Contents
- Peripheral artery disease
Peripheral artery disease
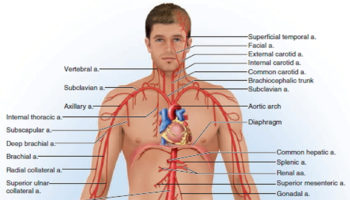
Peripheral artery disease is a disease in which plaque builds up in the arteries that carry blood to your head, organs and limbs 1. Plaque is made up of fat, cholesterol, calcium, fibrous tissue, and other substances in the blood.
Approximately 12% of the adult population has peripheral artery disease and the prevalence is equal in men and women 2.
Other names for Peripheral Artery Disease:
- Atherosclerotic peripheral arterial disease
- Intermittent Claudication
- Hardening of the arteries
- Leg cramps from poor circulation
- Peripheral arterial disease
- Peripheral vascular disease
- Poor circulation
- Vascular disease
When plaque builds up in the body’s arteries, the condition is called atherosclerosis. Atherosclerosis is a disease in which plaque builds up in the wall of an artery. Peripheral artery disease is usually caused by atherosclerosis in the peripheral arteries. Plaque is made up of deposits of fats, cholesterol and other substances. Plaque formations can grow large enough to significantly reduce the blood’s flow through an artery. Over time, plaque can harden and narrow the arteries. This limits the flow of oxygen-rich blood to your organs and other parts of your body 3. When a plaque becomes brittle or inflamed, it may rupture, triggering a blood clot to form. A clot may either further narrow the artery, or completely block it.
Where plaque occurs, two things can happen. One is that a piece of plaque may break off and be carried by the bloodstream until it gets stuck. The other is that a blood clot (thrombus) may form on the plaque’s surface. If either of these things happen, the artery can be blocked and blood flow cut off.
If the blocked artery supplies the heart or brain, a heart attack or stroke occurs. If an artery supplying oxygen to the extremities (often the legs) is blocked, gangrene can result. Gangrene is tissue death.
If the blockage remains in the peripheral arteries in the legs, it can cause pain, changes in skin color, sores or ulcers and difficulty walking. Total loss of circulation to the legs and feet can cause gangrene and loss of a limb.
If the blockage occurs in a carotid artery, it can cause a stroke.
Exactly how atherosclerosis begins or what causes it isn’t known, but some theories have been proposed. Many scientists believe plaque begins when an artery’s inner lining (called the endothelium) becomes damaged. Three possible causes of damage are:
- Elevated levels of cholesterol and triglycerides in the blood
- High blood pressure
- Cigarette smoking
Smoking has a big role in the growth of atherosclerosis in the coronary arteries, aorta and arteries in the legs. It makes fatty deposits more likely to form and to grow bigger and faster.
It’s important to learn the facts about peripheral artery disease. As with any disease, the more you understand, the more likely you’ll be able to help your healthcare professional make an early diagnosis and start treatment. Peripheral artery disease has common symptoms, but many people with peripheral artery disease never have any symptoms at all.
Peripheral artery disease usually affects the arteries in the legs, but it also can affect the arteries that carry blood from your heart to your head, arms, kidneys, and stomach. Peripheral artery disease is similar to coronary artery disease (coronary heart disease). Both peripheral artery disease and coronary artery disease are caused by atherosclerosis that narrows and blocks arteries in various critical regions of the body.
This article focuses on peripheral artery disease that affects blood flow to the legs.
Blocked blood flow to your legs can cause pain and numbness. It also can raise your risk of getting an infection in the affected limbs. Your body may have a hard time fighting the infection.
If severe enough, blocked blood flow can cause gangrene (tissue death). In very serious cases, this can lead to leg amputation.
If you have leg pain when you walk or climb stairs, talk with your doctor. Sometimes older people think that leg pain is just a symptom of aging. However, the cause of the pain could be peripheral artery disease. Tell your doctor if you’re feeling pain in your legs and discuss whether you should be tested for peripheral artery disease.
Smoking is the main risk factor for peripheral artery disease. If you smoke or have a history of smoking, your risk of peripheral artery disease increases. Other factors, such as age and having certain diseases or conditions, also increase your risk of peripheral artery disease.
Peripheral artery disease is mostly seen in people above 65 years of age. Diabetes, smoking, and high blood pressure increase the risk of peripheral artery disease.
The two main symptoms of peripheral artery disease are pain at rest and cramps in the legs mostly during physical activities (intermittent claudication).
