Contents
What is pneumomediastinum
Pneumomediastinum also known as mediastinal emphysema is an uncommon and usually a self-limited condition where there is air in the mediastinum 1, 2, 3, 4, 5, 6, 7. The mediastinum is the space in the middle of your chest, between your lungs and around your heart. The air or gas may originate from your lungs, trachea, central bronchi, esophagus, and peritoneal cavity and track from the mediastinum to your neck or abdomen.
Spontaneous pneumomediastinum is an uncommon condition presenting in approximately one in 1,000 to one in 40,000 emergency department referrals 8, 9, 10. Young patients with spontaneous pneumomediastinum typically present with a history of asthma or recent inhalation of cocaine, methamphetamine, ecstasy, marijuana or hydrocarbons 11, 12, 13, 14, 15, 16, 17, 18. Other causes include barotrauma in asthmatics and chronic obstructive pulmonary disease (COPD) patients, rapid ascent in scuba divers, valsalva maneuvers, vomiting, infections, blast injuries and iatrogenic injuries from endoscopy or surgery 19, but can also happen with no known cause (idiopathic).
Pneumomediastinum can either be spontaneous or secondary. Spontaneous pneumomediastinum (SPM) isn’t caused by injury or illness, or the cause is unknown (idiopathic). Secondary pneumomediastinum develops because of an injury, illness or surgery. While pneumomediastinum itself is usually harmless, the underlying causes can be serious. Potential life-threatening causes include esophageal rupture (Boerhaave syndrome) and tension pneumothorax, but these are historically evident at presentation 20.
Some people with pneumomediastinum don’t have any symptoms. Pneumomediastinum usually causes chest pain behind the breastbone (nonspecific pleuritic chest pain) with shortness of breath, which may spread to the neck or arms. The pain may be worse when you take a breath or swallow.
Seek immediate medical attention or go to the nearest emergency room immediately if you’re experiencing:
- Chest pain.
- Shortness of breath.
- Severe face or neck swelling.
- Lightheadedness.
Because a subset of patients with pneumomediastinum have serious underlying condition, extensive workups are often necessary. During a physical exam, your doctor may feel small bubbles of air under the skin of your chest, arms, or neck called subcutaneous emphysema. When examined, sometimes the person can look very puffy (swollen) in the face and eyes. This can look worse than it actually is. Hearing a crunching sound in time with your heartbeat (Hamman’s sign) is a sign that you might have air in your mediastinum.
A chest x-ray or CT scan of the chest may be done. This is to confirm that air is in the mediastinum, and to help diagnose a hole in the trachea or esophagus.
A barium swallow may be indicated if Boerhaave syndrome (esophageal rupture following vomiting) is suspected from the history. If the pneumomediastinum has not resolved after 1 week, a CT of the chest is indicated to look for a source of persistent air leak.
There’s no specific treatment for pneumomediastinum. Often, no treatment is needed because your body will gradually absorb the air on its own over a period of one to two weeks without intervention and rarely recur 21. Breathing high concentrations of oxygen may speed this process. If you have an underlying health condition, like an infection or injury to an internal organ, your doctor will treat you for that condition.
Your doctor may admit you to the hospital for 24 hours or longer for observation or treatment. While there, your doctor might treat you with:
- Oxygen therapy. Breathing in additional oxygen can help the air absorb into your body faster.
- Medication. Medication like pain relievers or cough suppressants can ease your symptoms until your body absorbs the extra air.
- Needle aspiration. If you have a lot of air that’s pressing on structures inside of your body, a doctor may remove some of the air with a needle or put a drain in. This is rare.
- Your doctor may put in a chest tube if you also have a collapsed lung (pneumothorax). You may also need treatment for the cause of the pneumomediastinum. A hole in the trachea or esophagus needs to be repaired with surgery.
Your outlook (prognosis) depends on the disease or events that caused the pneumomediastinum. People with spontaneous pneumomediastinum can make a full recovery and rarely have it happen again. People with spontaneous pneumomediastinum spend an average of three days in the hospital, but are sometimes there for a week or more. People with underlying causes of pneumomediastinum can be hospitalized for several weeks. If you have secondary pneumomediastinum, recovery will depend on the severity of your underlying condition. Some conditions that cause pneumomediastinum can be fatal.
