobin levels above 25%, cyanosis, headache, fatigue, and dyspnea. In these cases, cyanosis may be the only sign since most of congenital methemoglobinemia type 1 patients are asymptomatic.
- Congenital methemoglobinemia type 2 also called generalized cytochrome B5 reductase deficiency occurs when all cells lack the cytochrome B5 reductase enzyme 96. Congenital methemoglobinemia type 2 is caused by CYB5R3 gene mutations that lead to either low expression or low activity of the cytochrome B5 reductase enzyme in all the tissues and associated with alterations in the lipid metabolism and neurological involvement. In congenital methemoglobinemia type 2, 8% to 40% of the hemoglobin is in the form of methemoglobin (MetHb) 77. Congenital methemoglobinemia type 2 is associated with high morbidity and mortality because of severe neurologic involvements 72.
- In addition to the autosomal recessive methemoglobinemia subtypes above, a rare methemoglobin group called M group variants of hemoglobin or hemoglobin M disease, results from autosomal dominant mutations (variants) in the genes encoding alpha or beta globin proteins of hemoglobin due to substitution of an amino acid with tyrosine in the alpha‐globin (HBA1, HBA2), beta‐globin (HBB), or gamma‐globin (HBG1, HBG2) 72. In most forms of the hemoglobin M disease, tyrosine is substituted for either the proximal or the distal histidine. Tyrosine can form an iron‐phenolate complex that resists ferric (Fe3+) reduction to the divalent ferrous (Fe2+) state by the metabolic systems of the red blood cell. Patients with hemoglobin M disease are cyanotic but usually otherwise asymptomatic 72. In hemoglobin M disease, structural abnormalities in the globin portion of the molecule cause heme iron to auto‐oxidize 72, 77. The mutation in the alpha‐globin (HBA1, HBA2), beta‐globin (HBB), or gamma‐globin (HBG1, HBG2) leads to easier oxidation of the iron to the ferric (Fe3+) state and allows for the stabilization of iron in the ferric (Fe3+) state. Patients with hemoglobin M disease usually have methemoglobin levels between 15 to 30% and remain asymptomatic 82. Only one parent needs to pass on the abnormal gene for the child to inherit the disease (autosomal dominant inheritance pattern) 97. At least 13 variants of hemoglobin M have been reported (Boston, Fort Ripley, Hyde Park, Iwate, Kankakee, Osaka, Saskatoon) 98, 82, 99, 83. Four hemoglobin M diseases are a consequence of substitution of tyrosine for histidine in the proximal and distal sites of the alpha and beta chains. These four hemoglobin M diseases have been designated by the geographic names of their discovery, i.e. Boston, Saskatoon, Iwate, and Hyde Park. Analogous His→Tyr substitutions in the γ chain of fetal Hb (HbF) have also been documented and have been designated Hb F‐M‐Osaka 19 and Hb FM-Fort Ripley 100. Patients with hemoglobin M develop cyanosis. For the alpha‐globin variants, the dusky color is evident at birth, while the clinical manifestations of beta‐globin variants become evident only after beta chains have replaced the fetal gamma (γ) chains at 6 to 9 months of age. Hemolytic anemia with jaundice can be present, as observed in hemoglobin M Saskatoon and hemoglobin M Hyde Park 101. Additionally, some patients with unstable hemoglobin also have elevated methemoglobin (MetHb) levels associated with hemolytic anemia 102, 103. This is the case of hemoglobin Chile (β28 Leu → Met), an unstable hemoglobin characterized by chronic methemoglobinemia 104.
- In very rare cases, inherited methemoglobinemia is caused by deficiency of the electron acceptor cytochrome b5 84. This causes methemoglobinemia associated with ambiguous genitalia due to a homozygous variant in the CYB5A gene, encoding the microsomal cytochrome b5 85. This condition is due to isolated 17,20‐lyase deficiency since the cofactor cytochrome b5 is required for optimal 17,20‐lyase activity 86.
Acquired methemoglobinemia is more common than the inherited forms. Acquired methemoglobinemia occurs in some people after they are exposed to certain chemicals and drugs that cause oxidation of the hemoglobin either directly or indirectly, including 105, 106:
- Anesthetics such as benzocaine, bupivacaine, lidocaine, prilocaine
- Methylene blue
- Nitrobenzene
- Certain antibiotics (including dapsone and chloroquine)
- Nitrites (used as additives to prevent meat from spoiling)
- Adulterants used in cocaine (local anesthetics, phenacetin)
- Amyl nitrite (poppers)
- Isobutyl nitrite
- Sodium nitrite
- Aniline
- Chloramine
- Metoclopramide
- Nitrate
- Nitric oxide
- Nitrous oxide (laughing gas)
- Nitroglycerin
- Nitroprusside
- Nitrofuran
- Paraquat/monolinuron
- Phenazopyridine (Pyridium)
- Quinones (e.g., chloroquine)
- Rifampin
- Sulfonamides (e.g., sulfamethoxazole)
- Certain foods, such as spinach, beets or carrots contain natural nitrates in large amounts. These foods should not be given to children younger than 6 months of age.
This exposure results in the production of methemoglobin that exceeds the body’s capacity to convert the iron within the hemoglobin back to its ferrous (Fe2+) state. Acquired methemoglobinemia may be due to exposure to direct oxidizing agents (e.g. benzocaine and prilocaine), indirect oxidation (e.g. nitrates), or metabolic activation (e.g. aniline and dapsone) 90. Classic examples include patient exposure to benzocaine in endoscopy suite and infantile exposure to nitrites from groundwater and wells in rural areas 91.
Some recreational drugs are also associated with acquired methemoglobinemia, including amyl nitrate (poppers), nitrous oxide (laughing gas) and adulterants used in cocaine (local anesthetics, phenacetin). These can be associated with very high levels of methemoglobinemia (>90%) and fatalities have been reported 107.
Drugs that induce methemoglobinemia often also cause breakdown of red blood cells (hemolysis). Newborn infants are particularly susceptible to the development of methemoglobinemia because the activity of cytochrome b5 reductase is lower compared to adult period 108. Therefore, methemoglobinemia is observed in infants because of toxic materials, such as aniline dyes used on diapers 109 and the ingestion of nitrate‐contaminated water 110, 111 and even of consumption of silver beets and incorrect storage of homemade purées of mixed vegetables in infants 112.
Inhaled nitric oxide is approved for treatment of infants with pulmonary hypertension because of its vasodilatory effect on pulmonary vessels. During the binding and release of nitric oxide from hemoglobin, methemoglobin is formed at a higher rate. In a study of 163 infants with pulmonary hypertension treated with inhaled nitric oxide, methemoglobin was above 5% in one and between 2.5% and 5% in 16 infants 113.
Methemoglobinemia symptoms
Methemoglobinemia should be considered in the setting of shortness of breath (dyspnea), cyanosis and low level of oxygen in the blood (hypoxemia) that is refractory to supplemental oxygen, especially in the setting of exposure to a known oxidative agent 5. However, the presentation may vary in severity from minimally symptomatic to severe. The clinical presentation of methemoglobinemia is based on a spectrum illness that is associated with cyanosis, pallor, fatigue, weakness, headache, central nervous system depression, metabolic acidosis, seizures, dysrhythmias, coma, and death 5. The degree of symptom severity is multifactorial and depends on the patient’s percentage of methemoglobin, the rate at which methemoglobin was accumulated, the individual’s ability to intrinsically clear it, and the underlying health status of the patient. Duration and magnitude of exposure to an oxidizing agent may also play a role 5.
Methemoglobinemia symptoms are proportional to the fraction of methemoglobin and the resulting hypoxia. A normal methemoglobin fraction is about 1% (range, 0% to 3%). Symptoms associated with higher levels of methemoglobin are as follows 114:
- Less than 10% methemoglobin: None (patients with underlying diseases may have more symptoms at lower level)
- Methemoglobin 10% to 20%: Slight discoloration (eg, pale, gray, blue) of the skin
- Methemoglobin 20% to 30%: Anxiety, headache, tachycardia, lightheadedness
- Methemoglobin 30% to 50%: Dyspnea, weakness, confusion, chest pain
- Methemoglobin 50% to 70%: Arrhythmias; altered mental status, delirium, seizures, coma; profound acidosis
- Methemoglobin greater than 70%: Usually, death 115
The physical examination of patients with suspected methemoglobinemia should include examination of the skin and mucous membranes. Vital signs should be documented, and mental status should be assessed. Careful attention should be paid to the cardiac, respiratory, and circulatory examinations to assess for evidence of an underlying disease (either congenital or acquired).
Methemoglobinemia physical findings may include the following 116:
- Discoloration of the skin and blood (the most striking physical finding)
- Cyanosis – This occurs in the presence of 1.5 g/dL (10%) of methemoglobin (as compared with 5 g/dL of deoxygenated hemoglobin)
- Seizures
- Coma
- Dysrhythmia (eg, bradyarrhythmia or ventricular dysrhythmia)
- Acidosis
- Cardiac or neurologic ischemia
- Pallor of the skin or conjunctiva (suggestive of anemia and possible hemolysis)
- Skeletal abnormalities and intellectual disability
Symptoms of congenital methemoglobinemia type 1 include:
- Bluish coloring of the skin
Symptoms of congenital methemoglobinemia type 2 include:
- Developmental delay
- Failure to thrive
- Intellectual disability
- Seizures
Symptoms of hemoglobin M disease include:
- Bluish coloring of the skin (cyanosis)
Symptoms of acquired methemoglobinemia include:
- Bluish coloring of the skin
- Headache
- Fatigue
- Shortness of breath
- Lack of energy
Methemoglobinemia possible complications
Complications of methemoglobinemia include:
- Shock
- Seizures
- Death
Methemoglobinemia diagnosis and test
Methemoglobinemia is a clinical diagnosis based on history and presenting symptoms, including hypoxemia refractory to supplemental oxygen and the likely presence of chocolate-colored blood 5. Methemoglobinemia diagnosis is confirmed by arterial or venous blood gas with co-oximetry, which will speciate hemoglobin to determine the methemoglobin concentration and percentage 93.
Your blood oxygen level (blood oxygen saturation) is the amount of oxygen you have circulating in your blood. There are two main ways to measure or test blood oxygen levels: through a blood draw test also known as an arterial blood gas (ABG) test and through pulse oximetry using an oximeter. A blood draw test provides much more information about your oxygen levels than an pulse oximeter does.
A baby with methemoglobinemia will have a bluish skin color (cyanosis) at birth or shortly afterward. Your doctor will perform blood tests to diagnose methemoglobinemia. Laboratory studies that may be ordered include the following 117:
- Studies to rule out hemolysis – Complete blood count (CBC), reticulocyte counts, lactate dehydrogenase (LDH), indirect bilirubin, haptoglobin
- Studies to test for organ failure and general end-organ dysfunction – Liver function tests, electrolyte concentrations, blood urea nitrogen (BUN), creatinine
- Urine pregnancy tests
- Heinz body preparation (indicative of oxidative injury to the erythrocyte)
- Hemoglobin electrophoresis to identify hemoglobin M (Hb M); some difficult cases require DNA sequencing of the globin chain gene or mass spectrometry for diagnosis
- Specific enzyme assays for causative deficiencies
- Bedside tests for methemoglobinemia – Examination of blood color on white filter paper after exposure to room air or after aerating a tube of blood with 100% oxygen; if the blood remains dark with these maneuvers, then methemoglobinemia is likely
- Serum levels of nitrites or other offending drugs
Oxygen-carrying capacity of the blood may be determined with the help of the following 117:
- Arterial blood gas (ABG): Blood test to check levels of gases in the blood
- Pulse oximetry (SpO2): Typically less accurate than CO-oximetry in the setting of methemoglobinemia, with the exception of newer multiwavelength pulse oximeters
- CO-oximetry (if available): Measures concentration of oxyhemoglobin, carboxyhemoglobin, methemoglobin, and reduced hemoglobin
A pulse oximeter can also measure blood oxygen saturation levels through a small clip that’s usually placed on your finger or toe. An oximeter reading only indicates what percentage of your blood is saturated with oxygen, known as the SpO2 level, as well as your heart rate. It’s a quick and harmless way to check if someone’s blood oxygen level is too low. However, oxygen saturation (SpO2) measurements cannot be utilized to directly calculate the severity of methemoglobinemia. The traditional dual wave-length pulse oximetry is inaccurate in the setting of methemoglobinemia because these pulse oximeters measure the absorbance of light at two wavelengths at 660 and 940 nm 5. The ratio of this absorbance allows the distinction between oxyhemoglobin and deoxyhemoglobin, with the expressed percentage (SpO2), indicating the measured amount of hemoglobin that is oxygenated 5. Methemoglobin has high absorbance at both of these wavelengths, leading to the interference that causes an inaccurate SpO2 reading 5. When the level of methemoglobin approaches 30% to 35%, the ratio of absorbance of light (A660/A940) becomes 1.0. A ratio of absorbance (A660/A940) of 1.0 reads as a SpO2 of 85% 118. There is a disproportional, inverse relationship between methemoglobin concentration and SpO2, and despite SpO2 being consistently depressed, it is generally a falsely elevated indication of true oxygen saturation that varies depending on a specific device.
Whereas SpO2 measurements are inaccurate and depressed from wavelength interference, often to 75% to 90% even with supplemental oxygen, SaO2 calculations are falsely normal due to the assumption that all hemoglobin is either oxyhemoglobin or deoxyhemoglobin 93 The difference between the depressed SpO2 measurement and the falsely normal SaO2 calculation is known as the “saturation gap” 5. This additional diagnostic clue should hint at the presence of a hemoglobinopathy, but is nonspecific and cannot be used to confirm a diagnosis of methemoglobinemia 5. A saturation gap greater than 5% presents in cases of elevated abnormal forms of hemoglobin such as carboxyhemoglobin, methemoglobin, and sulfhemoglobin 119.
The key diagnostic tests in methemoglobinemia diagnosis are methemoglobin evaluation, measurement of CYB5R activity and DNA sequencing of CYB5R3 gene. Methemoglobin (MetHb) levels are best measured using the change of absorbance of methemoglobin (MetHb) at 630 nm that occurs when cyanide is added, converting the methemoglobin (MetHb) to cyan‐MetHb, as initially described in the spectrophotometric method by Evelyn‐Malloy 120, 121. Human blood contains less than 1% methemoglobin (MetHb). There is a direct correlation between methemoglobin (MetHb) levels and symptoms. CYB5R activity is best measured using ferricyanide as a receptor, measuring the rate of oxidation of NADH 122. In congenital CYB5R3 deficiency, the residual enzyme activity is usually less than 20% of normal. DNA sequencing of CYB5R3 gene allows characterization of the defect and confirmation of the diagnosis.