Peripheral artery disease increases your risk of coronary heart disease, heart attack, stroke, and transient ischemic attack (“mini-stroke”). Although peripheral artery disease. is serious, it’s treatable. If you have the disease, see your doctor regularly and treat the underlying atherosclerosis. peripheral artery disease. treatment may slow or stop disease progress and reduce the risk of complications. Treatments include lifestyle changes, medicines, and surgery or procedures. Researchers continue to explore new therapies for peripheral artery disease.
How can Peripheral Artery Disease Be Prevented ?
Taking action to control your risk factors can help prevent or delay peripheral artery disease and its complications. Know your family history of health problems related to peripheral artery disease. If you or someone in your family has the disease, be sure to tell your doctor.
Controlling risk factors includes the following:
- Be physically active.
- Be screened for peripheral artery disease. A simple office test, called an ankle-brachial index, can help determine whether you have peripheral artery disease.
- Follow heart-healthy eating.
- If you smoke, quit. Talk with your doctor about programs and products that can help you quit smoking.
- If you’re overweight or obese, work with your doctor to create a reasonable weight-loss plan.
The lifestyle changes described above can reduce your risk of developing peripheral artery disease. These changes also can help prevent and control conditions that can be associated with peripheral artery disease, such as coronary heart disease, diabetes, high blood pressure, high blood cholesterol, and stroke.
Living With Peripheral Artery Disease
If you have peripheral artery disease, you’re more likely to also have coronary heart disease, heart attack, stroke, and transient ischemic attack (“mini-stroke”) 4. However, you can take steps to treat and control peripheral artery disease and lower your risk for these other conditions.
- If you have peripheral artery disease, you may feel pain in your calf or thigh muscles after walking. Try to take a break and allow the pain to ease before walking again. Over time, this may increase the distance that you can walk without pain.
- Heart-healthy lifestyle changes can help prevent or delay peripheral artery disease and other related problems, such as coronary heart disease, heart attack, stroke, and transient ischemic attack. Heart-healthy lifestyle changes include physical activity, quitting smoking, and heart-healthy eating.
Talk with your doctor about taking part in a supervised exercise program. This type of program has been shown to reduce peripheral artery disease symptoms.
Check your feet and toes regularly for sores or possible infections. Wear comfortable shoes that fit well. Maintain good foot hygiene and have professional medical treatment for corns, bunions, or calluses.
Walking Improves Blood Flow
A regular walking program will improve blood flow as new, small blood vessels form. The walking program is mainly as follows:
- Warm up by walking at a pace that does not cause your normal leg symptoms.
- Then walk to the point of mild-to-moderate pain or discomfort.
- Rest until the pain goes away, then try walking again.
Your goal over time is to be able to walk 30 to 60 minutes. Always talk with your health care provider before you start an exercise program. Call your provider right away if you have any of these symptoms during or after exercise:
- Chest pain
- Breathing problems
- Dizziness
- An uneven heart rate
Make simple changes to add walking to your day:
- At work, try taking the stairs instead of the elevator, take a 5-minute walk break every hour, or add a 10- to 20-minute walk during lunch.
- Try parking at the far end of the parking lot, or even down the street. Even better, try walking to the store.
- If you ride the bus, get off the bus 1 stop before your normal stop and walk the rest of the way.
Lifestyle Changes
Stop smoking. Smoking narrows your arteries and increases the risk of blood clots forming. Other things you can do to stay as healthy as possible are to:
- Make sure your blood pressure is well-controlled.
- Reduce your weight, if you are overweight.
- Eat a low-cholesterol and low-fat diet.
- Test your blood sugar if you have diabetes, and keep it under control.
Take Care of Your Feet
Check your feet every day. Inspect the tops, sides, soles, heels, and between your toes. If you have vision problems, ask someone to check your feet for you. Look for:
- Dry and cracked skin
- Blisters or sores
- Bruises or cuts
- Redness, warmth, or tenderness
- Firm or hard spots
See your healthcare provider right way about any foot problems. DO NOT try to treat them yourself first.
