Contents
What is pelvic congestion syndrome
Pelvic congestion syndrome is defined as chronic pelvic pain in women due to incompetent (dilated and refluxing) pelvic veins 1. The characteristic severe dull aching pain of pelvic congestion syndrome is thought to be a direct result of the presence of ovarian and para-uterine varicosities, slow blood flow (congestion), retrograde flow and reflux, much like the leg pain resulting from lower extremity varicose veins 2. Most women with pelvic congestion syndrome present with a noncyclical pain lasting more than 6 months in duration 3.
Pelvic congestion syndrome may contribute up to 30% of all chronic pelvic pain referrals 1. Multiple studies have investigated this condition, including its diagnostic and therapeutic options. However, due to a lack of methodological consistency and robust data, the optimal diagnostic algorithm for pelvic congestion syndrome remain controversial 4.
Chronic pelvic pain is defined as constant or recurring, cyclical or non-cyclical pain in the lower abdomen or pelvis of a minimum of 6 months duration, causing functional disability or limitation in activities of daily living 5. Chronic pelvic pain may account for 10 to 15% of outpatient gynecologic visits in the United States 6. In the UK, the incidence of chronic pelvic pain is 38/1000 women annually, comparably common as asthma (37/1000) and back pain (41/1000) 7. Its socio-economic implications become more apparent when considering that approximately 10% of all gynecological referrals and operations are done for chronic pelvic pain 4.
Multiparous women seem to be predisposed to develop pelvic congestion syndrome 3. In patients with multiple previous pregnancies, there may have been a significant increase in intravascular volume at each term of gestation. Vein capacity can increase by 60%. Over time, venous distension can render the valves incompetent. Additionally, the weight gain and anatomic changes in the pelvic structures during pregnancy may cause chronic intermittent venous obstruction. Blood pooling in the pelvic and ovarian veins may cause further engorgement, thrombosis, and mass effect on nearby nerves, collectively contributing to pelvic pain 8. The majority of women affected are premenopausal, and a relationship between pelvic congestion syndrome and endogenous estrogen levels is suggested, as estrogen is known to weaken the vein walls.
On examination, patients can have cervical motion tenderness or point tenderness over the ovaries or uterus on bimanual exam. One may note hemorrhoids, varicose veins of the perineum, buttocks, or lower extremities. Additionally, these problems may overlap with concomitant pathology, making diagnosis and treatment even more difficult.
Identification of dilated and dysfunctional pelvic veins is crucial for the diagnosis. The gold standard in this field is digital subtraction venography, but comparable results can be obtained by non-invasive magnetic resonance venography 9, computed tomography (CT) and Doppler sonography 10. During diagnostic laparoscopy, dilated pelvic veins can be easily overlooked 11.
There are many treatment options for pelvic congestion syndrome. One of the best established is endovascular occlusion of the dilated vessels 12.
Pelvic congestion syndrome causes
The cause of pelvic congestion syndrome is still poorly understood but likely multifactorial, involving both mechanical and hormonal factors 1.
Obstructing anatomic anomalies may also lead to secondary pelvic congestion syndrome. In patients with a retroaortic left renal vein, there may be obstruction of the left ovarian vein leading to symptomatic pelvic varices 3. Additionally, the left ovarian vein and the left renal vein may by compressed by the superior mesenteric artery (Nutcracker phenomenon) as well. Finally, compression from the right common iliac artery on the left common iliac vein against the spine and pelvic brim is known to cause iliofemoral deep venous thrombosis (May–Thurner syndrome) as well as the pelvic varices of pelvic congestion syndrome 3.
