Contents
What is phantom pain
Phantom pain is pain that feels like it’s coming from a body part that’s no longer there. Scientists recognize that these real sensations originate in the spinal cord and brain.
Although phantom pain occurs most often in people who’ve had an arm or leg removed, the disorder may also occur after surgeries to remove other body parts, such as the breast, penis, eye or tongue.
For some people, phantom pain gets better over time without treatment. For others, managing phantom pain can be challenging. You and your doctor can work together to treat phantom pain effectively with medication or other therapies.
Most people who’ve had a limb removed report that it sometimes feels as if the amputated limb is still there. This painless phenomenon, known as phantom limb sensation, may rarely occur in people who were born without limbs.
Phantom limb sensations may include feelings of coldness, warmth, or itchiness or tingling — but should not be confused with phantom pain. Similarly, pain from the remaining stump of an amputated limb is not phantom pain. By definition, phantom pain feels as if the pain comes from a body part that no longer remains.
Characteristics of phantom pain include:
- Onset within the first few days of amputation
- Comes and goes or is continuous
- Often affects the part of the limb farthest from the body, such as the foot of an amputated leg
- May be described as shooting, stabbing, boring, squeezing, throbbing or burning
- Sometimes feels as if the phantom part is forced into an uncomfortable position
- May be triggered by pressure on the remaining part of the limb or emotional stress
With phantom sensation you may feel:
- Pain in your limb even though it is physically not there
- Tingly
- Prickly
- Numb
- Hot or cold
- Like your missing toes or fingers are moving
- Like your missing limb is still there, or is in a funny position
- Like your missing limb is getting shorter (telescoping)
Pain in the missing part of the arm or leg is called – phantom limb pain – phantom arm pain or phantom leg pain respectively. You may feel:
- Sharp or shooting pain
- Achy pain
- Burning pain
- Cramping pain
Some things may make phantom pain worse, such as:
- Being too tired
- Putting too much pressure on the stump or parts of the arm or leg that are still there
- Changes in the weather
- Stress
- Infection
- An artificial limb that does not fit properly
- Poor blood flow
- Swelling in the part of the arm or leg that is still there
How long does phantom pain last?
These feeling slowly get weaker and weaker. You should also feel them less often. They may not ever go away completely.
Self-care for phantom pain
Try to relax in a way that works for you. Do deep breathing or pretend to relax the missing arm or leg.
Reading, listening to music, or doing something that takes your mind off the pain may help. You may also try taking a warm bath if your surgery wound is completely healed.
Ask your health care provider if you can take acetaminophen (Tylenol), aspirin, ibuprofen (Advil or Motrin), or other medicines that help with pain.
These following may also help lessen phantom pain:
- Keep the remaining part of your arm or leg warm.
- Move or exercise the remaining part of your arm or leg.
- If you are wearing your prosthesis, take it off. If you are not wearing it, put it on.
- If you have swelling in the remaining part of your arm or leg, try wearing an elastic bandage.
- Wear a shrinker sock or compression stocking.
- Try gently tapping or rubbing your stump.
What is the sensory nervous system
The sensory nervous system is part of the peripheral nervous system.
