Contents
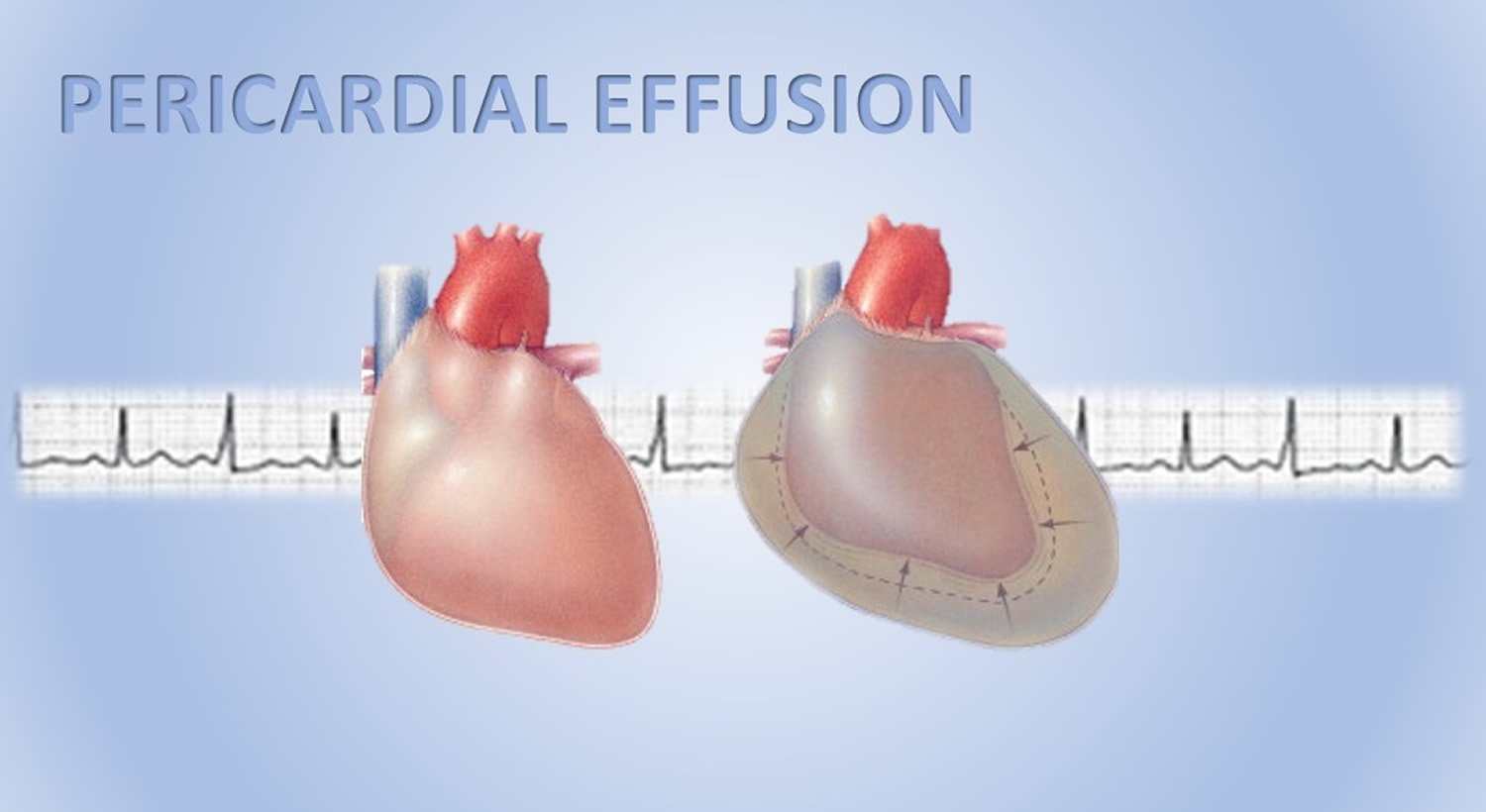
What is pericardial effusion
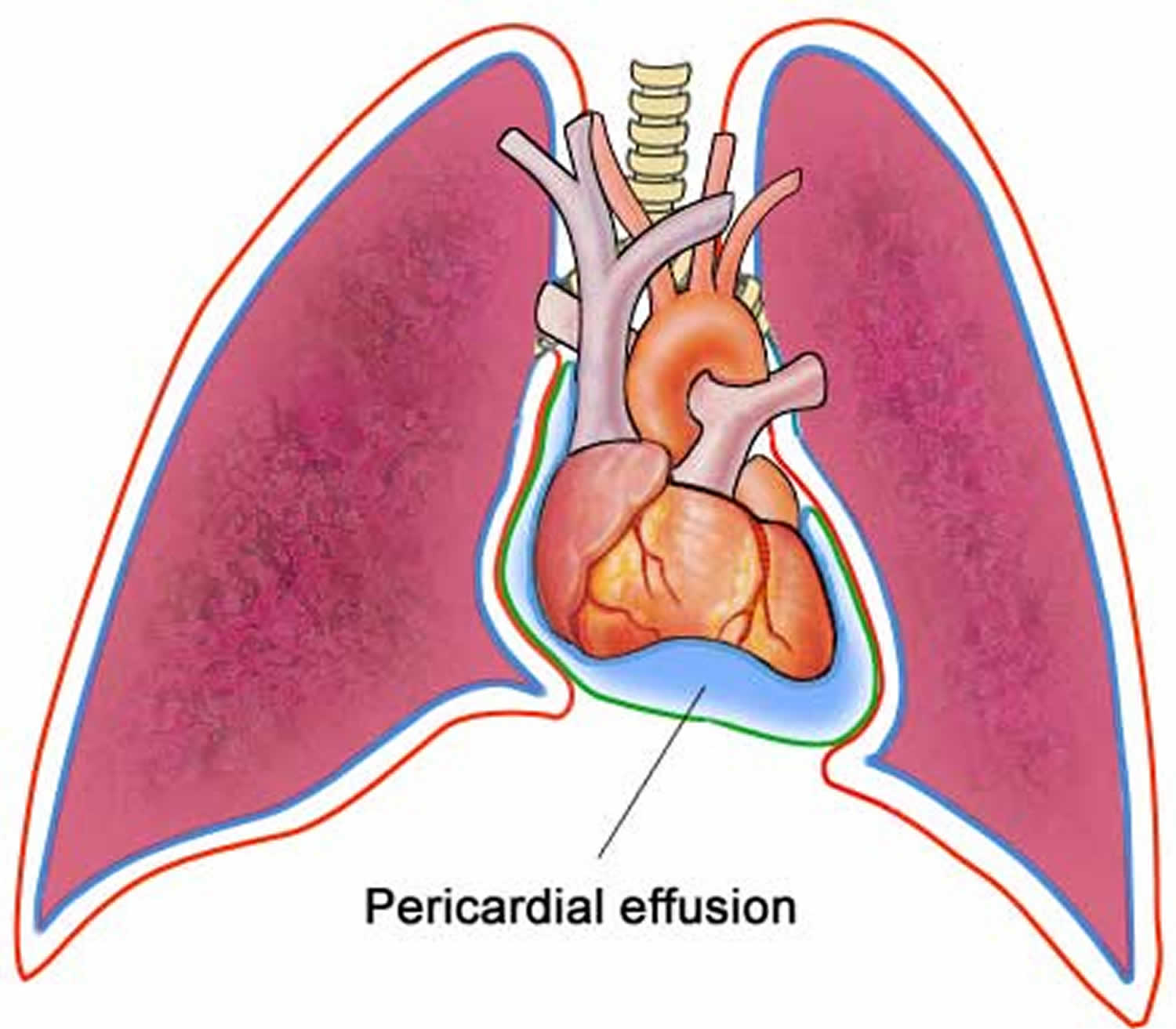
Pericardial effusion is the accumulation of too much fluid in the double-layered, sac-like structure around the heart (pericardium) -the space between the myocardium (heart muscle) and the pericardium (the outer covering sac of the heart).
