Contents
What is multiple sclerosis
Multiple sclerosis (MS) is chronic progressive destruction of myelin sheaths surrounding neurons that affects the central nervous system (CNS) – your brain and spinal cord 1. Multiple sclerosis (MS) damages the myelin sheath, the material that surrounds and protects your nerve cells.
In multiple sclerosis, the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body 2. Such attacks may be linked to an unknown environmental trigger, perhaps a virus. Eventually, the disease can cause the nerves themselves to deteriorate or become permanently damaged.
There’s no cure for multiple sclerosis. However, treatments can help speed recovery from attacks, modify the course of the disease and manage symptoms.
The prevalence of MS varies by geographic region, ranging from 110 cases per 100,000 persons in the northern United States to 47 per 100,000 in the southern United States 3. Women, smokers, and persons residing at higher latitudes or with a family history of multiple sclerosis are at increased risk of disease. Those with increased exposure to sunlight and higher 25-hydroxyvitamin D levels are at decreased risk 4. Total costs associated with multiple sclerosis may exceed $50,000 per person annually 5.
This damage slows down or blocks messages between your brain and your body, leading to the symptoms of multiple sclerosis. They can include:
- Visual disturbances
- Muscle weakness
- Trouble with coordination and balance
- Sensations such as numbness, prickling, or “pins and needles”
- Thinking and memory problems.
Multiple sclerosis (MS) symptoms can range from relatively benign to somewhat disabling to devastating, as communication between the brain and other parts of the body is disrupted.
Multiple sclerosis life expectancy
It is generally very difficult to predict the course of multiple sclerosis. The condition varies greatly in each individual but most people with multiple sclerosis can expect 95% of the normal life expectancy 6.
Some studies have shown that people who have few attacks in the first several years after diagnosis; long intervals between attacks; complete recovery from attacks and attacks that are sensory in nature (i.e. numbness or tingling) tend to have better outcomes in the long run.
People who have early symptoms of tremor, difficulty in walking, or who have frequent attacks with incomplete recoveries tend to have a more progressive disease course.
Types of Multiple Sclerosis
The most common form of multiple sclerosis is known as relapsing-remitting MS ~ 90 percent of cases. When people who have this kind of MS have flare-ups, the symptoms become noticeably worse. Then there is a period of recovery, when symptoms get better or disappear completely for some time. In relapsing-remitting MS, symptom flare-ups may be triggered by an infection, such as the flu. More than 50% of people who have relapsing-remitting MS develop the secondary progressive