Contents
What is placenta previa
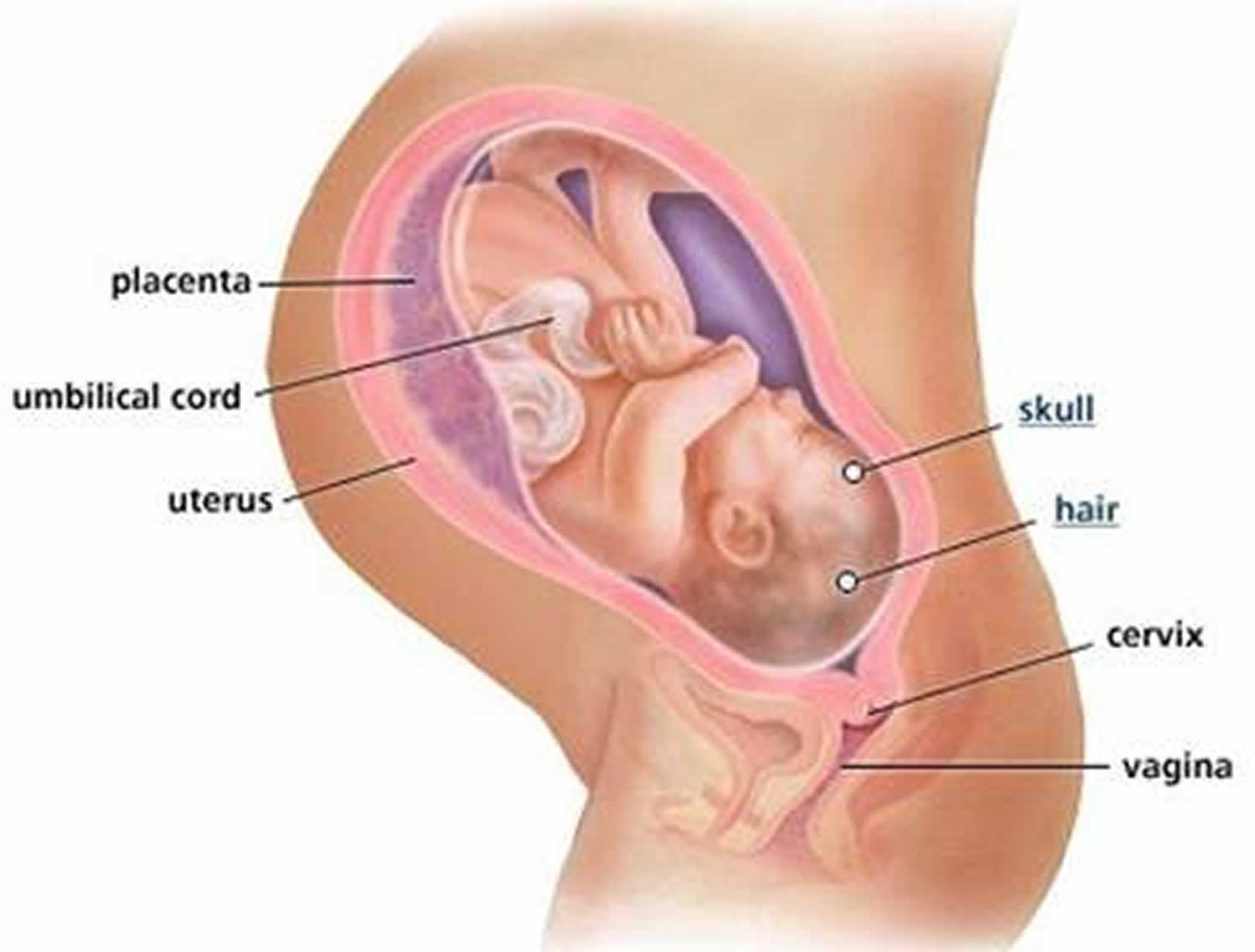
Placenta previa means your placenta is lying unusually low in your uterus, next to or covering your cervix. The cervix is the opening to the uterus that sits at the top of the vagina. This means that the placenta is lying either totally across the cervix (opening of the womb) or partially so. Placenta previa can cause life-threatening blood loss. The placenta (afterbirth) is the pancake-shaped organ normally located near the top of the uterus that supplies your baby with nutrients through the umbilical cord.
Classically patients with placenta previa present with an unprovoked, painless episode of vaginal bleeding. The amount of vaginal blood loss varies between minor to massive hemorrhage. Blood loss is most frequently intermittent with unpredictable recurrence.
Following an episode of bleeding, it is most likely that you will need to stay in hospital for a period of time so that both you and your baby can be monitored closely.
Placenta previa happens in about 1 in 200 pregnancies. The incidence has increased over time due to the rising incidence of cesarean section, which is a risk factor and improved diagnostics. While placental abruption can occur in women with no risk factors, there are factors, listed below, that increase the risk of a mother experiencing placenta previa.