The space between the layers normally contains a thin layer of fluid. But if the pericardium is diseased or injured, the resulting inflammation can lead to excess fluid. Fluid can also build up around the heart without inflammation, such as from bleeding after a chest trauma.
Pericardial effusion puts pressure on your heart, affecting the heart’s function. If untreated, pericardial effusion can lead to heart failure or death.
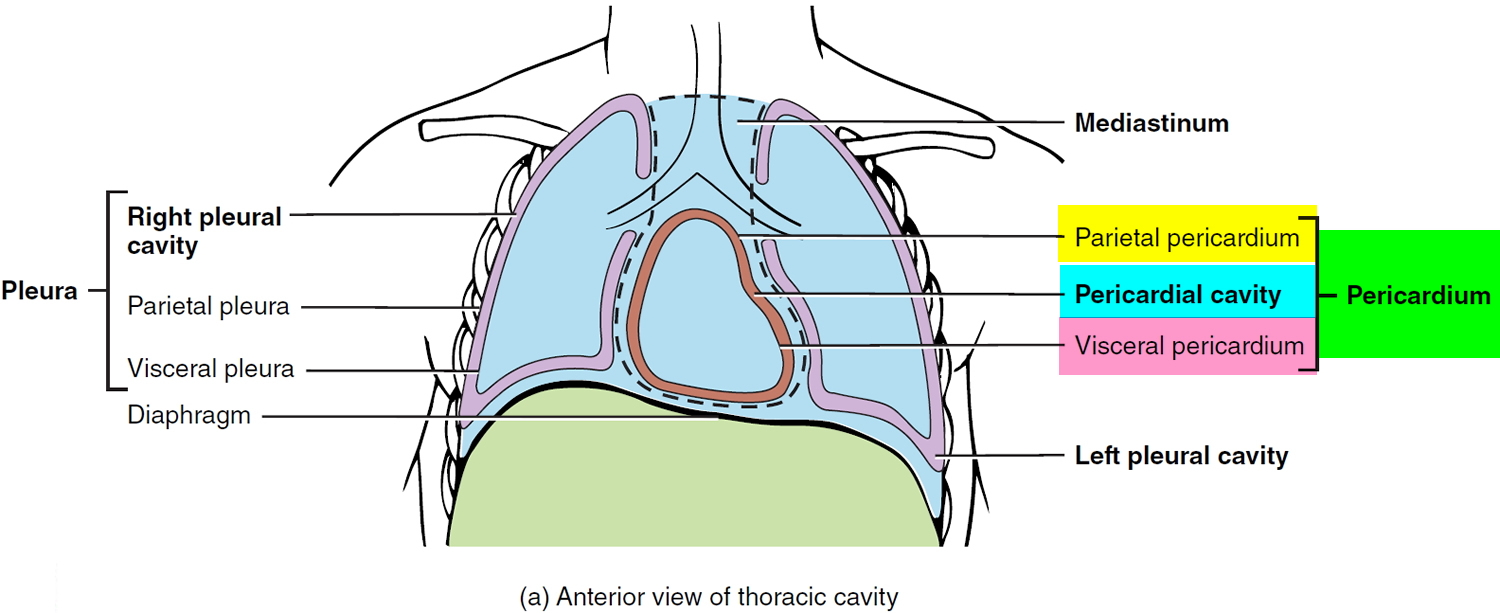
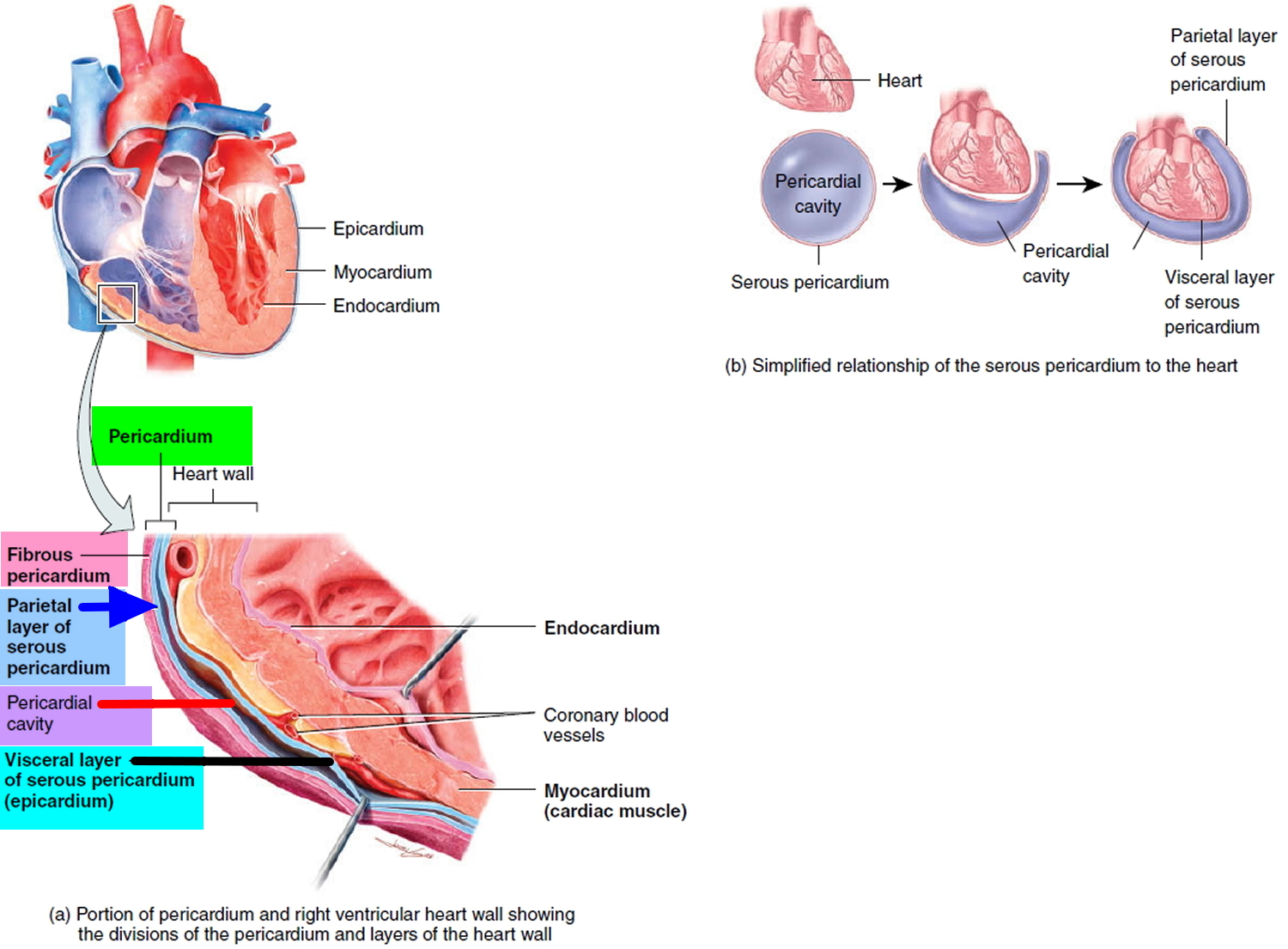
The pericardium
The pericardium is a thin double layered sac which encloses the heart. The inner layer is called the visceral pericardium. This is thin and watery in constitution. The outer layer is called the parietal layer – a tougher layer attached to other body organs like the diaphragm and cartilages between the ribs. Between the visceral and parietal pericardium is the pericardial cavity, filled with a small amount of lubricating serous fluid (see Figure 1).
