Contents
What is myocardial ischemia
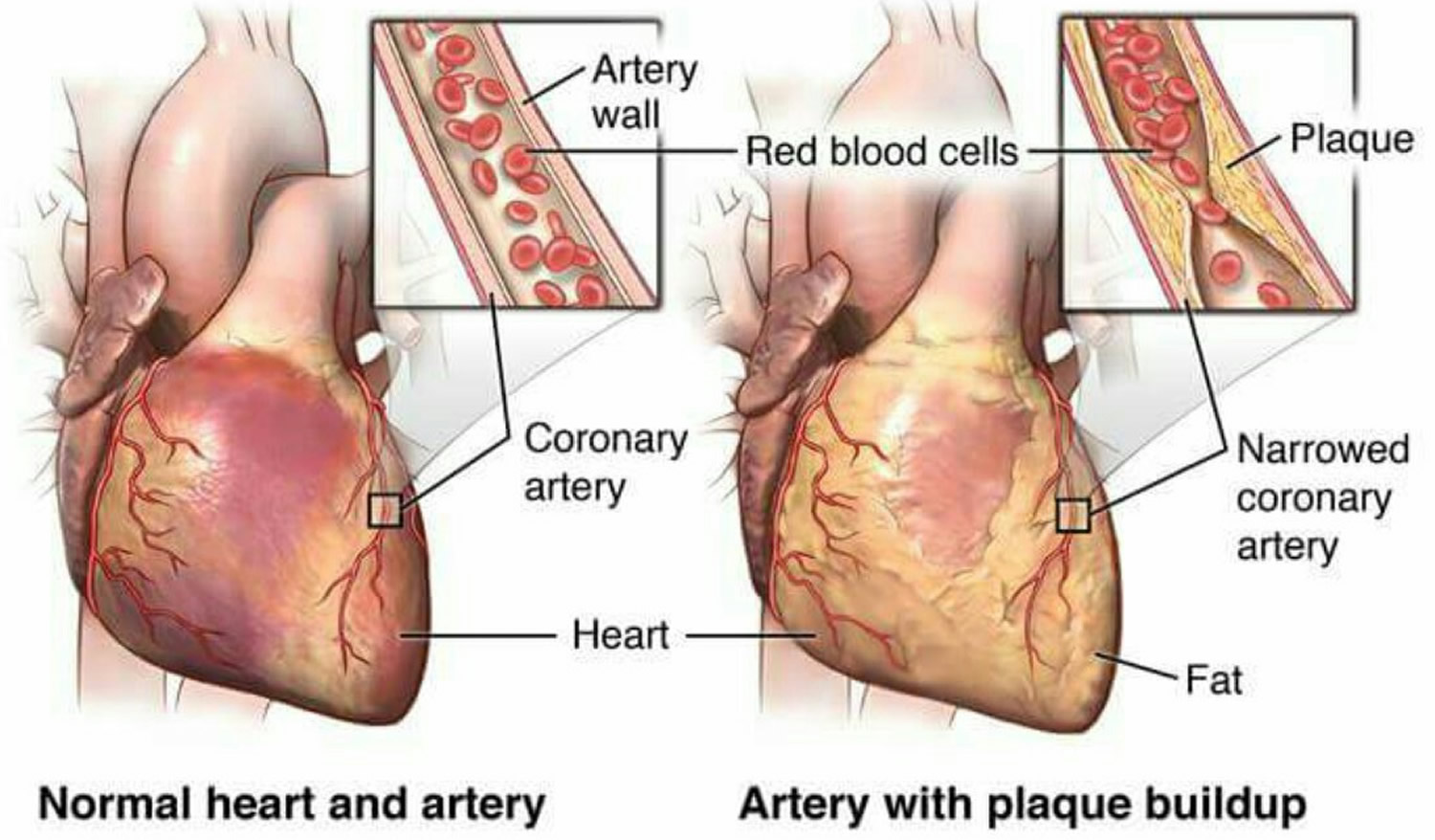
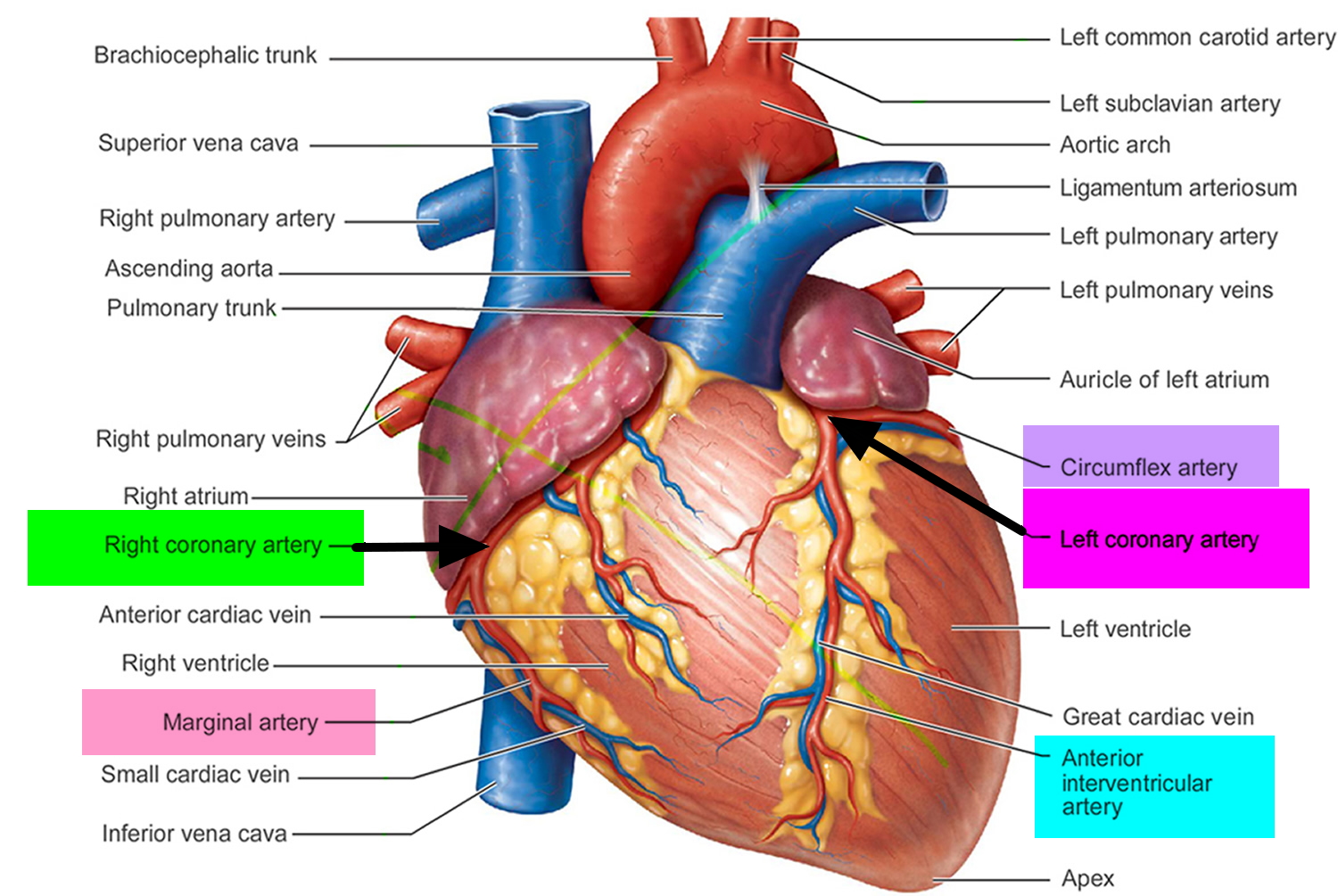
Myocardial ischemia occurs when blood flow to your heart is reduced, preventing the heart muscle from receiving enough oxygen. Myocardial ischemia is a disorder that is usually caused by partial or complete blockage of your heart’s coronary arteries, which is also known as atherosclerotic coronary artery disease (coronary heart disease) (see Figures 1 and 2). Coronary artery disease is the leading cause of death worldwide, and it is the second most common cause of emergency department visits in the United States. Atherosclerosis is a process in which blood, fats such as cholesterol and other substances build up on your artery walls. Eventually, deposits called plaques may form. The deposits may narrow — or block — your arteries. These plaques can also rupture, causing a blood clot.
