Contents
- What is multiple myeloma
- There are several types of plasma cell cancers
- Multiple myeloma symptoms and signs
- What Causes Myeloma
- Complications of multiple myeloma
- Multiple myeloma prognosis
- Multiple Myeloma Diagnosis
- Multiple Myeloma Stages
- Multiple myeloma treatment
- Immediate treatment may not be necessary
- Induction therapy
- Consolidation chemotherapy
- Maintenance therapy
- Refractory Multiple Myeloma
- Treatment options for myeloma
- How treatments are used
- Treating complications
- Supportive care
- Patients may want to take part in a clinical trial
- Alternative medicine
- Coping and support
- Treatment of Monoclonal Gammopathy of Undetermined Significance
- Treatment of Isolated Plasmacytoma of Bone
- Treatment of Extramedullary Plasmacytoma
What is multiple myeloma
Myeloma is a cancer where your bone marrow makes too many abnormal (cancer) plasma cells. Rather than produce helpful antibodies, the abnormal (cancer) plasma cells produce abnormal proteins that can cause complications. These abnormal plasma cells make M proteins, which are abnormal antibodies that build up in the bone marrow and can cause the blood to thicken or damage the kidneys. In contrast, healthy plasma cells are cells in the immune system that make antibodies that recognize and attack germs in order to help your body fight infections.
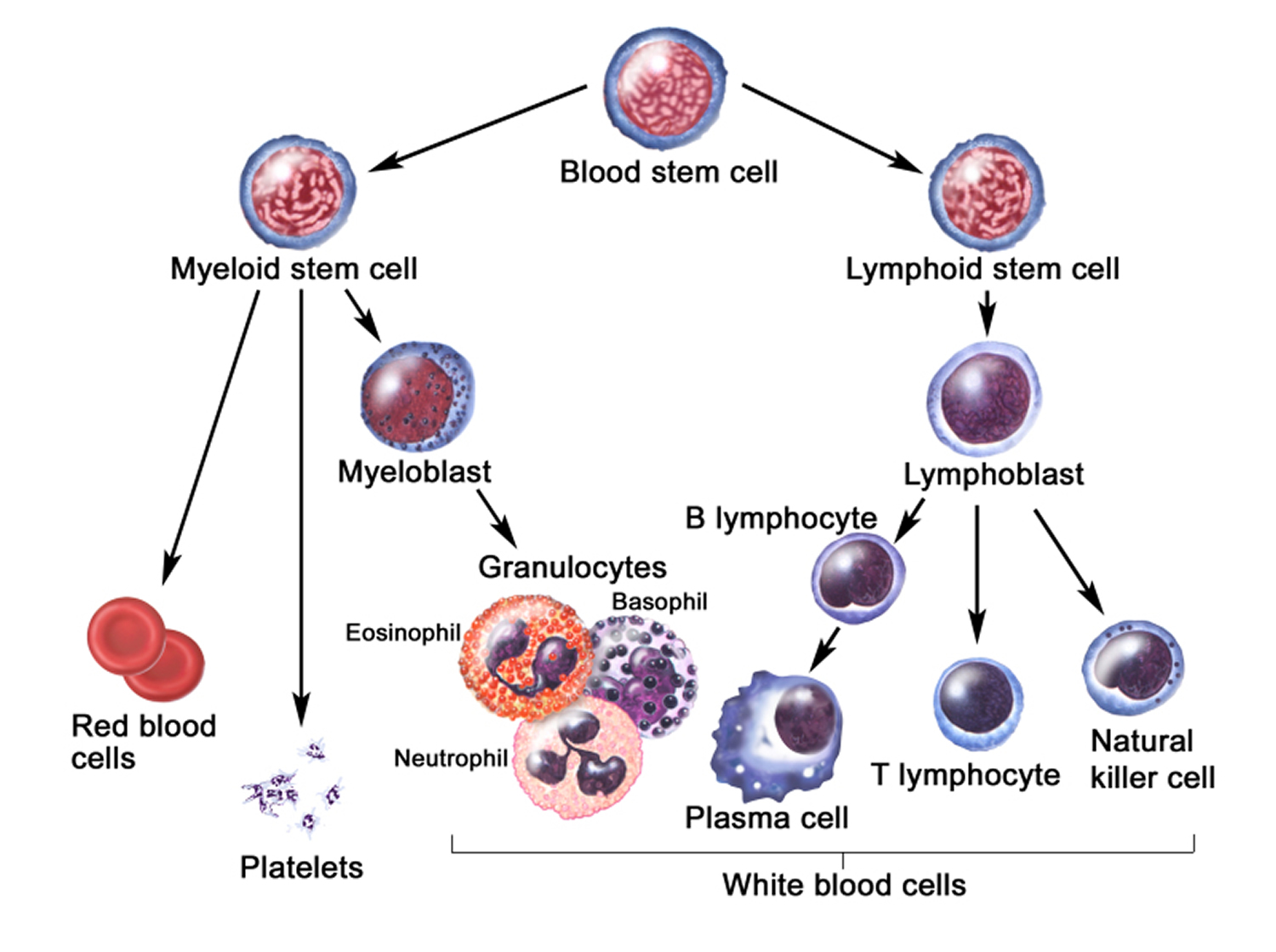
Your immune system is made up of several types of cells that work together to fight infections and other diseases. Lymphocytes (lymph cells) are the main cell type of the immune system. The major types of lymphocytes are T cells and B cells.
When B cells respond to an infection, they mature and change into plasma cells. Plasma cells make the antibodies (also called immunoglobulins = antibodies) that help the body attack and kill germs. Lymphocytes are in many areas of the body, such as lymph nodes, the bone marrow, the intestines and the bloodstream. Plasma cells, however, are mainly found in the bone marrow. Bone marrow is the soft tissue inside some hollow bones. In addition to plasma cells, normal bone marrow has cells that make the different normal blood cells (see Figures 2 and 3).
When plasma cells become cancerous and grow out of control, they can produce a tumor called a plasmacytoma. These tumors generally develop in a bone, but they are also rarely found in other tissues. If someone has only a single plasma cell tumor, the disease is called an isolated (or solitary) plasmacytoma. If someone has more than one plasmacytoma, they have multiple myeloma. Both are malignant (cancer).
Multiple myeloma causes cancerous plasma cells cells to accumulate in the bone marrow, where they crowd out healthy blood cells. Myeloma tumors can weaken the bone, cause too much calcium in the blood and damage the kidneys and other organs. Bone pain is a common symptom of advanced multiple myeloma. Other signs and symptoms include frequent infections, anemia, bleeding, numbness or tingling, and weakness.
