Contents
- What is neuromyelitis optica
- Other names for neuromyelitis optica
- Is there a link between migraine and neuromyelitis optica?
- Are there any dietary considerations/restrictions for people with neuromyelitis optica?
- What is a neuromyelitis optica relapse?
- Why do neuromyelitis optica relapses happen?
- What symptoms do neuromyelitis optica relapses cause?
- Can deficits that are present for many years be reversed?
- Neuromyelitis optica life expectancy
- Neuromyelitis optica causes
- Neuromyelitis optica symptoms
- Neuromyelitis optica diagnosis
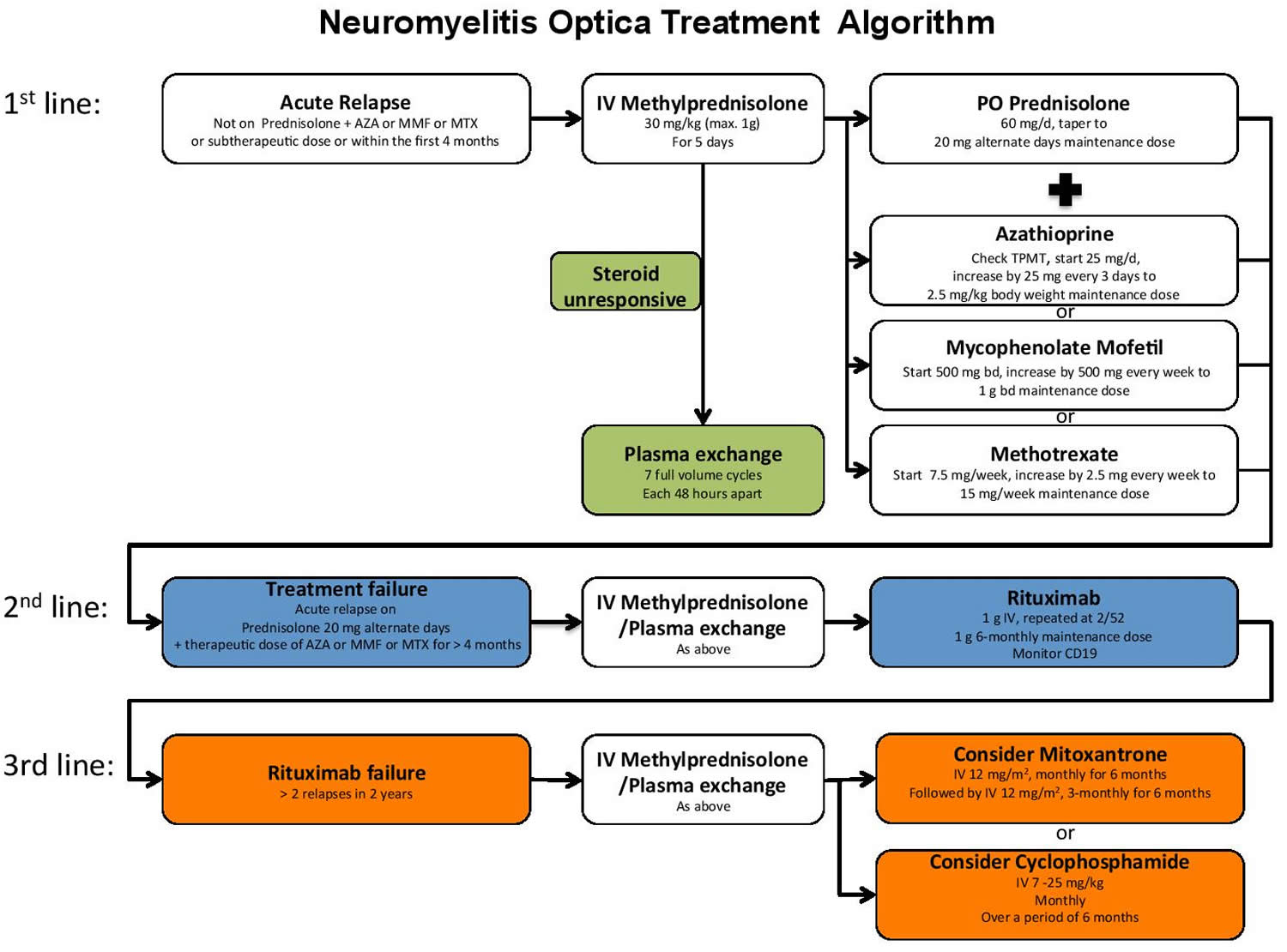
- Neuromyelitis optica treatment
What is neuromyelitis optica
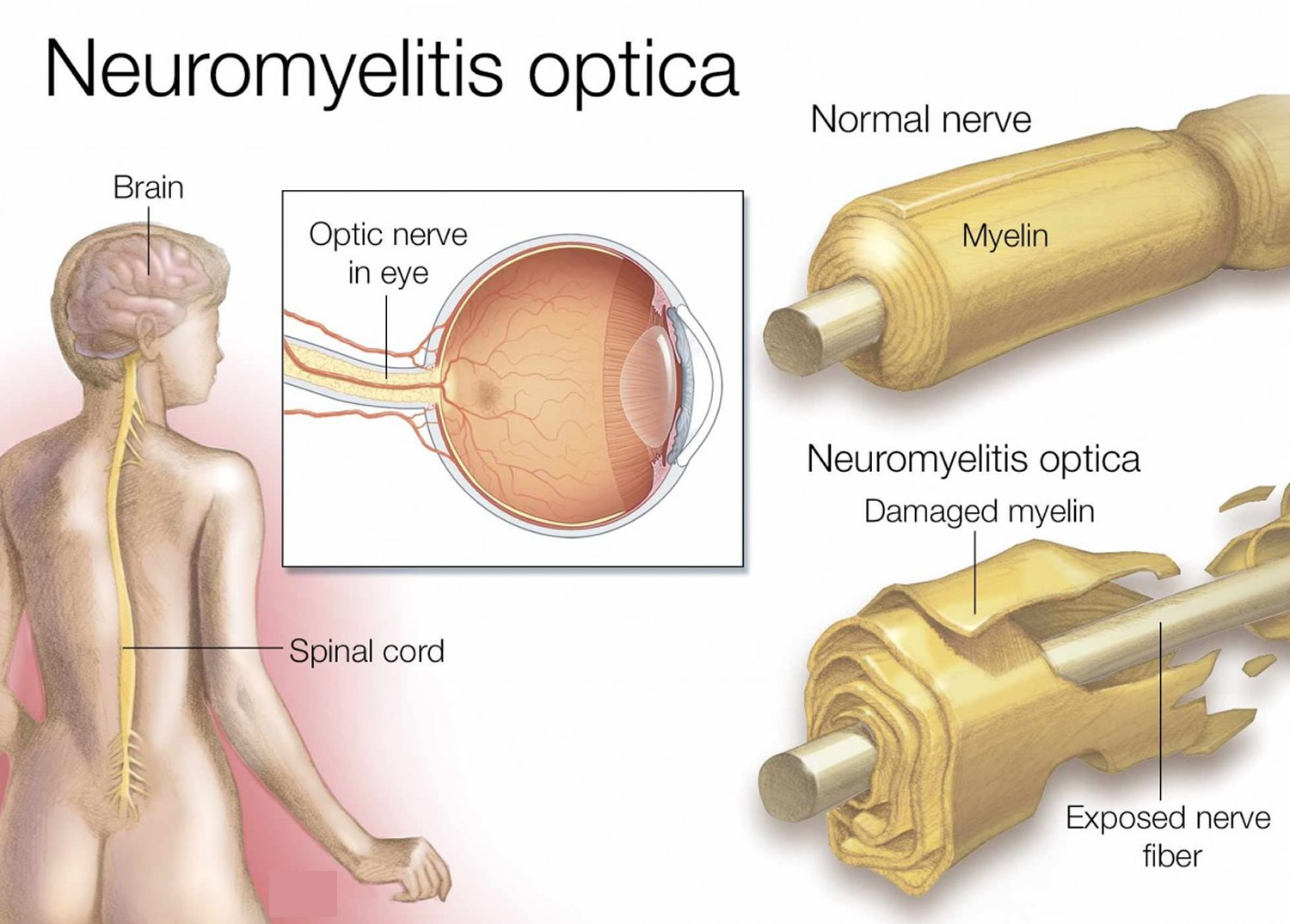
Neuromyelitis optica also known as Devic disease, is a very rare autoimmune disorder that affects the nerves of your eyes and the central nervous system, which includes the brain and spinal cord. Autoimmune disorders occur when the immune system malfunctions and attacks your body’s own tissues and organs. In neuromyelitis optica, the autoimmune attack causes inflammation of the optic nerve (optic neuritis) and inflammation of the spinal cord (myelitis) and the resulting damage leads to wide range of symptoms, such as weakness, blindness, nerve pain and muscle spasms. These will vary from person to person – some may only have one attack of symptoms and recover well, whereas others may be more severely affected and have a number of attacks that lead to disability. In its early stages, neuromyelitis optica may be confused with multiple sclerosis (MS).
