Contents
What is pelvic organ prolapse
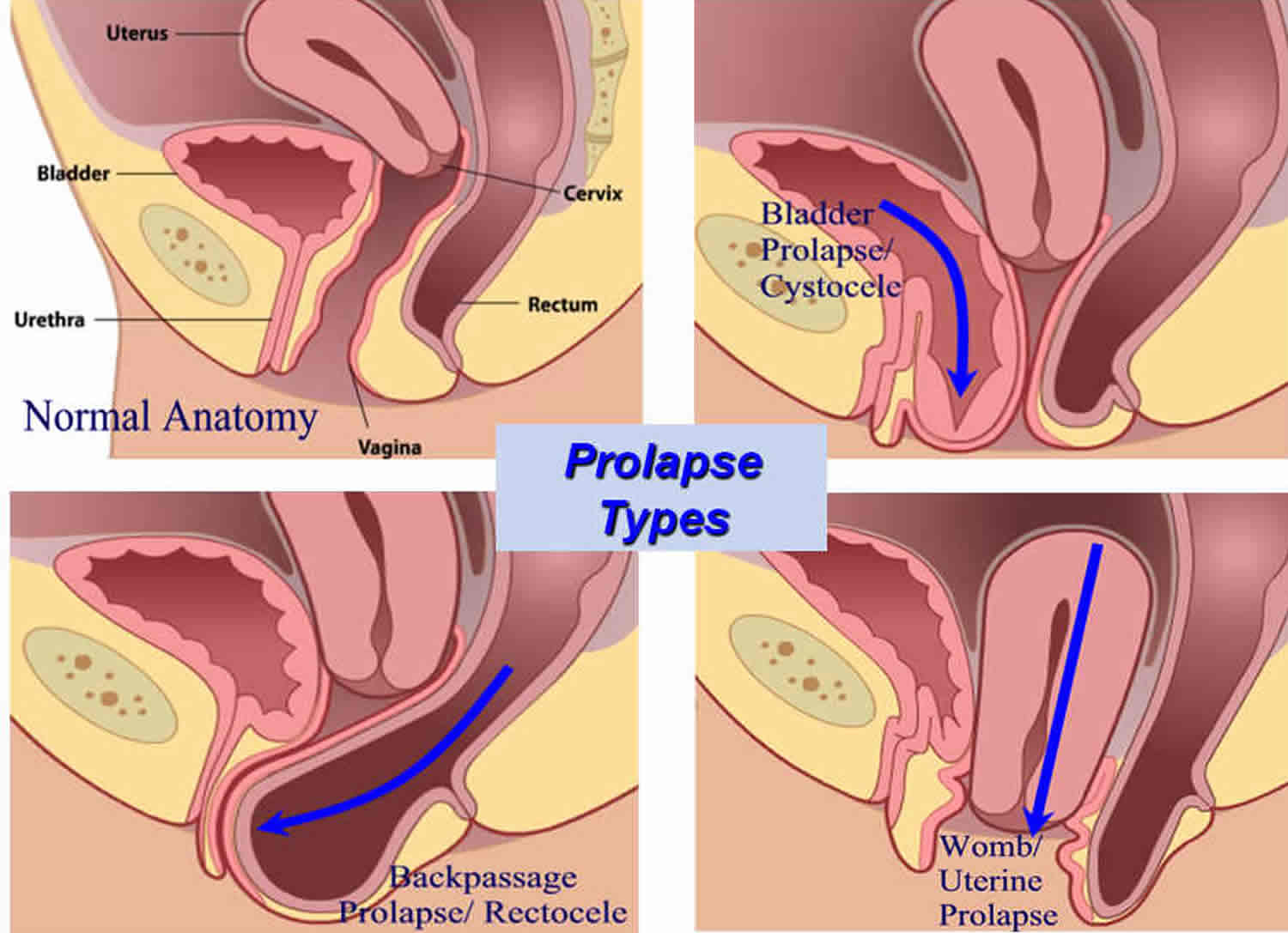
Pelvic organ prolapse is when one or more of the organs in the pelvis slip down from their normal position and bulge into the vagina. The prolapsed organ can be the womb (uterus), bowel (rectum), bladder or top of the vagina.
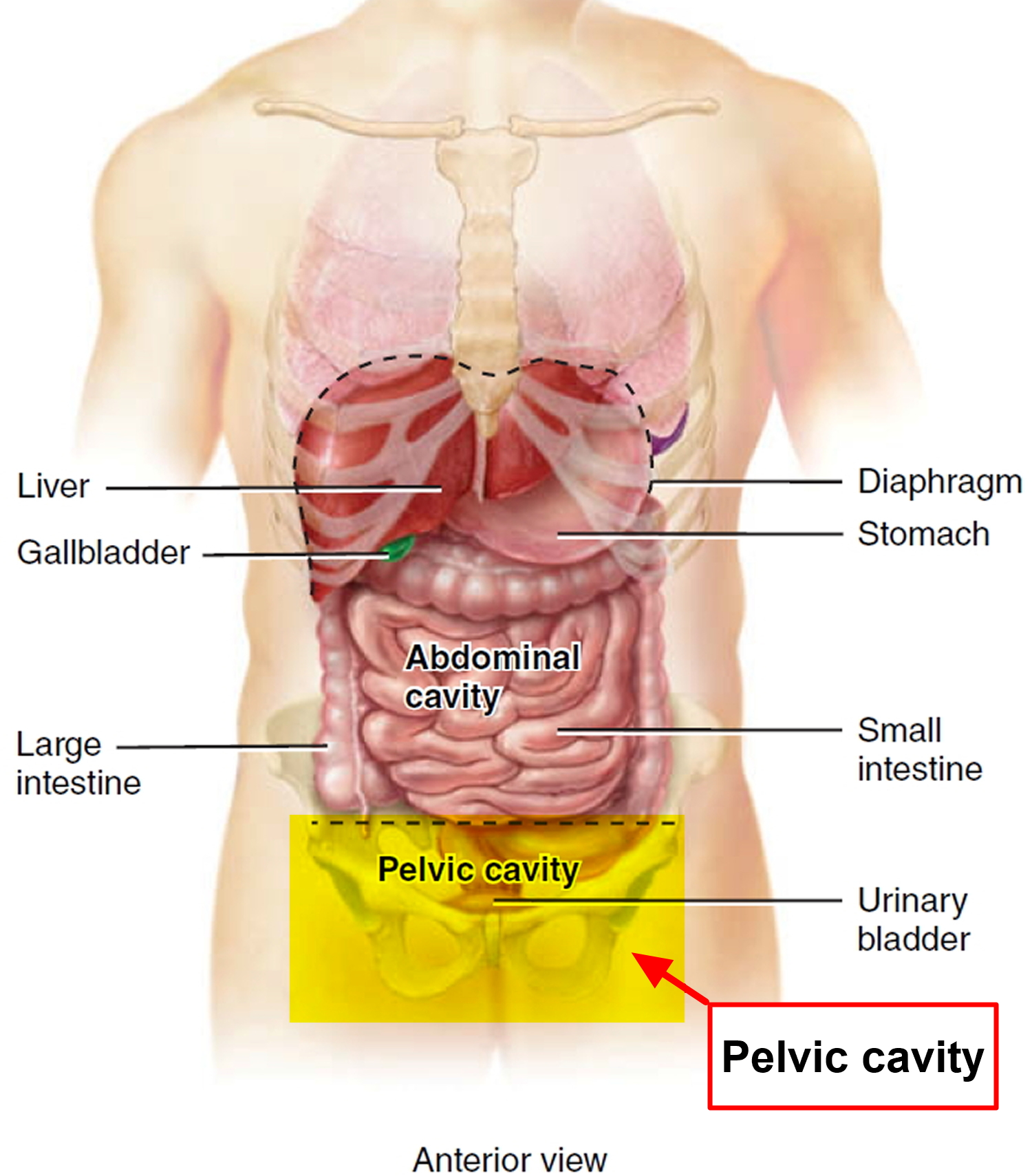
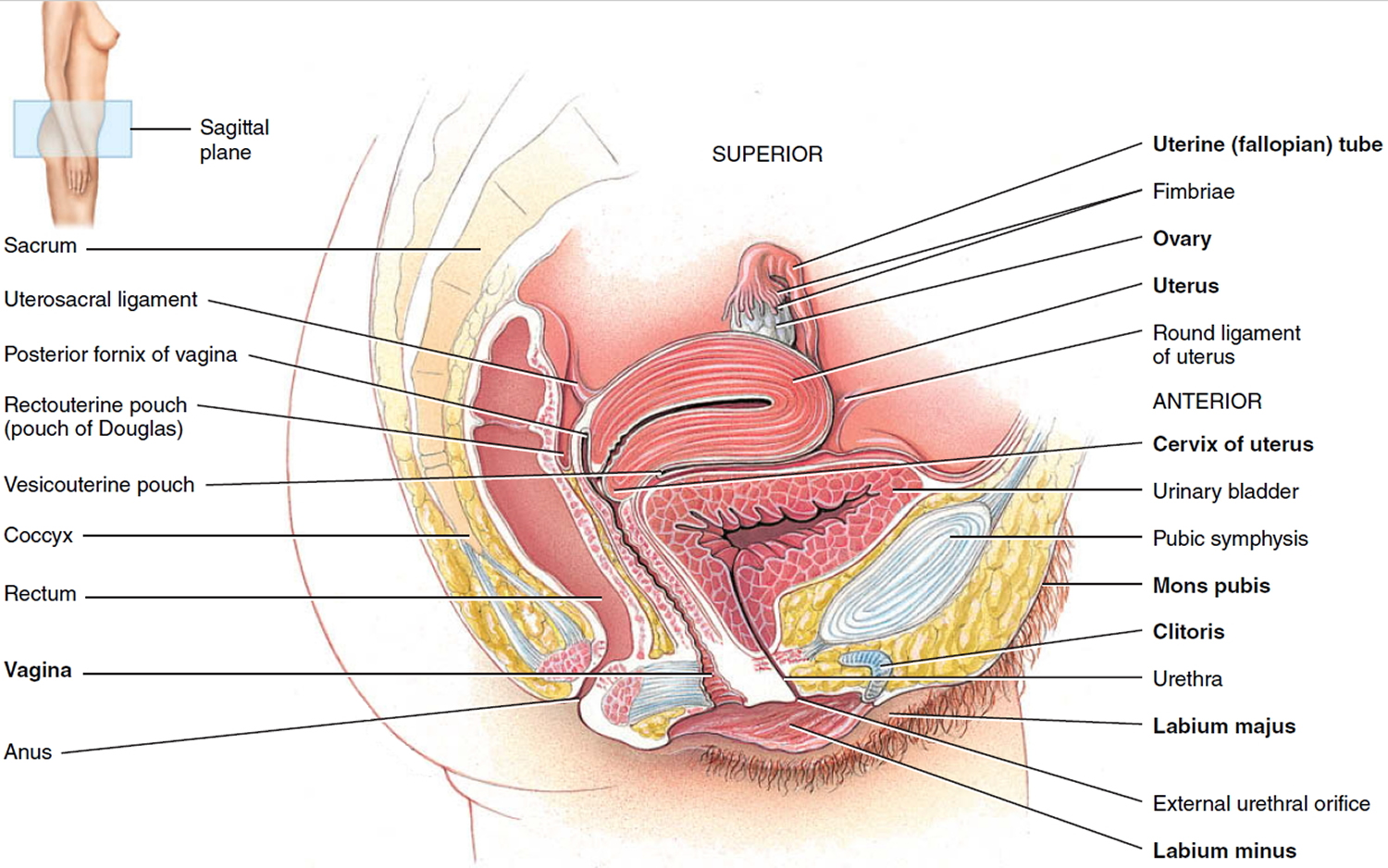
The pelvic organs within a woman’s pelvis (uterus, bladder and rectum) are normally held in place by ligaments and muscles known as the pelvic floor (see Figure 3 below). If these support structures are weakened by overstretching, the pelvic organs can bulge (prolapse) from their natural position into the vagina. When this happens it is known as pelvic organ prolapse. Sometimes a prolapse may be large enough to protrude outside the vagina.
