Contents
What is osteochondritis dissecans
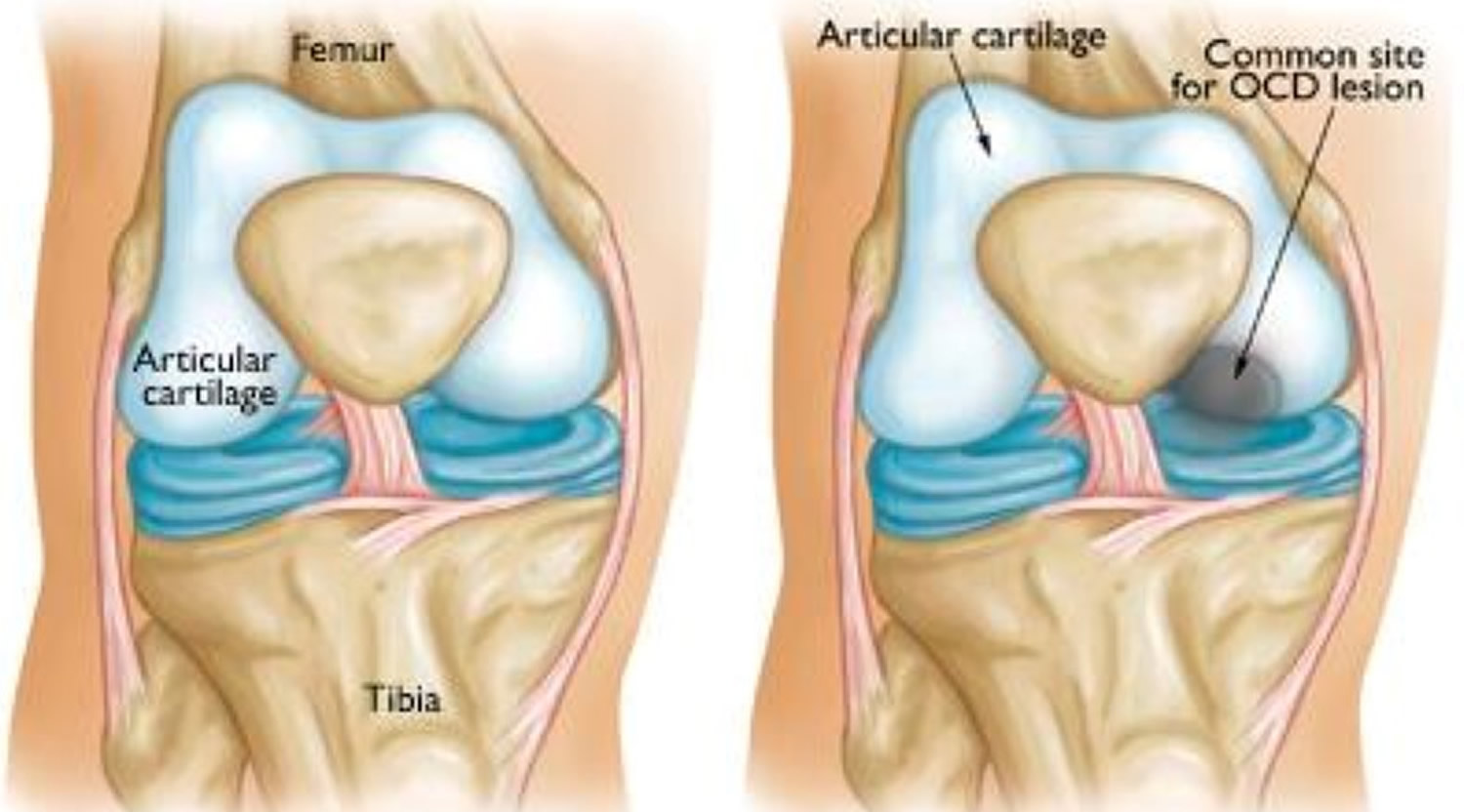
Osteochondritis dissecans is a joint condition that occurs when a piece of cartilage and the thin layer of bone beneath it, separates from the end of the bone due to a lack of blood supply. If the piece of cartilage and bone remain close to where they detached, they may not cause any symptoms. However, affected people may experience pain, weakness and/or decreased range of motion in the affected joint if the cartilage and bone travel into the joint space.
