Contents
What is a mini stroke
A “mini stroke” or transient ischemic attack (TIA) is caused by a temporary disruption in the blood supply to part of the brain.
The disruption in blood supply results in a lack of oxygen to the brain. This can cause sudden symptoms similar to a stroke, such as speech and visual disturbance, and numbness or weakness in the face, arms and legs.
However, a TIA doesn’t last as long as a stroke. The effects often only last for a few minutes or hours and fully resolve within 24 hours.
In the early stages of a TIA, it’s not possible to tell whether you’re having a TIA or a full stroke, so it’s important to call your local emergency number immediately and ask for an ambulance.
Even if the symptoms disappear while you’re waiting for the ambulance to arrive, an assessment in hospital should still be carried out.
- A TIA is a warning that you may be at risk of having a full stroke in the near future and an assessment can help doctors to determine the best way to reduce the chances of this happening.
- About 1 in 3 people who has a TIA goes on to experience a subsequent stroke. The risk of stroke is especially high within 48 hours after a TIA.
If you think you may have had a TIA previously, but the symptoms have passed and you didn’t seek medical advice at the time, make an urgent appointment with your doctor. They can determine whether to refer you for a hospital assessment.
Who’s most at risk of mini stroke?
Certain things can increase your chances of having a TIA. Some of these factors are changeable – such as your lifestyle.
Some of the main risk factors for TIA are:
- Age – although TIAs can occur at any age (including in children and young adults), they’re most common in people over 60
- Ethnicity – people of south Asian, African or Caribbean descent have a higher TIA risk, partly because rates of high blood pressure are higher in these groups
- Medical history – other health conditions such as diabetes can increase your risk of a TIA
- Weight and diet – your risk of having a TIA is higher if you’re overweight and/or have an unhealthy diet high in fat and salt
- Smoking and alcohol – smoking and/or regularly drinking excessive amounts of alcohol can increase your TIA risk
Tackling the things you can change will help to lower your risk of having a TIA, or reduce your chances or having a full stroke in the future.
 TIA vs Stroke
TIA vs Stroke
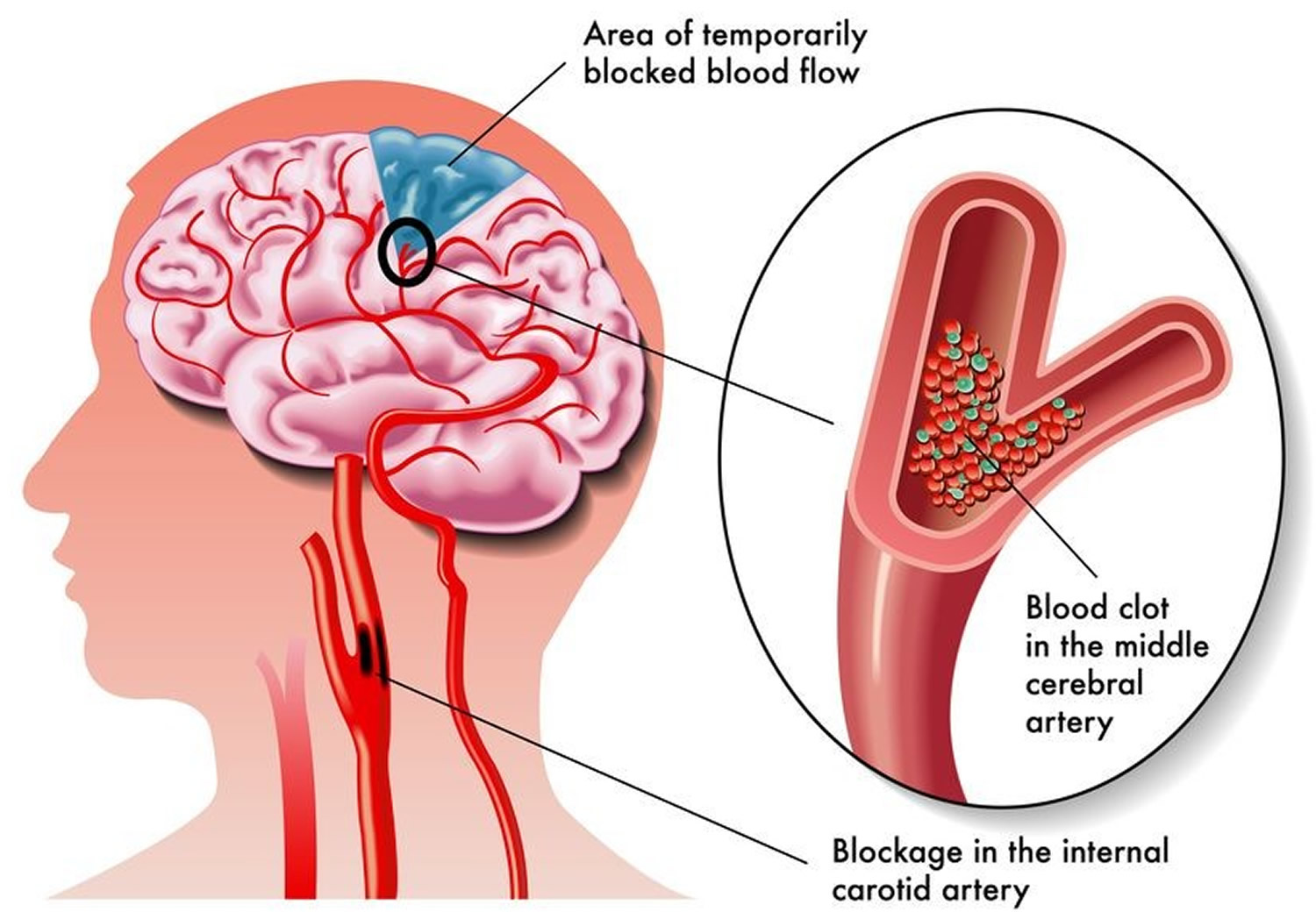
Transient ischemic attacks (TIAs) occur when one of the blood vessels that supply your brain with oxygen-rich blood becomes blocked.
This interruption in the flow of blood to the brain means it can’t carry out some of its normal functions properly, leading to symptoms such as slurred speech and weakness.
In TIAs, the blockage quickly resolves (transient or brief) and your brain’s blood supply returns to normal before there’s any significant damage. The TIA effects often only last for a few minutes or hours and fully resolve within 24 hours.