Multiple myeloma may not cause signs or symptoms for a long time and is often not found until it is advanced. Treatment for multiple myeloma isn’t always necessary for people who aren’t experiencing any signs or symptoms.
Multiple myeloma is a relatively uncommon cancer. In the United States, the lifetime risk of getting multiple myeloma is 1 in 143 (0.7%) 1.
The American Cancer Society’s estimates for multiple myeloma in the United States for 2017 are 1:
- About 30,280 new cases will be diagnosed (17,490 in men and 12,790 in women).
- About 12,590 deaths are expected to occur (6,660 in men and 5,930 in women).
The cause of multiple myeloma is currently unknown. This cancer usually occurs in people older than 60 years of age. It is slightly more common in men than in women. It can often run in families. Multiple myeloma is also more common in blacks than in whites. Some studies suggest that workers in agriculture or petroleum-based industries may be at greater risk due to exposure to chemicals.
Multiple myeloma life expectancy – 5-year relative survival, 2006-2012 1
- All stages combined 49 percent
- Localized 70 percent
- Distant 47 percent
For people with multiple myeloma who require treatment, a number of treatments are available to help control the disease.
Despite the development of novel therapies that have improved the depth and duration of responses and prolonged survival for many patients with this disease, multiple myeloma remains incurable in most patients, because of the emergence of resistant clones, leading to repeated relapses of the disease 2, 3.
One type of benign (not cancer) plasma cell neoplasm is called monoclonal gammopathy of undetermined significance (MGUS). In MGUS, there are low levels of M protein and there are no symptoms or damage to the body. In rare cases, MGUS can become multiple myeloma.
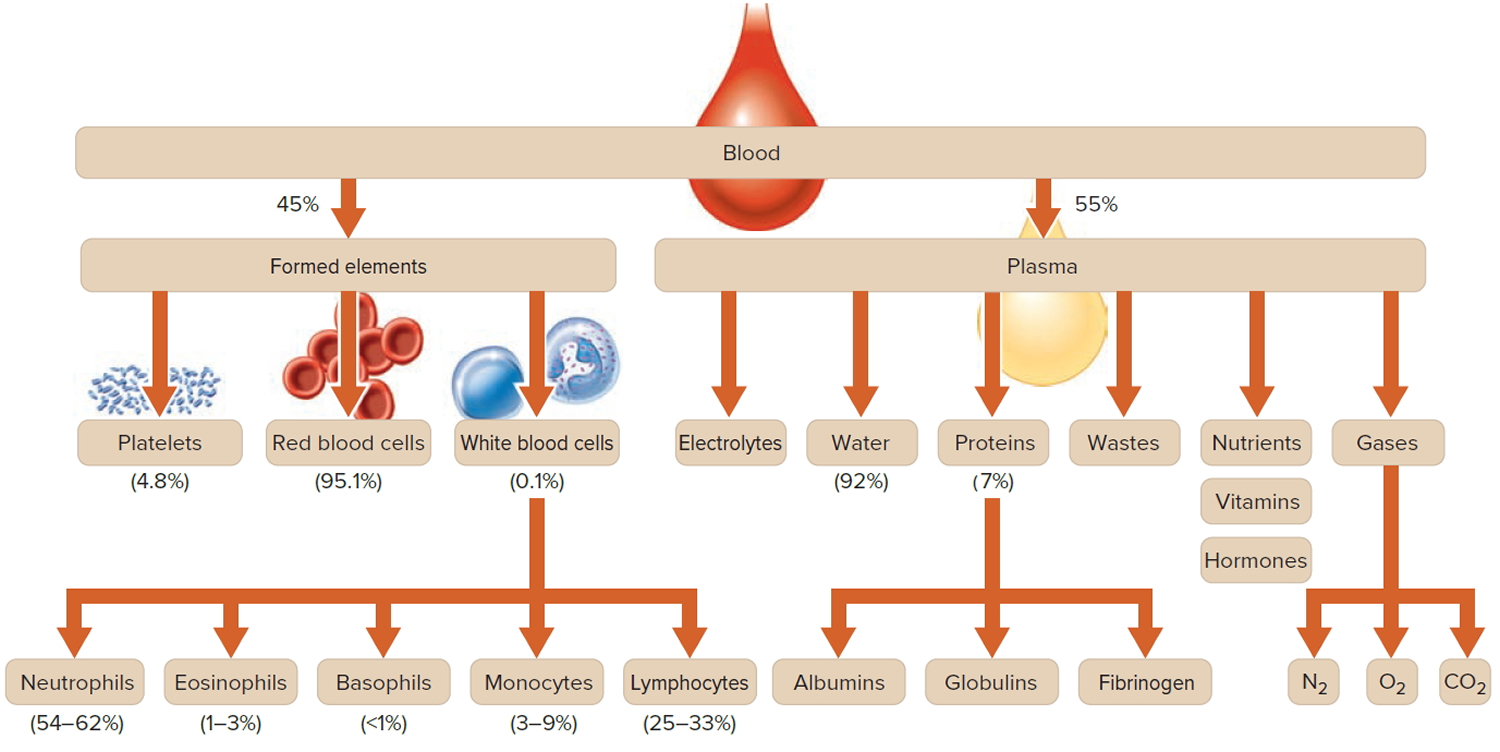
Figure 1. Blood composition
Note: Blood is a complex mixture of formed elements in a liquid extracellular matrix, called blood plasma. Note that water and proteins account for 99% of the blood plasma.