type in which there are relapses followed by a gradual worsening of the disease. About 15% to 20% of people who have MS have a form known as primary-progressive MS. In primary-progressive MS, the disease gets steadily worse, without any remissions. A fourth type—progressive relapsing MS—is rare, but the pattern follows a worsening of the disease with sudden, clear relapses. Often MS is mild, but some people lose the ability to write, speak or walk.
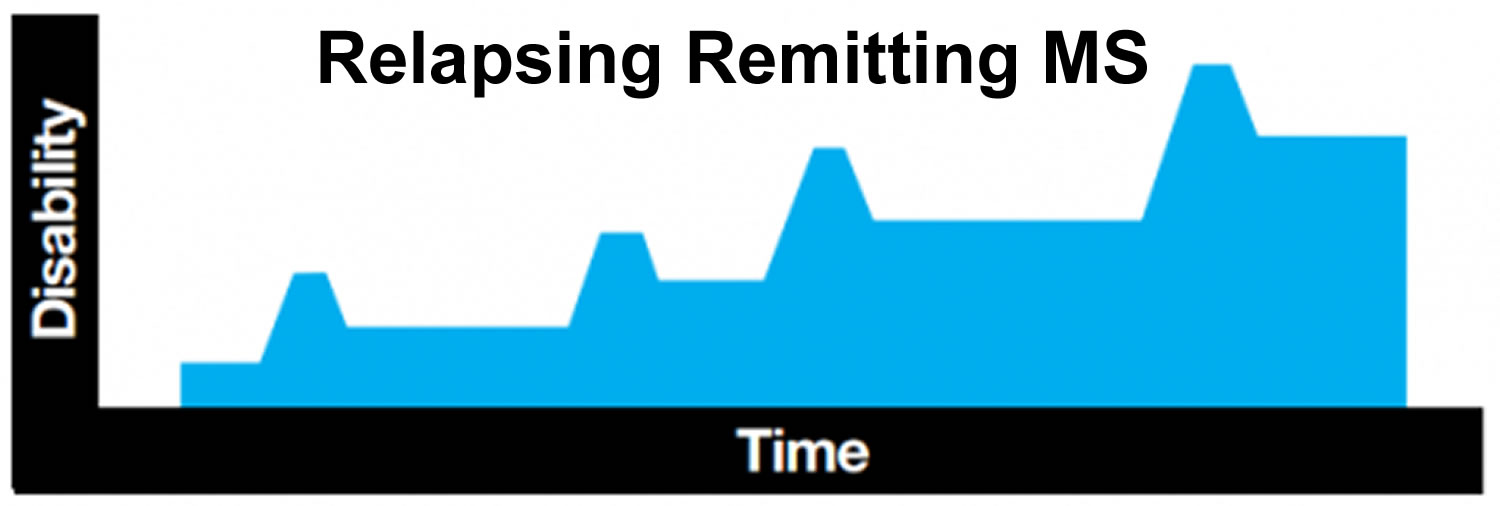
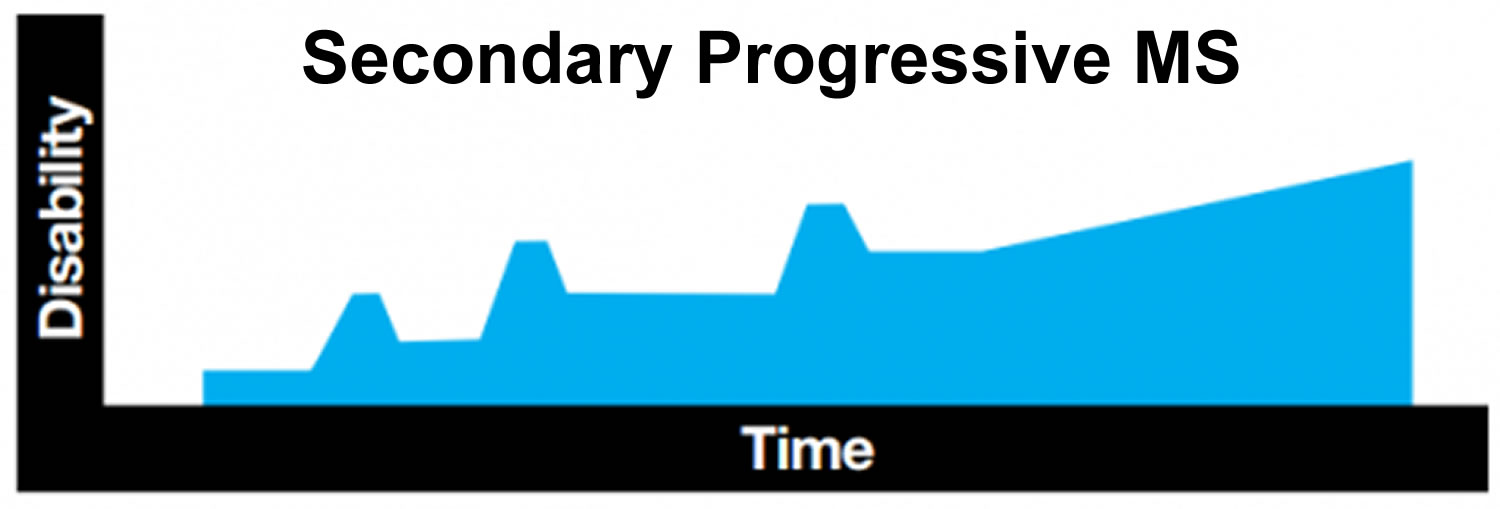
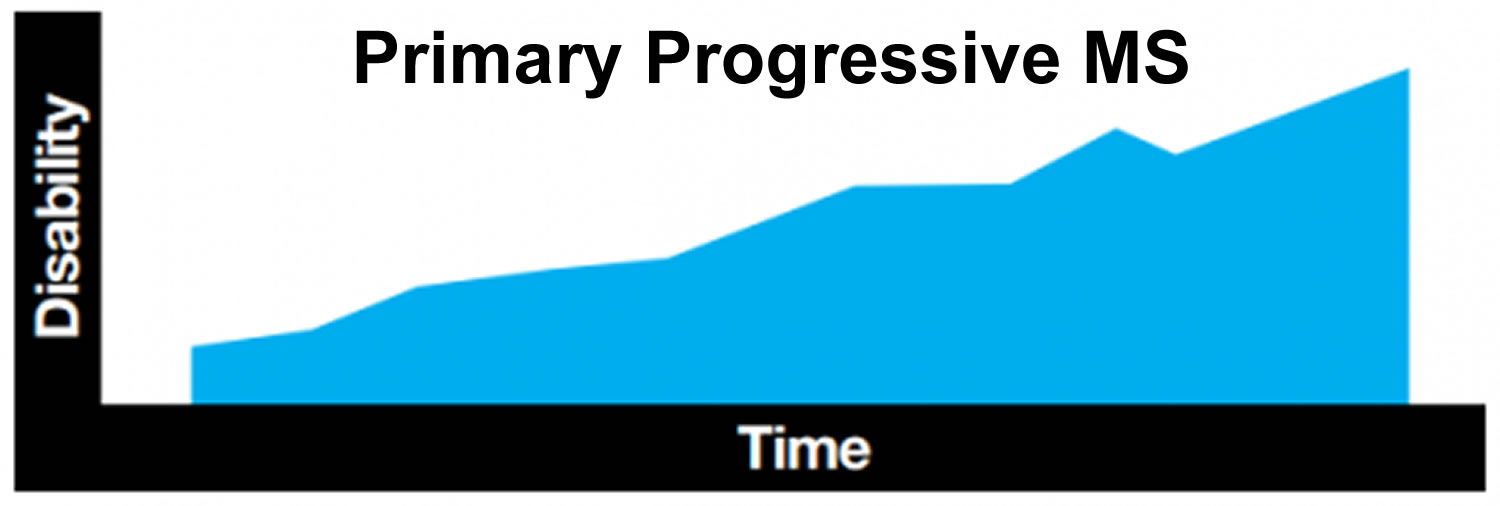
Table 1. Types of Multiple Sclerosis
| Type | Disease course |
|---|---|
Relapsing remitting (90% of cases) | Discrete attacks that evolve over days to weeks, followed by some degree of recovery over weeks to months; the patient has no worsening of neurologic function between attacks |
Secondary progressive* | Initial relapsing remitting disease, followed by gradual neurologic deterioration not associated with acute attacks |
Primary progressive and progressive relapsing (10% of cases) | Characterized by steady functional decline from disease onset; these types cannot be distinguished during early stages until attacks occur (progressive relapsing) or fail to occur (primary progressive); progressive relapsing is rarer than primary progressive |
*—Develops in about 50% of patients with relapsing remitting multiple sclerosis.
The nervous system
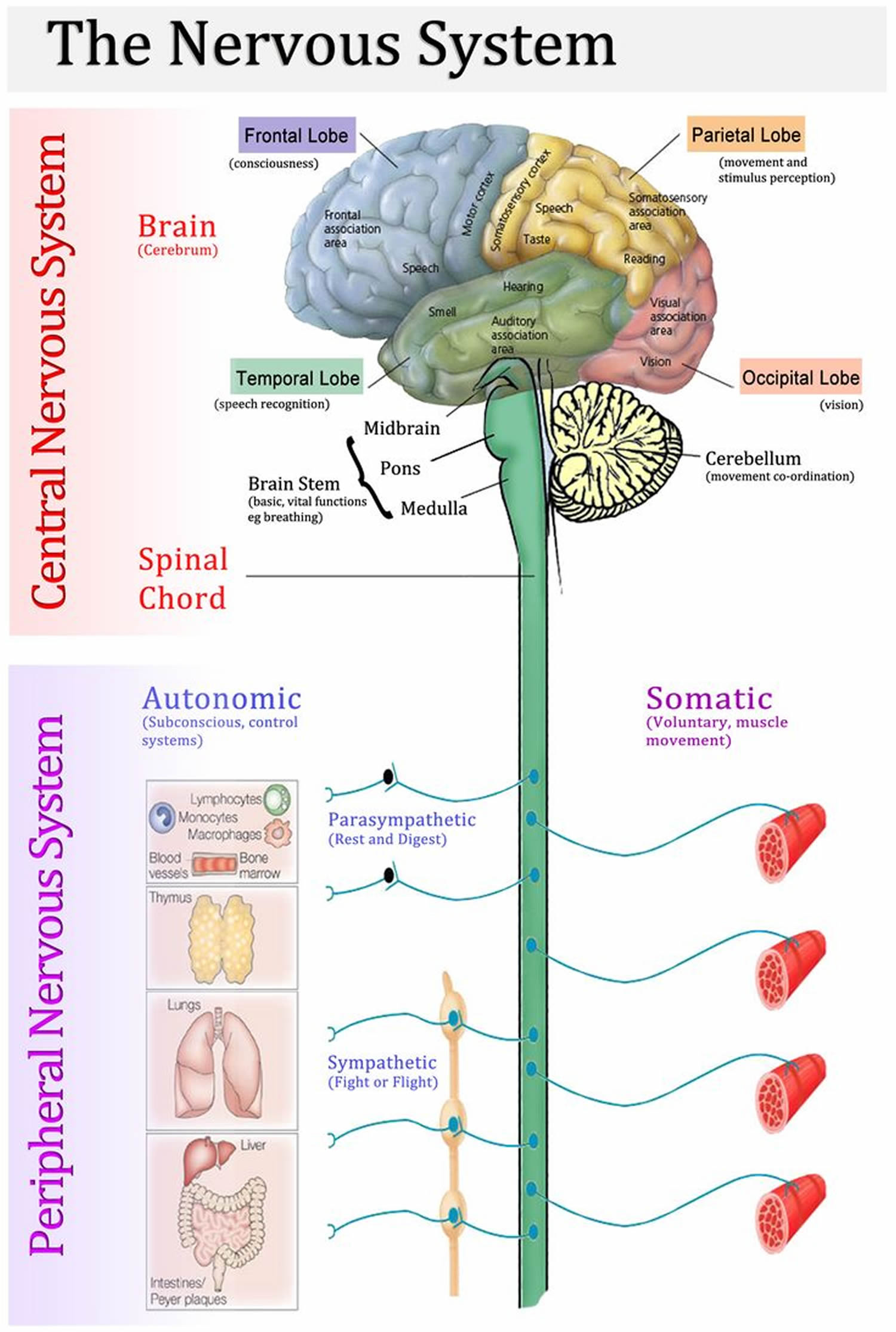
The nervous system has two major anatomical subdivisions:
- The central nervous system (CNS) consists of the brain and spinal cord, which are enclosed and protected by the cranium and vertebral column. The central nervous system is discussed further in the other posts: Human brain and Spinal cord.
- The peripheral nervous system (PNS) consists of all the rest; it is composed of nerves and ganglia. A nerve is a bundle of nerve fibers (axons) wrapped in fibrous connective tissue. Nerves emerge from the central nervous system (CNS) through foramina of the skull and vertebral column and carry signals to and from other organs of the body. A ganglion (plural, ganglia) is a knotlike swelling in a nerve where the cell bodies of peripheral neurons are concentrated.
Figure 1. Nervous system and its parts
Nervous system function
The communicative role of the nervous system is carried out by nerve cells, or neurons. These cells have three fundamental physiological properties that enable them to communicate with other cells:
- Excitability. All cells are excitable—that is, they respond to environmental changes (stimuli). Neurons exhibit this property to the highest degree.
- Conductivity. Neurons respond to stimuli by producing electrical signals that are quickly conducted to other cells at distant locations.
- Secretion. When the signal reaches the end of a nerve fiber, the neuron secretes a neurotransmitter that crosses the gap and stimulates the next cell.
