Contents
- What is patent ductus arteriosus
What is patent ductus arteriosus
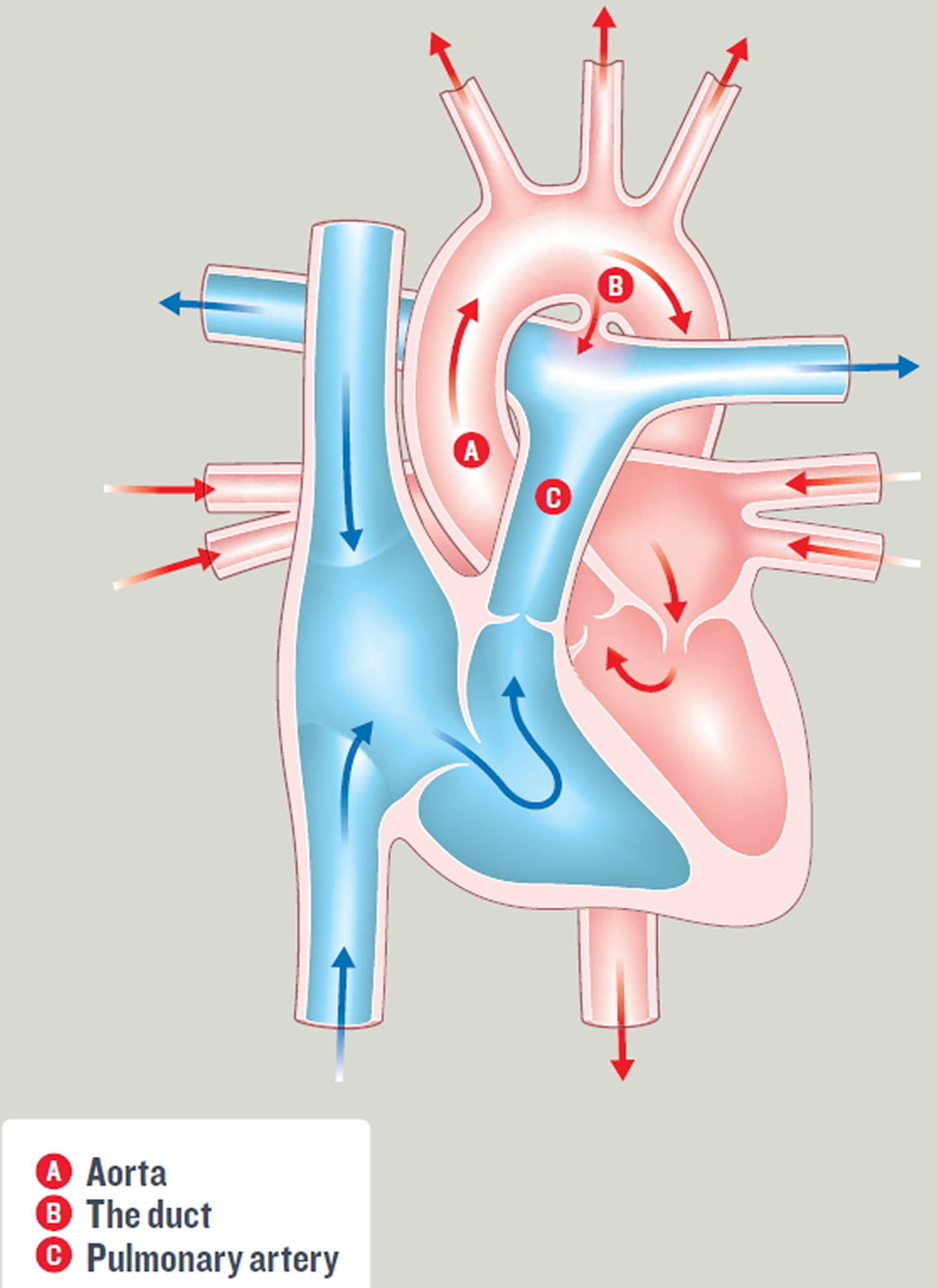
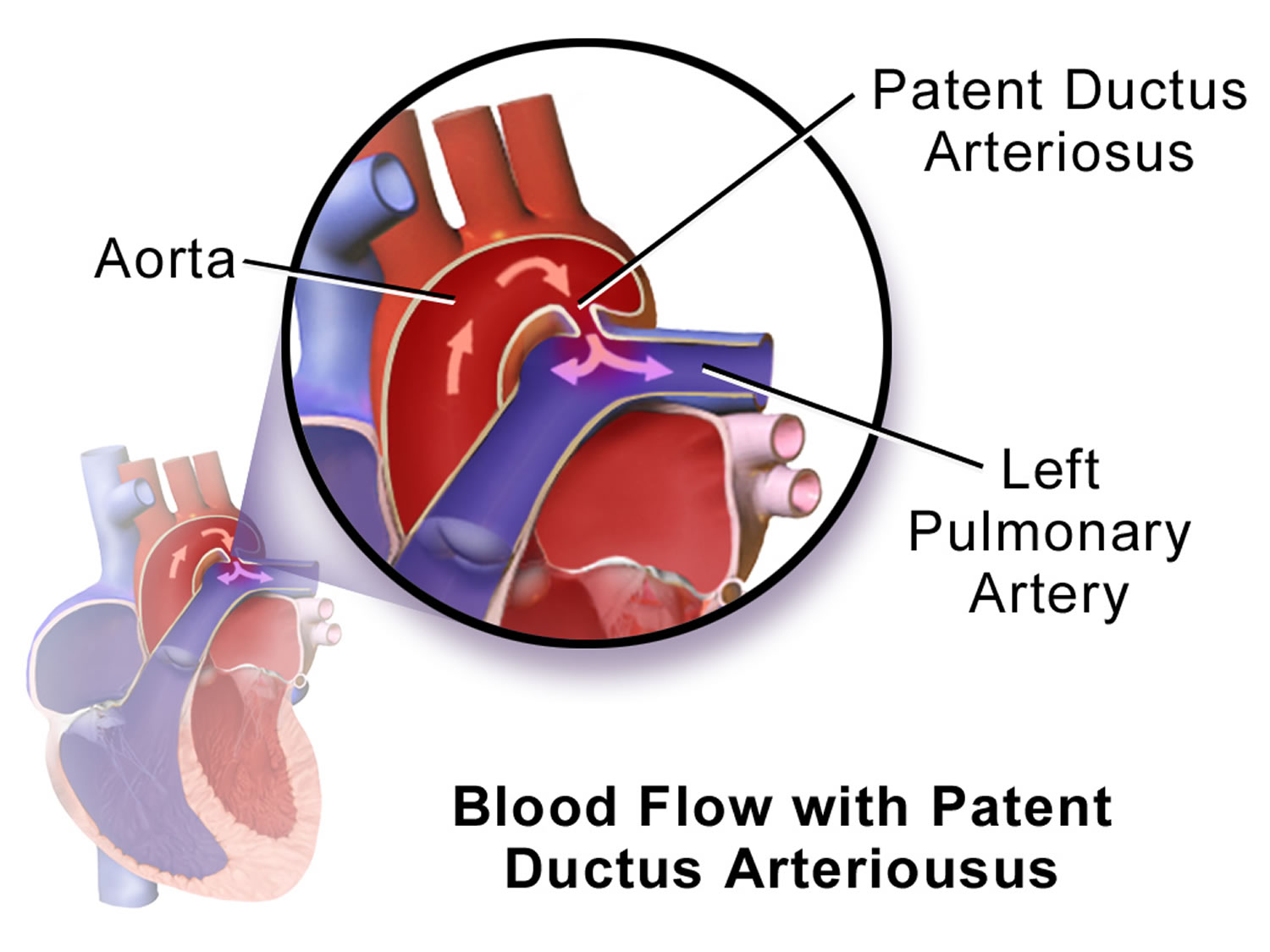
Patent ductus arteriosus (PDA) is a congenital heart problem that occurs soon after birth in some babies. A congenital heart defect is any type of heart problem that’s present at birth. The ductus arteriosus is a short blood vessel connecting the two main arteries of the babies heart – the aorta and the pulmonary artery (see Figure 3 below). In patent ductus arteriosus, abnormal blood flow occurs between two of the major arteries connected to the heart. Before a baby is born the duct (ductus arteriosus) allows blood to bypass their lungs. The ductus arteriosus (short blood vessel connecting the two main arteries of the babies heart – the aorta and the pulmonary artery) is an essential part of fetal blood circulation. After the baby is born and the lungs fill with air, the duct (ductus arteriosus) is no longer needed – it usually closes by itself as part of the normal changes occurring in the baby’s circulation within minutes or up to a few days after birth. Sometimes the duct (ductus arteriosus) fails to close by itself and remains open (patent). This is called patent ductus arteriosus or PDA. This opening allows oxygen-rich blood from the aorta to mix with oxygen-poor blood from the pulmonary artery. Patent ductus arteriosus causes too much blood to be delivered to the lungs. This can put strain on the heart and increase blood pressure in the lung arteries.