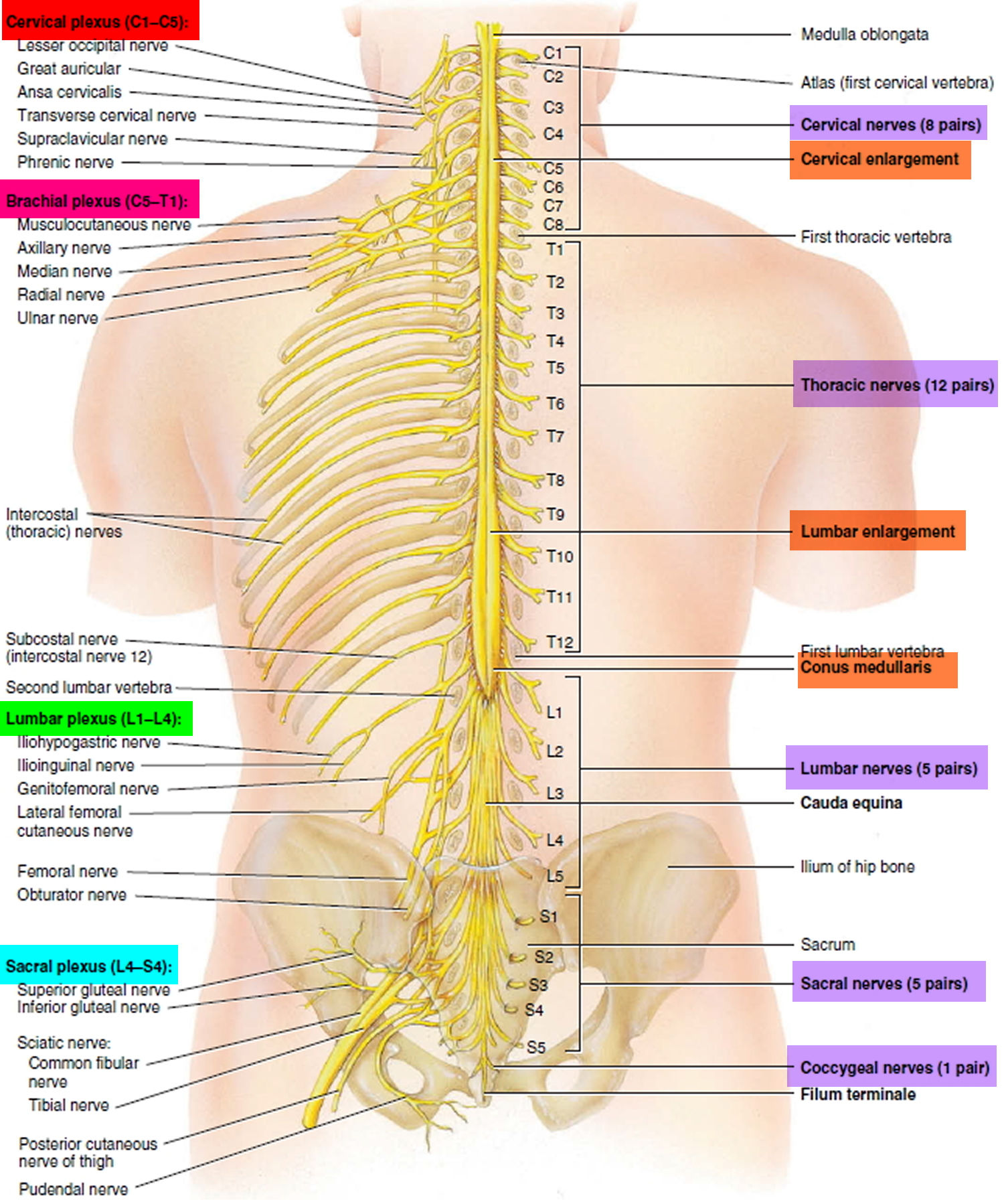
The nervous system has two major anatomical subdivisions:
- The central nervous system (CNS) consists of the brain and spinal cord, which are enclosed and protected by the cranium and vertebral column. The central nervous system is discussed further in the other posts: Human brain and Spinal cord.
- The peripheral nervous system (PNS) consists of all the rest; it is composed of nerves and ganglia. A nerve is a bundle of nerve fibers (axons) wrapped in fibrous connective tissue. Nerves emerge from the central nervous system (brain and spinal cord) through foramina of the skull and vertebral column and carry signals to and from other organs of the body. A ganglion (plural, ganglia) is a knotlike swelling in a nerve where the cell bodies of peripheral neurons are concentrated.