Women most commonly develop pelvic organ prolapse years after childbirth, after a hysterectomy or after menopause. However, it is difficult to know exactly how many women are affected by pelvic organ prolapse since many do not go to their doctor about it. However, it does appear to be very common, especially in older women. Half of women over 50 will have some symptoms of pelvic organ prolapse and by the age of 80 more than one in ten will have had surgery for prolapse.
A prolapse isn’t life-threatening, but it can cause pain and discomfort. Pelvic organ prolapse can affect quality of life by causing symptoms such as discomfort or a feeling of heaviness. It can cause bladder and bowel problems, and sexual activity may also be affected. Symptoms can usually be improved with pelvic floor exercises and lifestyle changes including stopping smoking, weight loss, exercise and avoiding constipation, as well as avoidance of activities that may make your prolapse worse such as heavy lifting, but sometimes medical and surgical treatment is needed.
What is the pelvic floor and why does it become weak in women?
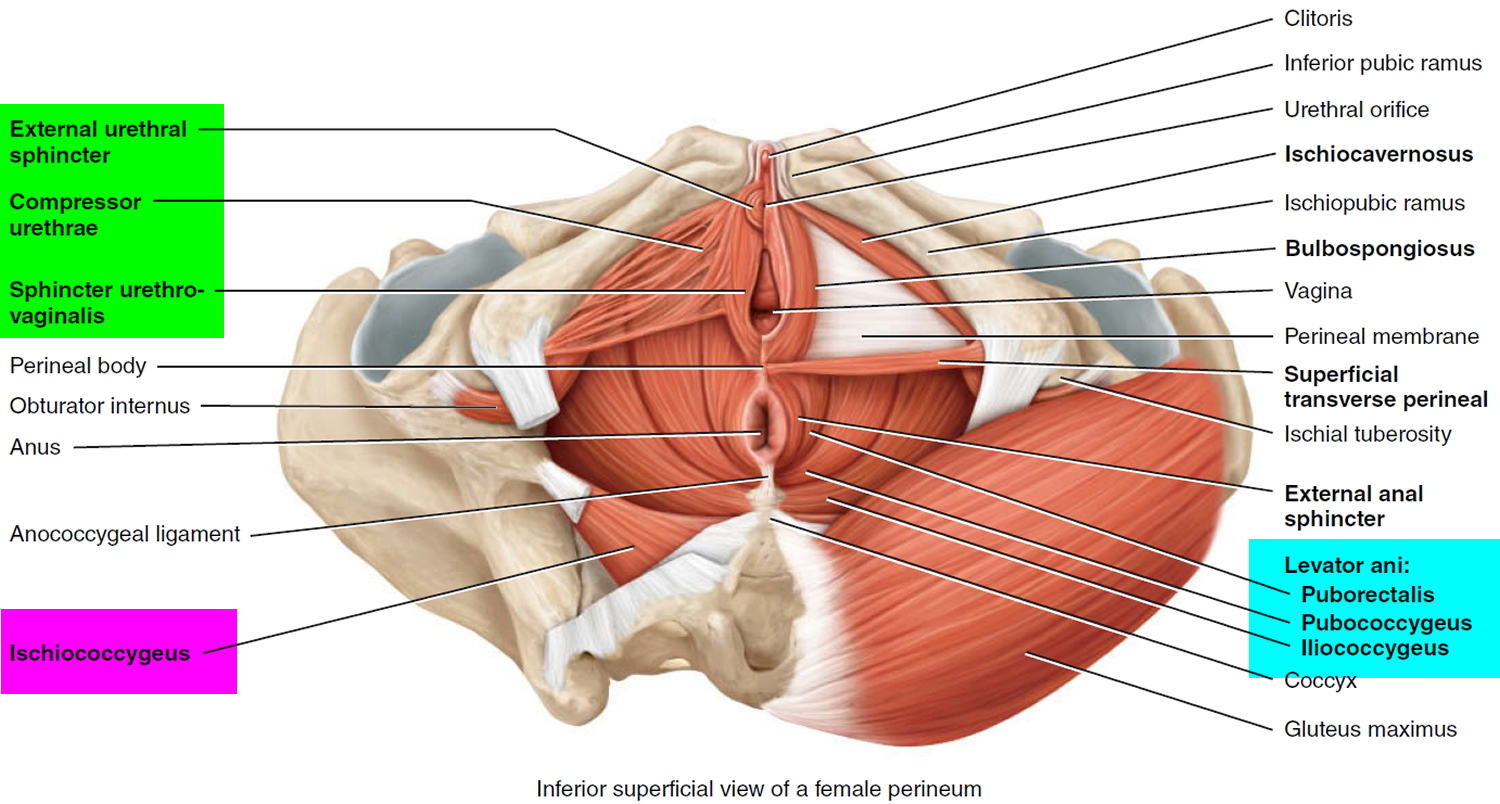
The pelvic floor is a complex layer of muscles and ligaments which stretches like a hammock from the pubic bone at the front of your pelvis to the coccyx at the bottom your spine (see Figure 3).
The muscles of the pelvic floor are the levator ani and ischiococcygeus. Along with the fascia covering their internal and external surfaces, these muscles are referred to as the pelvic diaphragm, which stretches from the pubis anteriorly to the coccyx posteriorly, and from one lateral wall of the pelvis to the other. This arrangement gives the pelvic diaphragm the appearance of a funnel suspended from its attachments. The pelvic diaphragm separates the pelvic cavity above from the perineum below. The anal canal and urethra pierce the pelvic diaphragm in both sexes, and the vagina also goes through it in females. The three components of the levator ani muscle are the pubococcygeus, puborectalis, and iliococcygeus. The levator ani is the largest and most important muscle of the pelvic floor. It supports the pelvic viscera and resists the inferior thrust that accompanies increases in intraabdominal pressure during functions such as forced exhalation, coughing, vomiting, urination, and defecation. The muscle also functions as a sphincter at the anorectal junction, urethra, and vagina. In addition to assisting the levator ani, the ischiococcygeus pulls the coccyx anteriorly after it has been pushed posteriorly during defecation or childbirth.