Electrophoresis at pH 7.1, can be used to identify hemoglobin M disease caused by mutations affecting alpha‐, beta‐, or rarely, gamma‐ globin genes. More than 13 different pathogenic variants have been reported to be associated with hemoglobin M disease in the HbVar database (https://globin.bx.psu.edu/hbvar/). However, when suspecting a hemoglobin M‐variant, targeted sequencing of the alpha‐ and the beta‐globin genes is commonly selected as the technically simpler, more widely available and more specific diagnostic procedure. Direct sequencing of the globin genes is also appropriate, and can be useful in the presence of transfused blood or to exclude electrophoretically silent variants.
Other studies that may be considered are as follows 117:
- Potassium cyanide test to distinguish methemoglobin from sulfhemoglobin
- CT of the head
- Chest radiography to exclude pulmonary or cardiac disease
- Echocardiography to determine the presence of congenital heart disease
Methemoglobinemia treatment
Treatment of methemoglobinemia includes removal of the inciting agent and consideration of treatment with methylene blue (tetramethylthionine chloride). High flow oxygen delivered by non-rebreather mask increases oxygen delivery to tissues and enhances the natural degradation of methemoglobin.
People with hemoglobin M disease don’t have symptoms. So, they may not need treatment.
Methylene blue is used to treat severe methemoglobinemia. Treatment decision should be made on clinical presentation and not withheld for confirmational laboratory values. The methylene blue dose is 1 to 2 mg/kg (0.1-0.2 mL/kg of 1% solution) intravenously over 5 minutes 81. Methylene blue dose can be repeated in 30 to 60 minutes if significant symptoms or methemoglobin levels remain above the treatment threshold.
In cases of acquired methemoglobinemia, treatment with methylene blue should occur when methemoglobin exceeds 20% to 30%, or at lower levels, if the patient is symptomatic 5.
Methylene blue acts by reacting within red blood cell to form leukomethylene blue, which is a reducing agent of oxidized hemoglobin converting the ferric iron (Fe3+) back to its oxygen carrying ferrous state (Fe2+) 123. Methylene blue usually works rapidly and effectively through its interaction with the secondary pathway of methemoglobin reduction, where NADPH-MetHb reductase reduces methylene blue to leukomethylene blue using NADPH from the G6PD-dependent hexose monophosphate shunt 5. Leukomethylene blue then acts as an electron donor to reduce methemoglobin to hemoglobin.
Vitamin C also known as ascorbic acid may also be used to reduce the level of methemoglobin. High-dose ascorbic acid (vitamin C), up to 10 g/dose intravenously, can be considered to treat methemoglobin. However, ascorbic acid (vitamin C) is generally ineffective and not considered standard of care 5. High dose ascorbic acid (vitamin C) administration is associated with increased urinary excretion of oxalate. In the presence of kidney disease, high dose ascorbic acid may be predisposed to kidney failure due to hyperoxaluria 124.
Alternative treatments include hyperbaric oxygen therapy, red blood cell transfusion and exchange transfusions.
In most cases of mild acquired methemoglobinemia, no treatment is needed. But you should avoid the medicine or chemical that caused the problem. Severe cases may need a blood transfusion.
How is methylene blue given?
Methylene blue is injected into a vein through an IV. A doctor will give you this injection. The IV infusion can take up to 30 minutes to complete.
Administration of methylene blue for both children and adults experiencing methemoglobinemia is done intravenously at a dose of 1 mg/kg of a 1% solution over 5 to 30 minutes 1.
Your breathing, blood pressure, oxygen levels, kidney function, and other vital signs will be watched closely while you are receiving methylene blue. Your blood will also need to be tested to help your doctor determine that the medicine is working.
You may only need to receive one dose of methylene blue. If you do need a second dose, it can be given 1 hour after your first dose.
Methylene blue will most likely cause your urine or stools to appear blue or green in color. This is a normal side effect of the medication and will not cause any harm. However, this effect may cause unusual results with certain urine tests.
As an oxidizing agent, methylene blue can actually precipitate methemoglobinemia or hemolysis in high doses or when ineffectively reduced 5. Methylene blue administration in a patient taking a serotonergic drugs such as Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Monoamine Oxidase Inhibitors (MAOIs), and Tricyclic Antidepressants (TCAs) due to the Monoamine Oxidase Inhibitor (MAOI) may precipitate serotonin syndrome (serotonin toxicity) 125. Methylene blue carries a Black Box warning for risk of serious or fatal serotonergic syndrome when used in combination with serotonergic drugs (eg, selective serotonin reuptake inhibitors [SSRIs], serotonin-norepinephrine reuptake inhibitors [SNRIs], and monoamine oxidase inhibitors [MAOIs]) or opioids.
Caution should also be practiced with treating neonates as they are also very sensitive to oxidizing agents. Also, methylene blue is a United States Food and Drug Administration (FDA) pregnancy category X drug, indicating that studies have shown concrete evidence of human fetal risk.
If methylene blue administration is ineffective after the second dose, underlying conditions including, but not limited to, glucose-6-phosphate dehydrogenase (G6PD) deficiency and NADPH-MetHb reductase deficiency should be considered as reasons for refractoriness to treatment. However, methemoglobinemia alone is not an indication to screen for these disease processes.
When treatment with methylene blue is ineffective or not recommended, additional options may include ascorbic acid (Vitamin C), exchange transfusion, hyperbaric oxygen therapy 126, 127.
Methemoglobinemia prognosis
In severe cases, methemoglobinemia prognosis is determined by the degree of anoxic end-organ damage. Death occurs when methemoglobin fractions approach 70% 115. Death can also occur at lower methemoglobin levels in patients with significant comorbidities. Complications of methemoglobinemia may include heart attack (myocardial infarction), seizure, coma, and death.
People with congenital methemoglobinemia type 1 and hemoglobin M disease often do well. Congenital methemoglobinemia type 2 is more serious. It often causes death within the first few years of life.
People with acquired methemoglobinemia often do very well once the drug, food, or chemical that caused the problem is identified and avoided. Most patients with methemoglobinemia respond well to treatment and can be discharged after brief period of observation.
Anyone with persistent symptoms after initial treatment or exacerbated underlying medical conditions should be considered for admission.
Vasoplegic syndrome
Vasoplegic syndrome is generally defined as an arterial pressure <50 mm Hg, cardiac index >2.5 L /min/m², right atrial pressure <5 mm Hg, left atrial pressure <10 mm Hg and low systemic vascular resistance <800 dyne/sec/cm 128.
Risk factors for vasoplegia
Recent studies have established various risk factors for postoperative vasoplegia. These include preoperative use of heparin, ACE inhibitors, congestive heart failure, poor left ventricular function, duration of cardiopulmonary bypass, re-operation, age of the patient and opiod anesthesia 129.
Mechanism of action of methylene blue in vasoplegia
It has been suggested that refractory vasoplegia may reflect a dysregulation of nitric oxide synthesis and vascular smooth cell guanylate cyclase activation. Based on recent pathophysiologic findings it appears that the soluble intracellular enzyme guanylate cyclase is activated to produce cyclic guanosine monophosphate (C-GMP) presumably under the influence of several mediators including nitric oxide 130.
Methylene blue acts by inhibiting guanylate cyclase, thus decreasing C-GMP and vascular smooth muscle relaxation 131.
Preoperative use in cardiac surgery
Methylene blue (1%) has been used IV over 30 min in ICU 1hour before surgery and found decreased incidence and severity of vasoplegic syndrome in high risk patients 128.
Intraoperative use in cardiac surgery
It has also been successfully added to cardiopulmonary bypass prime (2 mg/ kg) and continued as infusion (.25- 2mg/kg/hr) during cardiopulmonary bypass to treat refractory hypotension in septic endocarditis 132.
Postoperative use in cardiac surgery
It can also be used to treat severe vasoplegia in post operative transplant patient 133. Hence studies have concluded decreased mortality in vasoplegic patients after cardiac surgery with methylene blue as compared to placebo 134.
Methylene blue in septic shock
A release of nitric oxide has been incriminated in the cardiovascular alterations of septic shock. Since guanylate cyclase is the target enzyme in the endothelium dependent relaxation mediated by nitric oxide, Methylene blue a potent inhibitor of guanylate cyclase has been found very effective in improving the arterial pressure and cardiac function in septic shock 135, 136, 67.
Studies have found improvement in mean arterial pressure and systemic vascular resistance while decreasing vasopressor requirements in septic shock 137, 135, 138. This systematic review and meta-analysis found that the administration of methylene blue in critically ill adults with septic shock may reduce short-term mortality, duration of vasopressors, and hospital length of stay, with minimal evidence of adverse events 139.
Methylene blue infusion improved hemodynamic status, decreased length of ICU stay, and days on mechanical ventilation 140. In addition, there was no effect on methemoglobin (MHb) levels, suggesting that methylene blue infusion in sepsis and septic shock is safe 140. Early methylene blue start, in the first 8 hour of sepsis, and continuous methylene blue infusion for a longer time, due to a half-life of 5 to 6 hour are probably more effective 141, 142. A recent cohort study demonstrated that the method of methylene blue administration may impact its efficacy in patients experiencing shock, with a reduction in 28-day mortality observed in the group receiving methylene blue through bolus injection followed by continuous infusion 143.
Methylene blue and hepatopulmonary syndrome
The hypoxemia in hepatopulmonary syndrome results from widespread pulmonary vasodilatation due to increased C-GMP. Methylene blue is found to ↑PaO2 and ↓alveolar-arterial difference for partial pressure of oxygen in all pts with hepatopulmonary syndrome. This was due to ↓C-GMP levels by Methylene Blue-a potent inhibitor of guanylate cyclase 144.
Methylene blue as antimalarial
Methylene blue has already been used some 120 years ago against malaria, but it disappeared when chloroquine and other drugs entered the market 24, 25, 26, 2. However recent studies has shown the efficacy of Methylene blue as an effective and cheap antimalarial agent especially in countries with increasing resistance of Plasmodium falciparum malaria to existing 1st line antimalarial agents-chloroquine and pyrimethamine-sulfadoxine.
Methylene blue, a specific inhibitor of Plasmodium falciparum malaria glutathione reductase has the potential to reverse chloroquine resistance and it prevents the polymerization of heme into hemozoin similar to 4-amino-quinoline antimalarials 22, 145, 146, 147,although this concept has been questioned by other experimental evidence 148.
This 2018 review shows that methylene blue has substantial antimalarial activity against all types of malaria in various endemic areas and in combination with other antimalarials, against falciparum malaria in Africa 23. Although methylene blue alone appears to act rather slowly against the asexual parasites of Plasmodium falciparum malaria, it shows synergy with the artemisinin component in rapidly clearing the parasites and it is very effective in reducing the gametocytes and consequently mosquito transmission 23. Methylene blue appears to be a potential alternative to primaquine for reducing post-treatment infectivity in P. falciparum infections, a useful partner for triple combination therapy regimens with the goal of protecting the artemisinin component of the artemisinin-based combination therapy and of reducing the spread of drug-resistant parasites, and a potentially valuable partner drug for mass drug administration in malaria elimination programs 23. Further studies should investigate the efficacy, safety and community acceptance of different artemisinin-based combination therapy in combination with methylene blue against falciparum malaria in different areas inside and outside Africa, while well-designed pilot studies should investigate the effects of methylene blue and methylene blue-containing combination regimens as a treatment for Plasmodium vivax malaria 23.
A dose of 36-72mg/kg over 3 days is the most effective schedule 149.
Apart from the intrinsic antimalarial activity and chloroquine sensitizing action it was also considered to prevent methemoglobinemia- a serious complication of malarial anemia 150.
Methylene blue and cancer
Recent research suggests that methylene blue and other redox cyclers induce selective cancer cell apoptosis by NAD (P) H: quinine oxidoreductase (NQO1)-dependent bioreductive generation of cellular oxidative stress. Hence methylene blue is being investigated for the photodynamic treatment of cancer 151, 152.
The potential of methylene blue for cancer was investigated in several studies in ex vivo models (experiments conducted on living cells or tissues that have been removed) confirmed the cytotoxicity of the methylene blue dye in tumor cells 153, 154. Samy et al. 155 demonstrated a complete response in 55% of patients with basal cell carcinoma during six sessions of methylene blue photodynamic therapy. Matsubara et al 156 reported that methylene blue did not inhibit osteosarcoma growth in mice. In spite of the conflicting data, the results of this 2023 systematic review 157 showed the pronounced efficacy of methylene blue in anticancer photodynamic therapy against colorectal tumor, carcinoma, and melanoma. Also, photodynamic therapy with methylene blue may inhibit the development of breast cancer since during the treatment with photodynamic therapy with methylene blue the tumor growth was significantly lower than in control groups in several preclinical studies. The reasons of the different efficacies of treatment in various types of cancer are not clear since the mechanism of action did not change. It could conceivably be hypothesized that the bioavailability of methylene blue in different target tissues is not equal and this results in different intensities of pharmacological effect.
Methylene blue and ifosfamide-induced encephalopathy
Another, less well known use of methylene blue is its utility for treating ifosfamide neurotoxicity. A toxic metabolite of ifosfamide, chloroacetaldehyde, disrupts the mitochondrial respiratory chain, leading to accumulation of nicotinamide adenine dinucleotide hydrogen (NADH).
Methylene blue acts as an alternative electron acceptor, and reverses the NADH inhibition of hepatic gluconeogenesis while also inhibiting the transformation of chloroethylamine into Chloroacetaldehyde, and also inhibits multiple amine oxidase activities, preventing the formation of Chloroacetaldehyde 158.
Hence it has prophylactic and therapeutic role in ifosfamide – induced encephalopathy 159.
Methylene blue as dye and stain
Methylene blue infusion was found as a safe and effective method of localizing abnormal parathyroid glands 160.
Methylene blue has also been used for intraoperative endoscopic marking of intestinal lumen for location of lesions 161.
