Contents
What is pedialyte
Pedialyte is an oral rehydration solution that is used to add back fluid after fluid loss or to help prevent fluid and electrolyte problems. Pedialyte is a medical-grade hydration solution specially formulated with the optimal balance of sugar and electrolytes needed to help replenish vital fluids, minerals, and nutrients, which, when lost, can lead to dehydration 1. Pedialyte (oral rehydration solution) main purpose is to rehydrate your body from all sorts of dehydration causes. Both adults and kids can use Pedialyte for rehydration. Rehydrating with Pedialyte helps everyone with dehydration due to diarrhea and vomiting—adults and kids to feel better fast. For example, most people will experience diarrhea — loose watery stools — at some time in their life. Most people do not need any specific treatment for infectious diarrhea as it usually improves on its own in a couple of days. However, it is important to drink plenty of liquids to keep well hydrated. This is especially important for children and babies. Dehydration happens when you haven’t got enough fluids in your body. Dehydration means your body loses more fluids than you take in. If it isn’t treated it can get worse and become a serious problem. If severe, dehydration can cause serious problems.
Children under 5s should get plenty of fluids to avoid dehydration. It’s quite common for young children to become dehydrated. It can be serious if it’s not dealt with quickly. The body needs to have enough fluid to be able to function at its best. Children are at risk of dehydration, especially in hot weather and when they are exercising. By the time they feel thirsty, they are probably already dehydrated – so it’s up to parents and carers to make sure they are drinking enough.
What does your child need to stay well hydrated?
- Water is the best choice for children.
- Avoid sports drinks, fruit juices, soft drinks and flavoured mineral waters since they all contain sugar, which can lead to tooth decay.
The recommended daily intake of water for children is:
- 5 to 8 years old: 5 glasses (1 liter)
- 9 to 12 years old: 7 glasses (1.5 liters)
- 13 years old and over: 8 to 10 glasses (2 liters).
Children need even more water when they are exercising. Your child should drink before, during and after physical activity – even if they aren’t thirsty.
Tips to help your child stay hydrated
- make sure they always pack a water bottle
- choose water rather than sugary drinks
- remind them to drink before a sports game
- encourage them to have a few mouthfuls of water during any breaks in the game
- make sure they have a big drink afterwards to make up for any sweat they have lost.
Mild dehydration can be treated by giving your child more to drink. But serious dehydration – for example, if they are unwell – can be very serious. It’s important to know what to look out for.
How does pedialyte work?
Oral rehydration solutions like Pedialyte are specifically designed fluids that contain an appropriate amount of sodium, glucose and other electrolytes and are of the appropriate osmolality, to maximize water absorption from the gut. They use the principle of glucose-facilitated sodium transport whereby glucose enhances sodium and secondarily water transport across the mucosa of the upper intestine 2. The sodium and glucose concentrations and the osmolality are of vital importance.
The World Health Organisation (WHO) recommends an oral rehydration solution that has a sodium concentration of 60-90mmol/L 3.
The total substance concentration (including that contributed by glucose) should be within the range of 200-310 mmol/l.
Table 1. World Health Organisation (WHO) recommends an oral rehydration solution
| Glucose | should at least equal that of sodium but should not exceed 111 mmol/l |
| Sodium | should be within the range of 60-90 mEq/l |
| Potassium | should be within the range of 15-25 mEq/l |
| Citrate | should be within the range of 8-12 mmol/l |
| Chloride | should be within the range of 50-80 mEq/l |
New formula oral rehydration salts
A new formula for oral rehydration salts (ORS), has been released by the World Health Organization 3. The new formula oral rehydration salts (ORS), a sodium and glucose solution is widely used to treat children with acute diarrhea.
The new improved formula is the result of extensive research sponsored by WHO’s Department of Child and Adolescent Health and Development and supported by the United States Agency for International Development (USAID). The latest study was conducted in five developing countries among children from one month to two years old with acute diarrhoea and dehydration.
The study’s findings suggest that using the low-sodium, low-glucose ORS formulation reduces the need for intravenous fluids by 33 percent. The effect of this reduction could result in fewer children requiring hospitalization, fewer secondary infections, a diminished need to handle blood with its potentially dangerous consequences, and lower health care costs.
For the past 20 years, numerous studies have been undertaken to develop an “improved” oral rehydration solution. The goal was a product that would be at least as safe and effective as standard oral rehydration solution for preventing or treating dehydration from all types of diarrhoea but which, in addition, would reduce stool output or have other important clinical benefits. One approach has consisted in reducing the osmolarity of oral rehydration salts (ORS) solution to avoid possible adverse effects of hypertonicity on net fluid absorption. This was done by reducing the solution’s glucose and salt (NaCl) concentrations.
Studies to evaluate this approach were reviewed at a consultative technical meeting held in New York and technical recommendations were made to WHO and UNICEF on the efficacy and safety of reduced osmolarity oral rehydration salts (ORS) in children with acute non-cholera diarrhoea, and in adults and children with cholera.
These studies showed that the efficacy of oral rehydration salts (ORS) solution for treatment of children with acute non-cholera diarrhoea is improved by reducing its sodium concentration to 75 mEq/l, its glucose concentration to 75 mmol/l, and its total osmolarity to 245 mOsm/l. The need for unscheduled supplemental IV therapy in children given this solution was reduced by 33%. In a combined analysis of this study and studies with other reduced osmolar-ity Oral rehydration solution solutions (osmolarity 210-268 mOsm/l, sodium 50-75 mEq/l) stool output was also reduced by about 20% and the incidence of vomiting by about 30%. The 245 mOsm/l solution also appeared to be as safe and at least as effective as standard oral rehydration salts (ORS) for use in children with cholera.
Table 2. World Health Organisation (WHO) New formula oral rehydration salts
| Reduced osmolarity ORS | grams/litre | Reduced osmolarity ORS | mmol/litre |
| Sodium chloride | 2.6 | Sodium | 75 |
| Glucose, anhydrous | 13.5 | Chloride | 65 |
| Potassium chloride | 1.5 | Glucose, anhydrous | 75 |
| Trisodium citrate | Potassium | 20 | |
| dihydrate | 2.9 | Citrate | 10 |
| Total Osmolarity | 245 |
Note: ORS = oral rehydration salts
[Source: World Health Organisation (WHO) 3]In developed countries with non-cholera diarrhoea, it is generally thought that 90mmol/L is a little high, as non-cholera gastroenteritis does not result in the same sodium losses that are seen in cholera. Many different oral rehydration solutions with varying sodium concentrations have been developed. It has been shown 4 that water absorption across the lumen of the human intestine is maximal using solutions with a sodium concentration of 60mmol/L (such as Gastrolyte) and this is the concentration recommended by the European Society of Paediatric Gastroenterology and Nutrition 5. However some children who are not particularly dehydrated will refuse to drink such an oral rehydration solution because of its salty taste. Oral rehydration solutions with slightly less sodium such as Hydralyte may be more palatable, particularly as this comes in an iceblock form. Oral rehydration solutions with similar compositions to Hydralyte are safe and effective. These hypo-osmolar solutions (such as Gastrolyte and Hydralyte) are more effective at promoting water absorption than isotonic or hypertonic solutions 6.