Pelvic congestion syndrome symptoms
According to the literature, women with pelvic congestion syndrome-derived chronic pelvic pain are mostly multiparous and describe the abdominal pain as dull and achy with sharp exacerbations, getting worse after long periods of sitting, standing and walking; during or after intercourse (dyspareunia) or just before the onset of menses 13. The pain can be accompanied by other symptoms such as post-coital pelvic aching and ovarian point tenderness on bimanual examination 14. Other symptoms of pelvic congestion are nonspecific and variable in intensity. Affected women may have generalized lethargy, depression, abdominal or pelvic tenderness, vaginal discharge, dysmenorrhea, swollen vulva, lumbosacral neuropathy, rectal discomfort, or urinary frequency 3. Painful urination (dysuria), urinary frequency and urgency in women with unremarkable urine samples have also been described 15, as well as vulvar and lower extremity varicosities with lower limb chronic venous insufficiency 16.
Pelvic congestion syndrome diagnosis
For many women with pelvic congestion syndrome, the road toward a definitive diagnosis has been long and laborious. Certainly the diagnosis of pelvic congestion syndrome continues to challenge all physicians involved 3. However, a heightened awareness and clinical suspicion for the specific symptomatology and associated findings may bring about a more rapid progression to the much anticipated treatment.
When other pelvic pathology has been ruled out, an interventional radiologist may be consulted for additional evaluation and treatment of pelvic congestion syndrome. Several imaging modalities may already have been used by the time the patient presents to an interventional radiologist. However, the diagnosis of pelvic congestion syndrome is often missed, presumably because most imaging is done in the supine position, and venous distension may be underappreciated or even absent in this position.
Pelvic ultrasound and/or computed tomography (CT) scan are usually the first imaging modalities in the evaluation of patients with chronic pelvic pain 3. Both provide excellent resolution of the uterus. Although a CT scan has greater sensitivity for showing varicosities throughout the lower pelvis, US with Doppler examination provides dynamic information about visualized venous blood flow 17. Criteria for the sonographic diagnosis of varices includes (1) the visualization of dilated ovarian veins greater than 4 mm in diameter, (2) dilated tortuous arcuate veins in the myometrium that communicate with bilateral pelvic varicose veins, (3) slow blood flow (less than 3 cm/s), and reversed caudal or retrograde venous blood flow particularly in the left ovarian vein.5 Interestingly, more than 50% of women with pelvic congestion syndrome have associated cystic ovaries as well. The ultrasound appearance may range from classic polycystic ovarian syndrome to clusters of cysts in bilaterally enlarged ovaries (4 to 6 cysts of 5 to 15 mm in diameter) 18. The significance of these cystic changes in the ovary are unclear, particularly because most patients with pelvic congestion syndrome are not hirsute or amenorrheic. However, there is the repeated suggestion of estrogen overstimulation in women with pelvic congestion syndrome.
Either a CT scan or ultrasound may take only 20 to 30 minutes for most outpatients, and both modalities are readily accessible at most imaging centers. These studies have a relatively lower sensitivity for pelvic congestion syndrome compared with magnetic resonance imaging/MR venogram (MRI/ MRV) or diagnostic venogram; nevertheless, they are quite valuable in ruling out other pathologies especially underlying malignancies 19.
For most interventional radiologists who see pelvic congestion syndrome patients for treatment, MRI/MR venogram is the best primary imaging modality for this problem. The study is done as an outpatient, is noninvasive, requires no radiation, and is highly sensitive to the findings of pelvic varices. Typical findings of pelvic congestion syndrome on MRI include dilated, tortuous, enhancing tubular structures near the uterus and ovary that may extend to the broad ligament and pelvic sidewall. Imaging includes the following characteristics: On T1-weighted images, varices appear as flow voids; gradient-echo (GRE) shows varices have high signal intensity. On T2-weighted images, varices usually appear low in signal intensity. On 3-dimensional T1-weighted gradient-echo sequences with gadolinium, varices have high signal intensity 19. Contrast enhancement with gadolinium improves visualization, and may even increase sensitivity if sequences are obtained with the patient during a Valsalva maneuver. MR venogram images are excellent for demonstrating the complete network of pelvic venous anatomy as well as the extent of pathology.
