Contents
- What is tachycardia
- The heart’s electrical system
- Supraventricular tachycardia
- Junctional tachycardia
- Ventricular tachycardia
- Wide complex tachycardia
- Postural orthostatic tachycardia syndrome
- Postural orthostatic tachycardia syndrome diagnostic criteria
- Postural orthostatic tachycardia syndrome classifications
- Postural orthostatic tachycardia syndrome causes
- Postural orthostatic tachycardia syndrome signs and symptoms
- Postural orthostatic tachycardia syndrome treatment
- Postural orthostatic tachycardia syndrome prognosis
- Tachycardia causes
- Tachycardia prevention
- Tachycardia diagnosis
- Tachycardia treatment
What is tachycardia
A heart rate of more than 100 beats per minute in adults is called tachycardia. What’s too fast for you may depend on your age and physical condition. A healthy heart normally beats about 60 to 100 times a minute when at rest and is defined by signals that originate in the upper chambers of the heart (atria).
It’s normal for your heart rate to rise during exercise or as a physiological response to stress, trauma or illness (sinus tachycardia). But in tachycardia, the heart beats faster than normal in the upper or lower chambers of the heart or both while at rest.
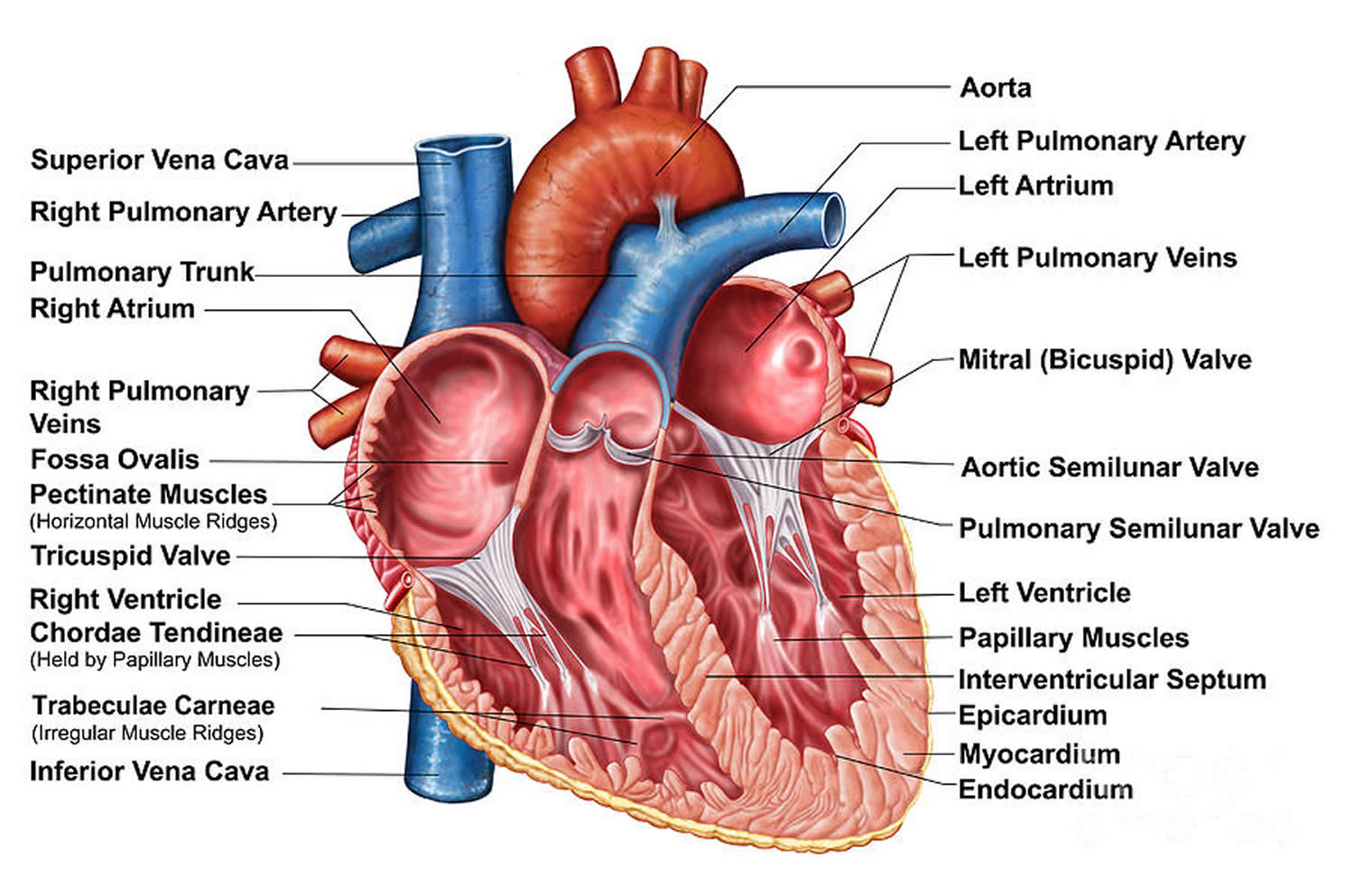
To understand the causes of tachycardia, it helps to understand how your heart’s internal electrical system works (see the Heart’s electrical system below). The heart’s electrical system controls the rate and rhythm of the heartbeat (see Figure 3).
Your heart is made up of four chambers — two upper chambers (atria) and two lower chambers (ventricles). The rhythm of your heart is normally controlled by a natural pacemaker called the sinus node, which is located in the right atrium. The sinus node produces electrical impulses that normally start each heartbeat.
From the sinus node, electrical impulses travel across the atria, causing the atria muscles to contract and pump blood into the ventricles.
The electrical impulses then arrive at a cluster of cells called the atrioventricular (AV) node — usually the only pathway for signals to travel from the atria to the ventricles.