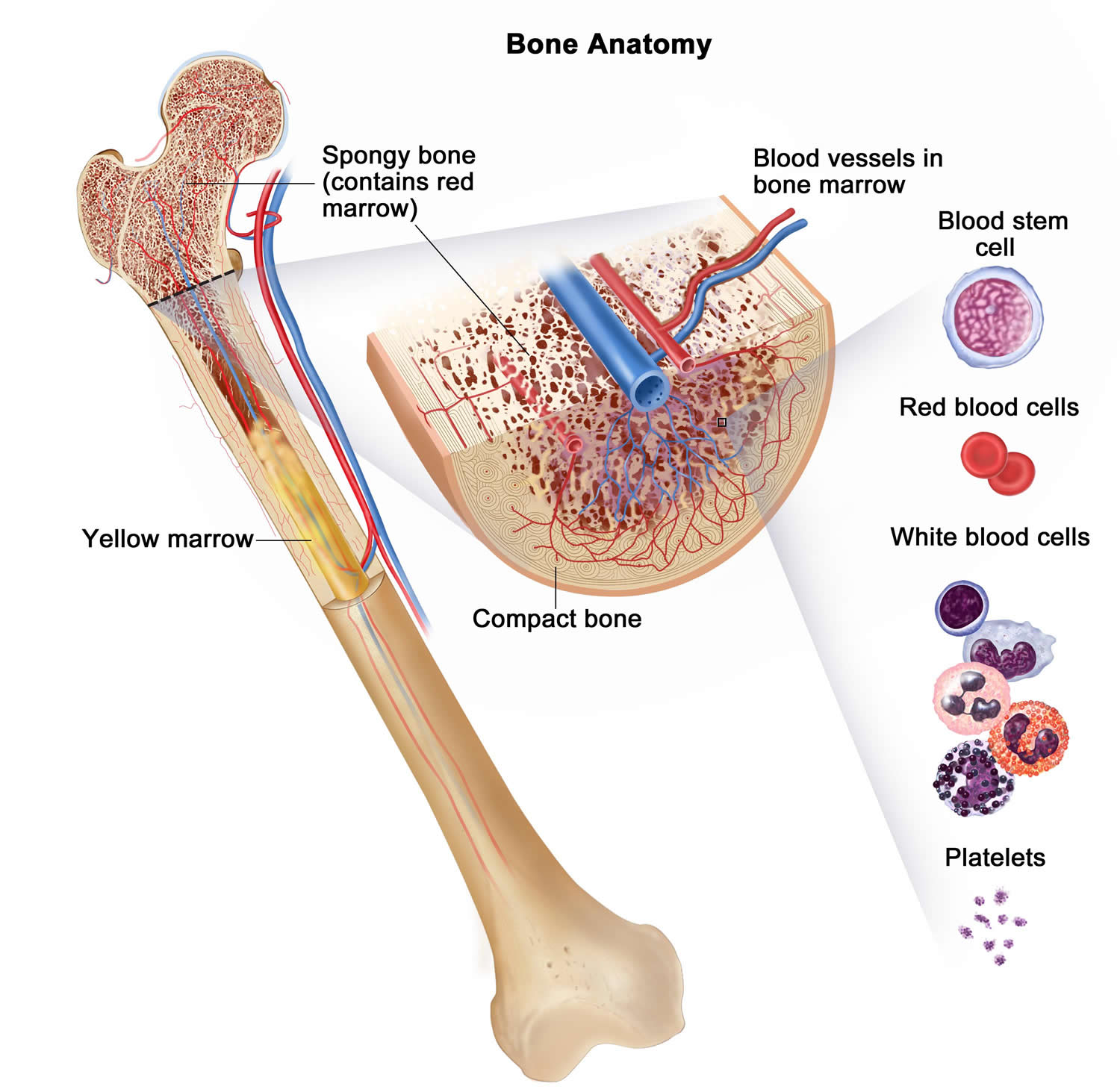
Figure 2. Bone marrow anatomy
Anatomy of the bone. The bone is made up of compact bone, spongy bone, and bone marrow. Compact bone makes up the outer layer of the bone. Spongy bone is found mostly at the ends of bones and contains red marrow. Bone marrow is found in the center of most bones and has many blood vessels. There are two types of bone marrow: red and yellow. Red marrow contains blood stem cells that can become red blood cells, white blood cells, or platelets. Yellow marrow is made mostly of fat.
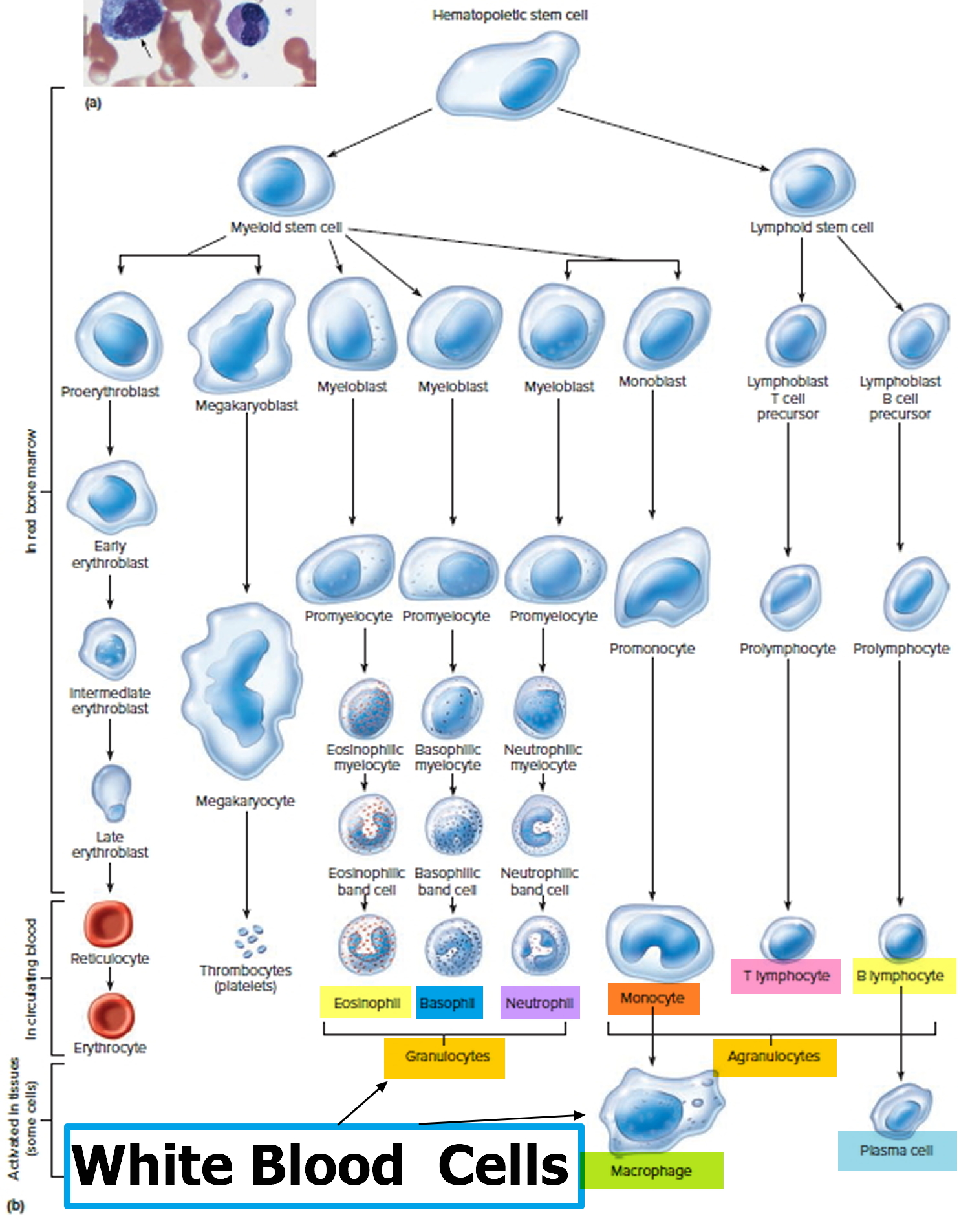
Figure 3. White blood cells development. A blood stem cell goes through several steps to become a red blood cell, platelet, or white blood cell
Figure 4. White blood cells development
Figure 5. Multiple myeloma plasma cells
There are several types of plasma cell cancers
Plasma cell neoplasms include the following:
Monoclonal gammopathy of undetermined significance (MGUS)
In monoclonal gammopathy of undetermined significance (MGUS), abnormal plasma cells produce many copies of the same antibody (a monoclonal antibody protein). However, in this type of plasma cell neoplasm, less than 10% of the bone marrow is made up of abnormal plasma cells and plasma cells do not form an actual tumor or mass and do not cause any of the other problems seen in multiple myeloma. MGUS usually does not affect a person’s health. In particular, it doesn’t cause weak bones, high calcium levels, kidney problems, or low blood counts. It’s most often found when a routine blood test finds a high level of protein in the blood and further testing shows the protein is a monoclonal antibody. In MGUS, the number of plasma cells may be increased, but they still make up less than 10% of the cells in the bone marrow.