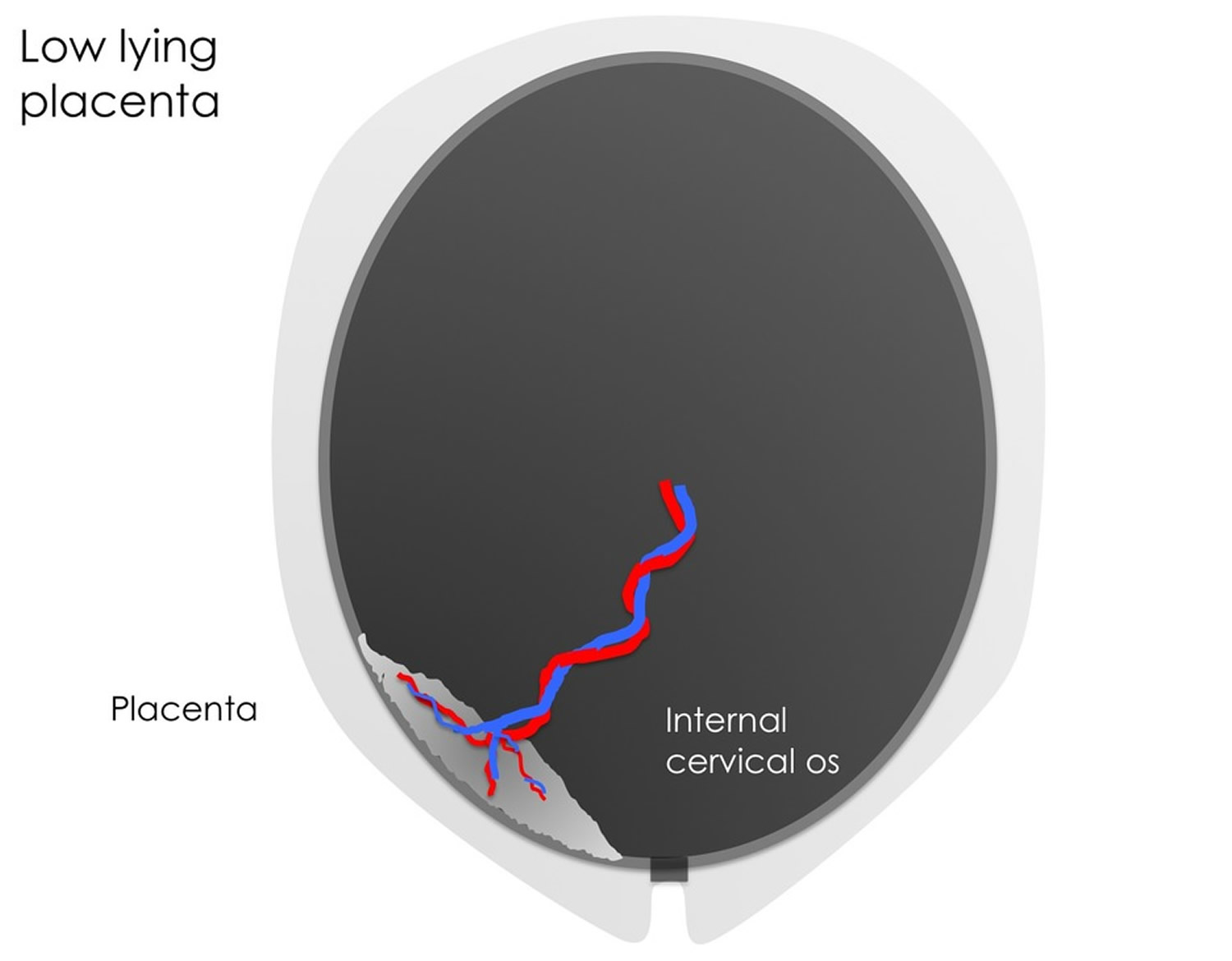
If you’re found to have placenta previa early in pregnancy, it’s not usually considered a problem. This is because your lower uterine segment only develops fully in the third trimester. This means that prior to the third trimester many placentas may appear to be located close to the cervix and are termed low lying placentas. However, as the pregnancy progresses and the lower segment develops fully, a large number (>90%) of low lying placentas detected in early pregnancy move away from the cervical opening. But if the placenta is still close to the cervix later in pregnancy, it can cause bleeding, which can lead to other complications and may mean that you’ll need to deliver early. If you have placenta previa when it’s time to deliver your baby, you’ll need to have a cesarean section.
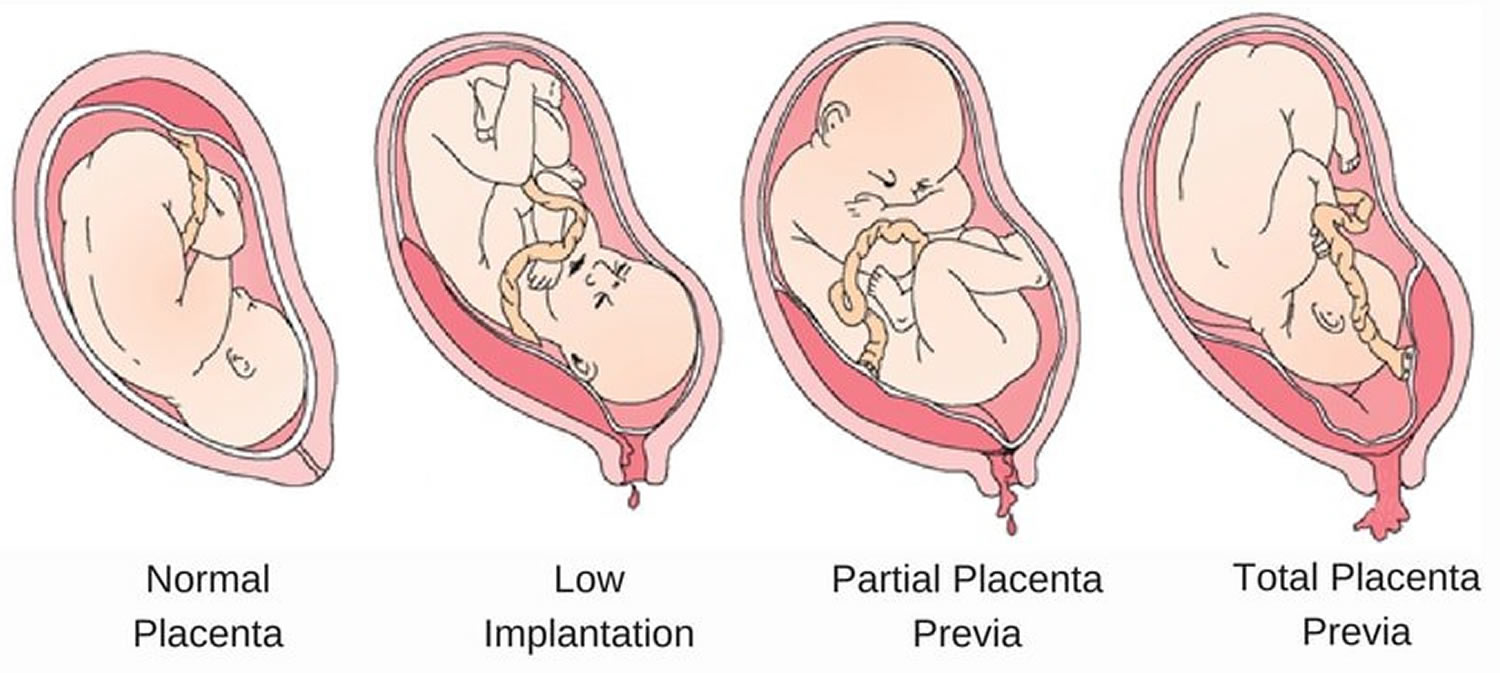
If the placenta covers the cervix completely, it’s called a complete or total previa. If placenta previa is right on the border of the cervix, it’s called a marginal previa. (You may also hear the term “partial previa,” which refers to a placenta that covers part of the cervical opening once the cervix starts to dilate.) If the edge of the placenta is within two centimeters of the cervix but not bordering it, it’s called a low-lying placenta.
