Contents
What is parathyroid gland
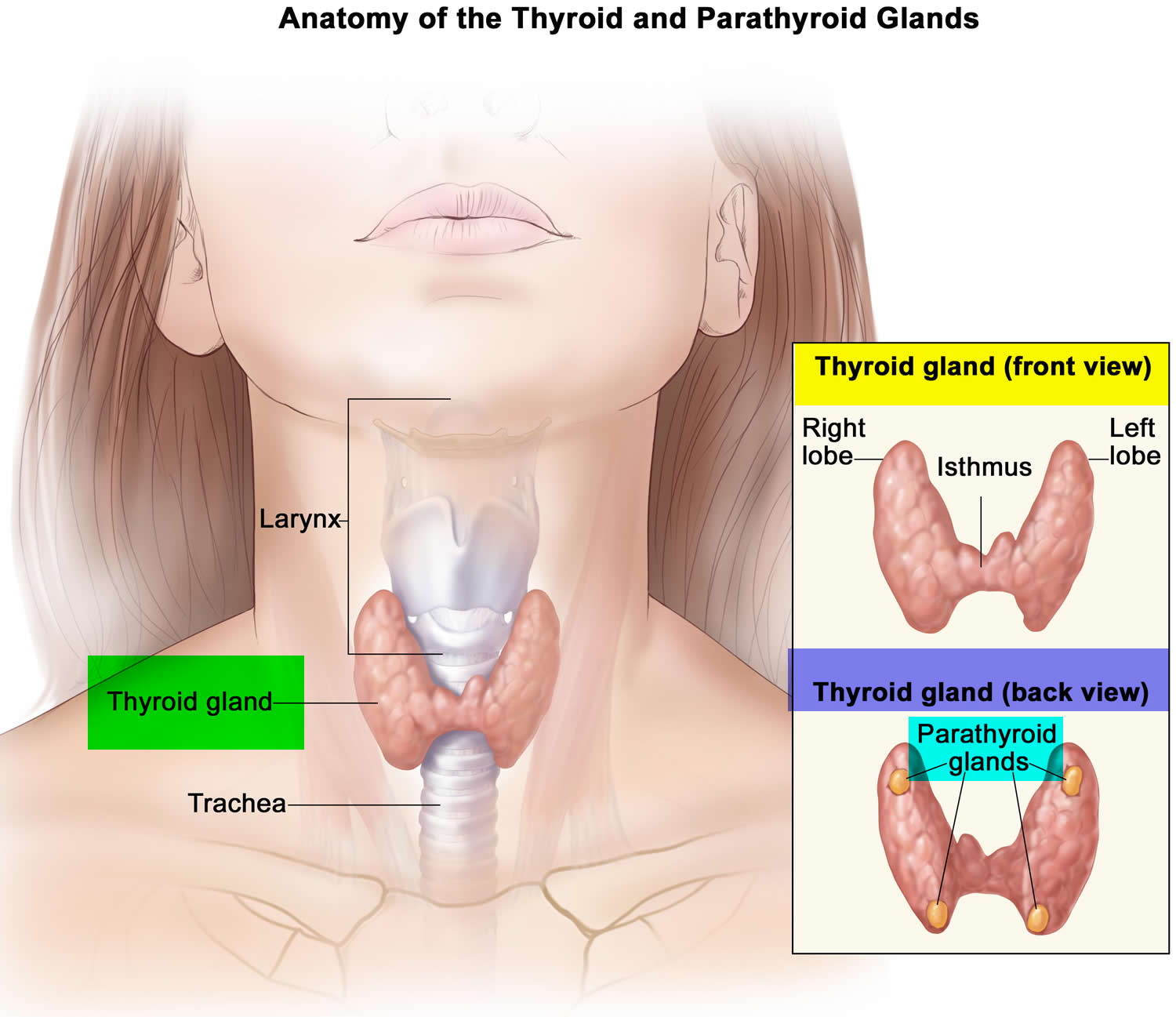
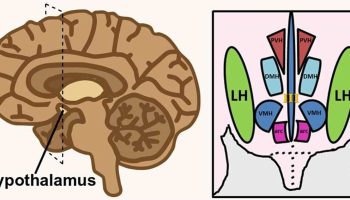
The parathyroid glands are ovoid glands, usually four in number, partially embedded in the posterior (behind) surface of the thyroid. Each parathyroid gland has a mass of about 40 mg and is about 3 to 8 mm long and 2 to 5 mm wide. Usually, one superior and one inferior parathyroid gland are attached to each lateral thyroid lobe, for a total of four. The parathyroid glands are separated from the thyroid follicles by a thin fibrous capsule and adipose tissue. Often, the parathyroid glands occur in other locations ranging from as high as the hyoid bone to as low as the aortic arch, and about 5% of people have more than four parathyroids.