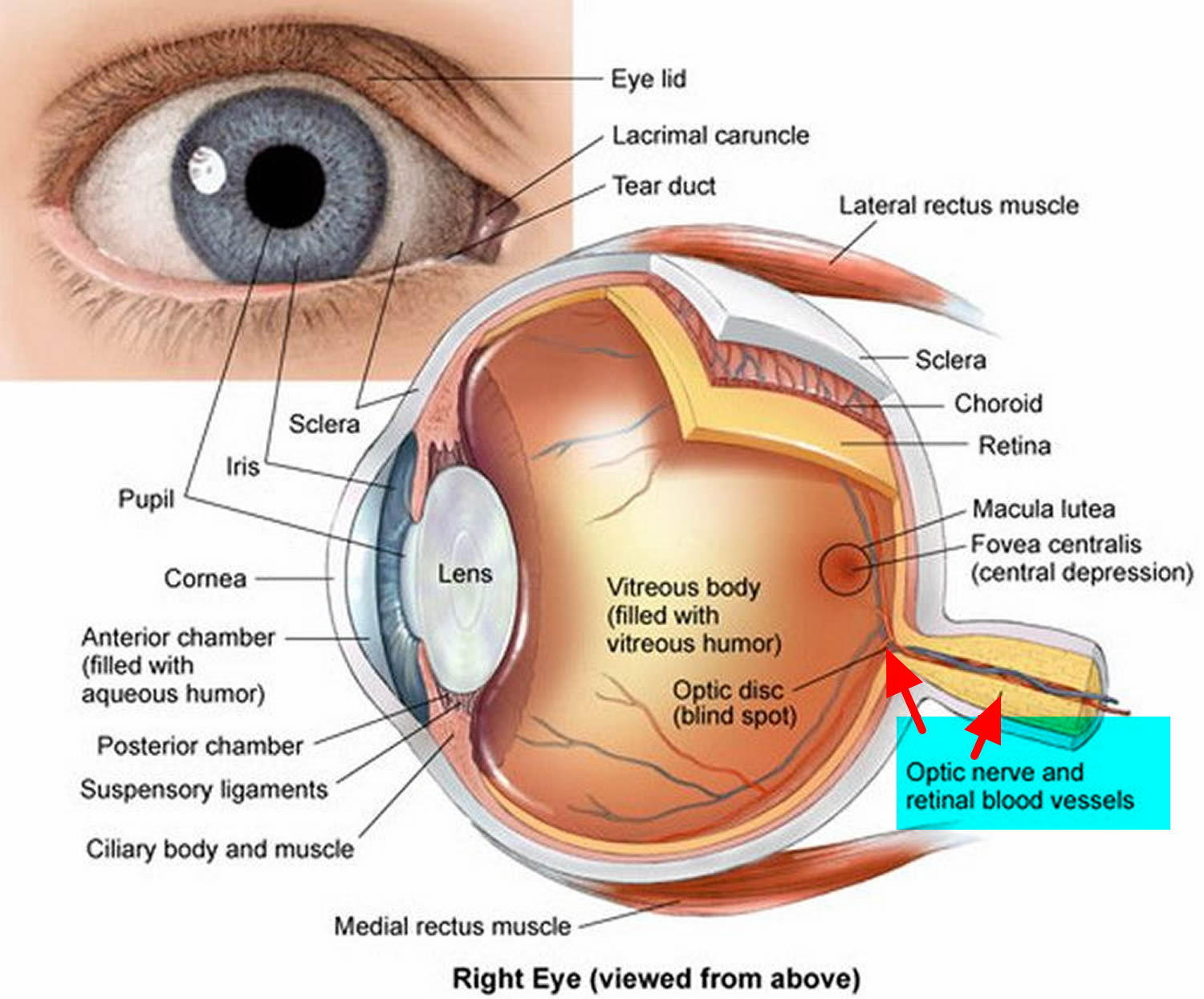
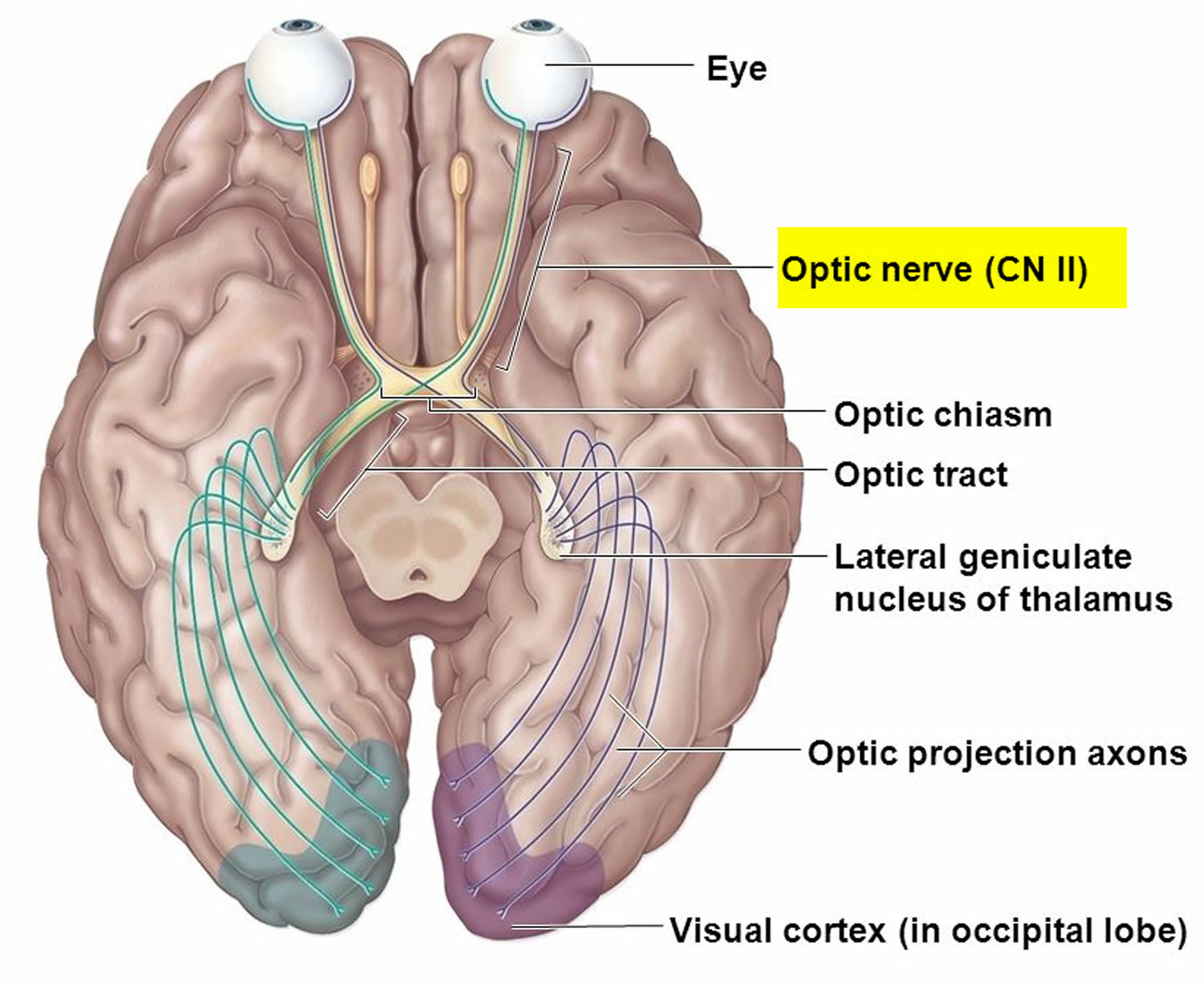
Neuromyelitis optica is characterized by optic neuritis, which is inflammation of the nerve that carries information from the eye to the brain (optic nerve). Optic neuritis causes eye pain and vision loss, which can occur in one or both eyes.