Myocardial ischemia, also called cardiac ischemia, can damage your heart muscle, reducing its ability to pump efficiently. A sudden, severe blockage of a coronary artery can lead to a heart attack. Myocardial ischemia might also cause serious abnormal heart rhythms.
Angina is chest pain that occurs when the blood supply to the muscles of the heart is restricted.
The pain and discomfort of angina feels like a dull, heavy or tight pain in the chest that can sometimes spread to the left arm, neck, jaw or back.
The pain is usually triggered by physical activity or stress and typically only lasts for a few minutes. This is often referred to as an angina attack.
Diagnosing myocardial ischemia prior to a heart attack is important because ischemic heart disease is responsible for approximately 14% of all deaths worldwide. Approximately 1.5 million Americans will have a heart attack this year as a result of myocardial ischemia; about 500,000 of those will be fatal. For approximately one third of patients, coronary heart disease is not diagnosed until after a heart attack (myocardial infarction) occurs. Fortunately, treating known coronary heart disease has tremendous benefits. Both coronary artery revascularization and medical therapies significantly reduce the morbidity and mortality rates of coronary heart disease. Since coronary heart disease is common and deadly, but treatable if detected early, early diagnosis of the condition is critical.
Treatment for myocardial ischemia involves improving blood flow to the heart muscle. Treatment may include medications, a procedure to open blocked arteries or bypass surgery.
Making heart-healthy lifestyle choices is important in treating and preventing myocardial ischemia.
Seek emergency care if you have prolonged or severe chest pain.
An ambulance is the best and safest way to get to the hospital. Emergency medical services (EMS) personnel can check how you are doing and start life-saving medicines and other treatments right away. People who arrive by ambulance often receive faster treatment at the hospital.
Figure 1. Heart coronary arteries
Figure 2. Development of atherosclerosis
Myocardial ischemia vs myocardial infarction
Myocardial infarction (MI) is a medical term for a heart attack. Myocardial infarction (heart attack) is a serious medical emergency in which the supply of blood to the heart is suddenly blocked, usually by a blood clot. Without the blood coming in, the heart can’t get oxygen. If not treated quickly, the heart muscle begins to die. But if you do get quick treatment, you may be able prevent or limit damage to the heart muscle. That’s why it’s important to know the symptoms of a myocardial infarction (heart attack). A myocardial infarction (heart attack) is a medical emergency. Dial your local emergency number and ask for an ambulance if you suspect a heart attack. You should call, even if you are not sure that it is a heart attack. Every minute matters if you’re having a heart attack!
- An ambulance is the best and safest way to get to the hospital. Emergency medical services (EMS) personnel can check how you are doing and start life-saving medicines and other treatments right away. People who arrive by ambulance often receive faster treatment at the hospital.
A lack of blood to the heart may seriously damage the heart muscle and can be life-threatening.
- When a heart attack happens, delay in treatment can be deadly.
- While waiting for an ambulance, it may help to chew and then swallow a tablet of aspirin (ideally 300mg) – as long as the person having a heart attack isn’t allergic to aspirin.
The aspirin helps to thin the blood and reduce the risk of a heart attack.
Each year more than 1.5 million Americans have a heart attack (myocardial infarction) 1 and about 500,000 of those will be fatal.
The most common symptoms of a myocardial infarction (heart attack) in men and women are:
- Chest discomfort or pain. It is often in center or left side of the chest. It usually lasts more than a few minutes. It may go away and come back. It can feel like pressure, squeezing, fullness, or pain. It also can feel like heartburn or indigestion.
- Shortness of breath. Sometimes this is your only symptom. You may get it before or during the chest discomfort. It can happen when you are resting or doing a little bit of physical activity.
- Discomfort in the upper body. You may feel pain or discomfort in one or both arms, the back, shoulders, neck, jaw, or upper part of the stomach.
You may also have other symptoms, such as nausea, vomiting, dizziness, and lightheadedness. You may break out in a cold sweat. Sometimes women will have different symptoms then men. For example, women are more likely to feel tired for no reason.