- A transient ischemic attack (TIA) can serve as both a warning and an opportunity — a warning of an impending stroke and an opportunity to take steps to prevent it. About 1 in 3 people who has a TIA goes on to experience a subsequent stroke. The risk of stroke is especially high within 48 hours after a TIA.
On the other hand, in a full stroke, the blood flow to your brain is disrupted for much longer, leading to more severe damage to the brain and longer-term problems.
- A stroke is a serious life-threatening medical condition.
- Strokes are a medical emergency and urgent treatment is essential.
- The sooner a person receives treatment for a stroke, the less damage is likely to happen.
Mini stroke side effects
A TIA is a temporary interruption of blood flow to part of the brain, spinal cord or retina, which may cause stroke-like symptoms but does not damage brain cells or cause permanent disability.
TIAs are often an early warning sign that a person is at risk of stroke.
- About 1 in 3 people who has a TIA goes on to experience a subsequent stroke. The risk of stroke is especially high within 48 hours after a TIA.
The symptoms of a TIA are similar to those of a stroke and include:
- Numbness or muscle weakness, usually on one side of the body
- Difficulty speaking or understanding speech
- Dizziness or loss of balance
- Double vision or difficulty seeing in one or both eyes
Symptoms of TIA usually last only a few minutes but may persist for up to 24 hours. Since the immediate signs and symptoms of TIA and stroke are identical, it’s important to seek medical attention.
You may need various diagnostic tests, such as a magnetic resonance imaging (MRI) scan or a computerized tomography (CT) scan, to help determine what caused the TIA.
Depending on the underlying cause, you may need medication to prevent blood clots or a procedure to remove fatty deposits (plaques) from the arteries that supply blood to your brain (carotid endarterectomy).
Mini stroke causes
During a TIA (transient ischemic attack), one of the blood vessels that supply your brain with oxygen-rich blood becomes blocked.
This blockage is usually caused by a blood clot that has formed elsewhere in your body and traveled to the blood vessels supplying the brain, although it can also be caused by pieces of fatty material or air bubbles.
This interruption in the flow of blood to the brain means it can’t carry out some of its normal functions properly, leading to symptoms such as slurred speech and weakness.
In TIAs, the blockage quickly resolves and your brain’s blood supply returns to normal before there’s any significant damage. In a full stroke, the blood flow to your brain is disrupted for much longer, leading to more severe damage to the brain and longer-term problems.