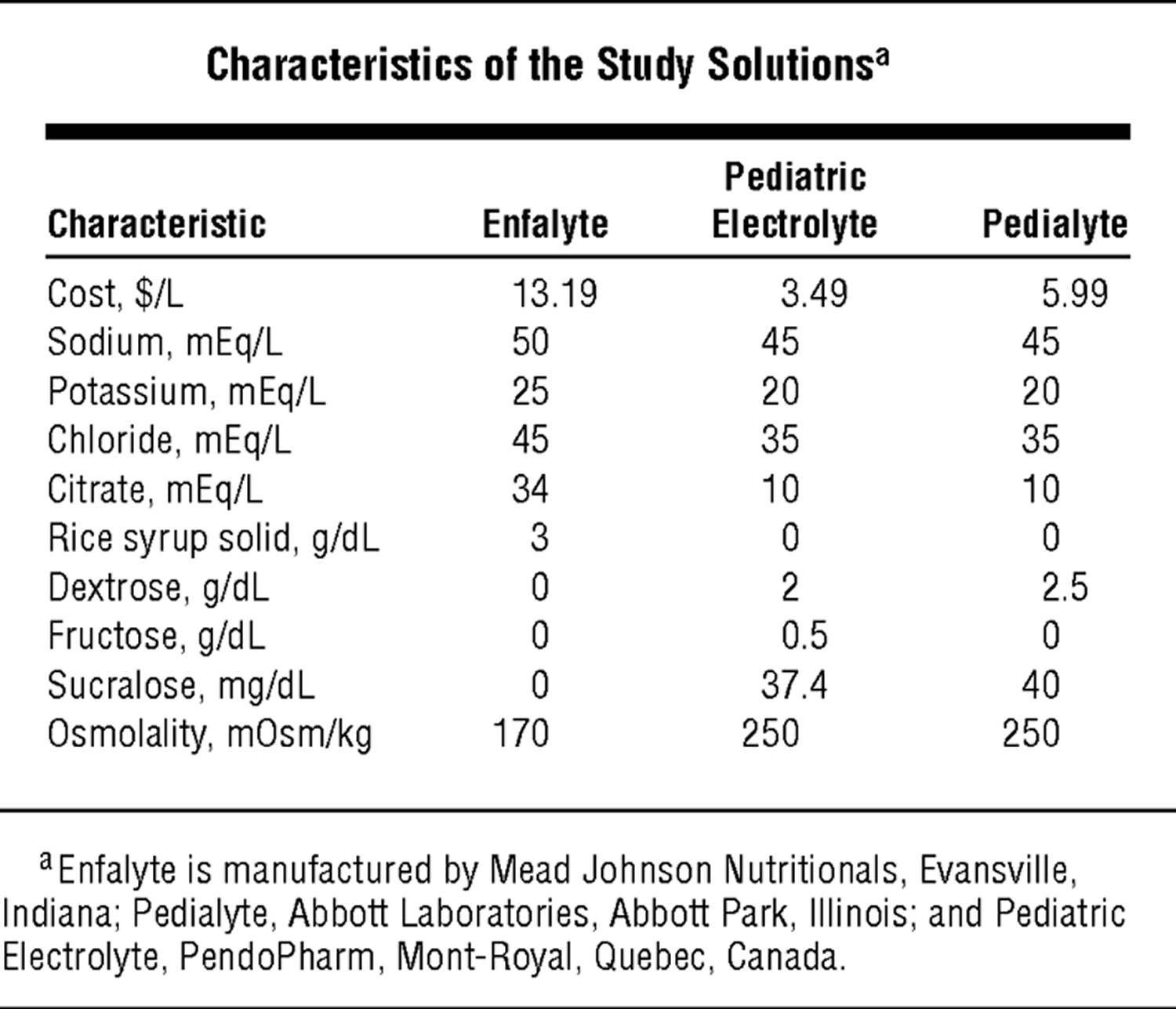
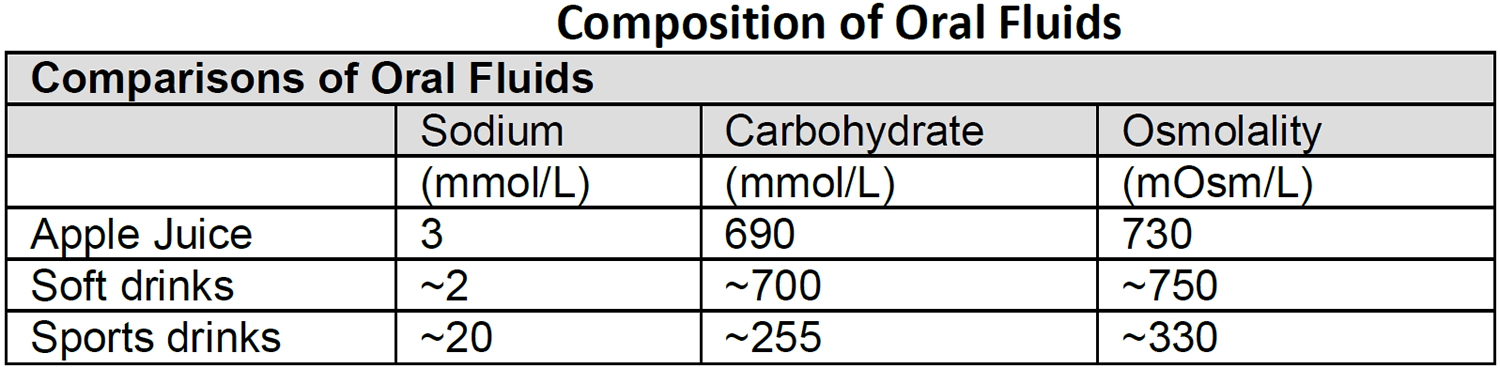
The composition of various oral rehydration solutions and other fluids is shown in Tables 3 and 4. Fruit juices and soft drinks are inappropriate because of the minimal sodium content and the excessive glucose content and hence excessive osmolality, which will worsen diarrhea. Although diluting juices and soft drinks reduces glucose concentration, the fluid has insufficient sodium to act as a rehydration fluid. Sports drinks have varying sodium and carbohydrate levels, and are considered inappropriate as rehydration solutions.