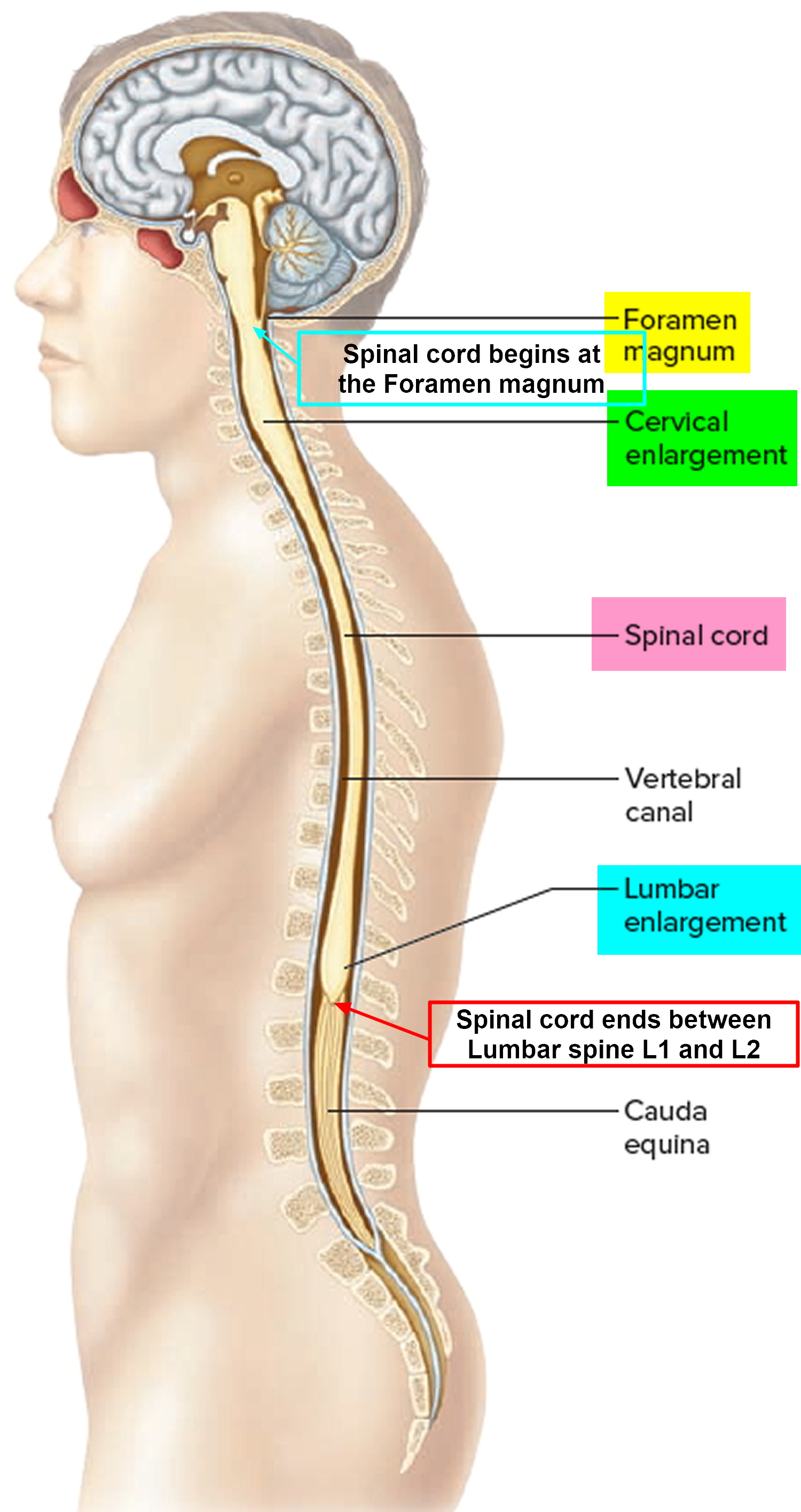
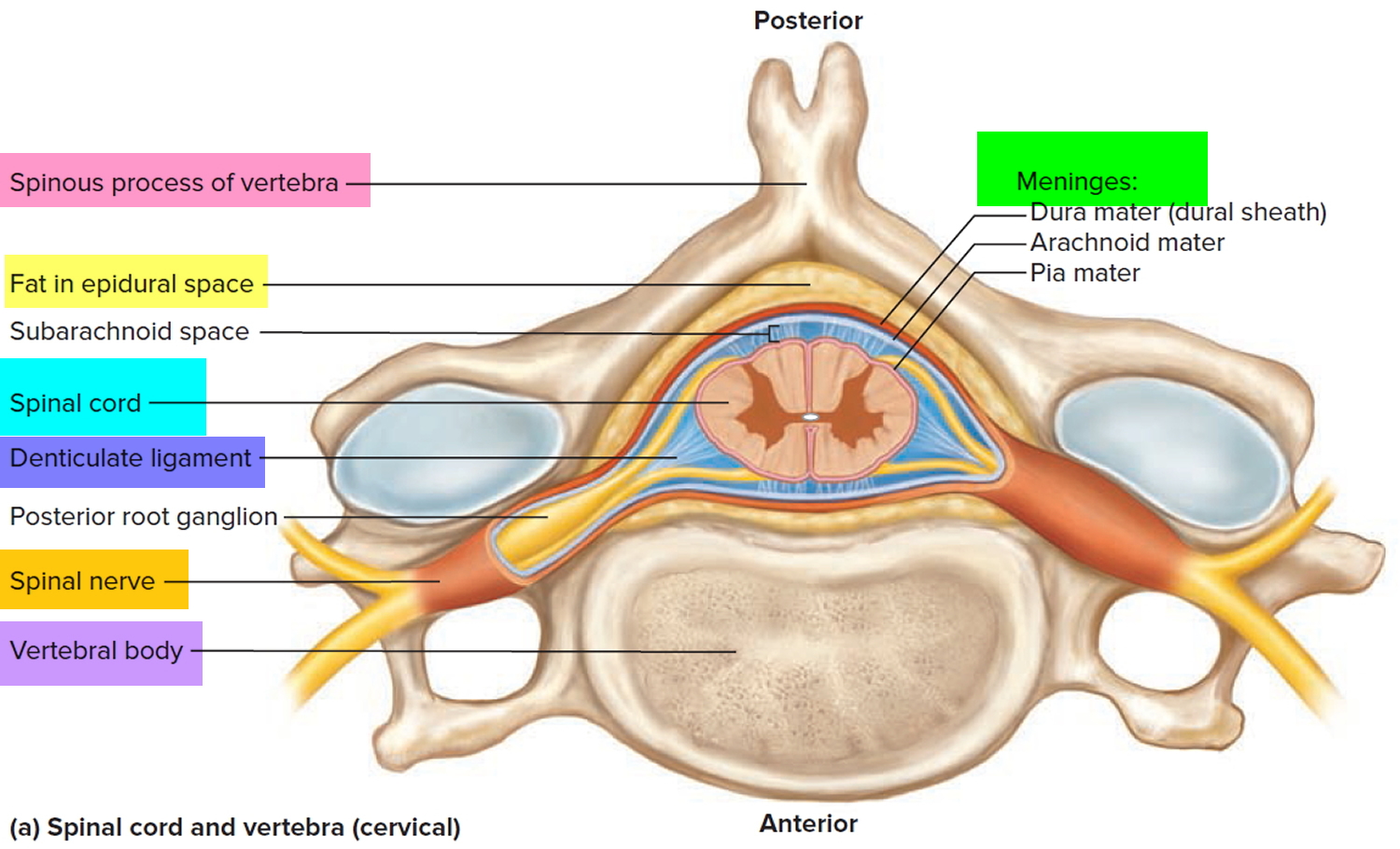
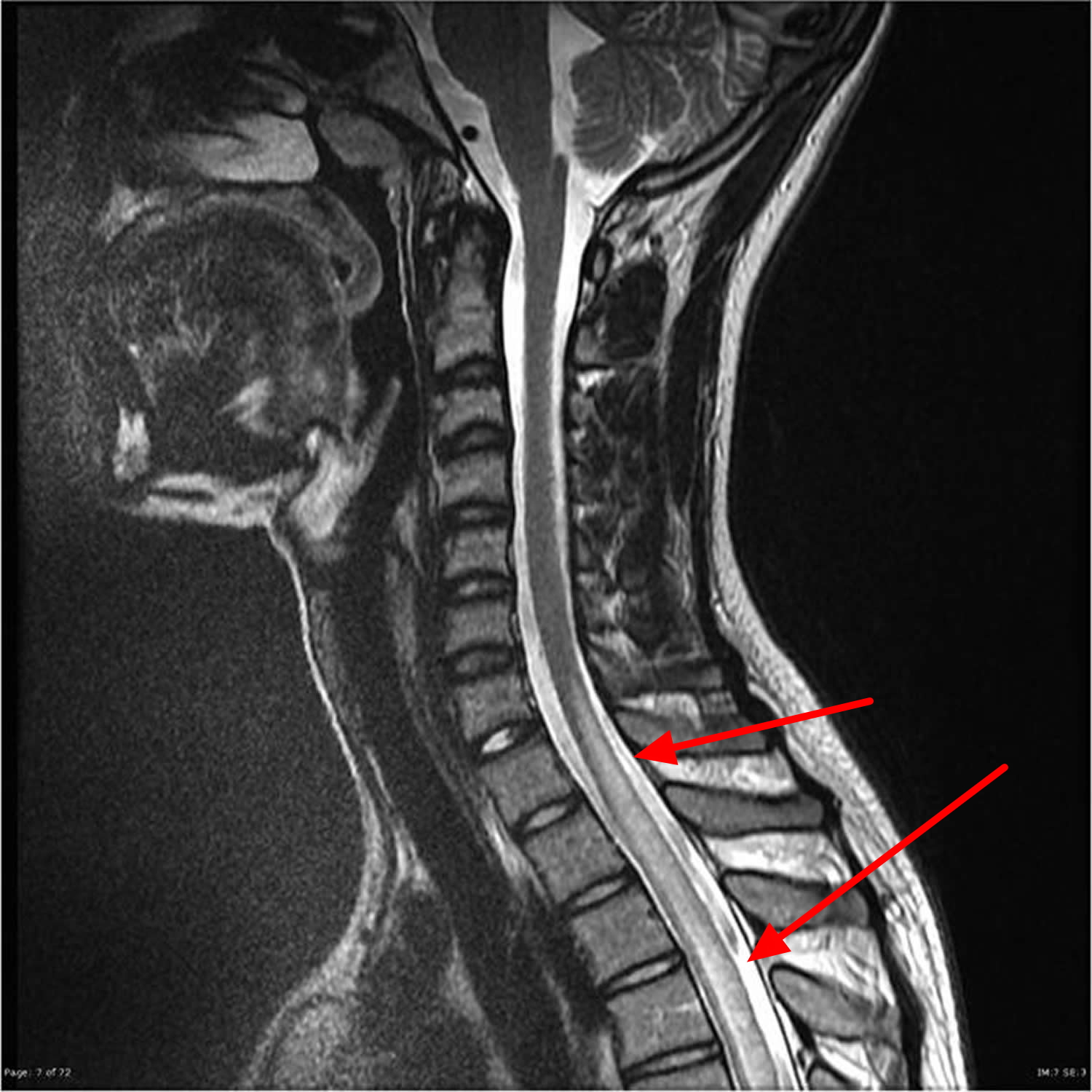
Neuromyelitis optica is also characterized by transverse myelitis, which is inflammation of the spinal cord. The inflammation associated with transverse myelitis damages the spinal cord, causing a lesion that often extends the length of three or more bones of the spine (vertebrae). In addition, myelin, which is the covering that protects nerves and promotes the efficient transmission of nerve impulses, can be damaged. Transverse myelitis causes weakness, numbness, and paralysis of the arms and legs. Other effects of spinal cord damage can include disturbances in sensations, loss of bladder and bowel control, uncontrollable hiccupping, and nausea. In addition, muscle weakness may make breathing difficult and can cause life-threatening respiratory failure in people with neuromyelitis optica.
Some people may only experience transverse myelitis or optic neuritis but, if they have a specific antibody associated with neuromyelitis optica (aquaporin-4 autoantibody — AQP4) in their blood, they will be said to have neuromyelitis optica spectrum disorder. Aquaporin-4 (AQP4) is a membrane water channel expressed in astrocytes 1. Studies suggest that this antibody is pathogenic. Binding of AQP4 immunoglobulin G (IgG) to AQP4 activates complement-dependent cytotoxicity, which leads to a cascade of inflammatory events including leukocyte infiltration and cytokine release along with breakdown of the blood-brain barrier. Inflammatory damage results in demyelination and axonal/neuronal damage responsible for the observed neurologic deficits 2.
Neuromyelitis optica spectrum disorder is not hereditary (it is very rarely found in more than one family member). People who inherit a tendency to develop an autoimmune disease are at increased risk of developing another autoimmune disease, such as diabetes or thyroid disease. You cannot pass on an increased risk of getting neuromyelitis optica to your family. It is not possible to catch neuromyelitis optica from another person.
Scientists do not fully understand the reason why someone develops neuromyelitis optica. As with all autoimmune conditions, the immune system mistakes certain parts of your body and decides it is ‘foreign’ and therefore tries to damage or destroy it. Sometimes the first episode of an neuromyelitis optica attack can be preceded by an episode of flu or other virus or even a vaccine. It is thought that the immune system may overreact to this and attack the body in error.
Symptoms of optic neuritis and transverse myelitis include:
- eye pain
- loss of vision
- colors appearing faded or less vivid
- weakness in the arms and legs
- pain in the arms or legs – described as sharp, burning, shooting or numbing – and increased sensitivity to cold and heat
- tight and painful muscle spasms in the arms and legs
- bladder, bowel and sexual problems
Neuromyelitis optica occurs in individuals of all races. Neuromyelitis optica affects approximately 1 to 5 per 100,000 people and seems to be similar worldwide. Relative to multiple sclerosis (MS) that it mimics, neuromyelitis optica occurs with greater frequency in individuals of Asian descent and possibly in individuals of African descent, but the majority of patients with neuromyelitis optica in Western countries are Caucasian. Individuals of any age may be affected, but typically neuromyelitis optica occurs in late middle-aged women. Children represent may also be affected by neuromyelitis optica; children more commonly develop brain symptoms at onset and seem to have a higher frequency of monophasic presentation. Women are affected by neuromyelitis optica more frequently than men.