Laparoscopy is often used in patients with chronic pelvic pain in search of a specific diagnosis. This direct visualization is excellent for ruling out other etiologies distinct from pelvic congestion syndrome such as endometriosis. However, because the examination is done supine and requires insufflation of CO2 gas, there may be compression of varices if present, thereby masking the diagnosis of pelvic congestion syndrome 20. Many Ob/Gyn physicians now opt to do the full laparoscopic view of the pelvis before insufflating with CO2; pelvic varices can then occasionally be seen filling at this point. Despite these efforts, laparoscopy can still be negative in 80 to 90% of patients who do have pelvic congestion syndrome.
Certainly, the diagnostic venogram continues to provide physicians with a reliable minimally invasive gold standard tool in patients with pelvic congestion syndrome 21. Using fluoroscopy, access is obtained through the common femoral vein. A catheter is then used to select the ovarian veins and pelvic veins respectively for contrast injection at each site. The diagnosis of pelvic congestion syndrome is confirmed with the following venographic findings: ovarian vein diameter > 6 mm in diameter, retrograde ovarian or pelvic venous flow, presence of several tortuous collateral pelvic venous pathways, and delayed or stagnant clearance of contrast at the end of injection. Although the venogram study does require radiation, the use of contrast, and is invasive, it has several advantages over other imaging. The diagnostic venogram gives immediate dynamic flow information and measurements of ovarian and pelvic veins with the option of changing patient position (e.g., on a tilt table) 22. Furthermore, the diagnostic venogram may be performed with balloon occlusion in the pelvis to further delineate venous reflux. And finally, once completed, the diagnostic venogram enables the treating interventional radiologist to immediately perform embolotherapy 22.
A transfundal pelvic venogram is an alternative diagnostic technique that has been performed by some physicians 23. Briefly, the catheter is placed directly 0.5 to 1 cm into the myometrium under fluoroscopic guidance with injection of contrast. This imaging will show venous abnormalities associated with the uterus, but there is incomplete evaluation of the ovarian veins, and other causes of pelvic varices.
Pelvic congestion syndrome treatment
Treatment options for pelvic congestion syndrome remained elusive until recently, due to controversial diagnostic methods and poor understanding of its cause ranging from psychosomatic origin to vascular causes. Since Topolanski-Sierra first noted an association in the 1950s between chronic pelvic pain and ovarian and pelvic varices 24, many treatment modalities have been proposed. Medical management with hormone analogues and analgesics, surgical ligation of ovarian veins, hysterectomy with or without bilateral salpingo-oophorectomy and transcatheter embolization have been described in the literature as treatment options for patients with pelvic congestion syndrome today.
Medical treatment of pelvic congestion syndrome includes psychotherapy, progestins, danazol, phlebotonics, gonadotropins receptor agonists (GnRH) with hormone replacement therapy (HRT), dihydroergotamine, and nonsteroidal antiinflammatory drugs (NSAIDS). Specifically, the literature supports use of medroxyprogesterone acetate (MPA), or the GnRH analogue goserelin in an effort to suppress ovarian function and/or increase venous contraction. Medroxyprogesterone acetate may be given orally 30 mg/day for 6 months. Goserelin acetate is dosed as an injection of 3.6 mg monthly over a 6-month period. As chemical ovarian ligation has numerous side effects, estrogen replacement or “add-back” therapy is frequently required as well 25.
In the 1980s, surgical treatment was described by Rundqvist et al 26, which consisted of extraperitoneal resection of the left ovarian vein, which proved to be useful in relieving symptoms of pelvic congestion syndrome. Subsequent studies described anatomic abnormalities with the proposed etiology being incompetent ovarian veins. This notion was supported by the fact that surgical treatment such as ventrosuspension of the retroverted uterus and hysterectomies proved to be of little benefit. Despite the curative intent of hysterectomy, studies reported residual pain in 33% of patients and a 20% recurrence rate 27, which led to the advent of surgical ligation or resection of ovarian veins. More recently, laparoscopic ligation bilateral ovarian veins has been gaining popularity among laparoscopic gynecologists, but surgical experience of ovarian vein ligation is anecdotal with only a few available case studies 21. The procedure is performed in a supine position with insufflation of pressurized carbon dioxide into the peritoneal cavity, forcing venous effacement and decompression, which potentially underestimates the number of actual varices thereby decreasing procedural efficacy 28. In addition, laparoscopy is an invasive procedure that generally requires anesthesia and may be associated with significant morbidity, poor cosmesis, and a hospital stay of at least 2 days 28.