Although osteochondritis dissecans can affect people of all ages, it is most commonly diagnosed in people between the ages of 10 and 20 years, with approximately a 2:1 male to female ratio 1. Trauma is the most recognized cause of osteochondritis dissecans. However, in most cases, the exact underlying cause is unknown. Rarely, osteochondritis dissecans can affect more than one family member (called familial osteochondritis dissecans); in these cases, osteochondritis dissecans is caused by changes (mutations) in the ACAN gene and is inherited in an autosomal dominant manner 2.
Osteochondritis dissecans can cause symptoms either after an injury to a joint or after several months of activity, especially high-impact activity such as jumping and running, that affects the joint. Osteochondritis dissecans occurs most commonly in the knee, but also occurs in elbows, ankles and other joints. Osteochondritis dissecans typically affects just one joint, however, some children can develop osteochondritis dissecans in several joints.
Doctors stage osteochondritis dissecans according to the size of the injury, whether the fragment is partially or completely detached, and whether the fragment stays in place. If the loosened piece of cartilage and bone stays in place, you may have few or no symptoms. In many cases of osteochondritis dissecans in young children whose bones are still developing, the affected bone and cartilage heal on their own. In grown children and young adults, osteochondritis dissecans can have more severe effects. The osteochondritis dissecans lesions have a greater chance of separating from the surrounding bone and cartilage, and can even detach and float around inside the joint.
Treatment for osteochondritis dissecans varies depending on many factors, including the age of the affected person and the severity of the symptoms, but may include rest; casting or splinting; surgery and/or physical therapy.
Surgery might be necessary if the fragment comes loose and gets caught between the moving parts of your joint or if you have persistent pain.
Osteochondritis dissecans knee
Osteochondritis dissecans mostly appears at the knee joint on the weight-bearing part of the medial femoral condyle (range 70-85% of cases) 3, but the weight-bearing surfaces of the lateral femoral condyle, tibia or patella may also be involved. Osteochondritis dissecans of the knee is a common cause of knee pain and dysfunction among skeletally immature and young adult patients. Osteochondritis dissecans is increasingly frequently seen in pediatric, adolescent and young adult athletes. If it is not recognized and treated appropriately, it can lead to secondary osteoarthritis with pain and functional limitation.
There is a history of trauma to the knee in 40% of patients. About 50% of the loose bodies in knee are due to osteochondritis dissecans lesions. Males are 3 times more likely to be affected than females.
Osteochondritis dissecans knee has a characteristic distribution 4:
- medial condyle: ~78.5% (range 70-85%)
- “classic” lateral surface of the medial condyle: ~70%
- lateral condyle: 15%
- inferocentral portion: 13%
- anterior surface: 2%
- patella: ~7.5% (range 5-10%)
- typically inferomedial
- patellofemoral groove (femoral trochlea): <1%
- weight-bearing surface of the tibia: uncommon
Although a direct trauma to the knee could result in a transchondral fracture, the classic location of osteochondritis dissecans in the posterolateral portion of the medial femoral condyle suggests that indirect trauma is a more likely cause. Repeated impingement of the tibial spine on the lateral aspect of the medial femoral condyle during internal rotation of the tibia has also been suggested to be a contributing factor 5.
Frequently osteochondritis dissecans of the knee present insidiously without a traumatic event as a painful knee with vague, poorly localized symptoms. The pain usually is only with the weightbearing and does not develop at rest. Sometimes “locking”, “popping”, or “clicking” will also be present with knee motion and walking. Swelling is variable.
The primary prognostic factors are patient age and skeletal maturity. The less mature the patient, the better the prognosis, with best results seen in the juvenile form (before adolescence), where full recovery is the usual outcome. In the adolescent type (partial skeletal maturity), outcome is unpredictable. With the adult type (skeletally mature), a guarded prognosis is the rule.
In the literature, the occurrence in the right knee joint is described frequently 6. Osteochondritis dissecans of the knee may be bilateral in 20-25% of cases. In a study of 47 knees that examined osteochondritis dissecans lesion reossification on serial plain films over 6 months of nonoperative treatment, Wall et al 7 found that smaller-sized lesions were more likely to progress to healing. They also found that patient age, lesion sidedness (left knee vs right), and lesion location (lateral vs medial femoral condyle) did not play a role in predicting healing potential. Similarly, in a study of 59 osteochondritis dissecans lesions, Edmonds et al 8 found a significant difference in the rate of healing between small and large lesions. Spontaneous healing is usual unless there is an unstable fragment. Signs of instability include large size (>1cm), cyst-like lesions beneath a fragment, contrast beneath a fragment on contrast arthrography, and loose body.