The location of your placenta will be checked during your mid-pregnancy ultrasound exam (usually done between 16 to 20 weeks) and again later if necessary.
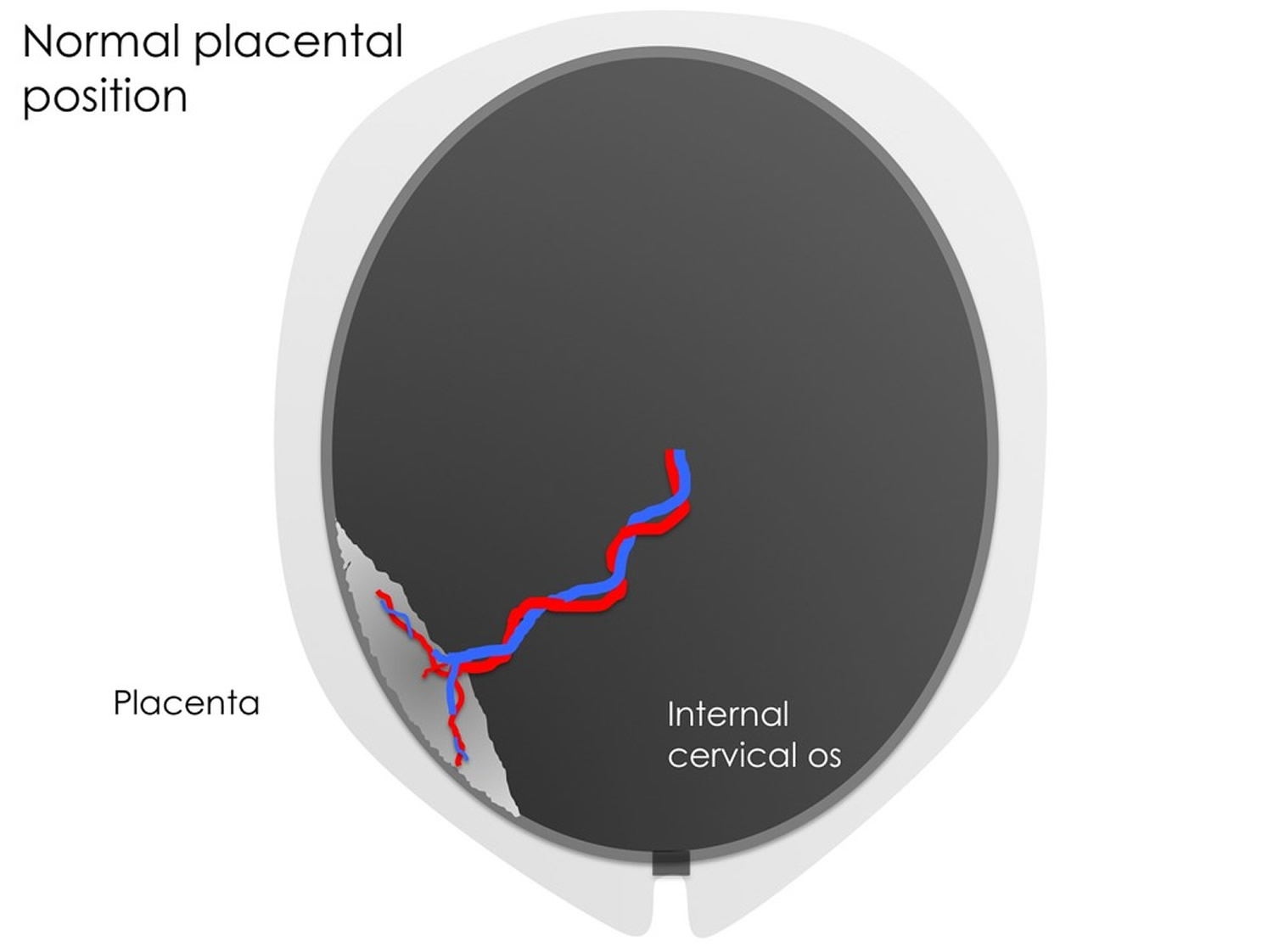
Normally, the placenta grows into the upper part of the uterus wall, away from the cervix. It stays there until your baby is born. During the last stage of labor, the placenta separates from the wall, and your contractions help push it into the vagina (birth canal). This is also called the afterbirth.
During labor, your baby passes through the cervix into the birth canal. If you have placenta previa, when the cervix begins to efface (thin out) and dilate (open up) for labor, blood vessels connecting the placenta to the uterus may tear. This can cause severe bleeding during labor and birth, putting you and your baby in danger.
A low-lying placenta is relatively common on the second trimester morphology ultrasound scan. As the fetus grows and the uterus expands, the lower uterine segment thins and grows disproportionately, such that in most cases the placenta is no longer low-lying by a follow-up study (usually performed at 32-34 weeks). This prospective study 1 indicates that women with a prior cesarean delivery and complete placenta previa diagnosed at second‐trimester ultrasound are less likely to have subsequent resolution of the placenta previa when compared to those without a history of cesarean delivery.
What is the placenta
The placenta is an organ attached to the lining of your womb during pregnancy.