Some people with MGUS will eventually develop multiple myeloma, lymphoma, or amyloidosis. Each year, about 1% of people with MGUS develops one of these diseases. The risk is higher in people whose protein levels are particularly high. Patients with MGUS don’t need treatment, but they are watched closely to see if they get a disease that does need to be treated, such as multiple myeloma.
Recently, scientists have studied the genes of the plasma cells in patients with MGUS. They found that the genetic make-up of these plasma cells resembles myeloma plasma cells more than it resembles that of normal plasma cells. This suggests that these cells are truly malignant, not just slow growing. Because people with MGUS are generally elderly, they may not live long enough for it to transform into myeloma.
The abnormal plasma cells make M protein, which is sometimes found during a routine blood or urine test. In most patients, the amount of M protein stays the same and there are no signs, symptoms, or health problems.
In some patients, MGUS may later become a more serious condition, such as amyloidosis, or cause problems with the kidneys, heart, or nerves. MGUS can also become cancer, such as multiple myeloma, lymphoplasmacytic lymphoma, or chronic lymphocytic leukemia.
Plasmacytoma
In this type of plasma cell neoplasm, the abnormal plasma cells (myeloma cells) are in one place and form one tumor, called a solitary plasmacytoma. Sometimes plasmacytoma can be cured. There are two types of plasmacytoma.
- In isolated plasmacytoma of bone, one plasma cell tumor is found in the bone, less than 10% of the bone marrow is made up of plasma cells, and there are no other signs of cancer. Plasmacytoma of the bone often becomes multiple myeloma.
- In extramedullary plasmacytoma, one plasma cell tumor is found in soft tissue but not in the bone or the bone marrow. Extramedullary plasmacytomas commonly form in tissues of the throat, tonsil, and paranasal sinuses.
Solitary plasmacytomas are most often treated with radiation therapy. Sometimes surgery may be used for a single extramedullary plasmacytoma. As long as no other plasmacytomas are found later on, the patient’s outlook is usually excellent. However, since many people with a solitary plasmacytoma will develop multiple myeloma, these people are watched closely for signs of this disease.
Signs and symptoms depend on where the tumor is.
- In bone, the plasmacytoma may cause pain or broken bones.
- In soft tissue, the tumor may press on nearby areas and cause pain or other problems. For example, a plasmacytoma in the throat can make it hard to swallow.
Multiple myeloma
In multiple myeloma, abnormal plasma cells (myeloma cells) build up in the bone marrow and form tumors in many bones of the body. These tumors may keep the bone marrow from making enough healthy blood cells. Normally, the bone marrow makes stem cells (immature cells) that become three types of mature blood cells:
- Red blood cells that carry oxygen and other substances to all tissues of the body.
- White blood cells that fight infection and disease.
- Platelets that form blood clots to help prevent bleeding.
As the number of myeloma cells increases, fewer red blood cells, white blood cells, and platelets are made. The myeloma cells also damage and weaken the bone.
Multiple myeloma is characterized by several features, including:
Low blood counts
In multiple myeloma, the overgrowth of plasma cells in the bone marrow can crowd out normal blood-forming cells, leading to low blood counts. This can cause anemia – a shortage of red blood cells. People with anemia become pale, weak, and fatigued. Multiple myeloma can also cause the level of platelets in the blood to become low (called thrombocytopenia). This can lead to increased bleeding and bruising. Another condition that can develop is leukopenia – a shortage of normal white blood cells. This can lead to problems fighting infections.
Bone and calcium problems
Myeloma cells also interfere with cells that help keep the bones strong. Bones are constantly being remade to keep them strong. Two major kinds of bone cells normally work together to keep bones healthy and strong. The cells that lay down new bone are called osteoblasts. The cells that break down old bone are called osteoclasts. Myeloma cells make a substance that tells the osteoclasts to speed up dissolving the bone. Since the osteoblasts do not get a signal to put down new bone, old bone is broken down without new bone to replace it. This makes the bones weak and they break easily. Fractured bones are a major problem in people with myeloma. This increase in bone break-down can also raise calcium levels in the blood.
Infections
Abnormal plasma cells do not protect the body from infections. As mentioned before, normal plasma cells produce antibodies that attack germs. For example, if you developed pneumonia, normal plasma cells would produce antibodies aimed at the specific bacteria that were causing the illness. These antibodies help the body attack and kill the bacteria. In multiple myeloma, the myeloma cells crowd out the normal plasma cells, so that antibodies to fight the infection can’t be made. The antibody made by the myeloma cells does not help fight infections. That’s because the myeloma cells are just many copies of the same plasma cell – all making copies of the same exact (or monoclonal) antibody.