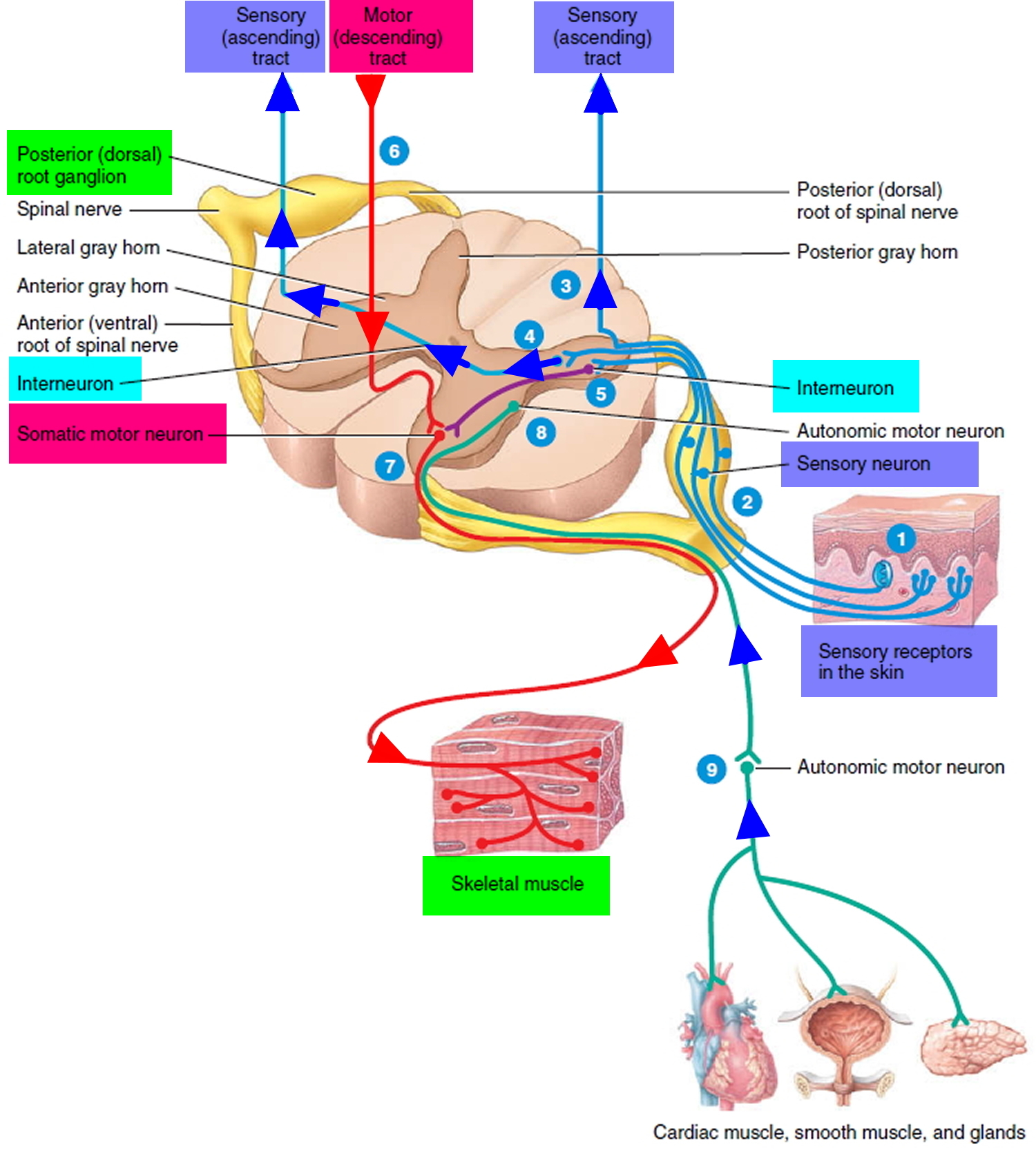
Functional Classes of Neurons
There are three general classes of neurons corresponding to the three major aspects of nervous system function listed above (e.g. excitability, conductivity and secretion):
- Sensory (afferent) neurons are specialized to detect stimuli such as light, heat, pressure, and chemicals, and transmit information about them to the central nervous system (CNS). Such neurons begin in almost every organ of the body and end in the central nervous system (CNS); the word afferent refers to signal conduction toward the central nervous system (CNS). Some receptors, such as those for pain and smell, are themselves neurons. In other cases, such as taste and hearing, the receptor is a separate cell that communicates directly with a sensory neuron.
- Interneurons lie entirely within the central nervous system (CNS). They receive signals from many other neurons and carry out the integrative function of the nervous system—that is, they process, store, and retrieve information and “make decisions” that determine how the body responds to stimuli. About 90% of our neurons are interneurons. The word interneuron refers to the fact that they lie between, and interconnect, the incoming sensory pathways and the outgoing motor pathways of the central nervous system (CNS).
- Motor (efferent) neurons send signals predominantly to muscle and gland cells, the effectors. They are called motor neurons because most of them lead to muscle cells, and efferent neurons to signify signal conduction away from the central nervous system (CNS).
Figure 2. Functional classes of neurons
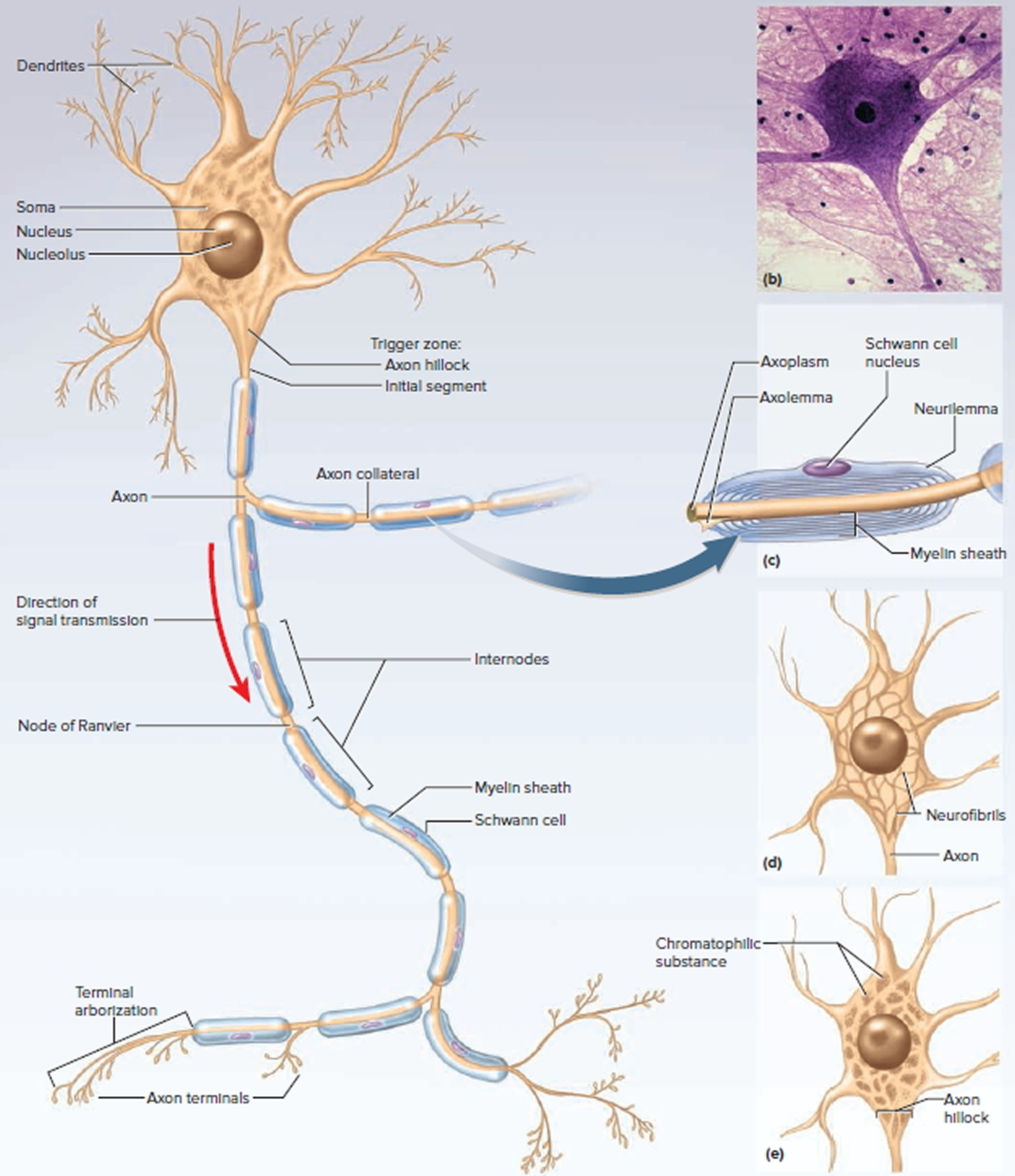
Structure of a Neuron
There are several varieties of neurons, but a good starting point for discussion is a motor neuron of the spinal cord. The control center of the neuron is the neurosoma, also called the soma or cell body. It has a centrally located nucleus with a large nucleolus. The cytoplasm contains mitochondria, lysosomes, a Golgi complex, numerous inclusions, and an extensive rough endoplasmic reticulum and cytoskeleton. The cytoskeleton consists of a dense mesh of microtubules and neurofibrils (bundles of actin filaments), which compartmentalize the rough endoplasmic reticulum into darkstaining regions called chromatophilic substance. This is unique to neurons and a helpful clue to identifying them in tissue sections with mixed cell types. Mature neurons have no centrioles and cannot undergo any further mitosis after adolescence. Consequently, neurons that die are usually irreplaceable; surviving neurons cannot multiply to replace those lost. However, neurons are unusually long-lived cells, capable of functioning for over a hundred years. But even in old age, there are unspecialized stem cells in some parts of the central nervous system (CNS) that can divide and regenerate nervous tissue to a limited extent.