It keeps your unborn baby’s blood supply separate from your own blood supply, as well as providing a link between the two. The link allows the placenta to carry out functions that your unborn baby can’t perform for itself.
The placenta is connected to your baby by the umbilical cord. Your baby is inside a bag of fluid called the amniotic sac, which is made of membranes.
What does the placenta do?
Oxygen and nutrients pass from your blood supply into the placenta. From there, the umbilical cord carries the oxygen and nutrients to your unborn baby. Waste products from the baby, such as carbon dioxide, pass back along the umbilical cord to the placenta and then into your bloodstream, for your body to dispose of them.
The placenta produces hormones that help your baby grow and develop. The placenta also gives some protection against infection for your baby while it’s in the womb, protecting it against most bacteria. However, it doesn’t protect your baby against viruses.
Alcohol, nicotine and other drugs can also cross the placenta and can cause damage to your unborn baby.
Towards the end of your pregnancy, the placenta passes antibodies from you to your baby, giving them immunity for about three months after birth. However, it only passes on antibodies that you already have.
Figure 1. Normal placenta and pregnancy – the placenta attaches to the wall of the uterus (womb) and supplies the baby with food and oxygen through the umbilical cord.
What happens after my baby is born?
After your baby is born, more contractions will push the placenta out through the vagina.
Your midwife will offer you a medicine to stimulate your contractions and help push the placenta out. They’ll inject the medicine into your thigh just as the baby is born. It makes your womb contract so the placenta comes away from the wall of your womb. This also helps prevent the heavy bleeding some women experience.
Breastfeeding your baby as soon as possible after the birth helps your womb to contract and push the placenta out.
You may choose to let your body push the placenta out in its own time, which may involve some loss of blood.
After the birth, your midwife will check the placenta and membranes, to make sure that they’re complete and nothing has been left behind.
If you have a caesarean section, after your baby is born, the placenta will also be delivered.
Placenta previa types
Low-lying placenta (Grade 1)
Low-lying placenta occurs when the placenta extends into the lower uterine segment and its edge lies too close to the internal os of the cervix, without covering it. The term is usually applied when the placental edge is within 0.5-5.0 cm of the internal cervical os 2. Some alternatively give the term when the placental edge is within 2 cm from the internal cervical os 3.
It has also classified under the benign end of the spectrum of type 1 placenta previa, although some restrict the term “previa” only for the situation in which the placenta covers the internal cervical os.
Figure 3. Low-lying placenta
The estimated prevalence of low-lying placenta may be as high as 10-30% of all pregnancies 4. The majority of placentas classified as low-lying in early pregnancy (12-14 weeks) reach a normal position on subsequent scanning later during the pregnancy due to placental trophotropism.
Transvaginal ultrasound is more accurate for evaluation of a low-lying placenta than transabdominal ultrasound 5.
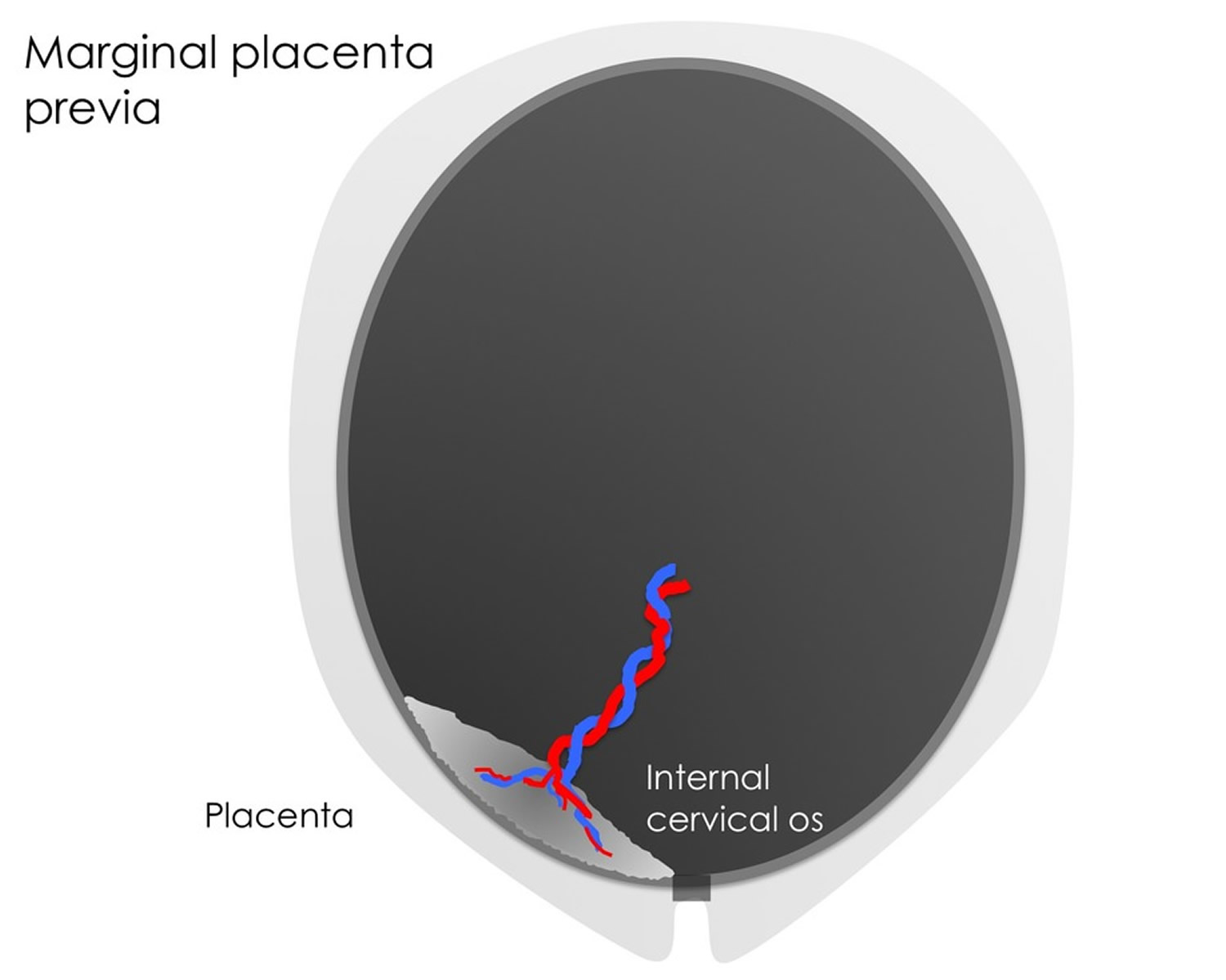
Marginal placenta previa (Grade 2)
The placental tissue reaches the margin or right on the border of the internal cervical os, but does not cover it.