Microscopically, the parathyroid glands contain two kinds of epithelial cells. The more numerous cells, called chief cells or principal cells, produce parathyroid hormone (PTH), also called parathormone. The function of the other kind of cell, called an oxyphil cell, is not known in a normal parathyroid gland. Oxyphil cells do not appear until after puberty, and then their numbers increase with age. However, its presence clearly helps to identify the parathyroid gland histologically due to its unique staining characteristics. Furthermore, in a cancer of the parathyroid glands, oxyphil cells secrete excess parathyroid hormone (PTH).
Attached to the chief cells of these parathyroid glands is a newly discovered molecule called the Calcium Sensing Receptor (CaSR). This Calcium Sensing Receptor (CaSR) responds to very small changes in the blood level of calcium to turn the parathyroid glands on and off when needed. The Calcium Sensing Receptor (CaSR) is working as the thermostat. If the body is not getting enough calcium from the diet, for example, the Calcium Sensing Receptor (CaSR) senses a need to get calcium from somewhere. The immediate response is for the parathyroid glands to make and secrete more of their active hormone – parathyroid hormone (PTH). This sets off a chain of events that get more calcium into the bloodstream. First, parathyroid hormone (PTH) goes to the calcium bank – namely your bones, where 98% of the body’s store of calcium is warehoused. This is good for the blood