Contents
Pancreas divisum
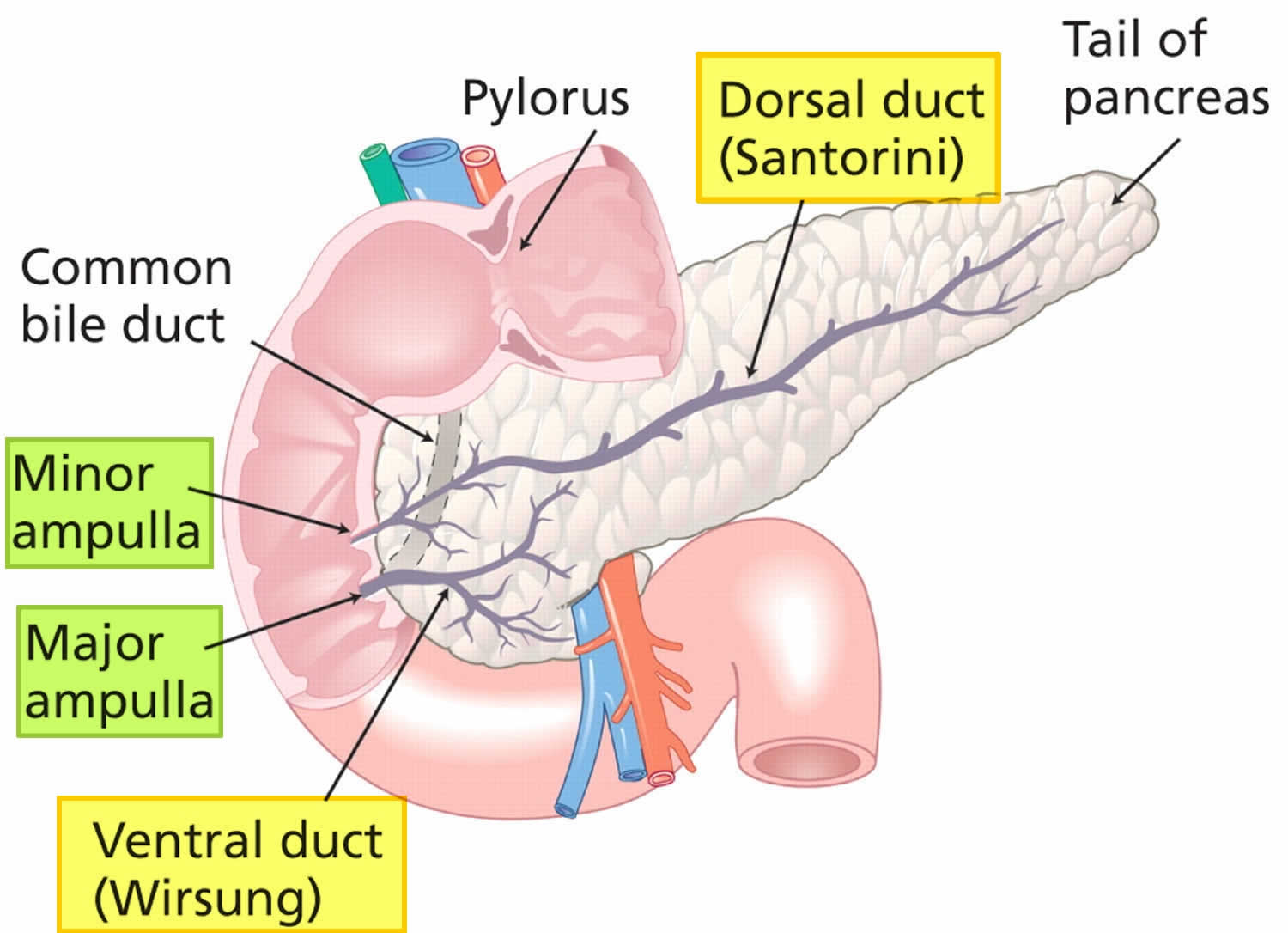
Pancreas divisum is the most common congenital (birth defect present at birth) anatomic variation of the pancreatic duct system in which the dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct) fail to fuse 1, 2, 3, 4, 2, 5, 6, 7, 8, 9, 10. As a result of nonunion of the dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct), a major portion of pancreatic exocrine secretions (exocrine gland secretes digestive enzymes) enter the duodenum via the dorsal pancreatic duct (duct of Santorini) and minor papilla (Figure 1) 11, 12, 13. In pancreas divisum, the majority of the pancreatic exocrine gland secretions drain into the minor papilla via the duct of Santorini, whereas the posterior head and uncinate process drain into the major papilla via the duct of Wirsung with the common bile duct 14. Rarely, pancreas divisum is associated with a focal cystic dilation of the terminal portions of the duct of Santorini, which is termed as a Santorinicele can also be visualized on an secretin-enhanced MRCP (S-MRCP) 8, 15, 16.
Pancreas divisum drainage through the minor papilla (instead of the major papilla) can result in inadequate pancreatic exocrine secretions drainage and pain caused by obstruction and pancreatitis in a small number of patients with pancreas divisum 17. Obstructive symptoms and pancreatitis typically affect adults. Pancreas divisum is reported in 3%–7% of cases of acute pancreatitis 11, 18, 19. Pancreas divisum underlies 12%–50% of cases of acute pancreatitis in patients whose pancreatitis would otherwise be considered idiopathic 17. However, no clear association exists between pancreas divisum and chronic pancreatitis 20.
Compared with patients with normal pancreatic anatomy who have pancreatitis, patients whose pancreatitis is a result of pancreas divisum are typically younger, less likely to drink alcohol, more likely to be female and more likely to have a pattern of recurrent acute pancreatitic attacks 17. Pancreas divisum may have a genetic component, including mutations or variants of the cystic fibrosis transmembrane conductance regulator gene (e.g., IVS8-5T variant) 21. However, the exact relation between genetic markers and pancreas divisum is unknown.
Pancreas divisum occurs in approximately 7% of autopsy series (range, 1% to 14%) 22. The frequency of finding pancreatic divisum varies greatly in endoscopic retrograde cholangiopancreatography (ERCP) series (4%-25%), depending on the population studied and the degree to which a complete pancreatogram is obtained 22. Pancreas divisum has geographic variations and is found in approximately 4%-10% of the white population and 1%-2% of the Asian population 23, 24, 25. Geographic variation could be secondary to the diagnostic procedure used.
Pancreas divisum has been found to be associated with other pancreatic and biliary anomalies 2. The most frequent association is with annular pancreas where there is an abnormal rotation of the ventral bud of the pancreas around the duodenum, leading to a ring or semi-ring of pancreatic tissue around the second part of the duodenum 26. Prior studies suggested that there is about a 30–38% co-existence between the two conditions 26, 27, 28 but a recent larger study suggested the prevalence is as high as 50% 29. There have been reports scattered in the literature with pancreas divisum co-existing with anomalous pancreatic-biliary junction and choledochal cysts 30, 31, 32, 33, 34. However, there have been no large-scale studies to support any specific associations between these congenital anomalies. It has also been reported recently that there is a higher prevalence of pancreatic and biliary tumors in patients with pancreas divisum than with a normal ductal system. (7.8% vs 3.5%) 35. There have been reports of partial agenesis of the dorsal pancreas with pancreas divisum with some debate as to whether the agenesis led to the pancreas divisum or a consequence 36, 37.
Patients with pancreas divisum who are otherwise well (e.g., those whose pancreas divisum is discovered during imaging done for another purpose) can be reassured that they have only a 5%–10% lifetime risk of developing pancreatitis 38, which is similar to the risk in the general population 39. In many cases, the patient might not have any symptoms.
A diagnosis of pancreas divisum does not routinely warrant treatment, especially when pancreas divisum is found incidentally on imaging and asymptomatic. The treatment of pancreas divisum generally involves symptomatic management.
In symptomatic patients, the choice of therapy and degree of intervention depends on the frequency, duration and intensity of symptoms and presence of complications. The approach and options for therapy of pancreatic disease remain the same irrespective of the variations in the pancreatic ductal system with a few exceptions/modifications for pancreas divisum.
In patients with infrequent or mild symptoms of pancreatic-type abdominal pain and no radiological features to suggest chronic pancreatitis, a conservative approach directed towards symptom management would be preferred over an intervention of the minor papilla or the dorsal pancreatic duct. Options include a low-fat diet (50 gm/day), non-narcotic analgesics, anti-spasmodic/anti-cholinergic medications and pancreatic enzyme supplementation 2.
In patients with acute pancreatitis and its complications, chronic pancreatitis and its complications leading to significant functional impairment, a comprehensive evaluation for the underlying etiology should be undertaken 2. This should include a detailed social and family history, medication history, genetic testing and evaluation of metabolic causes of pancreatic disease and direct therapy towards reduction of the inciting cause and risk factors 2.
Therapeutic intervention is reserved for patients with recurrent attacks of acute pancreatitis regardless of severity and can be considered in patients with one attack of severe pancreatitis with no other identifiable cause for the disease 2. Therapy is also offered in chronic pancreatitis if a modifiable target such as a stone, stricture or dilated dorsal duct can be identified. More commonly, in the setting of pancreas divisum and chronic pancreatitis, the entire gland is involved with changes of chronic pancreatitis and treatment should be recommended as it would in patients with normal pancreatic duct anatomy 2.
The primary management when the dorsal duct is normal, near normal or just dilated is directed towards relieving obstruction at the level of the minor papilla. Options for therapy include endoscopy (i.e. endoscopic retrograde cholangiopancreatography [ERCP]) and surgery. The choice of therapy depends on patient profile and preference as well as local institutional expertise. It is important not to ignore the standard management principles of acute pancreatitis as well.
In patients with symptomatic pancreas divisum, papillotomy of the minor papilla, with or without plastic stent implantation, is the first choice for therapeutic intervention. The surgery generally involves the widening of the minor papilla (opening the vent of the dorsal duct into the small intestine) and increasing the flow of the pancreatic juices. The gastroenterologist might insert a stent into the duct for further closure and blockage.
Pancreas divisum key points 2:
- Pancreas divisum is the most common birth defect of the pancreas and occurs due to a failure of fusion of the ductal systems of the dorsal and ventral pancreatic buds in the seventh week of intra-uterine life. This leads to a dominant dorsal pancreatic duct draining through the minor papilla and a small ventral pancreatic duct draining through the major papilla. The prevalence in the western population is about 10% with a lower frequency of 1–2% in Asians and Africans.
- More than 95% of patients with pancreas divisum lack pancreatic symptoms, with the pancreatic divisum found incidentally on abdominal imaging (e.g., Computerized Tomography, Magnetic Resonance Cholangiopancreatography) performed for unrelated symptoms and indications.
- The causal role and clinical significance of pancreas divisum in pancreatic disease such as pancreatic-type abdominal pain (intermittent or chronic), acute pancreatitis or chronic pancreatitis has been suggested based on its increased incidence in the idiopathic recurrent acute pancreatitis population, pathologic studies suggesting pancreatic disease limited to the dorsal pancreas and improvement in outcome following minor papilla interventions. However, this remains debatable with no clear causality identified.
- Pancreas divisum has been demonstrated to predispose to pancreatic disease in association with other factors such has genetic mutations of SPINK-1, CFTR, CTRC and therefore should be checked in pertinent clinical situations.
- Pancreas divisum has also been shown to decrease the threshold for other known causes of pancreatic disease such as alcohol, medications, toxins, trauma.
- Secretin augmented magnetic resonance cholangiopancreatography (S-MRCP) is the non-invasive imaging modality of choice for diagnosing pancreas divisum.
- The pathogenesis of pancreatic disease in pancreas divisum is not clearly defined but is believed to be due to an imbalance between the drainage of a larger and longer dominant dorsal pancreatic duct opening through a relatively smaller or stenotic minor papilla, causing inadequate drainage of pancreatic secretions and transient obstruction of flow. The resultant increase in intraductal pressure and distention of the dorsal duct may then lead to abdominal pain and pancreatitis.
- No further pancreatic evaluation or therapy is needed or recommended in patients with asymptomatic pancreas divisum.
- In patients deemed to be symptomatic from pancreas divisum, after a comprehensive evaluation for causes of pancreatic disease is completed, therapy is offered for patients suffering from recurrent attacks of acute pancreatitis and can be considered for a severe attack of acute pancreatitis and its complications, chronic pancreatitis and its associated complications and chronic pancreatic-type abdominal pain causing significant functional impairment and debility. It is important not to ignore the standard management principles of acute and chronic pancreatitis.
- In patients with mild or infrequent symptoms of pancreatic-type abdominal pain, conservative management is pursued and directed towards symptom control.
- Endoscopic Retrograde Cholangiopancreatography (ERCP) with minor papilla endotherapy is the current first line of therapy. Minor papilla sphincterotomy is the predominant intervention due to the adverse event profile of balloon dilation of the minor papilla and long-term pancreatic stents. The procedure-related risk profile is similar to that of major papilla pancreatic sphincterotomy in high-risk patients.
- Minor papilla surgical therapy has a comparable outcome with endotherapy but due to a less favorable adverse event profile is currently reserved for patients who fail endoscopic intervention. The choice of endoscopic or surgical therapy also depends on patient profile and preference as well as local institutional expertise.
- The response to either endoscopic or surgical therapy is variable with maximal benefit seen in patients with recurrent acute pancreatitis, less with chronic pancreatitis and least with chronic pancreatic-type abdominal pain.
- Data supporting either endoscopic or surgical therapy are of low quality as the studies are predominantly retrospective with a relatively short follow-up period.
- In patients who fail minor papilla therapy, management is directed towards symptom control, with options including periods of pancreas rest with post-ligament of Treitz enteral feeding, celiac plexus block, somatostatin analogues and placement of an intrathecal pain pump.
- Additional surgical options including a pancreatojejunostomy (Puestow or Frey procedure) or a total pancreatectomy with auto- islet cell transplantation may be an option for a subset of patients.
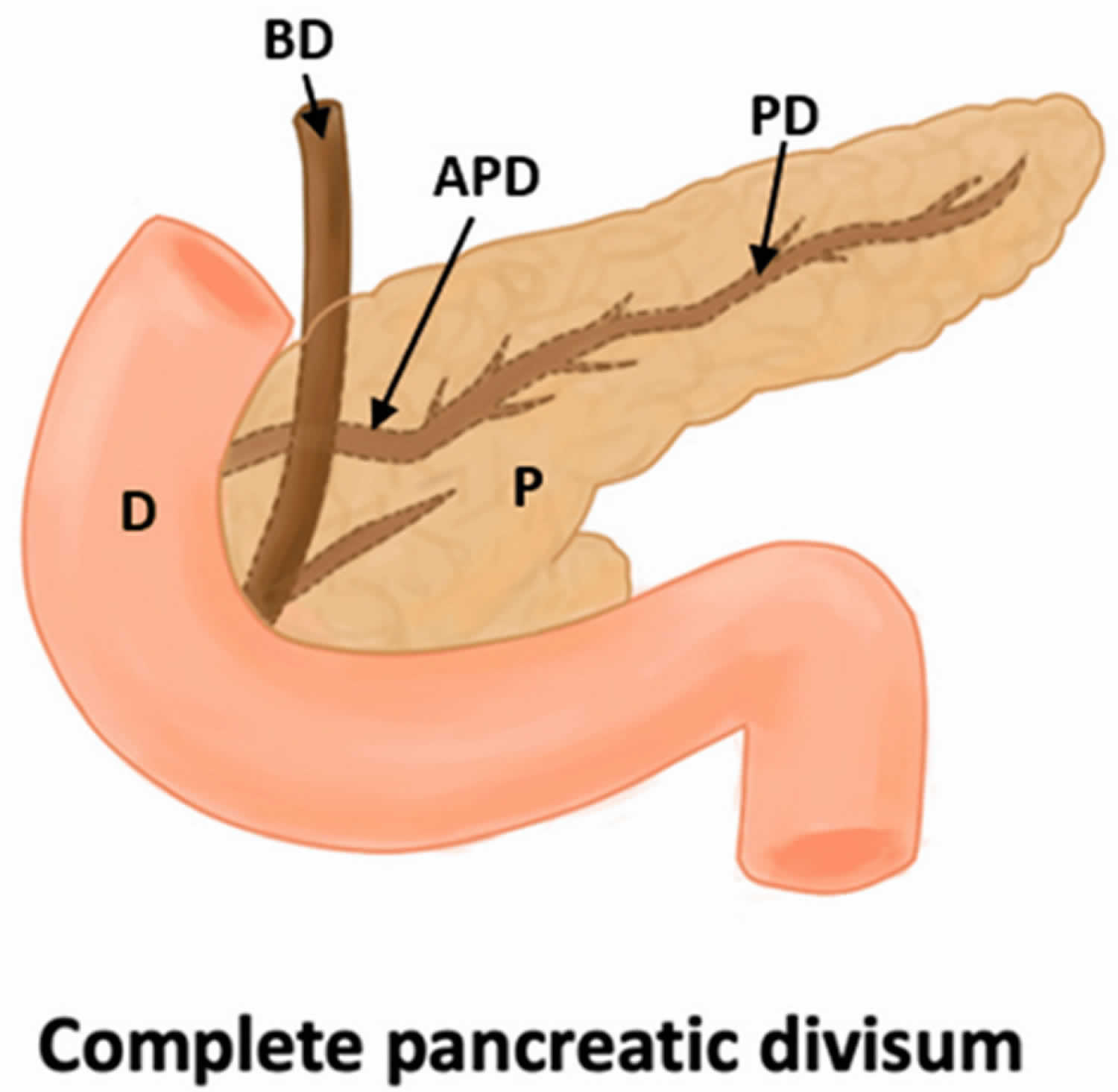
Figure 1. Pancreas divisum
Footnote: Pancreas divisum where the dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct) fail to fuse. As a result of nonunion of the dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct), a major portion of pancreatic exocrine secretions enter the duodenum via the dorsal pancreatic duct (duct of Santorini) and minor papilla (minor ampulla).