The blockage in the blood vessels responsible for most TIAs is usually caused by a blood clot that’s formed elsewhere in your body and traveled to the blood vessels supplying the brain. It can also be caused by pieces of fatty material or air bubbles.
In very rare cases, TIAs can be caused by a small amount of bleeding in the brain known as a hemorrhage.
Risk factors for mini stroke or TIA
Blood clots that cause TIAs may form in areas where arteries have been narrowed or blocked over time by the build-up of fatty deposits known as plaques. These plaques are formed during a process called atherosclerosis.
As you get older, the arteries can become narrower naturally, but certain things can dangerously accelerate the process. These include:
- Smoking
- Having high blood pressure (hypertension)
- Being obese
- Having high cholesterol levels
- Regularly drinking an excessive amount of alcohol
- Having atrial fibrillation (a type of irregular heartbeat)
- Having diabetes
- Family history. Your risk may be greater if one of your family members has had a TIA or a stroke.
- Age. Your risk increases as you get older, especially after age 55.
- Sex. Men have a slightly higher likelihood of a TIA and a stroke, but more than half of deaths from strokes occur in women.
- Prior transient ischemic attack. If you’ve had one or more TIAs, you’re 10 times more likely to have a stroke.
- Sickle cell disease. Also called sickle cell anemia, a stroke is a frequent complication of this inherited disorder. Sickle-shaped blood cells carry less oxygen and also tend to get stuck in artery walls, hampering blood flow to the brain. However, with proper treatment for sickle cell disease, you can lower your risk of a stroke.
- Race. Blacks are at greater risk of dying of a stroke, partly because of the higher prevalence of high blood pressure and diabetes among blacks.
People over 60 years of age, and people of Asian, African or Caribbean descent are also at a higher risk of having a TIA.
A type of irregular heartbeat called atrial fibrillation can also cause mini strokes. It can lead to the formation of blood clots that escape from the heart and become lodged in the blood vessels supplying the brain.
Risk factors you can take steps to control
You can control or treat a number of factors — including certain health conditions and lifestyle choices — that increase your risk of a stroke. Having one or more of these risk factors doesn’t mean you’ll have a stroke, but your risk particularly increases if you have two or more of them.
Health conditions
- High blood pressure. The risk of a stroke begins to increase at blood pressure readings higher than 140/90 millimeters of mercury (mm Hg). Your doctor will help you decide on a target blood pressure based on your age, whether you have diabetes and other factors.
- High cholesterol. Eating less cholesterol and fat, especially saturated fat and trans fat, may reduce the plaques in your arteries. If you can’t control your cholesterol through dietary changes alone, your doctor may prescribe a statin or another type of cholesterol-lowering medication.
- Cardiovascular disease. This includes heart failure, a heart defect, a heart infection or an abnormal heart rhythm.
- Carotid artery disease. The blood vessels in your neck that lead to your brain become clogged.
- Peripheral artery disease (PAD). The blood vessels that carry blood to your arms and legs become clogged.
- Diabetes. Diabetes increases the severity of atherosclerosis — narrowing of the arteries due to accumulation of fatty deposits — and the speed with which it develops.
- High levels of homocysteine. Elevated levels of this amino acid in your blood can cause your arteries to thicken and scar, which makes them more susceptible to clots.
- Excess weight. A body mass index of 25 or higher and a waist circumference greater than 35 inches (89 centimeters) in women or 40 inches (102 centimeters) in men increase risk.
Lifestyle choices
- Cigarette smoking. Smoking increases your risk of blood clots, raises your blood pressure and contributes to the development of cholesterol-containing fatty deposits in your arteries (atherosclerosis).
- Physical inactivity. Engaging in 30 minutes of moderate-intensity exercise most days helps reduce risk.
- Poor nutrition. Eating too much fat and salt, in particular, increases your risk of a TIA and a stroke.
- Heavy drinking. If you drink alcohol, limit yourself to no more than two drinks daily if you’re a man and one drink daily if you’re a woman.
- Use of illicit drugs. Avoid cocaine and other illicit drugs.
- Use of birth control pills. All oral contraceptives increase your risk of a stroke but taking certain ones may be more risky than others. If you’re using birth control pills, talk to your doctor about how the hormones may affect your risk of a TIA and a stroke.