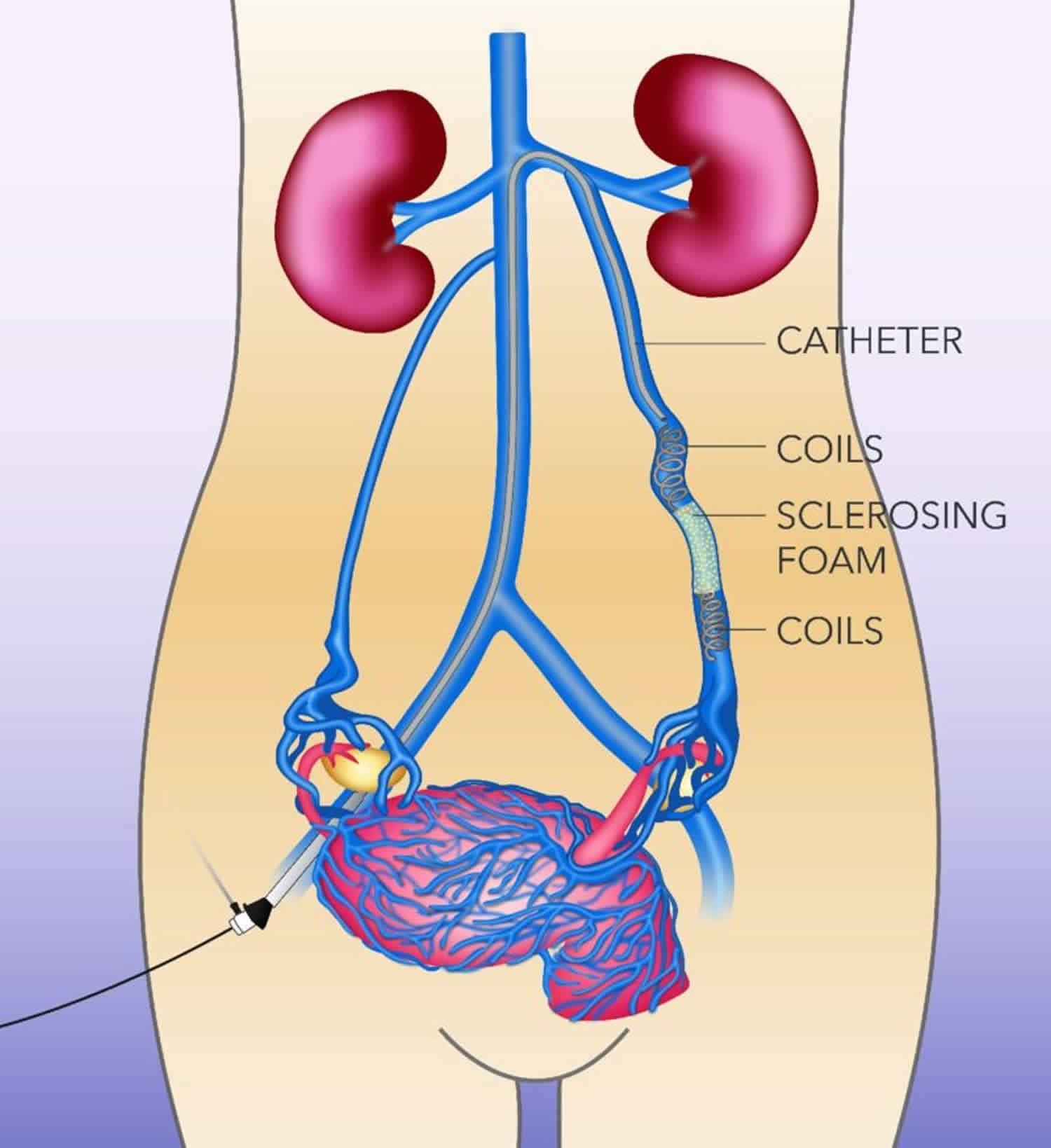
To improve clinical efficacy and reduce perioperative and postoperative morbidity, percutaneous pelvic vein embolization therapy has been utilized. Since its introduction in 1993 by Edwards et al 29, this modality has revolutionized the treatment of pelvic congestion syndrome. The procedure is usually performed at the time of diagnostic venography using a variety of embolic agents, including sclerosant foam and coils. In several published series in the 1990s, success rates for reduction of chronic pelvic pain ranged from 50 to 80%. With advancements in technique, clinical success is achieved in 70 to 85% of treated patients 20. Kim et al 30 found significant improvement in 83% of women in their overall pain perception levels with a mean of 45 months of long-term follow up.