Figure 4. Marginal placenta previa
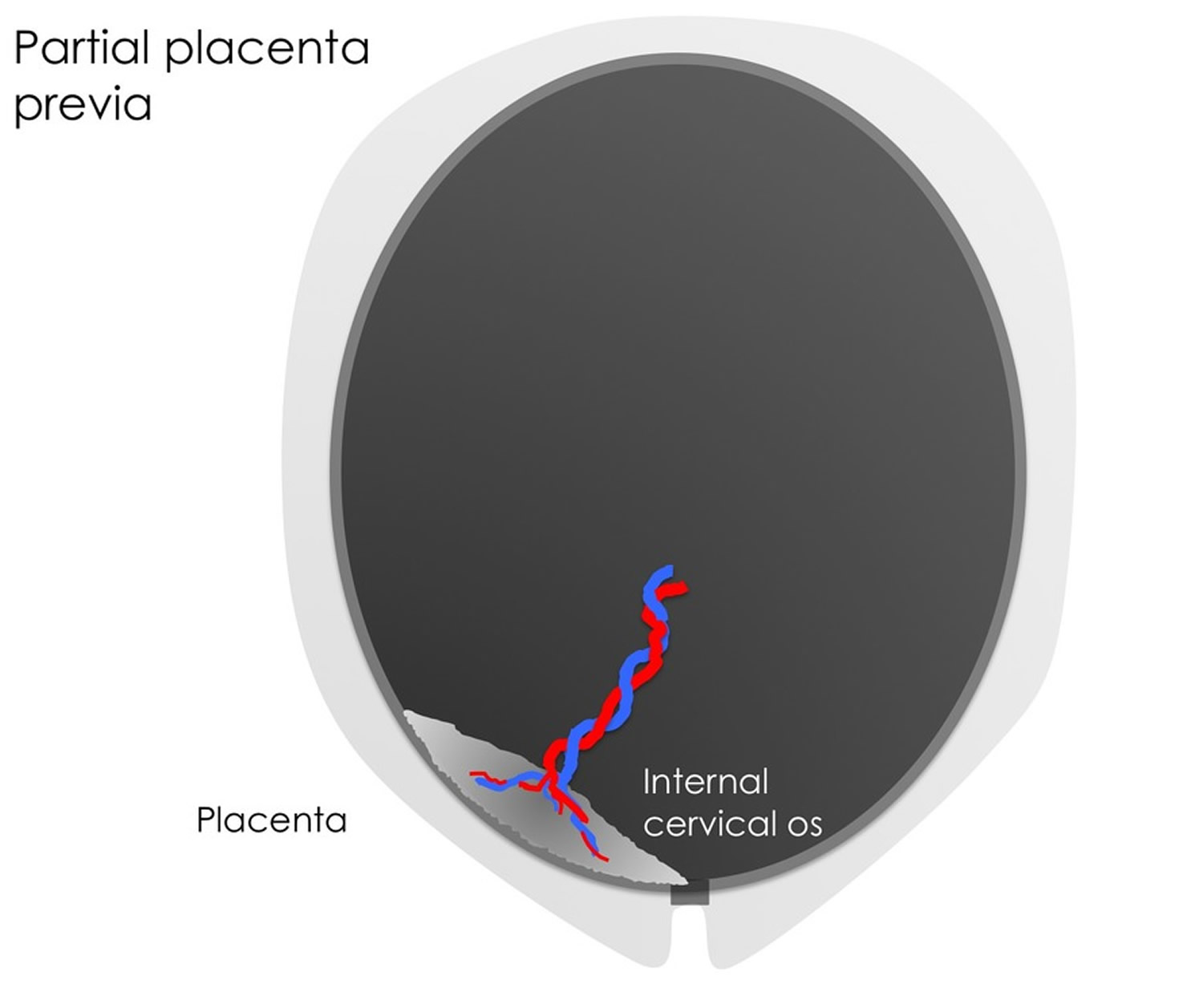
Partial placenta previa (Grade 3)
Refers to a placenta that covers part of the cervical opening once the cervix starts to dilate.