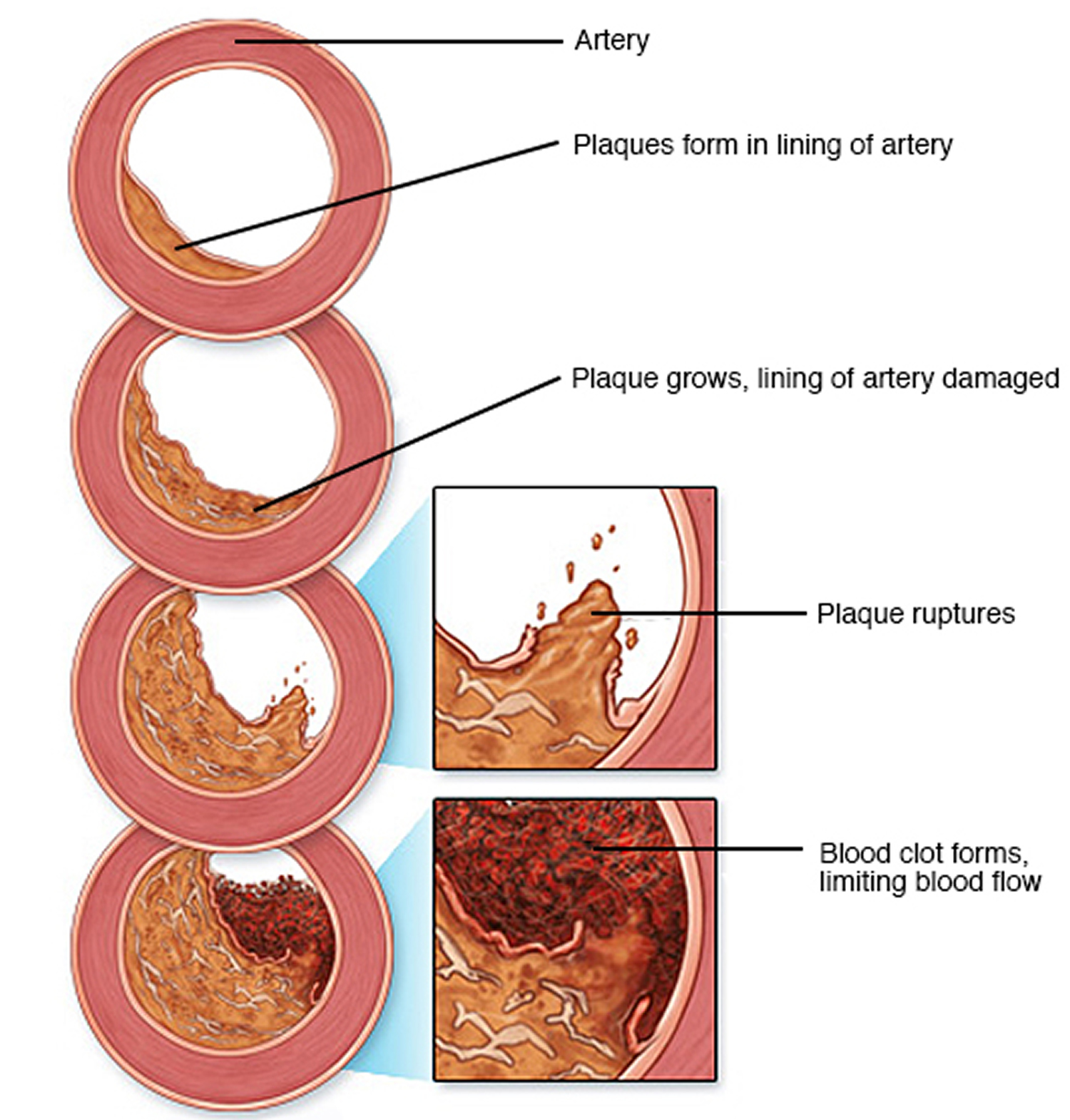
Figure 3. Myocardial infarction (heart attack)
Not all heart attacks begin with the sudden, crushing chest pain often seen on TV or in the movies, or other common symptoms such as chest discomfort. The symptoms of a heart attack can vary from person to person. Some people can have few symptoms and are surprised to learn they’ve had a heart attack. If you’ve already had a heart attack, your symptoms may not be the same for another one. It is important for you to know the most common symptoms of a heart attack and also remember these facts:
- Heart attacks can start slowly and cause only mild pain or discomfort. Symptoms can be mild or more intense and sudden. Symptoms also may come and go over several hours.