Fluid is contained within the layers (in an area called the pericardial space) and lubricates the two surfaces which constantly rub together. The space between these two inner layers is the pericardial cavity and normally contains a small amount of fluid (20-50 ml , which serves as lubricant between the visceral and the parietal pericardial layers) 1. When fluid builds up slowly, more than 2000mls can be accompanied in the space, before any changes are noticed.
If the fluid builds up quickly, as little as 200mls can trigger decompensation of the heart. Increased fluid results in increased pressure, which can decrease the efficiency of the heart’s pumping mechanisms and lower the body’s blood pressure.
Figure 1. Pericardium
Figure 2. Pericardium, pericardial cavity and heart wall
Figure 3. Pericardial effusion
Pericardial effusion complications
Depending on how quickly pericardial effusion develops, the pericardium can stretch somewhat to accommodate the excess fluid. However, too much fluid causes the pericardium to put pressure on the heart, which keeps the chambers from filling completely.
This condition, called tamponade, results in poor blood circulation and an inadequate supply of oxygen to the body. Tamponade is life-threatening and requires emergent/urgent attention.
Pericardial effusion vs cardiac tamponade
Cardiac tamponade is the compression of the heart caused by pericardial effusion. This is a medical emergency, with increasing fluid producing elevated pressures on the heart and preventing proper filling. If left untreated, the heart’s pumping chambers (ventricles) are compromised, resulting in shock and death.
Cardiac tamponade (clinical tamponade) is the most severe manifestation of hemodynamic compromise caused by a tense pericardial effusion (Figure 5). The picture is easily recognized through the presence of the typical findings of dyspnea, tachycardia, jugular venous distension, pulsus paradoxus, and in the more severe cases arterial hypotension and even shock.
Most pericardial effusions cause abnormalities in hemodynamic parameters as measured in the catheterization lab. Some of these patients have echocardiographic findings of tamponade, while only a relative minority of these patients have overt clinical tamponade. Therefore, clinical tamponade represents the highest degree of severity in the spectrum of hemodynamic compromise caused by pericardial effusion.
Figure 5. Pericardial effusion and cardiac tamponade – grading of severity of hemodynamic compromise caused by pericardial effusion.
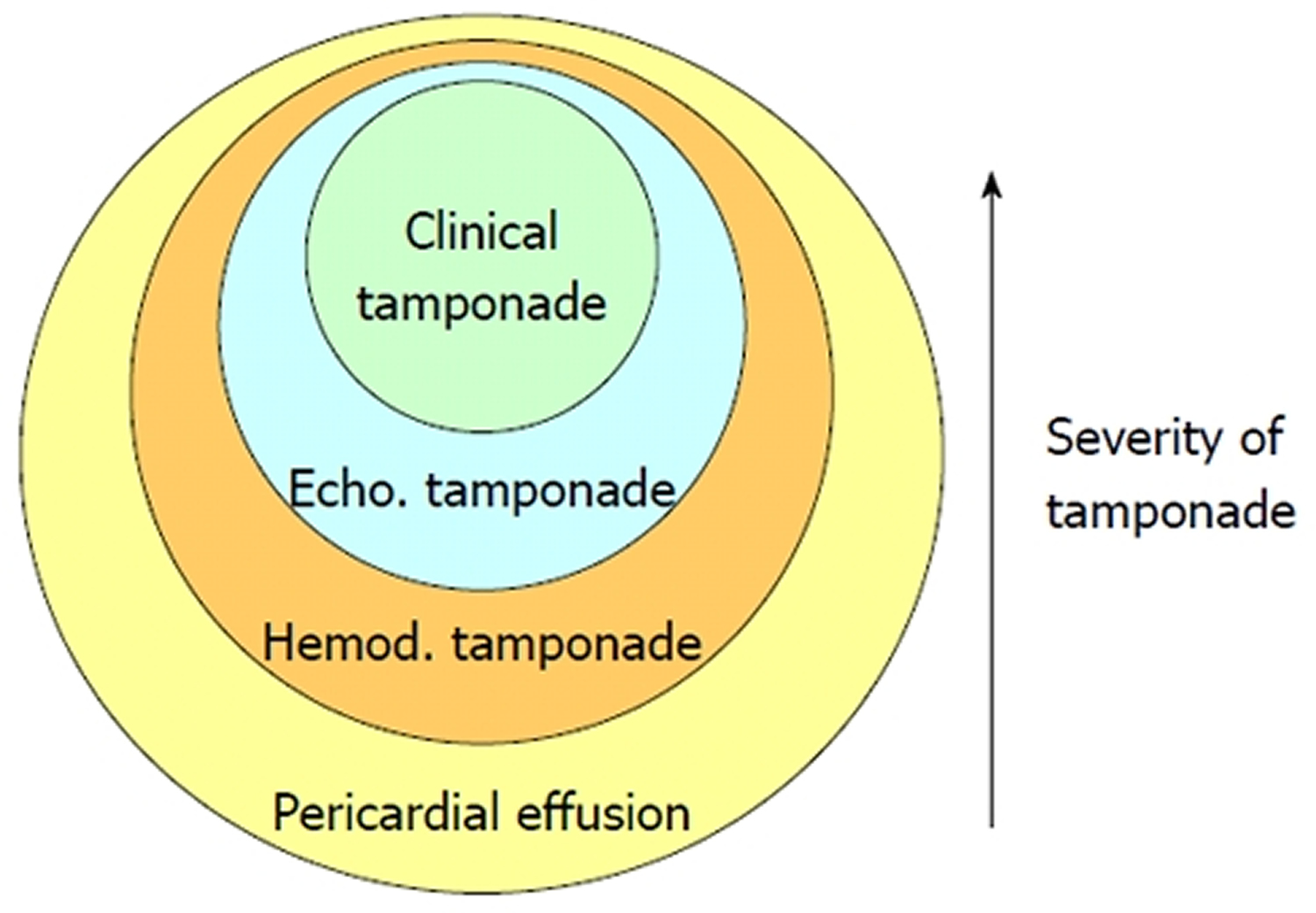 Note: Echo: Echocardiographic; Hemod: Hemodynamic. [Source 2]
Note: Echo: Echocardiographic; Hemod: Hemodynamic. [Source 2]Pericardial effusion causes
Pericardial effusion can result from inflammation of the pericardium (pericarditis) in response to illness or injury. Pericardial effusion can also occur when the flow of pericardial fluids is blocked or when blood accumulates within the pericardium, such as from a chest trauma.