calcium and for the cells that need calcium, but not good for the bones themselves. The second line of defense against a need for more calcium is the kidneys. Here parathyroid hormone (PTH) does two things. First, it limits the kidneys from excreting too much calcium, thereby keeping the blood levels up. Next, it works on the kidneys to produce another hormone called calcitriol or “active vitamin D.”
Figure 1. Parathyroid gland location (hidden behind the thyroid gland)
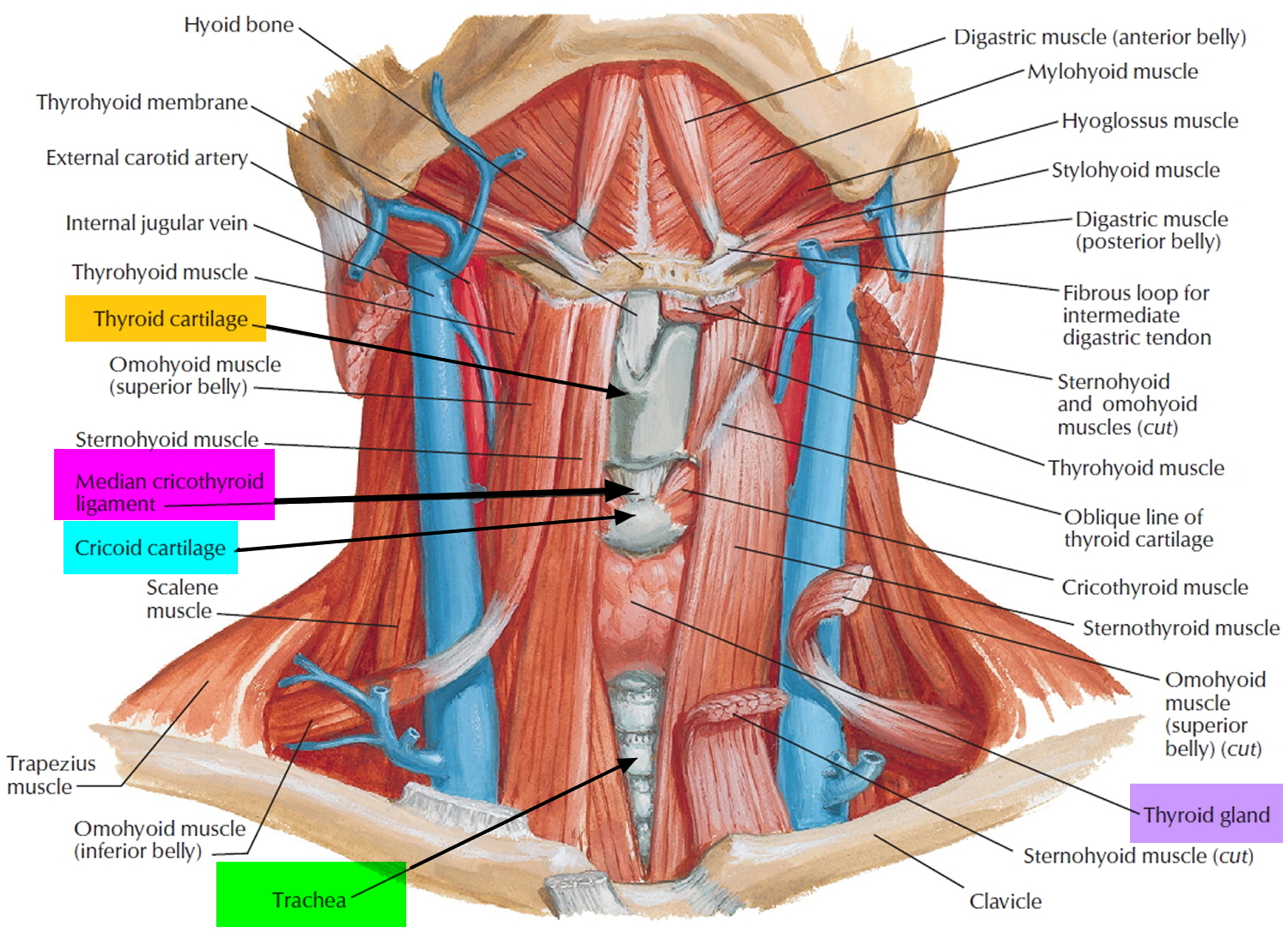
Figure 2. Thyroid gland location
Parathyroid gland function
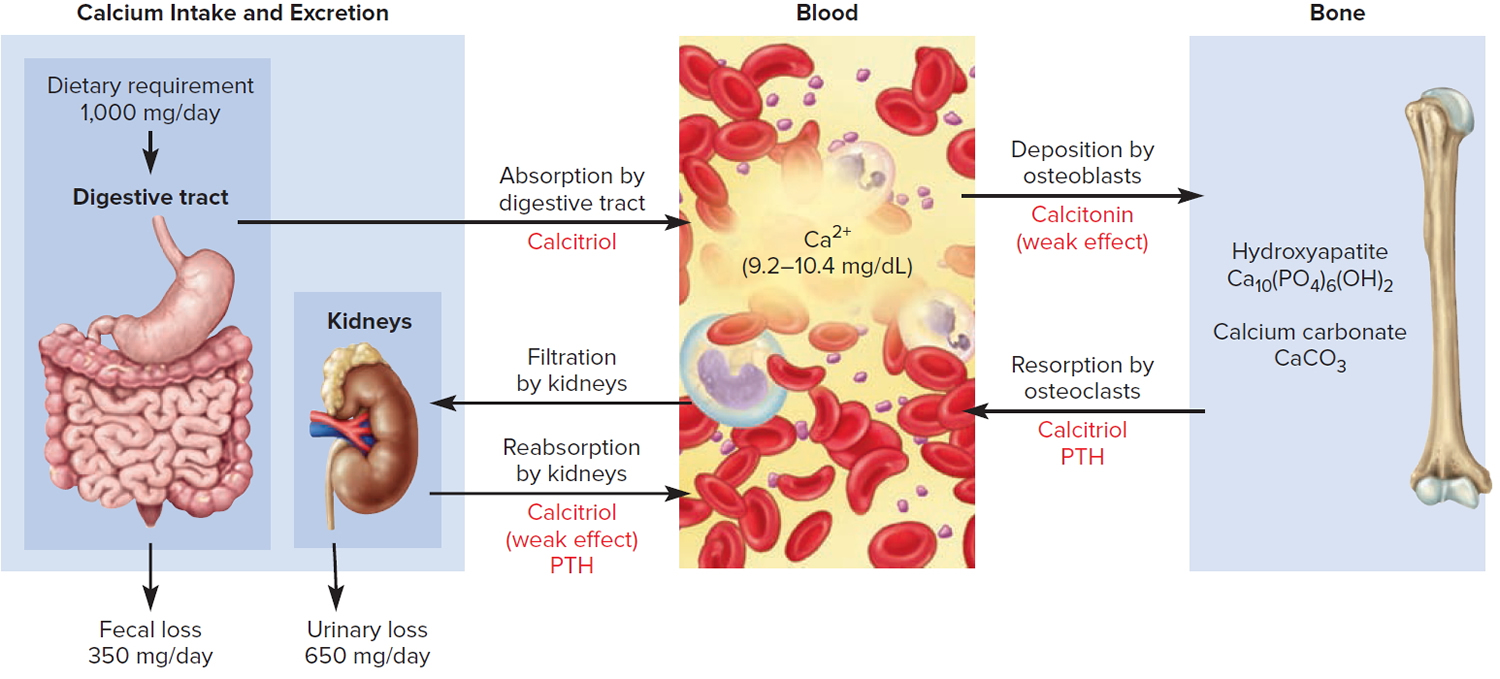
Parathyroid hormone (PTH) is secreted by the parathyroid glands, which regulates blood calcium levels (Ca 2+).
Furthermore, the parathyroid hormone (PTH) is also the major regulator of the levels of magnesium (Mg 2+), and phosphate (HPO4 2−) ions in the blood. The specific action of parathyroid hormone (PTH) is to increase the number and activity of osteoclasts. The result is elevated bone resorption, which releases ionic calcium (Ca 2+) and phosphates (HPO4 2−) into the blood.
Parathyroid hormone (PTH) also acts on the kidneys. First, it slows the rate at which Ca 2+ and magnesium (Mg 2+) are lost from blood into the urine. Second, it increases loss of phosphate (HPO4 2−) from blood into the urine. Because more phosphate (HPO4 2−) is lost in the urine than is gained from the bones, PTH decreases blood phosphate (HPO4 2−) level and increases blood Ca2+ and magnesium (Mg 2+) levels.