Kidney problems
The antibody made by myeloma cells can harm the kidneys. This can lead to kidney damage and even kidney failure.
Monoclonal gammopathy
Having many copies of the same antibody is known as a monoclonal gammopathy. This condition can be found with a blood test. Although people with multiple myeloma have a monoclonal gammopathy, not everyone with monoclonal gammopathy has multiple myeloma. It can also occur in other diseases, such as Waldenstrom macroglobulinemia and some lymphomas. It can also occur in a disorder known as monoclonal gammopathy of undetermined significance (MGUS), which does not cause problems like multiple myeloma does. However, some people with MGUS will eventually go on to develop multiple myeloma or other diseases.
Light chain amyloidosis
Antibodies are made up of protein chains joined together – 2 short light chains and 2 longer heavy chains. In light chain amyloidosis, abnormal plasma cells make too many light chains. These light chains can deposit in tissues, where they build up. This accumulation of light chains can lead to an abnormal protein in tissues known as amyloid. The buildup of amyloid in certain organs can lead them to enlarge and not work well. For example, when amyloid builds up in the heart, it can cause an irregular heart beat and cause the heart to enlarge and get weaker. A weak heart can lead to a condition called congestive heart failure, with symptoms like shortness of breath and swelling in the legs. Amyloid in the kidneys can cause them to work poorly. This may not cause symptoms early on, but the poor kidney function may be found on blood tests. If it gets worse, amyloid in the kidney can lead to kidney failure. See Signs and Symptoms of Multiple Myeloma for more information about the signs and symptoms of light chain amyloidosis.
Other names for light chain amyloidosis include AL and primary amyloidosis. This is sometimes considered a separate disease from multiple myeloma, but because treatment is often similar to that of myeloma, we will discuss it in this document.
Light chain amyloidosis is only one of the diseases where amyloid builds ups and causes problems. Amyloidosis can also be caused by a genetic (hereditary) disease called familial amyloidosis. Long-standing (chronic) infection and/or inflammation can also cause amyloidosis. This is known as secondary or AA amyloidosis.
Smoldering multiple myeloma
Sometimes multiple myeloma does not cause any signs or symptoms. This is called smoldering multiple myeloma. It may be found when a blood or urine test is done for another condition. Signs and symptoms may be caused by multiple myeloma or other conditions. Check with your doctor if you have any of the following:
- Bone pain, especially in the back or ribs.
- Bones that break easily.
- Fever for no known reason or frequent infections.
- Easy bruising or bleeding.
- Trouble breathing.
- Weakness of the arms or legs.
- Feeling very tired.
Multiple myeloma symptoms and signs
Signs and symptoms of multiple myeloma can vary and, early in the disease, there may be none.
When signs and symptoms do occur, they can include:
- Bone pain, especially in your spine or chest
- Nausea
- Constipation
- Loss of appetite
- Mental fogginess or confusion
- Fatigue
- Frequent infections
- Weight loss
- Weakness or numbness in your legs
- Excessive thirst
A multiple myeloma tumor can damage the bone and cause hypercalcemia (too much calcium in the blood). This can affect many organs in the body, including the kidneys, nerves, heart, muscles, and digestive tract, and cause serious health problems.
Hypercalcemia may cause the following signs and symptoms:
- Loss of appetite.
- Nausea or vomiting.
- Feeling thirsty.
- Frequent urination.
- Constipation.
- Feeling very tired.
- Muscle weakness.
- Restlessness.
- Confusion or trouble thinking.
Multiple myeloma and other plasma cell neoplasms may cause a condition called amyloidosis.
In rare cases, multiple myeloma can cause peripheral nerves (nerves that are not in the brain or spinal cord) and organs to fail. This may be caused by a condition called amyloidosis. Antibody proteins build up and stick together in peripheral nerves and organs, such as the kidney and heart. This can cause the nerves and organs to become stiff and unable to work the way they should.
Amyloidosis may cause the following signs and symptoms:
- Feeling very tired.
- Purple spots on the skin.
- Enlarged tongue.
- Diarrhea.
- Swelling caused by fluid in your body’s tissues.
- Tingling or numbness in your legs and feet.
What Causes Myeloma
It’s not clear what causes myeloma.
Doctors know that myeloma begins with one abnormal plasma cell in your bone marrow — the soft, blood-producing tissue that fills in the center of most of your bones. The abnormal cell multiplies rapidly.
Because cancer cells don’t mature and then die as normal cells do, they accumulate, eventually overwhelming the production of healthy cells. In the bone marrow, myeloma cells crowd out healthy white blood cells and red blood cells, leading to fatigue and an inability to fight infections.
The myeloma cells continue trying to produce antibodies, as healthy plasma cells do, but the myeloma cells produce abnormal antibodies that the body can’t use. Instead, the abnormal antibodies (monoclonal proteins, or M proteins) build up in the body and cause problems such as damage to the kidneys. Cancer cells can also cause damage to the bones that increases the risk of broken bones.
A connection with monoclonal gammopathy of undetermined significance (MGUS)
Multiple myeloma almost always starts out as a relatively benign condition called monoclonal gammopathy of undetermined significance (MGUS).
In the United States, about 3 percent of people older than age 50 have MGUS. Each year, about 1 percent of people with MGUS develop multiple myeloma or a related cancer.
MGUS, like multiple myeloma, is marked by the presence of M proteins — produced by abnormal plasma cells — in your blood. However, in MGUS, the levels of M proteins are lower and no damage to the body occurs.
Risk factors for myeloma
Factors that may increase your risk of multiple myeloma include:
- Increasing age. Your risk of multiple myeloma increases as you age, with most people diagnosed in their mid-60s.
- Male sex. Men are more likely to develop the disease than are women.
- Black race. Black people are about twice as likely to develop multiple myeloma as are white people.
- Family history of multiple myeloma. If a brother, sister or parent has multiple myeloma, you have an increased risk of the disease.
- Personal history of a monoclonal gammopathy of undetermined significance (MGUS). Every year 1 percent of the people with MGUS in the United States develop multiple myeloma.
- Being exposed to radiation or certain chemicals.
Complications of multiple myeloma
Complications of multiple myeloma include:
- Frequent infections. Myeloma cells inhibit your body’s ability to fight infections.
- Bone problems. Multiple myeloma can also affect your bones, leading to bone pain, thinning bones and broken bones.
- Reduced kidney function. Multiple myeloma may cause problems with kidney function, including kidney failure. Higher calcium levels in the blood related to eroding bones can interfere with your kidneys’ ability to filter your blood’s waste. The proteins produced by the myeloma cells can cause similar problems.