Methylene blue was also found as an effective and cheap alternative to isosulfan blue dye for sentinel lymph node localization in pt with breast cancer 162.
Methylene blue also has been used in diagnostic microbiology as a stain. It is an inexpensive and rapid method for detection of Helicobacter pylori (H.pylori) 163.
Methylene blue neutralization of heparin
Methylene blue effectively neutralizes heparin especially in pts with protamine allergy. However work still needs to be done to determine the safety of the drug at the higher doses necessary to neutralize heparin levels achieved in bypass patients 164.
Methylene blue and priapism
Methylene blue has been used to treat high flow priapism by intra-cavernous injection which is known to antagonize endothelial derived relaxation factor 165.
Methylene blue and Alzheimer’s disease
The relationship between methylene blue and Alzheimer’s disease has recently attracted increasing scientific attention. Methylene blue has been shown to attenuate the formations of amyloid plaques and neurofibrillary tangles and partial repair of impairments in mitochondrial function and cellular metabolism 166. Despite several large clinical trials involving more than 2,800 individuals, there is no clear overall benefit of methylene blue and/or derivatives of methylene blue in patients with dementia.
No human studies have tested whether methylene blue prevents dementia or age-related cognitive decline. Preclinical studies suggest that methylene blue does cross the blood-brain barrier 167. One randomized clinical trial investigated the effects of methylene blue in 26 healthy subjects between the ages of 22 and 62 168. Low dose (280 mg or about 4 mg/kg) methylene blue increased insular functional MR imaging (fMRI) activity during a sustained attention task as well as during short-term memory tasks, and significantly improved memory retrieval by 7% compared to placebo 168.
Another randomized clinical trial examined the effect of low dose methylene blue (260 mg or 4mg/kg per day) on a fear extinction task in 42 subjects with claustrophobia 169. Results indicated that methylene blue administration improved fear extinction after 1 month follow up 169. Methylene blue also improved contextual memory independent of its effects of fear extinction.
A randomized open-label study assessed the impact of methylene blue administration on postoperative delirium and early postoperative cognitive dysfunction 170. The study enrolled 248 elderly patients who were scheduled for non-cardiac surgery; they were randomized to receive either 2 mg/kg of methylene blue within the hour after induction of anesthesia or matching saline placebo 170. There were significantly fewer incidents of postoperative delirium in the methylene blue group as compared to the placebo group (7.3% vs. 24.2%); the same was seen with incidence of early postoperative cognitive dysfunction measured at postoperative day 7 (16.1% vs. 40.2%) 170.
Methylene blue is a redox molecule and depending on its environment, it can be present in either its oxidized form known as methylthioninium, or its reduced form known as leucomethylthioninium (LMT). While most applications use methylene blue, several Alzheimer’s disease trials have used a modified, stable form of leucomethylthioninium (LMT) that they have called leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM), hydromethylthionine mesylate (HMTM), or TRx0237, depending on the publication. These different versions of methylene blue are thought to have the same mechanism of action, but TRx0237 is thought to have improved absorption, bioavailability, and tolerance 171, 172. Several studies of methylene blue or methylene blue derivatives have been conducted in patients with
dementia. The results are controversial in the field and are complicated by the difficulty in blinding these trials. Methylene blue and its derivatives cause urine discoloration; therefore, it has been challenging to find an appropriate true placebo. Many studies have instead used lower doses of methylene blue to achieve the urine discoloration while presumably not achieving a biological effect, though later work indicated that perhaps the lower doses were also biologically active. It is unclear whether the urine discoloration is dose dependent and thus whether a lower dose does sufficiently blind patients, and it is unclear whether lower doses are in fact biologically active.
A 24-week phase 2 dose-finding study in 321 patients tested the effect of methylene blue in patients with mild-to-moderate Alzheimer’s disease not currently taking an acetylcholinesterase (AChE) inhibitor or memantine; the study was run by TauRx Therapeutics Ltd (a life sciences/pharmaceutical company incorporated in Singapore) 173. Patients were randomized to either 69, 138, or 228 mg total per day of methylene blue or matching placebo; doses were administered in three oral doses a day, taken with food. In patients with moderate Alzheimer’s, the group receiving 138 mg/day of methylene blue had reduced cognitive decline compared to those receiving placebo treatment (ADAS-cog scores dropped by 1 point from baseline, 5.42 points better than placebo). Likewise, there were improvements in ADCS-CGIC and MMSE scores compared to placebo and baseline. There were no significant differences between groups in cognitive performance in patients with mild Alzheimer’s disease, though the treatment group had reduced decline in relative cerebral blood flow than placebo group patients. Cognitive benefits were maintained during a 50-week extension on methylene blue. There were no benefits at the higher nominal dose of 228 mg/day; the authors speculate that this
was because of a formulation issue that resulted in less drug being bioavailable in the 228 mg/day dose than in the 138 mg/day dose 173. Importantly, the authors referred to their placebo as a placebo and did not comment on the composition of the placebo beyond that it was similar visually to the methylene blue capsules 173.
Methylene blue and TRx0237 treatment in animal models of Alzheimer’s disease and tau suggest mixed results. Some show benefits when treatment is administered before the onset of cognitive deficits but not after. Some suggest they can reverse cognitive deficits. Mixed results suggest that methylene blue and TRx0237 may reduce tau levels, reduce amyloid beta, increase autophagy, increase proteasome activity, reduce aggregation of α-synuclein, and improve cognition 174, 175, 176, 177, 178, 175, 179, while other studies have not replicated these findings; for instance, one preclinical study found that neither methylene blue nor LMTM provided protection against tau-mediated toxicity 180.
Methylene blue reduces oxidative stress in Alzheimer’s disease-like tau and beta-amyloid aggregation in test tube study models 181. In test tube study, methylene blue reduces mitochondrial superoxide production and mitigates free radical formation 182. Methylene blue may influence downstream events of mitochondrial respiration including lipid beta-oxidation, glycolysis, ATP synthesis, ECM production and Na+/K+ ATPase activity, thereby contributing to increased neuronal oxidative metabolic capacity 47. Methylene blue can readily cycle between oxidized (MB) and reduced (MBH2) forms, thereby serving as an electron carrier within the electron transport chain in the mitochondrial matrix 183. Furthermore, methylene blue treatment leads to increases in cellular O2 consumption, ATP production and glucose uptake in primary astrocytes 184.
TauRx Therapeutics Ltd tested TRx0237, a derivative of methylene blue with superior pharmaceutical properties in regards to solubility and parmacokinetics (PK), in a phase 3 study in 891 patients with mild-to-moderate Alzheimer’s disease 185. Patients were randomized to either 150 mg TRx0237 (75 mg twice daily), 250 mg TRx0237 (125 mg twice daily), or a control treatment of 8 mg of TRx0237 (4 mg twice daily) in order to control for urine discoloration; dosing lasted for 15 months 185. The drug failed to have any impact on cognition or function 185. However, a secondary analysis on patients taking the TRx0237 (a derivative of methylene blue) as a monotherapy as compared to as an additional therapy on top of acetylcholinesterase inhibitors (AChEIs) and/or memantine showed significantly reduced rates of cognitive decline (ADAS-Cog, ADCS-CGIC, MMSE), functional decline, (ADCS-ADL) and lateral ventricular volume loss. These benefits were seen even when comparing those taking the placebo (8 mg) as a monotherapy versus add-on therapy. It should be noted that there were only small numbers of patients receiving TRx0237 as a monotherapy, with approximately 25 to 35 patients per group receiving TRx0237 as monotherapy and approximately 130 to 220 patients per group receiving TRx0237 plus other Alzheimer’s disease treatment 185.
Given the findings in Gauthier et al 185 and to further examine these treatment effects, TauRx Therapeutics Ltd modified the statistical analysis of a then-ongoing 18-month phase 3 trial of TRx0237 in 800 patients with mild Alzheimer’s disease 186. Before unblinding, they amended their statistical plan; their primary analysis was changed to (1) compare 200 mg TRx0237 (100 mg twice daily) as a monotherapy to the control treatment of 8 mg TRx0237(4 mg twice daily), and to (2) compare the control treatment as a monotherapy compared to the control treatment as an add-on therapy 186. Results from this study were similar to the secondary analyses of the previous study: the authors reported that patients taking 200 mg TRx0237 as a monotherapy had statistically significantly slower decline in cognitive assessments and brain structural assessments as compared to all patients randomized to the control treatment of 8 mg TRx0237 186. Patients who received 8 mg TRx0237 as monotherapy also had significantly slower decline in cognitive assessments and brain structural assessments as compared to patients receiving 8 mg TRx0237 as add-on therapy 186. Exploratory analyses also split the 200 mg TRx0237 group into two subgroups: those taking TRx0237 as a monotherapy, and those taking TRx0237 as an add-on therapy, and also showed a statistically significant slowing of cognitive and structural decline for those receiving TRx0237 as a monotherapy instead of as an add-on therapy. The authors did not find any differences between patients receiving monotherapy of 8 mg TRx0237 compared to those receiving monotherapy of 200 mg TRx0237 186.
Several scientists and statisticians at the conference pointed out that there is a fundamental difference between patients who are receiving Alzheimer’s disease therapies like acetylcholinesterase inhibitors (AChEIs) and/or memantine compared to those who are not; those receiving symptomatic Alzheimer’s disease treatment are likely more ill and declining faster 187. The patients who received leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM) as a montotherapy in Wilcock et al 186 were less cognitively impaired at baseline and had larger brain volume and glucose uptake on structural imaging than those who were receiving Alzheimer’s disease treatment; while the authors tried to statistically control for these variables, it is unclear whether the statistical control can replicate a trial of only people not on Alzheimer’s disease treatments, and using a true placebo. Critics also stated that one of the primary comparisons – that of the higher dose study drug as a monotherapy versus all patients who received the lower dose whether as a monotherapy or add-on therapy – was not an appropriate comparison 188.
TauRx Therapeutics Ltd then performed pharmacokinetic analysis of samples from the patients in the studies reported in Gauthier et al 185 and Wilcock et al 186 to assess drug concentrations and efficacy outcomes. They reported a plasma drug concentration-response relationship for the drug at the 8 mg/day dose, and that higher doses were not associated with greater efficacy, as though the drug response had plateaued 189. They did identify pharmacological action even as add-on therapy, but with a lower effect size. They hypothesized that a monotherapy regimen of 16 mg per dose would achieve the plasma concentrations necessary to be pharmacologically active and that this would be the maximal effective dose 189. A pharmacokinetic analysis of patients from a trial in frontotemporal dementia (FTD) yielded similar results, with significant exposure dependent differences at 8 mg per day, but worse outcomes at higher concentrations 190.
TauRx Therapeutics Ltd proceeded to run a trial in patients with mild cognitive impairment or dementia who were not on acetylcholinesterase inhibitors (AChEIs) or memantine. The protocol underwent several significant changes over the course of the study, including changes to inclusion criteria, outcome measures, and duration of study. The final study protocol was published by
Wischik et al 191. The trial, known as Lucidity, enrolled 598 individuals with mild cognitive impairment or mild to moderate Alzheimer’s disease, and tested the same derivative of methylene blue as Gauthier et al 185 and Wilcock et al 186 used, though the compound was called hydromethylthionine mesylate (HMTM) in the Lucidity trial. The participants were randomized to one of three groups: control, 8 mg a day hydromethylthionine mesylate (HMTM), or 16 mg a day hydromethylthionine mesylate (HMTM). In order to control for the urine discoloration, the control group received approximately 2 tablets a week of 4 mg oxidized version of methylene blue; the rest of the tablets they received were blank. Therefore, the control dose was lower than the active treatment and a formulation that was hypothesized to be less bioactive than hydromethylthionine mesylate (HMTM), but the control dose nonetheless contained a potentially active ingredient. The trial was double-blinded and randomized for 12 months and was followed by a 12-month modified delayed-start open-label treatment phase 191. The primary endpoints assessed the change in cognitive function from baseline to week 52 in the group receiving 16 mg a day hydromethylthionine mesylate (HMTM) compared to the group receiving control. The results of this trial have not been published in a peer-reviewed journal.
At the Clinical Trials on Alzheimer’s. Disease (CTAD) 2022 meeting, TauRx Therapeutics Ltd announced that the trial failed to meet its primary endpoint; there was no difference in cognitive function from baseline to the end of the double-blind phase between the control group and 16 mg hydromethylthionine mesylate (HMTM) group. They also announced that a majority of the control group had blood levels of active drug that TauRx Therapeutics Ltd believed to be clinically active, and they hypothesized that this was why they didn’t see a difference between the intervention group and control group 192. At the Alzheimer’s Disease and Parkinson’s Disease (ADPD) 2024 conference 193, the authors announced that at the end of the 12-month doubled blinded phase, participants with mild cognitive impairment in the 16 mg/day group had a 48% lower incidence of progression to dementia diagnosis as measured by CDR score than mild cognitive impairment patients in the control group; some critics have pointed out that many trials use CDR-SB, as CDR-SB is thought to be a more sensitive tool in early stages of dementia. The authors also assessed the cognitive function assessments in the mild cognitive impairment group; while the high dose hydromethylthionine mesylate (HMTM) group did not have a significant change from their baseline cognitive scores and the end of the full 24-month trial, the control group appeared to
decline, and the difference between the high dose and control group was statistically significant. It is worth nothing that at the end of the 12-month randomized phase, there was no difference between these groups in terms of cognitive function; the difference only became significant at 18 and 24 months, when the control patients were then receiving 16 mg of hydromethylthionine mesylate (HMTM) daily. The investigators posit that this was due to disease progression in the first year of the trial. In terms of biomarkers, the investigators announced that at 12 months, there was a greater increase in levels of neurofilament light levels in control patients as compared to 16 mg daily hydromethylthionine mesylate (HMTM) patients. This was said to be a pre-specified analysis, though it was not in the published protocol. Finally, the authors compared the cognitive decline and brain volume decline of all patients in the trial (including control group) with matched controls from Alzheimer’s Disease Neuroimaging Initiative (ADNI), as well as meta-analytic controls from other trials, and found that patients in the Lucidity trial had significant reduction in cognitive decline and brain atrophy. This, too, attracted criticism at the conference, with some scientists noting that comparisons to Alzheimer’s Disease Neuroimaging Initiative (ADNI) or patients in other trials cannot replace proper controls 193.