Figure 5. Partial placenta previa
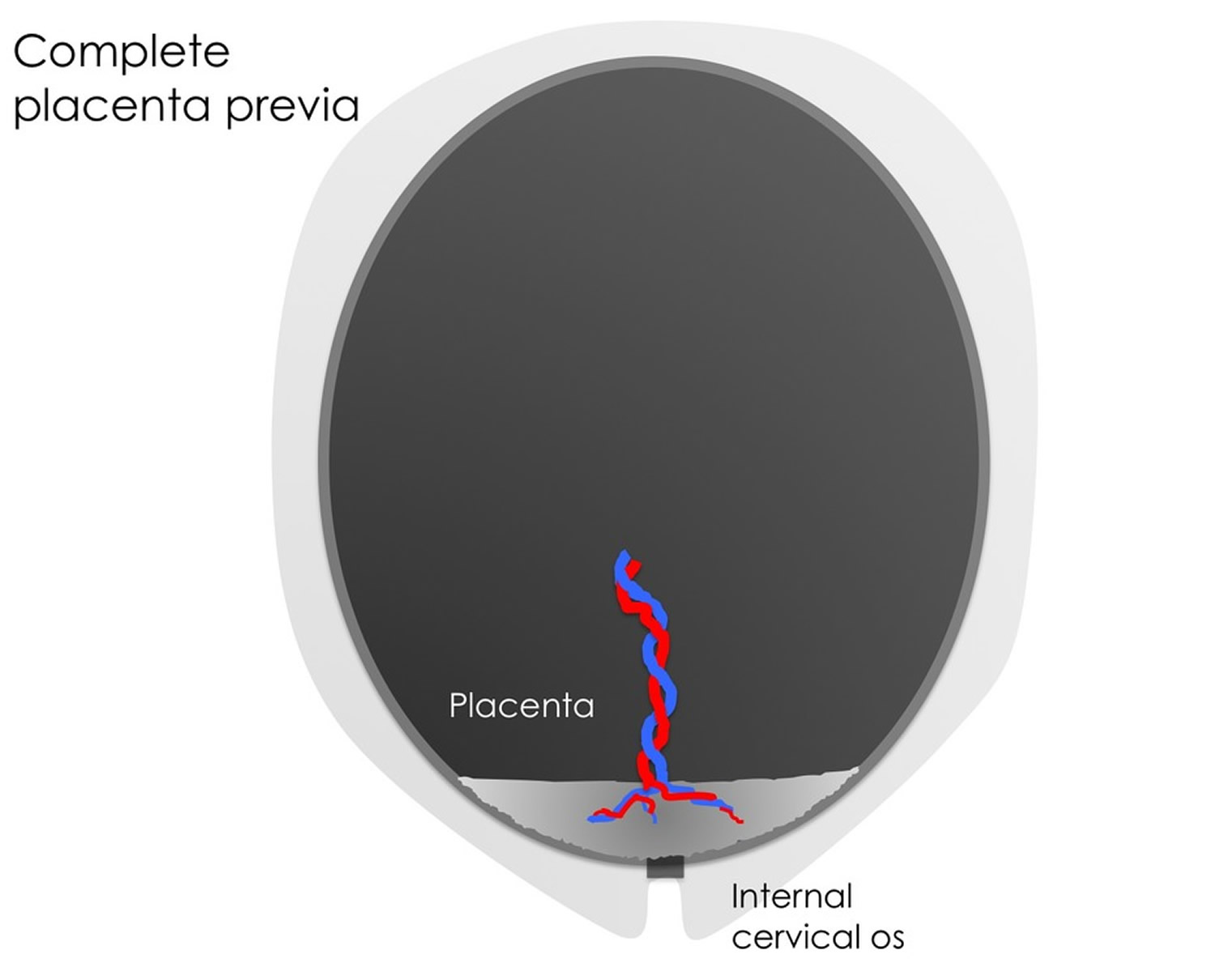
Complete placenta previa (Grade 4)
If the placenta covers the the internal cervical os completely, it’s called a complete or total placenta previa. In the case of a complete placenta praevia, a cesarian section is required for delivery to avoid the risk of fetal and maternal hemorrhage.
Sometimes grades 1 and 2 are termed a “minor” or “partial” placenta previa, and grades 3 and 4 are termed a “major” placenta previa 6.
Figure 6. Complete placenta previa
Placenta previa causes
Scientists don’t know what causes placenta previa. However, you may be at higher risk for placenta previa if:
- You smoke cigarettes.
- You use cocaine.
- You’re 35 or older.
- You’ve been pregnant before.
- You’ve had placenta previa in a past pregnancy.
- You’re pregnant with twins, triplets or more.
- You’ve had surgery on your uterus, including a c-section or a D&C (dilation and curettage). A D&C is when a doctor removes tissue from the lining of a woman’s uterus. Some women have a D&C after a miscarriage.
If you’ve had placenta previa in a past pregnancy, you have a 2 to 3 in 100 (2 to 3 percent) chance of having it again.
Associated conditions with placenta previa include placenta accreta, malpresentation, preterm premature rupture of membranes, intrauterine growth restriction, and vasa previa 7.
Risk Factors for placenta previa
The cause of placenta previa remains unknown, however risk factors include:
- High parity
- Increased maternal age
- Uterine abnormalities
- Smoking
- Cocaine use
- Multiple pregnancy
- Previous placenta previa
- Previous Cesarean section
- Termination of pregnancy
- Intrauterine surgery
- Maternal history of smoking
- Erythroblastosis fetalis. This occurs when the mother’s immune system attacks the blood cells of the baby. For example, a mother who has an Rh-negative blood type who is carrying a baby with an Rh-positive blood type may have an immune response that attacks and destroys the Rh-positive blood cells of the baby.
- Assisted reproductive techniques (in vitro fertilization and intracytoplasmic sperm injection).
The increased risk of placenta previa following caesarean section is highest for the pregnancy immediately following the caesarean and decreases in subsequent pregnancies. Prior cesarean delivery is one of the most important risk factors for development of placenta previa, and the risk of placenta previa increases as a woman has more cesarean deliveries. After 1 cesarean delivery, the risk of previa is reported to be approximately 1.9%; the risk increases to 5.5% after 2 cesarean deliveries and reaches 14.3% after 3 cesarean deliveries 8.
Placenta previa prevention
Scientists don’t know how to prevent placenta previa. But you may be able to reduce your risk by not smoking and not using cocaine. You also may be able to lower your chances of having placenta previa in future pregnancies by having a c-section only if it’s medically necessary. If your pregnancy is healthy and there are no medical reasons for you to have a c-section, it’s best to let labor begin on its own. The more c-sections you have, the greater your risk of placenta previa.
Placenta previa prognosis
If your placenta was determined as low lying from an ultrasound scan performed prior to the third trimester of pregnancy, it is most likely that as the lower segment of the uterus develops fully that your placenta will move away from the opening of the cervix.
For those women in which this does not occur, placenta previa can be responsible for bleeding from the vagina either during pregnancy, during labor or following labor. This may result in anemia, hysterectomy, a blood transfusion and/or possible infection. In the Western world, placenta previa is a rare cause of maternal mortality, approximately 0.03%.
Fetal death is slightly higher than maternal mortality, approximately 4-8%, and is associated with pre-term birth (50%) and intrauterine growth restriction. While the cause is unknown, the risk of birth defects in the fetus are doubled.