When to See the Doctor
Call your provider if you have:
- A leg or foot that is cool to the touch, pale, blue, or numb
- Chest pain or shortness of breath when you have leg pain
- Leg pain that does not go away, even when you are not walking or moving (called rest pain)
- Legs that are red, hot, or swollen
- New sores on your legs or feet
- Signs of infection (fever, sweats, red and painful skin, general ill feeling)
- Sores that do not heal
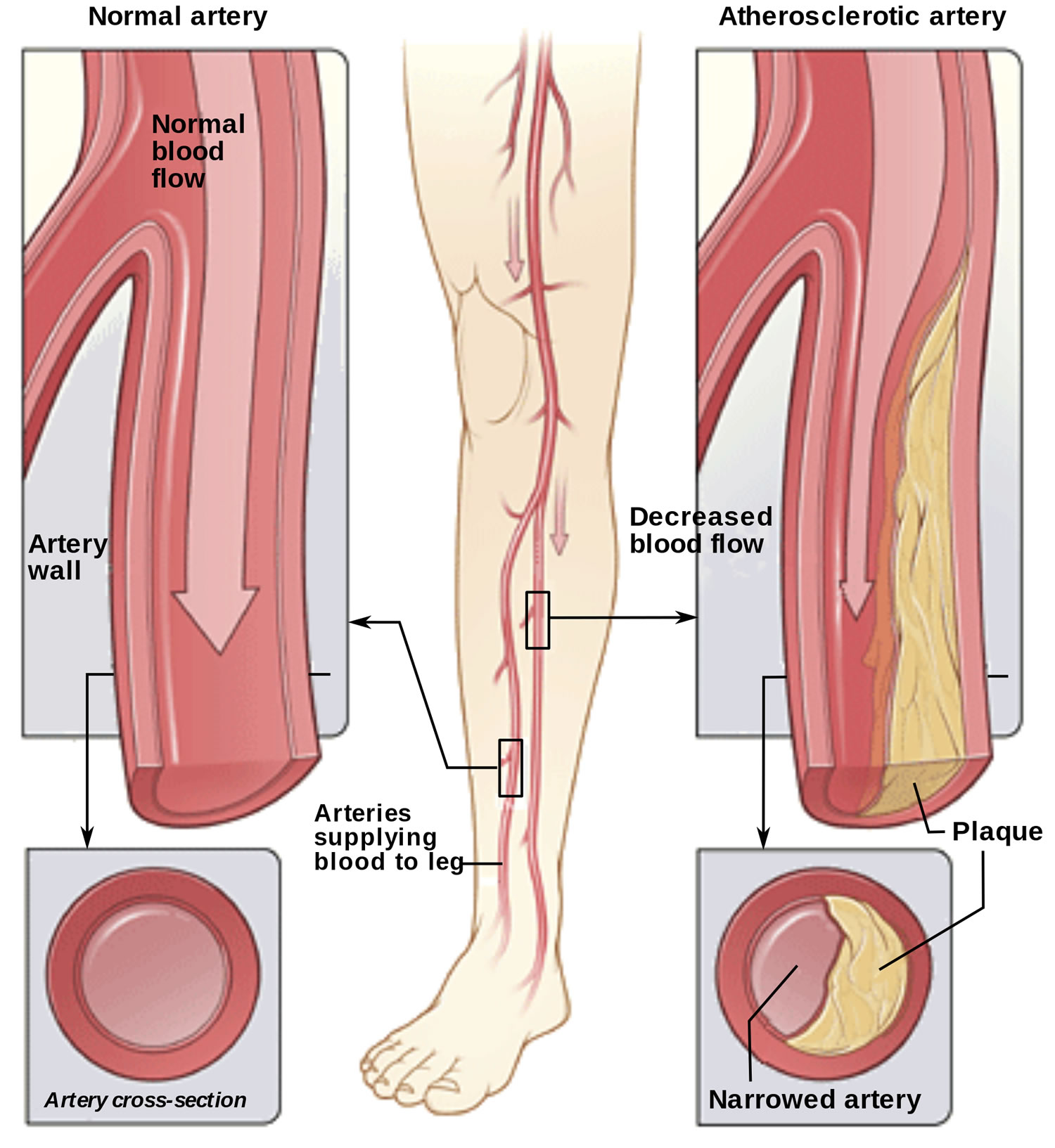
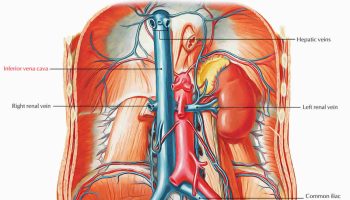
Figure 1. Peripheral artery disease
Note: The illustration shows how peripheral artery disease can affect arteries in the legs. Figure A shows a normal artery with normal blood flow. The inset image shows a cross-section of the normal artery. Figure B shows an artery with plaque buildup that’s partially blocking blood flow. The inset image shows a cross-section of the narrowed artery.
Risk factors for peripheral artery disease
The most common risk factors associated with peripheral artery disease are increasing age, diabetes, and smoking 5.
Age
Persons aged 65 years or older in the Framingham Heart Study and persons aged 70 years or older in the National Health and Nutrition Examination Survey (NHANES) were at increased risk for the development of peripheral artery disease 6. The prevalence was 4.3% in participants older than 40 years compared with 14.5% in those older than 70 years 7.