Mini stroke prevention
A TIA is often a sign that another one may follow and you’re at a high risk of having a full, life-threatening stroke in the near future.
Regardless of whether you’ve had a TIA or stroke in the past, there are a number of ways you can lower your risk of having either in the future. These include:
- Maintaining a healthy weight. Being overweight contributes to other risk factors, such as high blood pressure, cardiovascular disease and diabetes. Losing weight with diet and exercise may lower your blood pressure and improve your cholesterol levels.
- Eating healthily. Eat plenty of fruits and vegetables. These foods contain nutrients such as potassium, folate and antioxidants, which may protect against a TIA or a stroke.
- Exercise regularly. If you have high blood pressure, regular exercise is one of the few ways you can lower your blood pressure without drugs.
- Limit alcohol intake. Drink alcohol in moderation, if at all. The recommended limit is no more than one drink daily for women and two a day for men.
- Don’t smoke. Stopping smoking reduces your risk of a TIA or a stroke.
- Limit cholesterol and fat. Cutting back on cholesterol and fat, especially saturated fat and trans fat, in your diet may reduce buildup of plaques in your arteries.
- Limit sodium. If you have high blood pressure, avoiding salty foods and not adding salt to food may reduce your blood pressure. Avoiding salt may not prevent hypertension, but excess sodium may increase blood pressure in people who are sensitive to sodium.
- Don’t use illicit drugs. Drugs such as cocaine are associated with an increased risk of a TIA or a stroke.
- Control diabetes. You can manage diabetes and high blood pressure with diet, exercise, weight control and, when necessary, medication.
These lifestyle changes can reduce your risk of problems such as atherosclerosis (where arteries become clogged up by fatty substances), high blood pressure and high cholesterol levels, all of which can lead to TIAs.
If you’ve already had a TIA, making these changes can help reduce your risk of having a full stroke or another TIA in the future.
Healthy Diet
An unhealthy diet can increase your chances of having a TIA or stroke because it may raise your blood pressure and cholesterol levels.
A low-fat, high-fiber diet is usually recommended, including plenty of fresh fruit and vegetables (5 portions a day) and wholegrains.
Making sure you have a balanced diet is important. Don’t eat too much of any single food, particularly processed foods and foods high in salt.
You should limit the amount of salt you eat to no more than 1.5-2.3 g (1500 – 2300 mg) a day because too much salt will increase your blood pressure – 2.3 g of salt is about 1 teaspoonful.
Exercise
Combining a healthy diet with regular exercise is the best way to maintain a healthy weight.
Regular exercise can also help lower your cholesterol level and keep your blood pressure at a healthy level.
For most people, at least 150 minutes (2 hours and 30 minutes) of moderate-intensity aerobic activity, such as cycling or fast walking, every week is recommended.
Stop smoking
Smoking significantly increases your risk of having a TIA or stroke. This is because it narrows your arteries and makes your blood more likely to clot.
If you stop smoking, you can reduce your risk of having a TIA or stroke.
Not smoking will also improve your general health and reduce your risk of developing other serious conditions, such as lung cancer and heart disease.
Cut down on alcohol
Excessive alcohol consumption can lead to weight gain and high blood pressure, and trigger an irregular heartbeat (atrial fibrillation), all of which can increase your risk of having a TIA or stroke.
To keep health risks from alcohol to a low level if you drink most weeks:
- men and women are advised not to drink more than 14 units a week on a regular basis
- spread your drinking over 3 or more days if you regularly drink as much as 14 units a week
- if you want to cut down, try to have several drink-free days each week
Fourteen units is equivalent to 6 pints of average-strength beer or 10 small glasses of low-strength wine.
Managing underlying conditions
If you’ve been diagnosed with a condition that’s known to increase your risk of TIAs and strokes – such as high cholesterol, high blood pressure, atrial fibrillation or diabetes – making sure the condition is well controlled is also important.
These lifestyle changes can help control these conditions to a large degree, but you may also need to take regular medication.
Mini stroke signs and symptoms
The symptoms of a transient ischemic attack (TIA) are the same as those of a stroke, but they only last for a few minutes or hours.
Like a stroke, the signs and symptoms of a mini-stroke or TIA usually begin suddenly.
Most signs and symptoms of TIA disappear within an hour. The signs and symptoms of a TIA resemble those found early in a stroke.
The main TIA stroke symptoms can be remembered with the word FAST: Face-Arms-Speech-Time.