A third effect of PTH on the kidneys is to promote formation of the hormone calcitriol, the active form of vitamin D. Calcitriol, also known as 1,25-dihydroxyvitamin D3, increases the rate of calcium (Ca 2+), phosphate (HPO4 2−) and magnesium (Mg 2+) absorption from the gastrointestinal tract into the blood.
Figure 3. Hormonal control of calcium balance
Note: The central panel represents the blood reservoir of calcium and shows its normal (safe) range. Calcitriol and Parathyroid Hormone (PTH) regulate calcium exchanges between the blood and the small intestine and kidneys (left). Calcitonin, calcitriol, and Parathyroid Hormone (PTH) regulate calcium exchanges between blood and bone (right).
Control of Secretion of Calcitonin and Parathyroid Hormone
The blood calcium (Ca 2+) level directly controls the secretion of both calcitonin and parathyroid hormone (PTH) via negative feedback loops that do not involve the pituitary gland.
These parathyroid glands release PTH when blood calcium is low. A mere 1% drop in the blood calcium level doubles the secretion of PTH.
A lower-than-normal level of calcium ions (Ca 2+) in the blood stimulates chief cells of the parathyroid gland to release more parathyroid hormone (PTH).
PTH raises the blood calcium level by four mechanisms:
- PTH binds to receptors on the osteoblasts, stimulating them to secrete RANKL, which in turn raises the osteoclast population and promotes bone resorption of bone extracellular matrix, which releases Ca 2+ into the blood and slows loss of Ca 2+ in the urine, raising the blood level of Ca 2+.
- PTH promotes Ca 2+ reabsorption by the kidneys, so less calcium is lost in the urine.
- PTH promotes the final step of calcitriol synthesis in the kidneys, thus enhancing the calcium-raising effect of calcitriol. Calcitriol stimulates increased absorption of Ca 2+ from foods in the gastrointestinal tract, which helps increase the blood level of Ca 2+.
- TH inhibits collagen synthesis by osteoblasts, thus inhibiting bone deposition.
Once the levels of calcium have been brought back to normal, the system slows down and waits for the next call. Interestingly, and perhaps surprising to most, this chain of events happens without you knowing about or feeling anything wrong. Even the changes in blood calcium that set the whole system in motion are too small to be measured most of the time. The need to keep the blood calcium constant is so great that, when everything is working properly, even the minutest change triggers a response from the parathyroid glands. Yes, vitamin D is actually a hormone, not a vitamin. The vitamin D you get from your multi-vitamins, your diet or that is made by the action of sunlight on your skin is not very active at all. First, it has to go to the liver where it is turned into calcediol, which is more active than vitamin D but still not good enough. This calcediol is then carried in the blood to the kidneys where it is converted to calcitriol. This change from calcediol to calcitriol is controlled by PTH.
Figure 4. Correction of hypocalcemia (low blood calcium)