There are two forms of neuromyelitis optica:
- Relapsing form: The relapsing form is most common. This form is characterized by repeated attacks separated by periods of remission of optic neuritis and transverse myelitis. These episodes can be months or years apart, and there is usually partial recovery between episodes. In this form, the interval between attacks may be weeks, months or years. However, most affected individuals eventually develop permanent muscle weakness and vision impairment that persist even between episodes. For unknown reasons, approximately nine times more women than men have the relapsing form.
- Monophasic form: The monophasic form, which is less common, causes a single episode of neuromyelitis optica that can last several months. One or both optic nerves and the spinal cord are affected by a series of attacks over a short period of time (days or weeks) but, after the initial outburst, there is no recurrence. People with this form of the condition can also have lasting muscle weakness or paralysis and vision loss. This form affects men and women equally.
The onset of either form of neuromyelitis optica can occur anytime from childhood to adulthood, although the condition most frequently begins in a person’s forties. Equal numbers of men and women have the monophasic form that does not recur after the initial flurry of attacks, but women are four or five times more likely to be affected than men by the recurring (relapsing) form.
Approximately one-quarter of individuals with neuromyelitis optica have signs or symptoms of another autoimmune disorder such as myasthenia gravis, systemic lupus erythematosus (SLE), or Sjögren syndrome. Some scientists believe that a condition described in Japanese patients as optic-spinal multiple sclerosis (or opticospinal multiple sclerosis) that affects the nerves of the eyes and central nervous system is the same as neuromyelitis optica.
At present there is no cure for neuromyelitis optica so management focuses on the following key areas:
- Treating acute attacks/relapses
- Preventing relapses
- Treating the residual symptoms of the relapse
Other names for neuromyelitis optica
- Devic disease
- Devic neuromyelitis optica
- Devic syndrome
- Devic’s disease
- optic-spinal MS
- opticospinal MS
Is there a link between migraine and neuromyelitis optica?
Migraines do not cause neuromyelitis optica, but there is some anecdotal reports of patients with neuromyelitis optica experiencing migraine like headaches. It is important to remember that headaches and migraine are quite common in the general population.
Are there any dietary considerations/restrictions for people with neuromyelitis optica?
A healthy diet with adequate vegetables, fruits, calcium and vitamin D (remember steroids can cause bones to weaken) and proteins is needed to keep the body fit. It is often easy to put on weight due to side effects of steroids, and/or lack of exercise.
What is a neuromyelitis optica relapse?
A relapse, or an ‘attack’ of neuromyelitis optica, occurs when there is inflammation within the nervous system. In neuromyelitis optica, this inflammation is usually within the optic nerve and the spinal cord. The inflammation causes people to experience new symptoms, or recurrence of symptoms that they have had previously.
Why do neuromyelitis optica relapses happen?