- Low red blood cell count (anemia). As myeloma cells crowd out normal blood cells, multiple myeloma can also cause anemia and other blood problems.
Multiple myeloma prognosis
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis (chance of recovery) depends on the following:
- The type of plasma cell neoplasm.
- The stage of the disease.
- Whether a certain immunoglobulin (antibody) is present.
- Whether there are certain genetic changes.
- Whether the kidney is damaged.
- Whether the cancer responds to initial treatment or recurs (comes back).
Treatment options depend on the following:
- The type of plasma cell neoplasm.
- The age and general health of the patient.
- Whether there are signs, symptoms, or health problems, such as kidney failure or infection, related to the disease.
- Whether the cancer responds to initial treatment or recurs (comes back).
Multiple Myeloma Diagnosis
In some cases, your doctor may detect multiple myeloma accidentally when you undergo a blood test for some other condition. In other cases, your doctor may suspect multiple myeloma based on your signs and symptoms.
Tests and procedures used to diagnose multiple myeloma include:
- Blood tests. Laboratory analysis of your blood may reveal the M proteins produced by myeloma cells. Another abnormal protein produced by myeloma cells — called beta-2-microglobulin — may be detected in your blood and give your doctor clues about the aggressiveness of your myeloma.
Additionally, blood tests to examine your kidney function, blood cell counts, calcium levels and uric acid levels can give your doctor clues about your diagnosis.
- Urine tests. Analysis of your urine may show M proteins, which are referred to as Bence Jones proteins when they’re detected in urine.
Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of certain substances. An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. A higher than normal amount of protein may be a sign of multiple myeloma.
- Examination of your bone marrow. Your doctor may remove a sample of bone marrow for laboratory testing. The sample is collected with a long needle inserted into a bone (bone marrow aspiration and biopsy).
The following test may be done on the sample of tissue removed during the bone marrow aspiration and biopsy:
Cytogenetic analysis : A test in which cells in a sample of bone marrow are viewed under a microscope to look for certain changes in the chromosomes. Other tests, such as fluorescence in situ hybridization (FISH) and flow cytometry, may also be done to look for certain changes in the chromosomes to understand their genetic abnormalities. Tests are also done to measure the rate at which the myeloma cells are dividing.
- Imaging tests. Imaging tests may be recommended to detect bone problems associated with multiple myeloma. Tests may include an X-ray, MRI, CT or positron emission tomography (PET).
Skeletal bone survey: In a skeletal bone survey, x-rays of all the bones in the body are taken. The x-rays are used to find areas where the bone is damaged. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging (NMRI). An MRI of the spine and pelvis may be used to find areas where the bone is damaged.
CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, such as the spine, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
PET-CT scan : A procedure that combines the pictures from a positron emission tomography (PET) scan and a computed tomography (CT) scan. The PET and CT scans are done at the same time with the same machine. The combined scans give more detailed pictures of areas inside the body, such as the spine, than either scan gives by itself.
Multiple Myeloma Stages
After multiple myeloma has been diagnosed, tests are done to find out the amount of cancer in the body.
The process used to find out the amount of cancer in the body is called staging. It is important to know the stage in order to plan treatment. The following tests and procedures may be used in the staging process:
- Skeletal bone survey: In a skeletal bone survey, x-rays of all the bones in the body are taken. The x-rays are used to find areas where the bone is damaged. An x-ray is a type of energy beam that can go through the body and onto film, making a picture of areas inside the body.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body, such as the bone marrow. This procedure is also called nuclear magnetic resonance imaging (NMRI).
- Bone densitometry: A procedure that uses a special type of x-ray to measure bone density.
The stage of multiple myeloma is based on the levels of beta-2-microglobulin and albumin in the blood.
Beta-2-microglobulin and albumin are found in the blood. Beta-2-microglobulin is a protein found on plasma cells. Albumin makes up the biggest part of the blood plasma. It keeps fluid from leaking out of blood vessels. It also brings nutrients to tissues, and carries hormones, vitamins, drugs, and other substances, such as calcium, all through the body. In the blood of patients with multiple myeloma, the amount of beta-2-microglobulin is increased and the amount of albumin is decreased.
The following stages are used for multiple myeloma:
Stage I multiple myeloma
In stage I multiple myeloma, the blood levels are as follows:
- beta-2-microglobulin level is lower than 3.5 mg/L; and
- albumin level is 3.5 g/dL or higher.
Stage II multiple myeloma
- In stage II multiple myeloma, the blood levels are in between the levels for stage I and stage III.
- Stage III multiple myeloma
In stage III multiple myeloma, the blood level of beta-2-microglobulin is 5.5 mg/L or higher and the patient also has one of the following:
- high levels of lactate dehydrogenase (LDH); or
- certain changes in the chromosomes.
Assigning a stage and a risk category
If tests indicate you have multiple myeloma, your doctor will use the information gathered from the diagnostic tests to classify your disease as stage I, stage II or stage III. Stage I indicates a less aggressive disease, and stage III indicates an aggressive disease that may affect bone, kidneys and other organs.
Your multiple myeloma may also be assigned a risk category, which indicates the aggressiveness of your disease.
Your multiple myeloma stage and risk category help your doctor understand your prognosis and your treatment options.
Multiple myeloma treatment
If you’re experiencing symptoms, treatment can help relieve pain, control complications of the disease, stabilize your condition and slow the progress of multiple myeloma.
Immediate treatment may not be necessary
If you have multiple myeloma but aren’t experiencing any symptoms (also known as smoldering multiple myeloma), you may not need treatment. However, your doctor will regularly monitor your condition for signs that the disease is progressing. This may involve periodic blood and urine tests.
If you develop signs and symptoms or your multiple myeloma shows signs of progression, you and your doctor may decide to begin treatment.
Patients without signs or symptoms may not need treatment. When signs or symptoms appear, the treatment of multiple myeloma may be done in phases:
Induction therapy
This is the first phase of treatment. Its goal is to reduce the amount of disease, and may include one or more of the following:
- Corticosteroid therapy.
- Biologic therapy with lenalidomide, pomalidomide, or thalidomide therapy.
- Targeted therapy with proteasome inhibitors (bortezomib, carfilzomib, and ixazomib) or monoclonal antibodies (daratumumab and elotuzumab).
- Chemotherapy.
- Histone deacetylase inhibitor therapy with panobinostat.
- A clinical trial of different combinations of treatment.