This may only cause mild symptoms in young children (such as breathlessness) but if left untreated over a period of many years patent ductus arteriosus can lead to permanent damage to the heart and lungs. This could become life-threatening as your child reaches adulthood, so it is important that large ducts are treated when your child is young and before any damage is caused.
If the ductus arteriosus is small there is a very small risk of damage. But there is is also a risk that a serious infection could occur inside the duct later in your child’s life, so it is recommended that even small ducts are closed.
Patent ductus arteriosus is a fairly common congenital heart defect in the United States. Although the condition can affect full-term infants, it’s more common in premature infants. On average, patent ductus arteriosus occurs in about 8 out of every 1,000 premature babies, compared with 2 out of every 1,000 full-term babies. Premature babies also are more vulnerable to the effects of patent ductus arteriosus.
Patent ductus arteriosus is twice as common in girls as it is in boys.
If your baby has a patent ductus arteriosus but an otherwise normal heart, the patent ductus arteriosus may shrink and go away. However, some children need treatment to close their patent ductus arteriosuss.
Some children who have patent ductus arteriosuss are given medicine to keep the ductus arteriosus open. For example, this may be done if a child is born with another heart defect that decreases blood flow to the lungs or the rest of the body. Keeping the patent ductus arteriosus open helps maintain blood flow and oxygen levels until doctors can do surgery to correct the other heart defect.
Doctors treat patent ductus arteriosus with medicines, catheter-based procedures, and surgery. Most children who have patent ductus arteriosus live healthy, normal lives after treatment.