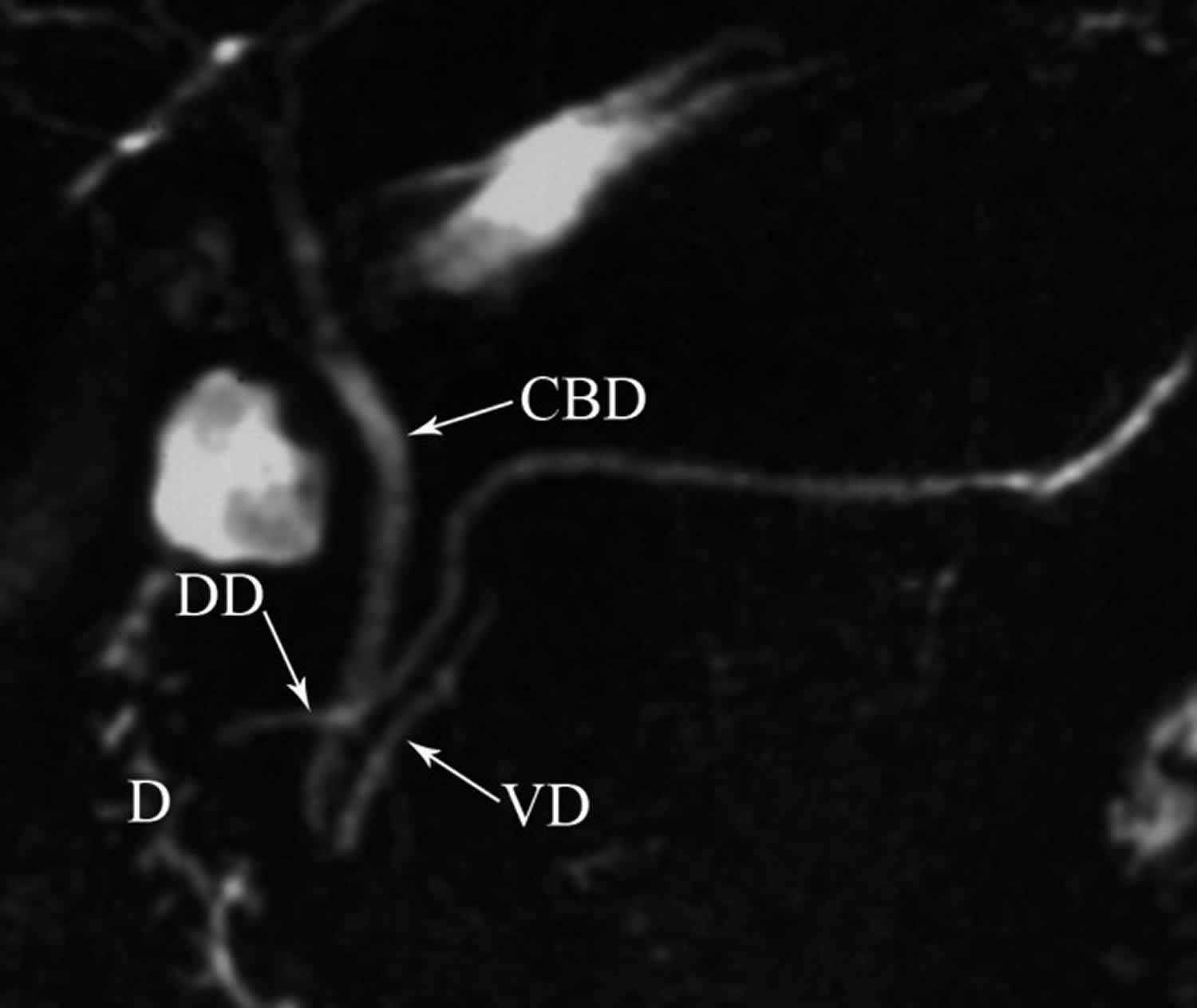
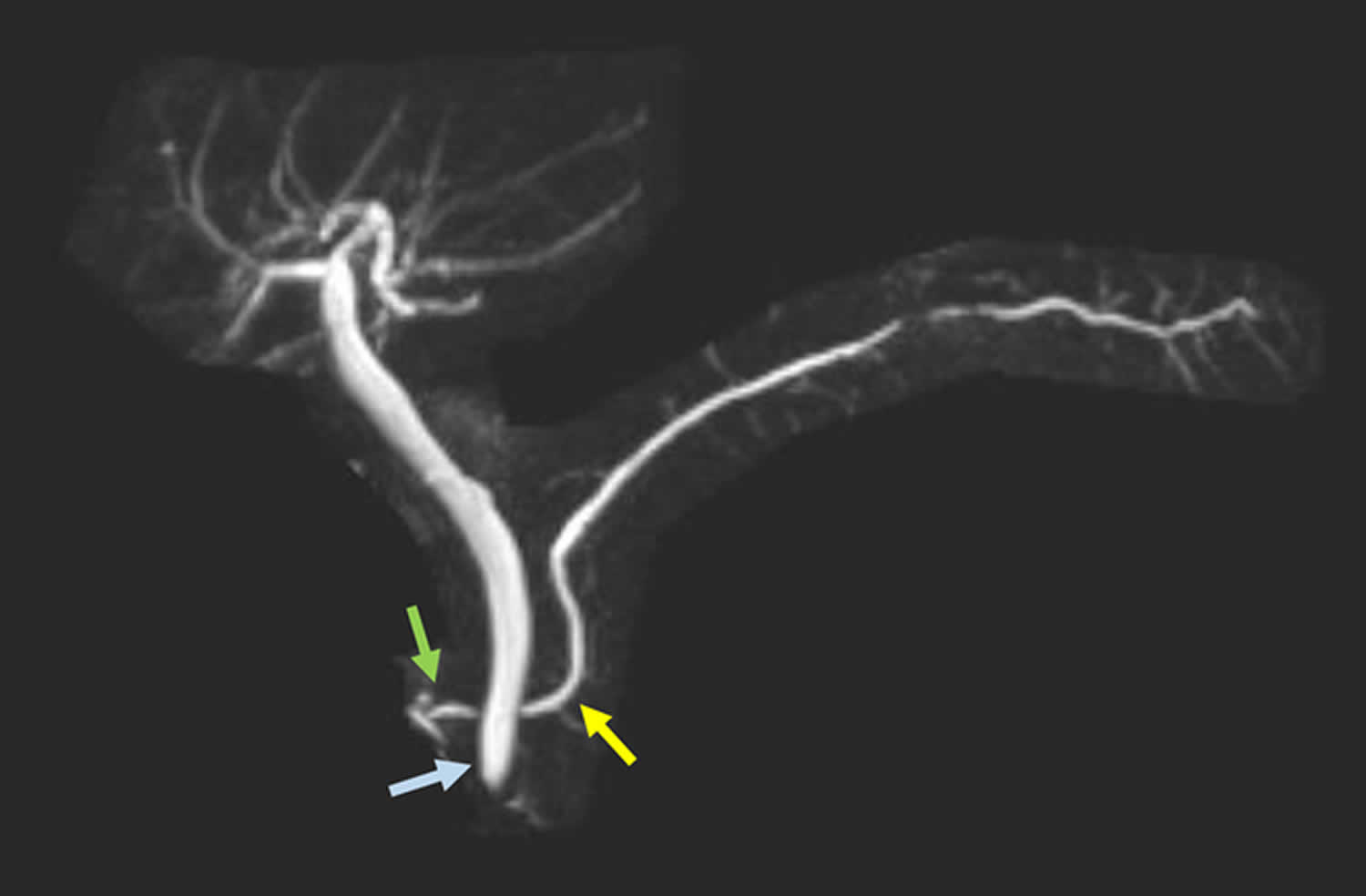
[Source 5 ]Figure 2. Pancreas divisum magnetic resonance cholangiopancreaticography (MRCP)
Footnotes: Pancreatic divisum magnetic resonance cholangiopancreaticography (MRCP) image showing (DD) dorsal pancreatic duct (duct of Santorini) crossing anterior to (CBD) common bile duct and emptying separately into minor papilla and CBD joining with (VD) ventral pancreatic duct (Wirsung duct) and both entering into major papilla in patient with pancreas divisum. D = duodenum
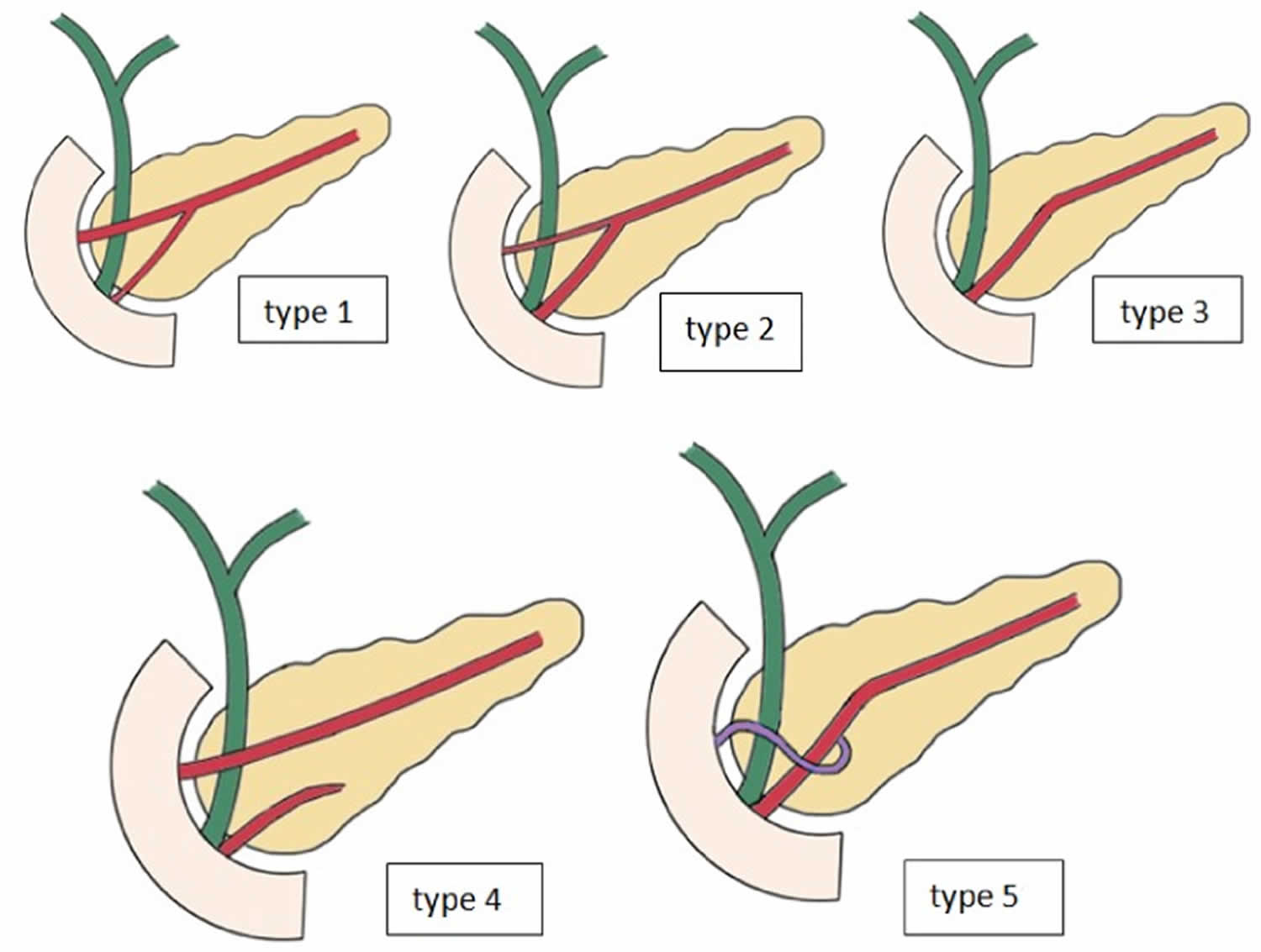
[Source 40 ]Figure 3. Different types of pancreatic duct configuration
Footnotes: Different types of pancreatic duct configuration. Type 1: Bifid configuration with dominant ventral pancreatic duct (Wirsung duct), Type 2: Bifid configuration with dominant dorsal pancreatic duct (duct of Santorini) without divisum, Type 3: Rudimentary non-draining dorsal pancreatic duct (duct of Santorini), Type 4: Pancreas divisum, Type 5: Ansa pancreatica where the dorsal pancreatic duct (duct of Santorini) formed an inferior loop and connected with a side branch of the ventral pancreatic duct (Wirsung duct) in the uncinate process 40, 8, 41.
[Source 13 ]Is pancreas divisum painful?
No, many people with pancreatic divisum are asymptomatic. Hence, patients with pancreatic divisum might not have any pain. However, if the patients experience any pain, that can be managed by a gastroenterologist or treated by a surgical method.
How serious is pancreatic divisum?
Pancreas divisum usually doesn’t cause any problems; however, it can occasionally result in acute pancreatitis. If the acute pancreatitis isn’t addressed, it might lead to chronic pancreatitis or kidney failure, eventually leading to death.
Is pancreas divisum hereditary?
Yes, pancreas divisum is hereditary. It is present at birth with an estimated 10% of total newborns. The symptoms of pancreas divisum are rare, and they might get treated with surgical intervention.
Can pancreatic divisum cured by surgery?
Yes, pancreatic divisum can be cured by surgery. However, the surgery selection is purely based on the type of pancreas divisum.