Table 3. Composition of Oral Rehydration Solutions
[Source 7]Table 4. Composition of Oral Fluids
[Source 2]How to make Oral Rehydration Solution at home
To prevent too much liquid being lost from the child’s body, an effective oral rehydration solution can be made using ingredients found in almost every household. One of these drinks should be given to the child every time a watery stool is passed.
Here’s how you can make your own One (1) Liter Oral Rehydration Solution [ORS] using Salt, Sugar and Water at Home
Mix an oral rehydration solution using one of the following recipes:
Ingredients:
- Half (1/2) level teaspoon of Salt
- Six (6) level teaspoons of Sugar
- One (1) Litre of clean drinking or boiled water and then cooled
Make 5 cupfuls (each cup about 200 ml.)
Preparation Method:
- Stir the mixture till the salt and sugar dissolve.
The following traditional remedies make highly effective oral rehydration solutions and are suitable drinks to prevent a child from losing too much liquid during diarrhoea:
- Breastmilk
- Gruels (diluted mixtures of cooked cereals and water)
- Carrot Soup
- Rice water – Congee
A very suitable and effective simple solution for rehydrating a child can also be made by using salt and sugar, if these ingredients are available.
If possible, add 1/2 cup orange juice or some mashed banana to improve the taste and provide some potassium.
Molasses and other forms of raw sugar can be used instead of white sugar, and these contain more potassium than white sugar.
If none of these drinks is available, other alternatives are:
- Fresh fruit juice
- Weak tea
- Green coconut water
If nothing else is available, give water from the cleanest possible source – (if possible brought to the boil and then cooled).
Method of giving oral fluids
It is important to give small amounts of fluid frequently, for example 0.5mL per kg body weight every five minutes 2. The fluid can be measured in a syringe and given to the child either by syringe, teaspoon or cup. The child is far more likely to tolerate these small amounts of fluid than if he/she drinks a large amount at once. Obviously if the child tolerates this fluid the parent can gradually increase the volume and decrease the frequency of the fluid offered.
Example of how much fluid to give to your child by age and body weight (approximates only):
- For infants less than 6 months old – See your doctor.
- For 6-23 months give 40 to 60 mL each hour.
- For 2-5 years give 60 to 100 mL each hour.
- For 6-10 years give 100 to 120 mL each hour.
- For 11-16 years give 120 to 160 mL each hour.
- For a 6 kg infant offer: 30mL every hour or 60mL every 2 hours.
- For a 12 kg toddler offer; 60mL every hour or 120mL every 2 hours.
IF YOU HAVE ANY CONCERNS ABOUT YOUR CHILD’S PROGRESS, CONTACT YOUR DOCTOR OR LOCAL HOSPITAL IMMEDIATELY!
Consult your doctor or local hospital, as soon as possible, if you have any concerns about your child’s progress – especially if:
- your child is less than six months old
- your child has other health problems
- you are unable to get your child to take the right amount of fluids (see the table over the page)
- your child keeps vomiting
- your child is very tired or drowsy
- there is blood or mucus in your child’s poo
- there is green vomit
- your child has ongoing tummy pain
- your child has high fevers
- if your child has unexpected symptoms(eg: pain when passing urine, headache etc)
- or if your child does not seem to be getting better and/or you are worried for any other reason.
Medicines to stop vomiting are occasionally used for children with persistent vomiting and dehydration. Medicines to stop diarrhea are not recommended and are usually not helpful as they can cause other problems in children.
If your child tolerates the fluid, gradually increase the amount and decrease the frequency of the fluid offered. It is important to start offering easily digested foods as soon as the vomiting stops and no later than after 24 hours EVEN if the poos are still loose.
Children who are not dehydrated should continue to be fed an age appropriate diet. Children who require rehydration should recommence age appropriate diets as soon as vomiting settles. This should be within the first 12-24 hours. Formula fed infants should recommence full strength formula.
It is important to note that small, frequent amounts of fluid will hopefully minimize the vomiting, but will not reduce the diarrhea. The aim is for the fluid input to exceed the output by enough to rehydrate and then maintain hydration. Occasional vomiting alone should not be considered as failure of oral rehydration therapy.
What to do for a breastfed infant
- Continue breast feeding on demand or at least every 2 hours.
- In between breast feeds, water or oral rehydration solution may be offered.
- Do not give solids if your child is vomiting.
When the vomiting has stopped or after 24 hours:
- Continue 2nd-3rd hourly feeds or on demand.
- In between breast feeds, oral rehydration solution or water may be offered.
- If your baby is on solids introduce simple foods such as rice cereal, potato or pumpkin – even if the poos are still loose.