Figure 1. Pelvic cavity
Figure 2. Female reproductive system
Figure 3. Pelvic floor female
Pelvic organ prolapse stages
There are different types of prolapse depending on which organ is bulging into the vagina. The uterus, bladder, or rectum may be involved. It is common to have more than one type of prolapse at the same time.
The 4 main types of prolapse are:
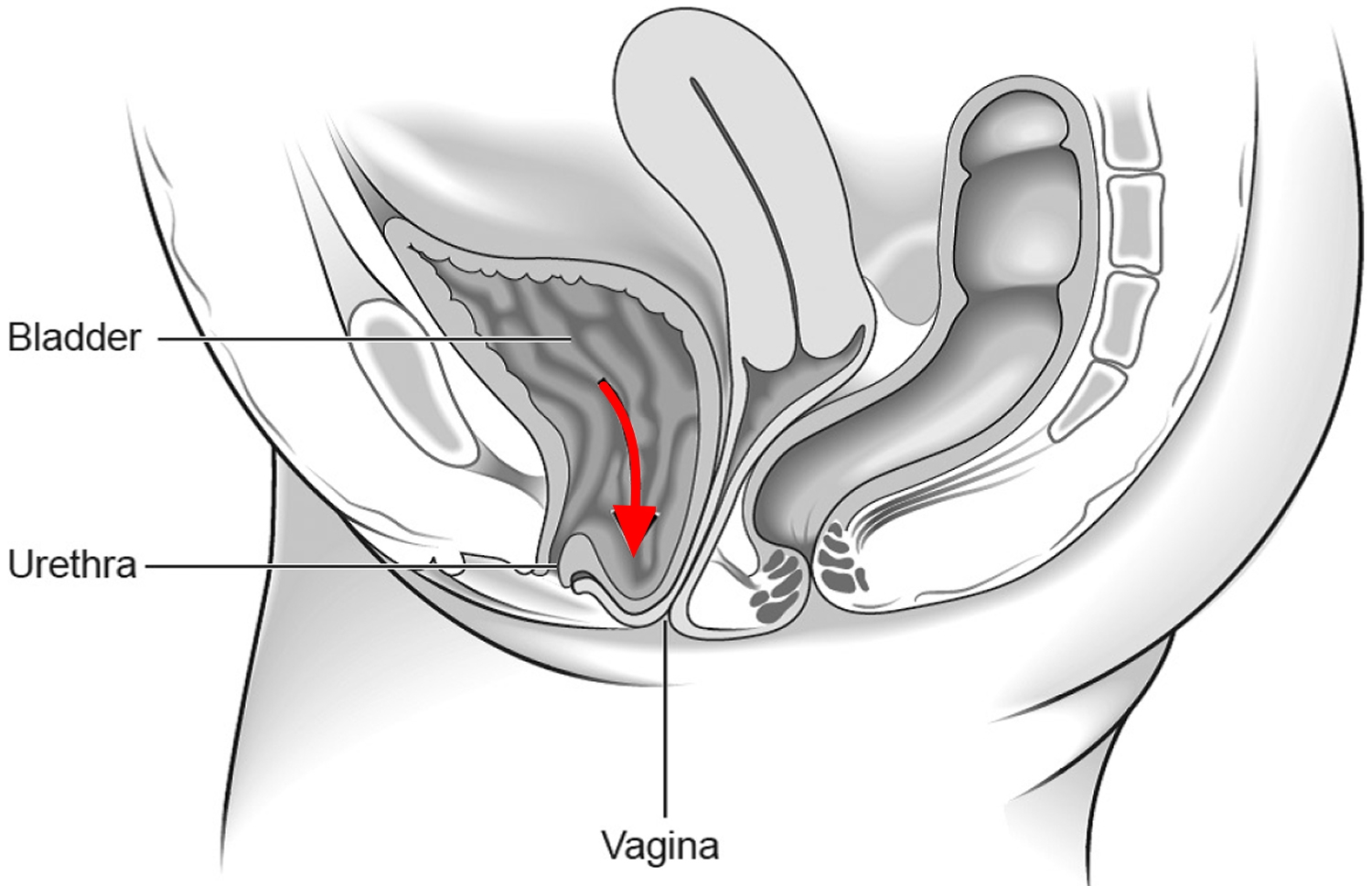
- The urinary bladder bulging into the front wall of the vagina (anterior prolapse). Anterior wall prolapse (cystocele) – when the bladder bulges into the front wall of the vagina (see Figure 4).