Smoking
Smoking is the single most important modifiable risk factor for the development of peripheral artery disease. It is unknown why the association between peripheral artery disease and smoking is about twice as strong as that between peripheral artery disease and coronary artery disease (coronary heart disease) 8. Smokers have a risk of peripheral artery disease that is 4 times that of nonsmokers and experience onset of symptoms almost a decade earlier. A dose-response relationship exists between pack-year history and peripheral artery disease risk 9, 10. Furthermore, smokers have poorer survival rates, a greater likelihood of progression to critical limb ischemia and amputation, and decreased artery bypass graft patency rates when compared with nonsmokers. Both former and current smokers are at increased risk of peripheral artery disease. However, patients who are able to stop smoking are less likely to develop critical limb ischemia and have improved survival 11.
Diabetes Mellitus
Diabetes increases the risk of developing symptomatic and asymptomatic peripheral artery disease by 1.5- to 4-fold and leads to an increased risk of cardiovascular events and early mortality 12. In NHANES 10, 26% of participants with peripheral artery disease were identified as having diabetes, whereas in the Edinburgh Artery Study 13, the prevalence of peripheral artery disease was greater in participants with diabetes or impaired glucose tolerance (20.6%) than in those with normal glucose tolerance (12.5%). Diabetes mellitus is a stronger risk factor for peripheral artery disease in women than men, and the prevalence of peripheral artery disease is higher in African American and Hispanic diabetic populations 14, 15. Diabetes (and poor foot care) is the most common cause for amputation in the United States 14.
Hyperlipidemia
In the Framingham Study, an elevated cholesterol level was associated with a 2-fold increased risk of claudication 16. In NHANES, more than 60% of patients with peripheral artery disease had hypercholesterolemia, whereas in the PARTNERS (Peripheral artery disease Awareness, Risk, and Treatment: New Resources for Survival) program, the prevalence of hyperlipidemia in patients with known peripheral artery disease was 77% 10. Hyperlipidemia increases the adjusted likelihood of developing peripheral artery disease by 10% for every 10 mg/dL rise in total cholesterol (to convert to mmol/L, multiply by 0.0259) 17. The 2001 National Cholesterol Education Program Adult Treatment Panel III considered peripheral artery disease a coronary artery disease risk equivalent 18.
Hypertension
Almost every study has shown a strong association between hypertension and peripheral artery disease, and as many as 50% to 92% of patients with peripheral artery disease have hypertension 19. The risk of developing claudication is increased 2.5- to 4-fold in both men and women with hypertension 16. In the Systolic Hypertension in the Elderly Program, 5.5% of the participants had an ankle brachial index (ABI) under 0.90 20. Cumulatively, these studies underscore the high prevalence of peripheral artery disease in patients with hypertension.
Nontraditional Risk Factors
Other risk factors that are associated with an increased prevalence of peripheral artery disease include race and ethnicity (African Americans and those of Hispanic origin are at higher risk), chronic kidney disease, the metabolic syndrome, and levels of C-reactive protein, β2-microglobulin, cystatin C, lipoprotein(a), and homocysteine 21, 22.
Peripheral artery disease causes
The most common cause of peripheral artery disease is atherosclerosis. Atherosclerosis is a disease in which plaque builds up in your arteries. The exact cause of atherosclerosis isn’t known.
The disease may start if certain factors damage the inner layers of the arteries. These factors include:
- Smoking
- High amounts of certain fats and cholesterol in the blood
- High blood pressure
- High amounts of sugar in the blood due to insulin resistance or diabetes
When damage occurs, your body starts a healing process. The healing may cause plaque to build up where the arteries are damaged.
Eventually, a section of plaque can rupture (break open), causing a blood clot to form at the site. The buildup of plaque or blood clots can severely narrow or block the arteries and limit the flow of oxygen-rich blood to your body.
Who is at Risk for Peripheral Artery Disease ?
Peripheral artery disease affects millions of people in the United States. The disease is more common in blacks than any other racial or ethnic group. The major risk factors for peripheral artery disease are smoking, older age, and having certain diseases or conditions.
Smoking
Smoking is the main risk factor for peripheral artery disease and your risk increases if you smoke or have a history of smoking. Quitting smoking slows the progress of peripheral artery disease. People who smoke and people who have diabetes are at highest risk for peripheral artery disease complications, such as gangrene (tissue death) in the leg from decreased blood flow.
Older Age
Older age also is a risk factor for peripheral artery disease. Plaque builds up in your arteries as you age. Older age combined with other risk factors, such as smoking or diabetes, also puts you at higher risk for peripheral artery disease.