TauRx Therapeutics Ltd’s drug has also been tested in patients with frontotemporal dementia (FTD); as frontotemporal dementia is a tauopathy and leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM) is thought to affect tau levels and/or aggregation, there was interest in whether leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM) might have beneficial effects in frontotemporal dementia patients. The study enrolled 220 patients with frontotemporal dementia and randomized them to either 8 mg leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM) daily, or 200 mg leuco-ethylthioninium bis(hydromethanesulphonate) (LMTM) daily 190. The trial failed to meet any primary or secondary outcomes; there were no significant differences between the groups; as
in the above Alzheimer’s disease trials, the authors posit that this is because the 8 mg daily dose was pharmacologically active 190. Posthoc analyses suggested that in the group that received 8 mg LMTM daily, that patients with higher plasma drug concentrations had significantly less decline on cognitive and functional measurements, but the authors caveat that these are hypothesis generating 190. There is also a case report of a single individual with a familial mutation associated with frontotemporal dementia; he received compassionate treatment with LMTM at the typical age of onset of clinical decline for his family and continued for 5 years 194. Over the course of the 5 years of treatment, the patient remained asymptomatic and experienced less brain volume atrophy than anticipated. However, as this is a case report and a rare mutation, it is difficult to draw any conclusions at this time 194.
Methylene blue photodynamic therapy
Photodynamic therapy using the light activated anti-microbial agent, Methylene blue kills methicillin resistant staphylococcus aureus (MRSA) in superficial and deep excisional wounds 195. Methylene blue in combination with light also inactivates viral nucleic acid of hepatitis-C and human immunodeficiency virus (HIV-1) and treats cases of resistant plaque psoriasis 196, 197.
Methylene blue in pain treatment
Methylene blue is thought to reduce pain via diverse routes, but there is a still lack of scientific evidence how this work. There are still a lot of blanks to be filled in the anti-inflammatory pathways and remain possible links to be uncovered between methylene blue and pain-related receptors. Methylene blue has been used to treat various painful syndromes, including postoperative pain, discogenic pain, and neuropathic pain e.g., intractable idiopathic pruritus ani, pain after open diathermy hemorrhoidectomy and chronic discogenic low back pain 11, 12, 13. There is evidence in the literature to support methylene blue for use as an analgesic for discogenic low back pain 14, 15, 16. In clinical cases, chronic discogenic low back pain patients were improved for at least 3 or 6 months after radiofrequency ablation or radiofrequency denervation with intradiscal methylene blue injection 198, 199, 200, 201. Peng et al. 202 conducted intradiscal methylene blue injection in patients with chronic discogenic low back pain to relieve pain for the first time. Most of patients showed encouraging results and this improvement lasted at least one year. Moreover, there were no noticeable side effects and complications in those patients even after prolonged follow-ups 203.
Methylene blue dose
Methemoglobinemia: Dose commonly used is 1-2mg/kg of 1% Methylene blue solution 123.
Vasoplegic syndrome: Methylene blue is used as a single dose of 1.5 to 2 mg/kg IV infused over 20 min to 1 hour for rescue treatment and may be given pre-operatively and post-operatively to reduce mortality 128, 204, 205.
Antimalarial: A methylene blue dose of 36-72 mg/kg over 3 days is the most effective schedule 149.
When using methylene blue for lymph node mapping, the most common two doses are 2 mL and 5 mL of a 1% solution given intraparenchymal 8.
When used to prevent post-injection pain, when used 45 seconds before propofol administration, the methylene blue dose is 50 mg given as a 2 mL bolus 10.
Treating ifosfamide-induced encephalopathy with methylene blue is given intravenously at a dose of 50 mg every 4 hours until asymptomatic 206.
When using methylene blue to identify the parathyroid glands, methylene blue is administered 1 hour intravenously at a dose of 5 mg/mL before the parathyroidectomy 9.
Using methylene blue to treating Plasmodium falciparum malaria requires 3 days of treatment at a dose of 300 to 1000 mg per day in adults and 20 to 300 mg per day in children of methylene blue, given in combination with chloroquine 207.
Methylene blue side effects
Methylene blue turns urine greenish blue and skin and mucosa bluish discoloration which is self limiting 208. Methylene blue may also cause blurred vision and may impair your thinking or reactions. Be careful if you drive or do anything that requires you to be alert and able to see clearly. Another common side effect of methylene blue is limb pain following IV administration. In adults, methylene blue can cause central nervous system-related symptoms such as dizziness, confusion, and headaches 209. Administration of methylene blue in newborn children (neonates) has led to hyperbilirubinemia, respiratory depression, pulmonary edema, phototoxicity, and hemolytic anemia 210, 211.
Methylene blue may contribute to serotonin syndrome (a serious and potentially life-threatening condition that results from excessive serotonergic activity or excess serotonin in the body) if combined with other serotonergic drugs such as Selective Serotonin Reuptake Inhibitors (SSRIs), Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), Monoamine Oxidase Inhibitors (MAOIs), and Tricyclic Antidepressants (TCAs) due to the Monoamine Oxidase Inhibitor (MAOI) activity that methylene blue has 212, 213. Serotonin syndrome increases sympathetic and neuromuscular activity; therefore, symptoms include diaphoresis, clonus, and tremors.
For at least 24 hours after treatment with methylene blue, avoid exposure to sunlight or tanning beds. This medicine can make you sunburn more easily. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Methylene blue also interferes with the pulse oximeter’s light emission resulting in falsely depressed oxygen saturation reading 41.
Check with your doctor or nurse immediately if any of the following side effects occur:
Incidence not known
- agitation
- bluish-colored lips, fingernails, or palms
- confusion
- cough
- dark urine
- diarrhea
- difficulty breathing
- difficulty swallowing
- dizziness or lightheadedness
- fast heartbeat
- fever
- headache
- hives or welts, itching, or skin rash
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- overactive reflexes
- pale skin
- poor coordination
- rapid heart rate
- redness of the skin
- restlessness
- shivering
- sore throat
- sweating
- talking or acting with excitement you cannot control
- tightness in the chest
- trembling or shaking
- twitching
- unusual bleeding or bruising
- unusual tiredness or weakness
Get emergency help immediately if any of the following symptoms of overdose occur:
Symptoms of methylene blue overdose
- abdominal or stomach pain
- bigger, dilated, or enlarged pupils (black part of the eye)
- blue staining of the urine, skin, and mucous membranes
- bluish-colored lips, fingernails, or palms
- blurred vision
- burning, crawling, itching, numbness, prickling, “pins and needles”, or tingling feelings
- confusion
- dark urine
- difficulty breathing
- dizziness or lightheadedness
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fear
- fever
- headache
- increased sensitivity of the eyes to light
- nausea
- pale skin
- rapid heart rate
- rapid shallow breathing
- shakiness in the legs, arms, hands, or feet
- sore throat
- tightness in the chest
- unusual bleeding or bruising
- unusual tiredness or weakness
- vomiting
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- change in taste
- changes in skin color
- feeling hot or cold
- increased sweating
- loss of taste
- muscle or joint pain
- pain at the infusion site
- pain in the arms or legs
Less common
- back pain
- bruising
- chills
- general feeling of discomfort or illness
- large, flat, blue or purplish patches in the skin
- loss of appetite
- muscle aches and pains
- muscle spasm
- runny nose
- trouble sleeping
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects.
Methylene blue toxicity
Methylene blue is a safe drug when used in therapeutic doses (<2mg/kg) 214. But methylene blue can cause toxicity in high doses. The features of toxicity being cardiac arrhythmias, coronary vasoconstriction, decreased cardiac output, renal blood flow and mesenteric blood flow; increased pulmonary vascular pressure and pulmonary vascular resistance and gas exchange deterioration 214, 215, 20.
Due to methylene blue tissue reactive properties, a case of skin and fat necrosis followed by a dry gangrene of the skin in a female patient with breast cancer who underwent sentinel lymph node biopsy localization using peri-tumoral injection of methylene blue dye has been reported 216.
Methylene blue can also cause hemolytic anemia characterized by Heinz body formation especially in people with severe kidney failure and glucose-6-phosphate dehydrogenase (G6PD) deficiency 41.
Neonates are particularly prone to adverse effects of methylene blue. It causes hyperbilirubinemia, methemoglobin (MetHb) formation, hemolytic anemia, respiratory distress, pulmonary edema, photo toxicity and bluish discoloration of tracheal secretions and urine 217, 218, 219, 220, 221, 222, 223, 224
Methylene blue due to its monoamine oxidase (MAO) inhibiting property may precipitate potentially fatal serotonin toxicity at doses >5mg/kg 225 and rarely can cause severe anaphylactic shock 226.
You can develop serotonin syndrome if you take methylene blue together with antidepressants called selective serotonin reuptake inhibitors (SSRIs), selective serotonin/norepinephrine reuptake inhibitors (SSNRIs) and monoamine oxidase inhibitors.
Common selective serotonin reuptake inhibitors (SSRIs) include citalopram (Celexa), sertraline (Zoloft), fluoxetine (Prozac), paroxetine (Paxil), and escitalopram (Lexapro). Selective serotonin/norepinephrine reuptake inhibitors (SSNRIs) include duloxetine (Cymbalta) and venlafaxine (Effexor). Common monoamine oxidase inhibitors include isocarboxazid (Marplan), phenelzine (Nardil), selegiline (Emsam) and tranylcypromine (Parnate).
If you take these medicines, be sure to read the warning on the packaging. It tells you about the potential risk of serotonin syndrome. However, do not stop taking your medicine. Talk to your doctor about your concerns first.
People with serotonin syndrome will likely stay in the hospital for at least 24 hours for close observation.
Serotonin syndrome treatment may include:
- Benzodiazepine medicines, such as diazepam (Valium) or lorazepam (Ativan) to decrease agitation, seizure-like movements, and muscle stiffness
- Cyproheptadine (Periactin), a drug that blocks serotonin production
- Intravenous (through the vein) fluids
- Withdrawal of medicines that caused the syndrome
In life-threatening cases, medicines that keep the muscles still (paralyze them), and a temporary breathing tube and breathing machine will be needed to prevent further muscle damage.
Serotonin syndrome prognosis
People may get slowly worse and can become severely ill if not quickly treated. Untreated, serotonin syndrome can be deadly. With treatment, symptoms usually go away in less than 24 hours.
Uncontrolled muscle spasms can cause severe muscle breakdown. The products produced when the muscles break down are released into the blood and eventually go through the kidneys. This can cause severe kidney damage if serotonin syndrome isn’t recognized and treated properly.
Serotonin syndrome symptoms occur within minutes to hours, and may include 227:
- Agitation or restlessness
- Diarrhea
- Fast heartbeat and high blood pressure
- Hallucinations
- Increased body temperature
- Loss of coordination
- Nausea and vomiting
- Overactive reflexes
- Rapid changes in blood pressure.