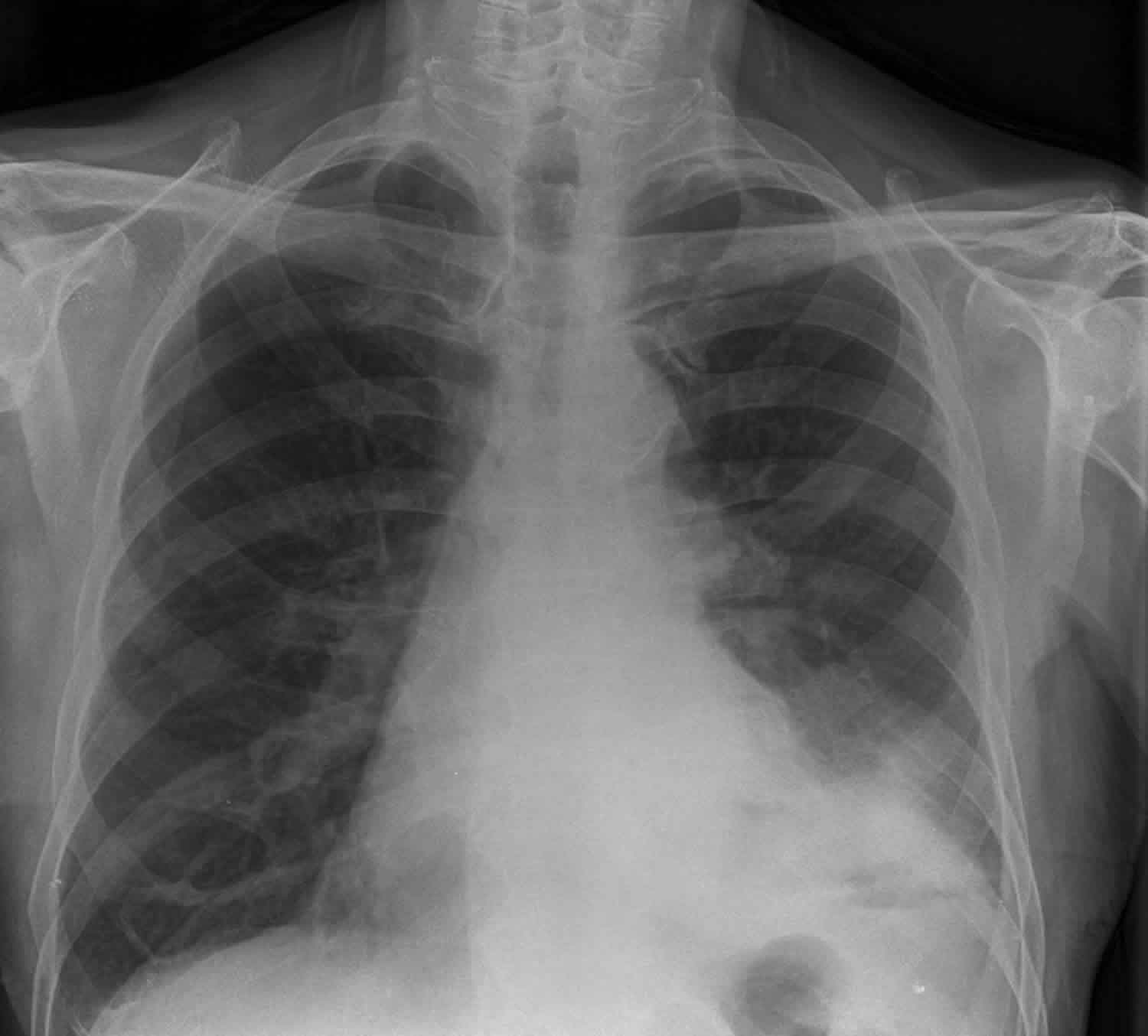
Figure 1. Pneumomediastinum
Footnotes: A 16 year old boy without asthma or smoking history presented with the sudden onset of behind the sternum chest pain for two days after performing a 4 hour push-up exercise. Chest X-ray shows gross subcutaneous emphysema over the neck and pneumomediastinum with a continuous diaphragm sign (black arrows). The gas outlining the mediastinum, aorta (red arrowheads), and heart (yellow arrowheads) extends into the neck.