- Face – the face may have dropped on one side, the person may not be able to smile, or their mouth or eye may have dropped.
- Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of arm weakness or numbness in one arm.
- Speech – their speech may be slurred or garbled or difficulty understanding others or the person may not be able to talk at all, despite appearing to be awake.
- Time – it is time to dial your local emergency immediately if you see any of these signs or symptoms.
It’s important for everyone to be aware of these signs and symptoms.
If you live with or care for somebody in a high-risk group, such as an elderly person or someone with diabetes or high blood pressure, being aware of the symptoms is even more important.
- Seek immediate medical attention if you suspect you’ve had a transient ischemic attack (TIA). Prompt evaluation and identification of potentially treatable conditions may help you prevent a stroke.
Other possible symptoms
Symptoms in the FAST test identify most strokes and TIAs, but they can occasionally cause different symptoms that typically appear suddenly (usually over a few seconds).
Other signs and symptoms may include:
- complete paralysis of one side of the body
- sudden loss or blurring of vision
- blindness in one or both eyes or double vision
- sudden, severe headache with no known cause
- dizziness or loss of balance or coordination
- confusion
- difficulty understanding what others are saying
- problems with balance and co-ordination
- difficulty swallowing (dysphagia)
However, there may be other causes for these symptoms.
Mini stroke diagnosis
It’s important to be assessed by a healthcare professional as soon as possible if you think you’ve had a transient ischaemic attack (TIA).
After an initial assessment, you may be referred to a specialist for further tests to help determine the cause of the TIA.
A TIA is a warning sign that you’re at risk of having a full stroke in the near future. A detailed assessment can help your doctor decide the best way to reduce this risk.
Initial assessment
TIAs are often over very quickly, so you may not have any symptoms by the time you see a doctor.
You’ll be asked about the symptoms you experienced during the TIA and how long they lasted. This will help to rule out other conditions that may have caused your symptoms.
Even if you no longer have symptoms, a neurological examination may still be needed. This involves simple tasks designed to check your strength, sensation and co-ordination skills.
Referral to a specialist
If a TIA is suspected, you’ll be referred to a specialist for further tests. People at a lower risk should be seen within seven days.
You’ll normally be offered aspirin to take while you’re waiting for specialist assessment, as this can help to reduce your risk of having a stroke or another TIA in the meantime.
You’ll usually be referred to a neurologist (a doctor who specialises in conditions that affect the brain and spine), or a consultant who specialises in strokes. This may be in a specialist stroke or TIA clinic, or on an acute stroke unit.
Mini Stroke Tests
Several tests may be carried out to confirm a TIA and look for underlying problems that may have caused it. Some of these tests include:
Blood pressure tests
Your blood pressure will be checked, because high blood pressure (hypertension) can lead to TIAs.
Blood tests
You might need blood tests to determine whether you have high cholesterol, and to check if you have diabetes.
Electrocardiogram (ECG)
An electrocardiogram (ECG) measures your heart’s electrical activity using a number of electrodes (small, sticky patches) attached to your skin.
An ECG can detect abnormal heart rhythms, which may be a sign of conditions such as atrial fibrillation (where your heart beats irregularly), which can increase your risk of TIAs.
Carotid ultrasound
A carotid ultrasound scan can show if there is narrowing or any blockages in the neck arteries leading to your brain.
A small probe (transducer) sends high-frequency sound waves into your body. When these sound waves bounce back, they can be used to create an image of the inside of your body.
Brain scans
Brain scans aren’t always necessary if you’ve had a TIA. They’re normally only carried out if it’s not clear which part of your brain was affected.
A magnetic resonance imaging (MRI) scan is most often carried out in these cases. This type of scan uses a strong magnetic field and radio waves to create an image of your brain.
Magnetic resonance angiography (MRA). This is a method of evaluating the arteries in your neck and brain. It uses a strong magnetic field similar to an MRI.
Occasionally, a computerised tomography (CT) scan may be used if an MRI scan isn’t suitable for you. This type of scan uses a series of X-rays to produce an image of the inside of brain.
Echocardiography
Your doctor may choose to perform a transthoracic echocardiogram (TTE) or transesophageal echocardiogram (TEE). A transthoracic echocardiogram (TTE) involves moving an instrument called a transducer across your chest. The transducer emits sound waves that echo off of different parts of your heart, creating an ultrasound image.