Sometimes the cause can’t be determined (idiopathic pericarditis).
What causes fluid around the heart
Causes of pericardial effusion
- Secondary to underlying known disease
- Acute myocardial infarction: Post-myocardial infarction = Dressler syndrome
- Cardiac surgery
- Inflammation of the pericardium following heart surgery or a heart attack
- Trauma or puncture wound near the heart
- Widespread known neoplasia
- Chest radiation: Radiation therapy for cancer if the heart was within the field of radiation
- Chemotherapy treatment for cancer, such as doxorubicin (Doxil) and cyclophosphamide
- End-stage renal failure
- Waste products in the blood due to kidney failure (uremia)
- Invasive cardiac procedures
- Underactive thyroid (hypothyroidism)
- Autoimmune diseases
- Viral, bacterial, fungal or parasitic infections
- Without underlying known disease
- Acute inflammatory pericarditis (infectious, autoimmune)
- Autoimmune disorders, such as rheumatoid arthritis or lupus
- Spread of cancer (metastasis), particularly lung cancer, breast cancer, melanoma, leukemia, non-Hodgkin’s lymphoma or Hodgkin’s disease
- Cancer of the pericardium or heart
- Certain prescription drugs, including hydralazine, a medication for high blood pressure; isoniazid, a tuberculosis drug; and phenytoin (Dilantin, Phenytek, others), a medication for epileptic seizures
- Idiopathic pericarditis where the cause can’t be determined
The finding of a pericardial effusion in patients with underlying malignancy creates a more complex dilemma, as not infrequently pericardial effusion is due to alternative causes and not to direct neoplastic pericardial involvement. In Posner’s series 3 malignant pericardial disease was diagnosed in 18 (58%) of 31 patients with underlying cancer and pericarditis, while 32% of the patients had idiopathic pericarditis and 10% had radiation induced pericarditis. Porte et al 4 studied 114 patients with recent or remote history of cancer and a pericardial effusion of unknown origin requiring drainage for diagnostic or therapeutic purposes. Pericardioscopy was performed in 112 patients with pericardial fluid analysis and biopsy of abnormal structures or deposits under direct visual control. Malignant pericardial disease was found in 44 (38%) patients, while 70 (61%) patients had non-malignant pericardial effusions (idiopathic in 33 patients, radiation-induced in 20 patients, infectious effusion in 10 patients, and hemopericardium as a result of coagulation disorders in 8 patients). These studies are important since they show that, in more than half of the patients with underlying cancer, a pericardial effusion is due to causes different than direct neoplastic involvement. Therefore, the precise cause of these effusions needs to be clarified, as obvious prognostic and therapeutic consequences ensue.
In the patients with no apparent cause of pericardial effusion at the time of diagnosis (40%) scientists found that the presence of inflammatory signs (characteristic chest pain, pericardial friction rub, fever or typical electrocardiographic changes) was predictive for acute idiopathic pericarditis, irrespective of the size of the effusion and the presence or absence of tamponade 2. Furthermore, severe pericardial effusion with absence of inflammatory signs and absence of cardiac tamponade was predictive for chronic idiopathic pericardial effusion and tamponade without inflammatory signs for neoplastic pericardial effusion 2.
Idiopathic chronic pericardial effusion
Most patients with a large (more than 20 mm), chronic (longer than 3 months), idiopathic pericardial effusion are asymptomatic and may remain clinically stable for many years. However, this condition may entail a less than good prognosis, as unexpected overt tamponade can develop in up to 29% of such patients 5. The trigger of tamponade is unknown, but hypovolemia, paroxysmal tachyarrhythmias, and intercurrent acute pericarditis may precipitate tamponade; accordingly, these events should be vigorously managed. Medical therapy, particularly corticosteroids, colchicine or antituberculous therapy, is not useful.
Pericardiocentesis is the first option in patients with overt tamponade. Scientists think that elective pericardial drainage has to be performed as well in asymptomatic patients as a prophylactic measure to prevent unexpected tamponade. In these patients pericardiocentesis should drain as much pericardial fluid as possible. In cases with relapsing effusion, a second pericardiocentesis is warranted. This sequence may result in definitive disappearance of chronic pericardial effusion as was the case in 8 of 19 patients with effusions present for at least 4 years 5. When a large pericardial effusion relapses after two pericardiocenteses we recommend surgical drainage with wide anterior pericardiectomy even in asymptomatic patients. In our experience this procedure is safe (no mortality has been observed) and is very effective in the long-term 5.
Risk Factors for pericardial effusion
There are many reasons why you might have a pericardial effusion.The three most common causes of pericardial effusion are malignancy, uremia (a toxic condition resulting from kidney disease due to retention in the bloodstream of waste products normally excreted in the urine), and irritation of the sac surrounding the heart, due to unknown causes.
Malignancy
If you have cancer, fluid can accumulate in the pericardial sac surrounding the heart. This fluid can build up and cause an increased pressure on the heart. Cancers can also cause bleeding into the pericardial sac. This build up of blood in a confined space can further compromise the heart.
Penetrating or Blunt Injury
A penetrating cardiac injury such as a stab wound to the chest, can result in leakage of blood into the pericardial sac (known as hemopericardium) and cause a rapid rise in the pressure around the heart.
Iatrogenic causes
Occasionally, pericardial effusion can be a result of medical interventions and procedures. These include; during central line placement, cardiac catheterization and pacemaker insertion.
Heart Attacks (Myocardial infarction)
After a heart attack, your heart muscle is weaker and more likely to rupture around the site of tissue that has sustained injury.
Infection
Pericardial effusion is often associated with pericarditis (inflammation of the pericardial sac) caused by bacterial or viral infections.
Pericardial effusion prognosis
The prognosis of pericardial effusion depends on the underlying cause 6 being especially poor in patients with neoplastic pericardial effusion secondary to lung cancer and positive cytologic study (presence of malignant cells) in pericardial fluid. Prognosis is very good in idiopathic/viral pericarditis. In patients with tuberculous or purulent pericarditis the prognosis depends on the precocity of the diagnosis and adequate treatment, but purulent pericarditis frequently occurs in patients with underlying debilitating disease (diabetes mellitus, liver cirrhosis, widespread infections). The prognosis is good in chronic idiopathic pericardial effusion but tamponade can occur.
Pericardial effusion symptoms
You can have significant pericardial effusion without signs or symptoms, particularly if the fluid has increased slowly.