The major inclusions in a neuron are glycogen granules, lipid droplets, melanin, and a golden brown pigment called lipofuscin, produced when lysosomes degrade worn-out organelles and other products. Lipofuscin accumulates with age and pushes the nucleus to one side of the cell. Lipofuscin granules are also called “wear-and-tear granules” because they are most abundant in old neurons. They seem harmless to neuron function.
Figure 3. General structure of a neuron
Myelin sheath
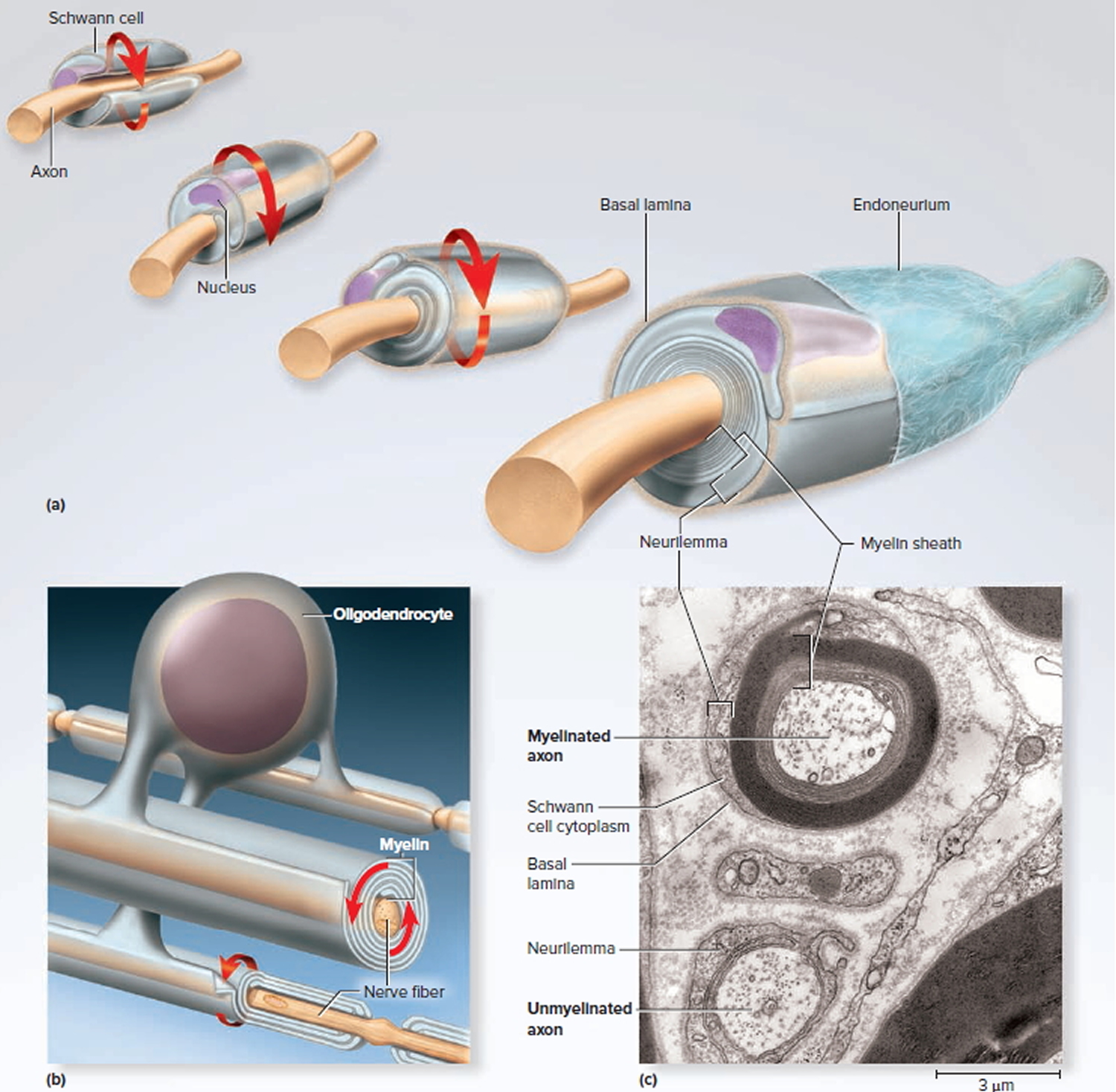
The myelin sheath is a spiral layer of insulation around a nerve fiber, formed by oligodendrocytes in the central nervous system (brain and spinal cord) and Schwann cells in the peripheral nervous system. Since it consists of the plasma membranes of glial cells, its composition is like that of plasma membranes in general. It is about 20% protein and 80% lipid, the latter including phospholipids, glycolipids, and cholesterol.
Production of the myelin sheath is called myelination. It begins in the fourteenth week of fetal development, yet hardly any myelin exists in the brain at the time of birth. Myelination proceeds rapidly in infancy and isn’t completed until late adolescence. Since myelin has such a high lipid content, dietary fat is important to early nervous system development. It is best not to give children under 2 years old the sort of low-fat diets (skimmed milk, etc.) that may be beneficial to an adult.
Figure 4. Myelination
Note:
- (a) A Schwann cell of the peripheral nervous system, wrapping repeatedly around an axon to form the multilayered myelin sheath.
The myelin spirals outward away from the axon as it is laid down. - (b) An oligodendrocyte of the central nervous system (brain and spinal cord) wrapping around the axons of multiple neurons. Here, the myelin spirals inward toward the axon as it is laid down.
- (c) A myelinated axon (top) and unmyelinated axon (bottom).
In the peripheral nervous system, a Schwann cell spirals repeatedly around a single nerve fiber, laying down up to 100 compact layers of its own membrane with almost no cytoplasm between the membranes. These layers constitute the myelin sheath. The Schwann cell spirals outward as it wraps the nerve fiber, finally ending with a thick outermost coil called the neurilemma. Here, the bulging body of the Schwann cell contains its nucleus and most of its cytoplasm. External to the neurilemma is a basal lamina and then a thin sleeve of fibrous connective tissue called the endoneurium. To visualize this myelination process, imagine that you wrap an almost-empty tube of toothpaste tightly around a pencil. The pencil represents the axon, and the spiral layers of toothpaste tube represent the myelin. The toothpaste, like the cytoplasm of the cell, would be forced to one end of the tube and form a bulge on the external surface of the wrapping, like the body of the Schwann cell.
In the central nervous system (brain and spinal cord), each oligodendrocyte reaches out to myelinate several nerve fibers in its immediate vicinity. Since it is anchored to multiple nerve fibers, it cannot migrate around any one of them like a Schwann cell does. It must push newer layers of myelin under the older ones, so myelination spirals inward toward the nerve fiber. Nerve fibers of the central nervous system (brain and spinal cord) have no neurilemma or endoneurium. The contrasting modes of myelination are called centrifugal myelination (“away from the center”) in the peripheral nervous system and centripetal myelination (“toward the center”) in the central nervous system (brain and spinal cord).