- People who have high blood sugar (diabetes) may have no symptoms or very mild ones.
- The most common symptom, in both women and men, is chest pain or discomfort. But women also are somewhat more likely to have shortness of breath, nausea and vomiting, unusual tiredness (sometimes for days), and pain in the back, shoulders, and jaw.
The most common cause of heart attacks is coronary artery disease (coronary heart disease). With coronary heart disease, there is a buildup of cholesterol and other material, called plaque, on their inner walls or the arteries. This is atherosclerosis. It can build up for years. Eventually an area of plaque can rupture (break open). A blood clot can form around the plaque and block the artery.
A less common cause of heart attack is a severe spasm (tightening) of a coronary artery. The spasm cuts off blood flow through the artery.
At the hospital, health care providers make a diagnosis based on your symptoms, blood tests, and different heart health tests. Treatments may include medicines and medical procedures such as coronary angioplasty. After a heart attack, cardiac rehabilitation and lifestyle changes can help you recover.
Myocardial ischemia causes
Myocardial ischemia occurs when the blood flow through one or more of your coronary arteries is decreased. The low blood flow decreases the amount of oxygen your heart muscle receives.
Myocardial ischemia can develop slowly as arteries become blocked over time. Or it can occur quickly when an artery becomes blocked suddenly.
Conditions that can cause myocardial ischemia include:
- Coronary artery disease (atherosclerosis). Plaques made up mostly of cholesterol build up on your artery walls and restrict blood flow. Atherosclerosis is the most common cause of myocardial ischemia.
- Blood clot. The plaques that develop in atherosclerosis can rupture, causing a blood clot. The clot might block an artery and lead to sudden, severe myocardial ischemia, resulting in a heart attack. Rarely, a blood clot might travel to the coronary artery from elsewhere in the body.
- Coronary artery spasm. This temporary tightening of the muscles in the artery wall can briefly decrease or even prevent blood flow to part of the heart muscle. Coronary artery spasm is an uncommon cause of myocardial ischemia.
Chest pain associated with myocardial ischemia can be triggered by:
- Physical exertion
- Emotional stress
- Cold temperatures
- Cocaine use
Risk factors for myocardial ischemia
Factors that can increase your risk of developing myocardial ischemia include:
- Tobacco. Smoking and long-term exposure to secondhand smoke can damage the inside walls of arteries. The damage can allow deposits of cholesterol and other substances to collect and slow blood flow in the coronary arteries. Smoking also increases the risk of blood clots in your coronary arteries.
- Diabetes. Type 1 and type 2 diabetes are linked to an increased risk of myocardial ischemia, heart attack and other heart problems.
- High blood pressure. Over time, high blood pressure can accelerate atherosclerosis, resulting in damage to the coronary arteries.
- High blood cholesterol level. Cholesterol is a major part of the deposits that can narrow your coronary arteries. A high level of “bad” (low-density lipoprotein, or LDL) cholesterol in your blood may be due to an inherited condition or a diet high in saturated fats and cholesterol.
- High blood triglyceride level. Triglycerides, another type of blood fat, may also contribute to atherosclerosis.
- Obesity. Obesity is associated with diabetes, high blood pressure and high blood cholesterol levels.
- Waist circumference. A waist measurement of more than 35 inches (89 centimeters) for women and 40 inches (102 cm) in men increases the risk of high blood pressure and heart disease.
- Lack of physical activity. An inactive lifestyle contributes to obesity and is associated with higher cholesterol and triglyceride levels. People who get regular aerobic exercise have better cardiovascular fitness, which is associated with a decreased risk of myocardial ischemia and heart attack. Exercise also lowers high blood pressure.
Myocardial ischemia complications
Myocardial ischemia can lead to serious complications, including:
- Myocardial infarction (heart attack). If a coronary artery becomes completely blocked, the lack of blood and oxygen can lead to a heart attack that destroys part of the heart muscle. The damage can be serious and sometimes fatal.
- Irregular heart rhythm (arrhythmia). An abnormal heart rhythm can weaken your heart and may be life-threatening.
- Heart failure. Myocardial ischemia can damage the heart muscle, reducing its ability to effectively pump blood to the rest of your body. Over time, this damage might lead to heart failure.