What is the risk of having another child with a congenital heart condition?
If you have one child with a congenital heart condition, there is around a 1 in 40 chance that if you have another child, they will have a heart condition too 1. However, this risk may be higher (or lower) depending on the type of congenital heart condition your child has. Because your risk of having another child with congenital heart condition is higher than it is for other people, your doctor may offer you a special scan at an early stage in future pregnancies, to look at the baby’s heart.
How Human Heart Works
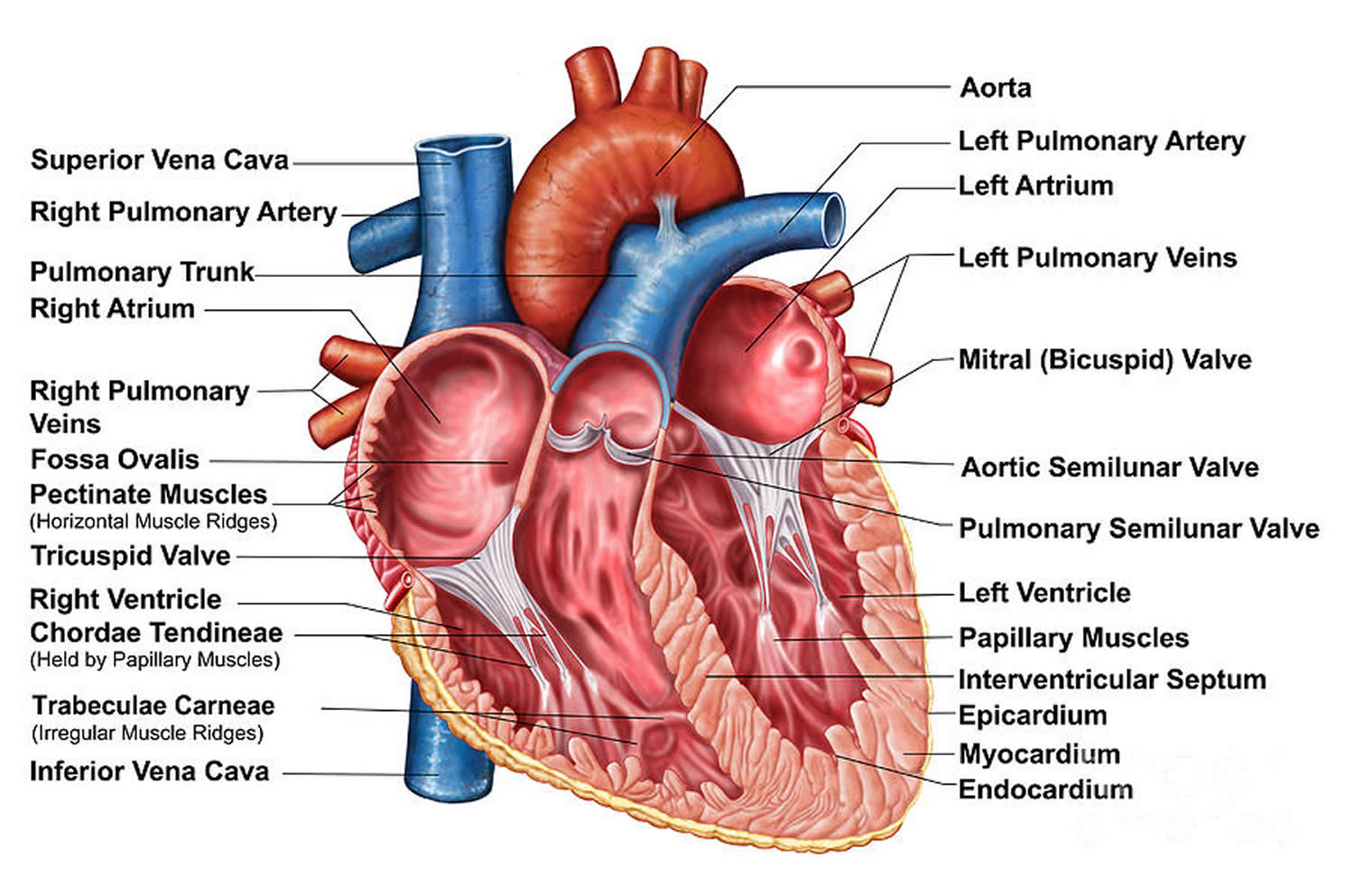
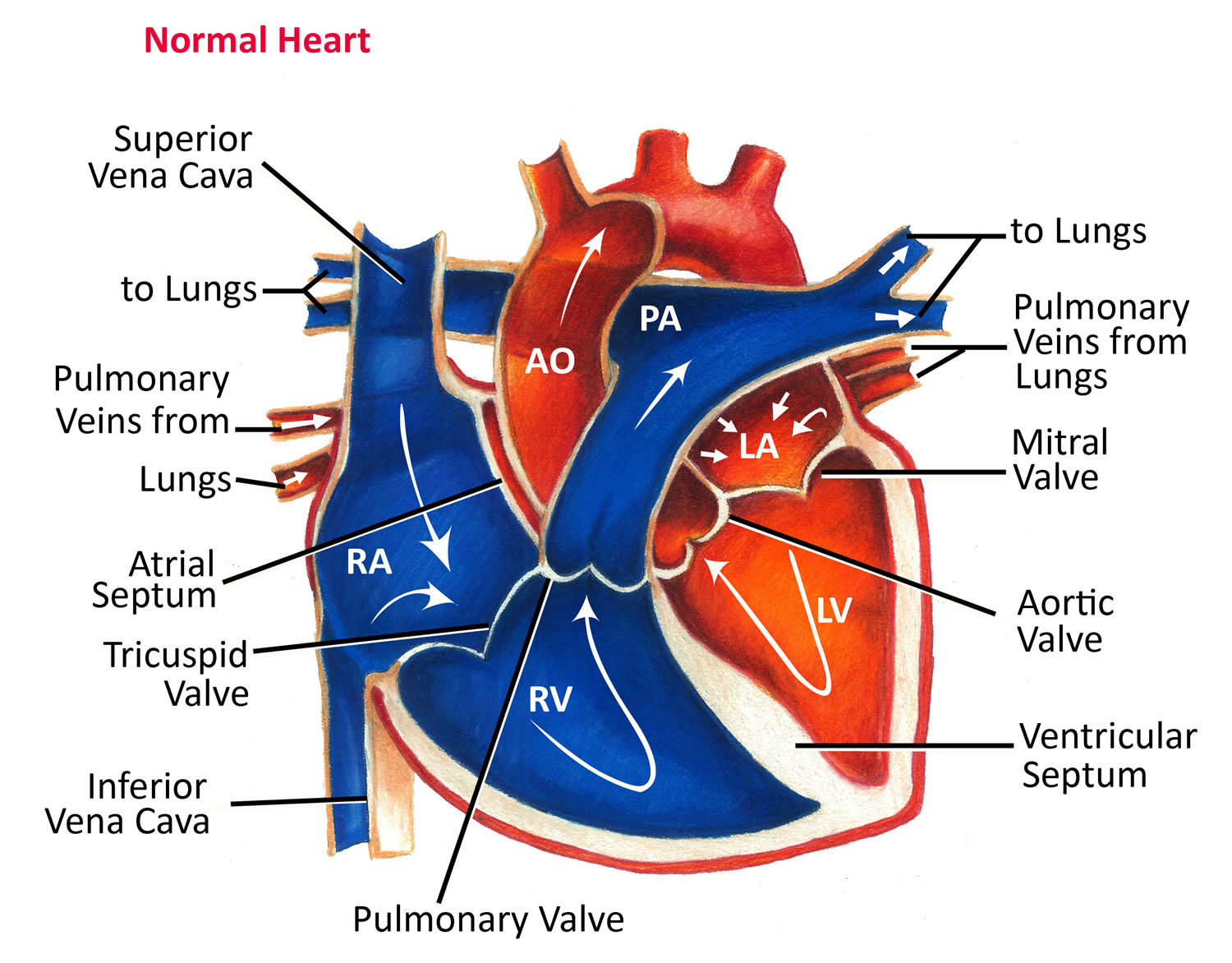
To understand patent ductus arteriosus, it helps to know how a normal heart works. Your child’s heart is a muscle about the size of his or her fist. It works like a pump and beats about 100,000 times a day.
The heart has two sides, separated by an inner wall called the septum. The right side of the heart pumps blood to the lungs to pick up oxygen. Then, oxygen-rich blood returns from the lungs to the left side of the heart, and the left side pumps it to the body.
The heart has four chambers and four valves and is connected to various blood vessels. Veins are the blood vessels that carry blood from the body to the heart. Arteries are the blood vessels that carry blood away from the heart to the body.
The heart has four chambers:
- The atria are the two upper chambers that collect blood as it flows into the heart.
- The ventricles are the two lower chambers that pump blood out of the heart to the lungs or other parts of the body.
Your heart has four heart valves to control the flow of blood from the atria to the ventricles and from the ventricles into the two large arteries connected to the heart.
- The tricuspid valve is in the right side of the heart, between the right atrium and the right ventricle.