Diseases and Conditions
Many diseases and conditions can raise your risk of peripheral artery disease, including:
- Diabetes
- High blood pressure
- High blood cholesterol
- Coronary heart disease
- Stroke
- Metabolic syndrome
Peripheral artery disease symptoms and signs
Many people who have peripheral artery disease don’t have any signs or symptoms.
The most common symptoms of peripheral artery disease involving the lower extremities are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. Typically, this pain goes away with rest and returns when you walk again.
- Many people mistake the symptoms of peripheral artery disease for something else.
- Peripheral artery disease often goes undiagnosed by healthcare professionals.
- People with peripheral arterial disease have a higher risk of coronary artery disease, heart attack or stroke.
- Left untreated, peripheral artery disease can lead to gangrene and amputation.
Added risks for peripheral artery disease:
- If you smoke, you have an especially high risk for peripheral artery disease.
- If you have diabetes, you have an especially high risk for peripheral artery disease.
- People with high blood pressure or high cholesterol are at risk for peripheral artery disease.
- Your risk increases with age.
Even if you don’t have signs or symptoms, ask your doctor whether you should get checked for peripheral artery disease if you’re:
- Aged 70 or older
- Aged 50 or older and have a history of smoking or diabetes
- Younger than 50 and have diabetes and one or more risk factors for atherosclerosis
Intermittent Claudication
People who have peripheral artery disease may have symptoms when walking or climbing stairs, which may include pain, numbness, aching, or heaviness in the leg muscles. Symptoms also may include cramping in the affected leg(s) and in the buttocks, thighs, calves, and feet. Symptoms may ease after resting. These symptoms are called intermittent claudication.
During physical activity, your muscles need increased blood flow. If your blood vessels are narrowed or blocked, your muscles won’t get enough blood, which will lead to symptoms. When resting, the muscles need less blood flow, so the symptoms will go away.
Other Signs and Symptoms
Other signs and symptoms of peripheral artery disease include:
- Weak or absent pulses in the legs or feet
- Sores or wounds on the toes, feet, or legs that heal slowly, poorly, or not at all
- A pale or bluish color to the skin
- A lower temperature in one leg compared to the other leg
- Poor nail growth on the toes and decreased hair growth on the legs
- Erectile dysfunction, especially among men who have diabetes
How is Peripheral Artery Disease Diagnosed ?
Peripheral artery disease is diagnosed based on your medical and family histories, a physical exam, and test results.
Peripheral artery disease often is diagnosed after symptoms are reported. A correct diagnosis is important because people who have peripheral artery disease are at higher risk for coronary heart disease (coronary artery disease), heart attack, stroke, and transient ischemic attack (“mini-stroke”). If you have peripheral artery disease, your doctor also may want to check for signs of these diseases and conditions.
Specialists Involved
Primary care doctors, such as internists and family doctors, may treat people who have mild peripheral artery disease. For more advanced peripheral artery disease, a vascular specialist may be involved. This is a doctor who specializes in treating blood vessel diseases and conditions.
A cardiologist also may be involved in treating people who have peripheral artery disease. Cardiologists treat heart problems, such as coronary heart disease and heart attack, which often affect people who have peripheral artery disease.
Medical and Family Histories
Your doctor may ask:
- Whether you have any risk factors for peripheral artery disease. For example, he or she may ask whether you smoke or have diabetes.
- About your symptoms, including any symptoms that occur when walking, exercising, sitting, standing, or climbing.
- About your diet.
- About any medicines you take, including prescription and over-the-counter medicines.
- Whether anyone in your family has a history of heart or blood vessel diseases.
Physical Exam
During the physical exam, your doctor will look for signs of peripheral artery disease. He or she may check the blood flow in your legs or feet to see whether you have weak or absent pulses.
Your doctor also may check the pulses in your leg arteries for an abnormal whooshing sound called a bruit. He or she can hear this sound with a stethoscope. A bruit may be a warning sign of a narrowed or blocked artery.
Your doctor may compare blood pressure between your limbs to see whether the pressure is lower in the affected limb. He or she also may check for poor wound healing or any changes in your hair, skin, or nails that may be signs of peripheral artery disease.