- Bistas E, Sanghavi DK. Methylene Blue. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557593[↩][↩][↩][↩]
- Schirmer RH, Adler H, Pickhardt M, Mandelkow E. Lest we forget you–methylene blue. Neurobiol Aging. 2011;32(12):2325. doi: 10.1016/j.neurobiolaging.2010.12.012[↩][↩][↩][↩]
- Mansouri A, Lurie AA. Concise review: methemoglobinemia. Am J Hematol. 1993;42(1):7–12. doi: 10.1002/ajh.2830420104[↩]
- Coleman MD, Coleman NA. Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf. 1996;14(6):394–405. doi: 10.2165/00002018-199614060-00005[↩]
- Ludlow JT, Wilkerson RG, Nappe TM. Methemoglobinemia. [Updated 2023 Aug 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537317[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- do Nascimento TS, Pereira RO, de Mello HL, Costa J. Methemoglobinemia: from diagnosis to treatment. Rev Bras Anestesiol. 2008 Nov-Dec;58(6):651-64. English, Portuguese. doi: 10.1590/s0034-70942008000600011[↩][↩]
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 34. ISBN 9780857111562.[↩]
- Li J, Chen X, Qi M, Li Y. Sentinel lymph node biopsy mapped with methylene blue dye alone in patients with breast cancer: A systematic review and meta-analysis. PLoS One. 2018 Sep 20;13(9):e0204364. doi: 10.1371/journal.pone.0204364[↩][↩]
- Dudley NE. Methylene blue for rapid identification of the parathyroids. Br Med J. 1971 Sep 18;3(5776):680-1. https://pmc.ncbi.nlm.nih.gov/articles/instance/1798947/pdf/brmedj02666-0044.pdf[↩][↩]
- Salman AE, Salman MA, Saricaoglu F, Akinci SB, Aypar Ü. Pain on injection of propofol: a comparison of methylene blue and lidocaine. J Clin Anesth. 2011 Jun;23(4):270-4. doi: 10.1016/j.jclinane.2010.09.008[↩][↩]
- Kim JH, Kim DH, Lee YP. Long-term follow-up of intradermal injection of methylene blue for intractable, idiopathic pruritus ani. Tech Coloproctol. 2019 Feb;23(2):143-149. doi: 10.1007/s10151-019-01934-x[↩][↩]
- Sim HL, Tan KY. Randomized single-blind clinical trial of intradermal methylene blue on pain reduction after open diathermy hemorrhoidectomy. Colorectal Dis. 2014;16:283–287. doi: 10.1111/codi.12587[↩][↩]
- Peng B, Pang X, Wu Y, Zhao C, Song X. A randomized placebo-controlled trial of intradiscal methylene blue injection for the treatment of chronic discogenic low back pain. Pain. 2010;149:124–129. doi: 10.1016/j.pain.2010.01.021[↩][↩]
- Guo X, Ding W, Liu L, Yang S. Intradiscal methylene blue injection for discogenic low back pain: a meta-analysis. Pain Pract. 2019;19(1):118–129. doi: 10.1111/papr.12725[↩][↩]
- Kallewaard JW, Wintraecken VM, Geurts JW, et al. A multicenter randomized controlled trial on the efficacy of intradiscal methylene blue injection for chronic discogenic low back pain: the IMBI study. Pain. 2019;160(4):945–953. doi: 10.1097/j.pain.0000000000001475[↩][↩]
- Farrokhi MR, Yazdanpanah H, Gholami M, Farrokhi F, Mesbahi AR. Pain and functional improvement effects of methylene blue injection on the soft tissue around fusion site after traumatic thoracolumbar fixation: a double-blind, randomized placebo-controlled study. Clin Neurol Neurosurg. 2016;150:6–12. doi: 10.1016/j.clineuro.2016.08.018[↩][↩]
- Lambden, S., Creagh-Brown, B.C., Hunt, J. et al. Definitions and pathophysiology of vasoplegic shock. Crit Care 22, 174 (2018). https://doi.org/10.1186/s13054-018-2102-1[↩]
- Heyman HM, Serrano RA. Vasoplegic Syndrome and Noncatecholamine Therapies. [Updated 2024 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK599553[↩][↩]
- Ginimuge PR, Jyothi SD. Methylene blue: revisited. J Anaesthesiol Clin Pharmacol. 2010 Oct;26(4):517-20. https://pmc.ncbi.nlm.nih.gov/articles/PMC3087269/[↩][↩][↩][↩]
- Leyh Reiner G, Kofidis Theo, Struber Martin, et al. Methylene Blue: The drug of choice for catecholamine-refractory vasoplegia after cardiopulmonary bypass? J Thorac Cardiovasc Surg. 2003;125:1426–31. doi: 10.1016/s0022-5223(02)73284-4[↩][↩]
- Levin Ricardo L, Degrange Marcela A, Bruno Gustavo F, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496–9. doi: 10.1016/S0003-4975(03)01510-8[↩]
- Schirmer RH, Coulibaly B, Stich A, Scheiwein M, Merkle H, Eubel J, Becker K, Becher H, Muller O, Zich T, et al. Methylene blue as an antimalarial agent. Redox Rep. 2003;8(5):272–275. doi: 10.1179/135100003225002899[↩][↩]
- Lu G, Nagbanshi M, Goldau N, Mendes Jorge M, Meissner P, Jahn A, Mockenhaupt FP, Müller O. Efficacy and safety of methylene blue in the treatment of malaria: a systematic review. BMC Med. 2018 Apr 25;16(1):59. doi: 10.1186/s12916-018-1045-3[↩][↩][↩][↩][↩][↩]
- Guttmann P, Ehrlich P. Über die wirkung des methylenblau bei malaria. Berliner Klin Wochenschr. 1891;28:935–956.[↩][↩]
- Wood HC. The use of methylene blue in malarial fevers. Proc Phila Co Med Soc. 1904;25:281–286.[↩][↩]
- Marshall DG. The “toxicity” of methylene-blue. Lancet. 1920;195(5051):1334. doi: 10.1016/S0140-6736(00)92632-1[↩][↩]
- Zulian GB, Tullen E, Maton B. Methylene blue for ifosfamide-associated encephalopathy. N Engl J Med. 1995;332(18):1239–1240. doi: 10.1056/NEJM199505043321817[↩]
- Kupfer A, Aeschlimann C, Wermuth B, Cerny T. Prophylaxis and reversal of ifosfamide encephalopathy with methylene-blue. Lancet. 1994;343(8900):763–764. doi: 10.1016/S0140-6736(94)91839-2[↩]
- Pelgrims J, De Vos F, Van den Brande J, Schrijvers D, Prové A, Vermorken JB. Methylene blue in the treatment and prevention of ifosfamide-induced encephalopathy: report of 12 cases and a review of the literature. Br J Cancer. 2000 Jan;82(2):291-4. doi: 10.1054/bjoc.1999.0917[↩]
- Ajithkumar T, Parkinson C, Shamshad F, Murray P. Ifosfamide encephalopathy. Clin Oncol (R Coll Radiol). 2007 Mar;19(2):108-14. doi: 10.1016/j.clon.2006.11.003[↩]
- Van der Horst C, Stuebinger H, Seif C, Melchior D, Martinez-Portillo FJ, Juenemann KP. Priapism – etiology, pathophysiology and management. Int Braz J Urol. 2003;29(5):391–400. doi: 10.1590/S1677-55382003000500002[↩]
- Juffermans NP, Vervloet MG, Daemen-Gubbels CRG, Binnekade JM, de Jong M, Groeneveld ABJ. A dose-finding study of methylene blue to inhibit nitric oxide actions in the hemodynamics of human septic shock. Nitric Oxide-Biol Ch. 2010;22(4):275–280. doi: 10.1016/j.niox.2010.01.006[↩]
- Levin RL, Degrange MA, Bruno GF, Del Mazo CD, Taborda DJ, Griotti JJ, Boullon FJ. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77(2):496–499. doi: 10.1016/S0003-4975(03)01510-8[↩]
- Oz M, Lorke DE, Petroianu GA. Methylene blue and Alzheimer’s disease. Biochem Pharmacol. 2009;78(8):927–932. doi: 10.1016/j.bcp.2009.04.034[↩]
- Wischik CM, Edwards PC, Lai RY, Roth M, Harrington CR. Selective inhibition of Alzheimer disease-like tau aggregation by phenothiazines. Proc Natl Acad Sci U S A. 1996;93(20):11213–11218. doi: 10.1073/pnas.93.20.11213[↩]
- Rojas JC, Bruchey AK, Gonzalez-Lima F. Neurometabolic mechanisms for memory enhancement and neuroprotection of methylene blue. Progress in Neurobiology. 2012;96(1):32-45. doi:10.1016/j.pneurobio.2011.10.007. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3265679/[↩][↩][↩]
- Gonzalez-Lima F, Bruchey AK. Extinction memory improvement by the metabolic enhancer methylene blue. Learn Mem. 2004;11:633–640 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC523083/[↩]
- Telch MJ, Bruchey AK, Rosenfield D, et al. Post-Session Administration of USP Methylene Blue Facilitates the Retention of Pathological Fear Extinction and Contextual Memory in Phobic Adults. The American journal of psychiatry. 2014;171(10):1091-1098. doi:10.1176/appi.ajp.2014.13101407. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4467026/[↩]
- Gillman P K. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006;61:1013–4 https://www.ncbi.nlm.nih.gov/pubmed/16978328[↩]
- Gillman PK. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006 Oct;61(10):1013-4. doi: 10.1111/j.1365-2044.2006.04808.x[↩]
- Clifton, Jack II, Leikin, Jerrold Methylene blue. American Journal of Therapeutics. 2003;10:289–91. doi: 10.1097/00045391-200307000-00009[↩][↩][↩]
- Dewachter P, Castro S, Nicaise‐Roland P, Chollet‐Martin S, Le Beller C, Lillo‐le‐Louet A and Mouton‐Faivre C, 2011. Anaphylactic reaction after methylene blue‐treated plasma transfusion. British Journal of Anaesthesia, 106, 687–689. https://doi.org/10.1093/bja/aer009[↩]
- Dyes in aquaculture and reference points for action. EFSA Journal 29 June 2017. https://efsa.onlinelibrary.wiley.com/doi/10.2903/j.efsa.2017.4920[↩]
- Shu Hui, Tang & Ahmad Zaini, Muhammad Abbas. (2015). Isotherm Studies of Methylene Blue Adsorption onto Potassium Salts-Modified Textile Sludge. Jurnal Teknologi. 74. 57-63. 10.11113/jt.v74.4699[↩]
- Oz M., Lorke D.E., Hasan M., Petroianu G.A. Cellular and molecular actions of Methylene Blue in the nervous system. Med. Res. Rev. 2011;31:93–117. doi: 10.1002/med.20177[↩]
- Xue H, Thaivalappil A, Cao K. The Potentials of Methylene Blue as an Anti-Aging Drug. Cells. 2021 Dec 1;10(12):3379. doi: 10.3390/cells10123379[↩]
- Rojas JC, Bruchey AK, Gonzalez-Lima F. Neurometabolic mechanisms for memory enhancement and neuroprotection of methylene blue. Prog Neurobiol. 2012 Jan;96(1):32-45. doi: 10.1016/j.pneurobio.2011.10.007[↩][↩]
- Clifton, Jack II, Leikin, Jerrold Methylene blue. American Journal of Therapeutics. 2003;10:289–91. https://www.ncbi.nlm.nih.gov/pubmed/12845393[↩]
- Clifton J 2nd, Leikin JB. Methylene blue. Am J Ther. 2003 Jul-Aug;10(4):289-91. doi: 10.1097/00045391-200307000-00009[↩]
- Kidd SA, Lancaster PA, Anderson JC, Boogert A, Fisher CC, Robertson R, Wass DM. Fetal death after exposure to methylene blue dye during mid-trimester amniocentesis in twin pregnancy. Prenat Diagn. 1996 Jan;16(1):39-47. doi: 10.1002/(SICI)1097-0223(199601)16:1<39::AID-PD789>3.0.CO;2-P[↩]
- Friedlaender P. (1877). Fortschritte der Theerfarbenfabrikation und verwandter Industriezweige. Berlin: Springer.[↩]
- Emadi E, Hamidi Alamdari D, Attaran D, Attaran S. Application of methylene blue for the prevention and treatment of COVID-19: A narrative review. Iran J Basic Med Sci. 2024;27(7):780-792. doi: 10.22038/IJBMS.2024.71871.15617[↩][↩]
- Ehrlich P. (1886). Ueber die Methylenblaureaction der lebenden Nervensubstanz. Dtsch. Med. Wochenschr. 12 (04), 49–52. 10.1055/s-0028-1139684[↩]
- Ehrlich P., Leppmann A. (1890). Ueber schmerzstillende wirkung des methylenblau. Dtsch. Med. Wochenschr. 16 (23), 493–494. 10.1055/s-0029-1209911[↩]
- Saikrupa B, Muthukumar M, Kavya S, Suma PK. Rational Use of Methylene Blue in COVID-19 Treatment. JDDT. 2022;12:181–186.[↩]
- Kaufmann P. (1919). Über die Wirkung von Methylenblau bei Malaria. Dtsch. Med. Wochenschr. 45 (49), 1365. 10.1055/s-0028-1138168[↩]
- Schirmer R. H., Coulibaly B., Stich A., Scheiwein M., Merkle H., Eubel J., et al. (2003). Methylene blue as an antimalarial agent. Redox Rep. 8 (5), 272–275. 10.1179/135100003225002899[↩]
- Giles GM. Recent German Researches on Malaria: Its Treatment by Methylene Blue. With Introductory Remarks. Ind Med Gaz. 1892 Nov;27(11):326-330. https://pmc.ncbi.nlm.nih.gov/articles/instance/5137094/pdf/indmedgaz71216-0006.pdf[↩]
- Moore J. The Use of Methylene Blue in Gonorrhoea. Br Med J. 1897 Jan 16;1(1881):140. https://pmc.ncbi.nlm.nih.gov/articles/instance/2432748/pdf/brmedj08647-0016a.pdf[↩]
- Frost GH. Methylene-Blue in Fevers. Ind Med Gaz. 1908 Oct;43(10):395. https://pmc.ncbi.nlm.nih.gov/articles/instance/5183153/pdf/indmedgaz73291-0041a.pdf[↩]
- Pan P. F., Wang Y., Li X. P., Yang C. B., Zhong H., Du X. X., et al. (2019). Effects of methylene blue on the nitric oxide-soluble guanylate cyclase-cyclic guanylyl monophosphate pathway and cytokine levels in rats with sepsis. Int. J. Clin. Exp. Med. 12 12203–12211.[↩]
- Wolin MS, Cherry PD, Rodenburg JM, Messina EJ, Kaley G. Methylene blue inhibits vasodilation of skeletal muscle arterioles to acetylcholine and nitric oxide via the extracellular generation of superoxide anion. J Pharmacol Exp Ther. 1990 Sep;254(3):872-6.[↩]