Consolidation chemotherapy
This is the second phase of treatment. Treatment in the consolidation phase is to kill any remaining cancer cells. High-dose chemotherapy is followed by either:
- one autologous stem cell transplant, in which the patient’s stem cells from the blood or bone marrow are used; or
- two autologous stem cell transplants followed by an autologous or allogeneic stem cell transplant, in which the patient receives stem cells from the blood or bone marrow of a donor; or
- one allogeneic stem cell transplant.
Maintenance therapy
After the initial treatment, maintenance therapy is often given to help keep the disease in remission for a longer time. Several types of treatment are being studied for this use, including the following:
- Chemotherapy.
- Biologic therapy with interferon.
- Corticosteroid therapy.
- Lenalidomide therapy.
- Targeted therapy with a proteasome inhibitor (bortezomib).
Refractory Multiple Myeloma
Treatment of refractory multiple myeloma may include the following:
- Watchful waiting for patients whose disease is stable.
- A different treatment than treatment already given, for patients whose tumor kept growing during treatment. (See Multiple Myeloma treatment options.)
- A clinical trial of a new therapy.
Treatment options for myeloma
Targeted therapy
Targeted therapy is a treatment that uses drugs or other substances to identify and attack specific cancer cells without harming normal cells. Several types of targeted therapy may be used to treat multiple myeloma and other plasma cell neoplasms.
Proteasome inhibitor therapy is a cancer treatment that blocks the action of proteasomes in cancer cells. A proteasome is a protein that removes other proteins no longer needed by the cell. When the proteins are not removed from the cell, they build up and may cause the cancer cell to die. Bortezomib (Velcade), carfilzomib (Kyprolis) and ixazomib (Ninlaro) are proteasome inhibitors used in the treatment of multiple myeloma and other plasma cell neoplasms. They block the action of a substance in myeloma cells that breaks down proteins. This action causes myeloma cells to die. Targeted-therapy drugs may be administered through a vein in your arm or in pill form.
Monoclonal antibody therapy is a cancer treatment that uses antibodies made in the laboratory, from a single type of immune system cell. These antibodies can identify substances on cancer cells or normal substances that may help cancer cells grow. The antibodies attach to the substances and kill the cancer cells, block their growth, or keep them from spreading. Monoclonal antibodies are given by infusion. They may be used alone or to carry drugs, toxins, or radioactive material directly to cancer cells. Daratumumab and elotuzumab are monoclonal antibodies used in the treatment of multiple myeloma and other plasma cell neoplasms.
Histone deacetylase (HDAC) inhibitor therapy is a type of targeted therapy that blocks enzymes needed for cell division and may stop the growth of cancer cells. Panobinostat is an HDAC inhibitor used in the treatment of multiple myeloma and other plasma cell neoplasms.
Biological therapy
Biologic therapy is a treatment that uses the patient’s immune system to fight cancer. Substances made by the body or made in a laboratory are used to boost, direct, or restore the body’s natural defenses against cancer. This type of cancer treatment is also called biotherapy or immunotherapy.
Immunomodulators are a type of biologic therapy. The drugs thalidomide (Thalomid), lenalidomide (Revlimid) and pomalidomide (Pomalyst) are immunomodulators enhance the immune system cells that identify and attack cancer cells. They are used to treat multiple myeloma and other plasma cell neoplasms. These medications are commonly taken in pill form.
Interferon is a type of biologic therapy. It affects the division of cancer cells and can slow tumor growth.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping them from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy). The way the chemotherapy is given depends on the type and stage of the cancer being treated.
High-dose chemotherapy with stem cell transplant
This treatment is a way of giving high doses of chemotherapy and replacing blood -forming cells destroyed by the cancer treatment. Stem cells (immature blood cells) are removed from the blood or bone marrow of the patient (autologous transplant) or a donor (allogeneic transplant) and are frozen and stored. After the chemotherapy is completed, the stored stem cells are thawed and given back to the patient through an infusion. These reinfused stem cells grow into (and restore) the body’s blood cells.
Corticosteroids
Corticosteroids, such as prednisone and dexamethasone, regulate the immune system to control inflammation in the body. They are also active against myeloma cells. Corticosteroids can be taken in pill form or administered through a vein in your arm.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
The way the radiation therapy is given depends on the type and stage of the cancer being treated. External radiation therapy is used to treat plasma cell neoplasms.
Bone marrow transplant
A bone marrow transplant, also known as a stem cell transplant, is a procedure to replace your diseased bone marrow with healthy bone marrow.
Before a bone marrow transplant, blood-forming stem cells are collected from your blood. You then receive high doses of chemotherapy to destroy your diseased bone marrow. Then your stem cells are infused into your body, where they travel to your bones and begin rebuilding your bone marrow.
Radiation therapy. This treatment uses beams of energy, such as X-rays and protons, to damage myeloma cells and stop their growth. Radiation therapy may be used to quickly shrink myeloma cells in a specific area — for instance, when a collection of abnormal plasma cells form a tumor (plasmacytoma) that’s causing pain or destroying a bone.
Surgery
Surgery to remove the tumor may be done and is usually followed by radiation therapy. Treatment given after the surgery, to lower the risk that the cancer will come back, is called adjuvant therapy.
Watchful waiting
Watchful waiting is closely monitoring a patient’s condition without giving any treatment until signs or symptoms appear or change.
New combinations of therapies
Clinical trials are studying different combinations of biologic therapy, chemotherapy, steroid therapy, and drugs. New treatment regimens using thalidomide or lenalidomide are also being studied.
How treatments are used
Which combination of treatments you’re likely to receive will depend on whether you’re considered a good candidate for bone marrow transplant. This depends on the risk of your disease progressing, your age and your overall health.
If you’re considered a candidate for bone marrow transplant, your initial therapy will likely include a combination of treatments, such as targeted therapy, biological therapy, corticosteroids and, sometimes, chemotherapy.
Your stem cells will likely be collected after you’ve undergone a few months of treatment. You may undergo the bone marrow transplant soon after your cells are collected or the transplant may be delayed until after a relapse, if it occurs. In some cases, doctors recommend two bone marrow transplants for people with multiple myeloma.
After your bone marrow transplant, you’ll likely receive targeted therapy or biological therapy as a maintenance treatment to prevent a recurrence of myeloma.
If you’re not considered a candidate for bone marrow transplant, your initial therapy will likely include chemotherapy combined with corticosteroids, targeted therapy or biological therapy.