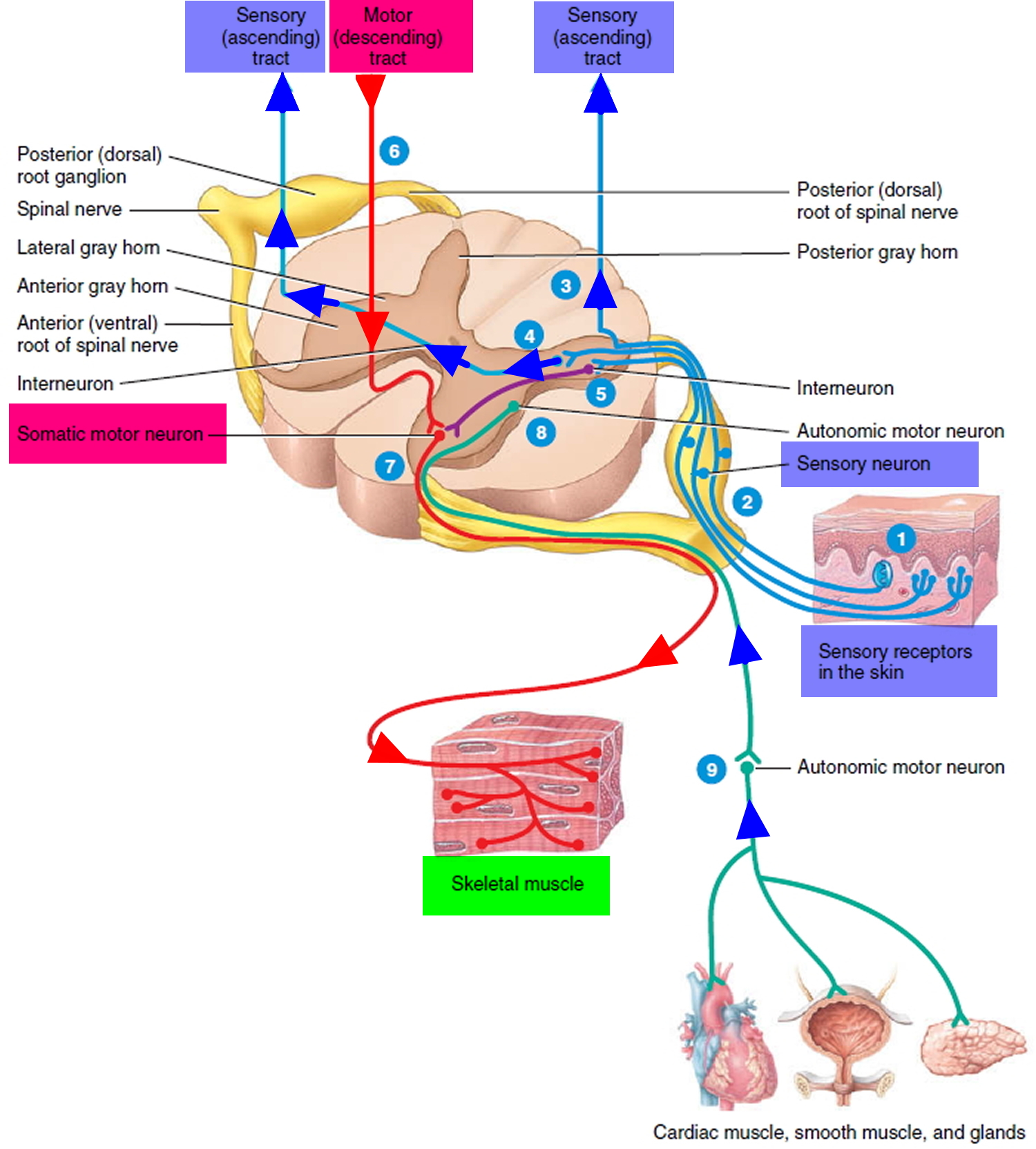
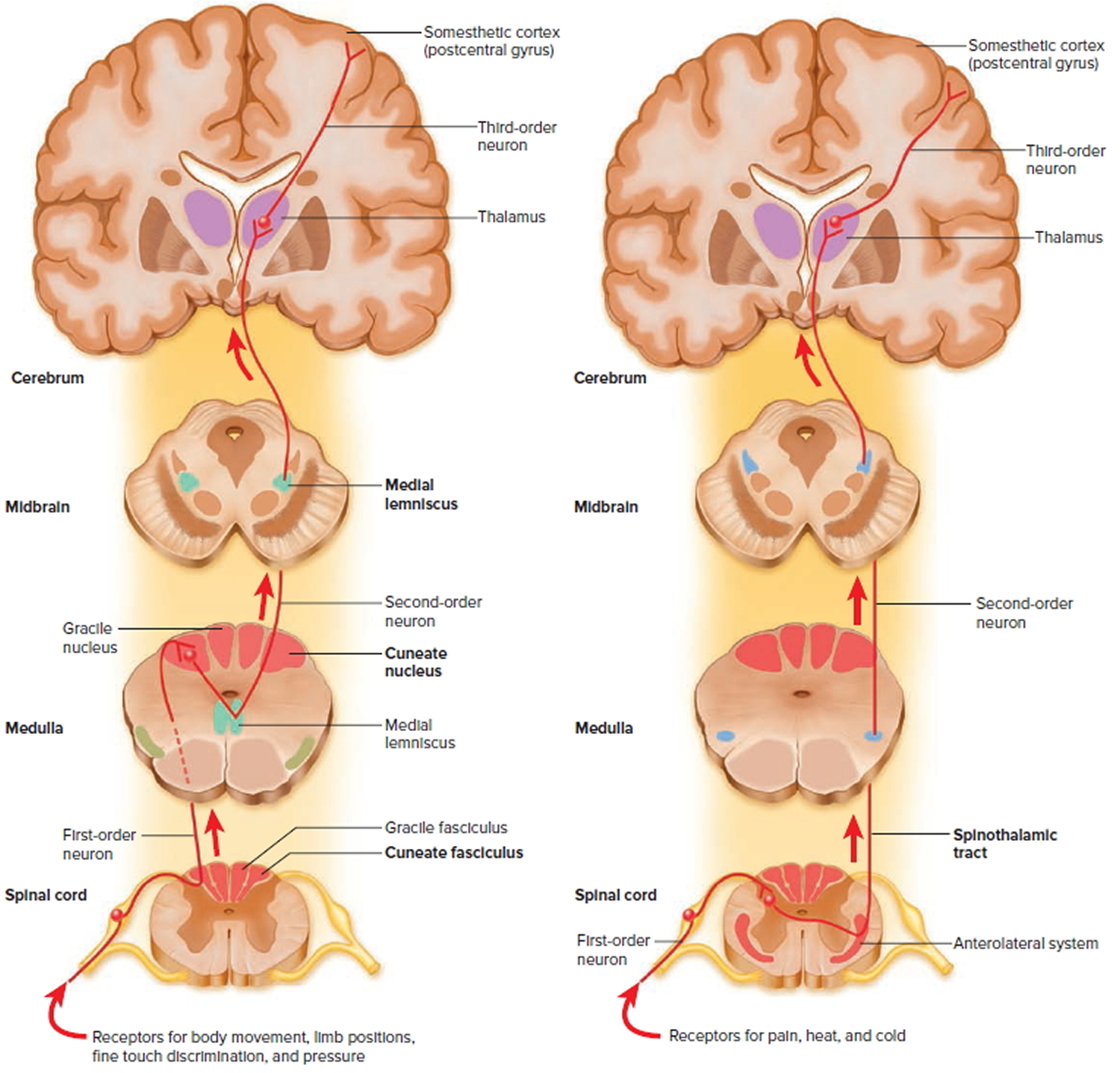
The sensory (afferent) nervous system carries signals from various receptors (sense organs and simple sensory nerve endings) to the central nervous system (CNS). This pathway informs the central nervous system (the brain and the spinal cord) of stimuli within and around the body.
The sensory systems keep the central nervous system (the brain and the spinal cord) informed of changes in the external and internal environments. The sensory information is integrated and processed by interneurons in the spinal cord and brain. Responses to the integrative decisions are brought about by motor activities (muscular contractions and glandular secretions). The cerebral cortex, the outer part of the brain, plays a major role in controlling precise voluntary muscular movements. Other brain regions provide important integration for regulation of automatic movements.
Within the sensory division of the peripheral nervous system (PNS), sensory inputs are differentiated as general (widespread) or special (localized, i.e., the special senses).
Sensory receptor. The distal end of a sensory neuron (dendrite) or an associated sensory structure serves as a sensory receptor. It responds to a specific stimulus—a change in the internal or external environment—by producing a graded potential called a generator (or receptor) potential. If a generator potential reaches the threshold level of depolarization, it will trigger one or more nerve impulses in the sensory neuron.
Figure 1. Spinal cord segments
Figure 2. Processing of sensory input and motor output by the spinal cord
Note: Sensory input is conveyed from sensory receptors to the posterior gray horns of the spinal cord, and motor output is conveyed from the anterior and lateral gray horns of the spinal cord to effectors (muscles and glands).