The technique of transcatheter embolotherapy for ovarian and pelvic varices is straightforward, and a brief summary of the technique is presented here. The ovarian and internal iliac veins may be approached from a jugular or femoral approach. A 7 French (7 F) femoral sheath is placed and a 7 F guiding catheter with a “Hopkins curve” shape is used to select the left renal vein. Once the catheter is “seated,” a 5 F coaxially directed catheter is advanced over a guide wire into the ovarian vein plexus. A slurry of Gelfoam and 5% sodium morrhuate is injected. After an interval of 3 to 5 minutes, the main left ovarian vein is occluded using coils. Other embolic agents including sclerosants and glue have also been detailed in the literature. From the inferior vena cava, the right ovarian vein is then selectively catheterized using a Simmons I or II guiding catheter. A second catheter is then advanced coaxially over a guide wire down into the right pelvic varices. The embolization procedure is then repeated 20.
Given the communications that exist between ovarian veins and internal iliac veins, bilateral venography and embolization of both ovarian and internal iliac veins is required to reduce the theoretical chance of recurrence. To evaluate the internal iliac veins, it may be helpful to advance a balloon catheter. Briefly, the balloon is inflated at the proximal vein, and venogram performed through the end hole of the catheter. This allows for improved visualization of the vein’s course and caliber. The balloon occlusion technique should be used to evaluate the internal iliac veins. If pelvic varices or communications with the ovarian varices are identified with the internal iliac veins, then transcatheter embolotherapy should be performed in these veins as well. To embolize the pelvic varices, balloon occlusion venography is followed by injection of the embolization/sclerosant mixture described above. The balloon remains inflated for ~5 to 10 minutes to reduce the dilutional effects of returning blood flow 20. Coils should be avoided in the internal iliac veins because of the difficulty in delivering these devices in capacious veins and the inherent risk of their embolization to the lungs.
Embolotherapy for pelvic congestion syndrome is an exciting therapy that has proven to be safer over the past 2 decades 3. A more recent article by Chung et al 31 examined the effect of patient stress level on treatment efficacy, directly comparing hysterectomy with oophorectomy versus venous embolization for the treatment of pelvic congestion syndrome. Using both the social readjustment rating scale and visual analog pain scale, patients were divided into subsets. Following directed comparison of the subgroups after treatment, analysis of pain scores showed that venous embolization was more effective than hysterectomy, especially for patients who are “typically or moderately highly stressed.” Kim et al 30 has demonstrated that pelvic congestion syndrome patients who underwent ovarian and pelvic venous embolization have a more durable result in reduction of their pelvic pain. In this study, 83% of patients had a positive treatment response clinically at long-term follow-up with the average duration of follow-up being ~48 months. Further, patients who had had venous embolotherapy showed no significant change in menses, fertility, or hormone levels. Finally, a subset of patients who had previously undergone hysterectomy before embolization still achieved significant improvement based on numeric pain perception scores. In their long-term results, Kim et al 30 reported no major complications and also did not find any significant changes in the basal follicle-stimulating hormone, luteinizing hormone, or estradiol levels.