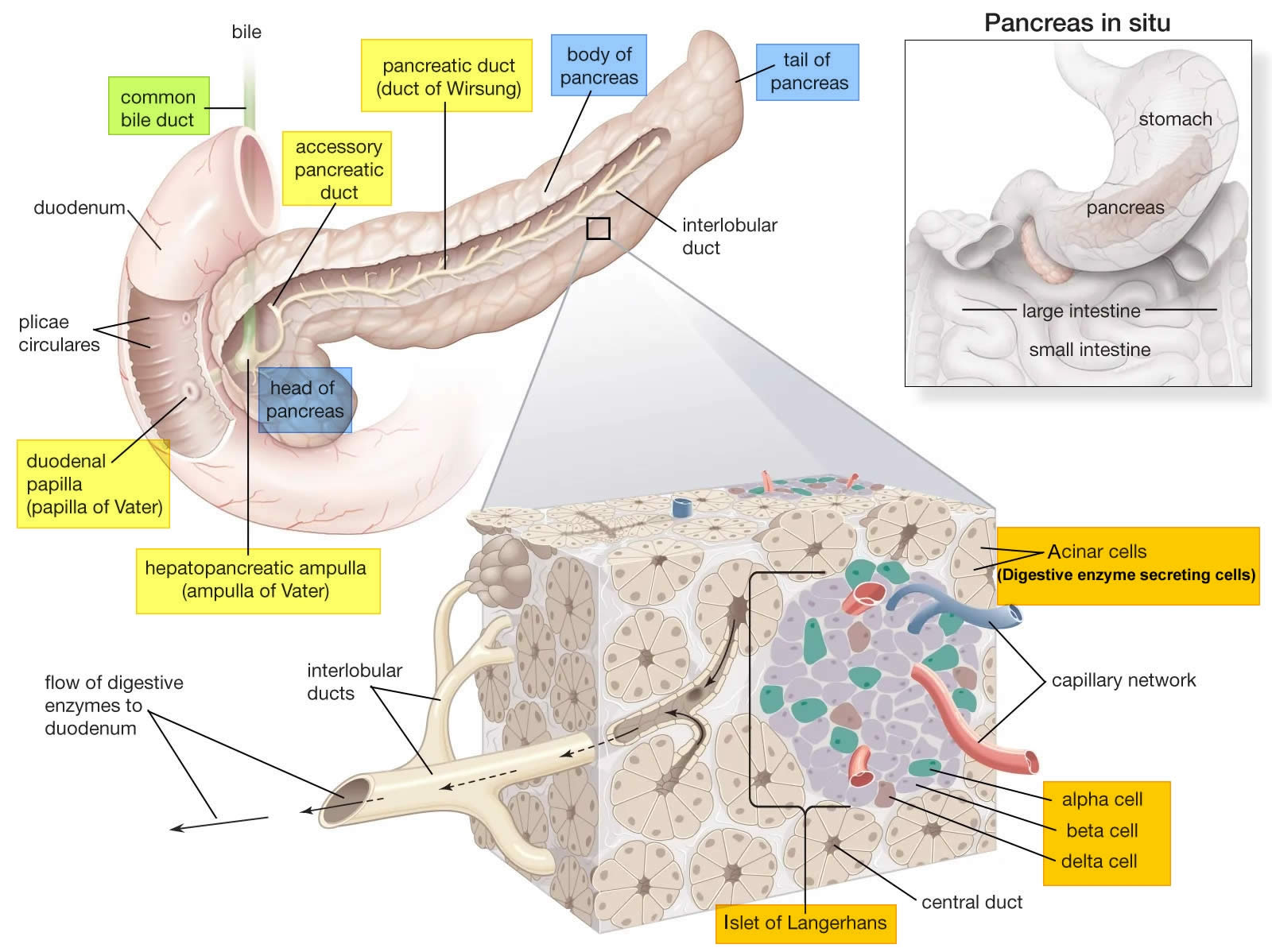
Pancreas anatomy
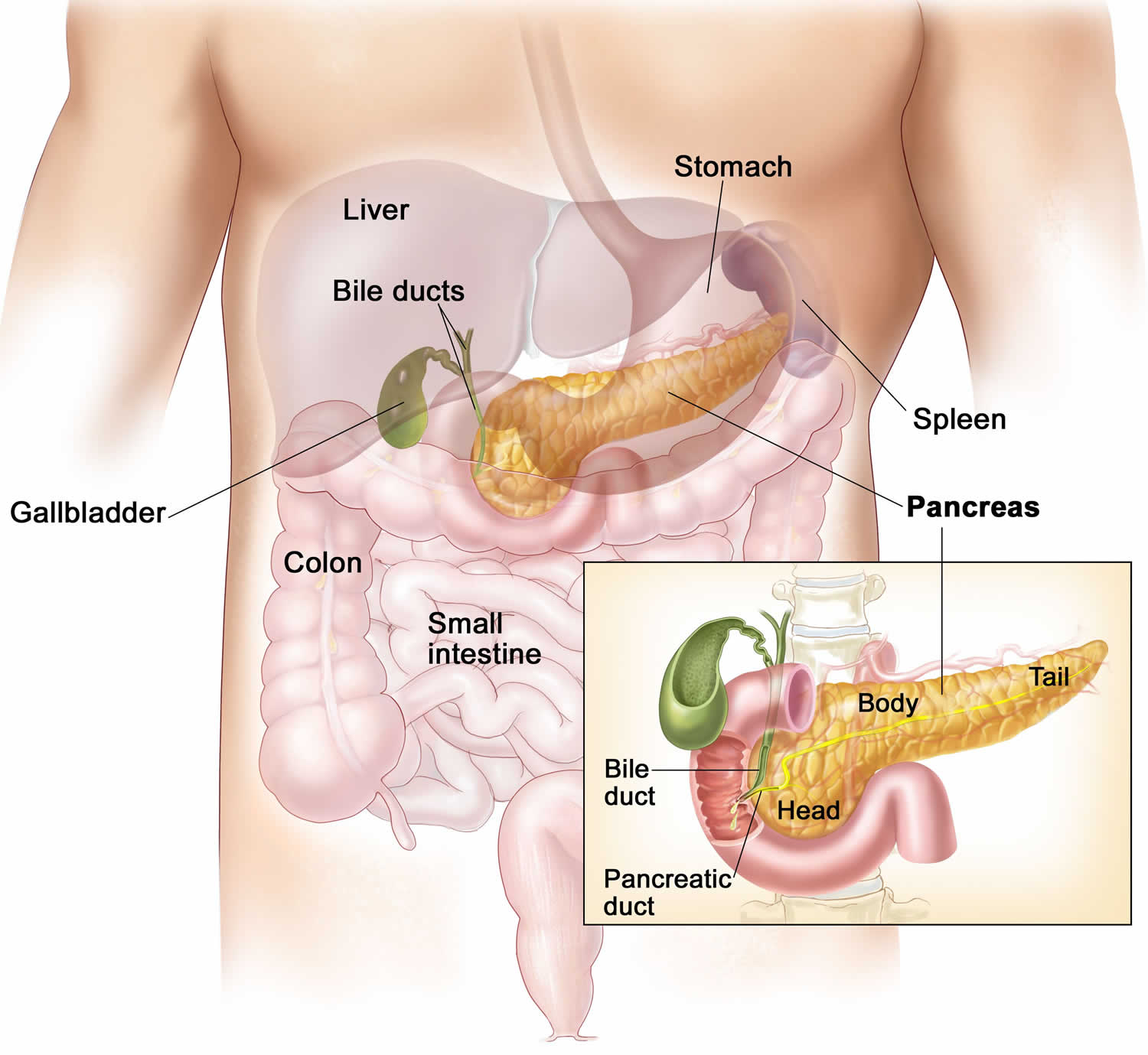
The pancreas is a large gland that sits behind the greater curvature of the stomach and close to the first part of the small intestine (the duodenum). The pancreas is shaped a bit like a fish with a wide head, a tapering body, and a narrow, pointed tail. In adults it’s about 12–15 cm (5–6 inches) long and 2.5 cm (1 in.) thick but less than 2 inches (5 centimeters) wide. The pancreas is both an endocrine and exocrine gland (see Figures 2 and 3).
The pancreas has 3 parts, the head, body, and tail.
- the wide end is called the head. The head of the pancreas is on the right side of the abdomen (belly), behind where the stomach meets the duodenum (the first part of the small intestine).
- the bit in the middle is called the body. The body of the pancreas is behind the stomach.
- the thin end is called the tail. The tail of the pancreas is on the left side of the abdomen next to the spleen.
About 99% of the pancreas is exocrine tissue made up of small clusters of glandular epithelial cells called acinar cells (acini), which secretes 1,200 to 1,500 mL of pancreatic juice per day – that are released into the small intestines to help you digest foods (especially fats). The digestive enzymes are first released into tiny tubes called central ducts. These merge to form larger ducts, which empty into the pancreatic duct (duct of Wirsung). The pancreatic duct merges with the common bile duct (the duct that carries bile from the liver), and empties into the duodenum (the first part of the small intestine) at the ampulla of Vater (also known as the hepatopancreatic ampulla). The ampulla of Vater (hepatopancreatic ampulla) is where the pancreatic duct and bile duct join together to drain into the duodenum, which is the first part of the small intestine. The passage of pancreatic juice and bile through the hepatopancreatic ampulla (ampulla of Vater) into the duodenum of the small intestine is regulated by a mass of smooth muscle surrounding the ampulla known as the sphincter of the hepatopancreatic ampulla, or sphincter of Oddi. The other major duct of the pancreas, the accessory duct (duct of Santorini), that branches from the main pancreatic duct and opens independently into the duodenum about 2.5 cm (1 in.) superior to the hepatopancreatic ampulla (ampulla of Vater) at the minor duodenal papilla. The accessory duct (duct of Santorini) bypasses the sphincter and allows pancreatic juice to be released into the duodenum even when bile is held back.
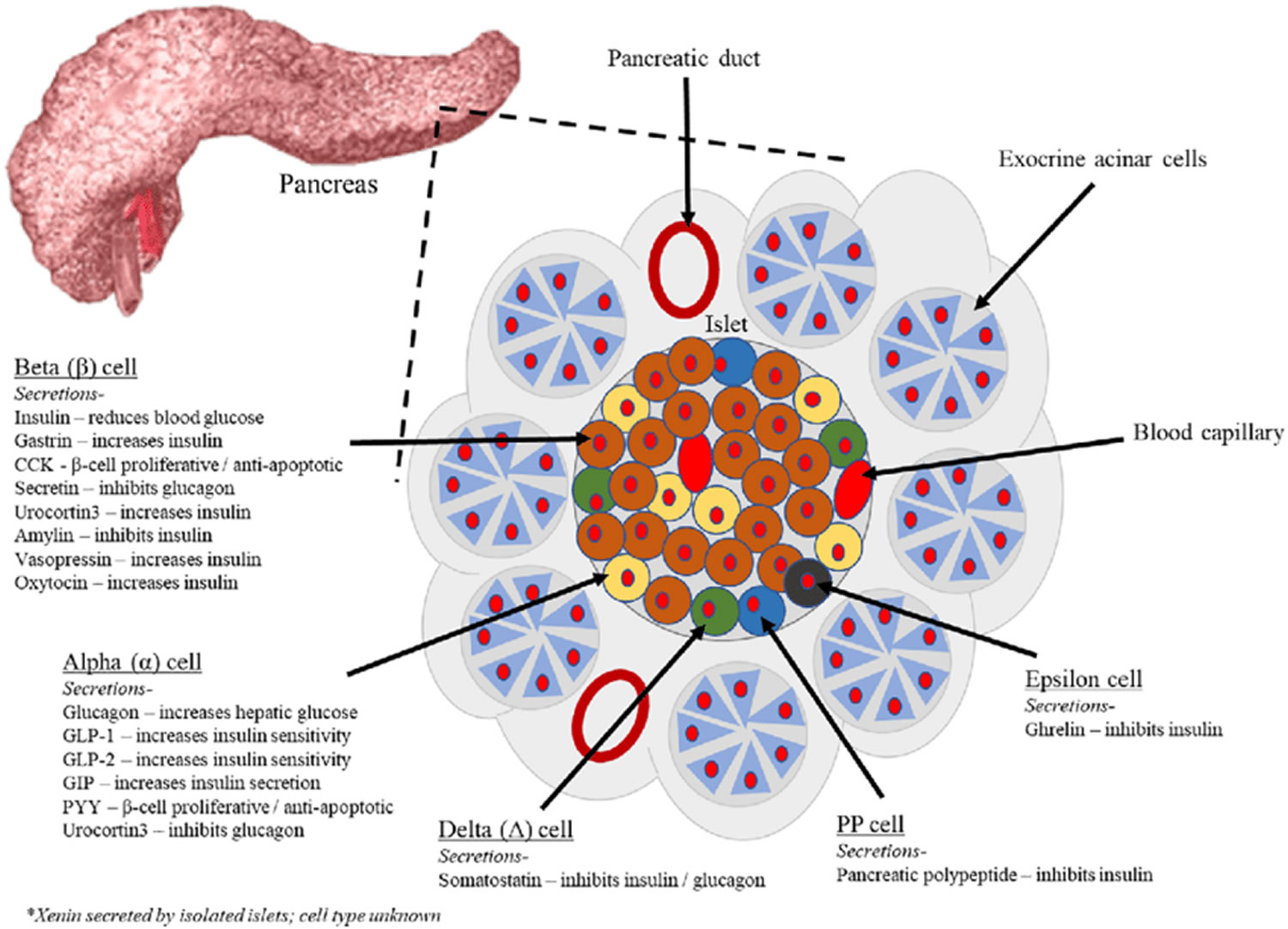
The endocrine part of the pancreas consists of groups of cells that are closely associated with blood vessels. These remaining 1% of the cell clusters form “islands” of cells called pancreatic islets (Islets of Langerhans). The Islets of Langerhans cells secrete the hormones glucagon, insulin, somatostatin, and pancreatic polypeptide (PP). Islets of Langerhans main cell types are alpha cells (20%), beta cells (70%), and delta cells (5%). The pancreatic islets alpha cells secrete the hormone glucagon, and beta cells secrete the hormone insulin (Figure 4). Both insulin and glucagon are important hormones which help control blood sugar levels and are released directly into the bloodstream.
The Islets of Langerhans Delta (δ) cells, or D cells, secrete somatostatin (growth hormone–inhibiting hormone) concurrently with the release of insulin by the beta cells. Somatostatin is a peptide hormone that inhibits the secretion of glucagon and insulin by the nearby alpha and beta cells. Somatostatin also work with amylin to limit the secretion of stomach acid.
Other, minor types of pancreatic cells, about 5% of the total, are called pancreatic polypeptide (PP) and G cells. Pancreatic polypeptide (PP) cells secrete pancreatic polypeptide, a hormone that may inhibit the exocrine activity of the pancreas.
Pancreatic islets (Islets of Langerhans) are relatively concentrated in the tail of the pancreas, whereas the head is more exocrine. Over 90% of pancreatic cancers arise from the ducts of the exocrine portion (ductal carcinomas), so cancer is most common in the head of the pancreas.
Figure 4. The pancreas
Figure 5. Pancreas cell types
Footnotes: Exocrine pancreatic acinar cells constitute most of the pancreatic tissue, these cells produce digestive enzymes which are transported via the pancreatic ducts. The endocrine pancreas is illustrated with all cell types; alpha, beta, delta, pancreatic polypeptide (PP) and epsilon. The endocrine pancreas cells are arranged in compact Islets of Langerhans and secrete a number of classical and ‘nonclassical’ peptides, as depicted.
Figure 6. Pancreas location
Figure 7. Relationship of the pancreas to the liver, gallbladder, and duodenum

Pancreas divisum causes
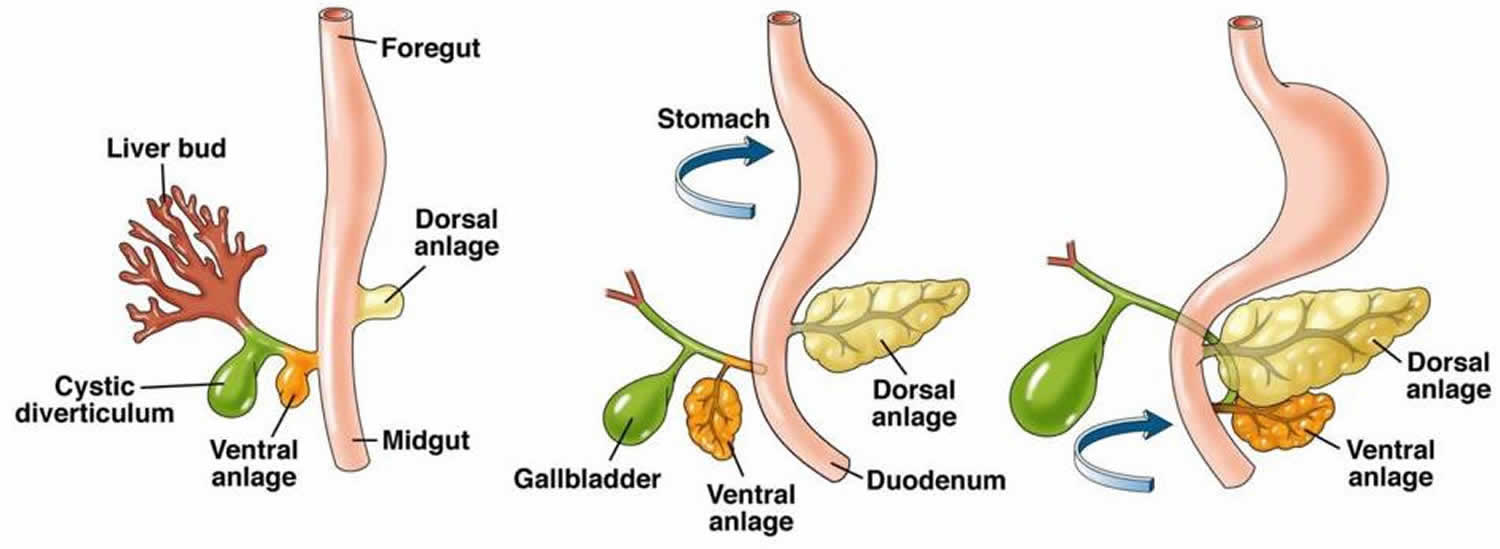
Pancreas divisum develops prenatally at approximately the 8th week of intrauterine life during embryologic development when the dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct) fail to join during development to form a main pancreatic duct, therefore, the majority of the pancreas drains into the minor papilla via the dorsal duct (duct of Santorini) 42. However, what cause the failure of the pancreatic ducts of the dorsal and ventral buds to fuse is unknown (idiopathic).
The pancreas develops from dorsal pancreatic bud (dorsal anlage) and ventral pancreatic bud (ventral anlage) that first appear in the 5th gestational week as outgrowths of the primitive foregut (Figure 8) 40, 2. By the 7th gestational week, expansion of the duodenum causes the ventral pancreatic bud (from which originates the hepatobiliary system) to rotate and pass behind the duodenum from right to left and fuse with the dorsal pancreatic bud in the foregut (Figure 8). The dorsal pancreatic bud forms a majority of the head of the pancreas as well as the uncinate process (<25% of pancreatic tissue), whereas the dorsal pancreatic bud forms the anterior head, all of the body, and tail of the pancreas 14. Following this fusion, the ductal systems anastomose, a complicated process with a wide spectrum of possible outcomes. The portion of the ventral duct between the dorsal-ventral fusion and major papilla is termed the duct of Wirsung. The portion of the dorsal duct upstream to the dorsalventral fusion point is called the main pancreatic duct that opens at the major papilla along with the common bile duct 40. The segment of the dorsal pancreatic duct downstream to the dorsal-ventral fusion point is termed the duct of Santorini, or accessory pancreatic duct, which drains at the papilla minor 14, 43, 36. The cause for pancreas divisum is the failure of fusion of the two ductal systems to a varying degree leading to three known variants/subtypes.
In over 90% of healthy people, the proximal one third of the dorsal pancreatic duct regresses as it fuses with the ventral duct, forming the main pancreatic duct 44. However, in about 10% of the population, fusion does not occur, resulting in pancreas divisum (Figure 1), which is the most common congenital ductal anomaly of the pancreas 6. The classic anatomy of pancreas divisum consists of a small ventral pancreatic duct (Wirsung duct), which drains through the larger major papilla, and the larger dorsal pancreatic duct (duct of Santorini), which drains through the smaller minor papilla 11, 18. If a pancreatic duct becomes blocked, swelling and tissue damage (pancreatitis) may develop.
Cases of incomplete pancreas divisum are the same as classic divisum, except a small branch connects the ventral and dorsal pancreas. In cases of pancreas divisum with nonpatent major papilla, the entire pancreatic ductal system drains via the minor papilla. In cases of reversed pancreas divisum, the small dorsal duct drains via minor papilla and the large ventral duct drains via major ampulla. This variant has no physiologic significance except in rare cases of pancreatic cancer that do not involve the main pancreatic duct.
Rarely, doubled pancreatic ducts may be formed, as in a 2018 case report 44.
Symptoms of pancreatic divisum probably are due to the high intrapancreatic dorsal ductal pressure caused by resistance to pancreatic secretion by a small minor papilla orifice. Possible alternate mechanism is intermittent obstruction of drainage by minor papilla proteinaceous plugs 45. Cystic fibrosis gene (CFTR gene) mutation has been found in some cases of pancreas divisum and may be responsible for variations in the occurrences of symptoms 46, 47, 7, 48, 49.