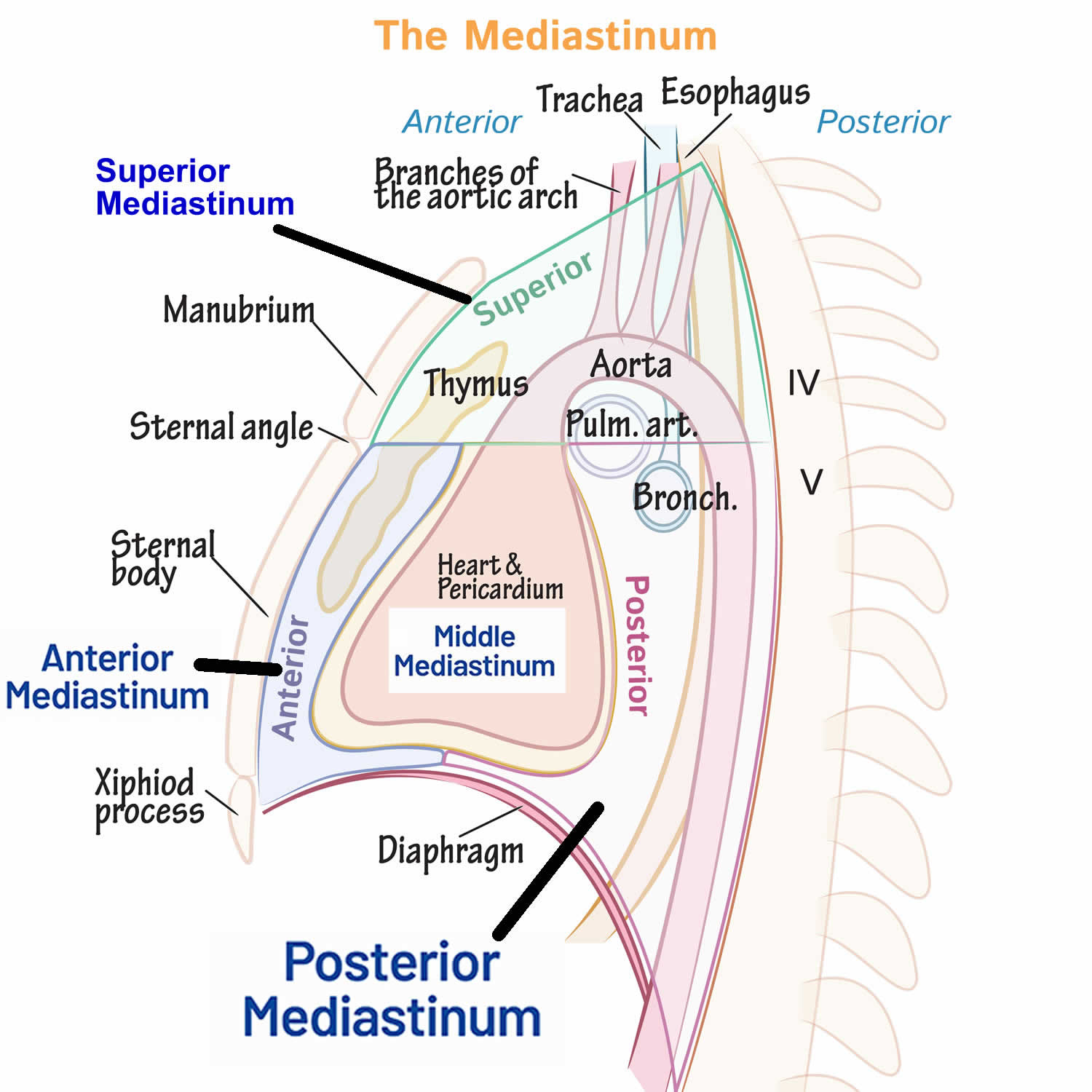
[Source 6 ]Figure 2. Mediastinum
Is pneumomediastinum an emergency?
Spontaneous pneumomediastinum is not an emergency. But if you have air in your mediastinum due to an injury or illness, you should be treated right away. Go to the nearest emergency room or seek medical care immediately if you have chest pain and shortness of breath. These could be signs of life-threatening illnesses or conditions.