Placenta previa complications
If you have placenta previa, your health care provider will monitor you and your baby to reduce the risk of these serious complications:
- Bleeding. Severe, possibly life-threatening vaginal bleeding (hemorrhage) can occur during labor, delivery or in the first few hours after delivery.
- Preterm birth. Severe bleeding may prompt an emergency C-section before your baby is full term.
Placenta previa signs and symptoms
The most common symptom of placenta previa is painless bright red vaginal bleeding during the second half of pregnancy. Some women also have contractions. However, not all women with placenta previa have vaginal bleeding. In fact, about one-third of women with placenta previa don’t have this symptom.
See your health care provider right away if you have vaginal bleeding anytime during your pregnancy. If the bleeding is severe, go to the hospital.
In many women diagnosed with placenta previa early in their pregnancies during their routine ante-natal check up and ultrasound scan, the placenta previa usually resolves. As your uterus grows, it might increase the distance between the cervix and the placenta. The more the placenta covers the cervix and the later in the pregnancy that it remains over the cervix, the less likely it is to resolve.
Placenta previa diagnosis
On examination, your doctor will be examining you for signs and symptoms of placental previa as well as other differential diagnoses depending on your presenting symptoms. They will be especially concerned with your vital signs, including heart rate and blood pressure to assess whether you are showing any signs of shock.
Other than your health, they will also be concerned with the health of your unborn child. They will be interested in if your baby is moving, its heart rate and how many weeks gestation your baby is. If there are any signs of fetal compromise, active bleeding, uterine activity or tenderness a cardiotocograph (CTG) will be applied for continuous monitoring.
Several blood tests will be ordered and an ultrasound may be necessary.
An ultrasound usually can find placenta previa and pinpoint the placenta’s location. In some cases, your provider may use a transvaginal ultrasound instead.
Diagnosis might require a combination of abdominal ultrasound and transvaginal ultrasound. Your health care provider will take care with the position of the transducer in your vagina so as not to disrupt the placenta or cause bleeding.
If your health care provider suspects placenta previa, he or she will avoid routine vaginal exams to reduce the risk of heavy bleeding. You might need additional ultrasounds to check the location of your placenta during your pregnancy to see if placenta previa resolves.
Even if you don’t have vaginal bleeding, a routine, second trimester ultrasound may show that you have placenta previa. Don’t be too worried if this happens. Placenta previa found in the second trimester fixes itself in most cases.
Ultrasound
Due to placental trophotropism, the diagnosis of a placenta previa is not usually made before 20 weeks.
During the ‘routine’ 18 to 21-week morphology scan, the distance between the lower edge of the placenta and the internal cervical os should be measured. If it lies within a few centimeters of the cervical os, then a repeat ultrasound at ~32 weeks should be performed to ensure that the edge has migrated further away.
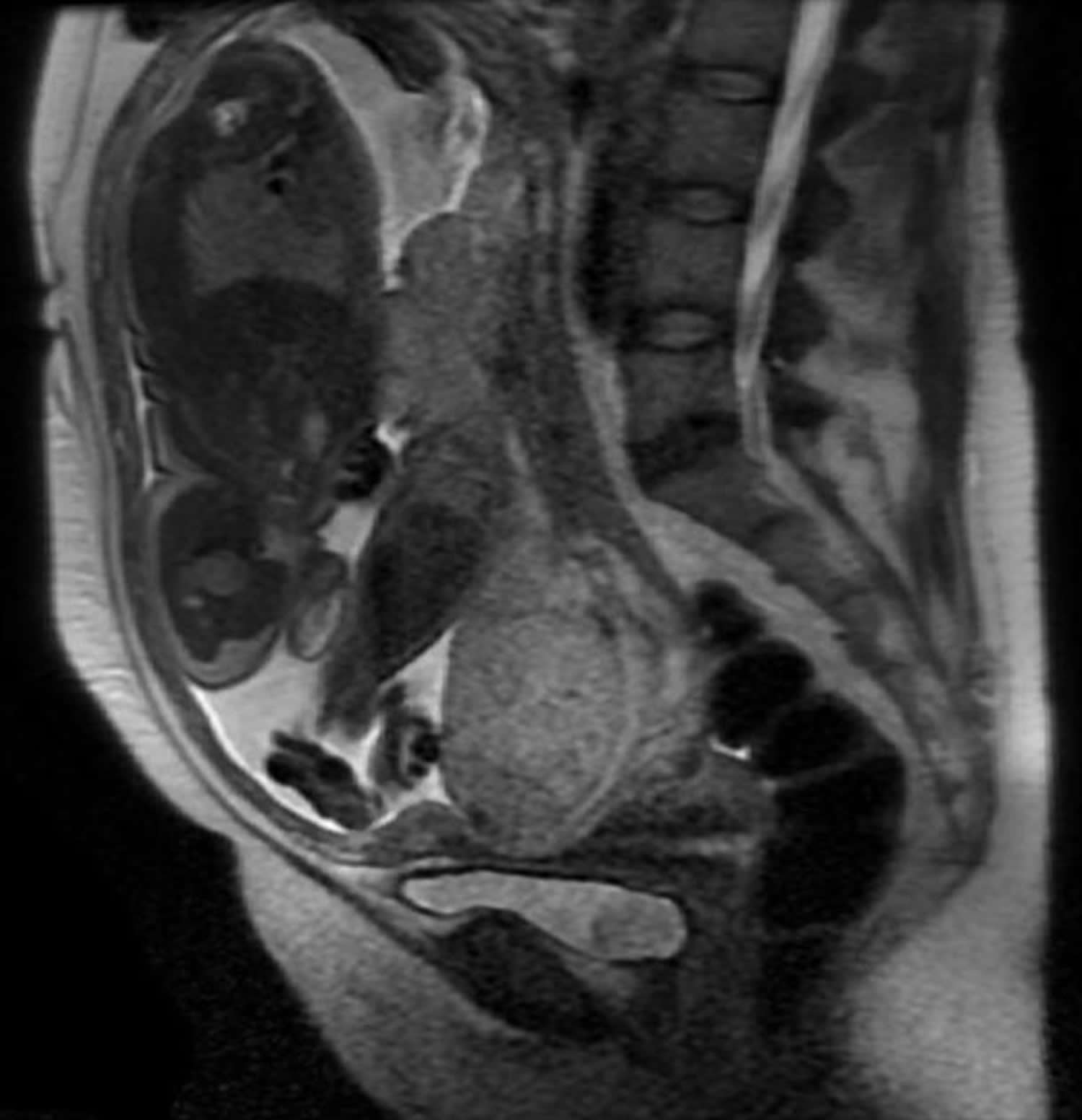
MRI (Magnetic Resonance Imaging)
MRI is the gold standard imaging modality for the placenta and its relationship to the cervix, although in most instances it is not required. Sagittal images best demonstrate the relationship of the placenta to the internal cervical os.