One study reported complications such as gonadal vein perforation, nontarget embolization including pulmonary coil embolization, and cardiac arrhythmias in 8% of their participants 32. Other reported complications of embolotherapy are rare (< 4%) and include ovarian vein thrombophlebitis, recurrence of varices, migration of embolic material, and radiation exposure to ovaries 33. Long-term data shows no demonstrable negative effects on menstrual cycle or fertility from transcatheter embolotherapy 30. It has proven to be a safe and effective nonsurgical approach in reducing chronic pelvic pain associated with pelvic venous incompetence. Moreover, the authors reported a 50% pregnancy rate in premenopausal women who would otherwise become infertile in exchange for pain relief with either medical or surgical therapies 30.
- Jurga-Karwacka A, Karwacki GM, Schoetzau A, Zech CJ, Heinzelmann-Schwarz V, Schwab FD. A forgotten disease: Pelvic congestion syndrome as a cause of chronic lower abdominal pain. PLoS One. 2019;14(4):e0213834. Published 2019 Apr 2. doi:10.1371/journal.pone.0213834 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6445463[↩][↩][↩]
- The relationship between pelvic vein incompetence and chronic pelvic pain in women: systematic reviews of diagnosis and treatment effectiveness. Champaneria R, Shah L, Moss J, Gupta JK, Birch J, Middleton LJ, Daniels JP. Health Technol Assess. 2016 Jan; 20(5):1-108.[↩]
- Ignacio EA, Dua R, Sarin S, et al. Pelvic congestion syndrome: diagnosis and treatment. Semin Intervent Radiol. 2008;25(4):361–368. doi:10.1055/s-0028-1102998 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3036528[↩][↩][↩][↩][↩][↩][↩][↩]
- Howard FM. Chronic pelvic pain. Obstet Gynecol. 2003. March;101(3):594–611[↩][↩]
- Soysal ME, Soysal S, Vicdan K, Ozer S. A randomized controlled trial of goserelin and medroxyprogesterone acetate in the treatment of pelvic congestion. Hum Reprod Oxf Engl. 2001. May;16(5):931–9[↩]
- Robinson J C. Chronic pelvic pain. Curr Opin Obstet Gynecol. 1993;5:740–743.[↩]
- Taylor HC. Life situations, emotions and gynecologic pain associated with congestion. Res Publ—Assoc Res Nerv Ment Dis. 1949. December;29:1051–6.[↩]
- Pelvic vascular congestion-half a century later. Stones RW. Clin Obstet Gynecol. 2003 Dec; 46(4):831-6.[↩]
- Asciutto G, Mumme A, Marpe B, Köster O, Asciutto KC, Geier B. MR venography in the detection of pelvic venous congestion. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2008. October;36(4):491–6.[↩]
- Malgor RD, Adrahtas D, Spentzouris G, Gasparis AP, Tassiopoulos AK, Labropoulos N. The role of duplex ultrasound in the workup of pelvic congestion syndrome. J Vasc Surg Venous Lymphat Disord. 2014. January;2(1):34–8. 10.1016/j.jvsv.2013.06.004[↩]
- Sharma D, Dahiya K, Duhan N, Bansal R. Diagnostic laparoscopy in chronic pelvic pain. Arch Gynecol Obstet. 2011. February;283(2):295–7. 10.1007/s00404-010-1354-z[↩]
- Nasser F, Cavalcante RN, Affonso BB, Messina ML, Carnevale FC, de Gregorio MA. Safety, efficacy, and prognostic factors in endovascular treatment of pelvic congestion syndrome. Int J Gynecol Obstet. 2014. April 1;125(1):65–8[↩]
- Champaneria R, Shah L, Moss J, Gupta JK, Birch J, Middleton LJ. The relationship between pelvic vein incompetence and chronic pelvic pain in women: systematic reviews of diagnosis and treatment effectiveness. Health Technol Assess Winch Engl. 2016. January;20(5):1–108[↩]