The AV node slows down the electrical signal before sending it to the ventricles. This slight delay allows the ventricles to fill with blood. When electrical impulses reach the muscles of the ventricles, they contract, causing them to pump blood either to the lungs or to the rest of the body.
When anything disrupts this complex system, it can cause the heart to beat too fast (tachycardia), too slow (bradycardia) or with an irregular rhythm.
It is possible to have tachycardia and have no symptoms.
People with symptoms most often feel:
- dizzy and light-headed
- palpitations, when you feel your heart pounding or beating irregularly
- short of breath
- chest pain
In severe situations you can have a heart attack or become unconscious.
In some cases, tachycardia may cause no symptoms or complications. Complications of tachycardia vary in severity depending on factors such as the type of tachycardia, the rate and duration of rapid heart rate, and the existence of other heart conditions. Possible complications include:
- Blood clots that can cause a stroke or heart attack
- Inability of the heart to pump enough blood (heart failure)
- Frequent fainting spells or unconsciousness
- Sudden death, usually only associated with ventricular tachycardia or ventricular fibrillation
Treatments, such as drugs, medical procedures or surgery, may help control a rapid heartbeat or manage other conditions contributing to tachycardia.
Sinus tachycardia
Sinus tachycardia is where the natural pacemaker in your heart sends electrical signals faster than normal. This can be in response to a stressor like fever, fear, anxiety and strenuous exercise. This is usually not a concern.
But sometimes sinus tachycardia signifies a health problem. Arrhythmias are one of the main risk factors for stroke.
Causes of abnormal tachycardia include:
- anemia
- some medicines
- thyroid gland problems
- heart-attack
- other problems with the heart
Or it can be a sign of anemia, problems with the thyroid gland or general ill-health.
Inappropriate sinus tachycardia
Inappropriate sinus tachycardia is a clinical syndrome and not just a physiological manifestation, so the definition of inappropriate sinus tachycardia is based on both symptoms and heart rate criteria – “a daytime sinus heart rate >100 bpm at rest, with a mean 24-hour heart rate >90 bpm not due to primary causes, and associated with distressing symptoms of palpitations” 1.