Figure 8. Pancreas embryologic development
Footnotes: Drawings show normal embryologic development of the pancreas. Rotation of the ventral pancreatic bud (anlage) from which originates the hepatobiliary system and fusion with the dorsal pancreatic bud (anlage) in the foregut. The failure of fusion of the ductal systems of the dorsal and ventral anlage results in pancreas divisum with the majority of the pancreas draining via the dorsal duct of Santorini through the minor papilla.
[Source 2 ]Pancreatic divisum types
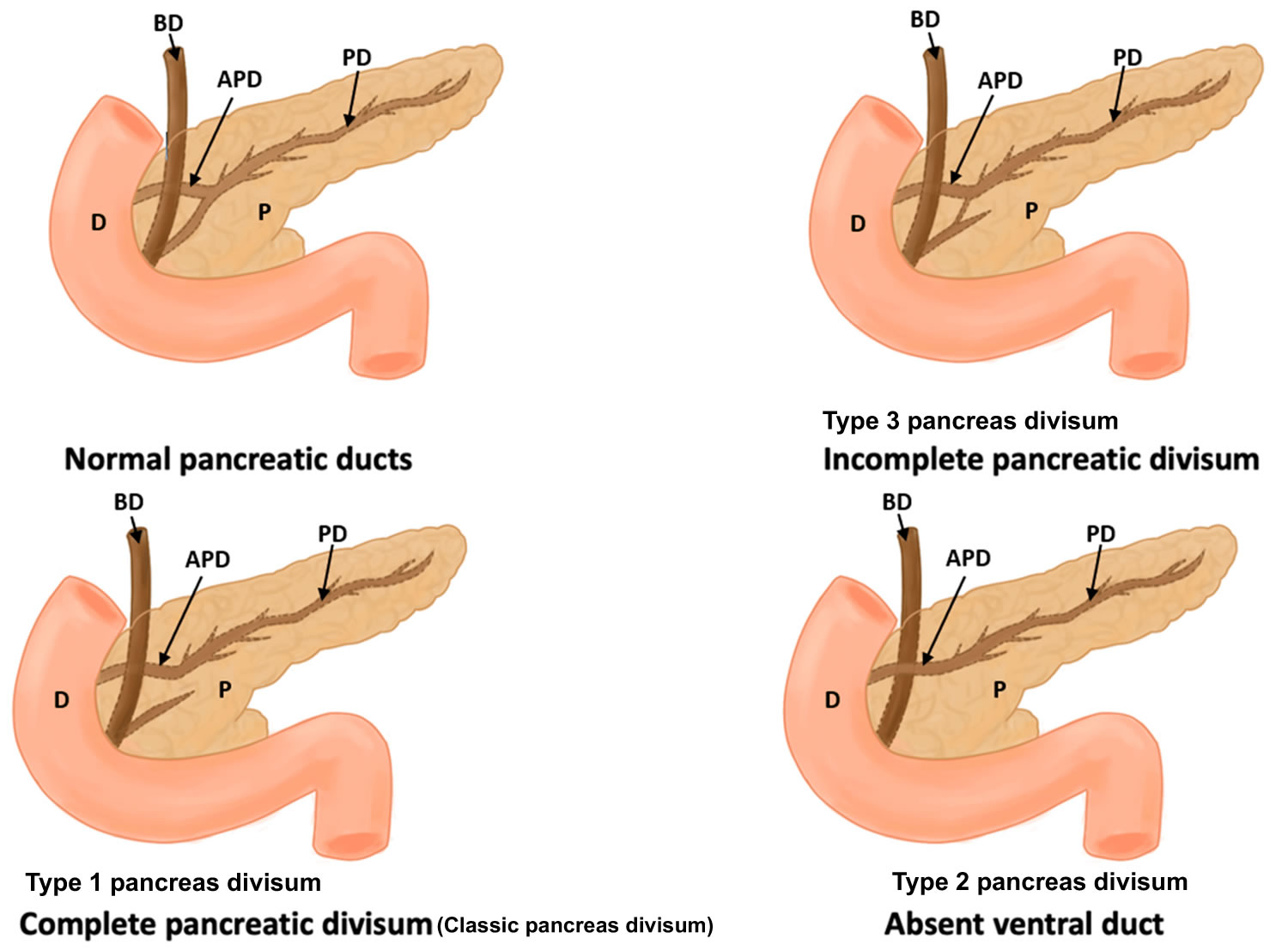
Based on the fusion and functionality of dorsal pancreatic duct (duct of Santorini) and ventral pancreatic duct (Wirsung duct), the pancreas divisum is broadly classified into four types 50, 40, 51, 38:
- Type 1 pancreas divisum
- Type 2 pancreas divisum
- Type 3 pancreas divisum
- Type 4 pancreas divisum
Figure 9. Pancreatic divisum types
Footnotes: (A) Normal pancreas; (B) Type 1 pancreas divisum also called classic pancreatic divisum or complete pancreas divisum; (C) Type 2 pancreas divisum there is an absence of the ventral pancreatic duct (Wirsung duct); (D) Type 3 pancreas divisum also called incomplete pancreas divisum (magnified image demonstrates the small communication between the dorsal and ventral pancreatic ductal systems); (E) Type 4 pancreas divisum also called reverse pancreas divisum
[Source 2 ]Type 1 pancreas divisum
Type 1 pancreas divisum also called classic pancreatic divisum or complete pancreas divisum, there is a complete failure of fusion between dorsal and ventral pancreatic duct (Figure 8 & 9). The ventral pancreatic duct (Wirsung duct) system is short and opens into the major papilla, while the longer dorsal pancreatic duct (duct of Santorini) system opens into the minor papilla with no communication between the two ducts. Classic pancreatic divisum or complete pancreas divisum is the major variant with an approximate prevalence of 70% 52, 53.
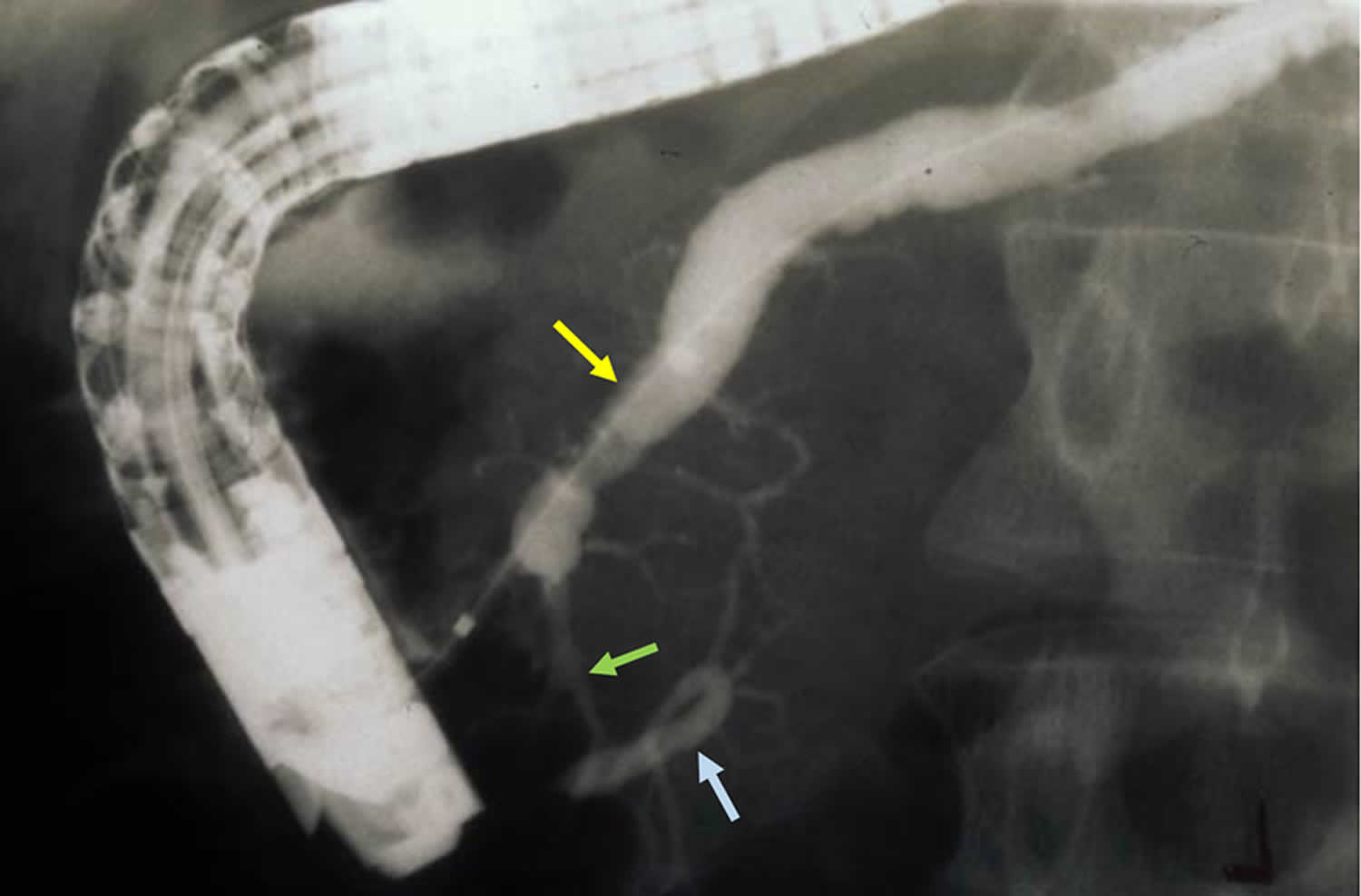
Figure 10. Classic pancreatic divisum
Footnote: The dorsal pancreatic duct (yellow arrow) crosses the bile duct (blue arrow) and empties at a separate orifice/minor papilla (green arrow).
Abbreviations: D = duodenum, P = pancreas, PD = pancreatic duct, APD = accessory pancreatic duct, and BD = bile duct
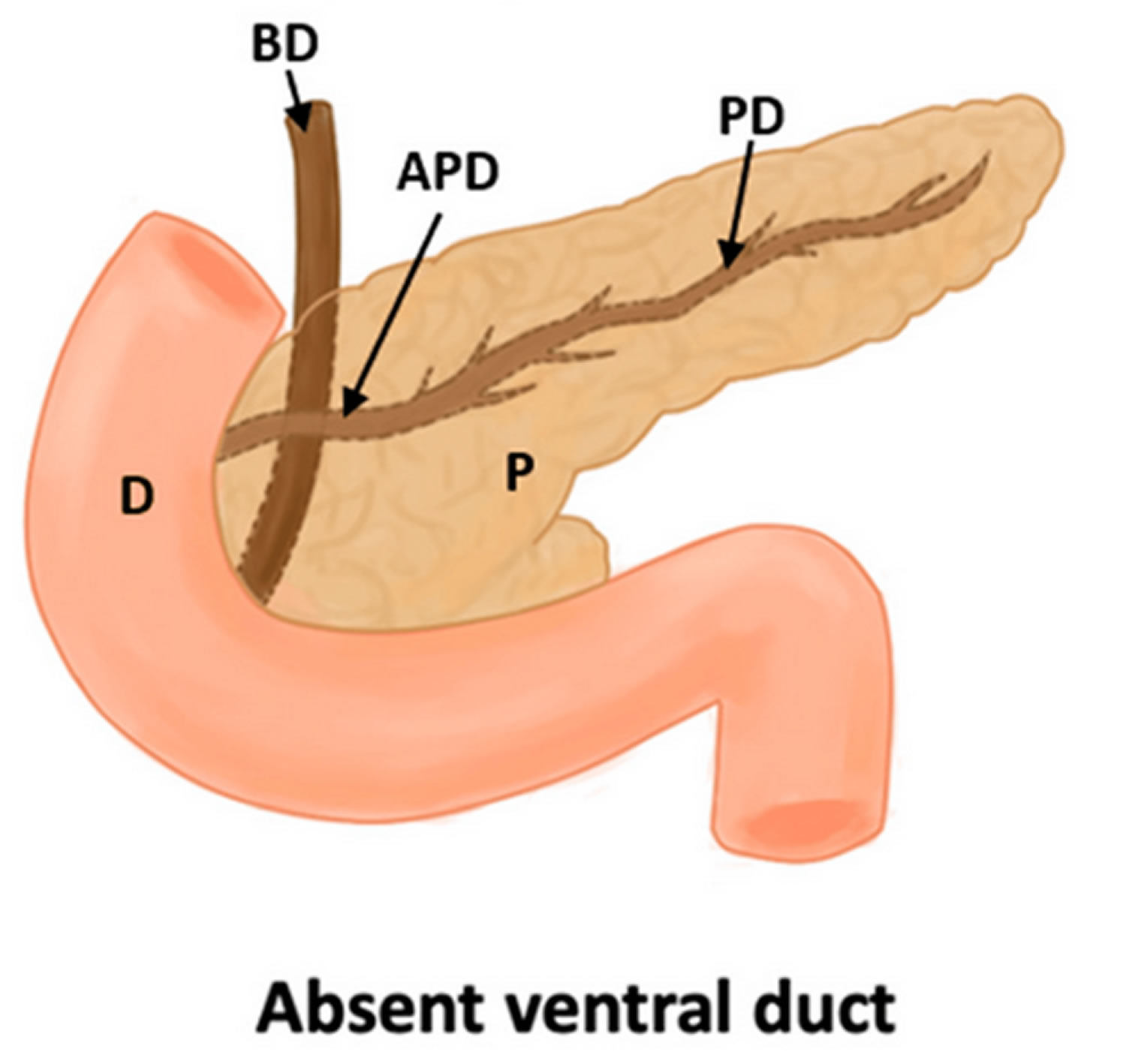
[Source 2, 50 ]Type 2 pancreas divisum
Type 2 pancreas divisum there is an absence of the ventral pancreatic duct (Wirsung duct); therefore, the minor papilla drains the entire pancreas while the major papilla drains a portion of the common bile duct.
Figure 11. Type 2 pancreas divisum
Abbreviations: D = duodenum, P = pancreas, PD = pancreatic duct, APD = accessory pancreatic duct, and BD = bile duct
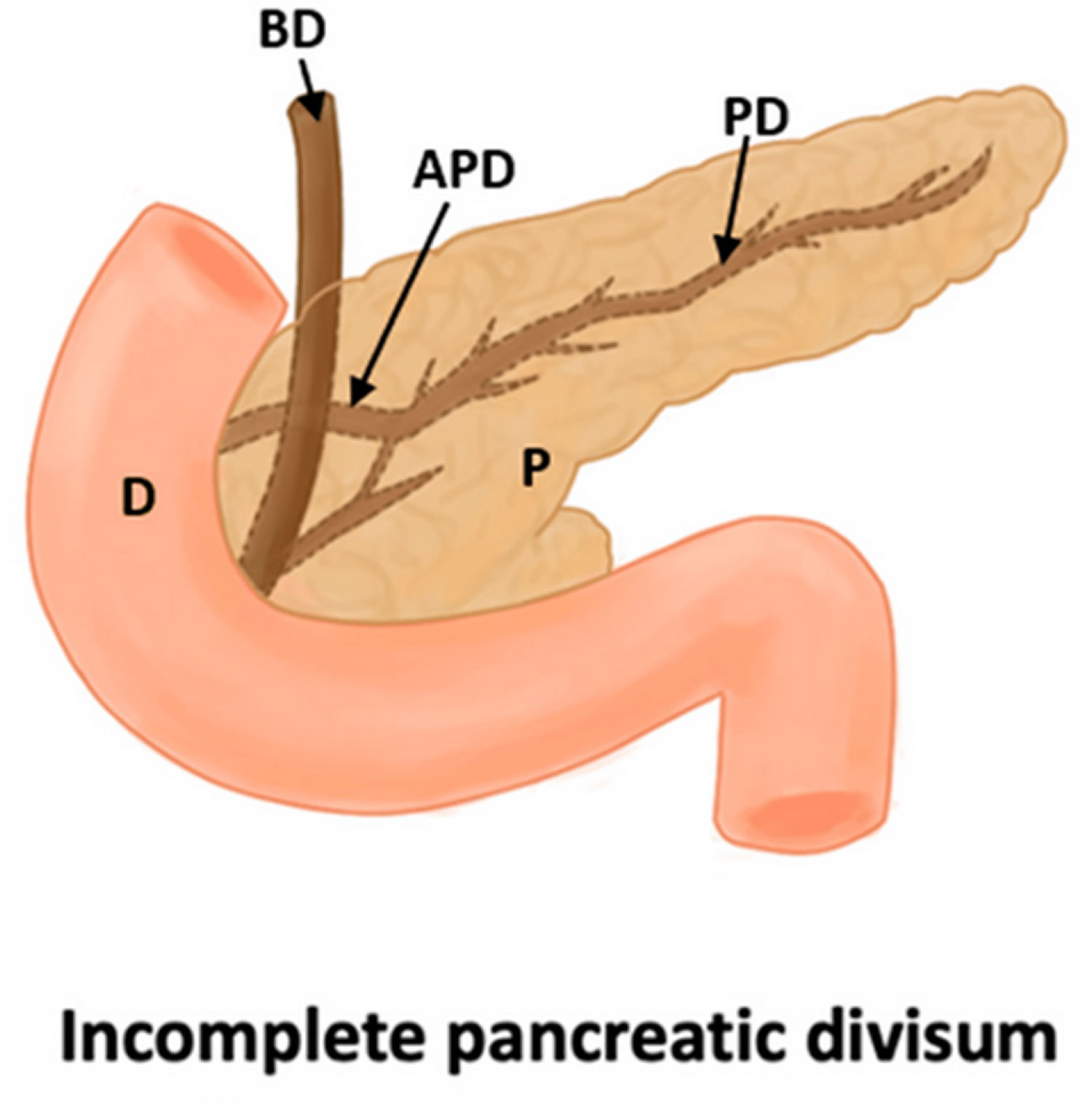
[Source 50 ]Type 3 pancreas divisum
Type 3 pancreas divisum also called incomplete pancreas divisum is characterized by small branch of communication between the dorsal duct and ventral duct. This can lead to opacification of the dorsal system during injection of contrast in the ventral duct during endoscopic retrograde cholangiopancreatography (ERCP). The prevalence of incomplete pancreas divisum is about 15% 54, 55, 56.