- Beard RW, Reginald PW, Wadsworth J. Clinical features of women with chronic lower abdominal pain and pelvic congestion. Br J Obstet Gynaecol. 1988. February;95(2):153–61[↩]
- Ganeshan A, Upponi S, Hon LQ, Uthappa MC, Warakaulle DR, Uberoi R. Chronic pelvic pain due to pelvic congestion syndrome: the role of diagnostic and interventional radiology. Cardiovasc Intervent Radiol. 2007. December;30(6):1105–11. 10.1007/s00270-007-9160-0[↩]
- Asciutto G, Mumme A, Marpe B, Köster O, Asciutto KC, Geier B. MR venography in the detection of pelvic venous congestion. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg. 2008. October;36(4):491–6[↩]
- Park S J, Lim J W, Ko Y T, et al. Diagnosis of pelvic congestion syndrome using transabdominal and transvaginal sonography. AJR Am J Roentgenol. 2004;182(3):683–688.[↩]
- Coakley F V, Varghese S L, Hricak H. CT and MRI of pelvic varices in women. J Comput Assist Tomogr. 1999;23:429–434[↩]
- Kuligowska E, Deeds L, Kang L. Pelvic pain: overlooked and underdiagnosed gynecologic conditions. Radiographics. 2005;25(1):3–20[↩][↩]
- Venbrux A C, Chang A H, Kim H S, et al. Pelvic congestion syndrome (pelvic venous incompetence): impact of ovarian and internal iliac vein embolotherapy on menstrual cycle and chronic pelvic pain. J Vasc Interv Radiol. 2002;13(2):171–178[↩][↩][↩][↩]
- Stones R W. Pelvic vascular congestion: half a century later. Clin Obstet Gynecol. 2003;46(4):831–836[↩][↩]
- Venbrux A C, Lambert D L. Embolization of the ovarian veins as a treatment for patients with chronic pelvic pain caused by pelvic venous incompetence (pelvic congestion syndrome) Curr Opin Obstet Gynecol. 1999;11:395–399[↩][↩]
- Beard R W, Highman J H, Pearce S, et al. Diagnosis of pelvic varicosities in women with chronic pelvic pain. Lancet. 1984;2:946–949[↩]
- Topolanski-Sierra R. Pelvic phlebography. Am J Obstet Gynecol. 1958;76:44–45[↩]
- Soysal M E, Soysal S, Vidcan K, Ozer S. A randomized controlled trial of goserelin and medroxyprogesterone acetate I in the treatment of pelvic congestion. Hum Reprod. 2001;16(5):931–939.[↩]
- Rundqvist E, Sandholm L E, Larsson G. Treatment of pelvic varicosities causing lower abdominal pain with extraperitoneal resolution of left ovarian vein. Ann Chir Gynaecol. 1984;73:339–341[↩]
- Carter J E. Surgical treatment for chronic pelvic pain. JSLS. 1998;2(2):129–139[↩]
- Venbrux A C, Chang A H, Kim H S, et al. Pelvic congestion syndrome (pelvic venous incompetence): impact of ovarian and internal iliac vein embolotherapy on menstrual cycle and chronic pelvic pain. J Vasc Interv Radiol. 2002;13(2):171–178.[↩][↩]
- Edwards R D, Robertson J R, MacLean A B, Hemmingway A P. Case report: pelvic pain syndrome – successful treatment of a case by ovarian vein embolization. Clin Radiol. 1993;47:429–431[↩]
- Kim H S, Malhotra A D, Rowe P C, Lee J M, Venbrux A C. Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol. 2006;17:289–297[↩][↩][↩][↩][↩]
- Chung M-H, Huh C-Y. Comparison of treatments for pelvic congestion syndrome. Tohoku J Exp Med. 2003;201:131–138[↩]
- Maleux G, Stockx L, Wilms G, et al. Ovarian vein embolization for the treatment of pelvic congestion syndrome: long term technical and clinical results. J Vasc Interv Radiol. 2000;11:859–864[↩]
- Ganeshan A, Upponi S, Hon L, Uthappa M C, Warakaulle D R, Uberoi R. Chronic pelvic pain due to pelvic congestion syndrome: the role of diagnostic and interventional radiology. Cardiovasc Intervent Radiol. 2007;30:1105–1111[↩]