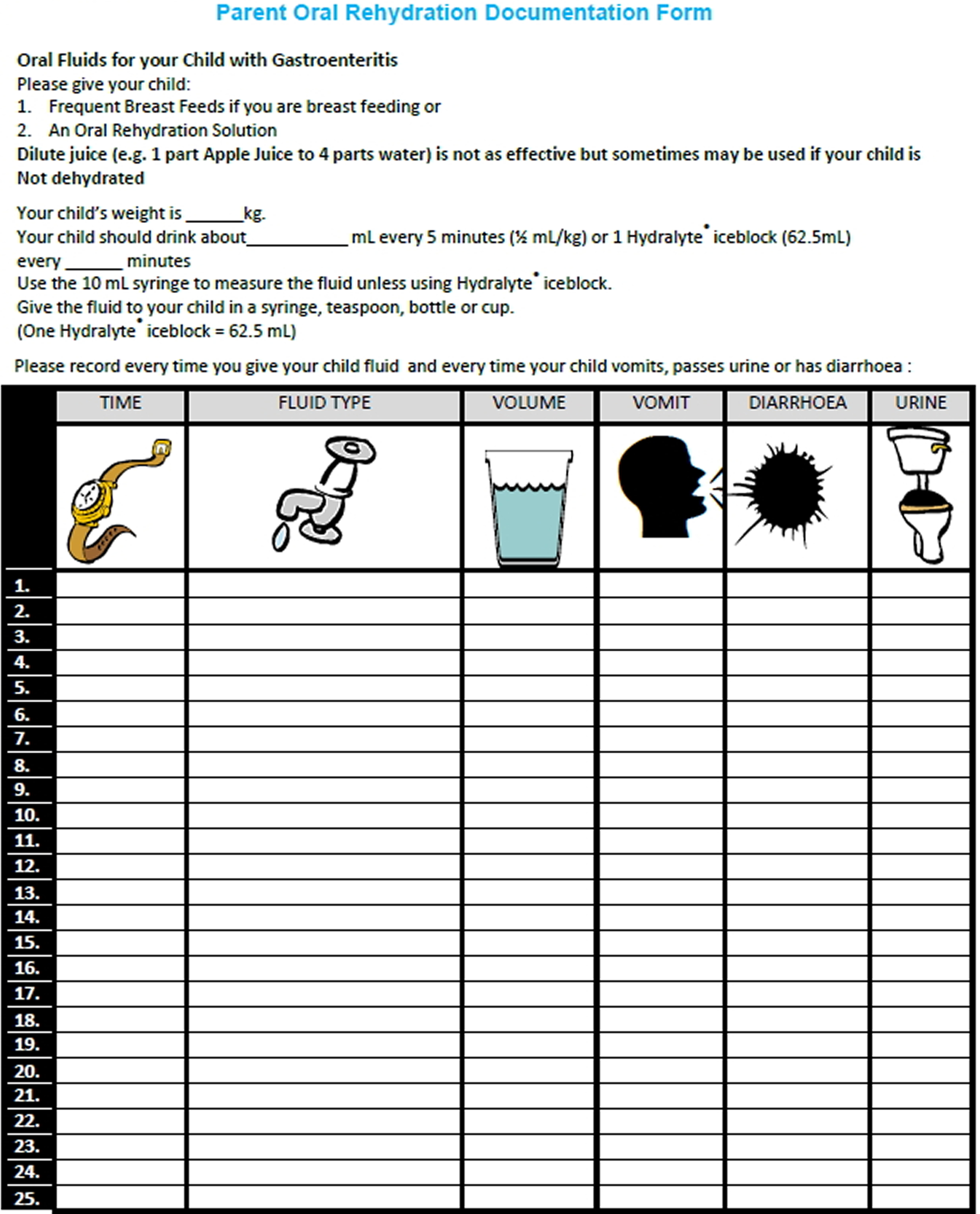
Parents can use the Parent Oral Rehydration Documentation Form below to record the fluid given and any vomits, diarrhea or urine passed.
Table 5. Parent Oral Rehydration Documentation Form
[Source 2]What to do for the bottle fed infant or older child
While your infant or child is still vomiting:
- Replace formula or usual drinks with oral rehydration fluid (from chemist) or suitable fluids.
- Aim to be back to usual strength formula/diet within 24 hours. If not, seek medical advice.
- Start usual formula or milk. Do not dilute.
- Continue giving feeds or drinks every 2-3 hours or more frequently if demanded.
- Offer age appropriate foods at meal times even if the poos are still loose.
- Occasionally children will develop lactose intolerance and the loose poos will continue. If that occurs, a doctor may advise that he/she will need lactose free milk for approximately 1 month.
Hydration tips for baby and children
Severe vomiting and diarrhea (runny poos) can quickly lead to dehydration in infants and young children. Seek medical attention promptly, if you are concerned. Frequent vomiting and runny poos means your child may be losing a lot of fluid from their body. Lost fluid must be replaced – initially with SUITABLE FLUIDS or BREAST MILK.
DO
- carry on breastfeeding or using formula, try to give small amounts more often than usual
- for babies on formula or solid foods – give them small sips of extra water
- give small children their usual diet
- give regular small sips of rehydration solution to replace lost fluids, salts and sugars – ask your pharmacist to recommend one
DON’T
- make baby formula weaker
- give young children fruit juice or fizzy drinks, it makes things like diarrhea or vomiting worse
Pedialyte for diarrhea
If you’re being sick or have diarrhea and are losing too much fluid you need to put back the sugar, salts and minerals that your body has lost.
Your pharmacist can recommend oral rehydration solution sachets like pedialyte. These are powders that you mix with water and then drink. Ask your pharmacist which ones are right for you or your child.
Oral Rehydration Solutions include Gastrolyte, Hydralyte, Pedialyte and Repalyte (available from chemist) are specially formulated to replace lost fluid. These should be mixed exactly to the manufacturer’s directions. It is very important to comply with the expiry dates of the rehydration solutions once they have been opened or made up. Oral rehydration solutions are specially designed to replace sugars and salts lost during an episode of gastroenteritis. It is better to give these over other clear fluids if it is available. Clear fluids such as juice, cordial or soft drink may be used with caution if an oral rehydration fluid is not available. However they must be diluted otherwise they may make the diarrhea worse.
Other suitable fluids include:
- Diluted cordial (one part cordial concentrate to 20 parts boiled then cooled water). For example, 5 mL (1 teaspoon) plus 100mL water.
- Diluted soft drink or juice (one part juice or soft drink to 5 parts boiled then cooled water). For example, 20 mL (1 tablespoon) plus 80mL water.
Ideally these drinks (preferably those that have been boiled) should contain:
- starches and/or sugars as a source of glucose and energy,
- some sodium and
- preferably some potassium.
Call your local emergency number or go to the hospital emergency room if:
- you’re feeling unusually tired
- you’re confused and disorientated
- any dizziness when you stand up doesn’t go away
- you haven’t peed for 8 hours
- your pulse is weak or rapid
- you have fits (seizures)
These can be signs of serious dehydration which need urgent treatment.
Call your local emergency number or take your baby or child to the hospital emergency room if they:
- seem drowsy
- breathe fast
- have few or no tears when they cry
- have a soft spot on their head that sinks inwards (sunken fontanelle)
- have a dry mouth
- have dark yellow pee
- have cold and blotchy-looking hands and feet
These can be signs of serious dehydration which need urgent treatment.
Once the dehydration has been treated your child will need to maintain their fluid levels.
What causes dehydration
Dehydration is when someone loses more fluids than they take in. When someone becomes dehydrated, it means the amount of water in their body has dropped below the level needed for normal body function. In hot weather it can be very easy for active children to become dehydrated. Some may even suffer heat exhaustion or even heat stroke. A child is more likely to be affected if they are involved in at least an hour of high intensity physical activity on a hot day. Some examples of high intensity activity include team sports (for example soccer, football or netball), swimming training, running or tennis.