Figure 3. Spinal cord ascending tracts to the brain
What is phantom limb pain
Phantom limb pain refers to the neuropathic pain some people experience after the surgical amputation of a limb. The pain may be associated with feelings that the amputated limb is still attached to the body. Phantom limb pain is often hard to distinguish from stump pain (pain felt in the stump remaining after amputation).
Phantom limb pain usually develops within the first few days after amputation. However, in some cases the onset is delayed for months or even years. Phantom limb pain is often associated with the phenomenon of “phantom sensation”, where patients perceive that their limb is present in its pre-amputation form. It may be associated with vivid feelings of movement in the missing limb. Over time, these sensations may change, with the distal part of the limb being felt to ‘telescope’ into the stump.
Phantom limb pain affects 50-80% of all amputees. The occurrence is similar in males and females. It also occurs independently of age, level or side of amputation. Patients with short lasting pre-amputation pain and patients who did not have pain in the limb the day before the amputation have a significantly lower incidence of phantom pain.
Phantom limb pain can also affect children. Recent studies have reported that it is present in at least 20% of congenitally limb-deficient children (those who are born without one or more limbs) and in half of all children who undergo amputation before the age of 6 years.
Several factors have been identified which increase the risk of developing phantom pain:
- Preamputation limb pain – the presence of pain in the limb the day prior to amputation.
- Persistent stump pain – pain felt at the end of an amputated limb’s stump, due to nerve damage.
- The presence of other pains, e.g. headache, bone, or joint pain.
- Bilateral limb amputations – having limb amputations on both sides of the body, eg. having both legs amputated.
- Lower limb amputations – amputation of the leg or part of the leg.
Phantom limb pain outlook (prognosis)
The probable outcome of phantom limb pain is poorly understood. It is thought that phantom limb pain reduces or vanishes in most cases in the two years following amputation. However, persistent phantom limb pain may occur in approximately 5% of amputees. Even in these persistent cases, the pain usually becomes less severe over time.
Phantom limb pain symptoms
Phantom limb pain is a type of neuropathic pain. This means that the pain is being caused not by a real injury but by a malfunction of the nervous system. Neuropathic pain is often described as having a burning or shooting quality and may be associated with bothersome paraesthesias (unusual sensations such as tingling or pins and needles). The pain reported may also be similar to the pain in the limb prior to amputation.
The pain is generally intermittent in nature, with only a minority of patients experiencing constant pain. Phantom pain is usually felt in the distal (far) part of the missing limb; for example, in lower limb amputation, phantom pain is usually felt in the toes, ball and top of the foot, and ankle.
Some patients with phantom limb pain are reluctant to discuss their symptoms with their doctor for fear that they will be told the pain is “all in their head”. However, it is a well-recognised pain syndrome for which treatment is available, so it is important to mention any pain that may be experienced.
Phantom limb pain treatment
Phantom limb pain is often difficult to treat. There are several different types of treatment available, and a pain specialist is usually involved in the patient’s care to help coordinate pain management.
Drug treatments
Simple analgesics such as paracetamol can be beneficial in some patients, but provide little pain relief in most. Opiate analgesia has been shown to be effective, but should be used with care in patients with chronic pain.
Anticonvulsants such as pregabalin (Lyrica) and gabapentin have proved beneficial in the treatment of other forms of neuropathic pain. It is suggested that these medications may also be effective for phantom limb pain, though further research is needed.
Tricyclic antidepressants such as amitriptyline are also known to be effective in the treatment of other forms of neuropathic pain, and may be tried in the management of phantom limb pain.
Calcitonin and ketamine have been shown to be effective for the reduction of phantom limb pain.
Non-drug therapies
In some patients, prosthesis revision can provide significant pain relief. Other techniques including acupuncture, heat and cold, ultrasound, massage and stump manipulation have been described in case reports. Transcutaneous electrical nerve stimulation (TENS) has been used with some success in the treatment of phantom limb pain.
Other techniques such as sympathetic nerve blockade and spinal cord stimulation have been used with inconsistent results. Prevention of phantom limb pain has also been attempted, with suggestions that preoperative epidural anaesthesia can reduce the incidence of phantom limb pain in the first few years following amputation.
Stump pain, which may trigger phantom limb pain, can be treated by identifying the trigger point on the stump and treating it locally.
All patients suffering from chronic pain are at increased risk of depression, and this should be identified and treated.