- The pulmonary valve is in the right side of the heart, between the right ventricle and the entrance to the pulmonary artery. This artery carries blood from the heart to the lungs.
- The mitral valve is in the left side of the heart, between the left atrium and the left ventricle.
- The aortic valve is in the left side of the heart, between the left ventricle and the entrance to the aorta. This artery carries blood from the heart to the body.
Heart valves are like doors that open and close. They open to allow blood to flow through to the next chamber or to one of the arteries. Then they shut to keep blood from flowing backward.
When the heart’s valves open and close, they make a “lub-DUB” sound that a doctor can hear using a stethoscope.
- The first sound—the “lub”—is made by the mitral and tricuspid valves closing at the beginning of systole. Systole is when the ventricles contract, or squeeze, and pump blood out of the heart.
- The second sound—the “DUB”—is made by the aortic and pulmonary valves closing at the beginning of diastole. Diastole is when the ventricles relax and fill with blood pumped into them by the atria.
The arteries are major blood vessels connected to your heart
- The pulmonary artery carries blood from the right side of the heart to the lungs to pick up a fresh supply of oxygen.
- The aorta is the main artery that carries oxygen-rich blood from the left side of the heart to the body.
- The coronary arteries are the other important arteries attached to the heart. They carry oxygen-rich blood from the aorta to the heart muscle, which must have its own blood supply to function.
The veins also are major blood vessels connected to your heart
- The pulmonary veins carry oxygen-rich blood from the lungs to the left side of the heart so it can be pumped to the body.