Scientists don’t understand what causes or triggers a relapse. Relapses are usually unpredictable and there is nothing that you may have done to cause them. Occasionally, a relapse may be triggered by infection or by stress.
What symptoms do neuromyelitis optica relapses cause?
In people with neuromyelitis optica, relapses usually affect either the optic nerve or the spinal cord.
When relapses affect the optic nerves they cause problems with the vision. Symptoms normally come on over a period of hours or days, or people may wake up one morning with visual symptoms. Symptoms include:
- Pain behind the eye or on movement
- Colors appear faded or ‘washed out’
- Vision may be blurred or lost completely
Brief ‘stabbing’ pain in and around the eye lasting only a few seconds or minutes is unlikely to be caused by a relapse. Many people with neuromyelitis optica find that their vision varies from day to day, for example if they are tired.
People with neuromyelitis optica may also experience relapses affecting the spinal cord. The spinal cord controls strength and sensation in the arms, legs and trunk and is also involved in bladder and bowel control. Inflammation in the spinal cord may cause many different symptoms including:
- Weakness in the arms and/or legs,
- Numbness or abnormal sensations in arms/legs/trunk
- A band like sensation around the trunk, like being squeezed
- Severe pain in the neck or between the shoulder blades
- Problems with the bladder such as difficulty or inability to pass urine
- Constipation or loss of control of bowel movement
Each of these symptoms may occur individually, or people may experience a combination of symptoms. Usually symptoms develop over hours or days. They are significant if they last for longer than 48 hours.
It is important to remember that most relapses of neuromyelitis optica need to be assessed and treated promptly.
If you feel that there is a sustained deterioration in your vision or experience any of the symptoms described above which lasts for longer than 48 hours, please contact your neuromyelitis optica specialist or medical team.
Initial Treatment
Once infection has been ruled out relapses are usually treated with Methylprednisolone either 500 mg orally for 7 days or 1 gm intravenously for 5 days. Research has shown that both options are equally effective in treating relapses. Sometimes, particularly in the case of vision changes, we might treat with plasma exchange which is given intravenously once daily for five days.
Recovery from Relapses
The time taken to recover and the amount of function recovered after a relapse can be affected by many factors and varies hugely from person to person. An important factor to always consider is that any new symptom or sustained worsening of an existing symptom (over 24 hrs) should be reported to your neuromyelitis optica medical team for further assessment. Early assessment and treatment may prevent long term damage.
Can deficits that are present for many years be reversed?
It is rare for this to happen. Physical adaptations (modifications in house, wheelchair etc) and lifestyle modifications (change of job, moving to a single floor house) should be planned in advance and money spent wisely rather than waiting for ‘miracles to happen’ or trying out costly alternative medicines or exotic cures.
Neuromyelitis optica life expectancy
Every person is affected differently. Some people only experience mild attacks and can have near complete recovery whilst at the other extreme, some patients can experience vision loss or become paralysed. However, there is currently no research data available on neuromyelitis optica life expectancy.
When scientists first discovered the antibodies associated with neuromyelitis optica in 2005, prognosis was poor however, scientists now understand the condition much better and treatment options have greatly improved as has the prognosis and severe residual issues are thankfully much more rare.
Most individuals with neuromyelitis optica have an unpredictable, relapsing course of disease with attacks occurring months or years apart. Disability is cumulative, the result of each attack damaging new areas of the central nervous system. Some individuals are severely affected by neuromyelitis optica and can lose vision in both eyes and the use of their arms and legs. Most individuals experience some degree of permanent limb weakness or vision loss from neuromyelitis optica. However, reducing the number of attacks with immunosuppressive medications may help prevent with accumulation of disability. Rarely, muscle weakness can be severe enough to cause breathing difficulties and may require the use of artificial ventilation.
In an epidemiology study, about half the patients with relapsing neuromyelitis optica had significant visual loss (less than 20/200 or 6/60) in at least one eye and/or could not walk due to leg weakness and was reliant on a walking aid such as a walking stick, frame or wheelchair.
However this information was a generalization drawn from an early study based on patients referred to a major hospital (i.e., they may already have been significantly impaired or had severe disease, and may not be representative of all patients. Furthermore, some patients were not treated. Early treatment may lead to better outcomes.
Figure 1. Optic nerve
Figure 2. Optic nerve and visual pathway
Figure 3. Normal optic nerve
Figure 4. Optic neuritis – the photo demonstrates, the optic nerve becomes swollen and the blood vessels become larger.
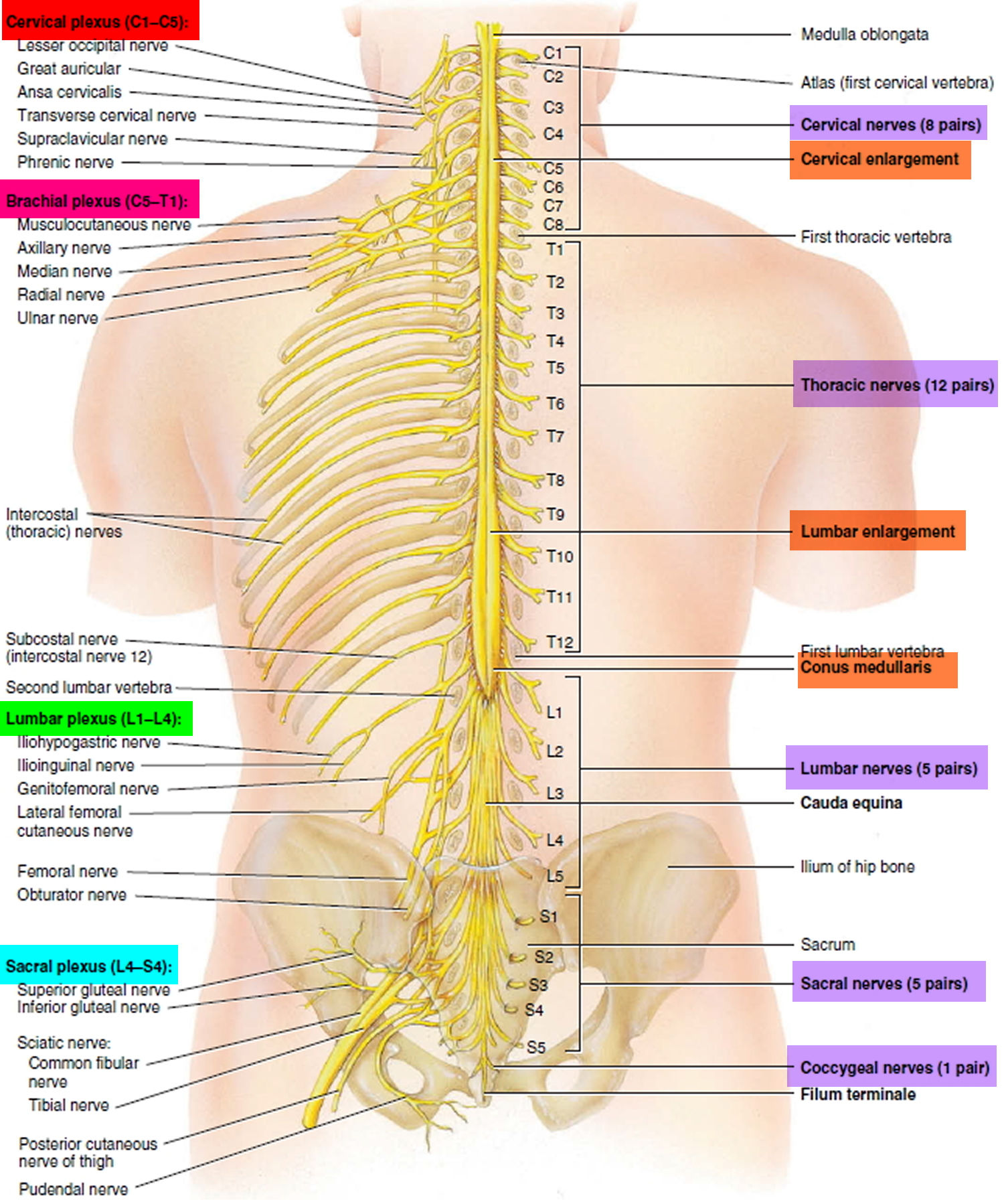
Figure 5. Spinal cord
Figure 6. Spinal cord segments
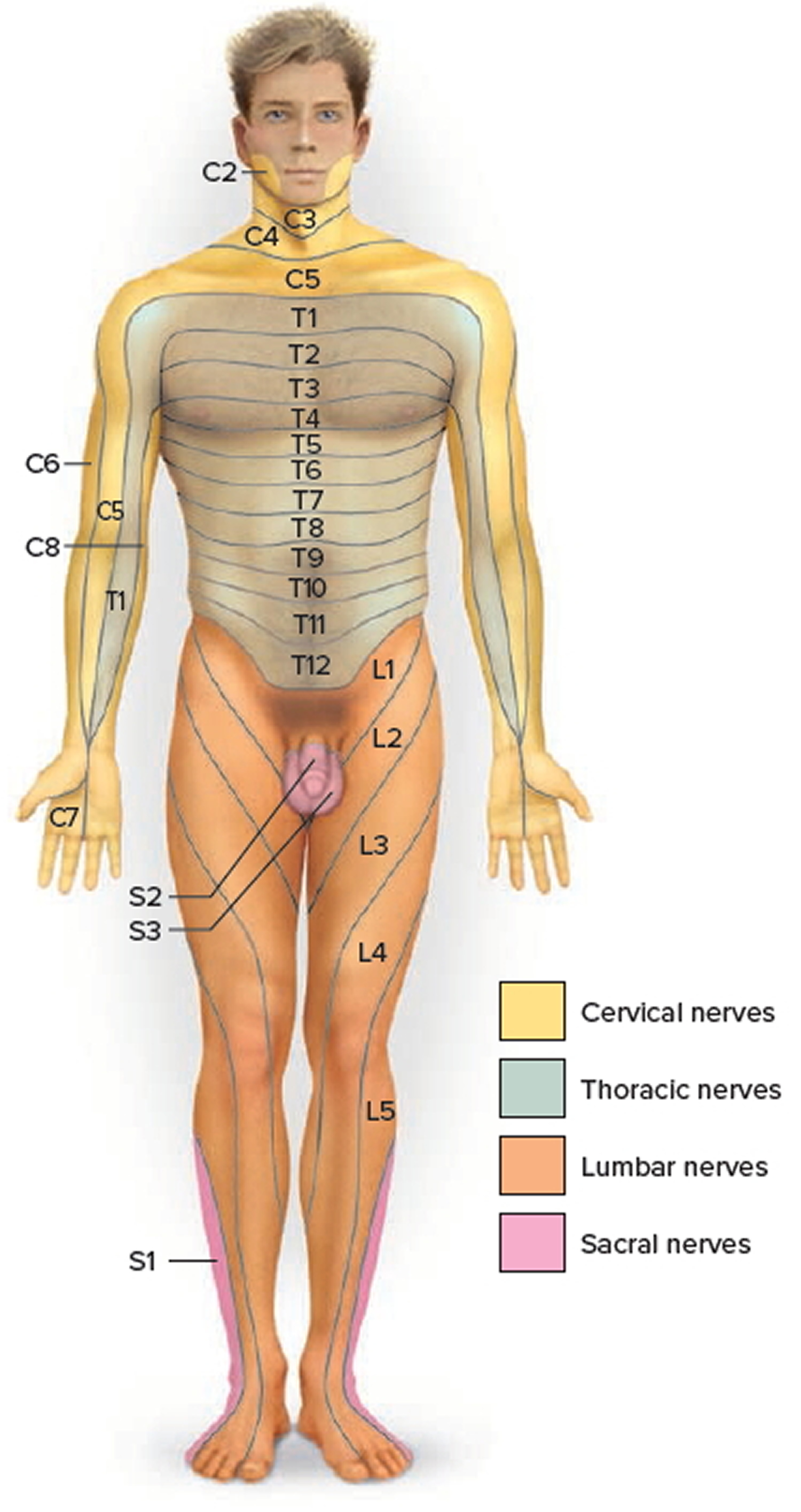
Figure 7. Dermatome (spinal nerves sensory innvervation)
Figure 8. Spinal cord anatomy