In children with open growth plates, there is a higher chance for spontaneous healing with activity modification or immobilization than in adults. If the articular surface is intact, protected activities and possible crutch use for 2-3 months may produce healing. This is especially true in girls younger than the age of 11 and boys younger than 13 years of age. If the articular surface is disrupted or there is a loose fragment, immobilization is unlikely to succeed, and surgical treatment is usually advocated.
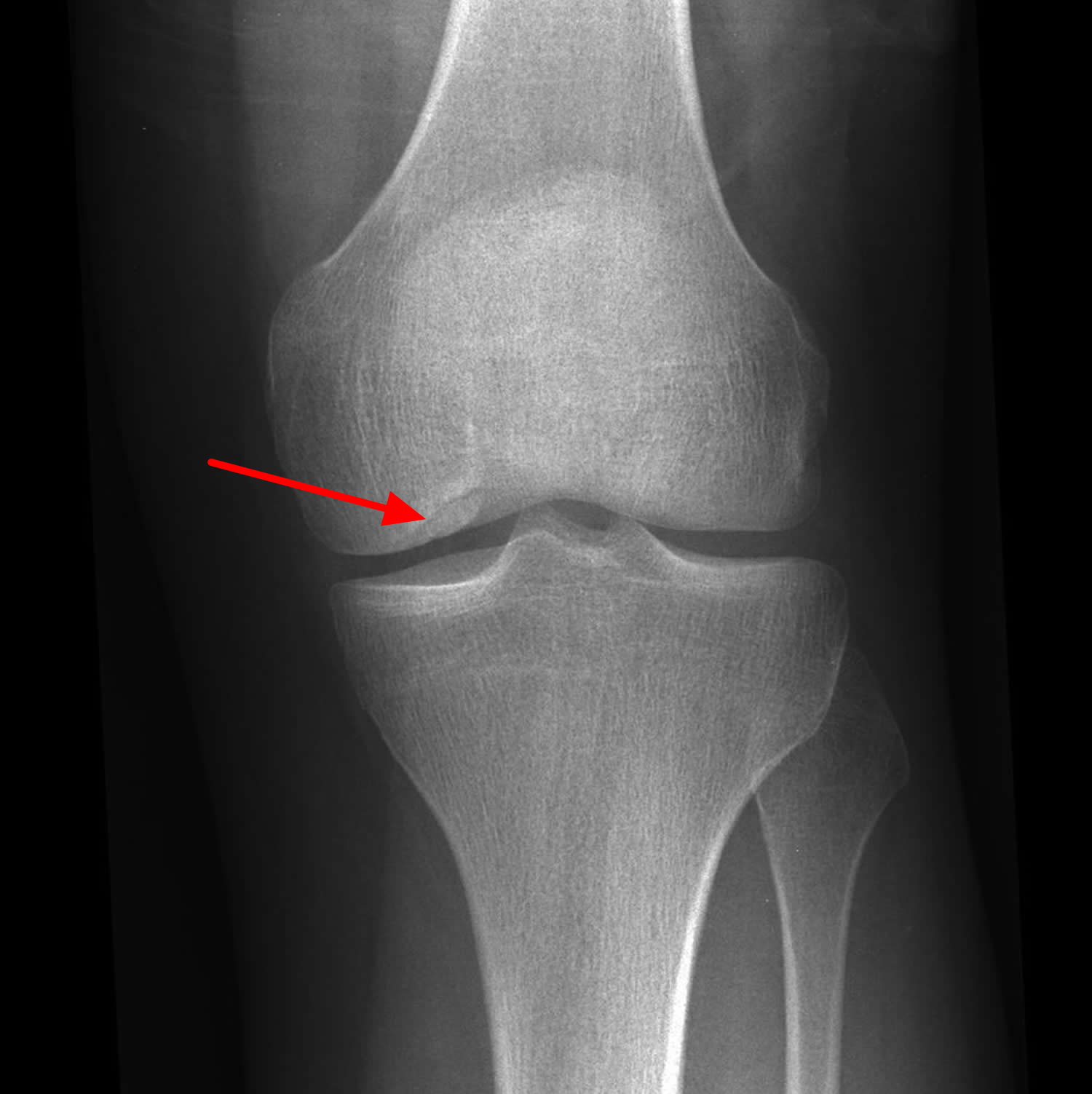
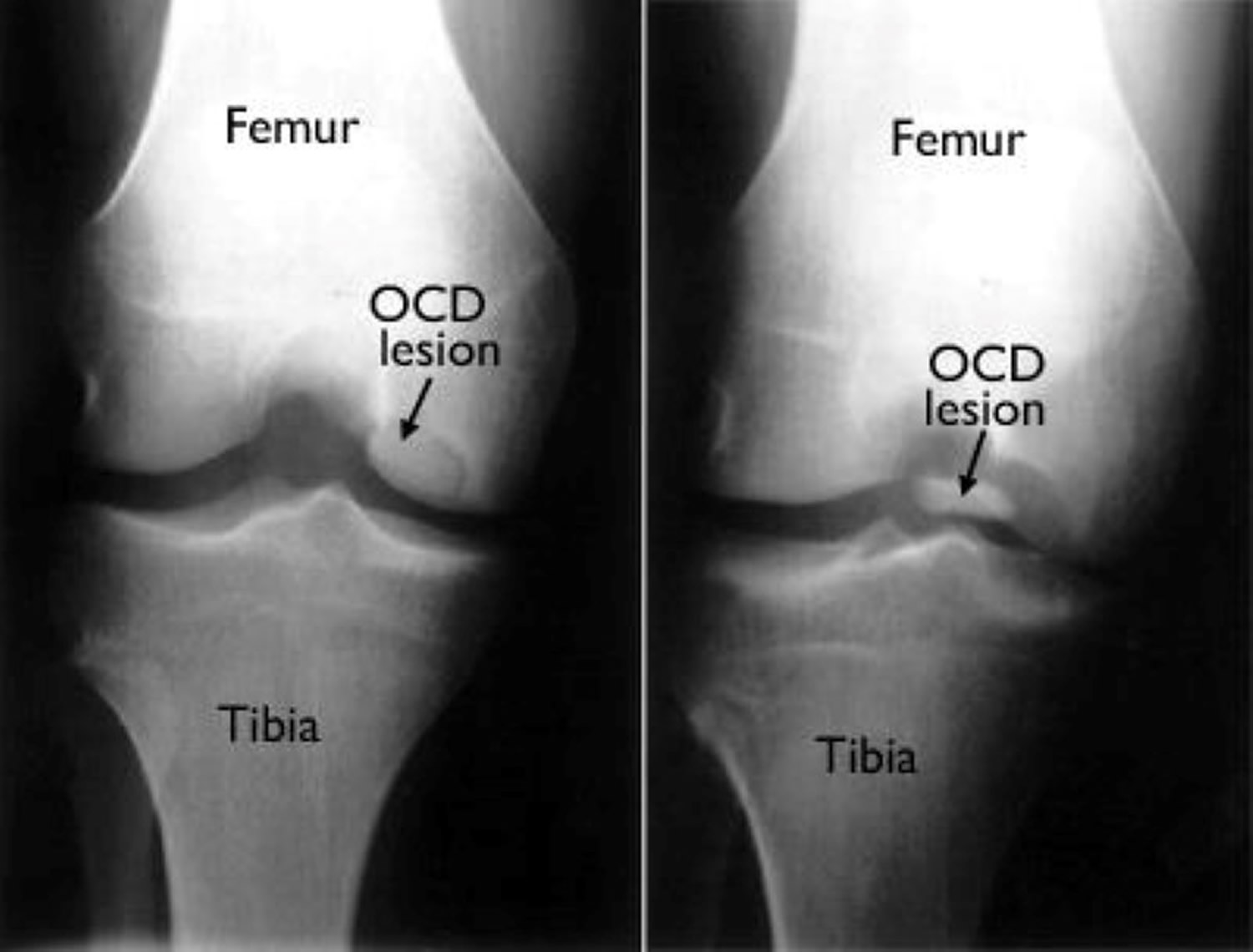
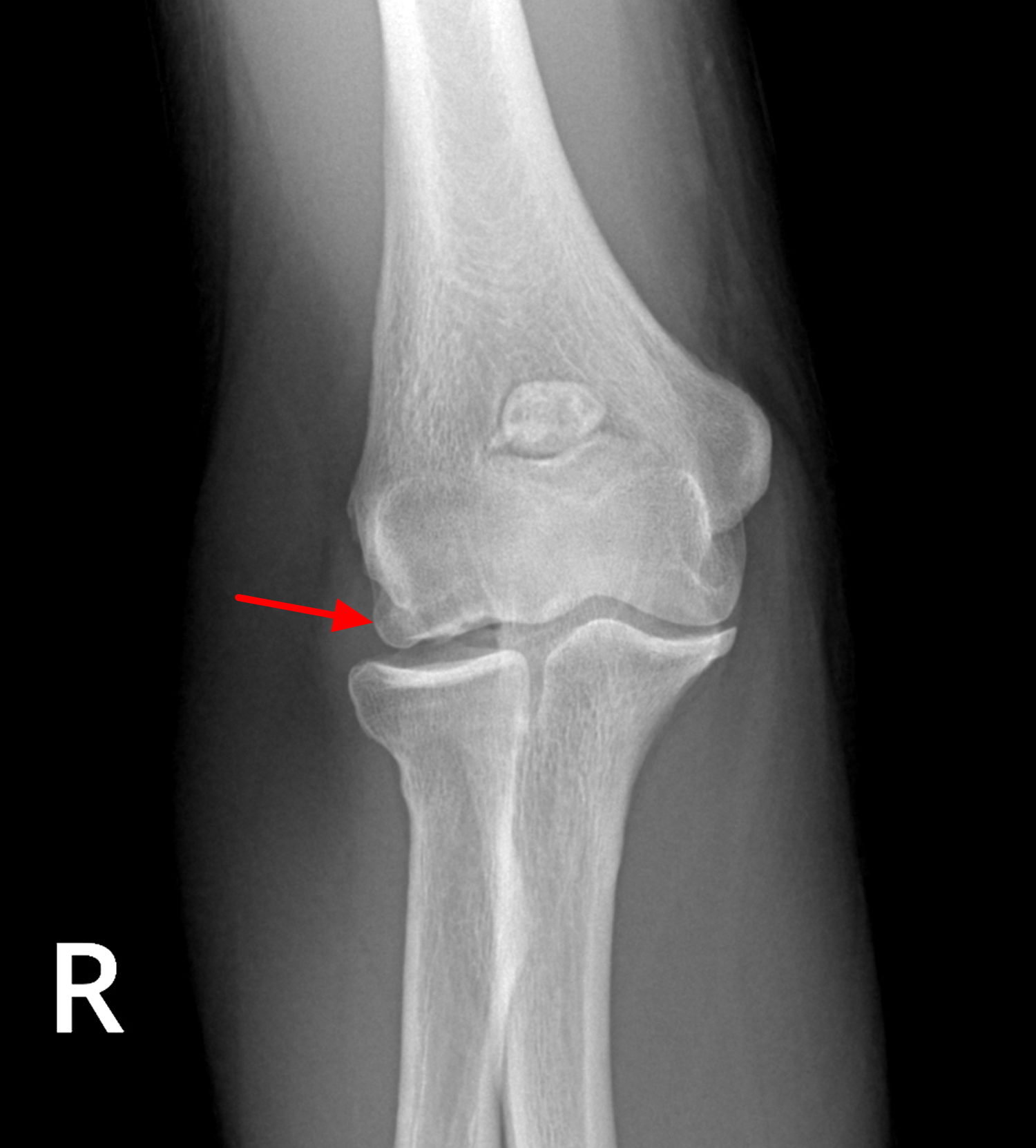
Figure 1. Osteochondritis dissecans knee
Figure 2. Osteochondritis dissecans knee
Note: These x-rays show osteochondritis dissecans of the knee in a skeletally mature adolescent. (Left) An osteochondritis dissecans lesion at the end of the femur. (Right) The lesion has detached from the femur and is floating within the knee joint.
Osteochondritis dissecans ankle
May be asymptomatic for a long period. A common complaint is an intermittent weight-bearing pain. When there is a loose body within the joint, symptoms may be more severe and include intense pain, swelling, instability during walking, and locking.