- The superior and inferior vena cavae are large veins that carry oxygen-poor blood from the body back to the heart.
The ductus arteriosus is a blood vessel that connects the aorta and pulmonary artery in unborn babies. This vessel allows blood to be pumped from the right side of the heart into the aorta, without stopping at the lungs for oxygen.
While a baby is in the womb, only a small amount of his or her blood needs to go to the lungs. This is because the baby gets oxygen from the mother’s bloodstream.
After birth, the baby no longer is connected to the mother’s bloodstream. Thus, the baby’s blood must travel to his or her own lungs to get oxygen. As the baby begins to breathe on his or her own, the pulmonary artery opens to allow blood into the lungs. Normally, the ductus arteriosus closes because the infant no longer needs it.
Once the ductus arteriosus closes, blood leaving the right side of the heart no longer goes into the aorta. Instead, the blood travels through the pulmonary artery to the lungs. There, the blood picks up oxygen. The oxygen-rich blood returns to the left side of the heart and is pumped to the rest of the body.
Sometimes the ductus arteriosus remains open (patent) after birth. A patent ductus arteriosus allows blood to flow from the aorta into the pulmonary artery and to the lungs. The extra blood flowing into the lungs strains the heart. It also increases blood pressure in the lung’s arteries.
Figure 1. The anatomy of the heart chambers
Figure 2. Normal heart blood flow
Figure 3. Patent ductus arteriosus – (Heart with patent ductus arteriosus. The duct (ductus arteriosus) [B] connects the aorta with the pulmonary artery. This allows oxygen-rich blood from the aorta to mix with oxygen-poor blood in the pulmonary artery.)
Effects of Patent Ductus Arteriosus
Full-term infants
A small patent ductus arteriosus might not cause any problems, but a large patent ductus arteriosus likely will cause problems. The larger the patent ductus arteriosus, the greater the amount of extra blood that passes through the lungs.
A large patent ductus arteriosus that remains open for an extended time can cause the heart to enlarge, forcing it to work harder. Also, fluid can build up in the lungs.
A patent ductus arteriosus can slightly increase the risk of infective endocarditis. Infective endocarditis is an infection of the inner lining of the heart chambers and valves.
In patent ductus arteriosus, increased blood flow can irritate the lining of the pulmonary artery, where the ductus arteriosus connects. This irritation makes it easier for bacteria in the bloodstream to collect and grow, which can lead to infective endocarditis.
Premature infants
Patent ductus arteriosus can be more serious in premature infants than in full-term infants. Premature babies are more likely to have lung damage from the extra blood flowing from the patent ductus arteriosus into the lungs. These infants may need to be put on ventilators. Ventilators are machines that support breathing.
Increased blood flow through the lungs also can reduce blood flow to the rest of the body. This can damage other organs, especially the intestines and kidneys.
If it is difficult to wean premature baby off the life support machine, your doctor will usually recommend using medication to try and close the patent ductus arteriosus. If this fails, or if medication is not considered appropriate, your child will need to have an operation to close the patent ductus arteriosus.
Sadly, there is a higher risk of premature babies with patent ductus arteriosus passing away shortly after birth, compared to babies with patent ductus arteriosus who were not born premature. This is rarely as a direct result of patent ductus arteriosus or its treatment, and may be caused by other problems related to their prematurity.
Patent ductus arteriosus in adults
If the patent ductus arteriosus is small, it doesn’t have to be closed because it doesn’t make the heart and lungs work harder.
Patients with a moderate- or large-sized patent ductus arteriosus may develop problems related to the increased blood flow to the lungs. These patients may have improvement if the patent ductus arteriosus is closed. Closing the patent ductus arteriosus can now usually be performed by catheter coil placement or other device insertion to plug the abnormal communication (referred to as interventional or therapeutic catheterization.)
Surgery may be the best treatment option for some patients. The surgeon doesn’t have to open the heart to fix the patent ductus arteriosus. An incision is made in the left side of the chest, between the ribs. The patent ductus arteriosus is closed by tying it with suture (thread-like material) or by permanently placing a small metal clip around the patent ductus arteriosus to squeeze it closed. Occasionally in the adult, a surgical patch is used. If there’s no other heart defect, this restores the circulation to normal. The long-term outlook is excellent, and usually no medicines and no additional surgery or catheterization are needed.
If the patent ductus arteriosus is small, or if the patent ductus arteriosus has been closed with catheterization or surgery, you may not need any special restrictions and may be able to participate in normal activities without increased risk.
Patients with moderate or large patent ductus arteriosuss and patients with pulmonary hypertension may need to restrict activity. They should discuss this with their cardiologist.
Medical Follow-up
Patients with a small patent ductus arteriosus need periodic follow-up with a cardiologist. Patients with a patent ductus arteriosus that’s been successfully closed rarely require long-term cardiology follow-up unless there’s additional cardiac disease. Only rarely will they need to take medicine after surgical or device closure. Your cardiologist can monitor you with noninvasive tests if needed.
Activity Restrictions
Most patients with a small unrepaired patent ductus arteriosus or a repaired patent ductus arteriosus don’t need any special precautions and can participate in normal activities without increased risk. After surgery or catheter closure, your cardiologist may advise some limitations on your physical activity for a short time even if there’s no pulmonary hypertension.