Figure 9. Transverse myelitis – MRI showing mild swelling (blue arrows) involves most of the conus, more patchy towards the tip
Neuromyelitis optica causes
Greater than 95% of patients with neuromyelitis optica report no relatives with the disease, but approximately 3% report having other relatives with the condition. There is a strong association with a personal or family history of autoimmunity, which are present in 50% of cases. Neuromyelitis optica is regarded as an autoimmune disease though the exact cause for the autoimmunity is unknown.
Autoimmune disorders occur when the body’s natural defenses against disease or invading organisms (such as bacteria), for unknown reasons, suddenly begin to attack healthy tissue. These defenses, for reasons not at all understood, attack proteins in the central nervous system, especially aquaporin-4 (AQP4). In some patients with neuromyelitis optica, especially those with the non-relapsing variant, antibodies to myelin oligodendrocyte glycoprotein have been discovered by investigators in the U.K. and Japan which may be associated with this disorder. Neuromyelitis optica may be immunologically heterogeneous.
No genes associated with neuromyelitis optica have been identified. However, a small percentage of people with this condition have a family member who is also affected, which indicates that there may be one or more genetic changes that increase susceptibility. It is thought that the inheritance of this condition is complex and that many environmental and genetic factors are involved in the development of the condition.
The aquaporin-4 protein (AQP4), a normal protein in the body, plays a role in neuromyelitis optica. The aquaporin-4 protein (AQP4) is found in several body systems but is most abundant in tissues of the central nervous system. Approximately 70 percent of people with this disorder produce an immune protein called an antibody that attaches (binds) to the aquaporin-4 protein. Antibodies normally bind to specific foreign particles and germs, marking them for destruction, but the antibody in people with neuromyelitis optica attacks a normal human protein; this type of antibody is called an autoantibody. The autoantibody in this condition is called neuromyelitis optica-IgG or anti-AQP4.
The binding of the neuromyelitis optica-IgG autoantibody to the aquaporin-4 protein turns on (activates) the complement system, which is a group of immune system proteins that work together to destroy pathogens, trigger inflammation, and remove debris from cells and tissues. Complement activation leads to the inflammation of the optic nerve and spinal cord that is characteristic of neuromyelitis optica, resulting in the signs and symptoms of the condition.
The levels of the neuromyelitis optica-IgG autoantibody are high during episodes of neuromyelitis optica, and the levels decrease between episodes with treatment of the disorder. However, it is unclear what triggers episodes to begin or end.
Neuromyelitis optica symptoms
The characteristic symptoms of neuromyelitis optica are either optic neuritis or myelitis; either may occur as the first symptom. Optic neuritis is inflammation, of the optic nerve (optic neuritis) leading to pain inside the eye which rapidly is followed by loss of clear vision (acuity). Usually, only one eye is affected (unilateral) although both eyes may be involved simultaneously (bilateral). Neuromyelitis optica may or may not be preceded by a prodromal upper respiratory infection.
Optic neuritis usually affects one eye. Symptoms might include:
- Pain. Most people who develop optic neuritis have eye pain that’s worsened by eye movement. Sometimes the pain feels like a dull ache behind the eye.
- Vision loss in one eye. Most people have at least some temporary reduction in vision, but the extent of loss varies. Noticeable vision loss usually develops over hours or days and improves over several weeks to months. Vision loss is permanent in some cases.
- Visual field loss. Side vision loss can occur in any pattern.
- Loss of color vision. Optic neuritis often affects color perception. You might notice that colors appear less vivid than normal.
- Flashing lights. Some people with optic neuritis report seeing flashing or flickering lights with eye movements.
The other cardinal syndrome is inflammation of the spinal cord, a condition known as transverse myelitis because the symptoms tend to affect all motor, sensory and autonomic functions (bladder and bowel) below a certain level on the body. Affected individuals may experience pain in the spine or limbs, and mild to severe paralysis (paraparesis to paraplegia) of the lower limbs, and loss of bowel and bladder control. Deep tendon reflexes may be diminished or absent initially and later become exaggerated. A variable degree of sensory loss may occur. Affected individuals may also have a stiff neck, back or limb pain, and/or headaches. This syndrome may be indistinguishable from other cases of “idiopathic” transverse myelitis.
Four classic features of transverse myelitis are:
- Weakness of the legs and arms. People with transverse myelitis may have weakness in the legs that progresses rapidly. If the myelitis affects the upper spinal cord it affects the arms as well. Individuals may develop paraparesis (partial paralysis of the legs) that may progress to paraplegia (complete paralysis of the legs), requiring the person to use a wheelchair. There are no medications to improve weakness. Exercise and stretching are good.
- Pain. Initial symptoms usually include lower back pain or sharp, shooting sensations that radiate down the legs or arms or around the torso. Pain symptoms vary based on on the part of your spinal cord that’s affected.