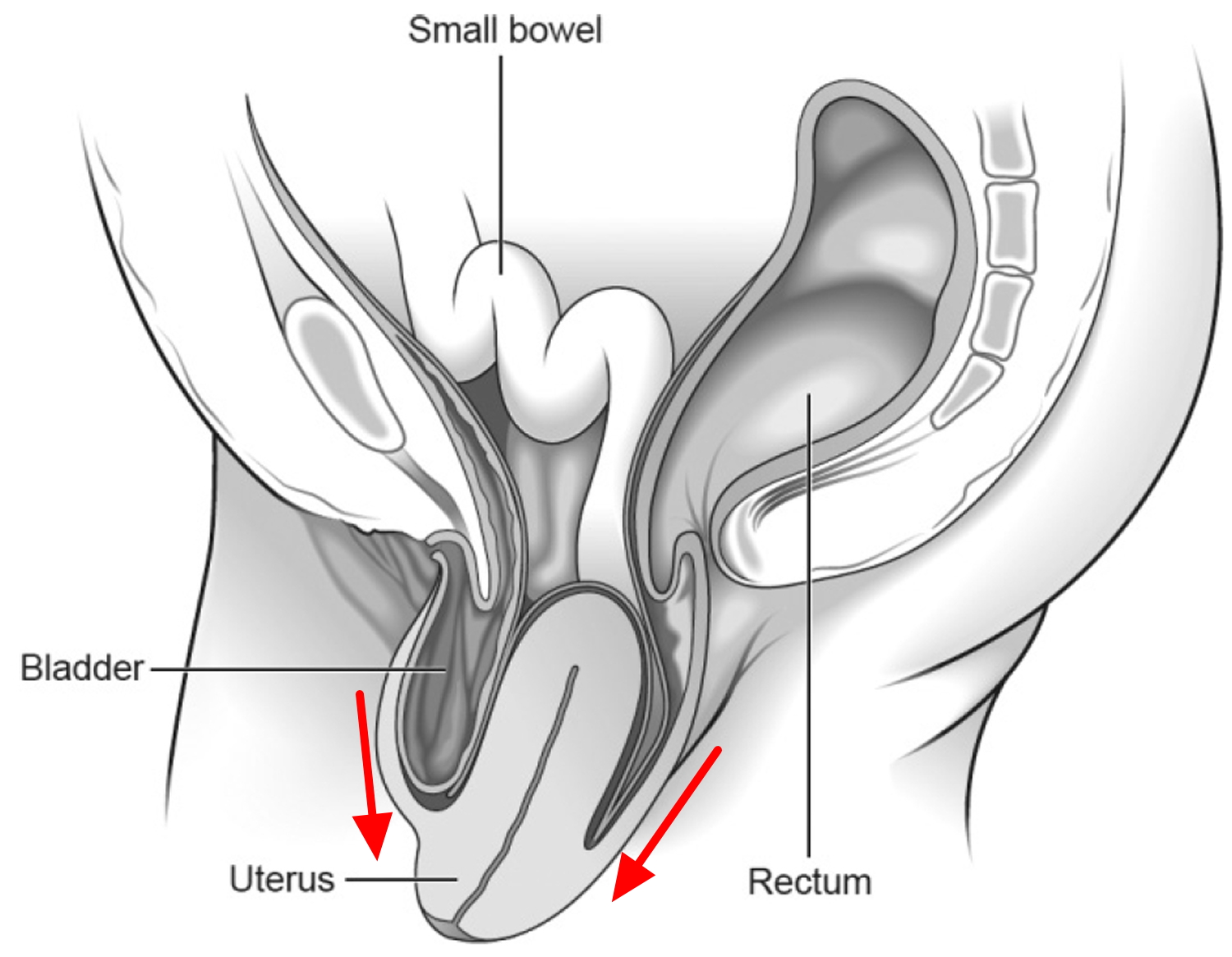
- The womb bulging or hanging down into the vagina (uterine prolapse) (see Figure 5).
- The top of the vagina (vault) sagging down (vault prolapse) – this happens to one in ten women who have had a hysterectomy to treat their original prolapse.
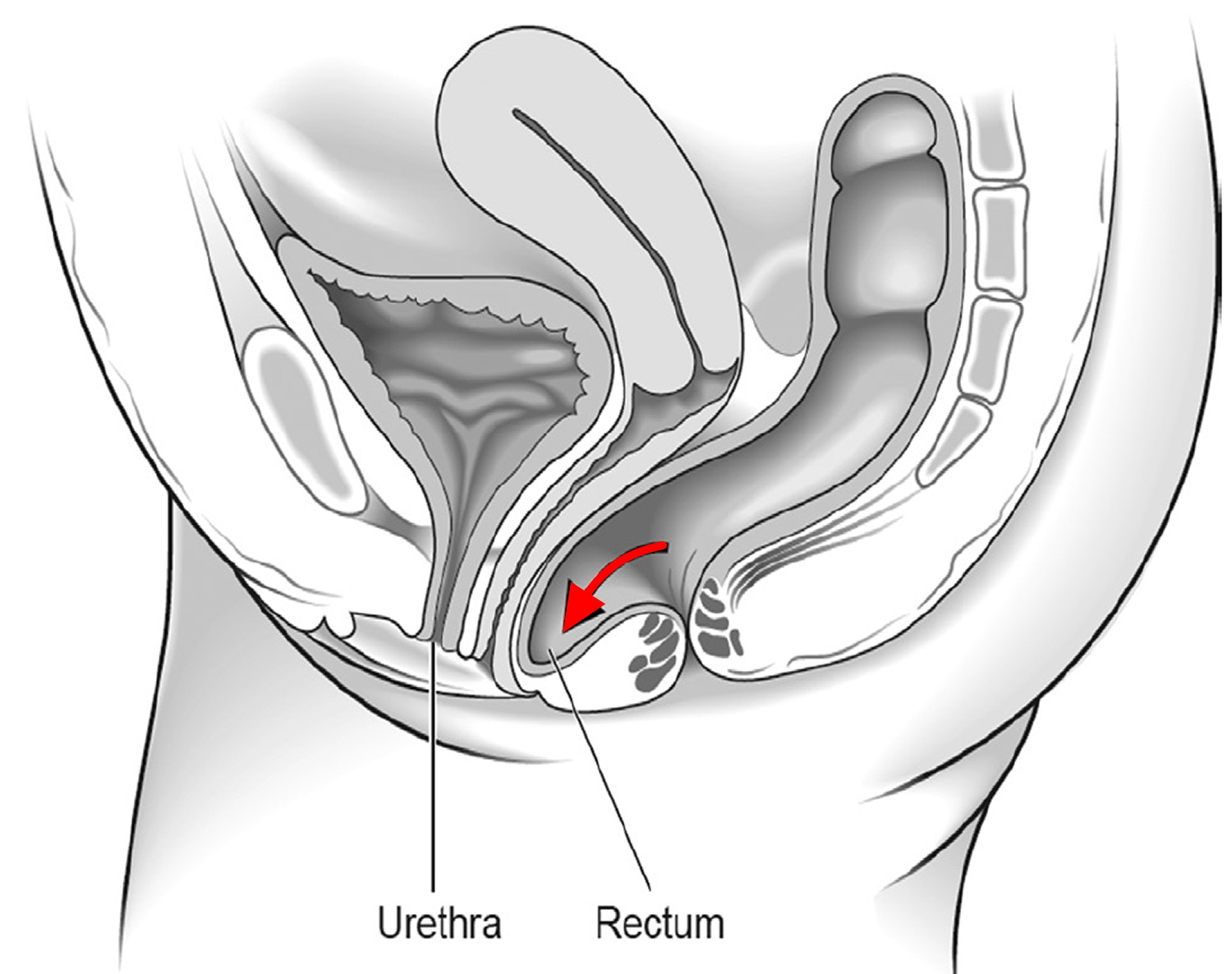
- The bowel (rectum) bulging forward into the back wall of the vagina (posterior wall prolapse) (see Figure 6)
It’s possible to have more than one of these at the same time.