Diagnostic Tests
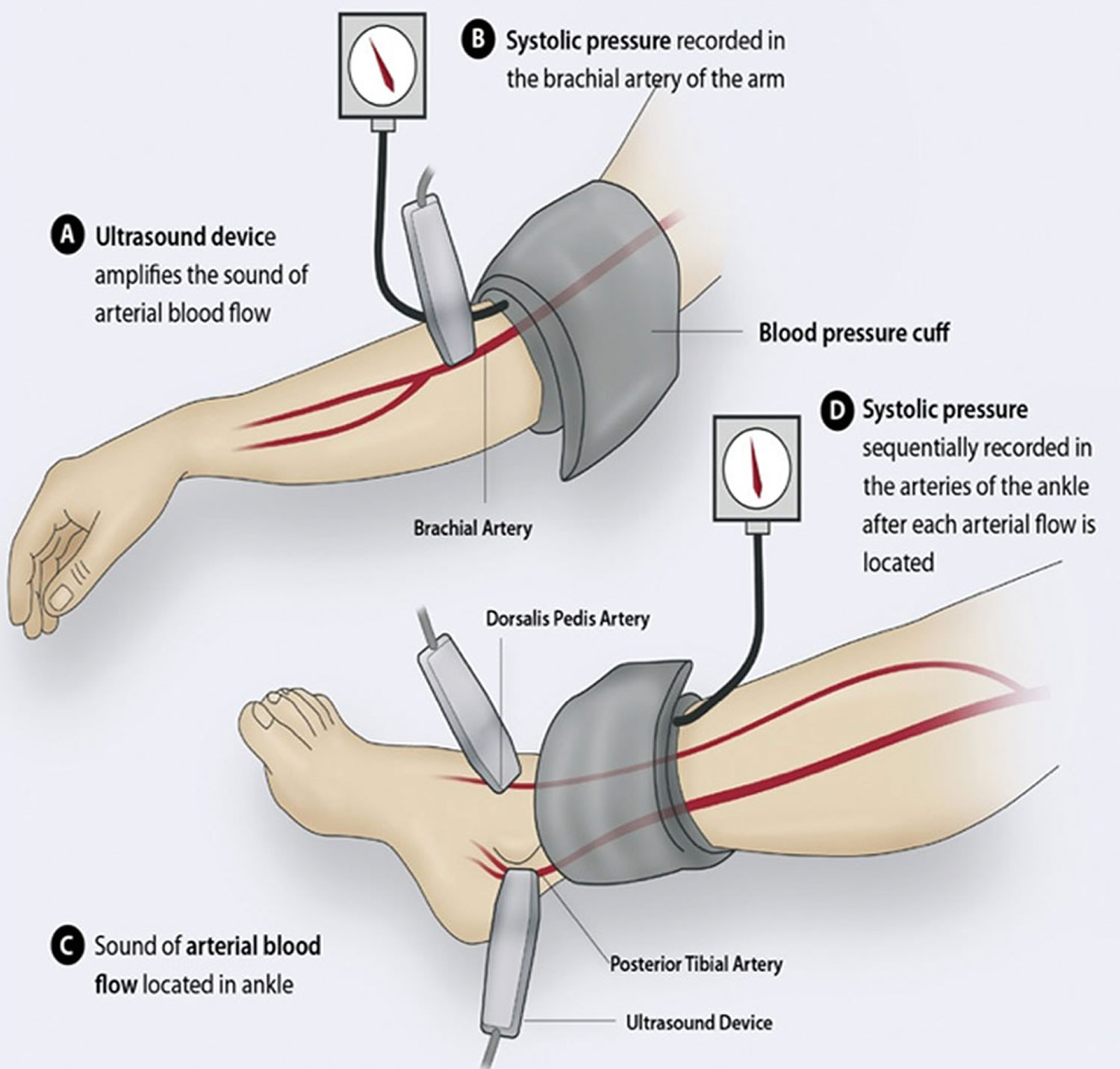
Ankle-Brachial Index
A simple test called an ankle-brachial index (ABI) often is used to diagnose peripheral artery disease. The ankle-brachial index compares blood pressure in your ankle to blood pressure in your arm. This test shows how well blood is flowing in your limbs.
Ankle-brachial index can show whether peripheral artery disease. is affecting your limbs, but it won’t show which blood vessels are narrowed or blocked.
A normal ankle-brachial index result is 1.0 or greater (with a range of 0.90 to 1.30). The test takes about 10 to 15 minutes to measure both arms and both ankles. This test may be done yearly to see whether peripheral artery disease is getting worse.
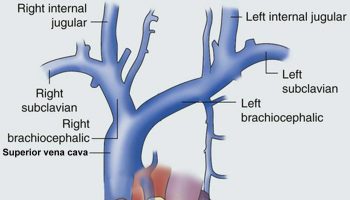
Figure 2. Ankle-Brachial Index
Note: The illustration shows the ankle-brachial index test. The test compares blood pressure in the ankle to blood pressure in the arm. As the blood pressure cuff deflates, the blood pressure in the arteries is recorded.