During a transesophageal echocardiogram (TEE), a flexible probe with a transducer built into it is placed in your esophagus — the tube that connects the back of your mouth to your stomach. Because your esophagus is directly behind your heart, clearer, detailed ultrasound images can be created. This allows a better view of some things, such as blood clots, that might not be seen clearly in a traditional echocardiography exam.
Arteriography
This procedure gives a view of arteries in your brain not normally seen in X-ray imaging. A radiologist inserts a thin, flexible tube (catheter) through a small incision, usually in your groin.
The catheter is manipulated through your major arteries and into your carotid or vertebral artery. Then the radiologist injects a dye through the catheter to provide X-ray images of the arteries in your brain. This procedure may be used in selected cases.
Mini stroke treatment
Although the symptoms of a TIA resolve in a few minutes or hours, you’ll need treatment to help prevent another TIA or a full stroke happening in the future.
A TIA is a warning sign that you’re at a significantly increased risk of having a full stroke in the near future. The highest risk is in the days and weeks following the attack.
A stroke is a serious health condition that can cause permanent disability and can be fatal in some cases, but appropriate treatment following a TIA can help to reduce your risk of having one.
Your treatment will depend on your individual circumstances, such as your age and medical history.
You’re likely to be given advice about lifestyle changes you can make to reduce your stroke risk, in addition to being offered medication to treat the underlying cause of your TIA.
In some cases, surgery may be needed to unblock the carotid arteries (the main blood vessels that supply the brain with blood).
Lifestyle changes
There are a number of lifestyle changes you can make that may help reduce your chances of having a stroke after a TIA.
These include:
- eating a healthy diet – a low-fat, reduced salt, high-fibre diet is usually recommended, including plenty of fresh fruit and vegetables
- exercising regularly – for most people, at least 150 minutes of moderate-intensity aerobic activity, such as cycling or fast walking, every week is recommended
- quitting smoking – if you smoke, stopping may significantly reduce your risk of having a stroke in the future
- cutting down on alcohol – you should aim not to exceed the recommended alcohol limits of three to four units a day for men and two to three units a day for women
Driving after a TIA
Although a TIA shouldn’t have any long-term impact on your daily activities, you must stop driving immediately.
If your doctor is happy that you have made a good recovery and there are no lasting effects after one month, you can start driving again.
Medication
In addition to lifestyle changes, most people who have had a TIA will need to take one or more daily medications indefinitely to help reduce their chances of having a stroke or another TIA.
Some of the main medications used include:
Antiplatelets
Platelets are blood cells that help blood to clot (thicken). If a blood vessel is damaged, platelets stick together to form a blood clot to prevent bleeding.
Antiplatelet medicines work by reducing the ability of the platelets to stick together and form clots. If you’ve had a TIA, it’s likely that you’ll be offered antiplatelet medication.
Two common antiplatelets offered to people who have had a TIA are aspirin and clopidogrel. Aspirin may also sometimes be taken with another antiplatelet medicine called dipyridamole because this can be more effective than taking these medications separately.
The main side effects of antiplatelet medications include indigestion and an increased risk of bleeding – for example, you may bleed for longer if you cut yourself, and you may bruise easily.
Anticoagulants
Anticoagulant medicines can help to prevent blood clots by changing the chemical composition of the blood in a way that prevents clots.
They’re usually offered to people who have had a TIA if the blood clot that caused your TIA originated in your heart. This is often due to a condition called atrial fibrillation, which causes your heart to beat irregularly.
Warfarin, apixaban, dabigatran, edoxaban and rivaroxaban are examples of anticoagulants offered to some people who have had a TIA.
A side effect of all anticoagulants is the risk of bleeding caused by the reduction in the blood’s ability to clot. You may need regular blood tests while taking warfarin, so doctors can ensure your dose is not too high or too low.
Antihypertensives (blood pressure medication)
If you have high blood pressure (hypertension), you’ll be offered a type of medication called an antihypertensive to control it. This is because high blood pressure significantly increases your risk of having a TIA or stroke.
There are lots of different types of medicine that can help control your blood pressure, including:
- thiazide diuretics (water pills)
- angiotensin-converting enzyme (ACE) inhibitors
- calcium channel blockers
- beta-blockers
Your doctor will advise you about which antihypertensive is the most suitable for you. Some people may be offered a combination of two or more different medications.