Phantom limb pain causes
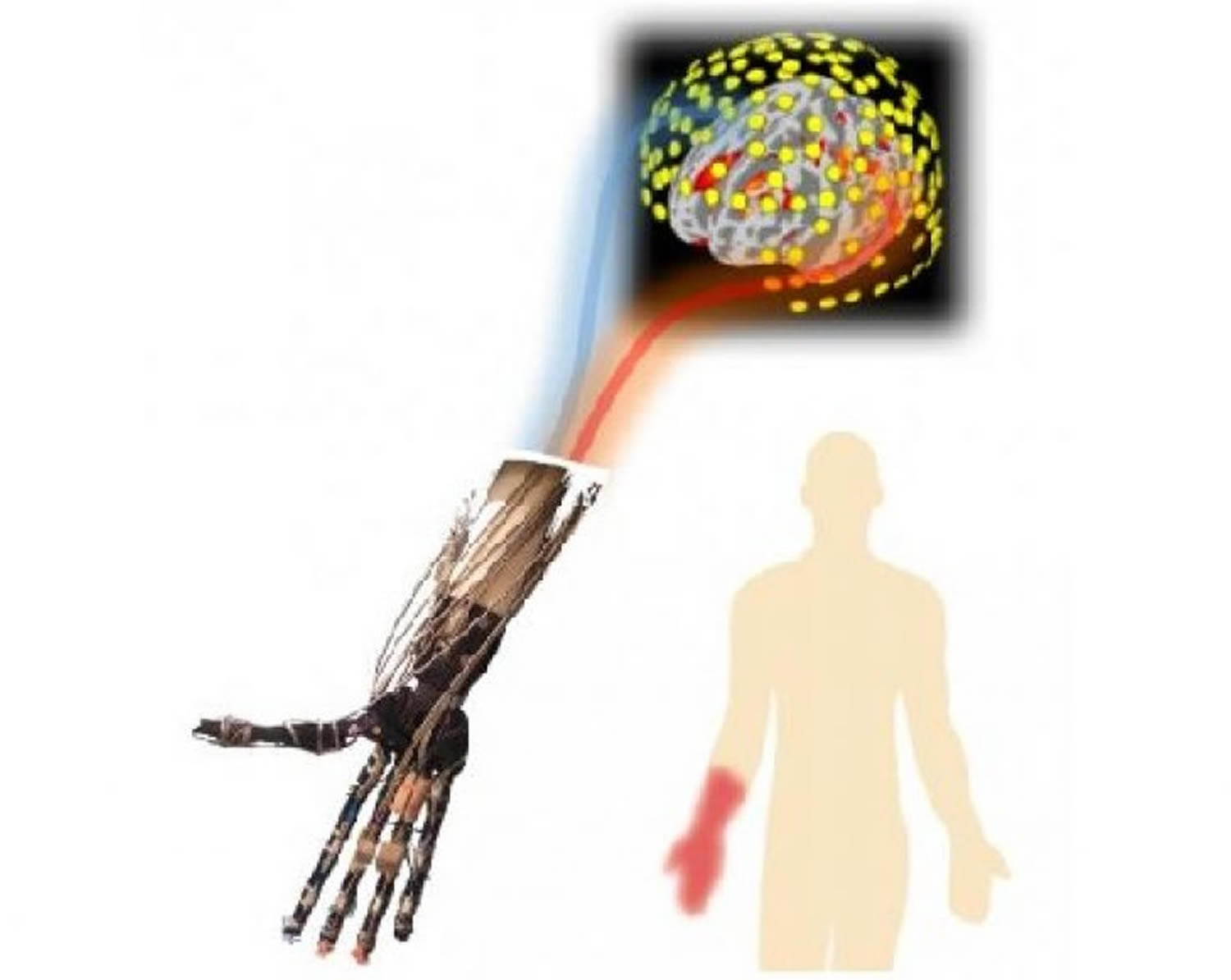
The exact cause of phantom pain is unclear, but it appears to originate in the spinal cord and brain. During imaging scans — such as magnetic resonance imaging (MRI) or positron emission tomography (PET) — portions of the brain that had been neurologically connected to the nerves of the amputated limb show activity when the person feels phantom pain.
Many experts believe phantom pain may be at least partially explained as a response to mixed signals from the brain. After an amputation, areas of the spinal cord and brain lose input from the missing limb and adjust to this detachment in unpredictable ways. The result can trigger the body’s most basic message that something is not right: pain.