In both the peripheral nervous system and central nervous system (brain and spinal cord), a nerve fiber is much longer than the reach of a single glial cell, so it requires many Schwann cells or oligodendrocytes to cover one nerve fiber. Consequently, the myelin sheath is segmented. Each gap between segments is called a node of Ranvier or myelin sheath gap; the myelin-covered segments from each node to the next are called internodes. The internodes are about 0.2 to 1.0 mm long. The short section of nerve fiber between the axon hillock and the first glial cell is called the initial segment. Since the axon hillock and initial segment play an important role in initiating a nerve signal, they are collectively called the trigger zone.
Conduction Speed of Nerve Fibers
The speed at which a nerve signal travels along a nerve fiber depends on two factors: the diameter of the fiber and the presence or absence of myelin. Signal conduction occurs along the surface of a fiber, not deep within its axoplasm. Large fibers have more surface area and conduct signals more rapidly than small fibers.
Myelin further speeds signal conduction. Nerve signals travel about 0.5 to 2.0 m/s in small unmyelinated fibers (2–4 μm in diameter); 3 to 15 m/s in myelinated fibers of the same size; and as fast as 120 m/s in large myelinated fibers (up to 20 μm in diameter). You might wonder why all of your nerve fibers are not large, myelinated, and fast; but if this were so, your nervous system would be impossibly bulky or limited to far fewer fibers. Large nerve fibers require large somas and a large expenditure of energy to maintain them. The evolution of myelin allowed for the subsequent evolution of more complex and responsive nervous systems with smaller, more energy-efficient neurons. Slow unmyelinated fibers are quite sufficient for processes in which quick responses are not particularly important, such as secreting stomach acid or dilating the pupil. Fast myelinated fibers are employed where speed is more important, as in motor commands to the skeletal muscles and sensory signals for vision and balance.
Multiple sclerosis symptoms early
Most people experience their first symptoms of multiple sclerosis between the ages of 20 and 40; the initial symptom of multiple sclerosis is often blurred or double vision, red-green color distortion, or even blindness in one eye.
Multiple sclerosis symptoms
The signs and symptoms of multiple sclerosis vary widely from person to person and depend on the amount of nerve damage and which nerves are affected. They can also come and go in any one person. Multiple sclerosis is unpredictable.
Some people with severe MS may lose the ability to walk independently or at all, while others may experience long periods of remission without any new symptoms.
Most multiple sclerosis patients experience muscle weakness in their extremities and difficulty with coordination and balance. These symptoms may be severe enough to impair walking or even standing. In the worst cases, multiple sclerosis can produce partial or complete paralysis. Most people with multiple sclerosis also exhibit paresthesias, transitory abnormal sensory feelings such as numbness, prickling, or “pins and needles” sensations. Some may also experience pain. Speech impediments, tremors, and dizziness are other frequent complaints. Occasionally, people with multiple sclerosis have hearing loss. Approximately half of all people with multiple sclerosis experience cognitive impairments such as difficulties with concentration, attention, memory, and poor judgment, but such symptoms are usually mild and are frequently overlooked. Depression is another common feature of multiple sclerosis.
The most common symptoms are:
- loss of control of the arms and legs leading to difficulty with walking, balance and coordination;
- muscle spasms and problems with weakness and coordination
- tiredness
- sensitivity to heat (a hot day or a hot bath, or even a hot cup of tea, can make symptoms worse)
- other problems related to the nervous system such as dizziness, pins and needles, pain due to a damaged nerve, and problems with eyesight
- problems with the bladder and bowel causing incontinence and/or constipation
- changes in memory, in concentration, in reasoning, in emotions, or in mood (such as depression).
Other symptoms of MS are:
- numbness or weakness in one or more limbs that typically occurs on one side of your body at a time, or the legs and trunk
- partial or complete loss of vision, usually in one eye at a time, often with pain during eye movement (optic neuritis)
- prolonged double vision
- tingling or pain in parts of your body
- electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign)
- tremor, lack of coordination or unsteady gait
- slurred speech
- fatigue
- dizziness
- problems with bowel and bladder function
- sexual dysfunction
Signs of MS are:
- Ataxia (loss of full control of bodily movements)
- Decreased sensation (pain, vibration, position)
- Decreased strength
- Hyperreflexia, spasticity
- Nystagmus (rapid involuntary movements of the eyes)
MS Disease course
Most people with MS have a relapsing-remitting disease course. They experience periods of new symptoms or relapses that develop over days or weeks and usually improve partially or completely. These relapses are followed by quiet periods of disease remission that can last months or even years.
Small increases in body temperature can temporarily worsen signs and symptoms of MS, but these aren’t considered disease relapses.
About 60 to 70 percent of people with relapsing-remitting MS eventually develop a steady progression of symptoms, with or without periods of remission, known as secondary-progressive MS.
The worsening of symptoms usually includes problems with mobility and gait. The rate of disease progression varies greatly among people with secondary-progressive MS.
Some people with MS experience a gradual onset and steady progression of signs and symptoms without any relapses. This is known as primary-progressive MS.
Multiple sclerosis causes
The cause of multiple sclerosis is unknown. It’s considered an autoimmune disease in which the body’s immune system attacks its own tissues. In the case of MS, this immune system malfunction destroys myelin (the fatty substance that coats and protects nerve fibers in the brain and spinal cord).
Myelin can be compared to the insulation coating on electrical wires. When the protective myelin is damaged and nerve fiber is exposed, the messages that travel along that nerve may be slowed or blocked. The nerve may also become damaged itself.
It isn’t clear why MS develops in some people and not others. A combination of genetics and environmental factors appears to be responsible.
Risk factors for multiple sclerosis
These factors may increase your risk of developing multiple sclerosis:
- Age. MS can occur at any age, but most commonly affects people between the ages of 15 and 60.
- Sex. Women are about twice as likely as men are to develop MS.
- Family history. If one of your parents or siblings has had MS, you are at higher risk of developing the disease.
- Certain infections. A variety of viruses have been linked to MS, including Epstein-Barr, the virus that causes infectious mononucleosis.
- Race. White people, particularly those of Northern European descent, are at highest risk of developing MS. People of Asian, African or Native American descent have the lowest risk.
- Climate. MS is far more common in countries with temperate climates, including Canada, the northern United States, New Zealand, southeastern Australia and Europe.
- Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have thyroid disease, type 1 diabetes or inflammatory bowel disease.
- Smoking. Smokers who experience an initial event of symptoms that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS.
Complications of multiple sclerosis
People with multiple sclerosis also may develop:
- Muscle stiffness or spasms
- Paralysis, typically in the legs
- Problems with bladder, bowel or sexual function
- Mental changes, such as forgetfulness or mood swings
- Depression
- Epilepsy
How is multiple sclerosis diagnosed ?
There are no specific tests for MS. Instead, a diagnosis of multiple sclerosis often relies on ruling out other conditions that might produce similar signs and symptoms, known as a differential diagnosis.
Your doctor is likely to start with a thorough medical history and examination. Your doctor may then recommend:
- Blood tests, to help rule out other diseases with symptoms similar to MS. Tests to check for specific biomarkers associated with MS are currently under development and may also aid in diagnosing the disease.
- Lumbar puncture (spinal tap), in which a small sample of fluid is removed from your spinal canal for laboratory analysis. This sample can show abnormalities in antibodies that are associated with MS. Spinal tap can also help rule out infections and other conditions with symptoms similar to MS.
- MRI, which can reveal areas of MS (lesions) on your brain and spinal cord. You may receive an intravenous injection of a contrast material to highlight lesions that indicate your disease is in an active phase.
- Evoked potential tests, which record the electrical signals produced by your nervous system in response to stimuli. An evoked potential test may use visual stimuli or electrical stimuli, in which you watch a moving visual pattern, or short electrical impulses are applied to nerves in your legs or arms. Electrodes measure how quickly the information travels down your nerve pathways.
In most people with relapsing-remitting MS, the diagnosis is fairly straightforward and based on a pattern of symptoms consistent with the disease and confirmed by brain imaging scans, such as MRI.
Diagnosing MS can be more difficult in persons with unusual symptoms or progressive disease. In these cases, further testing with spinal fluid analysis, evoked potentials and additional imaging may be needed.