Most children do not stop to drink as much as adults do. They may only stop to drink when they are very thirsty. By this time, children can already be mildly dehydrated.
People can get dehydrated:
- after strenuous exercise, especially in hot weather due to sweating
- after severe vomiting or diarrhea
- with a fever – a high temperature of 100.4 °F (38 °C) or more
- after drinking too much alcohol
- while taking certain medicines such as diuretics
- as a complication of diabetes
- if they don’t drink enough water
- been in the sun too long (heatstroke)
Anyone may become dehydrated, but babies, young children, older adults and people with long-term illnesses are at most risk.
You are dehydrated if your body doesn’t have enough water to keep it working properly. It can happen when your body loses too much fluid, such as from excessive sweating, vomiting or diarrhea.
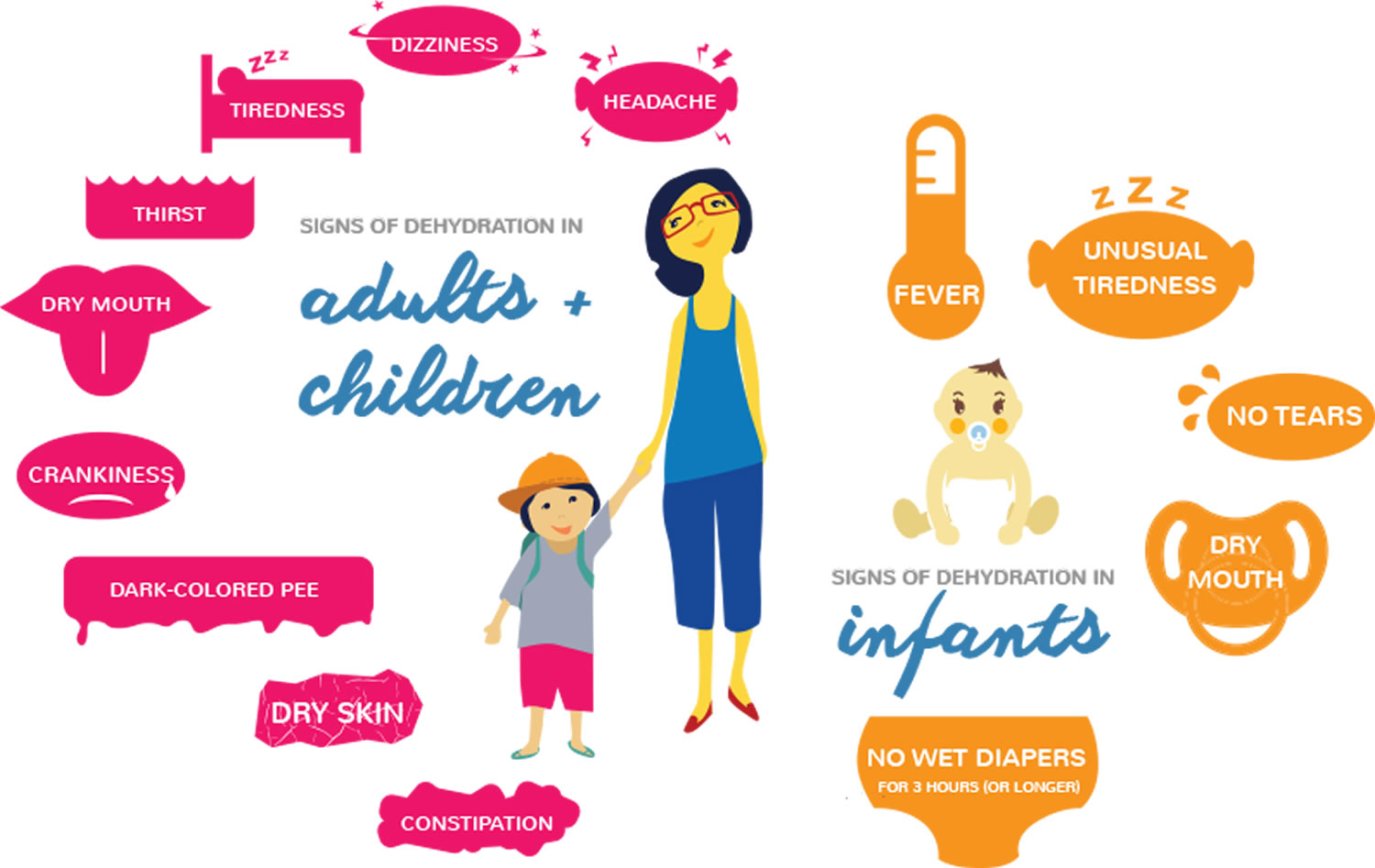
Dehydration signs and symptoms
If you have mild to moderate dehydration, you might:
- be thirsty
- have a dry mouth, lips, tongue and eyes
- have a headache
- have nausea
- have dark urine, and not so much of it
- feeling dizzy or light-headed, particularly when standing up
- peeing little and less than 4 times a day
If you have severe dehydration, you might:
- be extremely thirsty
- have a very dry mouth
- eyes are dark and sunken
- be breathing fast
- have a fast heart rate and a low blood pressure
- have a fever
- have little or no urine
- be irritable, drowsy or confused
Babies who are severely dehydrated have a sunken fontanel, the soft spot on top of a baby’s head.
Severe dehydration is a serious problem, especially in babies and young children.
 How you can reduce the risk of dehydration
How you can reduce the risk of dehydration
Drink fluids when you feel any dehydration symptoms. Keep taking small sips and gradually drink more if you can.
You can use a spoon to make it easier for your child to swallow the fluids.
You should drink enough during the day so that your pee is a pale clear color.
Drink when there is a higher risk of dehydrating. For example, if you’re vomiting, sweating or you have diarrhoea.
Carers: making sure someone drinks enough
Sometimes people you care for don’t have a sense of how much they’re drinking.
To help them:
- make sure they drink during meal times
- make drinking a social thing like “having a cup of tea”
- offer them food with a high water content – for example, soups, ice cream, jellies or fruits like melon
Children need to stay hydrated
Two thirds of our bodies are made up of water. Being dehydrated can cause poor sports performance, tiredness, headaches and crankiness – and it can lead to serious medical problems.
Signs your child could be dehydrated include:
- dizziness or light-headedness
- nausea
- a headache
- dark yellow or brown urine
- dry lips, tongue, mouth or throat.