Can pneumomediastinum be fatal?
Pneumomediastinum isn’t fatal on its own. But sometimes, serious, life-threatening health conditions can cause it. Your doctor will look for causes of the air leak and treat them if necessary.
Can pneumomediastinum be prevented?
Pneumomediastinum is rare and scientists don’t understand all the causes or risk factors. There aren’t any recommended ways to prevent it. Not smoking and not using inhaled recreational drugs might lower your risk.
What is the difference between pneumomediastinum and pneumothorax?
How do you recover from pneumomediastinum?
People with spontaneous pneumomediastinum spend an average of three days in the hospital, but are sometimes there for a week or more. People with underlying causes of pneumomediastinum can be hospitalized for several weeks.
Can pneumomediastinum be cured?
Spontaneous pneumomediastinum usually goes away on its own without treatment. If it wasn’t caused by an underlying health condition, it shouldn’t come back. The health conditions that cause it can sometimes be cured.
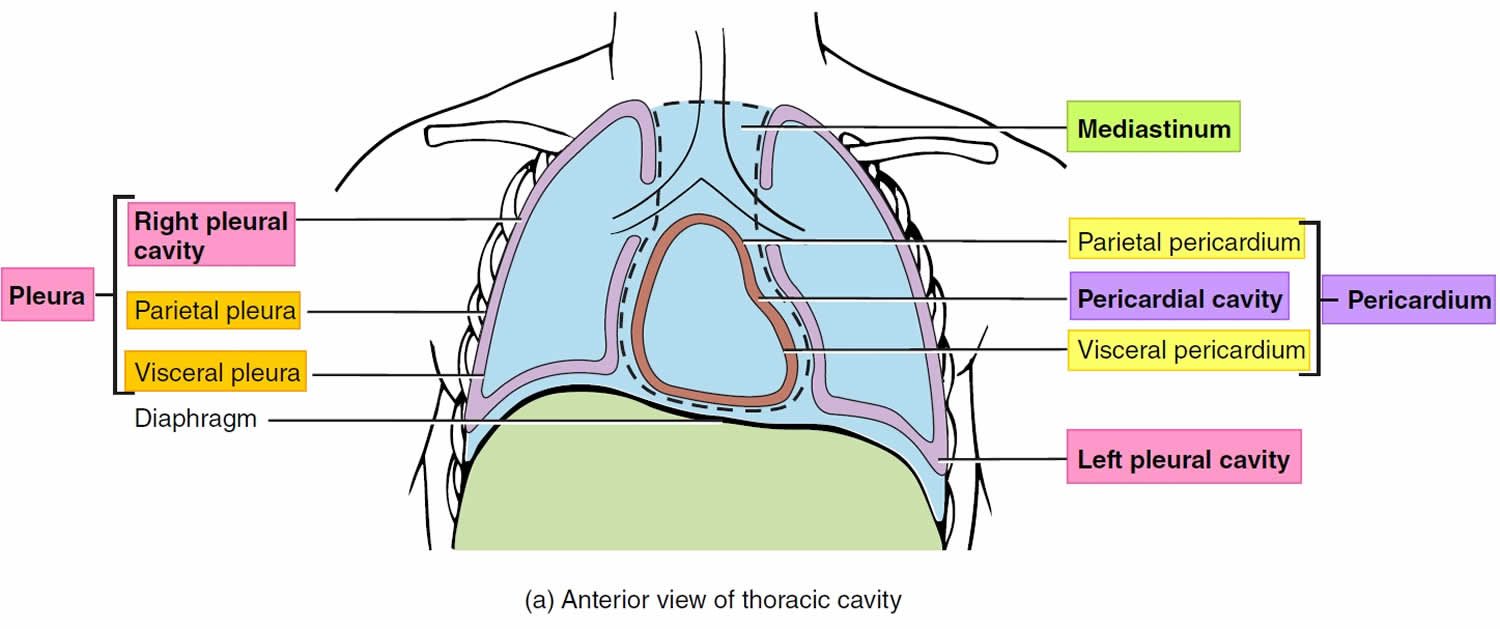
Chest anatomy
Your chest cavity also called the thoracic cavity is formed by the ribs, the muscles of the chest, the sternum (breastbone), and the thoracic portion of the vertebral column. Within your thoracic cavity are 3 smaller cavities: (a) 2 pleural cavities (fluid-filled spaces one around each lung), your left pleural cavity (holds your left lung) and your right pleural cavity (holds your right lung) and (b) a central portion of your thoracic cavity between your lungs called the mediastinum (media- = middle; -stinum = partition). The mediastinum is the central portion of your thoracic cavity between your lungs, extending from the base of your neck (from your first rib and sternum) to the diaphragm. The mediastinum contains your heart (pericardial cavity, peri- = around; -cardial = heart, a fluid-filled space that surrounds your heart), the major blood vessels connected to your heart and lungs, the trachea (windpipe) and bronchi, the esophagus (foodpipe), the thymus, and lymph nodes but not your lungs. Your right and left lungs are on either side of the mediastinum. The diaphragm is a dome-shaped muscle that separates the thoracic cavity from the abdominopelvic cavity.