Table 2. Conditions Potentially Confused with Multiple Sclerosis
| Disease | Examples | |
|---|---|---|
Central and peripheral nervous system disease | ||
Degenerative disease | Amyotrophic lateral sclerosis, Huntington disease | |
Demyelinating disease | Chronic inflammatory demyelinating polyneuropathy, progressive multifocal leukoencephalopathy | |
Infection | Human immunodeficiency virus infection, Lyme disease, mycoplasma, syphilis | |
Inflammatory disease | Behçet syndrome, sarcoidosis, Sjögren syndrome, systemic lupus erythematosus | |
Structural disease | Arteriovenous malformation, herniated disk, neoplasm | |
Vascular disease | Cerebrovascular accident, diabetes mellitus, hypertensive disease, migraine, vasculitis | |
Genetic disorder | Leukodystrophy, mitochondrial disease | |
Medication and illicit drug effects | Alcohol, cocaine, isoniazid, lithium, penicillin, phenytoin (Dilantin) | |
Nutritional deficiency | Folate deficiency, vitamin B12 deficiency, vitamin E deficiency | |
Psychiatric disease | Anxiety, conversion disorder, somatization | |
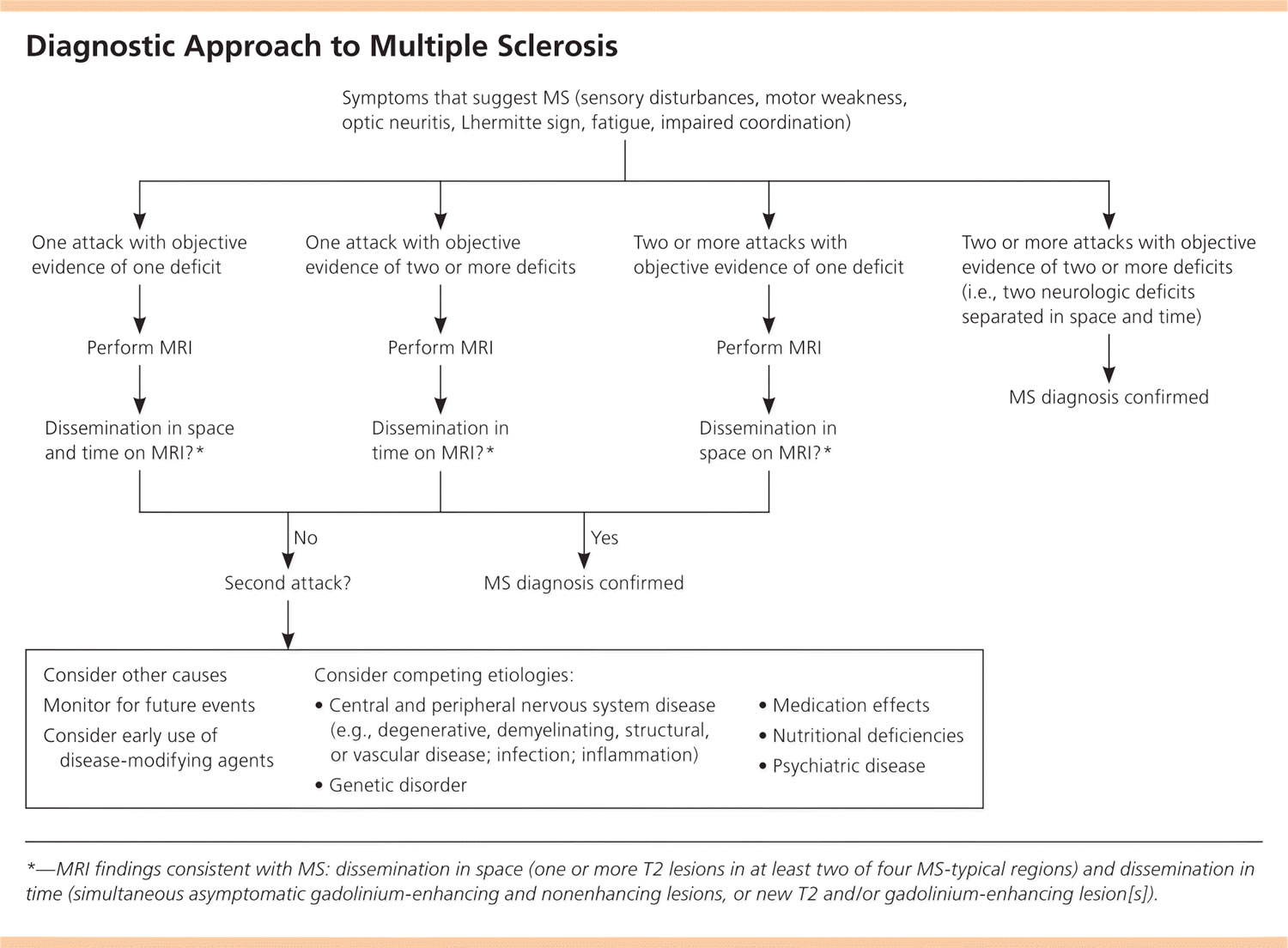
Diagnostic Criteria to Multiple Sclerosis
MS is a clinical diagnosis. Two neurologic deficits (e.g., focal weakness, sensory disturbances) separated in time and space, in the absence of fever, infection, or competing etiologies, are considered diagnostic 8, 9. Attacks may be patient-reported or objectively observed, and must last for a minimum of 24 hours. Corroborating magnetic resonance imaging (MRI) is the diagnostic standard (Figure 5) 8.
Figure 5. Diagnostic Criteria to Multiple Sclerosis
Note: MRI = magnetic resonance imaging; MS = multiple sclerosis.
[Source 7]Multiple sclerosis treatment
There is no cure for MS, but medicines may slow it down and help control symptoms. Physical and occupational therapy may also help.
There is no single test for multiple sclerosis. Doctors use a medical history, physical exam, neurological exam, MRI, and other tests to diagnose it.
Treatments for multiple sclerosis signs and symptoms
Physical therapy. A physical or occupational therapist can teach you stretching and strengthening exercises and show you how to use devices to make it easier to perform daily tasks.
Physical therapy along with the use of a mobility aid when necessary can also help manage leg weakness and other gait problems often associated with MS.
Muscle relaxants. You may experience painful or uncontrollable muscle stiffness or spasms, particularly in your legs. Muscle relaxants such as baclofen (Lioresal) and tizanidine (Zanaflex) may help.
Medications to reduce fatigue.
Other medications. Medications also may be prescribed for depression, pain, sexual dysfunction, and bladder or bowel control problems that are associated with MS.
NEUROGENIC BLADDER
More than 70% of patients with MS have urinary tract dysfunction, with 10% demonstrating urinary symptoms at initial diagnosis 10. Urinary dysfunction can be classified as failure to store or empty, and can be differentiated with postvoid residual testing.35 Failure-to-store symptoms are typically treated with anticholinergic medications, although patients should be cautioned about adverse effects, such as dry mouth and confusion. Nocturia may respond to limited evening fluid intake or intranasal desmopressin; if desmopressin is prescribed, patients should be cautioned about the potential for hyponatremia. Injectable onabotulinumtoxinA (Botox) may be used if symptoms do not respond to these agents. Failure-to-empty symptoms are treated with clean intermittent catheterization, although some may respond to an alpha adrenergic blocker 11.
NEUROGENIC BOWEL
Up to 75% of patients with MS experience constipation, incontinence, or both 12. Treatment should include dietary fiber, bulk-forming agents, and adequate hydration. Rectal stimulants, stool softeners, and enemas may be used if needed. Colostomy is an option for patients with intolerable symptoms 12.
SEXUAL DYSFUNCTION
About 50% to 90% of men and 40% to 85% of women with MS have some type of sexual dysfunction 13. Although sexual dysfunction may have a considerable negative impact on quality of life, it is often unaddressed. Men are primarily treated with peripherally acting phosphodiesterase-5 inhibitors. There is no established pharmacologic agent for women. Collaboration with a sex therapist or couples counselor may be beneficial 14.
PAIN
Approximately 85% of patients with MS report pain during the course of their illness 13. Those with pain report poorer health and poorer psychological functioning.