If pericardial effusion symptoms do occur, they might include:
- Shortness of breath or difficulty breathing (dyspnea)
- Discomfort when breathing while lying down (orthopnea)
- Chest pain, usually behind the breastbone or on the left side of the chest
- Chest fullness
In traumatic pericardial effusion, there may be history of an obvious penetrating chest injury. In these circumstances, you may be acutely short of breath and may become confused and drifting in and out of consciousness.
If you are affected by pericardial effusion, you may also have a history of medical diseases that can involve the sac surrounding the heart, such as end-stage kidney disease.
Pericardial effusion diagnosis
If your doctor suspects you have pericardial effusion, he or she will do a series of tests to look for it, identify possible causes and determine treatment.
Medical exam
Your doctor will perform a medical exam, including listening to your heart with a stethoscope.
Echocardiogram
An echocardiogram uses sound waves to create real-time images of your heart. With this procedure, a cardiologist can see the extent of pericardial effusion based on the amount of space between the two layers of the pericardium. An echocardiogram can also show decreased heart function due to pressure on the heart (cardiac tamponade).
Your cardiologist might be able to see whether one or more chambers of the heart have collapsed and how efficiently your heart is pumping blood. There are two types of echocardiograms:
- Transthoracic echocardiogram. This test uses a sound-emitting device (transducer) that is placed on your chest over your heart.
- Transesophageal echocardiogram. A tiny transducer on a tube is put down the part of your digestive tract that runs from your throat to your stomach (esophagus). Because the esophagus lies close to the heart, having the transducer placed there often provides a more-detailed image of the heart.
Electrocardiogram
An electrocardiogram — also called an ECG or EKG — records electrical signals as they travel through your heart. Your cardiologist can look for patterns that suggest tamponade.
Chest X-ray
This can show an enlarged heart silhouette if the amount of fluid in the pericardium is large.
Other imaging technologies
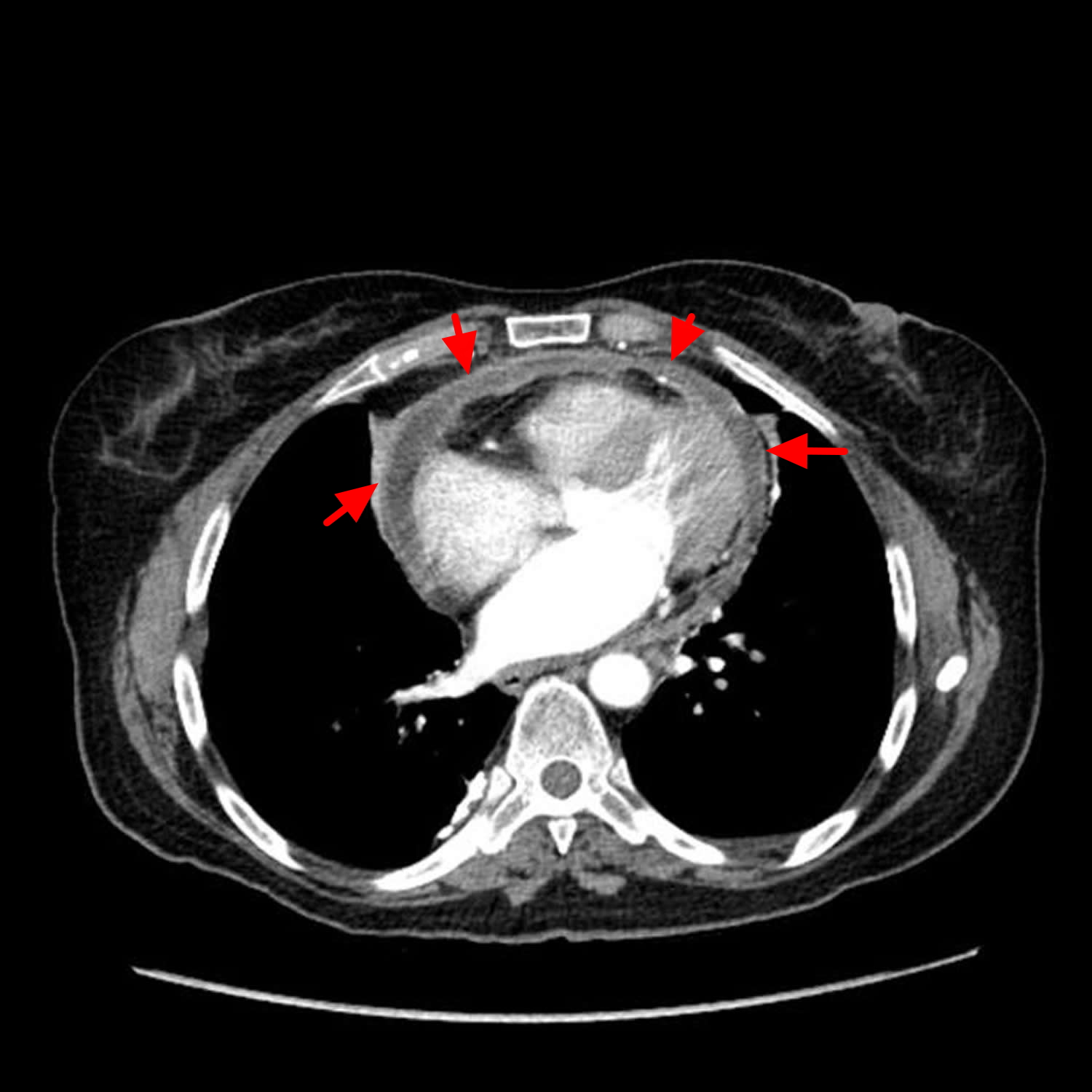
Computerized tomography (CT) scans and magnetic resonance imaging (MRI) are imaging technologies that can detect pericardial effusion, although they’re not generally used to look for the disorder. However, pericardial effusion may be diagnosed when these tests are done for other reasons.
Other tests
If there’s evidence of pericardial effusion, your doctor might order blood tests or other diagnostic tests to identify a cause.
Although echocardiography is the standard and most available method for the evaluation of pericardial effusion, CT and magnetic resonance imaging (MRI) can offer some advantages 7. These imaging techniques allow assessment of the entire chest and detection of associated abnormalities in the mediastinum, lungs and adjacent structures. CT and MRI are also less operator dependent and delineate more precisely the spacial distribution of pericardial effusion in complex pericardial collections. In addition, multidetector CT scanners and MRI may provide valuable information about the function and dynamics of the heart and pericardium. Some of the reported limitations of echocardiography are generally not present with CT, including the possibility of false-positive findings due to adjacent pathologic conditions that may simulate pericardial effusion. Another advantage of CT and MRI is the possibility of identifying hemorrhagic effusions or clots within the pericardium.
Pericardial effusion treatment
Treatment for pericardial effusion will depend on how much fluid has accumulated, what’s causing the effusion and whether you have or are likely to develop cardiac tamponade. Treating the cause of pericardial effusion often corrects the problem.