- Neuropathic (nerve) pain arising directly from damaged nerves in the spine, there are no particular triggers, this pain is described as burning, sharp, electrical shock, shooting or an uncomfortable numbness. Medication suggestions are Amitriptyline, Gabapentin, Pregabalin and Carbamazepine.
- Nociceptive (musculoskeletal) pain often has a more obvious cause, such as banging your knee. In neuromyelitis optica, the most common cause is pressure on joints from altered gait (the way you walk). Medication suggestions such as Paracetamol or Ibrufen may be helpful.
- Abnormal sensations. Transverse myelitis can cause paresthesias (abnormal sensations such as burning, tickling, pricking, numbness, coldness, or tingling) in the legs, and sensory loss. Some are especially sensitive to the light touch of clothing or to extreme heat or cold. You may feel as if something is tightly wrapping the skin of your chest, abdomen or legs. Abnormal sensations in the torso and genital region are common. Sometimes the shooting sensations occur when the neck is bent forward and resolve when the neck is brought back to normal position (a condition called Lhermitte’s phenomenon).
- Bladder dysfunction. Common symptoms include an increased frequency or urge to use the toilet (urgency), incontinence, difficulty voiding, nocturia (passing urine at night) and retention (unable to pass urine) due to damage on the spinal cord. Medicines like Oxybutynin, Tolterodine may be helpful or learning self-catheterisation, (a very simple technique).
- Bowel symptoms mainly constipation, urgency and sometimes faecal incontinence are also due to damage on the spinal cord and immobility. Laxatives, a high fiber diet and fluids as well as abdominal massage may be useful.
- Increased muscle tone and spasms arises from damaged nerves in spinal cord that affects the control of muscles, including when they contract and relax. This can present as prolonged contractions of the muscles, which are called spasms. Medication suggestions are Baclofen, Tizanidine, Gabapentin.
- Tonic spasms this is a painful spasm of the muscles that lasts seconds to minutes but frequently. Often it’s controlled by Carbamazepine at low doses.
- Joint stiffness is a discomfort after a period of inactivity (such as waking up in the morning or sitting for an extended period of time. Medication suggestions are Baclofen, Tizanidine, Dantrolene. Exercises and stretching are often useful.
- Sexual dysfunction where men may experience difficulty getting an erection, or reaching orgasm, and women may also have difficulty reaching orgasm due to a lack of sensation and numbness.
- Osteoporosis (brittle bones) may be the result of long-term use of steroid medication or a lack of weight-bearing activities.
- Depression – changes in lifestyle associated with the complications of neuromyelitis optica can increase the risk of developing depression.
Many individuals also report experiencing muscle spasms, a general feeling of discomfort, headache, fever, and loss of appetite, while some people experience respiratory problems. Other symptoms may include sexual dysfunction and depression and anxiety caused by lifestyle changes, stress, and chronic pain.
The segment of the spinal cord at which the damage occurs determines which parts of the body are affected. Damage at one segment will affect function at that level and below. In individuals with transverse myelitis, myelin damage most often occurs in nerves in the upper back, causing problems with leg movement and bowel and bladder control, which require signals from the lower segments of the spinal cord.
Early in the course of the disease, it may be difficult to distinguish between neuromyelitis optica and multiple sclerosis (MS) because both may cause optic neuritis and myelitis as symptoms. However, the optic neuritis and myelitis tend to be more severe in neuromyelitis optica; the brain MRI is more commonly normal, and the spinal fluid analysis does not usually show oligoclonal bands in neuromyelitis optica, which are features that help distinguish it from MS.
In most cases of neuromyelitis optica, the initial symptoms of vision loss or paralysis improve with standard treatment with high dose corticosteroids, and partial recovery of vision, motor, sensory, or bladder function occurs. However, in recurring cases, neuromyelitis optica frequently causes significant permanent disturbances of vision and/or spinal cord function leading to blindness or impaired mobility.
Neuromyelitis optica spectrum disorders include limited versions of neuromyelitis associated with positive test for aquaporin-4 autoantibodies and neuromyelitis optica brain syndromes associated with positive test for aquaporin-4 autoantibodies.
Some patients with neuromyelitis optica have only recurrent myelitis or only recurrent optic neuritis. When patients have antibodies to aquaporin-4 with just these manifestations, most investigators would argue that they should be treated as having neuromyelitis optica. Brain lesions may occur in patients with neuromyelitis optica, typically, but not always, in later phases of the disease. Intractable vomiting or hiccups is now a generally accepted specific syndrome of this condition and is the result of inflammation in the dorsal medulla of the brainstem and may be the initial symptom of neuromyelitis optica. Brainstem and hypothalamic syndromes are particularly common, but inflammation of the forebrain may also occur, often associated with prominent brain swelling (edema). Clinicians suspecting this disorder must have a strong index of suspicion for this condition especially in patients with a history of severe myelitis or optic neuritis.
Neuromyelitis optica can also be associated with systemic autoimmune disease.
Why do Symptoms persist after the relapse has recovered?
When a relapse occurs there is inflammation and swelling in the brain, so messages cannot get from the brain to their target, e.g., a relapse of the spinal cord does not allow nerve messages to pass to the area below the inflammation causing the symptoms of transverse myelitis.
Over time there is some spontaneous recovery and symptoms may improve over 2-6 months. However, if the nerves have been damaged or destroyed new pathways can not be made, resulting in permanent damage.
Some people will have very few residual symptoms from a relapse, whilst others may have more. The severity will also be different between individuals.
Symptoms such as:
- Loss of vision as a result of damage to the optic nerve.
- Paralysis of limbs due to damage to the spinal cord in the neck, which may affect legs and arms causing weakness and little function.
- Breathing difficulties due to damage in cervical (neck) area of spine causing muscle weakness which, in extreme cases will require artificial ventilation (a machine that helps you breathe).
OR
Symptoms may be indirectly caused resulting from damage of the nerves.
The symptoms are treated to try and improve your daily living either with medication or therapy. The medications do NOT prevent further relapses. There is no ‘right’ drug as individuals respond differently to different treatments. The overall aim of symptom management is to control or reduce symptoms impairing functional abilities and quality of life. You may have to trial several regimes to find the most suitable drug for you.
Neuromyelitis optica diagnosis
Your doctor will perform a thorough evaluation to rule out other nervous system (neurological) conditions that have signs and symptoms similar to neuromyelitis optica. Distinguishing neuromyelitis optica from multiple sclerosis (MS) and other conditions ensures that you receive the most appropriate treatment.
To diagnose your condition, your doctor will review your medical history and symptoms and perform a physical examination. Your doctor may also perform:
- Neurological examination. A neurologist will examine your movement, muscle strength, coordination, sensation, memory and thinking (cognitive) functions, and vision and speech. An eye doctor (ophthalmologist) also may be involved in your examination.
- Ophthalmological examination. An ophthalmologist is trained to pick up even very small changes in a patient’s vision.
- Opthalmoscopy (looking at the back of the eye with an ophthalmoscope) may show swelling of the optic disc. Often swelling is not seen, as the demyelination can be further away from the eye (retro bulbar neuritis).
- Visual Evoked Potential (VEP): Electrodes are placed on the scalp and measure the speed of nerve messages along the optic nerve from the eye to brain in response to being shown a flashing chessboard pattern on a computer screen. Damage to the optic nerve shows slower response time.
- Visual Field Tests: These show whether there are any areas of your peripheral vision missing, which can indicate optic neuritis.
- Low Contrast Test: By testing a person’s vision against increasingly faded images, it is possible to test how ‘washed out’ a persons vision has become.
- Ishihara Test: This is a series of 13 images that detect minor changes in color vision sensitivity.
- Optical Coherence Tomography (OCT): This is a very fast scan that can measure the thickness of the nerve fibres in the optic nerve. At present this is more a research tool than a clinical marker.
- Magnetic resonance imaging (MRI). An MRI uses powerful magnets and radio waves to create a detailed view of your brain, optic nerves and spinal cord. Your doctor may be able to detect lesions or damaged areas in your brain, optic nerves or spinal cord.
- Blood tests. Your doctor might test your blood for the autoantibody neuromyelitis optica-IgG (also known as the aquaporin-4 autoantibody — AQP4), which helps doctors distinguish neuromyelitis optica from MS and other neurological conditions. This is very helpful to request this test at the first significant suspicion of neuromyelitis optica, as it is frequently positive at the time of the very first symptom even before a confident clinical diagnosis is possible. However 20% of people with neuromyelitis optica do not have aquaporin 4 antibodies (AQP4). Successful diagnosis of neuromyelitis optica depends on distinguishing it from multiple sclerosis (MS). A myelin oligodendrocyte glycoprotein (MOG-IgG) antibody test may also be requested to look for another inflammatory disorder that mimics neuromyelitis optica.