Pelvic organ prolapse will usually be classified on a scale of 1 to 4 to show how severe it is, with 4 being a severe prolapse.
Figure 4. Anterior wall prolapse (cystocele)
Figure 5. Uterine prolapse – this third-degree uterine prolapse (procidentia)
Figure 6. Posterior wall prolapse
Pelvic organ prolapse causes
Pelvic organ prolapse happens when the group of muscles and tissues that normally support the pelvic organs, called the pelvic floor, becomes weakened and can’t hold the organs in place firmly.
A number of things can weaken your pelvic floor and increase your chance of developing pelvic organ prolapse, including:
- pregnancy and childbirth – especially if you had a long, difficult birth, or if you gave birth to a large baby or multiple babies
- getting older and going through the menopause
- being overweight or obese
- having long-term constipation or a long-term condition that causes you to cough and strain
- having a hysterectomy
- a job that requires a lot of heavy lifting
Some health conditions can also make a prolapse more likely, including:
- joint hypermobility syndrome
- Marfan syndrome
- Ehlers-Danlos syndromes
Pelvic organ prolapse symptoms
Your symptoms will depend on the type and severity of your pelvic organ prolapse.
Sometimes pelvic organ prolapse has no symptoms and is found during an internal examination carried out for another reason, such as cervical screening.
- The most common symptom is the sensation of a lump ‘coming down’ – feeling like there is something coming down into your vagina – it may feel like sitting on a small ball.
- You may also have had backache, heaviness or a dragging discomfort inside your vagina. These symptoms are often worse if you have been standing (or sitting) for a long time or at the end of the day. These symptoms often improve on lying down.
- You may be able to feel or see a lump or bulge in or coming out of your vagina. You should see your doctor if this is the case because the prolapse may become sore, ulcerated or infected.
- If your bladder has prolapsed into the vagina, you may:
- experience the need to pass urine more frequently
- have difficulty in passing urine or a sensation that your bladder is not emptying properly
- leak urine when coughing, laughing or lifting heavy objects
- have frequent urinary tract infections (cystitis).
- If your bowel is affected, you may experience low back pain, constipation or incomplete bowel emptying. You may need to push back the prolapse to allow stools to pass.
- Sex may be uncomfortable and you may also experience a lack of sensation during intercourse.
Pelvic organ prolapse diagnosis
Your doctor will ask if she/he can do an internal pelvic examination.
For this you will need to undress from the waist down and lie back on the examination bed. Your doctor will then feel for any lumps in your pelvic area and inside your vagina. They may gently put an instrument called a speculum into your vagina to hold the walls of it open so they can see if there is a prolapse.
Sometimes they will ask you to lie on your left-hand side and examine you in that position to get a better view of the prolapse. You may also be examined standing up.
Some women may put off going to their doctor if they’re embarrassed or worried about what the doctor may find. However, the examination is important. It only takes a few minutes and is similar to having a smear test.
You can ask for this examination to be done by a female doctor and, if you like, bring someone you trust along with you for support.
Further tests
If you have problems with your bladder, your doctor may refer you to hospital for further tests. These may include:
- a urine test to look for an infection
- inserting a small tube into your bladder to look for any problems
- special bladder tests known as urodynamics.
Pelvic organ prolapse treatment
There are several treatment options available for pelvic organ prolapse.
The most suitable will depend on:
- the severity of your symptoms
- the severity of the prolapse
- your age and health
- whether you’re planning to have children in the future
If you don’t have any symptoms, or the prolapse is mild and not bothering you, you may not need medical treatment. But making some lifestyle changes will probably still help.
If the prolapse is more severe, or your symptoms are negatively affecting your daily life, there are several medical treatment options to consider, including:
- lifestyle changes, such as stopping smoking, losing weight and pelvic floor exercises
- hormone treatment
- vaginal pessaries
- surgery
The recommended treatment will depend on the type and severity of the prolapse, your symptoms and your overall health. You and your doctor will decide together what is the best option for you.
Lifestyle changes
If you don’t have any symptoms, or the prolapse is mild, making some lifestyle changes can ease your symptoms and stop the prolapse getting worse. They can also help to reduce your risk of getting a prolapse in the first place.
They include:
- doing regular pelvic floor exercises to strengthen your muscles
- maintaining a healthy weight or losing weight if you’re overweight
- eating a high-fiber diet to avoid constipation
- avoiding lifting heavy objects
- avoiding high-impact exercise, such as trampolining
- quitting smoking – it can cause coughing and make the prolapse worse
Pelvic organ prolapse exercises
Pelvic floor muscle training exercises are a series of exercises designed to strengthen the muscles of the pelvic floor.
Pelvic floor muscle training exercises are recommended for:
- Women with urinary stress incontinence
- Men with urinary stress incontinence after prostate surgery
- People who have fecal incontinence
Pelvic floor muscle training exercises can help strengthen the muscles under the uterus, bladder, and bowel (large intestine). They can help both men and women who have problems with urine leakage or bowel control.
Step 1
Sit comfortably with your knees slightly apart. Imagine that you are trying to stop yourself passing wind from your bowel. To do this, you must squeeze the muscle around the back passage. Try lifting and squeezing the muscle as if you have wind. You should be able to feel the muscle move and your buttocks or legs should not move at all. You should notice that the skin around your back passage tightens up and creates the sensation of lifting you from your chair.
Step 2
Imagine that you are sitting on the toilet to pass urine and try to stop yourself from producing a stream of urine. You should be using the same group of muscles that you used before but you will find this a little more difficult. Do not try to stop the urinary stream when you are actually passing water because it can cause problems with bladder emptying.
Step 3
Try to tighten the muscles around your back passage and vagina, by lifting up inside as if you are trying to stop passing wind and urine at the same time. Do not tense your abdomen, squeeze your legs together, tighten your buttocks or hold your breath. If you can master this, most of the muscle contraction should be coming from the pelvic floor.
To perform pelvic organ prolapse exercises:
- Begin by emptying your bladder.
- Tighten (contract) your pelvic floor muscles as though you were trying to prevent urinating or passing gas.