Doppler Ultrasound
A Doppler ultrasound looks at blood flow in the major arteries and veins in the limbs. During this test, a handheld device is placed on your body and passed back and forth over the affected area. A computer converts sound waves into a picture of blood flow in the arteries and veins.
The results of this test can show whether a blood vessel is blocked. The results also can help show the severity of peripheral artery disease.
Treadmill Test
A treadmill test can show the severity of symptoms and the level of exercise that brings them on. You’ll walk on a treadmill for this test. This shows whether you have any problems during normal walking.
You may have an ankle-brachial index (ABI) test before and after the treadmill test. This will help compare blood flow in your arms and legs before and after exercise.
Magnetic Resonance Angiogram
A magnetic resonance angiogram (MRA) uses magnetic and radio wave energy to take pictures of your blood vessels. This test is a type of magnetic resonance imaging (MRI).
An magnetic resonance angiogram can show the location and severity of a blocked blood vessel. If you have a pacemaker, man-made joint, stent, surgical clips, mechanical heart valve, or other metallic devices in your body, you might not be able to have an magnetic resonance angiogram. Ask your doctor whether an magnetic resonance angiogram is an option for you.
Arteriogram
An arteriogram provides a “road map” of the arteries. Doctors use this test to find the exact location of a blocked artery.
For this test, dye is injected through a needle or catheter (tube) into one of your arteries. This may make you feel mildly flushed. After the dye is injected, an x ray is taken. The x ray can show the location, type, and extent of the blockage in the artery.
Some doctors use a newer method of arteriogram that uses tiny ultrasound cameras. These cameras take pictures of the insides of the blood vessels. This method is called intravascular ultrasound.
Blood Tests
Your doctor may recommend blood tests to check for peripheral artery disease risk factors. For example, blood tests can help diagnose conditions such as diabetes and high blood cholesterol.
Peripheral artery disease treatment
Treatments for peripheral artery disease include heart-healthy lifestyle changes, medicines, and surgery or procedures.
The overall goals of treating peripheral artery disease include reducing risk of heart attack and stroke; reducing symptoms of claudication; improving mobility and overall quality of life; and preventing complications. Treatment is based on your signs and symptoms, risk factors, and the results of physical exams and tests.
Treatment may slow or stop the progression of the disease and reduce the risk of complications. Without treatment, peripheral artery disease may progress, resulting in serious tissue damage in the form of sores or gangrene (tissue death) due to inadequate blood flow. In extreme cases of peripheral artery disease, also referred to as critical limb ischemia, removal (amputation) of part of the leg or foot may be necessary.
Heart-Healthy Lifestyle Changes
Treatment often includes making life-long heart-healthy lifestyle changes such as:
- Physical activity
- Quitting smoking
- Heart-healthy eating
Surgery or Procedures
Bypass Grafting
Your doctor may recommend bypass grafting surgery if blood flow in your limb is blocked or nearly blocked. For this surgery, your doctor uses a blood vessel from another part of your body or a synthetic tube to make a graft.
This graft bypasses (that is, goes around) the blocked part of the artery. The bypass allows blood to flow around the blockage. This surgery doesn’t cure peripheral artery disease, but it may increase blood flow to the affected limb.
Angioplasty and Stent Placement
Your doctor may recommend angioplasty to restore blood flow through a narrowed or blocked artery.
During this procedure, a catheter (thin tube) with a balloon at the tip is inserted into a blocked artery. The balloon is then inflated, which pushes plaque outward against the artery wall. This widens the artery and restores blood flow.
A stent (a small mesh tube) may be placed in the artery during angioplasty. A stent helps keep the artery open after angioplasty is done. Some stents are coated with medicine to help prevent blockages in the artery.
Atherectomy
Atherectomy is a procedure that removes plaque buildup from an artery. During the procedure, a catheter is used to insert a small cutting device into the blocked artery. The device is used to shave or cut off plaque.
The bits of plaque are removed from the body through the catheter or washed away in the bloodstream (if they’re small enough).
Doctors also can perform atherectomy using a special laser that dissolves the blockage.
Other Types of Treatment
Researchers are studying cell and gene therapies to treat peripheral artery disease. However, these treatments aren’t yet available outside of clinical trials.