Your mediastinum is divided into several parts, which researchers call compartments. The traditional or classical model divides your mediastinum into four parts:
- Superior mediastinum: The top part, located superior to (above) your heart.
- Anterior mediastinum: The part anterior to (in front of) your heart, between your heart and your sternum (breastbone).
- Middle mediastinum: The part that contains your heart.
- Posterior mediastinum: The part posterior to (behind) your heart.
A membrane is a thin, pliable tissue that covers, lines, partitions, or connects internal organs (viscera). One example is a slippery, double-layered membrane associated with body cavities that does not open directly to the exterior called a serous membrane. Serous membrane covers your internal organs (viscera) within the thoracic and abdominal cavities and also lines the walls of the thorax and abdomen. The parts of a serous membrane are (1) the parietal layer (outer layer), a thin epithelium that lines the walls of the cavities, and (2) the visceral layer (inner layer), a thin epithelium that covers and adheres to the viscera within the cavities. Between the two layers is a potential space that contains a small amount of lubricating fluid (serous fluid). The fluid allows the internal organs (viscera) to slide somewhat during movements, such as when the lungs inflate and deflate during breathing.
Within the right and left sides of your thoracic cavity (chest cavity), the compartments that contain your lungs, on either side of the mediastinum, are lined with a membrane called the parietal pleura (outer serous membrane) lining the inside of your rib cage (parietal pleura lines the chest wall) and covering the superior surface of the diaphragm. A similar membrane, called the visceral pleura (inner serous membrane), clings to the surface of your lungs forming the external surface of your lung. The visceral (inner) and parietal (outer) pleural membranes are separated only by a thin film of watery fluid called serous fluid, which is secreted by the parietal and visceral pleural membranes. Although no actual space normally exists between the parietal (outer) and visceral (inner) pleural membranes, the potential space between them is called the pleural cavity. The parietal pleura (outer membrane) and visceral pleura (inner membrane) slide with little friction across the cavity walls as your lungs move, expand and collapse during respiration.
Your heart, which is located in the broadest portion of the mediastinum, is surrounded by pericardial membranes called the pericardium. Your pericardium is a protective, fluid-filled sac that surrounds your heart and helps it function properly.
Figure 3. Chest anatomy
Figure 4. Thoracic cavity
Footnote: The black dashed lines indicate the borders of the mediastinum.
Pneumomediastinum causes
Pneumomediastinum is usually caused by air moving into your mediastinum from an injury or disease to an internal organ or structure. This includes your airways (trachea or bronchi), air sacs in your lungs (alveoli), tube from your throat to your stomach (esophagus) or intestines. Anything that increases pressure in your chest can cause spontaneous pneumomediastinum, though this is rare. Sometimes, doctors can’t find the cause (idiopathic).