- Cohen N., Robinson D., Ben-Ezzer J., Hemo Y., Hasharoni A., Wolmann Y., et al. (2000). Reduced NO accumulation in arthrotic cartilage by exposure to methylene blue. Acta Orthop. Scand. 71 630–636. 10.1080/000164700317362299[↩]
- Gachot B, Bedos J.P, Veber B, Wolff M, Regnier B. Short-term effects of methylene blue on hemodynamics and gas exchange in humans with septic shock. Intensive Care Medicine. 1995;21:1027–31. doi: 10.1007/BF01700666[↩]
- Bosoy , Dimitry , Axelband , et al. Utilization of methylene blue in the setting of hypotension associated with concurrent renal and hepatic failure: a concise review. OPUS 12 Scientist. 2008;2:21–9.[↩]
- Peter schenk, Christian Madl, Shahrzad Rezaie-Majd, Stephen Lehr, Christian Muller. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000;133:701–6.[↩]
- Preiser, Jean-Charles, Lejeune, et al. Methylene blue administration in septic shock: A Clinical Trial. Critical Care Medicine. 1995;23:259–64.[↩][↩]
- Lee SW, Han HC. Methylene Blue Application to Lessen Pain: Its Analgesic Effect and Mechanism. Front Neurosci. 2021 May 17;15:663650. doi: 10.3389/fnins.2021.663650[↩]
- Karuppan Perumal MK, Rajan Renuka R, Manickam Natarajan P. Evaluating the potency of laser-activated antimicrobial photodynamic therapy utilizing methylene blue as a treatment approach for chronic periodontitis. Front Oral Health. 2024 May 30;5:1407201. doi: 10.3389/froh.2024.1407201[↩]
- Dong Q, Kang Y, Zhang R. Treatment of Superficial Mycoses Using Photodynamic Therapy: A Systematic Review and Meta-Analysis. Photobiomodul Photomed Laser Surg. 2023 Feb;41(2):37-47. https://doi.org/10.1089/photob.2022.0117[↩]
- Arastoo M, Mazanetz MP, Miller S, Shiells H, Hull C, Robinson K, Storey JMD, Harrington CR, Wischik CM. Exploring the Anti-Hypoxaemia Effect of Hydromethylthionine: A Prospective Study of Phase 3 Clinical Trial Participants. Int J Mol Sci. 2023 Sep 6;24(18):13747. doi: 10.3390/ijms241813747[↩]
- Iolascon A, Bianchi P, Andolfo I, et al. SWG of red cell and iron of EHA and EuroBloodNet. Recommendations for diagnosis and treatment of methemoglobinemia. Am J Hematol. 2021 Dec 1;96(12):1666-1678. doi: 10.1002/ajh.26340[↩][↩][↩][↩][↩][↩]
- McQueen CA, ed. Comprehensive Toxicology. 3rd ed. Amsterdam, Netherlands: Elsevier; 2017. Vol 12.[↩]
- Benz EJ Jr, Ebert BL. Hemoglobin Variants Associated With Hemolytic Anemia, Altered Oxygen Affinity, and Methemoglobinemias. In: Hoffman R, Benz EJ Jr, Slberstein LE, Heslop H, Weitz J, Anastasi J, eds. Hematology: Basic Principles and Practice. 7th ed. Philadelphia, PA: Elsevier/Saunders; 2018. 608-15.[↩]
- Prchal J. Chapter 51: Methemoglobinemia and Other Dyshemoglobinemias. 10th ed. McGraw Hill; 2021.[↩]
- Wright RO, Lewander WJ, Woolf AD. Methemoglobinemia: etiology, pharmacology, and clinical management. Ann Emerg Med. 1999 Nov;34(5):646-56. doi: 10.1016/s0196-0644(99)70167-8[↩][↩]
- Percy MJ, Lappin TR. Recessive congenital methaemoglobinaemia: cytochrome b(5) reductase deficiency. Br J Haematol. 2008 May;141(3):298-308. doi: 10.1111/j.1365-2141.2008.07017.x[↩][↩][↩][↩][↩][↩]
- Dekker J, Eppink MH, van Zwieten R, de Rijk T, Remacha AF, Law LK, Li AM, Cheung KL, van Berkel WJ, Roos D. Seven new mutations in the nicotinamide adenine dinucleotide reduced-cytochrome b(5) reductase gene leading to methemoglobinemia type I. Blood. 2001 Feb 15;97(4):1106-14. doi: 10.1182/blood.v97.4.1106[↩][↩]
- Nicolas-Jilwan M. Recessive congenital methemoglobinemia type II: Hypoplastic basal ganglia in two siblings with a novel mutation of the cytochrome b5 reductase gene. Neuroradiol J. 2019 Apr;32(2):143-147. doi: 10.1177/1971400918822153[↩][↩]
- Burtseva TE, Ammosova TN, Protopopova NN, Yakovleva SY, Slobodchikova MP. Enzymopenic Congenital Methemoglobinemia in Children of the Republic of Sakha (Yakutia). J Pediatr Hematol Oncol. 2017 Jan;39(1):42-45. doi: 10.1097/MPH.0000000000000705[↩][↩]
- Skold A, Cosco DL, Klein R. Methemoglobinemia: pathogenesis, diagnosis, and management. South Med J. 2011 Nov;104(11):757-61. doi: 10.1097/SMJ.0b013e318232139f[↩][↩][↩]
- Curry S. Methemoglobinemia. Ann Emerg Med. 1982 Apr;11(4):214-21. doi: 10.1016/s0196-0644(82)80502-7[↩][↩][↩]
- Haymond S, Cariappa R, Eby CS, Scott MG. Laboratory assessment of oxygenation in methemoglobinemia. Clin Chem. 2005 Feb;51(2):434-44. doi: 10.1373/clinchem.2004.035154[↩][↩]
- Hegesh E, Hegesh J, Kaftory A. Congenital methemoglobinemia with a deficiency of cytochrome b5. N Engl J Med. 1986 Mar 20;314(12):757-61. doi: 10.1056/NEJM198603203141206[↩][↩]
- Kok RC, Timmerman MA, Wolffenbuttel KP, Drop SL, de Jong FH. Isolated 17,20-lyase deficiency due to the cytochrome b5 mutation W27X. J Clin Endocrinol Metab. 2010 Mar;95(3):994-9. doi: 10.1210/jc.2008-1745[↩][↩]
- Idkowiak J, Randell T, Dhir V, Patel P, Shackleton CH, Taylor NF, Krone N, Arlt W. A missense mutation in the human cytochrome b5 gene causes 46,XY disorder of sex development due to true isolated 17,20 lyase deficiency. J Clin Endocrinol Metab. 2012 Mar;97(3):E465-75. doi: 10.1210/jc.2011-2413[↩][↩]
- McGuigan MA. Benzocaine-induced methemoglobinemia. Can Med Assoc J. 1981 Oct 15;125(8):816. https://pmc.ncbi.nlm.nih.gov/articles/instance/1862717/pdf/canmedaj01353-0018a.pdf[↩]
- Kane GC, Hoehn SM, Behrenbeck TR, Mulvagh SL. Benzocaine-induced methemoglobinemia based on the Mayo Clinic experience from 28 478 transesophageal echocardiograms: incidence, outcomes, and predisposing factors. Arch Intern Med. 2007 Oct 8;167(18):1977-82. doi: 10.1001/archinte.167.18.1977[↩][↩]
- O’Donohue WJ, Moss LM, Angelillo VA. Acute Methemoglobinemia Induced by Topical Benzocaine and Lidocaine. Arch Intern Med. 1980;140(11):1508–1509. doi:10.1001/archinte.1980.00330220067023[↩]
- Bradberry SM. Occupational methaemoglobinaemia. Mechanisms of production, features, diagnosis and management including the use of methylene blue. Toxicol Rev. 2003;22(1):13-27. doi: 10.2165/00139709-200322010-00003[↩][↩]
- Johnson CJ, Kross BC. Continuing importance of nitrate contamination of groundwater and wells in rural areas. Am J Ind Med. 1990;18(4):449-56. doi: 10.1002/ajim.4700180416[↩][↩]
- Guay J. Methemoglobinemia related to local anesthetics: a summary of 242 episodes. Anesth Analg. 2009 Mar;108(3):837-45. doi: 10.1213/ane.0b013e318187c4b1[↩]
- Nappe TM, Pacelli AM, Katz K. An Atypical Case of Methemoglobinemia due to Self-Administered Benzocaine. Case Rep Emerg Med. 2015;2015:670979. doi: 10.1155/2015/670979[↩][↩][↩]
- Wilkerson RG. Getting the blues at a rock concert: a case of severe methaemoglobinaemia. Emerg Med Australas. 2010 Oct;22(5):466-9. doi: 10.1111/j.1742-6723.2010.01336.x[↩]
- CYB5R3 gene. https://medlineplus.gov/genetics/gene/cyb5r3[↩]
- Kedar PS, Gupta V, Warang P, Chiddarwar A, Madkaikar M. Novel mutation (R192C) in CYB5R3 gene causing NADH-cytochrome b5 reductase deficiency in eight Indian patients associated with autosomal recessive congenital methemoglobinemia type-I. Hematology. 2018 Sep;23(8):567-573. doi: 10.1080/10245332.2018.1444920[↩]
- Spears F, Banerjee A. Hemoglobin M variant and congenital methemoglobinemia: methylene blue will not be effective in the presence of hemoglobin M. Can J Anaesth. 2008 Jun;55(6):391-2. doi: 10.1007/BF03021499[↩]
- Kulozik AE. Hemoglobin variants and the rarer hemoglobin disorders. Pediatric Hematology; Wiley; 2006:231‐254.[↩]
- van Zwieten R, Verhoeven AJ, Roos D. Inborn defects in the antioxidant systems of human red blood cells. Free Radic Biol Med. 2014 Feb;67:377-86. doi: 10.1016/j.freeradbiomed.2013.11.022[↩]
- Priest JR, Watterson J, Jones RT, Faassen AE, Hedlund BE. Mutant fetal hemoglobin causing cyanosis in a newborn. Pediatrics. 1989 May;83(5):734-6.[↩]
- Wild B, Bain BJ. Investigation of abnormal haemoglobins and thalassaemia. Dacie and Lewis Practical Haematology. 10th ed. Churchill Livingstone; 2006:271‐310.[↩]
- Agarwal AM, Prchal JT. Methemoglobinemia and other dyshemoglobinemias. In: Kaushansky K, Lichtman MA, Prchal JT, et al., eds. Williams Hematology, 9e; McGraw‐Hill; 2015.[↩]
- Stamatoyannopoulos G, Nute PE, Giblett E, Detter J, Chard R. Haemoglobin M Hyde Park occurring as a fresh mutation: diagnostic, structural, and genetic considerations. J Med Genet. 1976 Apr;13(2):142-7. https://pmc.ncbi.nlm.nih.gov/articles/instance/1013374/pdf/jmedgene00309-0062.pdf[↩]
- Hojas-Bernal R, McNab-Martin P, Fairbanks VF, Holmes MW, Hoyer JD, McCormick DJ, Kubik KS. Hb Chile [beta28(B10)Leu–>Met]: an unstable hemoglobin associated with chronic methemoglobinemia and sulfonamide or methylene blue-induced hemolytic anemia. Hemoglobin. 1999 May;23(2):125-34. doi: 10.3109/03630269908996157[↩]
- King A., Menke N., Katz K. Toxic hemoglobinopathies in the emergency department. EM Critical Care. 2013;3(6):1–17.[↩]
- Ashurst J, Wasson M. Methemoglobinemia: a systematic review of the pathophysiology, detection, and treatment. Del Med J. 2011 Jul;83(7):203-8.[↩]
- Hunter L, Gordge L, Dargan PI, Wood DM. Methaemoglobinaemia associated with the use of cocaine and volatile nitrites as recreational drugs: a review. Br J Clin Pharmacol. 2011 Jul;72(1):18-26. doi: 10.1111/j.1365-2125.2011.03950.x[↩]
- Lo SC, Agar NS. NADH-methemoglobin reductase activity in the erythrocytes of newborn and adult mammals. Experientia. 1986 Dec 1;42(11-12):1264-5. doi: 10.1007/BF01946415[↩]
- Graubarth J, Bloom CJ, Coleman FC, Solomon HN. Dye poisoning in the nursery: a review of seventeen cases. JAMA. 1945;128(16):1155‐1157.[↩]
- Knobeloch L, Proctor M. Eight blue babies. WMJ. 2001;100(8):43-7.[↩]
- Lukens JN. The Legacy of Well-Water Methemoglobinemia. JAMA. 1987;257(20):2793–2795. doi:10.1001/jama.1987.03390200133028[↩]
- Sanchez-Echaniz J, Benito-Fernández J, Mintegui-Raso S. Methemoglobinemia and consumption of vegetables in infants. Pediatrics. 2001 May;107(5):1024-8. doi: 10.1542/peds.107.5.1024[↩]
- Hamon I, Gauthier-Moulinier H, Grelet-Dessioux E, Storme L, Fresson J, Hascoet JM. Methaemoglobinaemia risk factors with inhaled nitric oxide therapy in newborn infants. Acta Paediatr. 2010 Oct;99(10):1467-73. doi: 10.1111/j.1651-2227.2010.01854.x[↩]
- Methemoglobinemia. https://emedicine.medscape.com/article/204178-overview[↩]
- Mun SH, Park GJ, Lee JH, Kim YM, Chai HS, Kim SC. Two cases of fatal methemoglobinemia caused by self-poisoning with sodium nitrite: A case report. Medicine (Baltimore). 2022 Feb 18. 101 (7):e28810.[↩][↩]
- Methemoglobinemia Clinical Presentation. https://emedicine.medscape.com/article/204178-clinical#b3[↩]
- Methemoglobinemia Workup. https://emedicine.medscape.com/article/204178-workup[↩][↩][↩]
- Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med. 2013 Jun;107(6):789-99. doi: 10.1016/j.rmed.2013.02.004[↩]
- Akhtar J, Johnston BD, Krenzelok EP. Mind the gap. J Emerg Med. 2007 Aug;33(2):131-2. doi: 10.1016/j.jemermed.2006.11.016[↩]
- Evelyn KE, Malloy HT. Microdetermination of oxyhemoglobin, methemoglobin, and sulfhemoglobin in a single sample of blood. J Biol Chem. 1938;126(2):655‐662.[↩]
- Beutler E. Carboxyhemoglobin, methemoglobin, and sulfhemoglobin determinations. In: Beutler E, Lichtman MA, Coller BS, Kipps TJ, eds. Williams Hematology. McGraw‐Hill; 1995.[↩]
- Beutler E. Red Cell Metabolism: A Manual of Biochemical Methods. Grune & Stratton; 1984.[↩]
- Methemoglobinemia: a case study. Boylston M, Beer D. Crit Care Nurse. 2002 Aug; 22(4):50-5. http://ccn.aacnjournals.org/content/22/4/50.long[↩][↩]
- Lee KW, Park SY. High-dose vitamin C as treatment of methemoglobinemia. Am J Emerg Med. 2014 Aug;32(8):936. doi: 10.1016/j.ajem.2014.05.030[↩]
- Ramsay RR, Dunford C, Gillman PK. Methylene blue and serotonin toxicity: inhibition of monoamine oxidase A (MAO A) confirms a theoretical prediction. Br J Pharmacol. 2007 Nov;152(6):946-51. doi: 10.1038/sj.bjp.0707430[↩]