Figure 12. Incomplete pancreas divisum
Footnote: Incomplete pancreas divisum ERCP. Dorsal pancreatic duct (yellow arrow) is cannulated and opacified from the minor papilla with contrast passing into the ventral pancreatic duct (blue arrow) through a small communication between the two systems (green arrow).
Abbreviations: D = duodenum, P = pancreas, PD = pancreatic duct, APD = accessory pancreatic duct, and BD = bile duct
[Source 2, 50 ]Type 4 pancreas divisum
Type 4 pancreas divisum is also known as reverse pancreas divisum, is a unusual variation where the main pancreatic duct fuses with the ventral pancreatic duct (Wirsung duct) and a small residual dorsal pancreatic duct (duct of Santorini) does not communicate with the main pancreatic duct leading to a small isolated component of the dorsal pancreas and drains separately into the minor papilla 57, 58. The interruption in drainage system of the accessory pancreatic duct in reverse pancreas divisum can frequently be interpreted as an obstruction by a cancer or a benign stricture 2.
The clinical behavior of complete and incomplete pancreatic divisum is similar except for the variation at the time of ERCP 59, 60. However, a reverse pancreatic divisum behaves more like a normal pancreas wherein the severity of gallstone pancreatitis (from impaction of a gallstone at the major papilla) can be much worse as a significant portion of the pancreas drains through the major papilla unlike the preceding two variants where only a minority drains through the major papilla 2.
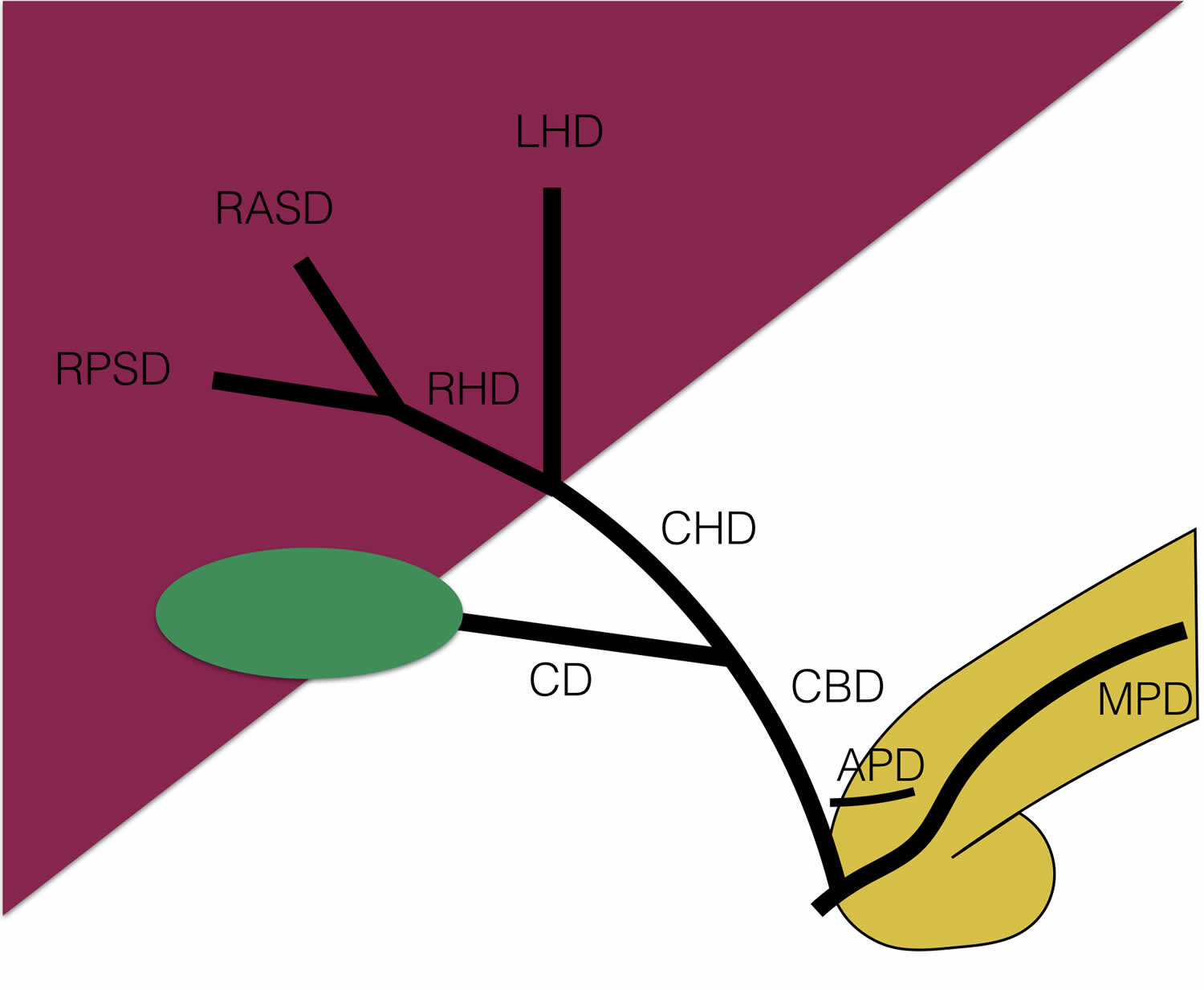
Figure 13. Type 4 pancreas divisum
Abbreviations: APD = accessory pancreatic duct; MPD = main pancreatic duct; CBD = common bile duct; CD = cystic duct; CHD = common hepatic duct; RHD = right hepatic duct; LHD = left hepatic duct; RPSD = right posterior sectorial duct; RASD = right anterior sectorial duct
[Source 61 ]Pseudo or False pancreas divisum
An obstruction of the main pancreatic duct of Wirsung downstream to the origin of the accessory duct of Santorini in a normal pancreas from injury due to acute pancreatitis, a stricture due to chronic pancreatitis or a malignancy can give the appearance of true pancreas divisum. This obstruction of the ventral duct in the head can lead to a decrease in its size and compensatory increase in size of the accessory duct draining the body and tail mimicking the anatomic findings of pancreas divisum on imaging and ERCP. It is important to recognize this condition due to the possibility of cancer.
Pancreas divisum symptoms
The vast majority of patients born with pancreatic divisum will show no signs or symptoms of the condition (asymptomatic) and is a coincidental finding. However, a few patients might show the following symptoms.
- Vomiting and nausea
- Pain in the abdomen (stomach)
- Inflammation of the pancreas (acute or chronic pancreatitis)
- Food intolerance
Pancreas divisum can be of clinical relevance in the following situations:
- At endoscopic retrograde cholangiopancreatography (ERCP), the small ventral duct must be differentiated from various causes of main pancreatic duct cutoff, such as pancreatic cancer and pancreatic pseudocysts.
- Dorsal pancreatic duct diseases can be missed because only the ventral portion of the pancreas can be viewed via standard major papilla cannulation.
- Patients with symptomatic pancreas divisum present with pancreatitis or chronic abdominal pain. Pancreatitis can be acute recurrent pancreatitis or chronic pancreatitis. Patients with chronic abdominal pain can have a pain syndrome consistent with pancreatitis without an identifiable etiologic cause for pain (serum amylase, lipase, and imaging findings are normal).
The most common symptoms of acute pancreatitis include:
- Suddenly getting severe pain in the center of your belly (abdomen)
- Pain in the upper belly that radiates to your back
- Tenderness when touching your belly
- Fever 100.4°F (38°C) or more
- Rapid pulse
- Upset stomach
- Vomiting
- Mild jaundice (yellowing of the whites of the eyes, and yellowing of the skin) although this may be less obvious on brown or black skin.
Chronic pancreatitis signs and symptoms include:
- Pain in the upper belly (abdomen)
- Belly pain that feels worse after eating
- Losing weight without trying
- Oily, smelly stools.
Some people with chronic pancreatitis only develop symptoms after they get complications of the disease.
Pancreas divisum complications
Pancreas divisum can cause chronic or acute pancreatitis, leading to malnutrition. With both acute and chronic pancreatitis, the pancreas may not produce enough enzymes for the digestive system. This can lead to malnutrition, diarrhea and weight loss.
The majority of patients with pancreas divisum are without pancreas symptoms and therefore there is considerable debate as to whether it is causally associated with pancreatitis or pancreatic-type abdominal pain 2. It has been theorized that a larger and longer dominant dorsal pancreatic duct (duct of Santorini) opening through a relatively smaller or stenotic minor papilla could lead to inadequate drainage of pancreatic secretions with obstruction of flow. The resultant increase in intraductal pressure and distention of the dorsal duct could then potentially lead to abdominal pain and even pancreatitis 2. As a consequence of this imbalance, the term “dominant duct syndrome” has been coined in the literature 1, 62. Manometry studies have shown an increased pressure in the dorsal pancreatic duct (duct of Santorini) and minor papilla when compared to the ventral pancreatic duct (Wirsung duct) and major papilla in pancreas divisum suggestive of dorsal duct and minor papilla hypertension 63. It has been suggested that this obstruction is transient and could be related to intermittent plugging of the minor papilla by proteinaceous material in the pancreatic secretions 64. However, the large majority of patients with a dilated dorsal duct in pancreas divisum are asymptomatic, suggestive of a poor correlation between obstruction and symptoms 17.
Some observational studies of patients with idiopathic recurrent acute pancreatitis and chronic pancreatitis have shown that the frequency of pancreatitis was similar in patients with pancreas divisum when compared to patients with normal duct variants 65, 66, 67. However, other studies have shown an increased prevalence of pancreas divisum (complete and incomplete) in adults 68, 69, 70, 71 and children 72 being evaluated for idiopathic recurrent acute pancreatitis and chronic pancreatitis, again supporting pancreas divisum as a potentially pathologic entity. Similar support for pancreas divisum as a potential pathologic entity is provided by studies that have shown pathological changes of pancreatitis limited to the dorsal pancreas (i.e normal ventral pancreas) in patients with pancreas divisum 70, 73. Studies have shown inconsistent and variable response to minor papilla and dorsal duct therapy in patients who present with pancreatic-type pain, with suboptimal results in the majority of patients 74, 75, 76, 77, 78, 79, 80, 81.
This heterogeneity suggests that pancreas divisum may not be a primary driving force of pancreatic pathology but rather a co-factor which in association with other factors leads to pancreatic disease 6. The basis for this line of thought comes from studies that show the prevalence of idiopathic recurrent acute pancreatitis and chronic pancreatitis is as high as 50% in adults and children with pancreas divisum when associated with certain genetic mutations of serine protease inhibitor Kazal type 1 gene (SPINK1), cystic fibrosis transmembrane conductance regulator gene (CFTR), chymotrypsin C gene (CTRC) 65, 72, 82, 83, 84. These gene mutations or polymorphisms have been reported to have an independent but not proven causal association with pancreatic disease 85, 86, 87. Additionally, it has also been postulated that the presence of pancreas divisum reduces the threshold for pancreatic disease from other known primary factors of pancreatitis such as alcohol, medications and trauma 63.
Acute pancreatitis
Acute pancreatitis is inflammation of the pancreas. Acute pancreatitis happens when digestive enzymes start digesting the pancreas itself. Acute pancreatitis occurs suddenly and is a short-term condition, meaning it appears suddenly and lasts for days. Most people with acute pancreatitis get better, and it goes away in several days with treatment. But some people can have a more severe form of acute pancreatitis and go on to develop serious complications, which requires a lengthy hospital stay. Acute pancreatitis is different to chronic pancreatitis, where the pancreas has become permanently damaged from inflammation over many years. Acute pancreatitis is becoming more common, for reasons that are not clear 88. Acute pancreatitis is the cause of up to 275,000 hospitalizations in the United States per year 89, 90. While mild acute pancreatitis carries a mortality of <1%, mortality rates for severe pancreatitis can reach as high as 30% 91. Drugs are responsible for 0.1%-2% of acute pancreatitis incidents. The majority of drug-induced pancreatitis cases are mild to moderate in severity; however, severe and even fatal cases can occur. Although pancreatitis is rare in children, the number of children with acute pancreatitis has grown.
Repeat episodes of acute pancreatitis may lead to chronic pancreatitis. Other complications of acute pancreatitis include:
- dehydration
- Bleeding
- Infection. Acute pancreatitis can make the pancreas vulnerable to infections. Pancreatic infections are serious and require intensive treatment, such as surgery or other procedures to remove the infected tissue.
- Kidney failure. Acute pancreatitis may result in the kidneys not filtering waste from the blood. Artificial filtering, called dialysis, may be needed for short-term or long-term treatment.
- Breathing problems. Acute pancreatitis can cause changes in how the lungs work, causing the level of oxygen in the blood to fall to dangerously low levels.
Chronic pancreatitis
Chronic pancreatitis is a long-lasting inflammation of the pancreas that slowly destroys the functions of the pancreas. The pancreas does not heal or improve. Instead, it gets worse over time, which can lead to lasting damage to your pancreas. For example, the pancreas may lose its ability to produce insulin and glucagon and digestive enzymes (pancreatic digestive juices). As a result, you can develop glucose intolerance or diabetes. Chronic pancreatitis can also cause weight loss because your body may be unable to digest fat and key elements of food. Chronic pancreatitis is less common than acute pancreatitis, with about 86,000 hospital stays per year 92. In the US, chronic pancreatitis affects African Americans more frequently than caucasians 93. In addition, chronic pancreatitis due to alcohol is more common in males, whereas that due to hyperlipidemia is more common in females 93. The median age at diagnosis is 45.
Complications of chronic pancreatitis include:
- chronic pain in your abdomen
- maldigestion, when you can’t digest food properly
- malnutrition and malabsorption
- problems with how well your pancreas works
- scars in your pancreas
- diabetes
- pancreatic cancer, which is more likely in people with both diabetes and pancreatitis
- osteopenia, osteoporosis and bone fractures
Diagnosing chronic pancreatitis relies on changes in diagnostic imaging and blood work in addition to clinical symptoms.
Pancreas divisum diagnosis
Pancreas divisum usually is a coincidental finding, and most individuals with pancreatic divisum are asymptomatic. The findings from an abdominal examination usually are normal. Epigastric tenderness and a palpable pseudocyst might be present during episodes of pancreatitis.
Magnetic resonance cholangiopancreatography (MRCP) is the most prevalent method of diagnosing pancreatic divisum by the gastroenterologist. Magnetic resonance cholangiopancreatography (MRCP) produces comprehensive pictures of the pancreas and pancreatic ducts using a strong magnetic field and radio waves. The patient will be administered with a contrast material intravenously. The patient needs to be in supine position in the magnetic resonance imaging (MRI) scanner while the pancreas is scanned. Magnetic resonance cholangiopancreatography (MRCP) is a very accurate, noninvasive technique for visualizing the pancreatic and biliary duct system without the side effects of a contrast agent and without the risk of causing acute pancreatitis 94, 95, 9, 96. Maximum-intensity projection images from MRCP appear to best illustrate the “crossing duct” sign, in which the dominant dorsal duct crosses the intrapancreatic common bile duct to empty into the minor papilla 12.
In a systematic review and meta-analysis comparing endoscopic ultrasonography (EUS) with MRCP in idiopathic acute pancreatitis, endoscopic ultrasonography (EUS) was more diagnostically accurate than MRCP (64% vs 34%), but MRCP after secretin stimulation (S-MRCP) was superior (12%) to MRCP alone (2%) as well as to EUS (2%) in diagnosing pancreatic divisum 97. The investigators indicated that EUS should be the preferred study for identifying a potential biliary condition and diagnosis of chronic pancreatitis and that MRCP after secretin stimulation (S-MRCP) can be helpful in identifying a potential anatomic alteration in the biliopancreatic duct system 97.
Endoscopic ultrasound (EUS) combines two techniques — endoscopy and ultrasound — to help doctors see, evaluate and diagnose conditions in and near the gastrointestinal tract. Endoscopic ultrasound is a minimally invasive procedure that uses a camera device (endoscope) together with high frequency sound waves (ultrasound) to examine the gastrointestinal tract and beyond. Endoscopic ultrasound (EUS) uses a special endoscope with a small ultrasound device on its tip, called an echoendoscope. Addition of ultrasound lets the doctor see the gastrointestinal tract and surrounding organs.
Other diagnostic methods include:
- Endoscopic retrograde cholangiopancreatography (ERCP). Endoscopic Retrograde Cholangiopancreatography (ERCP) is a non-invasive procedure where a flexible tube containing a tiny camera will be inserted into your mouth through the stomach and small intestine (duodenum). The gastroenterologist will inject a radiopaque dye and takes X-ray images of the pancreas. Upon endoscopic retrograde cholangiopancreatography (ERCP), the major papilla is often difficult to cannulate, and the duct of Wirsung (ventral duct) appears shortened and of small diameter (like a cutoff of the duct) with rapid filling of small accessory ducts. At this point, the accessory papilla should be cannulated. A variety of maneuvers have been used to facilitate cannulation. These include simple maneuvers, such as using the long scope position and accessories to include a taper cannula, slick wires, secretagogues, such as sincalide or secretin, and the application of vital dyes. This should reveal the duct of Santorini (dorsal duct) running the entire length of the pancreas.