Increased pressure in the lungs or airways may be caused by:
- Too much coughing
- Repeated bearing down to increase abdominal pressure (such as pushing during childbirth, a bowel movement or weight lifting)
- Sneezing
- Vomiting
- Idiopathic
Pneumomediastinum may also happen after:
- An infection in the neck or center of the chest (bacterial, fungal or viral infection)
- Severe injury (trauma) to your chest
- Rapid rises in altitude, or scuba diving
- Tearing of the esophagus (the tube that connects the mouth and stomach)
- Tearing of the trachea (windpipe)
- Rupture of the small sacs of your lungs (alveoli)
- Use of a breathing machine (positive pressure ventilation)
- Use of inhaled recreational drugs, such as marijuana or crack cocaine
- Surgery such as tooth extraction or digestive tract surgery
- Extensive voice exercise
- Excessive blowing
- Lung diseases such as asthma, bronchitis and pneumonia
- Valsalva maneuver (a procedure that involves forcefully exhaling against a closed airway that is used to quickly return an abnormal heart rhythm called paroxysmal supraventricular tachycardia (PSVT) to normal) 22
Pneumomediastinum also can occur with collapsed lung (pneumothorax) or other diseases.
Although it is rare, pneumomediastinum can occur spontaneously. This is considered benign and generally affects young adult males 23.
Risk factors for pneumomediastinum
You might be at higher risk for pneumomediastinum if you:
- Smoke.
- Have asthma, COPD or other lung conditions.
- Use inhaled recreational drugs.
- Recently had surgery on your abdomen, neck or chest.
- Recently gave birth.
Pneumomediastinum symptoms
Some people with pneumomediastinum don’t have any symptoms. Symptoms of pneumomediastinum include 24, 25, 26:
- Severe pain in the middle of your chest or breastbone. It may radiate to your arms or neck. The pain may be worse with breathing or swallowing.
- Shortness of breath.
- Air pockets under your skin on your face, neck or chest (subcutaneous emphysema).
- Neck or face swelling.
- High-pitched voice or other voice distortion.
- Throat pain.
- Neck pain.
- Painful swallowing (odynophagia).
- Difficulty swallowing (dysphagia).
Pneumomediastinum possible complications
Some rare complications of pneumomediastinum are life-threatening and need to be treated right away. They include:
- Air may build up and enter the space around your lungs (pleural space), causing your lung to collapse (pneumothorax).
- In rare cases, air may enter the area between your heart and the thin sac that surrounds the heart (pericardium). This condition is called a pneumopericardium.
- In other rare cases, so much air builds up in the middle of your chest that it pushes on your heart and the great blood vessels, so they cannot work properly.
All of these complications require urgent attention because they can be life threatening.
Pneumomediastinum diagnosis
During a physical examination, your doctor may feel small bubbles of air under the skin of your chest, arms, or neck called subcutaneous emphysema. Hearing a crunching sound in time with your heartbeat (Hamman’s sign) is a sign that you might have air in your mediastinum.
A chest X-ray or CT scan of your chest may be done. These are tests that take pictures of the inside of your chest. This is to confirm that air is in the mediastinum, and to help diagnose a hole in the trachea or esophagus.
A barium swallow may be indicated if Boerhaave syndrome (esophageal rupture following vomiting) is suspected from the history. If the pneumomediastinum has not resolved after 1 week, a CT of the chest is indicated to look for a source of persistent air leak.
Pneumomediastinum treatment
There’s no specific treatment for pneumomediastinum. Often, no treatment is needed because your body will gradually absorb the air on its own over a period of one to two weeks without intervention and rarely recur 21. Breathing high concentrations of oxygen may speed this process. If you have an underlying health condition, like an infection or injury to an internal organ, your doctor will treat you for that condition.
Your doctor may admit you to the hospital for 24 hours or longer for observation or treatment. While there, your doctor might treat you with:
- Oxygen therapy. Breathing in additional oxygen can help the air absorb into your body faster.
- Medication. Medication like pain relievers or cough suppressants can ease your symptoms until your body absorbs the extra air.
- Needle aspiration. If you have a lot of air that’s pressing on structures inside of your body, a doctor may remove some of the air with a needle or put a drain in. This is rare.
- Your doctor may put in a chest tube if you also have a collapsed lung (pneumothorax). You may also need treatment for the cause of the pneumomediastinum. A hole in the trachea or esophagus needs to be repaired with surgery.