Myocardial ischemia prevention
The same lifestyle habits that can help treat myocardial ischemia can also help prevent it from developing in the first place. Leading a heart-healthy lifestyle can help keep your arteries strong, elastic and smooth, and allow for maximum blood flow.
Myocardial ischemia signs and symptoms
Some people who have ischemia don’t experience any signs or symptoms (silent ischemia).
When signs and symptoms occur, the most common is chest pressure or pain, typically on the left side of the body (angina pectoris). Other signs and symptoms — which might be experienced more commonly by women, older people and people with diabetes — include:
- Neck or jaw pain
- Shoulder or arm pain
- Chest pressure or pain precipitated by exertion, eating, exposure to cold, or emotional stress, lasting for about 1-5 minutes and relieved by rest or nitroglycerin
- A fast heartbeat
- Shortness of breath when you are physically active
- Nausea and vomiting
- Sweating
- Fatigue
- Restlessness
Myocardial ischemia diagnosis
Your doctor will start with a medical history and physical exam. After that, your doctor might recommend:
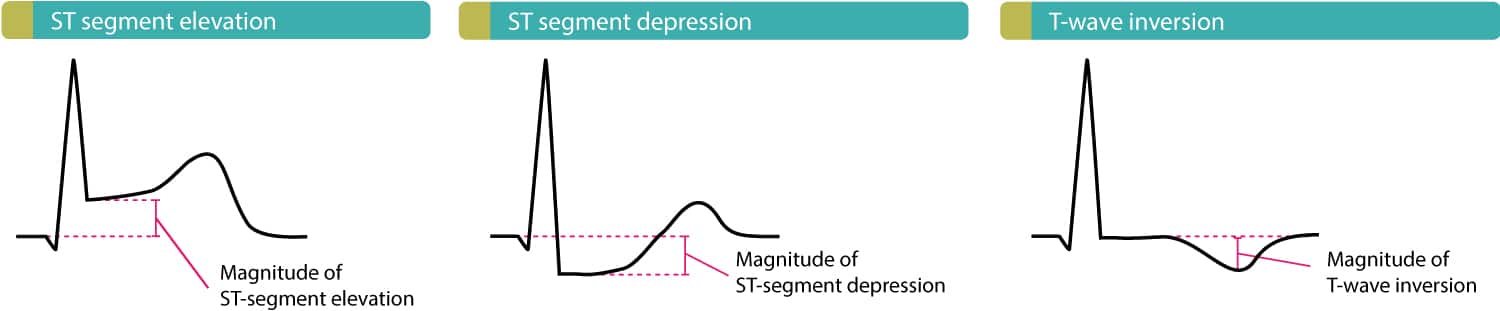
- Electrocardiogram (ECG). The electrical activity of your heart is recorded via electrodes attached to your skin. Certain abnormalities in your heart’s electrical activity may indicate myocardial ischemia.
- Echocardiogram. Sound waves directed at your heart from a wand-like device held to your chest produce video images of your heart. An echocardiogram can help identify whether an area of your heart has been damaged and isn’t pumping normally.
- Nuclear scan. Small amounts of radioactive material are injected into your bloodstream. While you exercise, the tracer is monitored as it flows through your heart and lungs —allowing blood-flow problems to be identified.
- Coronary angiography. A dye is injected into the blood vessels of your heart. An X-ray machine then takes a series of images (angiograms), offering a detailed look at the inside of your blood vessels.
- Positron emission tomography (PET) scan. A positron emission tomography (PET) scan is an imaging test that helps reveal how your tissues and organs are functioning. A PET scan uses a small amount of radioactive tracer. The tracer is given through a vein (IV). The needle is most often inserted on the inside of your elbow. The tracer travels through your blood and collects in organs and tissues. This helps the radiologist see certain areas more clearly.
- Cardiac CT scan. This test can determine if you have coronary artery calcification — a sign of coronary atherosclerosis. The heart arteries also can be seen using CT scanning (coronary CT angiogram).
- Stress test. Your heart rhythm, blood pressure and breathing are monitored while you walk on a treadmill or ride a stationary bike. Exercise makes your heart pump harder and faster than usual, so a stress test can detect heart problems that might not be noticeable otherwise.