What is the best drink to have?
- Water should always be the first choice. Children should be encouraged to keep a water bottle with them at all times and to stop and drink during activity.
- Drinks that contain some carbohydrate (sugar) and extra salts (such as sports drinks) can be useful, but are not always needed.
- Children who are involved in high intensity activity for over an hour, 2-3 times a week may benefit from using sports drinks.
- Have chilled water and sports drink with you on a hot day when children are involved in high intensity exercise. This will help to keep them hydrated and happy
- Sports drinks may be useful during exercise but are not a good choice for general drinking. They are high in sugar and can promote excess energy intake. Water is the best choice!
- Be careful when choosing sports drinks. Some “energy” type drinks may contain other additives such as caffeine. These are not suitable for children.
How much to drink?
- It is hard to work out how much fluid an active child needs on any one day. This is because different amounts of fluid are needed based on the weather and the intensity of the exercise. As a guide:
- A younger child (under 10 years) will need about 200mls of fluid at the start of exercise and at least 100mls for every 20 minutes they are involved in physical activity. This is equal to about a 300ml bottle of water or sports drink every hour.
- Older children (10 years and above) will need double this amount. They will need about 400mls of fluid at the start of exercise and at least 200mls for every 20 minutes they are involved in physical activity. This is equal to about a 600ml bottle of water or sports drink every hour.
Dehydration treatment
If your child is dehydrated, give them more fluid to drink. Water is best. This is especially important during hot weather and when they are exercising. Encourage your child to drink before, during and after exercise.
If they are sick, try to have them drink 1 cup (250ml) of water per hour for 4 hours. If they are vomiting or have diarrhea, try specially prepared children’s rehydration drinks like pedialyte, which you can buy from your local pharmacy.
Babies and young children are more at risk of severe dehydration, which is a medical emergency.
Pedialyte ingredients
Pedialyte Classic Ingredients
Water, Dextrose. Less than 2% of: Citric Acid, Natural & Artificial Flavor, Potassium Citrate, Salt, Sodium Citrate, Sucralose, Acesulfame Potassium, Zinc Gluconate, and Yellow 6.
Pedialyte AdvancedCare Ingredients
Contains milk ingredients.
Water, Dextrose. Less than 1.0% of: Galactooligosaccharides, Citric Acid, Potassium Citrate, Salt, Sodium Citrate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Zinc Gluconate, Red 40, and Blue 1.
Pedialyte AdvancedCare Plus Ingredients
Contains milk ingredients.
Water, Dextrose. Less than 1% of: Galactooligosaccharides, Salt, Citric Acid, Potassium Citrate, Natural & Artificial Flavor, Sodium Citrate, Sucralose, Acesulfame Potassium, Zinc Gluconate, and Blue 1.
Pedialyte Powder Packs Ingredients (Grape)
Anhydrous Dextrose, Citric Acid, Potassium Citrate, Salt, Sodium Citrate. Less than 2% of: Natural & Artificial Flavor, Beet Powder Color, Calcium Silicate, Acesulfame Potassium, Sucralose, and Blue 1.
Pedialyte AdvancedCare Plus Powder Packs Ingredients
Anhydrous Dextrose, Short-Chain Fructooligosaccharides, Citric Acid, Salt, Potassium Citrate, Sodium Citrate, Natural & Artificial Flavor. Less than 2% of: Calcium Silicate, Acesulfame Potassium, Sucralose, and Blue 1.
Pedialyte Freezer Pops Variety Pack Ingredients
Grape (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Red 40, Blue 1), Blue Raspberry (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Blue 1), Cherry (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Red 40), and Orange (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Yellow 6, Red 40).
Pedialyte nutrition facts
Pedialyte Classic Mixed Fruit
Serving size: 12 fl oz (360 mL)
Amount Per Serving % DV. The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 35
- Total Fat: 0 g (0% DV)
- Sodium: 370 mg (16% DV)
- Total Carbohydrate: 9 g (3% DV)
- Total Sugars: 9 g
- Added Sugars: 9 g (18% DV)
- Protein: 0g (0% DV)
Minerals
- Sodium: 370 mg (16% DV)
- Potassium: 280 mg (6% DV)
- Zinc: 2.8 mg (25% DV)
- Chloride: 440 mg (20% DV)
Pedialyte Classic Ingredients
Water, Dextrose. Less than 2% of: Citric Acid, Natural & Artificial Flavor, Potassium Citrate, Salt, Sodium Citrate, Sucralose, Acesulfame Potassium, Zinc Gluconate, and Yellow 6.
Use under medical supervision
- For infants under 1 year of age: Consult your doctor.
- For children 1 year and older and adults: Begin with small frequent sips every 15 minutes, increasing serving size as tolerated. Continue for as long as diarrhea is present.
- To maintain proper hydration, 1-2 liters (32 to 64 fl oz) of Pedialyte may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continues beyond 24 hours or if consumption needs are greater than 2 liters (64 fl oz) per day.
Directions of use
- Tastes best when served cold.
- Do not use if printed band around cap or inner foil seal is missing or broken.
- Remove protective band and twist off cap.
- Remove and throw away protective foil seal.
- Do not add water or dilute.
- After opening, replace cap, refrigerate and use within 48 hours.
- Store unopened bottles in a cool place. Avoid excessive heat.
- Do not reuse bottle.
Pedialyte AdvancedCare Strawberry Lemonade
Serving size: 12 fl oz (360 mL)
Amount Per Serving % DV. The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 25
- Total Fat: 0 g (0% DV)
- Sodium: 370 mg (16% DV)
- Total Carbohydrate: 6 g (2% DV)
- Total Sugars: 6 g
- Added Sugars: 6 g (12% DV)
- Protein: 0g (0% DV)
Minerals
- Sodium: 370 mg (16% DV)
- Potassium: 280 mg (6% DV)
- Zinc: 2.8 mg (25% DV)
- Chloride: 440 mg (20% DV)
Pedialyte AdvancedCare Ingredients
Contains milk ingredients.
Water, Dextrose. Less than 1.0% of: Galactooligosaccharides, Citric Acid, Potassium Citrate, Salt, Sodium Citrate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Zinc Gluconate, Red 40, and Blue 1.
Use under medical supervision
- For infants under 1 year of age: Consult your doctor.
- For children 1 year and older and adults: Begin with small frequent sips every 15 minutes, increasing serving size as tolerated. Continue for as long as diarrhea is present.