- Computed tomography (CT) scan. Computed tomography (CT) scan is a test that uses a combination of X-rays and computers to produce images of the pancreas. CT of the abdomen is very useful in finding and imaging pathologies of the pancreas, such as acute or chronic pancreatitis and pancreatic tumors, but it is not very good at imaging the pancreatic duct system.
- Magnetic resonance imaging (MRI). Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to produce images of the pancreas. During this exam, the patient lies in enormous tubular magnet machines. These machines realign the water molecules in the patient’s body before using radio waves to make cross-sectional photographs.
- Blood tests. Blood tests can give clues about how the immune system, pancreas and related organs are working.
- Stool tests. Stool tests can measure levels of fat that could suggest your digestive system isn’t absorbing nutrients as it should.
Your doctor may recommend other tests, depending on your symptoms or other conditions you may have.
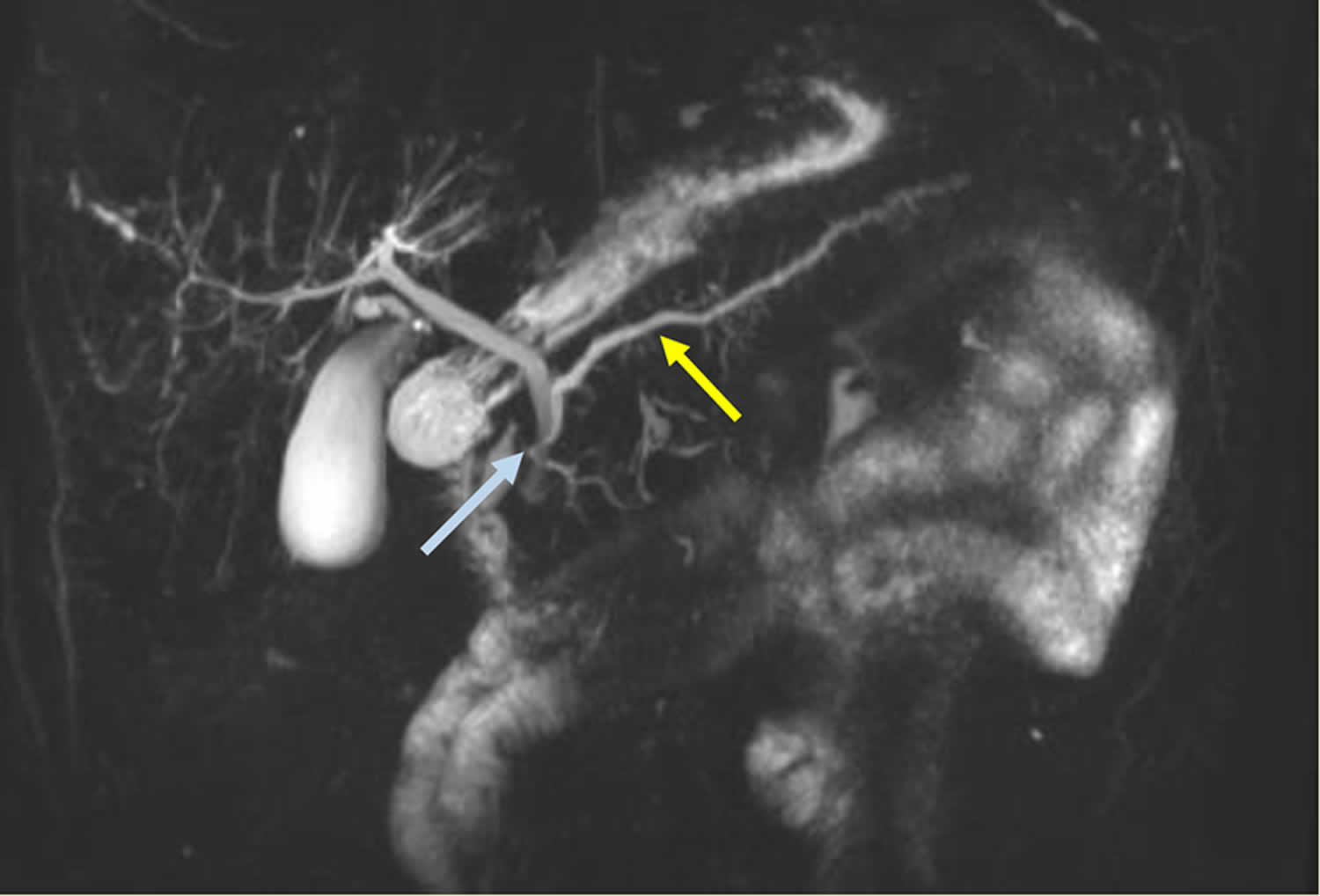
Figure 14. Pancreas divisum MRCP
Footnotes: Secretin-stimulated MRCP (S-MRCP) shows a dilated and irregular dorsal pancreatic duct (yellow arrow) crossing the bile duct and opening separately at the minor papilla (blue arrow). Irregular side branches are also seen and are more prominent than the non-secretin enhanced image (see Figure 2 above)
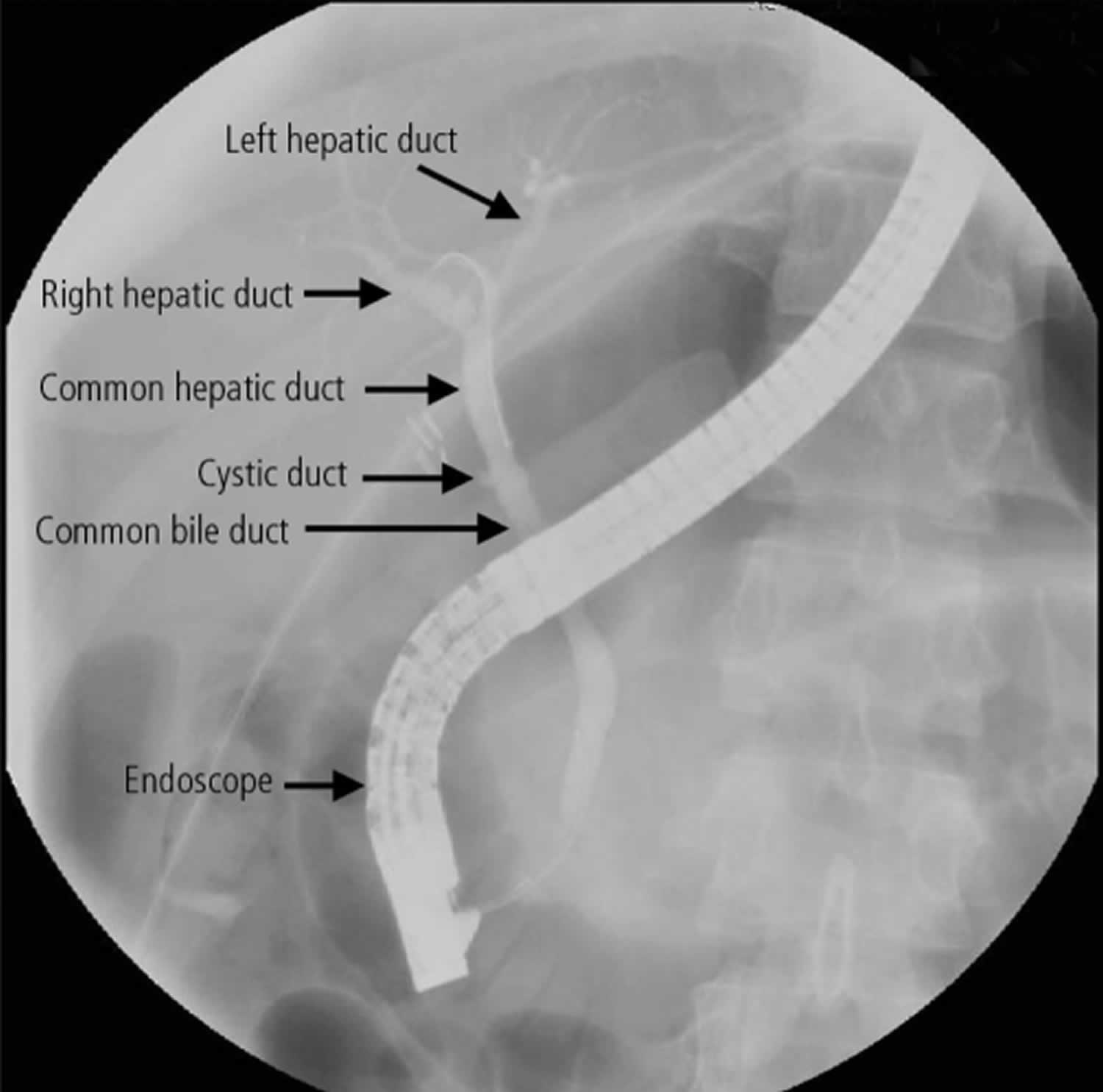
[Source 2 ]Figure 15. Pancreas divisum ERCP
Footnotes: 23-year-old woman presented to hospital with 2 months of intermittent discomfort in your upper abdomen following meals and nausea and vomiting. Based on the results of laboratory investigations (lipase > 1900 [normal < 286] U/L), acute pancreatitis was diagnosed. The results of other laboratory tests, including those for amylase, leukocytes and creatinine, were within normal limits. No obvious reversible causes of pancreatitis were initially identified. She was treated conservatively with analgesics and intravenous hydration. Ultrasonography performed 21 days after admission showed gallbladder “sludge” with no evidence of stones. Laparoscopic cholecystectomy was performed. The results of tests for autoimmune pancreatitis (antinuclear antibodies and IgG subtypes) were negative. However, the patient had persistent abdominal pain and an elevated lipase level above 1000 U/L. Twenty-eight days after admission, she underwent magnetic resonance cholangiopancreatography (MRCP), which showed pancreas divisum. Following endoscopic retrograde cholangiopancreatography (ERCP), a sphincterotomy on the major papilla was performed with no noteworthy clinical improvement. Six weeks later, endoscopic retrograde cholangiopancreatography (ERCP) was repeated, with sphincterotomy of the minor papilla and placement of a stent. The patient’s pain resolved, and her lipase levels returned to normal within 14 days.
[Source 5 ]Pancreas divisum differential diagnosis
Pancreas divisum differential diagnosis may include:
- Acute Pancreatitis
- Chronic Abdominal Pain
- Chronic Pancreatitis
- Hyperamylasemia
- Pancreatic Cancer
- Sphincter of Oddi Dysfunction
Pancreas divisum treatment
Because the anomaly of pancreatic divisum usually is asymptomatic, treatment is generally offered to symptomatic patients after conducting a complete workup for other causes of pancreatitis and abdominal pain 98. Patients with mild symptoms can be managed conservatively. Alternatively, patients with recurrent episodes of pancreatitis or chronic pain may need treatment, which can be performed endoscopically or surgically, to alleviate papillary stenosis. Endoscopic interventions include minor papilla papillotomy (needle-knife sphincterotomy over a stent or pull-type sphincterotomy), endoscopic stenting, and balloon dilation of the minor papilla 98.
Minor papilla stenosis causing resistance to the flow of pancreatic secretion can lead to increased intraductal pressure. The cause of pancreatitis and pain in the abdomen is thought to be secondary to increased minor papilla intraductal pressure and, thus, minor papilla ductal decompression is used for management 98.
Endoscopic minor papilla sphincterotomy can be performed alone or along with stenting.
Sphincterotomy can be performed using a papillotome to make a 4- to 6-mm incision in the 10- to 12-o’clock position or over a stent used as a guide. Patients may need stent exchange, which is usually performed in 3-12 months, and papillary sphincterotomy is repeated. Postendoscopic minor papilla sphincterotomy pancreatitis and hemorrhage are common complications of endotherapy. Papillary restenosis, stent restenosis, and stent migration can occur after endotherapy 99.
Lu et al 100 found evidence that endoscopic retrograde cholangiopancreatography (ERCP) is a safe and effective treatment for symptomatic pancreas divisum, with no significant differences between underaged (age ≤17 years) and adult (age ≥18 years) groups in procedures, complications, or long-term follow-up results. In this study 100, investigators divided symptomatic patients with pancreas divisum (N = 82) into underaged and adult groups, reviewed their clinical information, and contacted them by telephone or reviewed their medical records to determine their long-term follow-up outcomes. After a median follow-up of 41 months, the overall response rate was 62.3%.
In a systematic review on endotherapy and surgery for pancreas divisum, in which complete or partial pain relief was considered as “response” to treatment, the pooled response rate of endotherapy for acute recurrent pancreatitis was 79.2%, 69% for chronic pancreatitis, and 54.4% for patients with pain related to pancreas divisum 25. The pooled overall response rate to endotherapy was 69.4%, whereas the response rate to surgery was 74.9%; the difference between the two was not significant. Thus, endotherapy can be a reasonable first-line treatment option for pain relief in pancreas divisum.
In a Medline search to identify all studies that compared the outcomes of endoscopic or surgical therapy for pancreas divisum, (56 observational studies: 31 endoscopic studies, 25 surgical studies), Hafezi et al 101 found that, compared with endoscopic treatment, surgery had a higher success rate (72% vs 62.3%), lower complication rate (23.8% vs 31.3%), and lower reintervention rate (14.4% vs 28.3%).
Acute recurrent pancreatitis has a higher response rate than chronic pancreatitis or chronic abdominal pain associated with pancreas divisum 25, 102. Rustagi et al 103 found a similar result: a 94% response rate for acute recurrent pancreatitis, 57% for chronic pancreatitis, and 54% for chronic abdominal pain.
Endoscopic Therapy
Endoscopic therapy includes minor papilla endoscopic sphincterotomy, minor papilla orifice balloon dilation (the term sphincteroplasty is present in the literature but should not be used in this setting) and trans minor papilla dorsal duct stenting 2. Techniques for cannulation of the minor papilla to achieve endotherapy have been well described 104, 105, 106, 107. Cannulation is best achieved when the duodenoscope is pushed along the greater curvature of the stomach into what is described as a long position (80–90 cms from incisors) 2. Once deep minor papilla cannulation is achieved, the duodenoscope may be returned to the short position off the greater curve of the stomach (55–60 cms from incisors) to improve stability and manipulation of instruments 2. The minor papilla is almost always in the right upper quadrant of the visual field when facing the major papilla with a variable distance between the two orifices (10mm-30mm cephalad and anterior) 2. In the rare instances when a diagnostic dorsal pancreatogram is desired, a tapered 5Fr catheter with a 23G-25G blunt needle tip protruding beyond the tip of the catheter is usually preferred 2. In the majority of situations when deep dorsal pancreatic duct cannulation is desired, a highly tapered 3–4–5 Fr catheter with a 0.018–0.021 inch guidewire is employed 2. Once cannulation is achieved, the subsequent fluoroscopic and interventional techniques are similar to those used in conventional ERCP. The success rate of minor papilla cannulation is variable with some studies suggesting 73–83% success 108, 79, 109 but this increases to 90–95% in the hands of an experienced interventionalist 67, 73. Failures are usually related to an imperceptible or distorted minor papilla from inflammation (pancreatitis, duodenal peptic ulcer disease), duodenal diverticula or malignancy, or inability to achieve adequate angles of approach for cannulation 2.
Surgery
All patients selected for surgical treatment should have confirmation of pancreas divisum by endoscopic retrograde cholangiopancreatography (ERCP).
The choice of operation depends on the clinical picture and extent of the disease 110.
Surgical minor papilla sphincterotomy 111 and surgical minor papilla sphincteroplasty 62, 112 have both been described to provide comparable effective and durable relief of symptoms with maximal efficacy noted in patients with recurrent acute pancreatitis 2.
When patient categorization is detailed, meaning recurrent, acute pancreatitis, chronic pain alone, or chronic pancreatitis is present, patients with recurrent attacks of pancreatitis usually respond better to surgical therapy, mirroring the endoscopic therapy series results 113. The clinical presentation and response rates to endotherapy and surgery within the three types of pancreas divisum were not significantly different 113, 109. Similar to endoscopic therapy, maximal symptomatic improvement was seen in patients with recurrent acute pancreatitis (83%), with a lower response rate in chronic pancreatitis (67%), and the least with chronic pancreatic-type abdominal pain (52%) the overall response rate to surgery was 74.9% 25. The follow up period was between 6 to 120 months with most studies greater than 50 months.
Some studies have found that patients with chronic pancreatitis have better response to surgical procedure than endotherapy 101.
Given the comparable outcomes between endotherapy and surgery of minor papilla in alleviating symptoms but with endotherapy having a favorable complication and mortality rate, endoscopy (i.e. ERCP) is usually considered the first line treatment, with surgery reserved for patients who fail minor papilla cannulation, endotherapy or have altered anatomy (e.g., gastric bypass).
In patients with recurrent acute pancreatitis who unfortunately fail minor papilla therapy or have progressed to chronic pancreatitis, further therapeutic options are limited. These may include management of symptoms related to chronic pancreatitis, including periods of pancreas rest with small bowel nutrition, celiac plexus block, somatostatin analogues, and an intrathecal pain pump 114. Patients with significantly dilated dorsal pancreatic ducts may benefit from a lateral pancreatojejunostomy (Puestow or Frey procedure) 115, 116. Total dorsal pancreatectomy has been proposed for benign or low grade malignant pancreatic tumors limited to the dorsal pancreas as an alternative to total pancreatectomy and may be extrapolated to patients with changes of chronic pancreatitis limited to the dorsal pancreas 117. Total pancreatectomy with auto-islet cell transplantation is an emerging option for patients with disease refractory to endotherapy. Reports of outcomes of total pancreatectomy with auto-islet cell transplantation data performed in patients with a normal anatomy suggest favorable outcomes and potentially can be extrapolated to patients with pancreas divisum 118, 119, 120, 121.