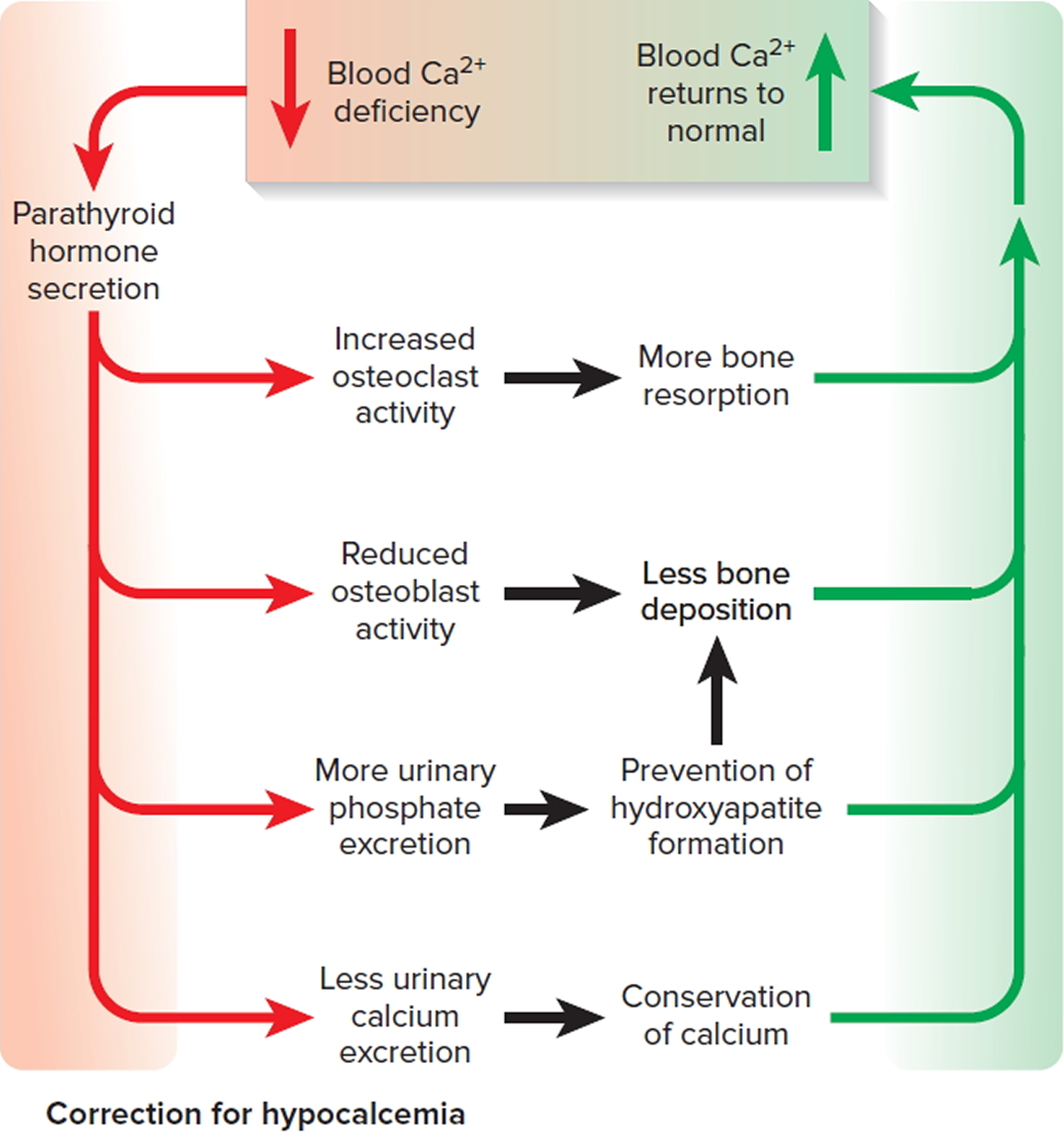
Note: The correction of hypocalcemia by parathyroid hormone (PTH).
- A higher-than-normal level of calcium ions (Ca 2+) in the blood stimulates parafollicular cells of the thyroid gland to release more calcitonin.
- Calcitonin inhibits the activity of osteoclasts, thereby decreasing the blood calcium ions (Ca 2+) level.
Parathyroid gland surgery
Parathyroidectomy is surgery to remove the parathyroid glands or parathyroid tumors 1. The parathyroid glands are right behind your thyroid gland in your neck. These glands help your body control the calcium level in the blood.
Why is the parathyroid gland surgery done ?
Your doctor may recommend this surgery if one or more of your parathyroid glands is producing too much parathyroid hormone. This condition is called hyperparathyroidism. It is often caused by a small non-cancerous (benign) tumor called an adenoma.
Your doctor will consider many factors when deciding whether to do surgery and what type of surgery would be best for you. Some of these factors are:
- Your age
- Calcium levels in your urine and blood
- Whether you have symptoms
Description of parathyroid gland surgery
You will receive general anesthesia (asleep and pain-free) for this surgery.
Usually the parathyroid glands are removed using a 2- to 4-inch (5- to 10- cm) surgical cut on your neck. During surgery:
- The cut is usually made in the center of your neck just under your Adam’s apple (thyroid cartilage).
- Your surgeon will look for the four parathyroid glands and remove any that are diseased.
- You may have a special blood test during surgery that will tell if all the diseased glands were removed.
- In rare cases, when all four of these glands need to be removed, part of one is transplanted into the forearm. This helps ensure your body’s calcium level stays at a healthy level.
The specific type of surgery depends on where the diseased parathyroid glands are. Types of surgery include:
- Minimally invasive parathyroidectomy: You may receive a shot of a very small amount of radioactive tracer before this surgery. This helps highlight the diseased glands. If you have this shot, your surgeon will use a special probe, like a Geiger counter, to locate the parathyroid gland. Your surgeon will make a small cut (1 to 2 inches; or 2.5 to 5 cm) on one side of your neck, and then remove the diseased gland through it. This procedure takes about 1 hour.
- Video-assisted parathyroidectomy: Your surgeon will make two small cuts in your neck. One is for instruments, and the other is for a camera. Your surgeon will use the camera to view the area and will remove the diseased glands with the instruments.
- Endoscopic parathyroidectomy: Your surgeon will make two or three small cuts in the front of your neck and one cut above the top of your collarbone. This reduces visible scarring, pain, and recovery time. This cut is less than 2 inches (5 cm) long. The procedure to remove any diseased parathyroid glands is similar to video-assisted parathyroidectomy.