Medications that reduce inflammation
If you don’t have tamponade or there’s no immediate threat of tamponade, your doctor might prescribe one of the following to treat inflammation of the pericardium that may be contributing to pericardial effusion:
- Aspirin
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as indomethacin (Indocin) or ibuprofen (Advil, Motrin IB, others)
- Colchicine (Colcrys)
- Corticosteroid, such as prednisone
Other treatments
If anti-inflammatory treatments don’t correct the problem, if you have a large collection of fluid causing symptoms and making you more prone to tamponade, or if you have tamponade, your cardiologist will likely recommend one of the following procedures to drain fluids or prevent fluids from accumulating again.
- Drain the fluid. Your doctor can enter the pericardial space with a needle and then use a small tube (catheter) to drain fluid — a procedure called pericardiocentesis. The doctor will use imaging devices — either echocardiography or a type of X-ray technology called fluoroscopy — to guide the work. An ECG machine monitors your heart during the procedure. In most cases, the catheter will be left in place to drain the pericardial space for a few days to help prevent the fluid from building up again.
- Open heart surgery. If there’s bleeding into the pericardium, especially due to recent heart surgery or other complicating factors, you might have surgery to drain the pericardium and repair damage. Occasionally, a surgeon may drain the pericardium and create a “passage” that allows it to drain as necessary into the abdominal cavity where the fluid can be absorbed.
- Open the layers. Balloon pericardiotomy is a rarely performed procedure in which a deflated balloon is inserted between the layers of the pericardium and inflated to stretch them.
- Remove the pericardium. The surgical removal of all or part of the pericardium (pericardiectomy) is usually reserved for treatment of recurring pericardial effusions despite catheter drainage.
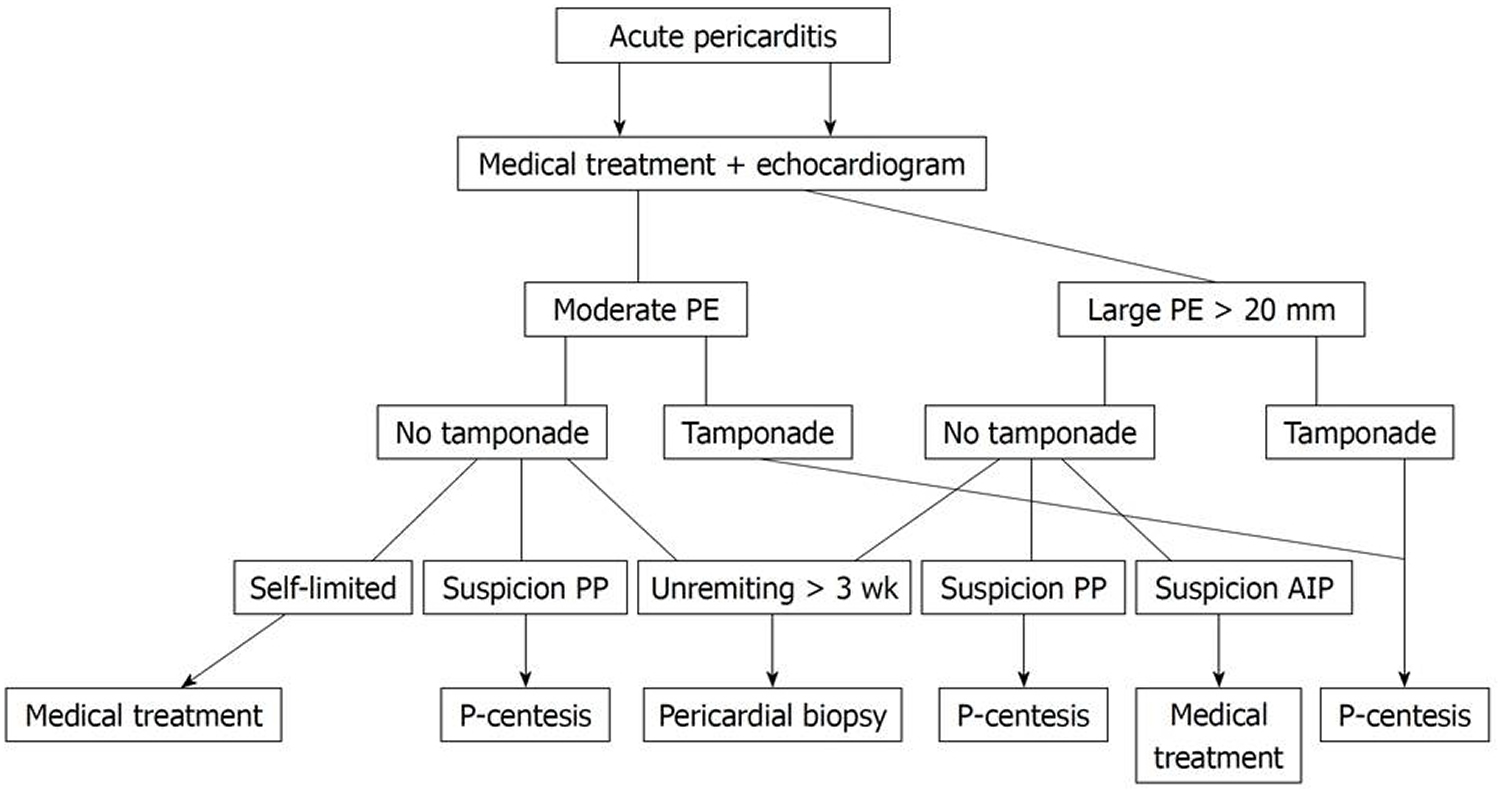
Patients with acute inflammatory signs (fever, chest pain, pericardial friction rub) should receive aspirin or non-steroid anti-inflammatory drugs. In the setting of acute inflammatory pericarditis steroids should be avoided as they increase the possibility of relapses 8. Colchicine is an established indication in patients with relapsing pericarditis 9 and has also been suggested to be useful in the first episode of acute pericarditis in order to avoid the appearance of recurrences 8. The patients with acute viral or idiopathic pericarditis can be managed on an out-of-hospital basis unless they have clinical predictors of poor prognosis (cardiac tamponade, severe pericardial effusion, immunosuppression, oral anticoagulant therapy or fever > 38°C (100.4 °F) 10. The global management of acute pericarditis is shown schematically in Figure 5. When specific cause is found (bacterial, tuberculous) the treatment should be directed against the causative agent with pericardial drainage if hemodynamic compromise is present. Strict control in the first weeks or months is necessary because of the possibility of evolution to constrictive pericarditis 11. When acute idiopathic or viral pericarditis is accompanied by moderate to severe effusion new echocardiographic controls should be performed (initially every week) until resolution of the disease. The management of neoplastic pericarditis has been excellently reviewed in this journal recently 12.
Figure 6. Proposed management strategy for patients with acute pericarditis pericardial effusion
Note: PE: Pericardial effusion; PP: Purulent pericarditis; AIP: Acute idiopathic pericarditis; P-centesis: Pericardiocentesis.
Proposed management strategy for patients with moderate or severe pericardial effusion accompanying acute pericarditis.