Pneumomediastinum prognosis
Your outlook (prognosis) depends on the disease or events that caused the pneumomediastinum. People with spontaneous pneumomediastinum can make a full recovery and rarely have it happen again. If you have secondary pneumomediastinum, recovery will depend on the severity of your underlying condition. Some conditions that cause pneumomediastinum can be fatal.
The mortality rate associated with pneumomediastinum may be as high as 50-70% as seen in Boerhaave syndrome (esophageal rupture following vomiting) 27. The development of air leak, according to Weg et al 28, is not associated with an increased mortality rate in patients with sepsis-induced acute respiratory distress syndrome (ARDS). Other predisposing conditions associated with high mortality rates include trauma (blunt and penetrating, especially high velocity injury), asthma, and tracheobronchial perforation.
The most common morbidities attributable to pneumomediastinum are symptoms such as chest pain, voice change, and cough. Rarely, tension pneumomediastinum may result in decreased cardiac output. Laryngeal compression leading to stridor has been reported. Gas embolism has rarely been reported.
- Iteen AJ, Bianchi W, Sharman T. Pneumomediastinum. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557440[↩]
- Choo MJ, Shin SO, Kim JS. A case of spontaneous cervical and mediastinal emphysema. J Korean Med Sci. 1998 Apr;13(2):223-6. https://pmc.ncbi.nlm.nih.gov/articles/instance/3054475/pdf/9610628.pdf[↩]
- Nożewski JB, Dura ML, Kłopocka M, Kwiatkowska MM, Konieczny JP, Nicpoń-Nożewska KK. A 39-Year-Old Woman with Cervicofacial and Mediastinal Emphysema 10 Hours After an Elective Lower Molar Dental Extraction. Am J Case Rep. 2021 Nov 5;22:e931793. doi: 10.12659/AJCR.931793[↩]
- Spille J, Wagner J, Spille DC, Naujokat H, Gülses A, Wiltfang J, Kübel P. Pronounced mediastinal emphysema after restorative treatment of the lower left molar-a case report and a systematic review of the literature. Oral Maxillofac Surg. 2023 Sep;27(3):533-541. doi: 10.1007/s10006-022-01088-5[↩]
- Abolnik I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest. 1991 Jul;100(1):93-5. doi: 10.1378/chest.100.1.93[↩]
- Tsay CY, Chen YL, Chen CS, Lin PC, Wu MY. Pediatric Spontaneous Pneumomediastinum after a Push-Up Exercise: An Uncommon Complication of a Common Exercise. Children (Basel). 2020 Dec 11;7(12):287. doi: 10.3390/children7120287[↩][↩]
- Chiang KH, Chou AS. Images in clinical medicine. Pneumomediastinum. N Engl J Med. 2006 Mar 16;354(11):1177. doi: 10.1056/NEJMicm050132[↩]
- Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest. 2005 Nov;128(5):3298-302. doi: 10.1378/chest.128.5.3298[↩]
- McMahon DJ. Spontaneous pneumomediastinum. Am J Surg. 1976;131:550–551. doi: 10.1016/0002-9610(76)90008-8[↩]
- Bodey GP. Medical Mediastinal Emphysema. Ann Intern Med. 1961;54:46–56.[↩]
- Badaoui R, El Kettani C, Fikri M, Ouendo M, Canova-Bartoli P, Ossart M. Spontaneous cervical and mediastinal air emphysema after ecstasy abuse. Anesth Analg. 2002 Oct;95(4):1123. doi: 10.1097/00000539-200210000-00071[↩]
- Pittman JA, Pounsford JC. Spontaneous pneumomediastinum and Ecstasy abuse. J Accid Emerg Med. 1997 Sep;14(5):335-6. https://pmc.ncbi.nlm.nih.gov/articles/instance/1343105/pdf/jaccidem00020-0063.pdf[↩]