Inappropriate sinus tachycardia, as a clinical syndrome, requires the element of distress. Not everyone with sinus tachycardia is distressed by their tachycardia and therefore do not have inappropriate sinus tachycardia. The specific heart rate criteria are based on the distributions of normal heart rates and are only modestly specific and sensitive. A good deal of clinical judgment is required in establishing the diagnosis.
The clinical manifestations of inappropriate sinus tachycardia syndrome are diverse and variable. Patients are mainly young women, and clinical symptoms range from intermittent palpitations to multisystem symptoms including light-headedness, pre-syncope, syncope, orthostatic intolerance, chest pain or pressure, headache, myalgia, dyspnea, fatigue, abdominal discomfort, anxiety, and depression 2.
The prevalence of the heart rate criteria for inappropriate sinus tachycardia was estimated in a middle-aged population of men and women to be 1.2 % 3. This includes both symptomatic and asymptomatic subjects. There is a general sense that inappropriate sinus tachycardia is chronic with no known mortality, but whether and how quickly patients improve is unknown. The pathophysiology is incompletely understood. It is likely that there are several different underlying pathologies that can result in this syndrome, including increased sinus node automaticity 4, increased sympathetic activity 5 and sensitivity, decreased parasympathetic activity 4 and impaired neurohumoral modulation.
Inappropriate sinus tachycardia diagnosis
A thorough history and physical exam should be performed focusing on possible causes of sinus tachycardia such as volume depletion, thyroid disease, drug use, psychological triggers, panic attacks and Postural Tachycardia Syndrome. A 12-lead ECG is useful in documenting tachycardia and in demonstrating sinus rhythm. A 24-hour Holter monitor can be useful in confirming the diagnosis, since one of the criteria is based on average 24-hour heart rate. Treadmill exercise testing might be useful to document an exaggerated tachycardia response to exertion 6. Cardiovascular autonomic testing is rarely useful.
Investigation of inappropriate sinus tachycardia syndrome according to the Heart Rhythm Society
- A complete history and physical exam and 12-lead ECG are recommended.
- It might be useful to obtain complete blood count and thyroid function studies.
- A 24-hour Holter monitoring might be performed.
- It might be useful to obtain urine/serum drug screen.
- It might be useful to consider autonomic testing.
- It might be useful to consider treadmill exercise testing.
Inappropriate sinus tachycardia treatment
There are no positive long-term prospective clinical trials of any therapeutic intervention and symptoms may continue despite heart rate control. inappropriate sinus tachycardia patients nearly always present distressed about the complexity of their problems. Lifestyle changes should be discussed early with all patients. β-adrenergic blockers may cause side-effects and should be used judiciously. Ivabradine holds considerable promise for the treatment of inappropriate sinus tachycardia. It blocks the “pacemaker” If current, is generally well tolerated and has a remarkable effect on heart rate. At doses of 5–7.5 mg twice daily it slows heart rate by 25–40 bpm 7. Ivabradine is not available in all countries but is likely to become increasingly so in the next 2–3 years.
Several groups have reported on the modification or ablation of the sinus node in inappropriate sinus tachycardia. Primary success rates are usually good, but the complication rates are significant. These include requirement for permanent pacing, transient or permanent phrenic nerve paralysis and transient superior vena cava syndrome. There is no evidence for long-term symptomatic improvement with radiofrequency ablation for inappropriate sinus tachycardia. Patients and physicians alike need to be aware that while patients may be highly motivated, the consequences of aggressive therapeutic attempts can seriously outweigh any potential benefit.