Risks of parathyroid gland surgery
Risks for anesthesia and surgery in general are:
- Reactions to medicines or breathing problems
- Bleeding, blood clots, or infection
Risks for parathyroidectomy are:
- Injury to the thyroid gland or the need to remove part of the thyroid gland
- Hypoparathyroidism. This can lead to low calcium levels that are dangerous to your health.
- Injury to the nerves going to the muscles that move your vocal cords. You may have a hoarse or weaker voice which could be temporary or permanent.
- Difficulty breathing. This is very rare and almost always goes away several weeks or months after surgery.
Before the parathyroid gland surgery
Parathyroid glands are very small. You may need to have tests that show exactly where your glands are. This will help your surgeon find your parathyroid glands during surgery. Two of the tests you may have are a CT scan and an ultrasound.
In addition to the CT scan and ultrasound test, before the surgery is scheduled you would also have a test called a Sestamibi scan. For the Sestamibi scan, you would be injected with a minute amount of radioactive material that goes directly to the abnormal parathyroid tissue and an image can be taken to guide the surgeon where to look. Like any test, this is not 100% perfect but it is pretty good, particularly if the person doing the scan has had lot of experience. The ultrasound test does not involve any radioactivity but is simply what it says – an ultrasound probe is passed over your neck looking for one or more parathyroids that appear to be larger than normal. Different surgeons favor one of these tests over the other, depending on their experience. Sometimes if one of the tests doesn’t give a clear-cut answer, you will also have the other test done to help the surgeon decide what to look for during the operation. The surgery itself is very straightforward when done by someone who knows what he or she is doing. Many centers are now doing this surgery without the patient needing to be admitted to the hospital.
Before surgery, an anesthesiologist will review your medical history with you and decide what type of anesthesia to use. The anesthesiologist is the doctor who will give you the medicine that allows you to sleep and be pain-free during surgery and who monitors you during surgery.
Tell your surgeon:
- If you are or might be pregnant
- What medicines, vitamins, herbs, and other supplements you’re taking, even ones you bought without a prescription
During the week before your surgery:
- Fill any prescriptions for pain medicine and calcium you’ll need after surgery.
- You may be asked to stop taking aspirin, ibuprofen (Advil, Motrin), vitamin E, warfarin (Coumadin), and any other drugs that make it hard for your blood to clot.
- Ask your surgeon which drugs you should still take on the day of your surgery.
On the day of your surgery:
- Follow instructions about not eating and drinking.
- Take the medicines your surgeon told you to take with a small sip of water.
- Arrive at the hospital on time.
After the parathyroid gland surgery
Often, people can go home the same day they have surgery. You can start your everyday activities in a few days. It will take about 1 to 3 weeks for you to fully heal.
The surgery area must be kept clean and dry. You may need to drink liquids and eat soft foods for a day.
- Call your surgeon if you have any numbness or tingling around your mouth in the 24 to 48 hours after surgery. This is caused by low calcium. Follow instructions about how to take your calcium supplements.
After this procedure, you should have routine blood tests to check your calcium level.
Outlook (Prognosis) of parathyroid gland surgery
People usually recover soon after this surgery. Recovery may be fastest when less invasive techniques are used.
Sometimes, another surgery is needed to remove more of the parathyroid glands.
Parathyroid gland disorders
The parathyroid glands make parathyroid hormone (PTH), which helps your body keep the right balance of calcium (Ca 2+), magnesium (Mg 2+) and phosphate (HPO4 2−) ions in the blood.
If your parathyroid glands make too much or too little hormone, it disrupts this balance. If they secrete extra PTH, you have hyperparathyroidism, and your blood calcium rises. In many cases, a benign tumor on a parathyroid gland makes it overactive. Or, the extra hormones can come from enlarged parathyroid glands. Very rarely, the cause is cancer.
If you do not have enough PTH, you have hypoparathyroidism. Your blood will have too little calcium and too much phosphorous. Causes include injury to the glands, endocrine disorders, or genetic conditions. Treatment is aimed at restoring the balance of calcium and phosphorous.
How do you know if your parathyroid glands are working properly ?
Most of the time you won’t notice anything wrong unless your doctor happens to order a blood calcium test and finds that the level is too high (not uncommon) or too low (quite uncommon). Slightly high blood calcium caused by overactive parathyroid glands can be present for many years without your being aware of it 2. That does not mean that it might not be doing you any harm. There can be gradual weakening of your bones, causing you to be at increased risk for having a fracture and osteoporosis.
There might also be an increased loss of calcium through the kidneys, increasing your chances of having a kidney stone. In fact, everyone with a fracture that isn’t the result of major trauma and everyone who has a kidney stone should have blood calcium and parathyroid hormone measured 2.
There are even more subtle changes that might be linked to overactive parathyroids. These include an increased risk of high blood diabetes and very subtle changes in your thinking capacity. These are all very common, even in people with normal parathyroid glands, so the link between the parathyroids and these conditions in any individual patient is not always very clear. Only occasionally are these conditions made better by correcting the abnormal parathyroids.