Minor papilla sphincterotomy and sphincteroplasty:
- Surgical sphincterotomy series and sphincteroplasty series seem to have similar outcomes.
Diet
In patients with pancreatic divisum, diet plays a crucial role in reducing the risk of flare-ups. The following measures can aid in the management of pancreatic divisum such as:
- Decrease the amount of fat intake. Because cholesterol appears to play a role in the formation of gallstones, it’s advisable to avoid eating too many foods with a high saturated fat content.
- Abstain from drinking alcohol. You can reduce your risk of developing acute pancreatitis by cutting back on drinking alcohol. This helps to prevent your pancreas being damaged.
- Reduce the frequency of food intake
- Take plenty of fluids and always be hydrated
- Losing weight. Being overweight, particularly being obese, increases the amount of cholesterol in your bile, which increases your risk of developing gallstones. You should control your weight by eating a healthy diet and taking plenty of regular exercise.
Pancreas divisum prognosis
Pancreas divisum is a the most common pancreatic anatomic birth defect with a prevalence of about 6–10% based on autopsy data 24, 52, imaging 122 and endoscopic studies 113, 123, with most patients (more than 95%) being without pancreatic symptoms and found incidentally. Studies have shown that pancreas divisum is prevalent in about 25 to 50% of the patients being evaluated for idiopathic recurrent acute pancreatitis 68, 123.
Pancreas divisum has been found to be associated with other pancreatic and biliary anomalies 2. The most frequent association is with annular pancreas where there is an abnormal rotation of the ventral bud of the pancreas around the duodenum, leading to a ring or semi-ring of pancreatic tissue around the second part of the duodenum 26. Prior studies suggested that there is about a 30–38% co-existence between the two conditions 26, 27, 28 but a recent larger study suggested the prevalence is as high as 50% 29. There have been reports scattered in the literature with pancreas divisum co-existing with anomalous pancreatic-biliary junction and choledochal cysts 30, 31, 32, 33, 34. However, there have been no large-scale studies to support any specific associations between these congenital anomalies. It has also been reported recently that there is a higher prevalence of pancreatic and biliary tumors in patients with pancreas divisum than with a normal ductal system. (7.8% vs 3.5%) 35. There have been reports of partial agenesis of the dorsal pancreas with pancreas divisum with some debate as to whether the agenesis led to the pancreas divisum or a consequence 36, 37.
- Madura JA. Pancreas divisum: stenosis of the dorsally dominant pancreatic duct. A surgically correctable lesion. Am J Surg. 1986 Jun;151(6):742-5. doi: 10.1016/0002-9610(86)90056-5[↩][↩]
- Gutta A, Fogel E, Sherman S. Identification and management of pancreas divisum. Expert Rev Gastroenterol Hepatol. 2019 Nov;13(11):1089-1105. doi: 10.1080/17474124.2019.1685871[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Inamdar S, Cote GA, Yadav D. Endotherapy for Pancreas Divisum. Gastrointest Endosc Clin N Am. 2023 Oct;33(4):789-805. doi: 10.1016/j.giec.2023.04.012[↩]
- Shayesteh S, Fouladi DF, Blanco A, Fishman EK, Kawamoto S. Idiopathic recurrent acute pancreatitis in the context of pancreas divisum: A case report. Radiol Case Rep. 2020 Sep 10;15(11):2255-2258. doi: 10.1016/j.radcr.2020.07.065[↩]
- Ng WK, Tarabain O. Pancreas divisum: a cause of idiopathic acute pancreatitis. CMAJ. 2009 Apr 28;180(9):949-51. doi: 10.1503/cmaj.080446[↩][↩][↩]
- Klein SD, Affronti JP. Pancreas divisum, an evidence-based review: part I, pathophysiology. Gastrointest Endosc. 2004 Sep;60(3):419-25. doi: 10.1016/s0016-5107(04)01815-2[↩][↩][↩]
- Bertin C, Pelletier AL, Vullierme MP, Bienvenu T, Rebours V, Hentic O, Maire F, Hammel P, Vilgrain V, Ruszniewski P, Lévy P. Pancreas divisum is not a cause of pancreatitis by itself but acts as a partner of genetic mutations. Am J Gastroenterol. 2012 Feb;107(2):311-7. doi: 10.1038/ajg.2011.424[↩][↩]
- Mortelé KJ, Rocha TC, Streeter JL, Taylor AJ. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006 May-Jun;26(3):715-31. doi: 10.1148/rg.263055164[↩][↩][↩]
- Bulow R, Simon P, Thiel R, Thamm P, Messner P, Lerch MM, Mayerle J. et al. Anatomic variants of the pancreatic duct and their clinical relevance: an MR-guided study in the general population. Eur Radiol. 2014;24(12):3142–3149. doi: 10.1007/s00330-014-3359-7[↩][↩]
- Mulholland MW, Moosa AR, Liddle RA. Pancreas: anatomy and structural anomalies. In: Yamada T, ed. Textbook of Gastroenterology. Philadelphia, Pa: JB Lippincott; 1995.[↩]
- Warshaw AL, Richter JM, Schapiro RH. The cause and treatment of pancreatitis associated with pancreas divisum. Ann Surg. 1983 Oct;198(4):443-52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1353182/pdf/annsurg00128-0041.pdf[↩][↩][↩]
- Li YL, Yu ML, Lee KH. The crossing duct sign. Abdom Radiol (NY). 2018 Jun;43(6):1506-1507. doi: 10.1007/s00261-017-1312-3[↩][↩]
- Dimitriou I, Katsourakis A, Nikolaidou E, Noussios G. The Main Anatomical Variations of the Pancreatic Duct System: Review of the Literature and Its Importance in Surgical Practice. J Clin Med Res. 2018 May;10(5):370-375. doi: 10.14740/jocmr3344w[↩][↩]
- Schulte SJ. Embryology, normal variation, and congenital anomalies of the pancreas. In: Stevenson GW, Freeny PC, Margulis AR, Burhenne HJ, editors. Margulis’ and Burhenne’s alimentary tract radiology. 5th ed. St. Louis: Mosby; 1994. pp. 1039–1051.[↩][↩][↩]
- Boninsegna E, Manfredi R, Ventriglia A, et al. Santorinicele: secretin-enhanced magnetic resonance cholangiopancreatography findings before and after minor papilla sphincterotomy. European radiology. 2015. August;25(8):2437–44. doi: 10.1007/s00330-015-3644-0[↩]
- Manfredi R, Brizi MG, Costamagna G, Masselli G, Vecchioli Scaldazza A, Marano P. Pancreas divisum and santorinicele: assessment by dynamic magnetic resonance cholangiopancreatography during secretin stimulation. Radiol Med. 2002 Jan-Feb;103(1-2):55-64. English, Italian.[↩]
- Cotton PB. Congenital anomaly of pancreas divisum as cause of obstructive pain and pancreatitis. Gut. 1980 Feb;21(2):105-14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1419363/pdf/gut00435-0033.pdf[↩][↩][↩][↩]
- Britt LG, Samuels AD, Johnson JW Jr. Pancreas divisum: is it a surgical disease? Ann Surg. 1983 Jun;197(6):654-62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1352886/pdf/annsurg00136-0024.pdf[↩][↩]
- Blair AJ 3rd, Russell CG, Cotton PB. Resection for pancreatitis in patients with pancreas divisum. Ann Surg. 1984 Nov;200(5):590-4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1250541/pdf/annsurg00117-0040.pdf[↩]
- Spicak J, Poulova P, Plucnarova J, Rehor M, Filipova H, Hucl T. Pancreas divisum does not modify the natural course of chronic pancreatitis. J Gastroenterol. 2007 Feb;42(2):135-9. doi: 10.1007/s00535-006-1976-x[↩]
- Dray X, Fajac I, Bienvenu T, Chryssostalis A, Sogni P, Hubert D. Association of pancreas divisum and recurrent acute pancreatitis with the IVS8-5T-12TG allele of the CFTR gene and CFTR dysfunction. Pancreas. 2007 Jul;35(1):90-3. doi: 10.1097/MPA.0b013e318054771f[↩]
- Pancreatic Divisum. https://emedicine.medscape.com/article/185307-overview[↩][↩]
- Saowaros V. Pancreas divisum: incidence and clinical evaluation in Thai patients. J Med Assoc Thai. 1992 Dec;75(12):692-6.[↩]
- Smanio T. Proposed nomenclature and classification of the human pancreatic ducts and duodenal papillae. Study based on 200 post mortems. Int Surg. 1969 Aug;52(2):125-41.[↩][↩]
- Liao Z, Gao R, Wang W, Ye Z, Lai XW, Wang XT, Hu LH, Li ZS. A systematic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy. 2009 May;41(5):439-44. doi: 10.1055/s-0029-1214505[↩][↩][↩][↩]
- Zyromski NJ, Sandoval JA, Pitt HA, et al. Annular pancreas: dramatic differences between children and adults. Journal of the American College of Surgeons. 2008. May;206(5):1019–25; discussion 1025–7. doi: 10.1016/j.jamcollsurg.2007.12.009[↩][↩][↩][↩]
- Sandrasegaran K, Patel A, Fogel EL, et al. Annular pancreas in adults. AJR American journal of roentgenology. 2009. August;193(2):455–60. doi: 10.2214/ajr.08.1596[↩][↩]
- Lehman GA, O’Connor KW. Coexistence of annular pancreas and pancreas divisum–ERCP diagnosis. Gastrointest Endosc. 1985 Feb;31(1):25-8. doi: 10.1016/s0016-5107(85)71960-8[↩][↩]
- Gromski MA, Lehman GA, Zyromski NJ, et al. Annular pancreas: endoscopic and pancreatographic findings from a tertiary referral ERCP center. Gastrointestinal endoscopy. 2018. September 18. doi: 10.1016/j.gie.2018.09.008[↩][↩]
- Cao J, Wang L, Zou X. Coexistence of Complete Pancreas Divisum and Anomalous Pancreaticobiliary Junction in a Patient With Type IA Choledochal Cyst. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2018. August 2. doi: 10.1016/j.cgh.2018.07.036[↩][↩]
- Patidar Y, Agarwal N, Gupta S, et al. Choledochocele with pancreas divisum: A rare co-occurrence diagnosed on magnetic resonance cholangiopancreatography. World journal of radiology. 2013. July 28;5(7):264–6. doi: 10.4329/wjr.v5.i7.264[↩][↩]
- Ng JW, Wong MK, Huang J, Chan YT. Incomplete pancreas divisum associated with abnormal junction of pancreaticobiliary duct system. Gastrointest Endosc. 1992 Jan-Feb;38(1):105-6. doi: 10.1016/s0016-5107(92)70364-2[↩][↩]
- Ransom-Rodriguez A, Blachman-Braun R, Sanchez-Garcia Ramos E, et al. A rare case of choledochal cyst with pancreas divisum: case presentation and literature review. Annals of hepato-biliary-pancreatic surgery. 2017. February;21(1):52–56. doi: 10.14701/ahbps.2017.21.1.52[↩][↩]
- Sanada Y, Sakuma Y, Sata N. Embryological etiology of pancreaticobiliary system predicted from pancreaticobiliary maljunction with incomplete pancreatic divisum: a case report. BMC surgery. 2018. August 2;18(1):50. doi: 10.1186/s12893-018-0385-4[↩][↩]
- Adibelli ZH, Adatepe M, Isayeva L, et al. Pancreas divisum: A risk factor for pancreaticobiliary tumors – an analysis of 1628 MR cholangiography examinations. Diagnostic and interventional imaging. 2017. February;98(2):141–147. doi: 10.1016/j.diii.2016.08.004[↩][↩]
- Kamisawa T, Takuma K, Egawa N, et al. A new embryological theory of the pancreatic duct system. Digestive surgery. 2010;27(2):132–6. doi: 10.1159/000286906[↩][↩][↩]
- Lehman GA, Kopecky KK, Rogge JD. Partial pancreatic agenesis combined with pancreas divisum and duodenum reflexum. Gastrointest Endosc. 1987 Dec;33(6):445-8. doi: 10.1016/s0016-5107(87)71686-1[↩][↩]
- Quest L, Lombard M. Pancreas divisum: opinio divisa. Gut. 2000 Sep;47(3):317-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1728027/pdf/v047p00317.pdf[↩][↩]
- DiMagno MJ, DiMagno EP. Chronic pancreatitis. Curr Opin Gastroenterol. 2005 Sep;21(5):544-54. https://core.ac.uk/reader/82542766[↩]
- Türkvatan A, Erden A, Türkoğlu MA, Yener Ö. Congenital variants and anomalies of the pancreas and pancreatic duct: imaging by magnetic resonance cholangiopancreaticography and multidetector computed tomography. Korean J Radiol. 2013 Nov-Dec;14(6):905-13. doi: 10.3348/kjr.2013.14.6.905[↩][↩][↩][↩][↩]
- Itoh S, Ikeda M, Ota T, Satake H, Takai K, Ishigaki T. Assessment of the pancreatic and intrapancreatic bile ducts using 0.5-mm collimation and multiplanar reformatted images in multislice CT. Eur Radiol. 2003 Feb;13(2):277-85. doi: 10.1007/s00330-002-1516-x[↩]
- Nguyen KT, Simeone DM. Pancreas: anatomy and structural anomalies. In: Podolsky DK, editor. Yamada’s textbook of gastroenterology. 6th ed. Hoboken (NJ): John Wiley & Sons Inc.; 2016. pp. 108–121.[↩]
- Kamisawa T, Koike M, Okamoto A. Embryology of the pancreatic duct system. Digestion. 1999. Mar-Apr;60(2):161–5. doi: 10.1159/000007642[↩]
- Shim JR, Park SJ, Park HM, Lee EC, Han SS. Are you prepared for pancreas bifidum? A case report. Ann Surg Treat Res. 2018 Jan;94(1):49-51. doi: 10.4174/astr.2018.94.1.49[↩][↩]
- Cotton PB. Pancreas divisum. Pancreas. 1988;3(3):245-7. doi: 10.1097/00006676-198805000-00001[↩]
- Cohn JA, Friedman KJ, Noone PG, Knowles MR, Silverman LM, Jowell PS. Relation between mutations of the cystic fibrosis gene and idiopathic pancreatitis. N Engl J Med. 1998 Sep 3;339(10):653-8. doi: 10.1056/NEJM199809033391002[↩]
- Sharer N, Schwarz M, Malone G, Howarth A, Painter J, Super M, Braganza J. Mutations of the cystic fibrosis gene in patients with chronic pancreatitis. N Engl J Med. 1998 Sep 3;339(10):645-52. doi: 10.1056/NEJM199809033391001[↩]
- Choudari CP, Imperiale TF, Sherman S, Fogel E, Lehman GA. Risk of pancreatitis with mutation of the cystic fibrosis gene. Am J Gastroenterol. 2004 Jul;99(7):1358-63. doi: 10.1111/j.1572-0241.2004.30655.x[↩]
- Gelrud A, Sheth S, Banerjee S, Weed D, Shea J, Chuttani R, Howell DA, Telford JJ, Carr-Locke DL, Regan MM, Ellis L, Durie PR, Freedman SD. Analysis of cystic fibrosis gener product (CFTR) function in patients with pancreas divisum and recurrent acute pancreatitis. Am J Gastroenterol. 2004 Aug;99(8):1557-62. doi: 10.1111/j.1572-0241.2004.30834.x[↩]
- Orellana-Donoso M, Milos-Brandenberg D, Benavente-Urtubia A, Guerra-Loyola J, Bruna-Mejias A, Nova-Baeza P, Becerra-Farfán Á, Sepulveda-Loyola W, Luque-Bernal RM, Valenzuela-Fuenzalida JJ. Incidence and Clinical Implications of Anatomical Variations in the Pancreas and Its Ductal System: A Systematic Review and Meta-Analysis. Life (Basel). 2023 Aug 9;13(8):1710. doi: 10.3390/life13081710[↩][↩][↩][↩]
- Kozu T, Suda K, Toki F. Pancreatic development and anatomical variation. Gastrointest Endosc Clin N Am. 1995 Jan;5(1):1-30.[↩]
- Stimec B, Bulajić M, Korneti V, Milosavljević T, Krstić R, Ugljesić M. Ductal morphometry of ventral pancreas in pancreas divisum. Comparison between clinical and anatomical results. Ital J Gastroenterol. 1996 Feb-Mar;28(2):76-80.[↩][↩]
- MacCarty RL, Stephens DH, Brown AL Jr, Carlson HC. Retrograde pancreatography in autopsy specimens. Am J Roentgenol Radium Ther Nucl Med. 1975 Feb;123(2):359-66. doi: 10.2214/ajr.123.2.359[↩]
- Kamisawa T, Egawa N, Tu Y, et al. Pancreatographic investigation of embryology of complete and incomplete pancreas divisum. Pancreas. 2007. January;34(1):96–102. doi: 10.1097/01.mpa.0000240607.49183.7e[↩]
- Moreira VF, Meroño E, Ledo L, San Román AL, Erdozain JC, Ruano JJ. Incomplete pancreas divisum. Gastrointest Endosc. 1991 Jan-Feb;37(1):104-5. doi: 10.1016/s0016-5107(91)70644-5[↩]
- Tulassay Z, Papp J, Farkas IE. Diagnostic aspects of incomplete pancreas divisum. Gastrointest Endosc. 1986 Dec;32(6):428. doi: 10.1016/s0016-5107(86)71934-2[↩]