- Hold the contraction for five seconds, and then relax for five seconds. If this is too difficult, start by holding for two seconds and relaxing for three seconds.
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three to five sets of 10 repetitions each day (morning, afternoon, and night).
Because these muscles control the bladder, rectum, and vagina, the following tips may help:
- Insert a finger into your vagina. Tighten the muscles as if you are holding in your urine, then let go. You should feel the muscles tighten and move up and down.
It is very important that you keep the following muscles relaxed while doing pelvic floor muscle training exercises:
- Abdominal
- Buttocks (the deeper, anal sphincter muscle should contract)
- Thigh
A pelvic floor muscle training exercise is like pretending that you have to urinate, and then holding it. You relax and tighten the muscles that control urine flow. It is important to find the right muscles to tighten.
The next time you have to urinate, start to go and then stop. Feel the muscles in your vagina, bladder, or anus get tight and move up. These are the pelvic floor muscles. If you feel them tighten, you have done the exercise right.
You can do these exercises at any time and place. Most people prefer to do the exercises while lying down or sitting in a chair. After 4 to 6 weeks, most people notice some improvement. It may take as long as 3 months to see a major change.
After a couple of weeks, you can also try doing a single pelvic floor contraction at times when you are likely to leak (for example, while getting out of a chair).
How do you practice the exercises?
You need to develop two types of muscle activity, slow and fast.
- to practice slow contractions
- do the exercises above and try to hold the pelvic floor tight for up to ten seconds. Rest for four seconds and then repeat the contraction as many times as you can, up to a maximum of ten
- to practice quick contractions
- draw the pelvic floor rapidly upwards and hold this for one second. Repeat up to a maximum of ten times. This will protect you against sudden leakage during coughing, laughing or exercise
- Aim to do one set of slow contractions followed by one set of fast contractions up to six times a day. Do not over-do it or the muscles will get tired. The exercises can be performed standing, sitting or lying down but you may find it easier at first to do them sitting down.
Other things that help
- Get into the habit of doing your exercises regularly and linking them to everyday activities e.g. do them after emptying your bladder, while answering the telephone, standing in a queue or whenever you turn on a tap
- If you are not sure you are doing the exercises correctly, insert a thumb or two fingers into the vagina and try the exercises; you should feel a gentle squeeze as the muscles contract
- Use the pelvic floor exercises to prevent leakage before you do anything which might make you leak; this way, your control will gradually improve
- Drink normally – six to eight cups (two litres) per day – avoiding caffeine and alcohol if you can
- Avoid going to the toilet “just in case”; go only when you feel that your bladder is full
- Watch your weight; extra weight puts more strain on your pelvic floor muscles and your bladder
- Avoid constipation. Straining can put excessive pressure on your bladder and bowels
- Pelvic floor exercises take three to six months to produce maximum benefit, but you should continue them for life to prevent problems recurring or worsening; you should seek help from a health professional there is little or no change in your symptoms after exercising for three months
- Other methods which help some women include weighted vaginal cones, biofeedback and electrical stimulation; consult your doctor, urologist or specialist nurse for more details
A word of caution: Some people feel that they can speed up the progress by increasing the number of repetitions and the frequency of exercises. However, over-exercising can instead cause muscle fatigue and increase urine leakage.
If you feel any discomfort in your abdomen or back while doing these exercises, you are probably doing them wrong. Breathe deeply and relax your body when you do these exercises. Make sure you are not tightening your stomach, thigh, buttock, or chest muscles.
When done the right way, pelvic floor muscle exercises have been shown to be very effective at improving urinary continence.
If you are still not sure whether you are tightening the right muscles, keep in mind that all of the muscles of the pelvic floor relax and contract at the same time.
A woman can also strengthen these muscles by using a vaginal cone, which is a weighted device that is inserted into the vagina. Then you try to tighten the pelvic floor muscles to hold the device in place.
Pelvic organ prolapse exercises may be most successful when they’re taught by a physical therapist and reinforced with biofeedback. If you are unsure whether you are doing the pelvic floor muscle training correctly, you can use biofeedback and electrical stimulation to help find the correct muscle group to work.
- Biofeedback is a method of positive reinforcement. Electrodes are placed on the abdomen and along the anal area. Some therapists place a sensor in the vagina in women or anus in men to monitor the contraction of pelvic floor muscles.
- A monitor will display a graph showing which muscles are contracting and which are at rest. The therapist can help find the right muscles for performing pelvic floor muscle training exercises.
There are physical therapists specially trained in pelvic floor muscle training. Many people benefit from formal physical therapy.
How can exercising the pelvic floor muscles help?
Exercising the pelvic floor muscles can strengthen them so that they provide the support you need. This will improve your bladder control and improve, or even stop, leakage of urine. Like all other muscles in the body, the more you use and exercise them, the stronger they become and stay.
Research suggests women who complete pelvic floor muscle training experience fewer leaking episodes and report a better quality of life.
In men, some studies have shown pelvic floor muscle training can reduce urinary incontinence, particularly after surgery to remove the prostate gland.
Hormone (estrogen) treatment
If you have a mild prolapse and have been through the menopause, your doctor may recommend treatment with the hormone estrogen to ease some of your symptoms, such as vaginal dryness or discomfort during sex.
Estrogen is available as:
- a cream you apply to your vagina
- a tablet you insert into your vagina
Vaginal pessaries
A device made of rubber (latex) or silicone is inserted into the vagina and left in place to support the vaginal walls and pelvic organs. Vaginal pessaries allow you to get pregnant in the future.
They can be used to ease the symptoms of moderate or severe prolapses and are a good option if you can’t or would prefer not to have surgery.
Vaginal pessaries come in different shapes and sizes depending on your need. The most common is called a ring pessary. You may need to try a few different types and sizes to find the one that works best for you.
A gynecologist (a specialist in treating conditions of the female reproductive system) or a specialist nurse usually fits a pessary. It may need to be removed, cleaned and replaced regularly.
Side effects of vaginal pessaries
Vaginal pessaries can occasionally cause:
- unpleasant smelling vaginal discharge, which could be a sign of an imbalance of the usual bacteria found in your vagina (bacterial vaginosis)
- some irritation and sores inside your vagina, and possibly bleeding
- stress incontinence, where you pass a small amount of urine when you cough, sneeze or exercise
- a urinary tract infection
- interference with sex – but most women can have sex without any problems
These side effects can usually be treated.