Studies also show that after an amputation the brain may remap that part of the body’s sensory circuitry to another part of the body. In other words, because the amputated area is no longer able to receive sensory information, the information is referred elsewhere — from a missing hand to a still-present cheek, for example.
So when the cheek is touched, it’s as though the missing hand also is being touched. Because this is yet another version of tangled sensory wires, the result can be pain.
A number of other factors are believed to contribute to phantom pain, including damaged nerve endings, scar tissue at the site of the amputation and the physical memory of pre-amputation pain in the affected area.
Risk factors for phantom limb pain
It’s still unknown why some people develop phantom pain after an amputation while others do not. Some factors that may increase your risk of phantom pain include:
- Pain before amputation. Some researchers have found that people who had pain in a limb before amputation are likely to have it afterward, especially immediately after amputation. This may be because the brain holds on to the memory of the pain and keeps sending pain signals, even after the limb is removed.
- Stump pain. People who have persistent stump pain usually have phantom pain, too. Stump pain can be caused by an abnormal growth on damaged nerve endings (neuroma) that often results in painful nerve activity.
- Poor-fitting artificial limb (prosthesis). Talk to your doctor to be sure you’re putting your artificial limb on correctly and that it fits properly. If you think your artificial limb may not fit properly, or is causing pain, talk to your doctor.
Phantom limb pain prevention
Because the risk of developing phantom pain is higher for people who have experienced pain in the limb before amputation, some doctors recommend regional anesthesia (spinal or epidural) in the few hours or days leading up to amputation. This may reduce pain immediately following surgery and reduce the risk of lasting phantom limb pain.
Phantom limb pain diagnosis
Although there’s no medical test to diagnose phantom pain, doctors can identify the condition by collecting information about your symptoms and the circumstances, such as trauma or surgery, which occurred before the pain started.
Describing your pain precisely can help your doctor pinpoint your problem. Even though it’s common to have phantom pain and stump pain at the same time, treatments for these two problems may differ.
Phantom pain treatment
Finding a treatment to relieve your phantom pain can be difficult. Doctors usually begin with medications and then may add noninvasive therapies, such as acupuncture or transcutaneous electrical nerve stimulation (TENS).
More-invasive options include injections or implanted devices. Surgery is done only as a last resort.
Phantom pain medications
Although no medications specifically for phantom pain exist, some drugs designed to treat other conditions have been helpful in relieving nerve pain.
No single drug works for everyone, and not everyone benefits from medications. You may need to try different medications to find one that works for you.
Medications used in the treatment of phantom pain include:
- Antidepressants. Tricyclic antidepressants may relieve the pain caused by damaged nerves. Examples include amitriptyline, nortriptyline (Pamelor) and tramadol (Conzip, Ultram). These drugs work by modifying chemical messengers that relay pain signals. Antidepressants may also help you sleep, which can make you feel better. Possible side effects include sleepiness, dry mouth, blurred vision, weight gain, and a decrease in sexual performance or desire.
- Anticonvulsants. Epilepsy drugs — such as gabapentin (Gralise, Neurontin), pregabalin (Lyrica) and carbamazepine (Carbatrol, Epitol, Tegretol) — are often used to treat nerve pain. They work by quieting damaged nerves to slow or prevent uncontrolled pain signals. Side effects may include depression, anxiety, suicidal thoughts, irritability, and allergic reactions such as hives, fever and swelling.
- Narcotics. Opioid medications, such as codeine and morphine, may be an option for some people. Taken in appropriate doses under your doctor’s direction, they may help control phantom pain. However, you may not be able to take them if you have a history of substance abuse. Even if you don’t have a history of substance abuse, these drugs can cause many side effects, including constipation, nausea, vomiting or sedation.
- N-methyl-d-aspartate (NMDA) receptor antagonists. This class of anesthetics works by binding to the NMDA receptors on the brain’s nerve cells and blocking the activity of glutamate, a protein that plays a large role in relaying nerve signals. In studies, NMDA receptor antagonists ketamine and dextromethorphan were effective in relieving phantom pain. Side effects of ketamine include mild sedation, hallucinations or loss of consciousness. No side effects were reported from the use of dextromethorphan.