Exercise restriction is recommended for patients with pulmonary hypertension related to patent ductus arteriosus.
Endocarditis Prevention
Endocarditis prophylaxis is generally not needed more than six months after patent ductus arteriosus device closure. However, endocarditis prophylaxis is recommended for patent ductus arteriosus patients with a history of endocarditis, for those with prosthetic valve material and for unrepaired patent ductus arteriosus with associated pulmonary hypertension and cyanosis.
Pregnancy
Unless there’s pulmonary hypertension or signs of heart failure, pregnancy is low risk in patients with patent ductus arteriosus.
Patent ductus arteriosus complications
A small patent ductus arteriosus might not cause complications. Larger, untreated defects could cause:
- High blood pressure in the lungs (pulmonary hypertension). Too much blood circulating through the heart’s main arteries through a patent ductus arteriosus can lead to pulmonary hypertension, which can cause permanent lung damage. A large patent ductus arteriosus can lead to Eisenmenger syndrome, an irreversible type of pulmonary hypertension.
- Heart failure. A patent ductus arteriosus can eventually cause the heart to enlarge and weaken, leading to heart failure, a chronic condition in which the heart can’t pump effectively.
- Heart infection (infective endocarditis). People who have structural heart problems, such as a patent ductus arteriosus, are at a higher risk of an inflammation of the heart’s inner lining (infectious endocarditis) than are people who have healthy hearts.
Patent ductus arteriosus and pregnancy
Most women who have a small patent ductus arteriosus can tolerate pregnancy without problems. However, having a larger defect or complications — such as heart failure, arrhythmias or pulmonary hypertension — can increase the risk of complications during pregnancy. If you have Eisenmenger syndrome, pregnancy should be avoided as it can be life-threatening.
If you have a heart defect, repaired or not, discuss family planning with your doctor. In some cases, preconception consultations with doctors who specialize in congenital cardiology, genetics and high-risk obstetric care are needed. Some heart medications can cause serious problems for a developing baby, and it might be necessary to stop or adjust the medications before you become pregnant.
Patent ductus arteriosus causes
The cause of patent ductus arteriosus isn’t known. Genetics may play a role in causing the condition. A defect in one or more genes might prevent the ductus arteriosus from closing after birth.
Risk Factors for patent ductus arteriosus
Patent ductus arteriosus is a relatively common congenital heart defect in the United States.
The condition occurs more often in premature infants (on average, occurring in about 8 of every 1,000 births). However, patent ductus arteriosus also occurs in full-term infants (on average, occurring in about 2 of every 1,000 births).
Patent ductus arteriosus also is more common in:
- Being female. Patent ductus arteriosus is twice as common in girls as it is in boys.
- Family history and other genetic conditions. A family history of heart defects and other genetic conditions, such as Down syndrome, increase the risk of having a patent ductus arteriosus.
- Infants whose mothers had German measles (rubella) during pregnancy.
- Being born at a high altitude. Babies born above 10,000 feet (3,048 meters) have a greater risk of a patent ductus arteriosus than babies born at lower altitudes.
Patent ductus arteriosus prevention
There’s no sure way to prevent having a baby with a patent ductus arteriosus. However, it’s important to do everything possible to have a healthy pregnancy. Here are some of the basics:
- Seek early prenatal care, even before you’re pregnant. Quitting smoking, reducing stress, stopping birth control — these are all things to talk to your doctor about before you get pregnant. Also discuss medications you’re taking.
- Eat a healthy diet. Include a vitamin supplement that contains folic acid.
- Exercise regularly. Work with your doctor to develop an exercise plan that’s right for you.
- Avoid risks. These include harmful substances such as alcohol, cigarettes and illegal drugs. Also avoid hot tubs and saunas.
- Avoid infections. Update your vaccinations before becoming pregnant. Certain types of infections can be harmful to a developing baby.
- Keep diabetes under control. If you have diabetes, work with your doctor to manage the condition before and during pregnancy.
If you have a family history of heart defects or other genetic disorders, consider talking with a genetic counselor before becoming pregnant.
Patent ductus arteriosus symptoms
Patent ductus arteriosus symptoms vary with the size of the defect and whether the baby is full term or premature.
Because babies and young children often don’t show any symptoms, patent ductus arteriosus may not be found until they are older. It’s not unusual for patent ductus arteriosus to be diagnosed in older children, teenagers or even in adults.
A heart murmur may be the only sign that a baby has patent ductus arteriosus. A heart murmur is an extra or unusual sound heard during the heartbeat. Heart murmurs also have other causes besides patent ductus arteriosus, and most murmurs are harmless.
Some infants may develop signs or symptoms of volume overload on the heart and excess blood flow in the lungs.
Signs and symptoms may include:
- Fast breathing, working hard to breathe, or shortness of breath. Premature infants may need increased oxygen or help breathing from a ventilator.
- Poor feeding and poor weight gain.
- Tiring easily.
- Sweating with exertion, such as while feeding.
Patent ductus arteriosus diagnosis
In full-term infants, patent ductus arteriosus usually is first suspected when the baby’s doctor hears a heart murmur during a regular checkup.
A heart murmur is an extra or unusual sound heard during the heartbeat. Heart murmurs also have other causes besides patent ductus arteriosus, and most murmurs are harmless.