Trigeminal neuralgia and dysesthetic (neuropathic) limb pain are common. Trigeminal neuralgia is initially treated with carbamazepine (Tegretol) and baclofen (Lioresal), as it is in persons without MS. Neuropathic pain in MS may be treated with tricyclic antidepressants, anticonvulsants, and selective serotonin reuptake inhibitors 15. Hydrotherapy has also been shown to be helpful in pain management, and is beneficial for the spasticity associated with MS 16. Cannabinoid therapy may be helpful for pain symptoms 17.
SPASTICITY
It is estimated that 70% to 80% of patients with MS experience muscle spasticity 13. These symptoms are best treated with a multidisciplinary approach, incorporating modalities such as physical, occupational, and electromagnetic therapy 18.
Baclofen is a first-line agent and works by decreasing alpha motor neuron activity. Oral baclofen has a short half-life and is associated with daytime sedation and muscle weakness. Intrathecal baclofen can be used to avoid daytime sedation, although muscle weakness may still occur. Diazepam (Valium) and gabapentin (Neurontin) may be used alone or in conjunction with baclofen 19. OnabotulinumtoxinA, with or without concomitant physical therapy, may also be helpful.36 Although cannabinoid therapy has been used for spasticity, the evidence for its effectiveness is mixed. The American Academy of Neurology states that patients should be counseled that these agents are probably ineffective for objective spasticity 17.
FATIGUE
More than 90% of patients with MS report fatigue; one-third report it to be their most troubling symptom, and many present with it 13. Although fatigue may occur as a result of comorbid depression, it also may appear independently. Fatigue has profound impacts on quality of life and is a leading cause of disability claims 14.
Treatment for fatigue is multifocal. After evaluating for comorbid causes of fatigue (e.g., sleep disorders, thyroid disease, vitamin B12 deficiency, anemia), environmental manipulation, such as controlling heat and humidity levels, may help prevent flare-ups. Energy conservation measures such as napping and the use of assistive devices for mobility may be recommended based on the individual patient. Amantadine has been used off label in a limited number of trials and has been found to be beneficial for fatigue, although it is associated with insomnia and confusion 20. Other medications, such as modafinil (Provigil), have been tried with mixed results, and are not FDA approved for patients with MS 21.
CHRONIC DISEASE MANAGEMENT
The prevalence of hypertension, hyperlipidemia, diabetes mellitus, and other vascular comorbidities in patients with MS is similar to that in the general population. The presence of these conditions may worsen the course of MS 22.
Treatments for MS attacks
Exacerbations affect 85% of patients with multiple sclerosis 23; infections and stress may play a role. For those with significant, acute symptoms, corticosteroids are the treatment of choice and have strong evidence of benefit 24. Although parenteral steroids build up to peak concentrations faster than oral preparations, a Cochrane review indicates no difference in effectiveness (as measured by clinical or radiologic markers) or safety between oral and parenteral preparations 25. If the disease is unresponsive to steroids, plasmapheresis may be performed. Plasma exchanges are relatively well tolerated and are usually performed every other day for 14 days 26.
Corticosteroids, such as oral prednisone and intravenous methylprednisolone, are prescribed to reduce nerve inflammation. Side effects may include insomnia, increased blood pressure, mood swings and fluid retention.
Plasma exchange (plasmapheresis). The liquid portion of part of your blood (plasma) is removed and separated from your blood cells. The blood cells are then mixed with a protein solution (albumin) and put back into your body. Plasma exchange may be used if your symptoms are new, severe and haven’t responded to steroids.
Treatments to modify progression of multiple sclerosis
The goal of disease-modifying therapy is to forestall disease, preserve function, and sustain healthy immune function while suppressing the T-cell autoimmune cascade thought to be responsible for demyelination and axonal damage. Early treatment at or before the diagnosis of clinically confirmed MS may delay damage to the central nervous system 27. The U.S. Food and Drug Administration (FDA) has approved seven agents for the treatment of MS: interferon beta, glatiramer (Copaxone), fingolimod (Gilenya), teriflunomide (Aubagio), dimethyl fumarate (Tecfidera), natalizumab (Tysabri), and mitoxantrone (Table 3). Because of the chronic nature and evolving treatment of MS, disease-modifying treatment is typically managed by a neurologist with expertise in prescribing these potentially toxic agents.
Table 3. Disease-Modifying Agents for Relapsing Remitting Multiple Sclerosis
| Agent | Dosage | Cost (yearly)* | Evidence (95% confidence interval) | Adverse effects | |
|---|---|---|---|---|---|
Interferon beta | $62,000 to $67,000 | Decrease in relapses: RR = 0.80 | Injection site reactions (e.g., edema, inflammation, pain); influenza-like symptoms; leukopenia; elevated liver enzyme levels; depression and suicidal thoughts (increased with preexisting depression, neutralizing antibodies) | ||
Interferon beta-1a IM (Avonex) | Intramuscular, weekly | Decrease in progression: RR = 0.69 | |||
Interferon beta-1a SC (Rebif) | Subcutaneous, three times per week | ||||
Interferon beta-1b (Betaseron) | Subcutaneous, every other day | ||||
Glatiramer (Copaxone) | Subcutaneous, daily | $70,000 | Decrease in relapses: MD = 0.51 | Injection site reactions, facial flushing, chest tightness, palpitations | |
Decrease in disability at two years: MD = 0.33 | |||||
Fingolimod (Gilenya) | Oral, daily | $67,000 | Annualized relapse rate vs. placebo: 0.18 vs. 0.40 | Bradycardia (contraindicated in recent heart disease or arrhythmia); elevated liver enzyme levels | |
Decrease in progression at two years: HR = 0.70 | Melanoma, macular edema, herpes encephalitis (only occurs at higher doses) | ||||
Teriflunomide (Aubagio) | Oral, daily | $63,000 | Annualized relapse rate vs. placebo: 0.37 vs. 0.54 | Alopecia, diarrhea, nausea, decreased white blood cell count, elevated liver enzyme levels, peripheral neuropathy | |
Decrease in progression: HR = 0.76 | |||||
Dimethyl fumarate (Tecfidera) | Oral, daily | $68,000 | Annualized relapse rate vs. placebo: 0.17 vs. 0.36 | Flushing, abdominal pain, lymphocytopenia, elevated liver enzyme levels | |
Decrease in progression: HR = 0.62 | |||||
Natalizumab (Tysabri) | Intravenous, once per month | $61,000 | Decrease in relapses: RR = 0.57 | Infusion reactions, headache, fatigue, progressive multifocal leukoencephalopathy | |
Decrease in progression at two years: RR = 0.74 | |||||
Mitoxantrone | Intravenous, every three months | $900 | Decrease in relapses: MD = 0.85 | Myelosuppression, elevated liver enzyme levels, decreased cardiac function, leukemia | |
Decrease in progression: OR = 0.30 | |||||
HR = hazard ratio; MD = mean difference; OR = odds ratio; RR = relative risk.
*—Estimated retail price of treatment for one year based on information obtained at http://www.goodrx.com. All prices are for brand name drugs except for mitoxantrone, which is available only as generic.
For primary-progressive MS, ocrelizumab (Ocrevus) is the only FDA-approved disease-modifying therapy. It slows worsening of disability in people with this type of MS.
For relapsing-remitting MS, several disease-modifying therapies are available.
Much of the immune response associated with MS occurs in the early stages of the disease. Aggressive treatment with these medications as early as possible can lower the relapse rate and slow the formation of new lesions.
Many of the disease-modifying therapies used to treat MS carry significant health risks. Selecting the right therapy for you will depend on careful consideration of many factors, including duration and severity of disease, effectiveness of previous MS treatments, other health issues, cost, and child-bearing status.
Treatment options for relapsing-remitting MS include:
Beta interferons. These medications are among the most commonly prescribed medications to treat MS. They are injected under the skin or into muscle and can reduce the frequency and severity of relapses.
Side effects of beta interferons may include flu-like symptoms and injection-site reactions.
You’ll need blood tests to monitor your liver enzymes because liver damage is a possible side effect of interferon use. People taking interferons may develop neutralizing antibodies that can reduce drug effectiveness.
Ocrelizumab (Ocrevus). This humanized immunoglobulin antibody medication is the only DMT approved by the FDA to treat both the relapse-remitting and primary progressive forms of MS. Clinical trials showed it reduced relapse rate in relapsing disease and slowed worsening of disability in both forms of the disease.