What is Hyperparathyroidism
Hyperparathyroidism is a disorder in which the parathyroid glands in your neck produce too much parathyroid hormone (PTH) 3.
Causes of hyperparathyroidism
There are 4 tiny parathyroid glands in the neck, near or attached to the back side of the thyroid gland.
The parathyroid glands help control calcium use and removal by the body. They do this by producing parathyroid hormone (PTH). PTH helps control calcium, phosphorus, and vitamin D levels in the blood and bone.
When calcium level is too low, the body responds by making more PTH. This causes the calcium level in the blood to rise.
About 1 in 600 to 1 in 1000 people have primary hyperparathyroidism 2. In 85-90% of these patients, only one of the four glands is involved and only that one is removed by the surgeon. Once that is done successfully, the disease is essentially cured and only rarely does it come back. In 10-15% of cases, all four glands are involved. Most often this is seen in people with a genetic or family history of hyperparathyroidism. In that case, the surgeon will remove three and a half glands and the remaining small piece of parathyroid gland tissue is enough to get by with. A recurrence of hyperparathyroidism is more common in such cases, but here too it is uncommon.
When one or both of the parathyroid glands grow larger, it leads to too much PTH. Most often, the cause is not known.
- The disease is most common in people over age 60, but it can also occur in younger adults. Hyperparathyroidism in childhood is very unusual.
- Women are more likely to be affected than men.
- Radiation to the head and neck increases the risk.
- In rare cases, the disease is caused by parathyroid cancer.
Medical conditions that cause low blood calcium or increased phosphate can also lead to hyperparathyroidism. Common conditions include:
- Conditions that make it hard for the body to remove phosphate
- Kidney failure
- Not enough calcium in the diet
- Too much calcium lost in the urine
- Vitamin D disorders (may occur in children who do not eat a variety of foods, and in older adults who do not get enough sunlight on their skin)
- Problems absorbing nutrients from food
Symptoms of hyperparathyroidism
Hyperparathyroidism is often diagnosed before symptoms occur.
Symptoms are mostly caused by damage to organs from high calcium level in the blood, or by the loss of calcium from the bones. Symptoms can include:
- Bone pain or tenderness
- Depression and forgetfulness
- Feeling tired, ill, and weak
- Fragile bones of the limbs and spine that can break easily
- Increased amount of urine produced and needing to urinate more often
- Kidney stones
- Nausea and loss of appetite
How is hyperparathyroidism diagnosed ?
The health care provider will do a physical exam and ask about symptoms.
Tests that may be done include:
- PTH blood test
- Calcium blood test
- Alkaline phosphatase
- Phosphorus
- 24-hour urine test
Bone x-rays and bone mineral density (DXA) tests can help detect bone loss, fractures, or bone softening.
X-rays, ultrasound, or CT scans of the kidneys or urinary tract may show calcium deposits or a blockage.
Treatment for hyperparathyroidism
If you have a mildly increased calcium level and don’t have symptoms, you may choose to have regular checkups or get treated.
If you decide to have treatment, it may include:
- Drinking more fluids to prevent kidney stones from forming
- Exercising
- Not taking a type of water pill called thiazide diuretic
- Estrogen for women who have gone through menopause
- Having surgery to remove the overactive glands (usually for people under age 50)
If you have symptoms or your calcium level is very high, you may need surgery to remove the parathyroid gland that is overproducing the hormone.
If you have hyperparathyroidism from a medical condition, your provider may prescribe vitamin D, if you have a low vitamin D level.
If hyperparathyroidism is caused by kidney failure, treatment may include:
- Extra calcium and vitamin D
- Avoiding phosphate in the diet
- The medicine cinacalcet (Sensipar)
- Dialysis or a kidney transplant
- Parathyroid surgery, if the parathyroid level becomes uncontrollably high
Outlook (Prognosis) for hyperparathyroidism
Outlook depends on the cause of hyperparathyroidism.
Possible Complications of hyperparathyroidism
Long-term problems that can occur when hyperparathyroidism is not well controlled include:
- Bones become weak, deformed, or can break
- High blood pressure and heart disease
- Kidney stones
- Long-term kidney disease
Parathyroid gland surgery can result in hypoparathyroidism and damage to the nerves that control the vocal cords.
What is Hypoparathyroidism
Hypoparathyroidism is a disorder in which the parathyroid glands in the neck do not produce enough parathyroid hormone (PTH) 4.
Causes of hypoparathyroidism
There are 4 tiny parathyroid glands in the neck, located near or attached to the back side of the thyroid gland.
The parathyroid glands help control calcium use and removal by the body. They do this by producing parathyroid hormone (PTH). PTH helps control calcium, phosphorus, and vitamin D levels in the blood and bone.
- Hypoparathyroidism occurs when the glands produce too little PTH. The blood calcium level falls, and the phosphorus level rises.