If a patent ductus arteriosus is large, the infant also may develop symptoms of volume overload and increased blood flow to the lungs. If a patent ductus arteriosus is small, it may not be diagnosed until later in childhood.
If your child’s doctor thinks your child has patent ductus arteriosus, he or she may refer you to a pediatric cardiologist. This is a doctor who specializes in diagnosing and treating heart problems in children.
Premature babies who have patent ductus arteriosus may not have the same signs as full-term babies, such as heart murmurs. Doctors may suspect patent ductus arteriosus in premature babies who develop breathing problems soon after birth. Tests can help confirm a diagnosis.
Diagnostic Tests
Echocardiography
Echocardiography (echo) is a painless test that uses sound waves to create a moving picture of your baby’s heart. During echo, the sound waves bounce off your child’s heart. A computer converts the sound waves into pictures of the heart’s structures.
The test allows the doctor to clearly see any problems with the way the heart is formed or the way it’s working. Echo is the most important test available to your baby’s cardiologist to both diagnose a heart problem and follow the problem over time.
In babies who have patent ductus arteriosus, echo shows how big the patent ductus arteriosus is and how well the heart is responding to it. When medical treatments are used to try to close a patent ductus arteriosus, echo is used to see how well the treatments are working.
EKG (Electrocardiogram)
An EKG (ECG) is a simple, painless test that records the heart’s electrical activity. For babies who have patent ductus arteriosus, an EKG (ECG) can show whether the heart is enlarged. The test also can show other subtle changes that can suggest the presence of a patent ductus arteriosus.
Chest X-ray
An X-ray image helps the doctor see the condition of your or your baby’s heart and lungs. An X-ray might reveal conditions other than a heart defect, as well.
Cardiac catheterization
This test isn’t usually necessary for diagnosing a patent ductus arteriosus alone, but it might be done to examine other congenital heart defects found during an echocardiogram or if a catheter procedure is being considered to treat a patent ductus arteriosus. A thin, flexible tube (catheter) is inserted into a blood vessel at your or your child’s groin or arm and guided through it into the heart. Through catheterization, the doctor may be able to do procedures to close the patent ductus arteriosus.
Patent ductus arteriosus treatment
Patent ductus arteriosus (patent ductus arteriosus) is treated with medicines, catheter-based procedures, and surgery. The goal of treatment is to close the patent ductus arteriosus. Closure will help prevent complications and reverse the effects of increased blood volume.
Small patent ductus arteriosuss often close without treatment. For full-term infants, treatment is needed if the patent ductus arteriosus is large or causing health problems. For premature infants, treatment is needed if the patent ductus arteriosus is causing breathing problems or heart problems.
Talk with your child’s doctor about treatment options and how your family prefers to handle treatment decisions.
Medicines
Your child’s doctor may prescribe medicines to help close your child’s patent ductus arteriosus.
Indomethacin is a medicine that helps close patent ductus arteriosuss in premature infants. This medicine triggers the patent ductus arteriosus to constrict or tighten, which closes the opening. Indomethacin usually doesn’t work in full-term infants.
Ibuprofen also is used to close patent ductus arteriosuss in premature infants. This medicine is similar to indomethacin.
Catheter-Based Procedures
Catheters are thin, flexible tubes that doctors use as part of a procedure called cardiac catheterization. Catheter-based procedures often are used to close patent ductus arteriosuss in infants or children who are large enough to have the procedure.
Your child’s doctor may refer to the procedure as “transcatheter device closure.” The procedure sometimes is used for small patent ductus arteriosuss to prevent the risk of infective endocarditis. Infective endocarditis is an infection of the inner lining of the heart chambers and valves.
Your child will be given medicine to help him or her relax or sleep during the procedure. The doctor will insert a catheter in a large blood vessel in the groin (upper thigh). He or she will then guide the catheter to your child’s heart.
A small metal coil or other blocking device (shaped like a tiny cork) is passed through the catheter and placed in the patent ductus arteriosus. This device blocks blood flow through the vessel.
Catheter-based procedures don’t require the child’s chest to be opened. They also allow the child to recover quickly.
These procedures often are done on an outpatient basis. You’ll most likely be able to take your child home the same day the procedure is done.
The patent ductus arteriosus does not always close completely as soon as the coil or plug is inserted. Sometimes it takes a few weeks for the body’s own tissue to grow around it as part of the healing process and seal it completely. Your child will be able to return to normal activities within a few days. They will need to attend the outpatient department a few weeks later for a check-up.
Complications from catheter-based procedures are rare and short term. They can include bleeding and infection. There is a very small risk that the closure device
may move out of position. If your child has a steel coil this is not usually serious – it is often possible to remove it using a keyhole technique and to put a larger coil in. If your child has a plug, and it moves out of position, a bigger operation may be needed to remove it.
There is also a small risk that the closure device will not completely close the patent ductus arteriosus. If there is only a very small space left around the device it may heal up on its own, but if not it is can be necessary to have further surgery one or two years later.
There is a very small risk that the device may become infected. Unfortunately, this is a very serious complication and would almost certainly require open-heart surgery to remove the device.
Patent ductus arteriosus surgery
Most patent ductus arteriosus are small (only a couple of millimeters or so wide) and can be safely closed using a ‘keyhole’ treatment. If your child has a larger duct they may need open-heart surgery.