- What Is Peripheral Artery Disease ? National Heart, Lung and Blood Institute. https://www.nhlbi.nih.gov/health/health-topics/topics/pad/[↩]
- Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344(21):1608-1621. http://www.nejm.org/doi/full/10.1056/NEJM200105243442108[↩]
- Nayor MG, Beckman JA. Atherosclerotic risk factors. In: Cronenwett JL, Johnston KW, eds. Rutherford’s Vascular Surgery. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:chap 28.[↩]
- Creager MA, Libby P. Peripheral artery disease. In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 58.[↩]
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, TASC II Working Group Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;45(suppl S):S5-S67. https://www.ncbi.nlm.nih.gov/pubmed/17223489[↩]
- ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation. 2006;113:e463-e654. https://doi.org/10.1161/CIRCULATIONAHA.106.174526. http://circ.ahajournals.org/content/circulationaha/113/11/e463.full.pdf[↩]
- Criqui MH, Fronek A, Barrett-Connor E, Klauber MR, Gabriel S, Goodman D. The prevalence of peripheral arterial disease in a defined population. Circulation 1985;71(3):510-515. https://www.ncbi.nlm.nih.gov/pubmed/3156006[↩]
- Kannel WB, Shurtleff D. The Framingham Study: cigarettes and the development of intermittent claudication. Geriatrics 1973;28(2):61-68. https://www.ncbi.nlm.nih.gov/pubmed/4683662[↩]
- Powell JT, Edwards RJ, Worrell PC, Franks PJ, Greenhalgh RM, Poulter NR. Risk factors associated with the development of peripheral arterial disease in smokers: a case-control study. Atherosclerosis 1997;129(1):41-48. https://www.ncbi.nlm.nih.gov/pubmed/9069515[↩]
- Selvin E, Hirsch AT. Contemporary Risk Factor Control and Walking Dysfunction in Individuals with Peripheral Arterial Disease: NHANES 1999-2004. Atherosclerosis. 2008;201(2):425-433. doi:10.1016/j.atherosclerosis.2008.02.002. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2771432/[↩][↩][↩]
- Jonason T, Bergstrom R. Cessation of smoking in patients with intermittent claudication: effects on the risk of peripheral vascular complications, myocardial infarction and mortality. Acta Med Scand. 1987;221(3):253-260. https://www.ncbi.nlm.nih.gov/pubmed/3591463[↩]
- American Diabetes Association Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26(12):3333-3341. https://www.ncbi.nlm.nih.gov/pubmed/14633825[↩]
- MacGregor AS, Price JF, Hau CM, Lee AJ, Carson MN, Fowkes FG. Role of systolic blood pressure and plasma triglycerides in diabetic peripheral arterial disease: The Edinburgh Artery Study. Diabetes Care 1999;22(3):453-458. http://care.diabetesjournals.org/content/22/3/453.long[↩]
- American Diabetes Association Peripheral arterial disease in people with diabetes. Diabetes Care 2003;26(12):3333-3341. http://care.diabetesjournals.org/content/26/12/3333.long[↩][↩]
- Wattanakit K, Folsom AR, Selvin E, et al. Risk factors for peripheral arterial disease incidence in persons with diabetes: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis 2005;180(2):389-397. https://www.ncbi.nlm.nih.gov/pubmed/15910867[↩]
- Kannel WB, McGee DL. Update on some epidemiologic features of intermittent claudication: the Framingham Study. J Am Geriatr Soc. 1985;33(1):13-18. https://www.ncbi.nlm.nih.gov/pubmed/3965550[↩][↩]
- Hiatt WR, Hoag S, Hamman RF, San Luis Valley Diabetes Study Effect of diagnostic criteria on the prevalence of peripheral arterial disease. Circulation 1995;91(5):1472-1479. http://circ.ahajournals.org/content/91/5/1472.long[↩]
- Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001;285(19):2486-2497. http://jamanetwork.com/journals/jama/article-abstract/193847[↩]
- Olin JW. Hypertension and peripheral arterial disease. Vasc Med. 2005;10(3):241-246. http://journals.sagepub.com/doi/pdf/10.1191/1358863x05vm591xx[↩]
- Newman AB, Tyrrell KS, Kuller LH. Mortality over four years in SHEP participants with a low ankle-arm index. J Am Geriatr Soc. 1997;45(12):1472-1478. https://www.ncbi.nlm.nih.gov/pubmed/9400557[↩]
- Albert MA, Ridker PM. The role of C-reactive protein in cardiovascular disease risk. Curr Cardiol Rep. 1999;1(2):99-104. https://www.ncbi.nlm.nih.gov/pubmed/10980827[↩]
- McDermott MM, Greenland P, Green D, et al. D-dimer, inflammatory markers, and lower extremity functioning in patients with and without peripheral arterial disease. Circulation 2003;107(25):3191-3198. http://circ.ahajournals.org/content/107/25/3191.long[↩]