- Quin GI, McCarthy GM, Harries DK. Spontaneous pneumomediastinum and ecstasy abuse. J Accid Emerg Med. 1999 Sep;16(5):382. https://pmc.ncbi.nlm.nih.gov/articles/instance/1347073/pdf/jaccidem00032-0064a.pdf[↩]
- Naidoo M, Govind M. On your toes: Detecting mediastinal air on the chest radiograph in ecstasy abusers. S Afr Med J. 2016 Mar 30;106(5):46-7. doi: 10.7196/SAMJ.2016.v106i5.9867[↩]
- Ezoubi S, Kahal H, Waring WS. Pneumomediastinum as a complication of MDMA (3,4-methylenedioxymetamfetamine, Ecstasy) ingestion. Acute Med. 2016;15(3):152-156.[↩]
- Malas M, Fatani N, Aljuhani Z. A Young Healthy Male with Spontaneous Subcutaneous Emphysema Occurring in Neck, Retropharyngeal and Mediastinal Spaces. Case Rep Otolaryngol. 2020 Feb 7;2020:6963796. doi: 10.1155/2020/6963796[↩]
- Obiechina NE, Jayakumar A, Khan Y, Bass J. Bilateral pneumothorax, surgical emphysema and pneumomediastinum in a young male patient following MDMA intake. BMJ Case Rep. 2018 Apr 7;2018:bcr2017223103. doi: 10.1136/bcr-2017-223103[↩]
- Johnson JN, Jones R, Wills BK. Spontaneous pneumomediastinum. West J Emerg Med. 2008 Nov;9(4):217-8. https://pmc.ncbi.nlm.nih.gov/articles/PMC2672281[↩]
- Bartelmaos T, Blanc R, Claviere GD, Benhamou D. Delayed pneumomediastinum and pneumothorax complicating laparoscopic extraperitoneal inguinal hernia repair. J Clin Anesth. 2005;17:209–212. doi: 10.1016/j.jclinane.2004.05.009[↩]
- Henderson JA, Péloquin AJ. Boerhaave revisited: spontaneous esophageal perforation as a diagnostic masquerader. Am J Med. 1989 May;86(5):559-67. doi: 10.1016/0002-9343(89)90385-9[↩]
- Lee CC, Chen TJ, Wu YH, Tsai KC, Yuan A. Spontaneous retropharyngeal emphysema and pneumomediastinum presented with signs of acute upper airway obstruction. Am J Emerg Med. 2005 May;23(3):402-4. doi: 10.1016/j.ajem.2005.02.011[↩][↩]
- Rodrigues AC, Picard MH, Carbone A, Arruda AL, Flores T, Klohn J, Furtado M, Lira-Filho EB, Cerri GG, Andrade JL. Importance of adequately performed Valsalva maneuver to detect patent foramen ovale during transesophageal echocardiography. J Am Soc Echocardiogr. 2013 Nov;26(11):1337-43. doi: 10.1016/j.echo.2013.07.016[↩]
- Jougon JB, Ballester M, Delcambre F, Mac Bride T, Dromer CE, Velly JF. Assessment of spontaneous pneumomediastinum: experience with 12 patients. Ann Thorac Surg. 2003 Jun;75(6):1711-4. doi: 10.1016/s0003-4975(03)00027-4[↩]
- Dionísio P., Martins L., Moreira S., Manique A., Macedo R., Caeiro F., Boal L., Bárbara C. Spontaneous pneumomediastinum: Experience in 18 patients during the last 12 years. J. Bras. Pneumol. Publicacao Soc. Bras. Pneumol. E Tisilogia. 2017;43:101–105. doi: 10.1590/s1806-37562016000000052[↩]
- Dajer-Fadel W.L., Argüero-Sánchez R., Ibarra-Pérez C., Navarro-Reynoso F.P. Systematic review of spontaneous pneumomediastinum: A survey of 22 years’ data. Asian Cardiovasc. Thorac. Ann. 2014;22:997–1002. doi: 10.1177/0218492313504091[↩]
- Takada K., Matsumoto S., Hiramatsu T., Kojima E., Watanabe H., Sizu M., Okachi S., Ninomiya K. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir. Med. 2008;102:1329–1334. doi: 10.1016/j.rmed.2008.03.023[↩]
- Pneumomediastinum Prognosis. https://emedicine.medscape.com/article/1003409-overview#a2[↩]
- Weg JG, Anzueto A, Balk RA, Wiedemann HP, Pattishall EN, Schork MA, Wagner LA. The relation of pneumothorax and other air leaks to mortality in the acute respiratory distress syndrome. N Engl J Med. 1998 Feb 5;338(6):341-6. doi: 10.1056/NEJM199802053380601[↩]