Statins
If you have high cholesterol, you’ll be advised to take a medicine known as a statin. Statins reduce the level of cholesterol in your blood by blocking an enzyme in the liver that produces cholesterol.
Statins may also help to reduce your risk of a stroke whatever your cholesterol level is. You may be offered a statin even if your cholesterol level is not particularly high.
Examples of statins often offered to people who have had a TIA include atorvastatin, simvastatin and rosuvastatin.
Surgery
In some cases, a surgical procedure called a carotid endarterectomy may be recommended after having a TIA.
Carotid endarterectomy
A carotid endarterectomy is an operation that involves removing part of the lining of the carotid artery, plus any blockage that has built up in the artery.
A carotid endarterectomy may be needed if one or both of your carotid arteries become narrowed because of a build-up of fatty deposits (plaque). This is known as carotid artery disease or carotid artery stenosis, and it significantly increases your risk of having a stroke or a transient ischemic attack (TIA).
The carotid arteries deliver blood to your brain. When fatty deposits build up inside the carotid arteries, they become hard and narrow, making it more difficult for blood to flow through them.
This is known as atherosclerosis and it can lead to TIAs and strokes if the blood supply to the brain becomes disrupted.
By unblocking the carotid arteries in people whose arteries are moderately or severely narrowed, a carotid endarterectomy can significantly reduce the risk of having a stroke or another TIA.
Carotid endarterectomy can be carried out using either local anesthetic or general anesthetic. The advantage of local anesthetic is it allows the surgeon to monitor brain function while you’re awake. However, there’s no evidence that either is safer or better.
During the procedure, a 7-10cm (2.5-4 inch) cut will be made between the corner of your jaw and your breastbone. A small cut is then made along the narrowed section of artery, and the fatty deposits that have built up are removed.
The artery is then closed with stitches or a patch and your skin is also closed with stitches.
Most people are well enough to go home within about 48 hours of the procedure.
In most cases, the only problems experienced after the operation are temporary numbness or discomfort in the neck.
However, there’s a small risk of more serious complications, which can include stroke or death in around 3% of cases. Nevertheless, this risk is much lower than in people with carotid artery disease who haven’t chosen to have the operation.
Are there any alternatives?
Carotid endarterectomy is the main treatment for narrowing of the carotid arteries, but sometimes an alternative procedure called carotid artery stent placement may be available.
This is a less invasive procedure than a carotid endarterectomy because it doesn’t involve a cut being made in the neck. Instead, a thin flexible tube is guided to the carotid artery through a small cut in the groin. A mesh cylinder (stent) is then placed into the narrowed section of artery to widen it and allow blood to flow through it more easily.
- Carotid stenting is currently thought to be associated with a higher risk of stroke during the procedure, especially if it’s performed in the first few days after symptoms appear. However, it’s a useful alternative for people who may be at a higher risk of complications from an operation.
Carotid artery stenting is carried out under local anesthetic and involves a narrow flexible tube called a catheter being inserted into an artery in your groin. It’s then threaded up into the carotid artery using X-rays to guide it into place.
A small balloon at the end of the catheter is inflated to around 5mm at the site of the narrowed artery, and a small mesh cylinder called a stent is then inserted. The balloon will be deflated and removed, leaving the stent in place to keep the artery open and allow blood to flow through it.
After the procedure, you’ll need to lie flat and keep still for about an hour to prevent any bleeding from the artery. You’ll need to stay in hospital overnight, but will be able to return home the next day.
Like carotid endarterectomy, there are some risks associated with stenting. The risk of having another stroke or dying is slightly higher than after carotid endarterectomy, especially when the procedure is performed soon after symptoms appear. But the long-term outcomes from a successful procedure are no different from a carotid endarterectomy.
The decision about which procedure you’ll have will be made based on your own personal wishes, your overall fitness, and an assessment of your clinical history. One major factor is how long it’s been since your most recent symptom.
The National Institute for Health and Care Excellence 1 has confirmed carotid artery stenting is a safe procedure and has good short-term results.
Evidence suggests a successful stent procedure has the same long-term risks of a stroke as carotid endarterectomy.
NICE advises that, provided the risks of carotid artery stenting are judged similar to those after surgery, it’s safe to offer this alternative.
- Carotid artery stent placement for symptomatic extracranial carotid stenosis. https://www.nice.org.uk/guidance/ipg389/informationforpublic[↩]