The most common cause of hypoparathyroidism is injury to the parathyroid glands during thyroid or neck surgery. It may also be caused by any of the following:
- Radioactive iodine treatment for hyperthyroidism
- Very low magnesium level in the blood
- Autoimmune attack on the parathyroid glands
DiGeorge syndrome is a childhood disease in which hypoparathyroidism occurs because all the parathyroid glands are missing at birth. This disease includes other health problems besides hypoparathyroidism.
Familial hypoparathyroidism occurs with other endocrine diseases such as adrenal insufficiency in a syndrome called type I polyglandular autoimmune syndrome (PGA I).
Symptoms of hypoparathyroidism
Symptoms may include any of the following:
- Abdominal pain
- Brittle nails
- Cataracts
- Calcium deposits in some tissues
- Decreased consciousness
- Dry hair
- Dry, scaly skin
- Muscle cramps
- Muscle spasms called tetany (can affect the larynx, causing breathing difficulties)
- Pain in the face, legs, and feet
- Painful menstruation
- Seizures
- Teeth that do not grow in on time, or at all
- Tingling lips, fingers, and toes
- Weakened tooth enamel (in children)
How is hypoparathyroidism diagnosed ?
The health care provider will do a physical exam and ask about symptoms.
Tests that will be done include:
- PTH blood test
- Calcium blood test
- Magnesium
- 24-hour urine test
Other tests that may be ordered include:
- ECG to check for an abnormal heart rhythm
- CT scan to check for calcium deposits in the brain
Treatment for hypoparathyroidism
The goal of treatment is to reduce symptoms and restore the calcium and mineral balance in the body.
- Treatment involves calcium carbonate and vitamin D supplements. These usually must be taken for life. Blood levels are measured regularly to make sure that the dose is correct. A high-calcium, low-phosphorous diet is recommended.
Injections of PTH may be recommended for some people. Your doctor can tell you if this medicine is right for you.
People who have life-threatening attacks of low calcium levels or prolonged muscle contractions are given calcium through a vein (IV). Precautions are taken to prevent seizures or larynx spasms. The heart is monitored for abnormal rhythms until the person is stable. When the life-threatening attack has been controlled, treatment continues with medicine taken by mouth.
Outlook (Prognosis) of hypoparathyroidism
The outcome is likely to be good if the diagnosis is made early. But changes in the teeth, cataracts, and brain calcifications cannot be reversed in children who have undiagnosed hypoparathyroidism during development.
Possible Complications of hypoparathyroidism
Hypoparathyroidism in children may lead to poor growth, abnormal teeth, and slow mental development.
Too much treatment with vitamin D and calcium can cause high blood calcium (hypercalcemia) or high urine calcium (hypercalciuria). Excess treatment may sometimes interfere with kidney function, or even cause kidney failure.
Hypoparathyroidism increases the risk of:
- Addison disease (only if the cause is autoimmune)
- Cataracts
- Parkinson disease
- Pernicious anemia (only if the cause is autoimmune)
When to see a Medical Professional
Call your provider if you develop any symptoms of hypoparathyroidism.
- Seizures or breathing problems are an emergency. Call your local emergency number right away.
Low blood calcium
Low blood calcium is much less common, particularly when caused by a parathyroid gland problem 2. There are some conditions that are present from birth and are quickly detected and treated immediately. The treatment must be lifelong! Gradually the body adapts to this lower calcium level and symptoms can be minimal even if you are not always faithful about taking your medicine. Forget to take it for too long and bad things happen starting with tingling around the lips and in the fingers and toes. If you don’t do anything about this you will likely develop severe painful cramps in your hand. This is known as tetany – it sounds like the infection tetanus, but it is not at all related. A more common cause of low blood calcium due to a parathyroid problem is seen in patients who have major neck operations for conditions such as throat or thyroid cancer. In order to remove as much as the cancer as possible from the neck, it is sometimes necessary to remove the parathyroid glands as well, even though they are not directly involved in the cancer. If not checked, this can cause a rapid drop in calcium and the development of tingling and cramps in the hands and feet. This does not happen often because the surgeon will be carefully monitoring your blood calcium if he or she has done extensive neck surgery. Making sure you get plenty of calcium by mouth and intravenously should always be done, and many times there is also treatment with the active vitamin D, calcitriol. Patients who are left with underactive parathyroids after such surgery do not really adapt well to this and are at much increased risk of having symptoms from their low calcium. The medicines cannot be skipped!
- Parathyroid gland removal. Medline Plus. https://medlineplus.gov/ency/article/002931.htm[↩]
- About the Parathyroid Glands. American Association of Clinical Endocrinologists. https://www.empoweryourhealth.org/endocrine-conditions/parathyroid[↩][↩][↩][↩]
- Hyperparathyroidism. Medline Plus. https://medlineplus.gov/ency/article/001215.htm[↩]
- Hypoparathyroidism. Medline Plus. https://medlineplus.gov/ency/article/000385.htm[↩]