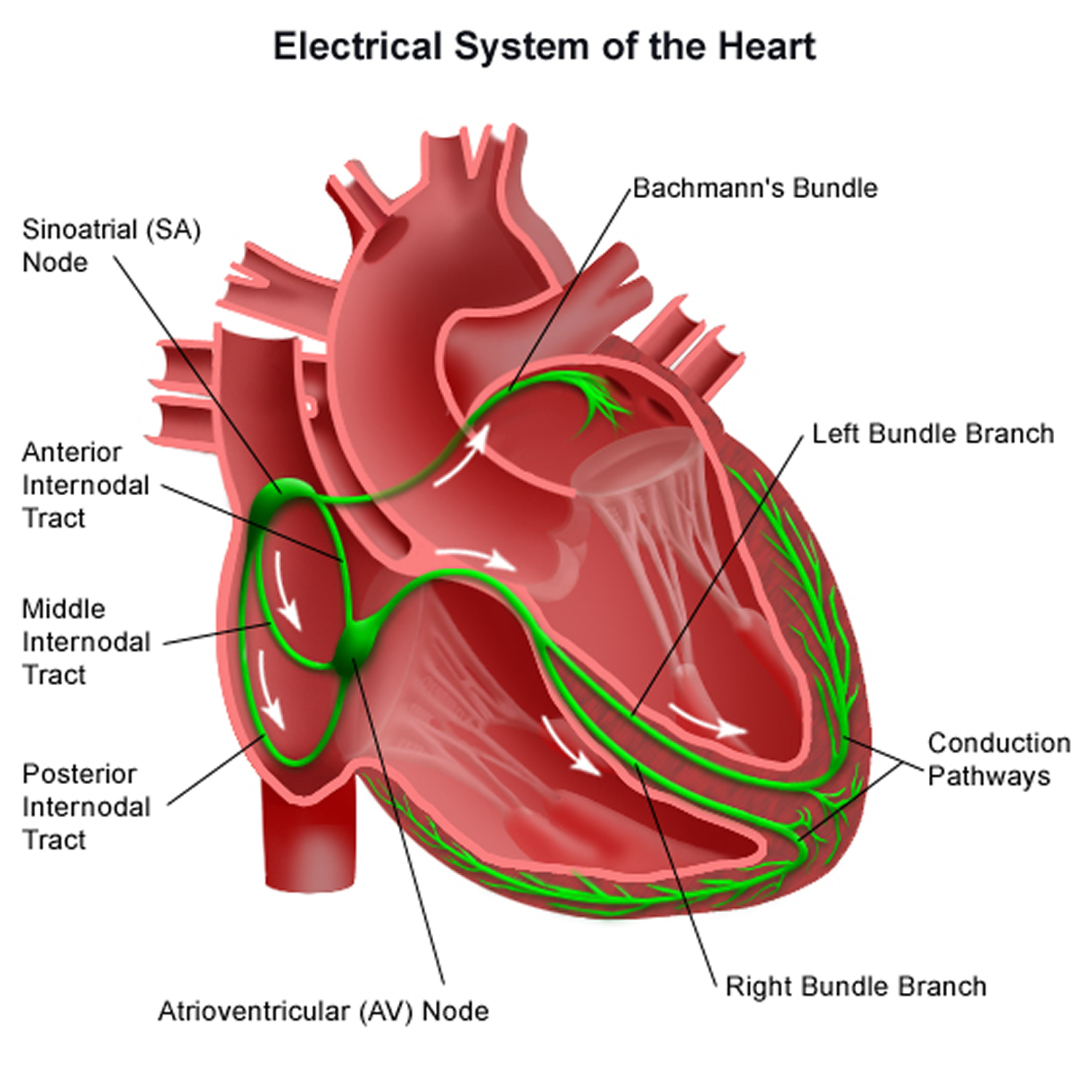
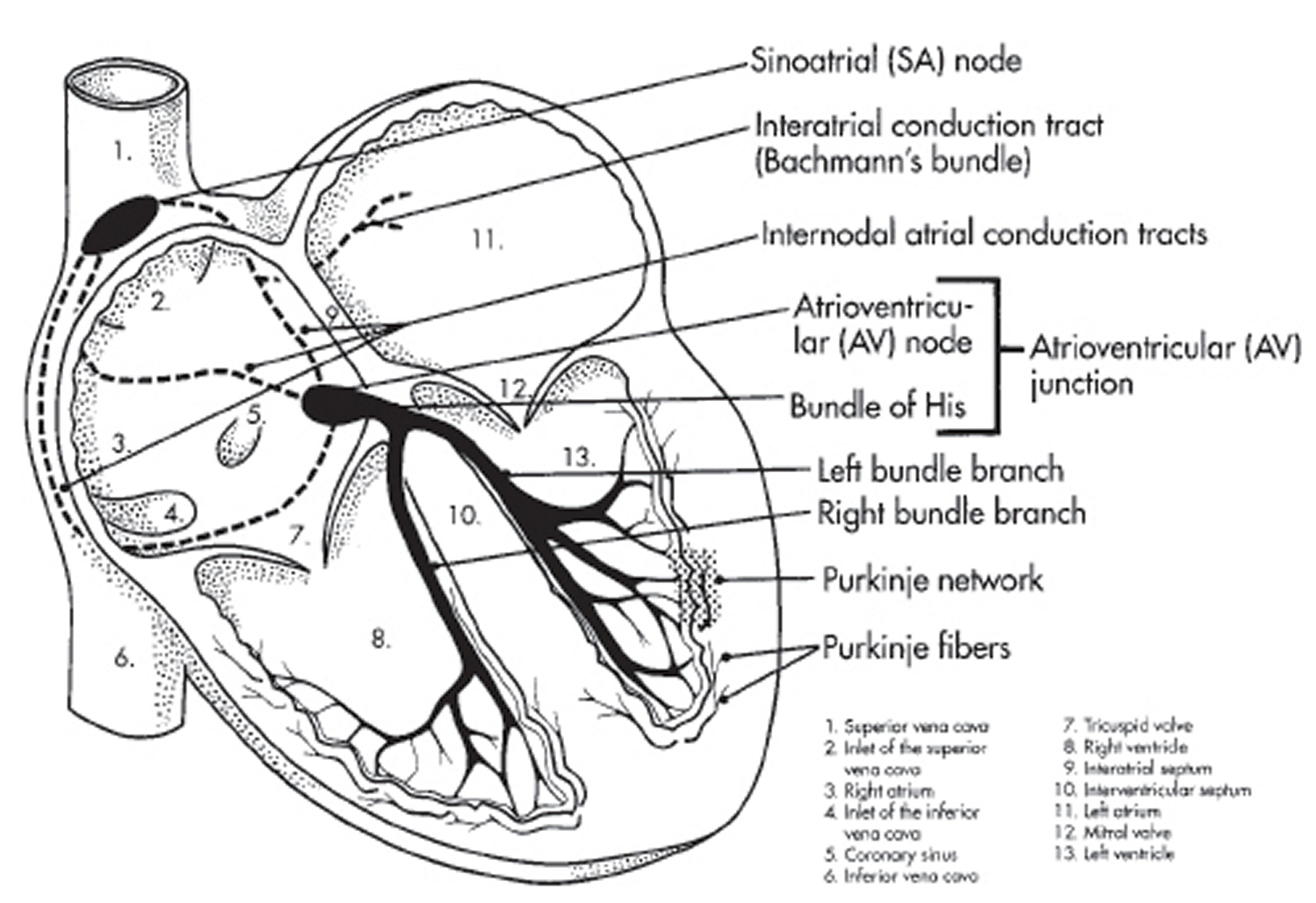
The heart’s electrical system
With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As the signal travels, it causes the heart to contract and pump blood.
Each electrical signal begins in a group of cells called the sinus node or sinoatrial (SA) node. The SA node is located in the right atrium (see Figure 2 and 3). In a healthy adult heart at rest, the SA node sends an electrical signal to begin a new heartbeat 60 to 100 times a minute. (This rate may be slower in very fit athletes.)
From the sinoatrial (SA) node, the electrical signal travels through the right and left atria. It causes the atria to contract and pump blood into the ventricles.