Figure 8. Placenta previa MRI scan – MRI demonstrates a complete placenta previa
Placenta previa treatment
Treatment depends on how far along you are in your pregnancy, the seriousness of your bleeding and the health of you and your baby. The goal is to keep you pregnant as long as possible. Obstetricians recommend cesarean birth (c-section) for nearly all women with placenta previa to prevent severe bleeding.
Management of the bleeding depends on various factors, including:
- The amount of bleeding
- Whether the bleeding has stopped
- How far along your pregnancy is
- Your health
- Your baby’s health
- The position of the placenta and the baby
In cases where the fetus is pre-term and the bleeding is minimal, the goal is to delay the delivery to allow for maturation of the fetus without increasing the risk to the mother. In most cases this will involve admission to hospital where you and your baby can be monitored closely. Unless there is spontaneous labor of heavy sustained bleeding necessitating emergency caesarean delivery, delivery is by planned caesarean section at 37-38 weeks gestation.
If you are bleeding as a result of placenta previa, you need to be closely monitored in the hospital. If tests show that you and your baby are doing well, your obstetrician may give you treatment to try to keep you pregnant for as long as possible.
If you have a lot of bleeding, you may be treated with blood transfusions. A blood transfusion is having new blood put into your body. Your obstetrician also may give you medicines called corticosteroids. These medicines help speed up development of your baby’s lungs and other organs.
Your obstetrician may want you to stay in the hospital until you give birth. If the bleeding stops, you may be able to go home. If you have severe bleeding due to placenta previa at about 34 to 36 weeks of pregnancy, your obstetrician may recommend an immediate c-section.
At 36 to 37 weeks, your obstetrician may suggest an amniocentesis to test the amniotic fluid around your baby to see if her/his lungs are fully developed. If they are, your obstetrician may recommend an immediate c-section to avoid risks of future bleeding.
At any stage of pregnancy, a c-section may be necessary if you have dangerously heavy bleeding or if you and your baby are having problems.
If the bleeding becomes life threatening, resuscitation and stabilization of the mother is the primary focus followed by delivery of the baby by emergency cesarean section.
Coping and support
If you’re diagnosed with placenta previa, you’re sure to worry about how your condition will affect you, your baby and your family. Some of these strategies might help you cope:
- Learn about placenta previa. Having information about your condition can help ease your fears. Talk to your health care provider, research on your own and connect with other women who’ve had placenta previa.
- Prepare for a C-section. Placenta previa might prevent you from delivering your baby vaginally. Remind yourself that you and your baby’s health are more important than the method of delivery.
- Make the best of rest. Although you won’t be confined to bed, you will have to take it easy. Fill your days by planning for your baby’s arrival. Read about newborn care or purchase newborn necessities, either online or by phone. Or use the time to catch up on thank-you notes or other nontaxing tasks.
- Take care of yourself. Surround yourself with things that comfort you, such as good books or music you love. Give your partner, friends and loved ones suggestions for ways to help, such as visiting or making one of your favorite foods.
- Lal, A. K., Nyholm, J. , Wax, J. , Rose, C. H. and Watson, W. J. (2012), Resolution of Complete Placenta Previa. Journal of Ultrasound in Medicine, 31: 577-580. doi:10.7863/jum.2012.31.4.577 https://onlinelibrary.wiley.com/doi/10.7863/jum.2012.31.4.577[↩]
- Merz E, Bahlmann F. Ultrasound in obstetrics and gynecology. Thieme Medical Publishers. (2005) ISBN:1588901475.[↩]
- Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental Imaging: Normal Appearance with Review of Pathologic Findings. Radiographics : a review publication of the Radiological Society of North America, Inc. 37 (3): 979-998. doi:10.1148/rg.2017160155 https://www.ncbi.nlm.nih.gov/pubmed/28493802[↩]
- Chama CM, Wanonyi IK, Usman JD. From low-lying implantation to placenta praevia: a longitudinal ultrasonic assessment. J Obstet Gynaecol. 2004;24 (5): 516-8. doi:10.1080/01443610410001722545 https://www.ncbi.nlm.nih.gov/pubmed/15369930[↩]
- Lauria MR, Smith RS, Treadwell MC, Comstock CH, Kirk JS, Lee W, Bottoms SF. The use of second-trimester transvaginal sonography to predict placenta previa. Ultrasound in obstetrics & gynecology : the official journal of the International Society of Ultrasound in Obstetrics and Gynecology. 8 (5): 337-40. doi:10.1046/j.1469-0705.1996.08050337.x https://www.ncbi.nlm.nih.gov/pubmed/8978009[↩]
- Impey L. Obstetrics & gynaecology. Wiley-Blackwell. (2004) ISBN:1405107219.[↩]
- Ananth CV, Demissie K, Smulian JC, Vintzileos AM. Relationship among placenta previa, fetal growth restriction, and preterm delivery: a population-based study. Obstet Gynecol 2001; 98:299–306. https://www.ncbi.nlm.nih.gov/pubmed/11506849[↩]
- Lilić V, Tasić M, Radović-Janosević D, Stefanović M, Antić V. Placental complications after a previous cesarean section [in Serbian]. Med Pregl 2009; 62:212–216. https://www.ncbi.nlm.nih.gov/pubmed/19650556[↩]