- Grauman Neander N, Loner CA, Rotoli JM. The Acute Treatment of Methemoglobinemia in Pregnancy. J Emerg Med. 2018 May;54(5):685-689. doi: 10.1016/j.jemermed.2018.01.038[↩]
- Cho Y, Park SW, Han SK, Kim HB, Yeom SR. A Case of Methemoglobinemia Successfully Treated with Hyperbaric Oxygenation Monotherapy. J Emerg Med. 2017 Nov;53(5):685-687. doi: 10.1016/j.jemermed.2017.04.036[↩]
- Ertugrul Ozal, Erkan Kuralay, Vedat Yildirim, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79:1615–9. https://www.ncbi.nlm.nih.gov/pubmed/15854942[↩][↩][↩]
- Armand Mekontso-Dessap, Remi Houel, Celine Soustelle, Matthias Kirsch, Dominique Thebert, Daniel Y. Loisance.Risk factors for post-cardiopulmonary bypass vasoplegia in patients with preserved left ventricular function. Ann Thorac Surg. 2001;71:1428–32. https://www.ncbi.nlm.nih.gov/pubmed/11383777[↩]
- Levin Ricardo L, Degrange Marcela A, Bruno Gustavo F, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496–9. https://www.ncbi.nlm.nih.gov/pubmed/14759425[↩]
- Gachot B, Bedos J.P, Veber B, Wolff M, Regnier B. Short-term effects of methylene blue on hemodynamics and gas exchange in humans with septic shock. Intensive Care Medicine. 1995;21:1027–31 https://www.ncbi.nlm.nih.gov/pubmed/8750129[↩]
- Grayling M, Deakin C D. Methylene blue during cardiopulmonary bypass to treat refractory hypotension in septic endocarditis. J Thorac Cardiovasc Surg. 2003;125:426–7.[↩]
- Kofidis T, Struber M, Wilhelmi M, et al. Reversal of severe vasoplegia with single-dose methylene blue after heart transplantation. J Thoracic Cardiovasc Surg. 2001;122:823–4.[↩]
- Levin Ricardo L, Degrange Marcela A, Bruno Gustavo F, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004;77:496–9.[↩]
- Arias-Ortiz J, Vincent JL. Administration of methylene blue in septic shock: pros and cons. Crit Care. 2024 Feb 16;28(1):46. doi: 10.1186/s13054-024-04839-w[↩][↩]
- Rudiger A, Singer M. Decatecholaminisation during sepsis. Crit Care. 2016 Oct 4;20(1):309. doi: 10.1186/s13054-016-1488-x[↩]
- Ibarra-Estrada M, Kattan E, Aguilera-González P, Sandoval-Plascencia L, Rico-Jauregui U, Gómez-Partida CA, Ortiz-Macías IX, López-Pulgarín JA, Chávez-Peña Q, Mijangos-Méndez JC, Aguirre-Avalos G, Hernández G. Early adjunctive methylene blue in patients with septic shock: a randomized controlled trial. Crit Care. 2023 Mar 13;27(1):110. doi: 10.1186/s13054-023-04397-7[↩]
- Edmund S, Kwok H, Howers Daniel. Use of methylene blue in sepsis: A Systematic Review. Journal of Intensive Care Medicine. 2006;21:359–63.[↩]
- Fernando SM, Tran A, Soliman K, Flynn B, Oommen T, Wenzhe L, Adhikari NKJ, Kanji S, Seely AJE, Fox-Robichaud AE, Wax RS, Cook DJ, Lamontagne F, Rochwerg B. Methylene Blue in Septic Shock: A Systematic Review and Meta-Analysis. Crit Care Explor. 2024 Jun 21;6(7):e1110. doi: 10.1097/CCE.0000000000001110[↩]
- Ballarin RS, Lazzarin T, Zornoff L, Azevedo PS, Pereira FWL, Tanni SE, Minicucci MF. Methylene blue in sepsis and septic shock: a systematic review and meta-analysis. Front Med (Lausanne). 2024 Apr 18;11:1366062. doi: 10.3389/fmed.2024.1366062[↩][↩]
- Belletti A, Musu M, Silvetti S, Saleh O, Pasin L, Monaco F, et al. Non-adrenergic vasopressors in patients with or at risk for vasodilatory shock. A systematic review and Meta-analysis of randomized trials. PLoS One. (2015) 10:e0142605. doi: 10.1371/journal.pone.0142605[↩]
- Zhao CC, Zhai YJ, Hu ZJ, Huo Y, Li ZQ, Zhu GJ. Efficacy and safety of methylene blue in patients with vasodilatory shock: a systematic review and meta-analysis. Front Med (Lausanne). 9:950596. doi: 10.3389/fmed.2022.950596[↩]
- Sari-Yavuz S, Heck-Swain KL, Keller M, Magunia H, Feng YS, Haeberle HA, Wied P, Schlensak C, Rosenberger P, Koeppen M. Methylene blue dosing strategies in critically ill adults with shock-A retrospective cohort study. Front Med (Lausanne). 2022 Oct 28;9:1014276. doi: 10.3389/fmed.2022.1014276. Erratum in: Front Med (Lausanne). 2022 Nov 23;9:1094735. doi: 10.3389/fmed.2022.1094735[↩]
- Peter schenk, Christian Madl, Shahrzad Rezaie-Majd, Stephen Lehr, Christian Muller. Methylene blue improves the hepatopulmonary syndrome. Ann Intern Med. 2000;133:701–6[↩]
- Farber PM, Arscott LD, Williams CH, Jr, Becker K, Schirmer RH. Recombinant Plasmodium falciparum glutathione reductase is inhibited by the antimalarial dye methylene blue. FEBS Lett. 1998;422(3):311–314. doi: 10.1016/S0014-5793(98)00031-3[↩]
- Sarma GN, Savvides SN, Becker K, Schirmer M, Schirmer RH, Karplus PA. Glutathione reductase of the malarial parasite Plasmodium falciparum: crystal structure and inhibitor development. J Mol Biol. 2003;328(4):893–907. doi: 10.1016/S0022-2836(03)00347-4[↩]
- Buchholz K, Schirmer RH, Eubel JK, Akoachere MB, Dandekar T, Becker K, Gromer S. Interactions of methylene blue with human disulfide reductases and their orthologues from Plasmodium falciparum. Antimicrob Agents Chemother. 2008;52(1):183–191. doi: 10.1128/AAC.00773-07[↩]
- Pastrana-Mena R, Dinglasan RR, Franke-Fayard B, Vega-Rodriguez J, Fuentes-Caraballo M, Baerga-Ortiz A, Coppens I, Jacobs-Lorena M, Janse CJ, Serrano AE. Glutathione reductase-null malaria parasites have normal blood stage growth but arrest during development in the mosquito. J Biol Chem. 2010;285(35):27045–27056. doi: 10.1074/jbc.M110.122275[↩]
- Meissner Peter E, Germain Mandi, Boubacar Coulibaly, et al. Methylene blue for malaria in Africa: results from a dose-finding study in combination with chloroquine. Malaria Journal. 2006;5:84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1617109/[↩][↩]
- Schirmer R.H, Coulibaly B, Stich A, et al. Methylene blue as an antimalarial agent. Redox rep. 2003;8:272–5. https://www.ncbi.nlm.nih.gov/pubmed/14962363[↩]
- Wondrak GT. NQO1-activated phenothiazinium redox cyclers for the targeted bioreductive induction of cancer cell apoptosis. Free Radic Biol Med. 2007;43:178–90 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2705808/[↩]
- Cecatto R. B., de Magalhaes L. S., Rodrigues M. F. S. D., Pavani C., Lino-dos-Santos-Franco A., Gomes M. T., et al. (2020). Methylene blue mediated antimicrobial photodynamic therapy in clinical human studies: the state of the art. Photodiagnosis Photodyn. Ther. 31, 101828. 10.1016/j.pdpdt.2020.101828[↩]
- Sahu A., Choi W. I., Lee J. H., Tae G. (2013). Graphene oxide mediated delivery of methylene blue for combined photodynamic and photothermal therapy. Biomaterials 34 (26), 6239–6248. 10.1016/j.biomaterials.2013.04.066[↩]
- Moghassemi S., Dadashzadeh A., de Azevedo R. B., Amorim C. A. (2022). Secure transplantation by tissue purging using photodynamic therapy to eradicate malignant cells. J. Photochem. Photobiol. B, Biol. 234, 112546. 10.1016/j.jphotobiol.2022.112546[↩]
- Samy N. A., Salah M. M., Ali M. F., Sadek A. M. (2015). Effect of methylene blue-mediated photodynamic therapy for treatment of basal cell carcinoma. Lasers Med. Sci. 30, 109–115. 10.1007/s10103-014-1609-1[↩]
- Matsubara T, Kusuzaki K, Matsumine A, Satonaka H, Shintani K, Nakamura T, Uchida A. Methylene blue in place of acridine orange as a photosensitizer in photodynamic therapy of osteosarcoma. In Vivo. 2008 May-Jun;22(3):297-303. https://iv.iiarjournals.org/content/invivo/22/3/297.full.pdf[↩]
- Taldaev A, Terekhov R, Nikitin I, Melnik E, Kuzina V, Klochko M, Reshetov I, Shiryaev A, Loschenov V, Ramenskaya G. Methylene blue in anticancer photodynamic therapy: systematic review of preclinical studies. Front Pharmacol. 2023 Sep 28;14:1264961. doi: 10.3389/fphar.2023.1264961[↩]
- Alici-Evcimen Y, Breitbart WS. Ifosfamide neuropsychiatric toxicity in patients with cancer. Psychooncology. 2007;16:956–60.[↩]
- Pelgrims J, De Vos F, Van den Brande J, Schrijvers D, Prové, Vermorken JB. Methylene blue in the treatment and prevention of ifosfamide-induced encephalopathy: report of 12 cases and a review of the literature. British Journal of Cancer. 2000;82:291–4 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2363270/pdf/82-6690917a.pdf[↩]
- Gordan Donald L, Airan Mohan C, Thomas William, Seidman Leon H. Parathyroid identification by methylene blue infusion. British Journal of Surgery. 2005;62:747–9.[↩]
- Beretvas RI, Ponsky J. Endoscopic marking: an adjunct to laparoscopic gastrointestinal surgery. Surgical endoscopy. 2001;15:1202–3.[↩]
- Simmons RM, Smith SM, Osborne MP. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Breast J. 2001;7:181–3.[↩]
- Misra V, Misra SP, Dwivedi M, Gupta SC. The Loeffler’s methylene blue stain: An inexpensive and rapid method for detection of helicobacter pylori. Journal of Gastroenterology and Hepatology. 2008;9:512–3.[↩]
- Sloand EM, Kessler CM, Mcintosh CL, Klein HG. Methylene blue for neutralization of heparin. Thromb Res. 1989;54:677–86[↩]
- Steers WD, Selby JB. Use of methylene blue and selective embolization of the pudendal artery for high flow priapism refractory to medical and surgical treatments. J Urol. 1991;146:1361–3.[↩]
- Murat Oz, Lorke Dietrich E, Petroianu George A. Methylene blue and Alzheimer’s disease. Biochemical pharmacology. 2009;78:927–32[↩]
- Peter C, Hongwan D, Küpfer A, Lauterburg BH. Pharmacokinetics and organ distribution of intravenous and oral methylene blue. Eur J Clin Pharmacol. 2000 Jun;56(3):247-50. doi: 10.1007/s002280000124[↩]
- Rodriguez P, Zhou W, Barrett DW, Altmeyer W, Gutierrez JE, Li J, Lancaster JL, Gonzalez-Lima F, Duong TQ. Multimodal Randomized Functional MR Imaging of the Effects of Methylene Blue in the Human Brain. Radiology. 2016 Nov;281(2):516-526. doi: 10.1148/radiol.2016152893[↩][↩]
- Telch MJ, Bruchey AK, Rosenfield D, Cobb AR, Smits J, Pahl S, Gonzalez-Lima F. Effects of post-session administration of methylene blue on fear extinction and contextual memory in adults with claustrophobia. Am J Psychiatry. 2014 Oct;171(10):1091-8. doi: 10.1176/appi.ajp.2014.13101407[↩][↩]
- Deng Y, Wang R, Li S, Zhu X, Wang T, Wu J, Zhang J. Methylene blue reduces incidence of early postoperative cognitive disorders in elderly patients undergoing major non-cardiac surgery: An open-label randomized controlled clinical trial. J Clin Anesth. 2021 Feb;68:110108. doi: 10.1016/j.jclinane.2020.110108[↩][↩][↩]
- Baddeley TC, McCaffrey J, Storey JM, Cheung JK, Melis V, Horsley D, Harrington CR, Wischik CM. Complex disposition of methylthioninium redox forms determines efficacy in tau aggregation inhibitor therapy for Alzheimer’s disease. J Pharmacol Exp Ther. 2015 Jan;352(1):110-8. doi: 10.1124/jpet.114.219352[↩]
- Schelter BO, Shiells H, Baddeley TC, et al. Concentration-Dependent Activity of Hydromethylthionine on Cognitive Decline and Brain Atrophy in Mild to Moderate Alzheimer’s Disease. J Alzheimers Dis. 2019;72(3):931-946. doi: 10.3233/JAD-190772[↩]
- Wischik CM, Staff RT, Wischik DJ, Bentham P, Murray AD, Storey JM, Kook KA, Harrington CR. Tau aggregation inhibitor therapy: an exploratory phase 2 study in mild or moderate Alzheimer’s disease. J Alzheimers Dis. 2015;44(2):705-20. doi: 10.3233/JAD-142874[↩][↩][↩]
- Medina DX, Caccamo A, Oddo S. Methylene blue reduces aβ levels and rescues early cognitive deficit by increasing proteasome activity. Brain Pathol. 2011 Mar;21(2):140-9. doi: 10.1111/j.1750-3639.2010.00430.x[↩]
- Zakaria A, Hamdi N, Abdel-Kader RM. Methylene Blue Improves Brain Mitochondrial ABAD Functions and Decreases Aβ in a Neuroinflammatory Alzheimer’s Disease Mouse Model. Mol Neurobiol. 2016 Mar;53(2):1220-1228. doi: 10.1007/s12035-014-9088-8[↩][↩]
- Spires-Jones TL, Friedman T, Pitstick R, Polydoro M, Roe A, Carlson GA, Hyman BT. Methylene blue does not reverse existing neurofibrillary tangle pathology in the rTg4510 mouse model of tauopathy. Neurosci Lett. 2014 Mar 6;562:63-8. doi: 10.1016/j.neulet.2014.01.013[↩]