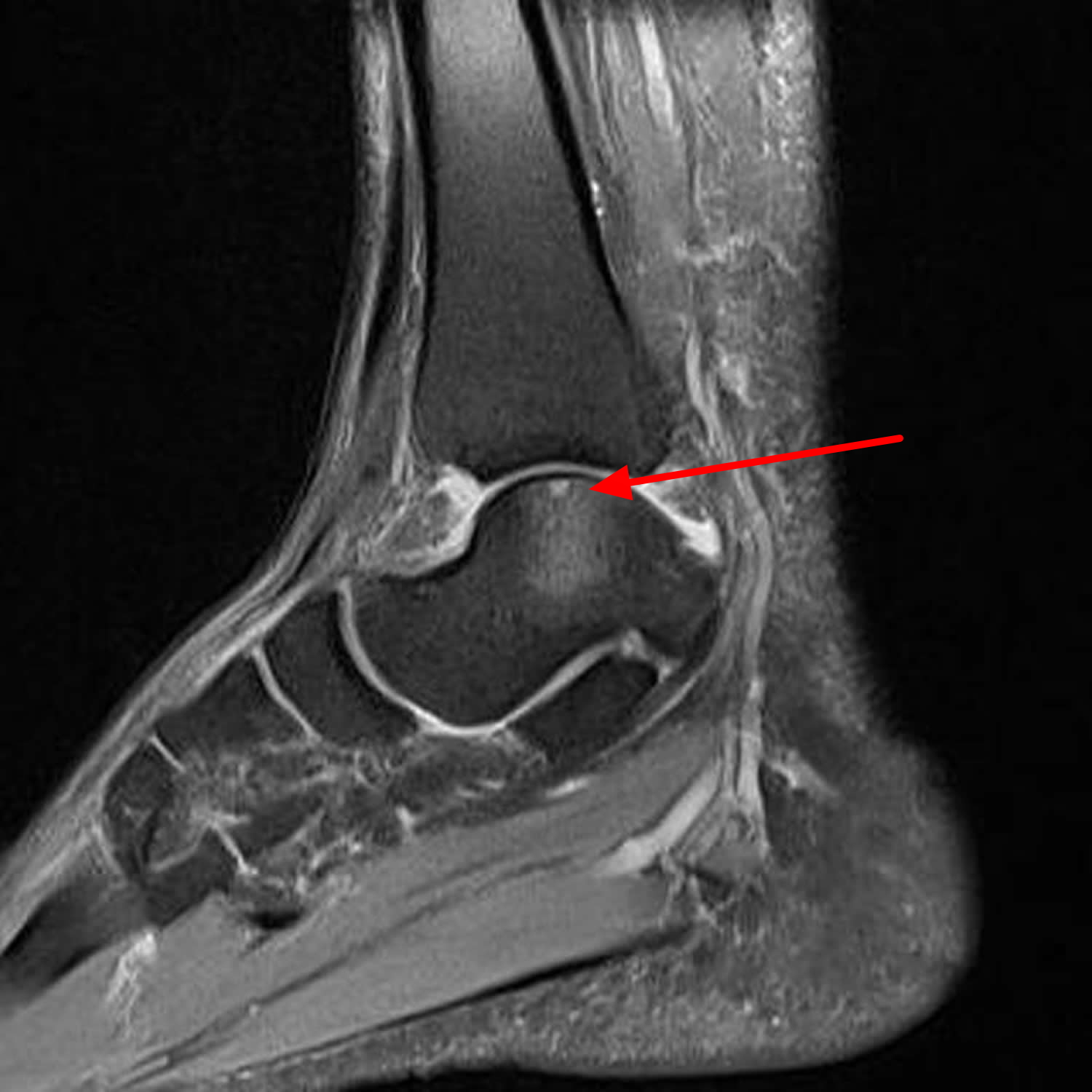
Figure 3. Osteochondritis dissecans talus MRI – note subchondral altered signals of talar dome with subchondral cyst and marrow edema.
Osteochondritis dissecans elbow
Elbow involvement in osteochondritis dissecans is rare. It is defined as a localised fragmentation of bone overlying the capitellum cartilage. In the elbow, the capitellum and the radius touch to absorb some of the pressure transmitted from the wrist. In certain sports, like baseball and gymnastics, and in professions that require heavy lifting, more pressure than normal is transmitted to the outside of the elbow. Most commonly seen in young baseball pitchers.
Clinical features may include:
- pain along the outside (lateral) of elbow that is worse with throwing or lifting heavy objects
- something catching in the elbow or that the elbow locks up
- swelling
- laxity of medial collateral ligament
Figure 4. Osteochondritis dissecans elbow
Osteochondritis dissecans classification
Osteochondritis dissecans classification according to International Cartilage Repair Society 9.