- Aquaporin 4 -antibodies (AQP-4): Aquaporin 4 (AQP4) is a water channel protein found on cells known as astrocytes that surround the blood-brain barrier, (a layer of cells responsible for preventing dangerous substances in the blood from crossing into the brain). It is presumed that the blood brain barrier allows the AQP4 antibodies to enter the central nervous system. This causes an inflammation and demyelination and symptoms of a relapse. Approximately 80% of people diagnosed with neuromyelitis optica have Aquaporin 4 antibodies in their blood.
- Lumbar puncture (spinal tap). During this test, your doctor will insert a needle into your lower back to remove a small amount of cerebrospinal fluid (CSF). Doctors test the levels of immune cells, proteins and antibodies in the cerebrospinal fluid (CSF). This test may help your doctor differentiate neuromyelitis optica from multiple sclerosis (MS). In neuromyelitis optica, the spinal fluid may show markedly elevated white blood cells during neuromyelitis optica episodes, greater than normally seen in multiple sclerosis (MS), although this doesn’t always happen.
- Stimuli response test. To learn how well your brain responds to stimuli such as sounds, sights or touch, you’ll undergo a test called evoked potentials (they may also be called evoked response tests). During these tests, doctors attach small wires (electrodes) to your scalp and, in some cases, your earlobes, neck, arm, leg and back. Equipment attached to the electrodes records your brain’s responses to stimuli. These tests help your doctor to find lesions or damaged areas in the nerves, spinal cord, optic nerve, brain or brainstem.
Neuromyelitis optica treatment
Neuromyelitis optica can’t be cured, though long-term remission may be possible with the right management. Neuromyelitis optica treatment involves therapies to reverse recent symptoms and prevent future attacks.
- Relapses/Attacks – Reversing recent symptoms. In the early stage of an neuromyelitis optica attack, your doctor may give you high-dose corticosteroids, methylprednisolone (Solu-Medrol), through a vein in your arm (intravenously). You’ll be given the medication for about five days, and then the medication will be tapered off slowly over several days.
- Steroids work by dampening the immune system and reducing inflammation around the site of nerve damage. They are given:
- Intravenously (through a vein) 1g daily for 5-7 days or
- Orally (taken by mouth) 500mg-2g daily for 5-7 days,
- In combination of intravenous and oral, followed by
- A tapering course of oral steroids over several months.
- Steroids work by dampening the immune system and reducing inflammation around the site of nerve damage. They are given:
- Plasma exchange is frequently recommended as the first or second treatment, usually in addition to steroid therapy. In this procedure, some blood is removed from your body, and blood cells are mechanically separated from fluid (plasma). Doctors mix your blood cells with a replacement solution and return the blood into your body. Doctors can also help manage other symptoms you may experience, such as pain or muscle problems.
- Preventing future attacks. For long-term suppression of the disease, no specific treatment has been studied in controlled clinical trials, but a variety of immunosuppressive drugs are regarded by many clinicians as first-line therapy. Doctors may recommend that you take a lower dose of corticosteroids for an extensive period of time to prevent future neuromyelitis optica attacks and relapses. Your doctor may also recommend taking a medication that suppresses your immune system, in addition to corticosteroids, to prevent future neuromyelitis optica attacks. Immunosuppressive medications that may be prescribed include azathioprine (Imuran, Azasan), mycophenolate mofetil (Cellcept) or rituximab (Rituxan). Typically, azathioprine or mycophenolate mofetil are prescribed along with low doses of corticosteroids. Rituximab has been shown to be helpful in retrospective studies, including in patients who fail first-line immunosuppressive treatments. Immunomodulatory drugs for multiple sclerosis are ineffective, and in the case of interferon beta, there is some evidence that suggest that they may be harmful.
- Symptom treatment may also involve the use of low doses of carbamazepine to control paroxysmal (sudden) tonic spasms that often occur during attacks of neuromyelitis optica and antispasticity agents to treat long term complication of spasticity that frequently develops in those with permanent motor deficits.
Figure 10. Neuromyelitis optica treatment plan
[Source 3]Drugs commonly used in neuromyelitis optica
Oral Prednisolone tablets
Steroids are good immunosuppressants. After a diagnosis of neuromyelitis optica, oral steroids are used until other treatments are in place (Azathioprine for example can take 3-6 months to get to an effective level). In many patients relapses may occur even on gradual reduction of the steroids and they may need to continue on a low dose of steroids for longer periods. Often a maintenance dose is required.
Long-term treatment side effects including; weight gain, acne, indigestion, cataracts, osteoporosis (thinning of the bones), deterioration of the head of the thigh bone and diabetes. To reduce the side effects of Prednisolone other medication is taken such as an antacid Omeprazole or Lansoprazole, tablets for bone protection Alendronic acid and calcium supplements.
Azathioprine (also known as Immuran), Methotrexate and Mycophenolate (cellcept) have similar efficacy when it comes to suppressing the immune system. They all have side effects that are well understood, but need to be explained to you before you take the medication.
A certain percentage of patients will either not tolerate or relapse whilst on the above medications. If this happens, your doctor will consider a different medication to try and prevent relapses.
Other treatments available
These medications are considered to be “2nd line” treatments (i.e. used after trying the above medications). As with most medications, the more effective they are, the higher the risk of side effects. This is always a consideration when offering you medications.
Rituximab
This is an intravenous medication, treatment commences with 2 infusions 2 weeks apart, followed by a 6 month break until the next course which may consist of one or two infusions around 6-12 months later. It is from a family of drugs called “monoclonal antibodies” which are capable of depleting B-cells that are responsible for producing neuromyelitis optica antibodies. A version is of Rituximab called Truxima is being used widely in UK.
Cyclophosphamide
This is another well established chemotherapy that suppresses the immune system. There is very little evidence for its use in neuromyelitis optica.
Intravenous Immunoglobulins (IVIG) is a treatment made from donated blood that contains healthy antibodies. These are given to help stop the harmful antibodies damaging your nerves. Intravenous Immunoglobulins (IVIG) is given directly into a vein. Most people need treatment once a day for around five days.
Complementary Therapies
Complementary therapies can be used to target a specific physical, mental, emotional or spiritual problem, or as a preventative measure or purely for relaxation, and may increase your feeling of well-being. Reflexology, Massage, Reiki or Acupuncture may improve relaxation, sleep patterns, relieve pain or reduce stress and tension.
There is little research to show how effective many of these treatments may be.
Future Treatments for neuromyelitis optica
Future research
Eciluzimab trials are currently underway for the prevention of relapses in neuromyelitis optica. This is a five year trial and due to finish in late 2020.
Tociluzumab is being used in a small number of patients where relapses are occurring whilst they are on Rituximab infusions. It is also a monoclonal antibody which targets Interleukin-6 receptor and binds to them effectively blocking their role in the immune inflammatory response.
Future research
Over the last few years research has increased worldwide, particularly assessing immunology, radiology, causes and possible future treatments for neuromyelitis optica. However as the condition is so rare, it is difficult to organise clinical trials (and hence the need to identify as many people with neuromyelitis optica as possible).
Please speak to your local neuromyelitis optica team to get the most up to date information on trials and research.
What about stem cells?
Currently, research into stem cell treatment is only in its initial stages. Some researchers are hopeful that stem cell treatments may be helpful for people with neuromyelitis optica in the future.
Managing permanent disability
Many symptoms overlap with each other for example pain interferes with all activities such as housework, work, exercise and consequently has an impact on a person’s mood, affecting family relationships. Though problems can be tackled on their own a multi-disciplinary approach is essential to provide holistic care.
Combined efforts by doctors, nurses, occupational therapists, physiotherapists, orthoptics and social services will help the complex requirements of the individual patient. Visual aids, walking aids, motorised wheelchairs, and home adaptations can improve quality of life remarkably and many patients live an active life.
- Lennon VA, Kryzer TJ, Pittock SJ, Verkman AS, Hinson SR. IgG marker of optic-spinal multiple sclerosis binds to the aquaporin-4 water channel. J Exp Med 2005;202:473–477. http://jem.rupress.org/content/202/4/473[↩]
- Ratelade J, Verkman AS. Neuromyelitis optica: aquaporin-4 based pathogenesis mechanisms and new therapies. Int J Biochem Cel Biol 2012;44:1519–1530.[↩]
- http://www.nmouk.nhs.uk/wp-content/uploads/2011/06/NMO-Treatment-Algorithm5.pdf[↩]