The electrical signal then moves down to a group of cells called the atrioventricular (AV) node, located between the atria and the ventricles. Here, the signal slows down slightly, allowing the ventricles time to finish filling with blood.
The electrical signal then leaves the AV node and travels to the ventricles. It causes the ventricles to contract and pump blood to the lungs and the rest of the body. The ventricles then relax, and the heartbeat process starts all over again in the SA node.
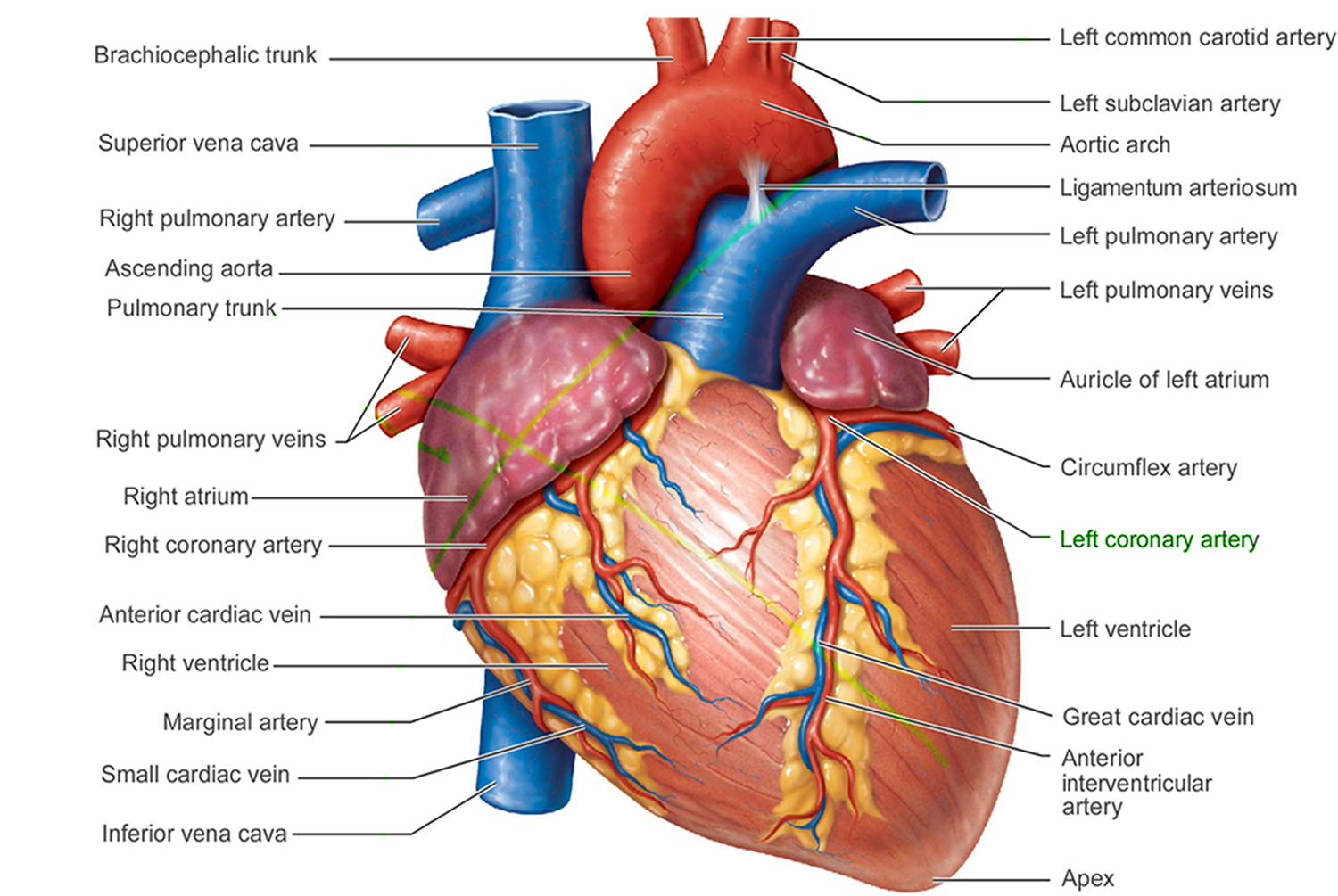
Figure 1. The anatomy of the heart
Supraventricular tachycardia
Supraventricular tachycardia (SVT), also called paroxysmal supraventricular tachycardia, is defined as an abnormally fast heartbeat. It’s a broad term that includes many forms of heart rhythm problems (heart arrhythmias) that originate above the ventricles (supraventricular) in the atria or AV node. “Paroxysmal” means from time to time. In most cases, supraventricular tachycardia is temporary and lasts for a few seconds, minutes, or in some cases hours.