Pelvic organ prolapse surgery
If non-surgical options have not worked or the prolapse is more severe, surgery may be an option.
There are several different surgical treatments for pelvic organ prolapse. Your doctor will discuss the benefits and risks of different treatments, and you will decide together which is best for you.
No operation can be guaranteed to cure your prolapse, but most offer a good chance of improving your symptoms. The benefits of some last longer than others.
About 25–30 out of 100 women having surgery for prolapse will develop another prolapse in the future. There is a higher chance of the prolapse returning if you are overweight, constipated, have a chronic cough or undertake heavy physical activities. Prolapse may occur in another part of the vagina and may need repair at a later date.
Surgical repair
There are several different types of surgery that involve lifting and supporting the pelvic organs. This could be by stitching them into place or supporting the existing tissues to make them stronger.
Surgical repairs are usually done by making cuts (incisions) in the wall of the vagina under general anesthetic. This means you’ll be asleep during the operation and won’t feel any pain.
You may need 6 to 12 weeks off work to recover, depending on the type of surgery you have.
If you would like to have children in the future, your doctors may suggest delaying surgery until you’re sure you no longer want to have any more because pregnancy can cause the prolapse to happen again.
A pelvic floor repair if you have prolapse of the anterior or posterior walls of the vagina (cystocele or rectocele); this is where the walls of your vagina are tightened up to support the pelvic organs. This is usually done through your vagina so you do not need a cut in your abdomen. In recent years a number of new operations have been developed where mesh (supporting material) is sewn into the vaginal walls. The risks and benefits of mesh are unclear and it is currently recommended that operations using mesh are only performed as part of an audit.
Sacrocolpopexy or sacrospinous fixation. Operations that aim to lift up and attach your uterus or vagina to a bone towards the bottom of your spine or a ligament within your pelvis. These may be done by keyhole surgery.
Hysterectomy
For women with a prolapsed womb who have been through the menopause or don’t wish to have any more children, a doctor may recommend surgery to remove the womb (a hysterectomy).
It can help to relieve pressure on the walls of the vagina and reduce the chance of a prolapse returning.
You can’t get pregnant after having a hysterectomy, and sometimes it may cause you to go through the menopause early.
You may need 6 to 12 weeks off work to recover.
Closing the vagina
Occasionally, an operation that closes part or all the vagina (colpocleisis) may be an option.
This treatment is only offered to women who have advanced prolapse, when other treatments haven’t worked and they are sure they don’t plan on having sexual intercourse again in the future.
This operation can be a good option for frail women who wouldn’t be able to have more complex surgery.
Pelvic organ prolapse surgery complications
Your surgeon will explain the risks of your surgery in more detail, but possible side effects could include:
- risks associated with anesthesia
- bleeding, which may require a blood transfusion
- damage to the surrounding organs, such as your bladder or bowel
- an infection – you may be given antibiotics to take during and after surgery to reduce the risk
- changes to your sex life, such as discomfort during intercourse – but this should improve over time
- vaginal discharge and bleeding
- experiencing more prolapse symptoms, which may require further surgery
- a blood clot forming in one of your veins (deep vein thrombosis), such as in your leg – you may be given medication to help reduce this risk after surgery
If you experience any of the following symptoms after your surgery, let your surgeon or doctor know as soon as possible:
- a high temperature (fever) of 100.4 °F (38 °C) or more
- severe pain low in your tummy
- heavy vaginal bleeding
- a stinging or burning sensation when you pass urine
- abnormal vaginal discharge – this may be an infection.
Pelvic organ prolapse surgery recovery time
You will probably need to stay in hospital overnight or for a few days following surgery.
You may have a drip in your arm to provide fluids, and a thin plastic tube (catheter) to drain urine from your bladder. Some gauze may be placed inside your vagina to act as a bandage for the first 24 hours, which may be slightly uncomfortable.
For the first few days or weeks after your operation, you may have some vaginal bleeding similar to a period, as well as some vaginal discharge. This may last 3 or 4 weeks. During this time, you should use sanitary towels rather than tampons.
Your stitches will usually dissolve on their own after a few weeks.
You should try to move around as soon as possible but with good rests every few hours.
You should be able to have a shower and bathe as normal once you’ve left hospital, but you may need to avoid swimming for a few weeks.
It’s best to avoid having sex for around 4 to 6 weeks, until you’ve healed completely. Generally speaking, you should avoid heavy lifting after surgery and avoid sexual intercourse for 6–8 weeks.
Your care team will advise about when you can return to work.
Use of vaginal mesh
Surgical repair for pelvic organ prolapse may not always be successful, and the prolapse can return.
For this reason, synthetic (non-absorbable) and biological (absorbable) meshes were introduced to support the vaginal wall and/or internal organs.
Most women treated with mesh respond well to this treatment. But the Medicines and Healthcare products Regulatory Agency has received reports of complications associated with meshes. These include:
- long-lasting pain
- incontinence
- constipation
- sexual problems
- mesh exposure through vaginal tissues and occasionally injury to nearby organs, such as the bladder or bowel
The National Institute for Health and Care Excellence has recently published new guidance stating that mesh should only be used for the treatment of pelvic organ prolapse under research circumstances. If you join a research study, the National Institute for Health and Care Excellence recommends that you’re regularly monitored for any complications.
If you’re thinking about having vaginal mesh inserted, you may want to ask your surgeon some of these questions before you proceed:
- what are the alternatives?
- what are the chances of success with the use of mesh versus use of other procedures?
- what are the pros and cons of using mesh, and what are the pros and cons of alternative procedures?
- what experience have you had with implanting mesh?
- how successful has it been for the people you have treated?
- what has been your experience in dealing with any complications?
- what if the mesh doesn’t correct my problems?
- if I have a complication related to the mesh, can it be removed and what are the consequences associated with this?
- what happens to the mesh over time?
If you’ve recently had vaginal mesh inserted and think you’re experiencing complications, or you want to find out about the risks involved, speak to your doctor.