- Ferri V, Vicente E, Quijano Y, Ielpo B, Duran H, Diaz E, Fabra I, Caruso R. Diagnosis and treatment of pancreas divisum: A literature review. Hepatobiliary Pancreat Dis Int. 2019 Aug;18(4):332-336. doi: 10.1016/j.hbpd.2019.05.004[↩]
- Adibelli ZH, Adatepe M, Imamoglu C, Esen OS, Erkan N, Yildirim M. Anatomic variations of the pancreatic duct and their relevance with the Cambridge classification system: MRCP findings of 1158 consecutive patients. Radiol Oncol. 2016 Sep 8;50(4):370-377. doi: 10.1515/raon-2016-0041[↩]
- Kamisawa T, Tu Y, Egawa N, Tsuruta K, Okamoto A. Clinical implications of incomplete pancreas divisum. JOP. 2006 Nov 10;7(6):625-30.[↩]
- Kim MH, Lee SS, Kim CD, Lee SK, Kim HJ, Park HJ, Joo YH, Kim DI, Yoo KS, Seo DW, Min YI. Incomplete pancreas divisum: is it merely a normal anatomic variant without clinical implications? Endoscopy. 2001 Sep;33(9):778-85. doi: 10.1055/s-2001-16521[↩]
- Pancreatic duct anatomic variation (diagram). https://radiopaedia.org/cases/pancreatic-duct-anatomic-variation-diagram[↩]
- Warshaw AL, Simeone JF, Schapiro RH, Flavin-Warshaw B. Evaluation and treatment of the dominant dorsal duct syndrome (pancreas divisum redefined). Am J Surg. 1990 Jan;159(1):59-64; discussion 64-6. doi: 10.1016/s0002-9610(05)80607-5[↩][↩]
- Staritz M, Meyer zum Büschenfelde KH. Elevated pressure in the dorsal part of pancreas divisum: the cause of chronic pancreatitis? Pancreas. 1988;3(1):108-10. doi: 10.1097/00006676-198802000-00019[↩][↩]
- Cotton PB. Pancreas divisum–curiosity or culprit? Gastroenterology. 1985 Dec;89(6):1431-5. doi: 10.1016/0016-5085(85)90667-5[↩]
- Bertin C, Pelletier AL, Vullierme MP, et al. Pancreas divisum is not a cause of pancreatitis by itself but acts as a partner of genetic mutations. The American journal of gastroenterology. 2012. February;107(2):311–7. doi: 10.1038/ajg.2011.424[↩][↩]
- Delhaye M, Cremer M. Clinical significance of pancreas divisum. Acta Gastroenterol Belg. 1992 May-Jun;55(3):306-13.[↩]
- Delhaye M, Engelholm L, Cremer M. Pancreas divisum: congenital anatomic variant or anomaly? Contribution of endoscopic retrograde dorsal pancreatography. Gastroenterology. 1985 Nov;89(5):951-8. doi: 10.1016/0016-5085(85)90193-3[↩][↩]
- Takuma K, Kamisawa T, Hara S, et al. Etiology of recurrent acute pancreatitis, with special emphasis on pancreaticobiliary malformation. Advances in medical sciences. 2012;57(2):244–50. doi: 10.2478/v10039-012-0041-7[↩][↩]
- Morgan DE, Logan K, Baron TH, et al. Pancreas divisum: implications for diagnostic and therapeutic pancreatography. AJR American journal of roentgenology. 1999. July;173(1):193–8. doi: 10.2214/ajr.173.1.10397125[↩]
- Wang DB, Yu J, Fulcher AS, et al. Pancreatitis in patients with pancreas divisum: imaging features at MRI and MRCP. World journal of gastroenterology. 2013. August 14;19(30):4907–16. doi: 10.3748/wjg.v19.i30.4907[↩][↩]
- Dhar A, Goenka MK, Kochhar R, Nagi B, Bhasin DK, Singh K. Pancrease divisum: five years’ experience in a teaching hospital. Indian J Gastroenterol. 1996 Jan;15(1):7-9.[↩]
- Lin TK, Abu-El-Haija M, Nathan JD, et al. Pancreas Divisum in Pediatric Acute Recurrent and Chronic Pancreatitis: Report From INSPPIRE. Journal of clinical gastroenterology. 2018. June 2. doi: 10.1097/mcg.0000000000001063[↩][↩]
- Benage D, McHenry R, Hawes RH, O’Connor KW, Lehman GA. Minor papilla cannulation and dorsal ductography in pancreas divisum. Gastrointest Endosc. 1990 Nov-Dec;36(6):553-7. doi: 10.1016/s0016-5107(90)71162-5[↩][↩]
- Borak GD, Romagnuolo J, Alsolaiman M, et al. Long-term clinical outcomes after endoscopic minor papilla therapy in symptomatic patients with pancreas divisum. Pancreas. 2009. November;38(8):903–6. doi: 10.1097/MPA.0b013e3181b2bc03[↩]
- Chacko LN, Chen YK, Shah RJ. Clinical outcomes and nonendoscopic interventions after minor papilla endotherapy in patients with symptomatic pancreas divisum. Gastrointestinal endoscopy. 2008. October;68(4):667–73. doi: 10.1016/j.gie.2008.01.025[↩]
- Heyries L, Barthet M, Delvasto C, et al. Long-term results of endoscopic management of pancreas divisum with recurrent acute pancreatitis. Gastrointestinal endoscopy. 2002. March;55(3):376–81. doi: 10.1067/mge.2002.121602[↩]
- Kwan V, Loh SM, Walsh PR, et al. Minor papilla sphincterotomy for pancreatitis due to pancreas divisum. ANZ journal of surgery. 2008. April;78(4):257–61. doi: 10.1111/j.1445-2197.2008.04431.x[↩]
- Siegel JH, Ben-Zvi JS, Pullano W, et al. Effectiveness of endoscopic drainage for pancreas divisum: endoscopic and surgical results in 31 patients. Endoscopy. 1990. May;22(3):129–33. doi: 10.1055/s-2007-1010727[↩]
- Lans JI, Geenen JE, Johanson JF, Hogan WJ. Endoscopic therapy in patients with pancreas divisum and acute pancreatitis: a prospective, randomized, controlled clinical trial. Gastrointest Endosc. 1992 Jul-Aug;38(4):430-4. doi: 10.1016/s0016-5107(92)70471-4[↩][↩]
- Lehman GA, Sherman S, Nisi R, Hawes RH. Pancreas divisum: results of minor papilla sphincterotomy. Gastrointest Endosc. 1993 Jan-Feb;39(1):1-8. doi: 10.1016/s0016-5107(93)70001-2[↩]
- Keith RG, Shapero TF, Saibil FG, Moore TL. Dorsal duct sphincterotomy is effective long-term treatment of acute pancreatitis associated with pancreas divisum. Surgery. 1989 Oct;106(4):660-6; discussion 666-7[↩]
- Garg PK, Khajuria R, Kabra M, et al. Association of SPINK1 gene mutation and CFTR gene polymorphisms in patients with pancreas divisum presenting with idiopathic pancreatitis. Journal of clinical gastroenterology. 2009. October;43(9):848–52. doi: 10.1097/MCG.0b013e3181a4e772[↩]
- Gelrud A, Sheth S, Banerjee S, et al. Analysis of cystic fibrosis gener product (CFTR) function in patients with pancreas divisum and recurrent acute pancreatitis. The American journal of gastroenterology. 2004. August;99(8):1557–62. doi: 10.1111/j.1572-0241.2004.30834.x[↩]
- Choudari CP, Imperiale TF, Sherman S, et al. Risk of Pancreatitis with Mutation of the Cystic Fibrosis Gene [Original Contribution]. American Journal Of Gastroenterology. 2004. 07/01/online;99:1358. doi: 10.1111/j.1572-0241.2004.30655.x[↩]
- Cohn JA, Friedman KJ, Noone PG, et al. Relation between mutations of the cystic fibrosis gene and idiopathic pancreatitis. The New England journal of medicine. 1998. September 3;339(10):653–8. doi: 10.1056/nejm199809033391002[↩]
- Witt H, Luck W, Hennies HC, et al. Mutations in the gene encoding the serine protease inhibitor, Kazal type 1 are associated with chronic pancreatitis. Nature genetics. 2000. June;25(2):213–6. doi: 10.1038/76088[↩]
- Bhatia E, Choudhuri G, Sikora SS, Landt O, Kage A, Becker M, Witt H. Tropical calcific pancreatitis: strong association with SPINK1 trypsin inhibitor mutations. Gastroenterology. 2002 Oct;123(4):1020-5. doi: 10.1053/gast.2002.36028[↩]
- Definition & Facts for Pancreatitis. https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitis/definition-facts[↩]
- Jones MR, Hall OM, Kaye AM, Kaye AD. Drug-induced acute pancreatitis: a review. Ochsner J. 2015 Spring;15(1):45-51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4365846[↩]
- Forsmark CE, Vege SS, Wilcox CM. Acute Pancreatitis. N Engl J Med. 2016 Nov 17;375(20):1972-1981. doi: 10.1056/NEJMra1505202[↩]
- Vege SS, Yadav D, Chari ST. Pancreatitis. In: Talley NJ, GR Locke, Saito YA, editors. GI Epidemiology. Malden, MA: Blackwell Publishing;; 2007.[↩]
- Ketwaroo GA, Freedman SD, Sheth SG. Approach to patients with suspected chronic pancreatitis: a comprehensive review. Pancreas. 2015 Mar;44(2):173-80. doi: 10.1097/MPA.0000000000000239[↩]
- Benjamin O, Lappin SL. Chronic Pancreatitis. [Updated 2022 Jun 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482325[↩][↩]
- Turkvatan A, Erden A, Turkoglu MA, Yener O. Congenital variants and anomalies of the pancreas and pancreatic duct: imaging by magnetic resonance cholangiopancreaticography and multidetector computed tomography. Korean J Radiol. 2013;14(6):905–913. doi: 10.3348/kjr.2013.14.6.905[↩]
- Adibelli ZH, Adatepe M, Imamoglu C, Esen OS, Erkan N, Yildirim M. Anatomic variations of the pancreatic duct and their relevance with the Cambridge classification system: MRCP findings of 1158 consecutive patients. Radiol Oncol. 2016;50(4):370–377. doi: 10.1515/raon-2016-0041[↩]
- Vitellas KM, Keogan MT, Spritzer CE, Nelson RC. MR cholangiopancreatography of bile and pancreatic duct abnormalities with emphasis on the single-shot fast spin-echo technique. Radiographics. 2000 Jul-Aug;20(4):939-57; quiz 1107-8, 1112. doi: 10.1148/radiographics.20.4.g00jl23939. Erratum in: Radiographics 2000 Sep-Oct;20(5):1494.[↩]
- Wan J, Ouyang Y, Yu C, Yang X, Xia L, Lu N. Comparison of EUS with MRCP in idiopathic acute pancreatitis: a systematic review and meta-analysis. Gastrointest Endosc. 2018 May;87(5):1180-1188.e9. doi: 10.1016/j.gie.2017.11.028[↩][↩]
- Pancreatic Divisum Treatment & Management. https://emedicine.medscape.com/article/185307-treatment[↩][↩][↩]
- Bor R, Madácsy L, Fábián A, Szepes A, Szepes Z. Endoscopic retrograde pancreatography: When should we do it? World J Gastrointest Endosc. 2015 Aug 25;7(11):1023-31. doi: 10.4253/wjge.v7.i11.1023[↩]
- Lu Y, Xu B, Chen L, Bie LK, Gong B. Endoscopic Intervention through Endoscopic Retrograde Cholangiopancreatography in the Management of Symptomatic Pancreas Divisum: A Long-Term Follow-Up Study. Gut Liver. 2016 May 23;10(3):476-82. doi: 10.5009/gnl15362[↩][↩]
- Hafezi M, Mayschak B, Probst P, Büchler MW, Hackert T, Mehrabi A. A systematic review and quantitative analysis of different therapies for pancreas divisum. Am J Surg. 2017 Sep;214(3):525-537. doi: 10.1016/j.amjsurg.2016.12.025[↩][↩]
- Borak GD, Romagnuolo J, Alsolaiman M, Holt EW, Cotton PB. Long-term clinical outcomes after endoscopic minor papilla therapy in symptomatic patients with pancreas divisum. Pancreas. 2009 Nov;38(8):903-6. doi: 10.1097/MPA.0b013e3181b2bc03[↩]
- Rustagi T, Golioto M. Diagnosis and therapy of pancreas divisum by ERCP: a single center experience. J Dig Dis. 2013 Feb;14(2):93-9. doi: 10.1111/1751-2980.12004[↩]
- Lehman GA, Sherman S. Pancreas divisum. Diagnosis, clinical significance, and management alternatives. Gastrointest Endosc Clin N Am. 1995 Jan;5(1):145-70.[↩]
- Lehman GA, Sherman S. Diagnosis and therapy of pancreas divisum. Gastrointest Endosc Clin N Am. 1998 Jan;8(1):55-77.[↩]
- McCarthy J, Fumo D, Geenen JE. Pancreas divisum: a new method for cannulating the accessory papilla. Gastrointest Endosc. 1987 Dec;33(6):440-2. doi: 10.1016/s0016-5107(87)71684-8[↩]
- O’Connor KW, Lehman GA. An improved technique for accessory papilla cannulation in pancreas divisum. Gastrointest Endosc. 1985 Feb;31(1):13-7. doi: 10.1016/s0016-5107(85)71956-6[↩]
- Ertan A Long-term results after endoscopic pancreatic stent placement without pancreatic papillotomy in acute recurrent pancreatitis due to pancreas divisum. Gastrointestinal endoscopy. 2000. July;52(1):9–14. doi: 10.1067/mge.2000.106311[↩]
- Jacob L, Geenen JE, Catalano MF, Johnson GK, Geenen DJ, Hogan WJ. Clinical presentation and short-term outcome of endoscopic therapy of patients with symptomatic incomplete pancreas divisum. Gastrointest Endosc. 1999 Jan;49(1):53-7. doi: 10.1016/s0016-5107(99)70445-1[↩][↩]
- Schneider L, Müller E, Hinz U, Grenacher L, Büchler MW, Werner J. Pancreas divisum: a differentiated surgical approach in symptomatic patients. World J Surg. 2011 Jun;35(6):1360-6. doi: 10.1007/s00268-011-1076-9[↩]
- Keith RG, Shapero TF, Saibil FG, Moore TL. Dorsal duct sphincterotomy is effective long-term treatment of acute pancreatitis associated with pancreas divisum. Surgery. 1989 Oct;106(4):660-6; discussion 666-7.[↩]
- Bradley EL 3rd, Stephan RN. Accessory duct sphincteroplasty is preferred for long-term prevention of recurrent acute pancreatitis in patients with pancreas divisum. J Am Coll Surg. 1996 Jul;183(1):65-70.[↩]
- Liao Z, Gao R, Wang W, et al. A systematic review on endoscopic detection rate, endotherapy, and surgery for pancreas divisum. Endoscopy. 2009. May;41(5):439–44. doi: 10.1055/s-0029-1214505[↩][↩][↩]
- Anderson MA, Akshintala V, Albers KM, et al. Mechanism, assessment and management of pain in chronic pancreatitis: Recommendations of a multidisciplinary study group. Pancreatology : official journal of the International Association of Pancreatology (IAP) [et al]. 2016. Jan-Feb;16(1):83–94. doi: 10.1016/j.pan.2015.10.015[↩]
- Pappas SG, Pilgrim CH, Keim R, et al. The Frey procedure for chronic pancreatitis secondary to pancreas divisum. JAMA surgery. 2013. November;148(11):1057–62. doi: 10.1001/jamasurg.2013.3728[↩]
- Skorzewska M, Romanowicz T, Mielko J, et al. Frey operation for chronic pancreatitis associated with pancreas divisum: case report and review of the literature. Przeglad gastroenterologiczny. 2014;9(3):175–8. doi: 10.5114/pg.2014.43581[↩]
- Conci S, Ruzzenente A, Bertuzzo F, et al. Total Dorsal Pancreatectomy, an Alternative to Total Pancreatectomy: Report of a New Case and Literature Review. Digestive surgery. 2018. July 13:1–6. doi: 10.1159/000490198[↩]
- Bellin MD, Abu-El-Haija M, Morgan K, et al. A multicenter study of total pancreatectomy with islet autotransplantation (TPIAT): POST (Prospective Observational Study of TPIAT). Pancreatology : official journal of the International Association of Pancreatology (IAP) [et al]. 2018. April;18(3):286–290. doi: 10.1016/j.pan.2018.02.001[↩]
- Bellin MD, Kerdsirichairat T, Beilman GJ, et al. Total Pancreatectomy With Islet Autotransplantation Improves Quality of Life in Patients With Refractory Recurrent Acute Pancreatitis. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2016. September;14(9):1317–23. doi: 10.1016/j.cgh.2016.02.027[↩]
- Wilson GC, Sutton JM, Salehi M, et al. Surgical outcomes after total pancreatectomy and islet cell autotransplantation in pediatric patients. Surgery. 2013. October;154(4):777–83; discussion 783–4. doi: 10.1016/j.surg.2013.07.003[↩]
- Wilson GC, Sutton JM, Smith MT, et al. Completion pancreatectomy and islet cell autotransplantation as salvage therapy for patients failing previous operative interventions for chronic pancreatitis. Surgery. 2015. October;158(4):872–8; discussion 879–80. doi: 10.1016/j.surg.2015.04.045[↩]
- Bulow R, Simon P, Thiel R, et al. Anatomic variants of the pancreatic duct and their clinical relevance: an MR-guided study in the general population. European radiology. 2014. Dec;24(12):3142–9. doi: 10.1007/s00330-014-3359-7[↩]
- Bernard JP, Sahel J, Giovannini M, Sarles H. Pancreas divisum is a probable cause of acute pancreatitis: a report of 137 cases. Pancreas. 1990 May;5(3):248-54. doi: 10.1097/00006676-199005000-00002[↩][↩]