- To maintain proper hydration, 1-2 liters (32 to 64 fl oz) of Pedialyte AdvancedCare may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continues beyond 24 hours or if consumption needs are greater than 2 liters (64 fl oz) per day.
Directions of use
- Do not use if printed band around cap or inner foil seal is missing or broken.
- Remove protective band and twist off cap.
- Remove and throw away protective foil seal.
- After opening, replace cap, refrigerate and use within 48 hours.
- Store unopened bottles in a cool place. Avoid excessive heat.
- Do not reuse bottle.
Pedialyte AdvancedCare Plus Berry Frost
Serving size: 12 fl oz (360 mL)
Amount Per Serving % DV. The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 25
- Total Fat: 0 g (0% DV)
- Sodium: 490 mg (21% DV)
- Total Carbohydrate: 6 g (2% DV)
- Total Sugars: 6 g
- Added Sugars: 6 g (12% DV)
- Protein: 0g (0% DV)
Minerals
- Sodium: 490 mg (21% DV)
- Potassium: 280 mg (6% DV)
- Zinc: 2.8 mg (25% DV)
- Chloride: 630 mg (25% DV)
Pedialyte AdvancedCare Plus Ingredients
Contains milk ingredients.
Water, Dextrose. Less than 1% of: Galactooligosaccharides, Salt, Citric Acid, Potassium Citrate, Natural & Artificial Flavor, Sodium Citrate, Sucralose, Acesulfame Potassium, Zinc Gluconate, and Blue 1.
Use under medical supervision
- For infants under 1 year of age: Consult your doctor.
- For children 1 year and older and adults: Begin with small frequent sips every 15 minutes, increasing serving size as tolerated. Continue for as long as diarrhea is present.
- To maintain proper hydration, 1-2 liters (32 to 64 fl oz) of Pedialyte may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continues beyond 24 hours or if consumption needs are greater than 2 liters (64 fl oz) per day.
Directions of use
- Tastes best when served cold.
- Do not use if printed band around cap or inner foil seal is missing or broken.
- Remove protective band and twist off cap.
- Remove and throw away protective foil seal.
- Do not add water or dilute.
- After opening, replace cap, refrigerate and use within 48 hours.
- Store unopened bottles in a cool place. Avoid excessive heat.
- Do not reuse bottle.
Pedialyte Powder Packs Grape
Serving size: 9 g (1/2 packet) prepared with 1 cup [237 mL] water. For ages 4+
Amount Per Serving % DV (Daily Value). The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 25
- Total Fat: 0 g (0% DV)
- Sodium: 240 mg (10% DV)
- Potassium: 180 mg (5% DV)
- Total Carbohydrate: 6 g (2% DV)
- Total Sugars: 6 g
- Protein: 0g (0% DV)
Minerals
- Sodium: 10.6 mEq
- Potassium: 4.7 mEq
- Chloride: 294 mg
- Chloride: 8.3 mEq (8% DV)
Pedialyte Powder Packs Ingredients (Grape)
Anhydrous Dextrose, Citric Acid, Potassium Citrate, Salt, Sodium Citrate. Less than 2% of: Natural & Artificial Flavor, Beet Powder Color, Calcium Silicate, Acesulfame Potassium, Sucralose, and Blue 1.
Use under medical supervision
- Pedialyte Powder Packs and Freezer Pops are NOT for use for children under 1 year of age.
- For children 1 year and older and adults: Begin with small frequent sips every 15 minutes, increasing serving size as tolerated. Continue for as long as diarrhea is present.
- To maintain proper hydration, 4 – 8 servings (32 to 64 fl oz) of Pedialyte may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continues beyond 24 hours or if consumption needs are greater than 2 liters (64 fl oz) per day.
Directions of use
- Tastes best served cold.
- Reconstitute only with water.
- Mix one pack of Pedialyte Powder with 16 fl oz (2 cups) water. Stir to dissolve.
- Store unused, reconstituted product in sealed container in refrigerator for up to 24 hours.
- Do not store powder packs at extreme temperatures.
Pedialyte AdvancedCare Plus Powder Packs (Strawberry Freeze)
Serving size: 17 g (1 Packet)
Amount Per Serving % DV (Daily Value). The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 30
- Total Fat: 0 g (0% DV)
- Sodium: 650 mg (28% DV)
- Potassium: 370 mg (8% DV)
- Total Carbohydrate: 8 g (3% DV)
- Total Sugars: 8 g
- Added Sugars: 8 g (16% DV)
- Protein: 0g (0% DV)
Minerals
- Sodium: 650 mg (28% DV)
- Potassium: 370 mg (8% DV)
- Chloride: 840 mg (35% DV)
Pedialyte AdvancedCare Plus Powder Packs Ingredients
Anhydrous Dextrose, Short-Chain Fructooligosaccharides, Citric Acid, Salt, Potassium Citrate, Sodium Citrate, Natural & Artificial Flavor. Less than 2% of: Calcium Silicate, Acesulfame Potassium, Sucralose, and Blue 1.
Use under medical supervision
- For infants under 1 year of age: Consult your doctor.
- For children 1 year and older and adults: Begin with small frequent sips every 15 minutes, increasing serving size as tolerated. Continue for as long as diarrhea is present.
- To maintain proper hydration, 1-2 liters (32 to 64 fl oz) of Pedialyte may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continues beyond 24 hours or if consumption needs are greater than 2 liters (64 fl oz) per day.
Directions of use
- Tastes best when served cold.
- Do not use if printed band around cap or inner foil seal is missing or broken.
- Remove protective band and twist off cap.
- Remove and throw away protective foil seal.
- Do not add water or dilute.
- After opening, replace cap, refrigerate and use within 48 hours.
- Store unopened bottles in a cool place. Avoid excessive heat.
- Do not reuse bottle.
Pedialyte Freezer Pops Variety Pack
- Grape, Blue Raspberry, Cherry, and Orange
Serving size: 63 mL (1 pop). Children over 4 and adults
Amount Per Serving % DV (Daily Value). The % Daily Value (DV) tells you how much a nutrient in a serving of food contributes to a daily diet. 2,000 calories a day is used for general nutrition advice.