If your myeloma recurs or doesn’t respond to treatment, your doctor may recommend repeating another course of the treatment that initially helped you. Another option is trying one or more of the other treatments typically used as first line therapy, either alone or in combination.
Research on a number of new treatment options is ongoing, and you may be eligible for a clinical trial in order to gain access to those experimental treatments. Talk to your doctor about what clinical trials may be available to you.
Treating complications
Because multiple myeloma can cause a number of complications, you may also need treatment for those specific conditions. For example:
- Bone pain. Pain medications, radiation therapy and surgery may help control bone pain.
- Kidney complications. People with severe kidney damage may need dialysis.
- Infections. Your doctor may recommend certain vaccines to prevent infections, such as the flu and pneumonia.
- Bone loss. Your doctor may recommend medications called bisphosphonates, such as pamidronate (Aredia) or zoledronic acid (Zometa), to help prevent bone loss.
- Anemia. If you have persistent anemia, your doctor may recommend medications to increase your red blood cell count.
Supportive care
Supportive care is given to lessen the problems caused by the disease or its treatment.
This therapy controls problems or side effects caused by the disease or its treatment, and improves quality of life. Supportive care is given to treat problems caused by multiple myeloma and other plasma cell neoplasms.
Supportive care may include the following:
- Plasmapheresis: If the blood becomes thick with extra antibody proteins and interferes with circulation, plasmapheresis is done to remove extra plasma and antibody proteins from the blood. In this procedure blood is removed from the patient and sent through a machine that separates the plasma (the liquid part of the blood) from the blood cells. The patient’s plasma contains the unneeded antibodies and is not returned to the patient. The normal blood cells are returned to the bloodstream along with donated plasma or a plasma replacement. Plasmapheresis does not keep new antibodies from forming.
- High-dose chemotherapy with stem cell transplant: If amyloidosis occurs, treatment may include high-dose chemotherapy followed by stem cell transplant using the patient’s own stem cells.
- Biologic therapy: Biologic therapy with thalidomide, lenalidomide, or pomalidomide is given to treat amyloidosis.
- Targeted therapy: Targeted therapy with proteasome inhibitors is given to decrease how much immunoglobulin M is in the blood and treat amyloidosis.
- Radiation therapy: Radiation therapy is given for bone lesions of the spine.
- Chemotherapy: Chemotherapy is given to reduce back pain from osteoporosis or compression fractures of the spine.
- Bisphosphonate therapy: Bisphosphonate therapy is given to slow bone loss and reduce bone pain. See the following PDQ summaries for more information on bisphosphonates and problems related to their use:
- Cancer Pain
- Oral Complications of Chemotherapy and Head/Neck Radiation
Patients may want to take part in a clinical trial
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. For more information on trials at the Clinical Center, see National Cancer Institute Center for Cancer Research 4 and Developmental Therapeutics Clinic 5.
Many of today’s standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Alternative medicine
No alternative medicines have been found to treat multiple myeloma. But alternative medicine may help you cope with the stress and side effects of myeloma and myeloma treatment.
Talk to your doctor about your options, such as:
- Art therapy
- Exercise
- Meditation
- Music therapy
- Relaxation exercises
- Spirituality
Talk with your doctor before trying any of these techniques to make sure they don’t pose any risks for you.
Coping and support
A cancer diagnosis can be shocking and devastating. With time, you’ll find ways to cope with the stress and uncertainty of living with cancer. Until you find what works best for you, consider trying to:
Learn enough to make decisions about your care. Learn enough about multiple myeloma so that you’re able to participate in decisions about your treatment and care. Ask your doctor about your treatment options and their side effects.
- You may find additional help gathering information through your local library and online. Start with the National Cancer Institute 6 and the International Myeloma Foundation 7.
Maintain a strong support system. Having a strong support system can help you cope with issues and anxieties that might occur. Your friends and family may be willing to offer support.
You might also find that support from a formal support group or others coping with cancer may be helpful. Friends you meet in support groups may be willing to share practical advice for coping with cancer and cancer treatment. Support groups are also available online.
Set reasonable goals. Having goals helps you feel in control and can give you a sense of purpose. But don’t choose goals you can’t possibly reach. You may not be able to work a 40-hour week, for example, but you may be able to work at least part time. In fact, many people find that continuing to work during cancer treatment can be helpful in maintaining some normalcy.
Take time for yourself. Eating well, relaxing and getting enough rest can help combat the stress and fatigue of cancer. Also, plan ahead for the downtimes when you may need to rest more or limit what you do.
Treatment of Monoclonal Gammopathy of Undetermined Significance
Treatment of monoclonal gammopathy of undetermined significance (MGUS) is usually watchful waiting. Regular blood tests to check the level of M protein in the blood and physical exams to check for signs or symptoms of cancer will be done.
Treatment of Isolated Plasmacytoma of Bone
Treatment of isolated plasmacytoma of bone is usually radiation therapy to the bone lesion.
Treatment of Extramedullary Plasmacytoma
Treatment of extramedullary plasmacytoma may include the following:
- Radiation therapy to the tumor and nearby lymph nodes.
- Surgery, usually followed by radiation therapy.
- Watchful waiting after initial treatment, followed by radiation therapy, surgery, or chemotherapy if the tumor grows or causes signs or symptoms.
- https://cancerstatisticscenter.cancer.org/#!/cancer-site/Myeloma[↩][↩][↩]
- Continued improvement in survival in multiple myeloma: changes in early mortality and outcomes in older patients. Kumar SK, Dispenzieri A, Lacy MQ, Gertz MA, Buadi FK, Pandey S, Kapoor P, Dingli D, Hayman SR, Leung N, Lust J, McCurdy A, Russell SJ, Zeldenrust SR, Kyle RA, Rajkumar SV. Leukemia. 2014 May; 28(5):1122-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4000285/[↩]
- Dingli D, Ailawadhi S, Bergsagel PL, et al. Therapy for Relapsed Multiple Myeloma: Guidelines From the Mayo Stratification for Myeloma and Risk-Adapted Therapy. Mayo Clinic proceedings. 2017;92(4):578-598. doi:10.1016/j.mayocp.2017.01.003. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5554888/[↩]
- National Cancer Institute. https://ccr.cancer.gov/clinical-trials/patients[↩]
- Developmental Therapeutics Clinic. https://dtc.cancer.gov/trials/search.htm[↩]
- National Cancer Institute. https://www.cancer.gov/types/myeloma/patient/myeloma-treatment-pdq[↩]
- International Myeloma Foundation. https://www.myeloma.org/[↩]