Most people with rare episodes of supraventricular tachycardia live healthy lives without restrictions or interventions. For others, treatment and lifestyle changes can often control or eliminate rapid heartbeats.
Episodes of supraventricular tachycardia occur when a problem develops in the heart electrical system. Electrical signals in the heart’s upper chambers fire abnormally, which interferes with electrical signals coming from the sinoatrial (SA) node — the heart’s natural pacemaker. A series of early beats in the atria speeds up the heart rate. The rapid heartbeat does not allow enough time for the heart to fill before it contracts so blood flow to the rest of the body is compromised. These ineffective contractions of the heart may cause you to feel light-headed or dizzy because the brain isn’t receiving enough blood and oxygen.
Types of supraventricular tachycardia
There are several different types of supraventricular tachycardia, which are classified by the specific problem in the heart that disrupts the electrical system.
- Atrioventricular nodal reentry tachycardia is the most common type of supraventricular tachycardia. Episodes often start and end suddenly, and occur because of a reentrant circuit — also called an accessory pathway — located in or near the AV node that causes the heart to beat prematurely. Atrioventricular nodal reentry tachycardia tends to occur more often in young women, but it can affect both males and females of any age.
- Atrioventricular reciprocating tachycardia. Atrioventricular reciprocating tachycardia is the second most-common type of supraventricular tachycardia. It’s most commonly diagnosed in younger people.
- A type of supraventricular tachycardia called Wolff-Parkinson-White syndrome occurs as a result of an abnormal electrical connection between the atria and ventricles, which creates a short circuit in the heart’s electrical system. This happens because people with Wolff-Parkinson-White syndrome are born with an extra strand of muscle tissue between these chambers.
- Atrial tachycardia: Atrial tachycardia is the least common type of supraventricular tachycardia. It’s generally seen in children with underlying heart disorders such as congenital heart disease, particularly those who’ve had heart surgery. Atrial tachycardia may also be triggered by factors such as an infection or drug or alcohol use. For some people, atrial tachycardia increases during pregnancy or exercise. Atrial tachycardia episodes typically begin slowly, gradually increasing to more than 100 beats per minute before returning to a normal heart rate of around 60 to 80 beats per minute. In some cases, these episodes occur more abruptly or occur continuously.
Other types of supraventricular tachycardia include:
- Sinus tachycardia
- Inappropriate sinus tachycardia
- Multifocal atrial tachycardia
- Junctional ectopic tachycardia
- Nonparoxysmal junctional tachycardia
In other cases of supraventricular tachycardia, a short circuit occurs, even though the heart is otherwise normal.
Supraventricular tachycardia can also be caused by an electrical signal from another part of the heart overriding the signal from the sinoatrial node.
Who is likely to have supraventricular tachycardia?
- Supraventricular tachycardia is the most common type of arrhythmia in children
- More common in women, but may occur in either sex
- Anxious young people
- People who are physically fatigued
- People who drink large amounts of coffee (or caffeinated substances)
- People who drink alcohol heavily
- People who smoke heavily
- People who use medications, including asthma medications, herbal supplements and cold remedies
- Tiredness, stress or emotional upset
Supraventricular tachycardia symptoms
Signs and symptoms of supraventricular tachycardia may include:
- A fluttering in your chest
- Rapid heartbeat or “palpitations” or fluttering feeling in chest or bounding pulse
- Shortness of breath
- Angina (chest pain), pressure or tightness
- Lightheadedness or dizziness
- Sweating
- A pounding sensation in the neck
- Fainting (syncope) or near fainting
- Fatigue/tiredness
In infants and very young children, signs and symptoms may be difficult to identify. Sweating, poor feeding, pale skin and infants with a pulse rate greater than 200 beats per minute may have supraventricular tachycardia.