Nutrition Information
- Calories: 5
- Total Fat: 0 g (0% DV)
- Sodium: 65 mg (3% DV)
- Potassium: 50 mg (1% DV)
- Total Carbohydrate: 2 g (1% DV)
- Total Sugars: 2 g
- Protein: 0g (0% DV)
Minerals
- Chloride: 2.2 mEq (2% DV)
Pedialyte Freezer Pops Variety Pack Ingredients
Grape (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Red 40, Blue 1), Blue Raspberry (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Blue 1), Cherry (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Red 40), and Orange (Water, Anhydrous Dextrose; Less than 2% of: Citric Acid, Salt, Sodium Carboxymethylcellulose, Potassium Citrate, Potassium Sorbate, Sodium Benzoate, Natural & Artificial Flavor, Sucralose, Acesulfame Potassium, Yellow 6, Red 40).
Use under medical supervision
- Pedialyte Powder Packs and Freezer Pops are NOT for use for children under 1 year of age.
- For children 1 year and older and adults: Offer Pedialyte Freezer Pops as frequently as desired.
- To maintain proper hydration, 16 to 32 Freezer Pops (or a total of 32 to 64 fl oz of any Pedialyte product) may be needed per day. Consult your doctor if vomiting, fever, or diarrhea continue beyond 24 hours or if consumption needs are greater than 32 Freezer Pops (64 fl oz) per day.
- Freezer Pops can be consumed without freezing, but the flavors are best when frozen.
- NOTE: Like colored ices, Pedialyte Freezer Pops may temporarily color mouth.
Directions of use
- To eat frozen
- Remove Pops from carton and freeze before separating.
- Tear or cut carefully between sleeves along perforations.
- Cut off top of sleeve.
- To drink
- Cut carefully between sleeves along perforations.
- Cut off top of sleeve and pour liquid into cup or glass and drink.
- Discard unused portion of opened product.
- Do not reuse plastic sleeves.
- Store unopened pops in cool place. Avoid excessive heat.
Is pedialyte good for you
Pedialyte is a medical-grade rehydration solution. It is good for adding back fluid after fluid loss or to help prevent fluid and electrolyte problems during bouts of diarrhea or vomiting.
Can you drink pedialyte everyday
Pedialyte is a medical-grade rehydration solution that is meant to treat serious dehydration caused by vomiting or diarrhea and is not meant to be used everyday. Furthermore, Pedialyte drinks are usually high in kilojoules (energy) and added sugar and provide very few nutrients. They can also contribute to poor nutrition, tooth decay and weight gain.
It is really important to limit the number of sugary drinks that you and your children have and to encourage them to have healthier options like water. Drinking water is the best way to quench a thirst – and it doesn’t come with the sugar and the kilojoules.
Pedialyte vs Gatorade
Pedialyte is a medical-grade rehydration solution. It is good for adding back fluid after fluid loss or to help prevent fluid and electrolyte problems during bouts of diarrhea or vomiting.
Gatorade is a sports beverage like other sports beverages are designed to give athletes carbs, electrolytes, and fluid during high-intensity workouts that last an hour or more. For average people, they’re just another source of sugar and calories.
Sports drinks provide a simple and effective way to replace fluid and carbohydrate simultaneously during exercise. Of course, specialized products such as Gatorade are expensive and are best used in the right sporting situation. Some people use cordial or carbohydrate foods such as fruit, bars, confectionary or sandwiches to provide a fuel boost during exercise. A carbohydrate intake of about 50 g per hour is generally recommended for prolonged events. Successful strategies are ultimately decided by individual preferences and experience.
Water is a cheap and readily available fluid, and is often quoted to be the “best” drink for active people. However, carbohydrate intake is known to improve performance during events of longer than 90 minutes, by providing the muscles and brain with extra fuel. Recently a number of studies have shown that carbohydrate intake may also be of benefit for a workout of as little as one hour. It certainly won’t harm performance, although some individuals may need to count the cost or the kilojoules involved.
Examples of 50g carbohydrate snacks include:
- 750 mL sports drink or cordial
- 500 mL fruit juice or soft drink
- 250 mL og liquid meal supplement (eg. Sustagen)
- 250 mL fruit smoothie
- 3 medium pieces of fruit
- honey or jam sandwich
- 60g packet of jelly beans or jubes
- 1 carton of fruit yoghurt + 250 mL of fruit juice
- bowl cereal + skim milk
- carton of fromage frais + granola bar
Pedialyte side effects
There are no known drug interactions for Pedialyte (electrolyte replacement solutions). However, this does not necessarily mean no interactions exist. Always consult with your doctor or pharmacist.
Applies to electrolyte replacement solutions: oral packet, oral powder for solution, oral powder for suspension, oral solution, oral tablet
Along with its needed effects, electrolyte replacement solutions (the active ingredient contained in Pedialyte) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor as soon as possible if any of the following side effects occur while taking electrolyte replacement solutions:
Symptoms of too much sodium (hypernatremia) in the body
- Convulsions (seizures)
- dizziness
- fast heartbeat
- high blood pressure
- irritability
- muscle twitching
- restlessness
- swelling of feet or lower legs
- weakness
Symptoms of too much fluid in the body
- Puffy eyelids
Some side effects of electrolyte replacement solutions may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Vomiting (mild)
Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
- Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
- Signs of fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, a heartbeat that does not feel normal, very bad dizziness or passing out, fast heartbeat, more thirst, seizures, feeling very tired or weak, not hungry, unable to pass urine or change in the amount of urine produced, dry mouth, dry eyes, or very bad upset stomach or throwing up.
- What is Pedialyte? https://pedialyte.com/what-is-pedialyte[↩]
- Infants and Children: Management of Acute Gastroenteritis, Fourth Edition 19-Dec-2014. http://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2014_024.pdf[↩][↩][↩][↩]
- New formula oral rehydration salts. http://apps.who.int/medicinedocs/en/d/Js4950e/2.4.html[↩][↩][↩][↩]
- Aperia A. et al. Salt and water homeostasis during oral rehydration therapy. J Pediatr 1983;103:364-69[↩]
- Booth I, Ferreira R, Desjeux JF et al. Recommendation for composition of oral rehydration solutions for the children of Europe. Report of an ESPGAN working group. J Pediatric Gastroenterology and Nutrition. 1992;14:113-115.[↩]
- International Study Group on Reduced-osmolarity ORS solutions. Multicentre evaluation of reduced-osmolarity oral rehydration salts solution. Lancet. 1995;345:282-285.[↩]
- Assessing the Palatability of Oral Rehydration Solutions in School-aged ChildrenA Randomized Crossover Trial. Arch Pediatr Adolesc Med. 2010;164(8):696-702. doi:10.1001/archpediatrics.2010.129 https://jamanetwork.com/journals/jamapediatrics/fullarticle/383602[↩]