The diagnosis of coronary heart disease can be difficult to make. Frequently, the disease is diagnosed only after the patient has had a heart attack. The symptoms of coronary heart disease range from unstable angina to no symptoms at all. Although guidelines exist for the screening of hyperlipidemia and hypertension, no screening method has been uniformly accepted for coronary heart disease. The disease occurs in both the young and the old, in both women and men, and in both patients with and patients without comorbidities.
Several studies have been designed to help the clinician determine a patient’s coronary heart disease risk level 2. With this information, the clinician can decide, with reasonable certainty, which type of workup is indicated. For the low-risk population, exercise treadmill testing alone is frequently sufficient; however, in patients with a moderate-to-high risk for coronary heart disease, an imaging study is essential along with the stress test.
The nuclear myocardial scan is the best initial imaging study for the detection of myocardial ischemia; however, in some locales, stress echocardiography is performed more often because it is more readily available and because local clinicians are better trained in echocardiography and are more comfortable with the technology. Nonetheless, the wealth of research into nuclear scanning makes a strong case for its role as the best and preferred test for detecting coronary heart disease.
The assessment of myocardial perfusion and function using positron emission tomography (PET) and hybrid positron emission tomography (PET)/CT imaging is becoming more available as the cost of the technology decreases and as positron-emitting radiopharmaceuticals become more available. Cardiac PET has the advantage of higher spatial resolution, temporal resolution, and, in many cases, a decreased radiation exposure to patients. Newer gamma cameras using simultaneous 180° acquisition appear to have the potential of offering similar benefits as PET technology but are able to use the less costly Tc-99m-based radiopharmaceuticals and Tl-201.
One potentially important physiologic parameter obtained by these newer technologies is the myocardial perfusion reserve (MPR). In patients with ischemic heart disease who undergo revascularization based on PET viability assessment with F-18 FDG, those with a low myocardial perfusion reserve were at an increased risk of adverse cardiac events 3.
Currently, nuclear myocardial scans include both perfusion and gated wall motion images. Coronary artery blood flow can be assessed, and the scans can also be used to accurately determine the left ventricular ejection fraction, the end-systolic volume of the left ventricle, regional wall motion, and wall thickening 4. In addition, solid evidence links these findings to clinical outcomes.
Myocardial ischemia ECG
Electrocardiography (ECG) is useful for evaluating persons with angina pectoris; however, findings are variable among patients.
Approximately 50% of patients with angina pectoris have normal findings after a resting ECG. However, abnormalities such as evidence for prior myocardial infarction (heart attack), intraventricular conduction delay, various degrees of atrioventricular block, arrhythmias, or ST-T–wave changes may be seen.
During an attack of angina pectoris, 50% of patients with normal findings after resting ECG show abnormalities. A 1-mm or greater depression of the ST segment below the baseline, measured 80 milliseconds from the J point, is the most characteristic change. Reversible ST-segment elevation occurs with Prinzmetal angina. Some patients with coronary artery disease may show pseudonormalization of the resting ECG ST-T–wave abnormalities during episodes of chest pain.
Exercise with ECG monitoring
Exercise with ECG monitoring alone is the initial procedure of choice in patients without baseline ST-segment abnormalities or in whom anatomic localization of ischemia is not a consideration. Note the following:
- Horizontal or down-sloping ST-segment depression of at least 1 mm, measured 80 milliseconds from the J point, is considered the characteristic ischemic response.
- ST-segment depression of more than 2 mm at a low workload or that persists for more than 5 minutes after termination of exercise and a failure of blood pressure to rise or an actual drop in blood pressure are signs of severe ischemic heart disease and a poor prognosis.
- Withhold beta-blockers for approximately 48 hours before the stress test, whenever possible. Patients on digoxin and those with LV hypertrophy with repolarization abnormalities more often show positive results. Exercise stress tests have lower sensitivity and specificity in women and in patients with left bundle-branch block.
- Pharmacologic agents (eg, dobutamine, dipyridamole, adenosine) can be used in patients who are unable to exercise.
Ambulatory ECG monitoring
Ambulatory ECG monitoring can be used for diagnostic purposes in patients with chest pain suggestive of Prinzmetal angina but is primarily used to evaluate the frequency of silent ischemia. Silent ischemia has been shown to be an independent predictor of mortality in patients with angina pectoris.