[Source 2]Pericardial drainage procedures can be performed for diagnostic or therapeutic purposes (patients with cardiac tamponade). In patients without hemodynamic compromise the diagnostic yield of pericardial fluid or pericardial tissue is very low 13. In a study 14, which included 71 patients with large pericardial effusion without clinical tamponade, scientists found that pericardial drainage procedures (performed in 26 patients) had a diagnostic yield of only 7%. On the other hand, no patients developed cardiac tamponade or died as a result of pericardial disease, nor did any new diagnosis become apparent in the 45 patients who did not undergo pericardial drainage initially. Furthermore, moderate or large effusions persisted in only 2 of 45 patients managed conservatively. Even patients with echocardiographic collapses rarely require pericardial drainage for therapeutic purposes during the initial admission. Therefore, pericardial drainage procedures are not justified on a routine basis in patients without hemodynamic compromise. Three exceptions to this rule should be noted. Patients with a strong suspicion of purulent or tuberculous pericarditis merit invasive pericardial procedures 2. On the other hand, in patients with underlying malignancies examination of pericardial fluid is indicated in order to determine whether the effusion is secondary to neoplastic pericardial involvement or is an epiphenomenon (non-malignant effusion) related to the management of the cancer (such as previous thoracic irradiation) or effusions of unknown origin 2. Lastly, doctors recommend pericardiocentesis in asymptomatic patients with massive idiopathic chronic pericardial effusion because some of these patients develop unexpected overt tamponade 2.
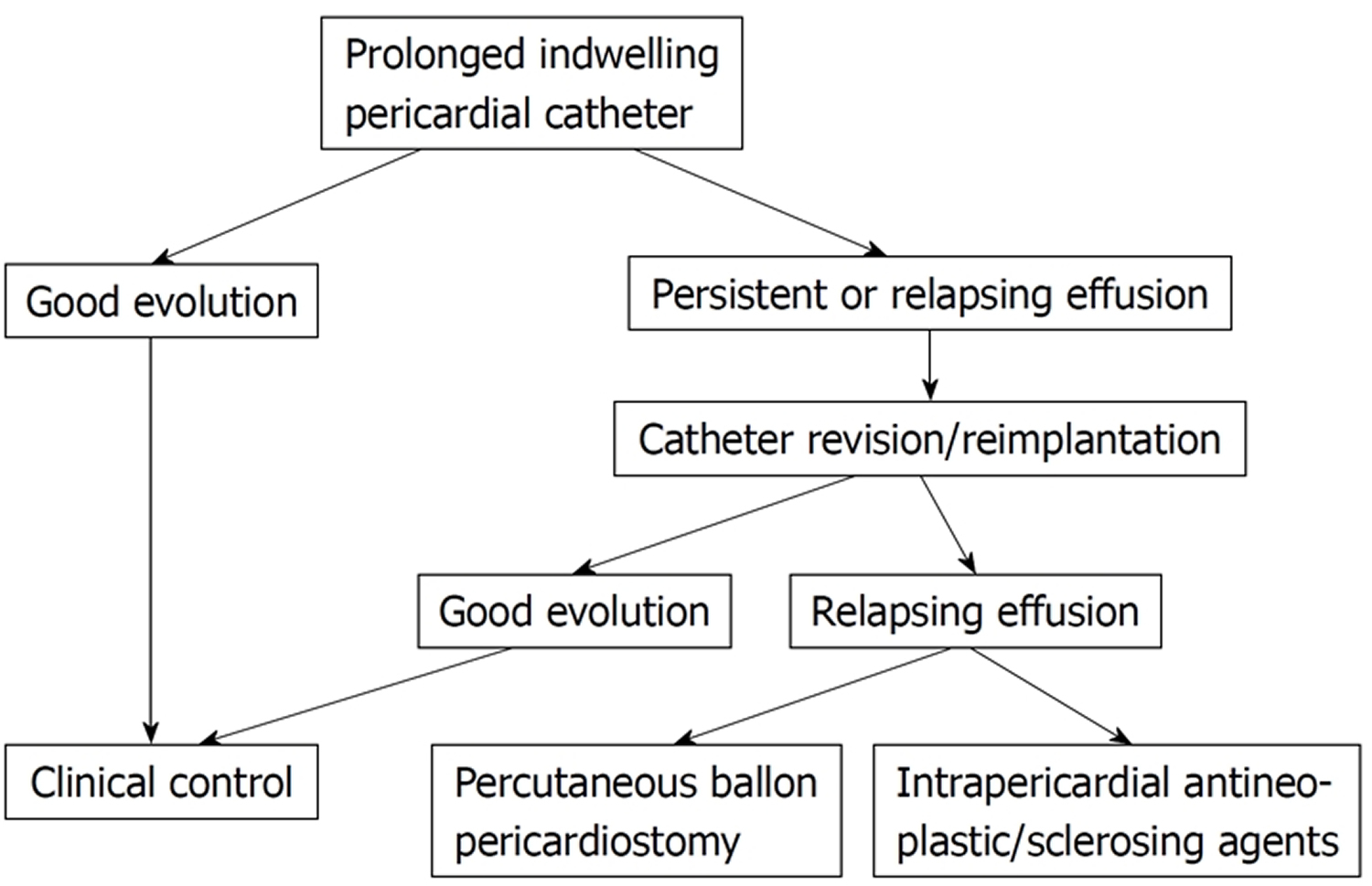
Figure 7. Proposed management strategy for patients with neoplastic pericardial effusion
[Source 2]Procedures of pericardial drainage
A variety of procedures, ranging from simple needle pericardiocentesis to open surgical drainage, are useful for pericardial drainage. The selection of a particular procedure largely depends on the etiology of the pericardial effusion. In patients with idiopathic or viral pericarditis simple pericardiocentesis is usually sufficient as the illness is self-limited in days or a few weeks and tamponade rarely relapses. Purulent pericarditis should be drained surgically, usually through subxiphoid pericardiotomy.
Selection of pericardial drainage procedures
- Pericardiocentesis only
- Indwelling pericardial catheter
- Percutaneous ballon pericardiotomy
- Subxiphoid pericardiotomy
- Pleuropericardial window
- Partial pericardiectomy
- Wide anterior pericardiectomy
The management of cardiac tamponade in patients with neoplastic pericardial involvement merits a special comment. The goals of the treatment are relief of tamponade and prevention of reaccumulation of fluid, which is frequent in these patients. As a rule, less invasive procedures should be preferred, especially in patients with advanced disease and poor general condition. Simple pericardiocentesis alleviates symptoms in most cases but pericardial effusion relapses in as many as 40%-50% of patients 15. Therefore, pericardiocentesis is the procedure of choice in terminal patients, when recurrence of effusion is not a real issue. In patients with a longer expected survival the treatment has to contemplate possible fluid reaccumulation. Indwelling pericardial catheters have a success rate (defined as alleviation of tamponade and no need of further procedures) of 75% approximately. The catheter should be maintained as long as the amount of drainage is greater than 25 mL/d. In different series 16 the duration of catheter drainage averaged 4.8 days. Catheter infection is a potential complication. The aims of a prolonged indwelling pericardial catheter are to achieve a complete pericardial drainage and to provoke adherence between the two layers of the pericardium in order to prevent recurrence of pericardial effusion. This goal can be favored by intrapericardial sclerosis with tetracycline or other agents. However, some authors 17 have observed no additional advantages over indwelling pericardial catheters and sclerosing agents can provoke “excessive” sclerosis with evolution to constrictive pericarditis with clinical repercussion. Therefore, some doctors think that instillation of sclerosing agents should be avoided in patients with relatively good life expectancy. Balloon pericardiotomy is an alternative to surgical creation of a pericardial window. Access to the pericardial space is gained via a conventional subxiphoid pericardiocentesis. A guide wire is advanced into the pericardium, and a balloon catheter is straddled across the pericardium and inflated to create a window 18. The fluid drains into the pleura or the peritoneal spaces. This technique has been especially adopted for patients with malignancy and reduced life expectancy, and it is successful in more than 80% of cases 18. Reported complications include fever, pneumothorax, left pleural effusion and bleeding from pericardial blood vessels 19.