Osteochondritis dissecans can be classified at surgery into 4 stages:
Stage I
- stable
- lesion in continuity with the host bone
- covered by intact cartilage
Stage II
- stable on probing
- partial discontinuity of the lesion from the host bone
Stage III
- unstable on probing
- fragment not dislocated
- complete discontinuity of the “dead in situ” lesion
Stage IV
- dislocated fragment
Osteochondritis dissecans complications
Osteochondritis dissecans can increase your risk of eventually developing osteoarthritis in that joint.
Osteochondritis dissecans causes
In most cases, the exact underlying cause of osteochondritis dissecans is not completely understood. Scientists suspect that it may be due to decreased blood flow to the end of the affected bone, which may occur when repetitive episodes of minor injury and/or stress damage a bone overtime 10.
Trauma
The majority of osteochondritis dissecans cases thought to be the result of trauma 11. In up to 40% of cases, patients give a history of trauma as the inciting event 1. Other postulated causes include 11:
- avascular necrosis
- fat emboli
- microtrauma
- familial dysplasia
Ischemia
Ischemia has been investigated as a potential cause of osteochondritis dissecans. Enneking 12 found the vascular supply to the subchondral bone to be similar to the vascular supply to the bowel mesentery, with poor anastomoses to surrounding arterioles. This propensity for ischemia would naturally lead subchondral bone to form sequestra, making it particularly vulnerable to traumatic insult, resultant fracture, and potential separation. Instead, Rogers and Gladstone 13 studied the vascularity of the distal part of the femur and found numerous anastomoses to intramedullary cancellous bone.
Genetics
In some families, osteochondritis dissecans is caused by changes (mutations) in the ACAN gene. In these cases, which are referred to as familial osteochondritis dissecans, the condition generally affects multiple joints and is also associated with short stature and early-onset osteoarthritis. The ACAN gene encodes a protein that is important to the structure of cartilage. Mutations in this gene weaken cartilage, which leads to the various signs and symptoms of familial osteochondritis disssecans.
Risk factors for osteochondritis dissecans
Osteochondritis dissecans occurs most commonly in children and adolescents between the ages of 10 and 20 who are highly active in sports.
Osteochondritis dissecans symptoms
Depending on the joint that’s affected, signs and symptoms of osteochondritis dissecans might include:
- Pain. This most common symptom of osteochondritis dissecans might be triggered by physical activity — walking up stairs, climbing a hill or playing sports.
- Swelling and tenderness. The skin around your joint might be swollen and tender.
- Joint popping or locking. Your joint might pop or stick in one position if a loose fragment gets caught between bones during movement.
- Joint weakness. You might feel as though your joint is “giving way” or weakening.
- Decreased range of motion. You might be unable to straighten the affected limb completely.
Osteochondritis dissecans diagnosis
During the physical exam, your doctor will press on the affected joint, checking for areas of swelling or tenderness. In some cases, you or your doctor will be able to feel a loose fragment inside your joint. Your doctor will also check other structures around the joint, such as the ligaments.
Your doctor will also ask you to move your joint in different directions to see if the joint can move smoothly through its normal range of motion.
Imaging tests
Your doctor might order one or more of these tests:
- X-rays. X-rays can show abnormalities in the joint’s bones.
- MRI. Using radio waves and a strong magnetic field, an MRI can provide detailed images of both hard and soft tissues, including the bone and cartilage. If X-rays appear normal but you still have symptoms, your doctor might order an MRI.
- CT. This technique combines X-ray images taken from different angles to produce cross-sectional images of internal structures. CT scans allow your doctor to see bone in high detail, which can help pinpoint the location of loose fragments within the joint.
Osteochondritis dissecans treatment
The primary aim of treatment for osteochondritis dissecans is to restore normal function of the affected joint, relieve pain and prevent osteoarthritis. No single treatment works for everybody. Treatment for the condition varies depending on many factors including the age of the affected person and the severity of the symptoms. In children and young teens whose bones are still growing, osteochondritis dissecans often heals overtime without surgical treatment. These cases are often managed with rest and in some cases, crutches and/or splinting to relieve pain and swelling. In general, most children start to feel better over a 2- to 4-month course of rest and nonsurgical treatment. They usually return to all activities as symptoms improve.
Initially, your doctor will likely recommend conservative measures, which might include:
- Resting your joint. Avoid activities that stress your joint, such as jumping and running if your knee is affected. You might need to use crutches for a time, especially if pain causes you to limp. Your doctor might also suggest wearing a splint, cast or brace to immobilize the joint for a few weeks.