- Hochgräfe K, Sydow A, Matenia D, Cadinu D, Könen S, Petrova O, Pickhardt M, Goll P, Morellini F, Mandelkow E, Mandelkow EM. Preventive methylene blue treatment preserves cognition in mice expressing full-length pro-aggregant human Tau. Acta Neuropathol Commun. 2015 May 10;3:25. doi: 10.1186/s40478-015-0204-4[↩]
- Melis V, Magbagbeolu M, Rickard JE, Horsley D, Davidson K, Harrington KA, Goatman K, Goatman EA, Deiana S, Close SP, Zabke C, Stamer K, Dietze S, Schwab K, Storey JM, Harrington CR, Wischik CM, Theuring F, Riedel G. Effects of oxidized and reduced forms of methylthioninium in two transgenic mouse tauopathy models. Behav Pharmacol. 2015 Jun;26(4):353-68. doi: 10.1097/FBP.0000000000000133[↩]
- Schwab K, Chasapopoulou Z, Frahm S, Magbagbeolu M, Cranston A, Harrington CR, Wischik CM, Theuring F, Riedel G. Glutamatergic transmission and receptor expression in the synucleinopathy h-α-synL62 mouse model: Effects of hydromethylthionine. Cell Signal. 2022 Sep;97:110386. doi: 10.1016/j.cellsig.2022.110386[↩]
- Lim S, Shin S, Sung Y, Lee HE, Kim KH, Song JY, Lee GH, Aziz H, Lukianenko N, Kang DM, Boesen N, Jeong H, Abdildinova A, Lee J, Yu BY, Lim SM, Lee JS, Ryu H, Pae AN, Kim YK. Levosimendan inhibits disulfide tau oligomerization and ameliorates tau pathology in TauP301L-BiFC mice. Exp Mol Med. 2023 Mar;55(3):612-627. doi: 10.1038/s12276-023-00959-5[↩]
- Wischik CM, Edwards PC, Lai RY, Roth M, Harrington CR. Selective inhibition of Alzheimer disease-like tau aggregation by phenothiazines. Proc Natl Acad Sci U S A. 1996 Oct 1;93(20):11213-8. doi: 10.1073/pnas.93.20.11213[↩]
- Poteet E, Winters A, Yan LJ, Shufelt K, Green KN, Simpkins JW, Wen Y, Yang SH. Neuroprotective actions of methylene blue and its derivatives. PLoS One. 2012;7(10):e48279. doi: 10.1371/journal.pone.0048279[↩]
- Atamna H, Kumar R. Protective role of methylene blue in Alzheimer’s disease via mitochondria and cytochrome c oxidase. J Alzheimers Dis. 2010;20 Suppl 2:S439-52. doi: 10.3233/JAD-2010-100414[↩]
- Roy Choudhury G, Winters A, Rich RM, Ryou MG, Gryczynski Z, Yuan F, Yang SH, Liu R. Methylene blue protects astrocytes against glucose oxygen deprivation by improving cellular respiration. PLoS One. 2015 Apr 7;10(4):e0123096. doi: 10.1371/journal.pone.0123096[↩]
- Gauthier S, Feldman HH, Schneider LS, Wilcock GK, Frisoni GB, Hardlund JH, Moebius HJ, Bentham P, Kook KA, Wischik DJ, Schelter BO, Davis CS, Staff RT, Bracoud L, Shamsi K, Storey JM, Harrington CR, Wischik CM. Efficacy and safety of tau-aggregation inhibitor therapy in patients with mild or moderate Alzheimer’s disease: a randomised, controlled, double-blind, parallel-arm, phase 3 trial. Lancet. 2016 Dec 10;388(10062):2873-2884. doi: 10.1016/S0140-6736(16)31275-2[↩][↩][↩][↩][↩][↩][↩]
- Wilcock GK, Gauthier S, Frisoni GB, Jia J, Hardlund JH, Moebius HJ, Bentham P, Kook KA, Schelter BO, Wischik DJ, Davis CS, Staff RT, Vuksanovic V, Ahearn T, Bracoud L, Shamsi K, Marek K, Seibyl J, Riedel G, Storey JMD, Harrington CR, Wischik CM. Potential of Low Dose Leuco-Methylthioninium Bis(Hydromethanesulphonate) (LMTM) Monotherapy for Treatment of Mild Alzheimer’s Disease: Cohort Analysis as Modified Primary Outcome in a Phase III Clinical Trial. J Alzheimers Dis. 2018;61(1):435-457. doi: 10.3233/JAD-170560[↩][↩][↩][↩][↩][↩][↩][↩]
- Schneider LS, Insel PS, Weiner MW; Alzheimer’s Disease Neuroimaging Initiative. Treatment with cholinesterase inhibitors and memantine of patients in the Alzheimer’s Disease Neuroimaging Initiative. Arch Neurol. 2011 Jan;68(1):58-66. doi: 10.1001/archneurol.2010.343[↩]
- Tau Inhibitor Fails Again—Subgroup Analysis Irks Clinicians at CTAD. https://www.alzforum.org/news/conference-coverage/tau-inhibitor-fails-again-subgroup-analysis-irks-clinicians-ctad[↩]
- Schelter BO, Shiells H, Baddeley TC, Rubino CM, Ganesan H, Hammel J, Vuksanovic V, Staff RT, Murray AD, Bracoud L, Riedel G, Gauthier S, Jia J, Bentham P, Kook K, Storey JMD, Harrington CR, Wischik CM. Concentration-Dependent Activity of Hydromethylthionine on Cognitive Decline and Brain Atrophy in Mild to Moderate Alzheimer’s Disease. J Alzheimers Dis. 2019;72(3):931-946. doi: 10.3233/JAD-190772[↩][↩]
- Shiells H, Schelter BO, Bentham P, Baddeley TC, Rubino CM, Ganesan H, Hammel J, Vuksanovic V, Staff RT, Murray AD, Bracoud L, Wischik DJ, Riedel G, Gauthier S, Jia J, Moebius HJ, Hardlund J, Kipps CM, Kook K, Storey JMD, Harrington CR, Wischik CM. Concentration-Dependent Activity of Hydromethylthionine on Clinical Decline and Brain Atrophy in a Randomized Controlled Trial in Behavioral Variant Frontotemporal Dementia. J Alzheimers Dis. 2020;75(2):501-519. doi: 10.3233/JAD-191173[↩][↩][↩][↩]
- Wischik CM, Bentham P, Gauthier S, Miller S, Kook K, Schelter BO. Oral Tau Aggregation Inhibitor for Alzheimer’s Disease: Design, Progress and Basis for Selection of the 16 mg/day Dose in a Phase 3, Randomized, Placebo-Controlled Trial of Hydromethylthionine Mesylate. J Prev Alzheimers Dis. 2022;9(4):780-790. doi: 10.14283/jpad.2022.63[↩][↩]
- Odd Twist in Phase 3 Alzheimer’s Trial for Novel Tau Inhibitor. https://www.medscape.com/viewarticle/984863[↩]
- TauRx Parses Subgroups to Make the Case for Methylene Blue Derivative, Again. https://www.alzforum.org/news/conference-coverage/taurx-parses-subgroups-make-case-methylene-blue-derivative-again[↩][↩]
- Bentham P, Staff RT, Schelter BO, Shiells H, Harrington CR, Wischik CM. Long-Term Hydromethylthionine Treatment Is Associated with Delayed Clinical Onset and Slowing of Cerebral Atrophy in a Pre-Symptomatic P301S MAPT Mutation Carrier. J Alzheimers Dis. 2021;83(3):1017-1023. doi: 10.3233/JAD-210390[↩][↩]
- Zolfaghari PS, Packer S, Singer M, Nair SP, Bennett J, Street C, Wilson M. In vivo killing of Staphylococcus aureus using a light-activated antimicrobial agent. BMC Microbiol. 2009 Feb 4;9:27. doi: 10.1186/1471-2180-9-27[↩]
- Müller-Breitkreutz K, Mohr H. Hepatitis C and human immunodeficiency virus RNA degradation by methylene blue/light treatment of human plasma. J Med Virol. 1998 Nov;56(3):239-45. doi: 10.1002/(sici)1096-9071(199811)56:3<239::aid-jmv11>3.0.co;2-9[↩]
- Salah M, Samy N, Fadel M. Methylene blue mediated photodynamic therapy for resistant plaque psoriasis. J Drugs Dermatol. 2009 Jan;8(1):42-9.[↩]
- Kim S. H., Ahn S. H., Cho Y. W., Lee D. G. (2012). Effect of intradiscal methylene blue injection for the chronic discogenic low back pain: one year prospective follow-up study. Ann. Rehabil. Med. 36 657–664. 10.5535/arm.2012.36.5.657[↩]
- Maas ET, Ostelo RW, Niemisto L, Jousimaa J, Hurri H, Malmivaara A, van Tulder MW. Radiofrequency denervation for chronic low back pain. Cochrane Database Syst Rev. 2015 Oct 23;2015(10):CD008572. doi: 10.1002/14651858.CD008572.pub2[↩]
- Zhang X, Hao J, Hu Z, Yang H. Clinical Evaluation and Magnetic Resonance Imaging Assessment of Intradiscal Methylene Blue Injection for the Treatment of Discogenic Low Back Pain. Pain Physician. 2016 Nov-Dec;19(8):E1189-E1195. https://www.painphysicianjournal.com/current/pdf?article=MzExOQ%3D%3D&journal=100[↩]
- Al-Najjim M, Shah R, Rahuma M, Gabbar OA. Lumbar facet joint injection in treating low back pain: Radiofrequency denervation versus SHAM procedure. Systematic review. J Orthop. 2017 Oct 27;15(1):1-8. doi: 10.1016/j.jor.2017.10.001[↩]
- Peng B., Zhang Y., Hou S., Wu W., Fu X. (2007). Intradiscal methylene blue injection for the treatment of chronic discogenic low back pain. Eur. Spine J. 16 33–38. 10.1007/s00586-006-0076-1[↩]
- Peng B., Pang X., Wu Y., Zhao C., Song X. (2010). A randomized placebo-controlled trial of intradiscal methylene blue injection for the treatment of chronic discogenic low back pain. Pain 149 124–129. 10.1016/j.pain.2010.01.021[↩]
- Shanmugam G. Vasoplegic syndrome–the role of methylene blue. Eur J Cardiothorac Surg. 2005 Nov;28(5):705-10. doi: 10.1016/j.ejcts.2005.07.011[↩]
- Levin RL, Degrange MA, Bruno GF, Del Mazo CD, Taborda DJ, Griotti JJ, Boullon FJ. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004 Feb;77(2):496-9. doi: 10.1016/S0003-4975(03)01510-8[↩]
- Küpfer A, Aeschlimann C, Wermuth B, Cerny T. Prophylaxis and reversal of ifosfamide encephalopathy with methylene-blue. Lancet. 1994 Mar 26;343(8900):763-4. doi: 10.1016/s0140-6736(94)91839-2[↩]
- Meissner PE, Mandi G, Coulibaly B, Witte S, Tapsoba T, Mansmann U, Rengelshausen J, Schiek W, Jahn A, Walter-Sack I, Mikus G, Burhenne J, Riedel KD, Schirmer RH, Kouyaté B, Müller O. Methylene blue for malaria in Africa: results from a dose-finding study in combination with chloroquine. Malar J. 2006 Oct 8;5:84. doi: 10.1186/1475-2875-5-84[↩]
- Ertugrul Ozal, Erkan Kuralay, Vedat Yildirim, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79:1615–9.[↩]
- Martindale SJ, Stedeford JC. Neurological sequelae following methylene blue injection for parathyroidectomy. Anaesthesia. 2003 Oct;58(10):1041-2. doi: 10.1046/j.1365-2044.2003.03415_23.x[↩]
- Cragan JD. Teratogen update: methylene blue. Teratology. 1999 Jul;60(1):42-8. doi: 10.1002/(SICI)1096-9926(199907)60:1<42::AID-TERA12>3.0.CO;2-Z[↩]
- Crooks J. Haemolytic jaundice in a neonate after intra-amniotic injection of methylene blue. Arch Dis Child. 1982 Nov;57(11):872-3. https://pmc.ncbi.nlm.nih.gov/articles/instance/1628038/pdf/archdisch00752-0066.pdf[↩]
- Gillman PK. CNS toxicity involving methylene blue: the exemplar for understanding and predicting drug interactions that precipitate serotonin toxicity. J Psychopharmacol. 2011 Mar;25(3):429-36. doi: 10.1177/0269881109359098[↩]
- Pascale Dewachter, Claudie Moutan-Faivre, Philippe Trechot, Jean-Claude Lleu, Paul Michel Mertes. Severe anaphylactic shock with methylene blue instillation. Anesth Analg. 2005;101:149–50. doi: 10.1213/01.ANE.0000153497.60047.80[↩]
- Ginimuge PR, Jyothi SD. Methylene Blue: Revisited. Journal of Anaesthesiology, Clinical Pharmacology. 2010;26(4):517-520. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3087269/[↩][↩]
- Ertugrul Ozal, Erkan Kuralay, Vedat Yildirim, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005;79:1615–9. doi: 10.1016/j.athoracsur.2004.10.038[↩]
- Salhab M, Al sarakbi W, Mokbel K. Skin and fat necrosis of the breast following methylene blue dye injection for sentinel node biopsy in a patient with breast cancer. Int Semin Surg Oncol. 2005;2:26. doi: 10.1186/1477-7800-2-26[↩]
- Crooks J. Haemolytic jaundice in a neonate after intra-amniotic injection of methylene blue. Arch Dis Child. 1982;57:872–3. doi: 10.1136/adc.57.11.872[↩]
- Fish WH, Chazen EM. Toxic effects of methylene blue on the fetus. Am J Dis Child. 1992;146:1412–3. doi: 10.1001/archpedi.1992.02160240022004[↩]
- Cowett RM, Hakanson DO, Kocon RW, Oh W. Untoward neonatal effect of intraamniotic administration of methylene blue. Obstet Gynecol. 1976 Jul;48(1 Suppl):74S-75S.[↩]
- Serota FT, Bernbaum JC, Schwartz E. The methylene-blue baby. Lancet. 1979;2:1142–3. doi: 10.1016/s0140-6736(79)92548-0[↩]
- Spahr RC, Salsburey DJ, Krissberg A, Prin W. Intraamniotic injection of methylene blue leading to methemoglobinemia in one of twins. Int J Gynaecol Obstet. 1980;17:477–8. doi: 10.1002/j.1879-3479.1980.tb00192.x[↩]
- Vincer MJ, Allen AC, Evans JR, Nwaesei C, Stinson DA. Methylene-blue-induced hemolytic anemia in a neonate. CMAJ. 1987 Mar 1;136(5):503-4. https://pmc.ncbi.nlm.nih.gov/articles/instance/1491649/pdf/cmaj00137-0049.pdf[↩]
- Troche BI. The methylene blue baby. N Engl J Med. 1989 Jun 29;320(26):1756-7.[↩]
- Plukett GD. Neonatal complications. Obstet Gynecol. 1973 Mar;41(3):476-7.[↩]
- Gillman P K. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia. 2006;61:1013–4. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1365-2044.2006.04808.x[↩]
- Pascale Dewachter, Claudie Moutan-Faivre, Philippe Trechot, Jean-Claude Lleu, Paul Michel Mertes. Severe anaphylactic shock with methylene blue instillation. Anesth Analg. 2005;101:149–50. https://www.ncbi.nlm.nih.gov/pubmed/15976222[↩]
- Serotonin syndrome. https://medlineplus.gov/ency/article/007272.htm[↩]