Surgical drainage procedures should be considered in some patients. Some confusion exists about the precise surgical technique of the different procedures (complete pericardiectomy, partial pericardiectomy, subxiphoid pericardiotomy, anterior transthoracic window, pleuropericardial window) but probably all these procedures have a similar efficacy in relieving pericardial effusion (80%-90%). However, inherent perioperative risks, especially if performed under general anesthesia, are a concern. In fact, the overall 30 d mortality for surgical drainage of malignant pericardial effusion has been reported to be 19.4% 20. In general, the more complex the procedure, the higher the mortality rate.
If patients with neoplastic pericardial effusion is to begin with an indwelling pericardial catheter, this procedure can be repeated in cases of relapse. The second option would be a subxiphoid percutaneous pericardiotomy or instillation of sclerosing agents. In our experience, surgical drainage techniques are rarely required. The global management strategy is shown schematically in Figure 7 above.
Some patients show persistence of clinical findings of systemic venous hypertension after effective drainage of the pericardial effusion. In these cases, a possible component of additional constriction physiology should be suspected (“effusive-constrictive pericarditis”) 21.
- Spodick DH. The Pericardium: A Comprehensive Textbook. New York: Marcel Dekker; (1997).[↩]
- Sagristà-Sauleda J, Mercé AS, Soler-Soler J. Diagnosis and management of pericardial effusion. World Journal of Cardiology. 2011;3(5):135-143. doi:10.4330/wjc.v3.i5.135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3110902/[↩][↩][↩][↩][↩][↩][↩][↩]
- Posner MR, Cohen GI, Skarin AT. Pericardial disease in patients with cancer. The differentiation of malignant from idiopathic and radiation-induced pericarditis. Am J Med. 1981;71:407–413. https://www.ncbi.nlm.nih.gov/pubmed/7282729[↩]
- Porte HL, Janecki-Delebecq TJ, Finzi L, Métois DG, Millaire A, Wurtz AJ. Pericardoscopy for primary management of pericardial effusion in cancer patients. Eur J Cardiothorac Surg. 1999;16:287–291. https://www.ncbi.nlm.nih.gov/pubmed/10554845[↩]
- Sagristà-Sauleda J, Angel J, Permanyer-Miralda G, Soler-Soler J. Long-term follow-up of idiopathic chronic pericardial effusion. N Engl J Med. 1999;341:2054–2059. http://www.nejm.org/doi/full/10.1056/NEJM199912303412704[↩][↩][↩]
- Colombo A, Olson HG, Egan J, Gardin JM. Etiology and prognostic implications of a large pericardial effusion in men. Clin Cardiol. 1988;11:389–394. https://www.ncbi.nlm.nih.gov/pubmed/3293859[↩]
- Restrepo CS, Lemos DF, Lemos JA, Velasquez E, Diethelm L, Ovella TA, Martinez S, Carrillo J, Moncada R, Klein JS. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007;27:1595–1610. https://www.ncbi.nlm.nih.gov/pubmed/18025505[↩]
- Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005;112:2012–2016. http://circ.ahajournals.org/content/112/13/2012.long[↩][↩]
- Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25:587–610. https://www.ncbi.nlm.nih.gov/pubmed/15120056[↩]
- Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042–1046. https://www.sciencedirect.com/science/article/pii/S0735109704000038[↩]
- Sagristà-Sauleda J, Barrabés JA, Permanyer-Miralda G, Soler-Soler J. Purulent pericarditis: review of a 20-year experience in a general hospital. J Am Coll Cardiol. 1993;22:1661–1665. https://www.sciencedirect.com/science/article/pii/073510979390592O[↩]
- Lestuzzi C. Neoplastic pericardial disease: Old and current strategies for diagnosis and management. World J Cardiol. 2010;2:270–279. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2999066/[↩]
- Permanyer-Miralda G, Sagristá-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985;56:623–630. https://www.ncbi.nlm.nih.gov/pubmed/4050698[↩]
- Mercé J, Sagristà-Sauleda J, Permanyer-Miralda G, Soler-Soler J. Should pericardial drainage be performed routinely in patients who have a large pericardial effusion without tamponade? Am J Med. 1998;105:106–109. https://www.ncbi.nlm.nih.gov/pubmed/9727816[↩]
- Vaitkus PT, Herrmann HC, LeWinter MM. Treatment of malignant pericardial effusion. JAMA. 1994;272:59–64. https://www.ncbi.nlm.nih.gov/pubmed/8007081[↩]
- Patel AK, Kosolcharoen PK, Nallasivan M, Kroncke GM, Thomsen JH. Catheter drainage of the pericardium. Practical method to maintain long-term patency. Chest. 1987;92:1018–1021. https://www.ncbi.nlm.nih.gov/pubmed/3677806[↩]
- Spodick DH. Neoplastic pericardial disease. In: Spodick DH, editor. The pericardium: A Comprehensive Textbook. New York: Marcel Dekker; 1997. pp. 301–313.[↩]
- Palacios IF, Tuzcu EM, Ziskind AA, Younger J, Block PC. Percutaneous balloon pericardial window for patients with malignant pericardial effusion and tamponade. Cathet Cardiovasc Diagn. 1991;22:244–249. https://www.ncbi.nlm.nih.gov/pubmed/2032271[↩][↩]
- Swanson N, Mirza I, Wijesinghe N, Devlin G. Primary percutaneous balloon pericardiotomy for malignant pericardial effusion. Catheter Cardiovasc Interv. 2008;71:504–507. https://www.ncbi.nlm.nih.gov/pubmed/18307242[↩]
- Piehler JM, Pluth JR, Schaff HV, Danielson GK, Orszulak TA, Puga FJ. Surgical management of effusive pericardial disease. Influence of extent of pericardial resection on clinical course. J Thorac Cardiovasc Surg. 1985;90:506–516. https://www.ncbi.nlm.nih.gov/pubmed/4046619[↩]
- Sagristà-Sauleda J, Angel J, Sánchez A, Permanyer-Miralda G, Soler-Soler J. Effusive-constrictive pericarditis. N Engl J Med. 2004;350:469–475. https://www.ncbi.nlm.nih.gov/pubmed/14749455[↩]