Surgery to correct a patent ductus arteriosus may be done if:
- A premature or full-term infant has health problems due to a patent ductus arteriosus and is too small to have a catheter-based procedure
- A catheter-based procedure doesn’t successfully close the patent ductus arteriosus
- Surgery is planned for treatment of related congenital heart defects
Often, surgery isn’t done until after 6 months of age in infants who don’t have health problems from their patent ductus arteriosuss. Doctors sometimes do surgery on small patent ductus arteriosuss to prevent the risk of infective endocarditis.
For the surgery, your child will be given medicine so that he or she will sleep and not feel any pain. The surgeon will make a small incision (cut) between your child’s ribs to reach the patent ductus arteriosus. He or she will close the patent ductus arteriosus using stitches or clips.
Complications from surgery are rare and usually short term. They can include hoarseness, a paralyzed diaphragm (the muscle below the lungs), infection, bleeding, or fluid buildup around the lungs.
Open-heart surgery for patent ductus arteriosus
If your child has a larger patent ductus arteriosus they may need open-heart surgery. If your baby has this surgery, they will be given a general anesthetic. The
surgeon will make a cut in their chest to get access to their heart. They will then will tie the duct to close it, and your child’s chest will be stitched closed. Your child will need to stay in hospital for a few days following the operation, and then return to the outpatient’s department a few weeks later for a check-up. Most children return to normal activities a few weeks after surgery. Your child will have a scar along the side of their chest afterwards.
What are the risks of open-heart surgery?
The good news is open-heart surgery to close a patent ductus arteriosus is usually very successful and carries a very low risk of fatality. The majority of children survive the surgery without any major complications.
There is a small risk that the patent ductus arteriosus may not completely close, even after surgery. If this is the case it is almost always possible to complete further treatment using the keyhole method, rather than a second open-heart surgery.
After Surgery
After surgery, your child will spend a few days in the hospital. He or she will be given medicine to reduce pain and anxiety. Most children go home 2 days after surgery. Premature infants usually have to stay in the hospital longer because of their other health issues.
The doctors and nurses at the hospital will teach you how to care for your child at home. They will talk to you about:
- Limits on activity for your child while he or she recovers
- Followup appointments with your child’s doctors
- How to give your child medicines at home, if needed
When your child goes home after surgery, you can expect that he or she will feel fairly comfortable. However, you child may have some short-term pain.
Your child should begin to eat better and gain weight quickly. Within a few weeks, he or she should fully recover and be able to take part in normal activities.
Long-term complications from surgery are rare. However, they can include narrowing of the aorta, incomplete closure of the patent ductus arteriosus, and reopening of the patent ductus arteriosus.
Living with patent ductus arteriosus
Most children who have patent ductus arteriosuss live healthy, normal lives after treatment. Full-term infants will likely have normal activity levels, appetite, and growth after patent ductus arteriosus treatment, unless they had other congenital heart defects.
If you or your child has a congenital heart defect or has had surgery to correct one, you might have some concerns about aftercare. Here are some issues you might be thinking about:
- Preventing infection. For most people who have a patent ductus arteriosus, regularly brushing and flossing teeth and regular dental checkups are the best ways to help prevent infection.
- Exercising and play. People and parents of children who have congenital heart defects often worry about the risks of vigorous activity and rough play, even after successful treatment. Although some children and adults might need to limit the amount or type of exercise, most people who have patent ductus arteriosus will lead normal lives. Your or your child’s doctor can advise you about which activities are safe.
For premature infants, the outlook after patent ductus arteriosus treatment depends on other factors, such as:
- How early the child was born
- Whether the child has other illnesses or conditions, such as other congenital heart defects
Ongoing Care
Children who have patent ductus arteriosuss are at slightly increased risk for infective endocarditis. Infective endocarditis is an infection of the inner lining of the heart chambers and valves.
Your child’s doctor will tell you whether your child needs antibiotics before certain medical procedures to help prevent infective endocarditis. According to the most recent American Heart Association guidelines, most children who have patent ductus arteriosuss don’t need antibiotics.
Today, antibiotics before dental procedures are only recommended for patients with the highest risk of infective endocarditis, those who have 2:
- A prosthetic heart valve or who have had a heart valve repaired with prosthetic material.
- A history of endocarditis.
- A heart transplant with abnormal heart valve function
- Certain congenital heart defects including:
- Cyanotic congenital heart disease (birth defects with oxygen levels lower than normal), that has not been fully repaired, including children who have had a surgical shunts and conduits.
- A congenital heart defect that’s been completely repaired with prosthetic material or a device for the first six months after the repair procedure. †
- Repaired congenital heart disease with residual defects, such as persisting leaks or abnormal flow at or adjacent to a prosthetic patch or prosthetic device.
Note: † Prophylaxis is reasonable because endothelialization of prosthetic material occurs within six months after the procedure.
Additionally, taking antibiotics just to prevent endocarditis is not recommended for patients who have procedures involving the reproductive, urinary or gastrointestinal tracts.
- Gill HR, Splitt M, Sharland GK, Simpson JM. 2003. Patterns of recurrence of congenital heart disease: An analysis of 6,640 consecutive pregnancies evaluated by detailed fetal echocardiography. Journal of the American College of Cardiology; 42: 923-9.[↩]
- Infective Endocarditis. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/TheImpactofCongenitalHeartDefects/Infective-Endocarditis_UCM_307108_Article.jsp[↩]