Figure 4. Myocardial ischemia ECG
Myocardial ischemia treatment
Treatment of myocardial ischemia is directed at improving blood flow to the heart muscle. Depending on the severity of your condition, you may be treated with medications, surgery or both.
Medications
Medications to treat myocardial ischemia include:
- Aspirin. A daily aspirin or other blood thinner can reduce your risk of blood clots, which might help prevent obstruction of your coronary arteries. Ask your doctor before starting to take aspirin because it might not be appropriate if you have a bleeding disorder or if you’re already taking another blood thinner.
- Nitrates. These medications temporarily open arteries, improving blood flow to and from your heart. Better blood flow means your heart doesn’t have to work as hard.
- Beta blockers. These medications help relax your heart muscle, slow your heartbeat and decrease blood pressure so blood can flow to your heart more easily.
- Calcium channel blockers. These medications relax and widen blood vessels, increasing blood flow in your heart. Calcium channel blockers also slow your pulse and reduce the workload on your heart.
- Cholesterol-lowering medications. These medications decrease the primary material that deposits on the coronary arteries.
- Angiotensin-converting enzyme (ACE) inhibitors. These medications help relax blood vessels and lower blood pressure. Your doctor might recommend an ACE inhibitor if you have high blood pressure or diabetes in addition to myocardial ischemia.
- Ranolazine (Ranexa). This medication helps relax your coronary arteries to ease angina. Ranolazine may be prescribed with other angina medications, such as calcium channel blockers, beta blockers or nitrates.
Procedures to improve blood flow
Sometimes, more-aggressive treatment is needed to improve blood flow. Procedures that may help include:
- Angioplasty and stenting. A long, thin tube (catheter) is inserted into the narrowed part of your artery. A wire with a tiny balloon is threaded into the narrowed area and inflated to widen the artery. A small wire mesh coil (stent) is usually inserted to keep the artery open.
- Coronary artery bypass surgery. A surgeon uses a vessel from another part of your body to create a graft that allows blood to flow around the blocked or narrowed coronary artery. This type of open-heart surgery is usually used only for people who have several narrowed coronary arteries.
- Enhanced external counterpulsation. This noninvasive outpatient treatment might be recommended if other treatments haven’t worked. Cuffs that have been wrapped around your legs are gently inflated with air then deflated. The resulting pressure on your blood vessels can improve blood flow to the heart.
Lifestyle and home remedies
To follow a heart-healthy lifestyle:
- Quit smoking. Talk to your doctor about smoking cessation strategies. Also try to avoid secondhand smoke.
- Manage underlying health conditions. Treat diseases or conditions that can increase your risk of myocardial ischemia, such as diabetes, high blood pressure and high blood cholesterol.
- Eat a healthy diet. Limit saturated fat and eat lots of whole grains, fruits and vegetables. Know your cholesterol numbers and ask your doctor if you’ve reduced them to the recommended level.
- Exercise. Talk to your doctor about starting a safe exercise plan to improve blood flow to your heart.
- Maintain a healthy weight. If you’re overweight, talk to your doctor about weight-loss options.
- Decrease stress. Practice healthy techniques for managing stress, such as muscle relaxation and deep breathing.
It’s important to have regular medical checkups. Some of the main risk factors for myocardial ischemia — high cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can set the stage for a lifetime of better heart health.
- Heart Attack: Know the Facts and Act Fast. https://www.nhlbi.nih.gov/files/docs/public/heart/heart_attack_fs_en.pdf[↩]
- Eggers KM, Oldgren J, Nordenskjöld A, Lindahl B. Combining different biochemical markers of myocardial ischemia does not improve risk stratification in chest pain patients compared to troponin I alone. Coron Artery Dis. 2005 Aug. 16(5):315-9.[↩]
- Slart RH, Zeebregts CJ, Hillege HL, et al. Myocardial perfusion reserve after a PET-driven revascularization procedure: a strong prognostic factor. J Nucl Med. 2011 Jun. 52(6):873-9.[↩]
- Kapetanopoulos A, Ahlberg AW, Taub CC, Katten DM, Heller GV. Regional wall-motion abnormalities on post-stress electrocardiographic-gated technetium-99m sestamibi single-photon emission computed tomography imaging predict cardiac events. J Nucl Cardiol. 2007 Nov-Dec. 14(6):810-7. [↩]