- Physical therapy. Most often, this therapy includes stretching and range-of-motion exercises and strengthening exercises for the muscles that support the involved joint. Physical therapy is commonly recommended after surgery, as well.
Surgery
Your doctor may recommend surgery if:
- Nonsurgical treatment fails to relieve pain and swelling
- The lesion is separated or detached from the surrounding bone and cartilage, moving around within the joint
- The lesion is very large (greater than 1 centimeter in diameter), especially in older teens
The type of surgery will depend on the size and stage of the injury and how mature your bones are.
There are different surgical techniques for treating osteochondritis dissecans, depending upon the individual case.
- Drilling into the lesion to create pathways for new blood vessels to nourish the affected area. This will encourage healing of the surrounding bone.
- Holding the lesion in place with internal fixation (such as pins and screws).
- Replacing the damaged area with a new piece of bone and cartilage (called a graft). This can help regenerate healthy bone and cartilage in the area damaged by osteochondritis dissecans.
Following surgery, physical therapy is often necessary to improve the strength and range of motion of the affected joint.
In general, crutches are required for about 6 weeks after surgical treatment, followed by a 2- to 4-month course of physical therapy to regain strength and motion in the affected joint.
A gradual return to sports may be possible after about 4 to 5 months.
- Michael JW, Wurth A, Eysel P et-al. Long-term results after operative treatment of osteochondritis dissecans of the knee joint-30 year results. Int Orthop. 2008;32 (2): 217-21. doi:10.1007/s00264-006-0292-7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2269012/[↩][↩]
- Familial osteochondritis dissecans. Genetics Home Reference. https://ghr.nlm.nih.gov/condition/familial-osteochondritis-dissecans[↩]
- Funke E, Munzinger U, Marty M, Drobny T (1994) Operative Langzeitresultate der Osteochondrosis dissecans des Kniegelenkes bei Jugendlichen unter 16 Jahren. Z Unfallchirurg Vers Med Band 87(3):178–185 https://www.ncbi.nlm.nih.gov/pubmed/7986640[↩]
- Zanon G, DI Vico G, Marullo M. Osteochondritis dissecans of the knee. (2014) Joints. 2 (1): 29-36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295664/[↩]
- Disease-specific clinical problems associated with the subchondral bone. Pape D, Filardo G, Kon E, van Dijk CN, Madry H. Knee Surg Sports Traumatol Arthrosc. 2010 Apr; 18(4):448-62. https://www.ncbi.nlm.nih.gov/pubmed/20151111/[↩]
- Venbrocks R, Albrecht T (1992) Ergebnisse der konservativen und operativen Therapie der Osteochondrosis dissecans des Kniegelenkes. Arthroskopie 5:6–9[↩]
- Wall EJ, Vourazeris J, Myer GD, et al. The healing potential of stable juvenile osteochondritis dissecans knee lesions. J Bone Joint Surg Am. 2008;90(12):2655–2664. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2663329/[↩]
- Edmonds EW, Albright J, Bastrom T, Chambers HG. Outcomes of extra-articular, intra-epiphyseal drilling for osteochondritis dissecans of the knee. J Pediatr Orthop. 2010;30(8):870–878. https://www.ncbi.nlm.nih.gov/pubmed/21102215[↩]
- Boutin Robert D., Jennifer A. Januario, Arthur H. Newberg et al. “MR Imaging Features of Osteochondritis Dissecans of the Femoral Sulcus.” Am. J. Roentgenol. 180, no. 3 (March 1, 2003): 641-645. https://www.ajronline.org/doi/full/10.2214/ajr.180.3.1800641[↩]
- Grant Cooper, MD. Osteochondritis Dissecans. http://emedicine.medscape.com/article/1253074-overview#a0112[↩]
- Maeurer J. Imaging strategies for the knee. Thieme Publishing Group. (2006) ISBN:3131405619.[↩][↩]
- Enneking WF. Clinical Musculoskeletal Pathology. Ed 3. Gainesville, Florida: University of Florida Press; 1990. p. 166.[↩]
- Rogers WM, Gladstone H. Vascular foramina and arterial supply of the distal end of the femur. J Bone Joint Surg Am. 1950;32( A:4):867–874. https://www.ncbi.nlm.nih.gov/pubmed/14784497[↩]