Ocrevus is given via an intravenous infusion by a medical professional. Side effects may infusion-related reactions including irritation at the injection site, low blood pressure, fever, and nausea among others. Ocrevus may also increase the risk of some types of cancer, particularly breast cancer.
Glatiramer acetate (Copaxone). This medication may help block your immune system’s attack on myelin and must be injected beneath the skin. Side effects may include skin irritation at the injection site.
Dimethyl fumarate (Tecfidera). This twice-daily oral medication can reduce relapses. Side effects may include flushing, diarrhea, nausea and lowered white blood cell count.
Fingolimod (Gilenya). This once-daily oral medication reduces relapse rate.
You’ll need to have your heart rate monitored for six hours after the first dose because your heartbeat may be slowed. Other side effects include headache, high blood pressure and blurred vision.
Teriflunomide (Aubagio). This once-daily medication can reduce relapse rate. Teriflunomide can cause liver damage, hair loss and other side effects. It is harmful to a developing fetus and should not be used by women who may become pregnant and are not using appropriate contraception, or their male partner.
Natalizumab (Tysabri). This medication is designed to block the movement of potentially damaging immune cells from your bloodstream to your brain and spinal cord. It may be considered a first line treatment for some people with severe MS or as a second line treatment in others. This medication increases the risk of a viral infection of the brain called progressive multifocal leukoencephalopathy in some people.
Alemtuzumab (Lemtrada). This drug helps reduce relapses of MS by targeting a protein on the surface of immune cells and depleting white blood cells. This effect can limit potential nerve damage caused by the white blood cells, but it also increases the risk of infections and autoimmune disorders.
Treatment with alemtuzumab involves five consecutive days of drug infusions followed by another three days of infusions a year later. Infusion reactions are common with alemtuzumab. The drug is only available from registered providers, and people treated with the drug must be registered in a special drug safety monitoring program.
Mitoxantrone. This immunosuppressant drug can be harmful to the heart and is associated with development of blood cancers. As a result, its use in treating MS is extremely limited. Mitoxantrone is usually used only to treat severe, advanced MS.
Home remedies for multiple sclerosis
To help relieve the signs and symptoms of MS, try to:
- Get plenty of rest.
- Exercise. If you have mild to moderate MS, regular exercise can help improve your strength, muscle tone, balance and coordination. Swimming or other water exercises are good options if you’re bothered by heat. Other types of mild to moderate exercise recommended for people with MS include walking, stretching, low-impact aerobics, stationary bicycling, yoga and tai chi.
- Cool down. MS symptoms often worsen when your body temperature rises. Avoiding exposure to heat and using devices such as cooling scarves or vests can be helpful.
- Eat a balanced diet. Results of small studies suggest that a diet low in saturated fat but high in omega-3 fatty acids, such as those found in olive and fish oils, may be beneficial. But further research is needed. Studies also suggest that vitamin D may have potential benefit for people with MS.
- Relieve stress. Stress may trigger or worsen your signs and symptoms. Yoga, tai chi, massage, meditation or deep breathing may help.
Many people with MS use a variety of alternative or complementary treatments or both to help manage their symptoms, such as fatigue and muscle pain.
Activities such as exercise, meditation, yoga, massage, eating a healthier diet, acupuncture and relaxation techniques may help boost overall mental and physical well-being, but there are few studies to back up their use in managing symptoms of MS.
Guidelines from the American Academy of Neurology recommend the use of oral cannabis extract for muscle spasticity and pain, but do not recommend cannabis in any other form for other MS symptoms due to a lack of evidence.
The guidelines also do not recommend the use of herbal supplements such as Ginkgo biloba and bee venom or magnetic therapy for MS symptoms.
- Multiple Sclerosis. Medline Plus. https://medlineplus.gov/multiplesclerosis.html[↩]
- Multiple sclerosis. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269[↩]
- Noonan CW, Wiliamson DM, Henry JP, et al. The prevalence of multiple sclerosis in 3 US communities. Prev Chronic Dis. 2010;7(1):A12.[↩]
- Ramagopalan SV, Sadovnick AD. Epidemiology of multiple sclerosis. Neurol Clin. 2011;29(2):207–217.[↩]
- Adelman G, Rane SG, Villa KF. The cost burden of multiple sclerosis in the United States: a systematic review of the literature. J Med Econ. 2013;16(5):639–647.[↩]
- Types of MS. MS Australia. https://www.msaustralia.org.au/about-ms/types-ms[↩]
- Multiple Sclerosis: A Primary Care Perspective. Am Fam Physician. 2014 Nov 1;90(9):644-652. http://www.aafp.org/afp/2014/1101/p644.html[↩][↩][↩][↩]
- Polman CH, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69(2):292–302.[↩][↩]
- Sicotte NL. Magnetic resonance imaging in multiple sclerosis: the role of conventional imaging. Neurol Clin. 2011;29(2):343–356.[↩]
- Fowler CJ, et al. A UK consensus on the management of the bladder in multiple sclerosis. Postgrad Med J. 2009;85(1008):552–559.[↩]
- Habek M, et al. The place of the botulinum toxin in the management of multiple sclerosis. Clin Neurol Neurosurg. 2010;112(7):592–596.[↩]
- Preziosi G, Emmanuel A. Neurogenic bowel dysfunction: pathophysiology, clinical manifestations and treatment. Expert Rev Gastroenterol Hepatol. 2009;3(4):417–423.[↩][↩]
- Samkoff LM, Goodman AD. Symptomatic management in multiple sclerosis. Neurol Clin. 2011;29(2):449–463.[↩][↩][↩][↩]
- Ben-Zacharia AB. Therapeutics for multiple sclerosis symptoms. Mt Sinai J Med. 2011;78(2):176–191.[↩][↩]
- Leandri M. Therapy of trigeminal neuralgia secondary to multiple sclerosis. Expert Rev Neurother. 2003;3(5):661–671.[↩]
- Castro-Sánchez AM, et al. Hydrotherapy for the treatment of pain in people with multiple sclerosis: a randomized controlled trial. Evid Based Complement Alternat Med. 2012;2012:473963.[↩]
- Yadav V, Bever C Jr, Bowen J, et al. Summary of evidence-based guideline: complementary and alternative medicine in multiple sclerosis: report of the guideline development subcommittee of the American Academy of Neurology. Neurology. 2014;82(12):1083–1092.[↩][↩]
- Amatya B, et al. Non pharmacological interventions for spasticity in multiple sclerosis. Cochrane Database Syst Rev. 2013;(2):CD009974.[↩]
- Calabresi PA. Diagnosis and management of multiple sclerosis. Am Fam Physician. 2004;70(10):1935–1944.[↩]
- Brown JN, Howard CA, Kemp DW. Modafinil for the treatment of multiple sclerosis-related fatigue. Ann Pharmacother. 2010;44(6):1098–1103.[↩]
- Nayak S, et al. Use of unconventional therapies by individuals with multiple sclerosis. Clin Rehabil. 2003;17(2):181–191.[↩]
- Marrie RA, et al.; CIHR Team in Epidemiology and Impact of Comorbidity on Multiple Sclerosis. Rising prevalence of vascular comorbidities in multiple sclerosis: validation of administrative definitions for diabetes, hypertension, and hyperlipidemia. Mult Scler. 2012;18(9):1310–1319.[↩]
- Grosset KA, Grosset DG. Prescribed drugs and neurological complications. J Neurol Neurosurg Psychiatry. 2004;75(suppl 3):iii2–iii8.[↩]
- The National Collaborating Centre for Chronic Conditions. Multiple sclerosis: national clinical guideline for diagnosis and management in primary and secondary care. London, United Kingdom: Royal College of Physicians of London; 2014. https://www.nice.org.uk/guidance/cg186[↩]
- Burton JM, et al. Oral versus intravenous steroids for treatment of relapses in multiple sclerosis. Cochrane Database Syst Rev. 2012;(12):CD006921.[↩]
- Repovic P, Lublin FD. Treatment of multiple sclerosis exacerbations. Neurol Clin. 2011;29(2):389–400.[↩]
- Bates D. Treatment effects of immunomodulatory therapies at different stages of multiple sclerosis in short-term trials. Neurology. 2011;76 (1 suppl 1):S14–S25.[↩]