Noninvasive therapies
As with medications, treating phantom pain with noninvasive therapies is a matter of trial and observation. The following techniques may relieve phantom pain:
- Nerve stimulation. In a procedure called transcutaneous electrical nerve stimulation (TENS), a device sends a weak electrical current via adhesive patches on the skin near the area of pain. This may interrupt or mask pain signals, preventing them from reaching your brain. Used properly, TENS is safe. To avoid an unintentional shock, don’t wear a TENS device in the shower or tub or turn it up too high.
- Mirror box. This device contains mirrors that make it look like an amputated limb exists. The mirror box has two openings — one for the intact limb and one for the stump. The person then performs symmetrical exercises, while watching the intact limb move and imagining that he or she is actually observing the missing limb moving. Studies have found that this exercise may help relieve phantom pain.
- Acupuncture. The National Institutes of Health has found that acupuncture can be an effective treatment for some types of chronic pain. In acupuncture, the practitioner inserts extremely fine, sterilized stainless steel needles into the skin at specific points on the body. It’s thought that acupuncture stimulates your central nervous system to release the body’s natural pain-relieving endorphins. Acupuncture is generally considered safe when performed correctly.
Minimally invasive therapies
- Injection. Sometimes injecting pain-killing medications — local anesthetics, steroids or both — into the stump can provide relief of phantom limb pain.
- Spinal cord stimulation. Your doctor inserts tiny electrodes along your spinal cord. A small electrical current delivered to the spinal cord can sometimes relieve pain.
- Nerve blocks. This method uses medications that interrupt pain messages between the brain and the site of the phantom pain.
Surgery
Surgery may be an option if other treatments haven’t helped. Surgical options include:
- Brain stimulation. Deep brain stimulation and motor cortex stimulation are similar to spinal cord stimulation except that the current is delivered within the brain. A surgeon uses a magnetic resonance imaging (MRI) scan to position the electrodes correctly. Although the data are still limited, brain stimulation appears to be a promising option in selected individuals.
- Stump revision or neurectomy. If phantom pain is triggered by nerve irritation in the stump, surgical resection or revision can sometimes be helpful. But cutting nerves also carries the risk of making the pain worse.
New treatment options on the horizon
Newer approaches to relieve phantom pain include virtual reality goggles. The computer program for the goggles mirrors the person’s intact limb, so it looks like there’s been no amputation. The person then moves his or her virtual limb around to accomplish various tasks, such as batting away a ball hanging in midair.
Although this technique has been tested on only a few people, it appears to help relieve phantom pain.
Lifestyle and home remedies
You may not have control over whether you develop phantom pain after surgery, but you can reduce your discomfort and improve your quality of life. One or more of these approaches may help you get through a flare-up of phantom pain:
- Look for distractions. Find activities that take your focus off the pain, such as reading or listening to music.
- Stay physically active. Get your exercise by doing activities that you enjoy, such as gardening, walking, swimming or cycling.
- Take your medications. Follow your doctor’s directions in taking prescribed and over-the-counter pain medications. If you try herbal and other alternative medications, be sure to tell your doctor.
- Find ways to relax. Practice activities that reduce your emotional and muscular tension. Take a warm bath — not too hot, as heat may aggravate the pain. Lie down and follow helpful relaxation techniques, such as rhythmic breathing, meditation or visualization.
- Seek the support of other people. Find ways to get closer to others. Call friends, or join a support group or a group involved in your favorite hobby.
- Take care of your stump. Removing or putting on your prosthesis, massaging the stump, and applying TENS, cold or heat may reduce the pain.
Remember that managing phantom pain can make a big difference in how you feel. If one approach doesn’t provide relief, try something else rather than give up.
Coping and support
Learning to live without a limb, especially if you have phantom pain, can be challenging. Depression often accompanies pain. You may find it helpful to talk to a counselor or therapist.
An in-person or online support group can put you in touch with others who know what you’re going through. To find support, ask your doctor for a referral, either to a counselor or to a support group.
You also can contact the Amputee Coalition 1 for information on its National Peer Network, which can put you in touch with a variety of support services, including its Peer Visitor Program. This program can connect you with someone who’s been in your place and can talk to you about healing, share his or her experiences and offer advice.
- Amputee Coalition. https://www.amputee-coalition.org/[↩]