In extreme cases, supraventricular tachycardia may cause:
- Unconsciousness
- Cardiac arrest
Supraventricular tachycardia causes
For some people, a supraventricular tachycardia episode is related to an obvious trigger, such as psychological stress, lack of sleep or physical activity. For others, there may be no noticeable trigger. Things that may lead to, or cause, an episode include:
- Heart failure
- Thyroid disease
- Heart disease
- Chronic lung disease
- Smoking
- Drinking too much alcohol
- Consuming too much caffeine
- Drug use, such as cocaine and methamphetamines
- Certain medications, including asthma medications and over-the-counter cold and allergy drugs
- Surgery
- Pregnancy
- Certain health conditions, such as Wolff-Parkinson-White syndrome
Risk factors for supraventricular tachycardia
Supraventricular tachycardia is the most common type of arrhythmia in infants and children. It also tends to occur twice as often in women, particularly pregnant women, though it may occur in either sex.
Other factors that may increase your risk of supraventricular tachycardia include:
- Age. Some types of supraventricular tachycardia are more common in people who are middle-aged or older.
- Coronary artery disease, other heart problems and previous heart surgery. Narrowed heart arteries, a heart attack, abnormal heart valves, prior heart surgery, heart failure, cardiomyopathy and other heart damage increase your risk of developing supraventricular tachycardia.
- Congenital heart disease. Being born with a heart abnormality may affect your heart’s rhythm.
- Thyroid problems. Having an overactive or underactive thyroid gland can increase your risk of supraventricular tachycardia.
- Drugs and supplements. Certain over-the-counter cough and cold medicines and certain prescription drugs may contribute to an episode of supraventricular tachycardia.
- Anxiety or emotional stress
- Physical fatigue
- Diabetes. Your risk of developing coronary artery disease and high blood pressure greatly increases with uncontrolled diabetes.
- Obstructive sleep apnea. This disorder, in which your breathing is interrupted during sleep, can increase your risk of supraventricular tachycardia.
- Nicotine and illegal drug use. Nicotine and illegal drugs, such as amphetamines and cocaine, may profoundly affect the heart and trigger an episode of supraventricular tachycardia.
Supraventricular tachycardia prevention
To prevent an episode of supraventricular tachycardia, it’s important to know what triggers the episodes to occur and try to avoid them. You might want to try:
- Eating a heart-healthy diet
- Increasing your physical activity
- Avoiding smoking
- Keeping a healthy weight
- Limiting or avoiding alcohol
- Reducing stress
- Getting plenty of rest
- Using over-the-counter medications with caution, as some cold and cough medications contain stimulants that may trigger a rapid heartbeat
- Avoiding stimulant drugs such as cocaine and methamphetamines
For most people with supraventricular tachycardia, moderate amounts of caffeine do not trigger an episode. Large amounts of caffeine should be avoided, however.
Consider keeping a diary to help identify your triggers. Track your heart rate, symptoms and activity at the time of an supraventricular tachycardia episode.
Supraventricular tachycardia diagnosis
To diagnose supraventricular tachycardia, your doctor will review your symptoms and your medical history and conduct a physical examination. Your doctor may ask about — or test for — conditions that may trigger your supraventricular tachycardia, such as heart disease or a problem with your thyroid gland. Your doctor may also perform heart-monitoring tests specific to arrhythmia. These may include:
- Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat.
- Holter monitor. This portable ECG device can be worn for a day or more to record your heart’s activity as you go about your routine.
- Event monitor. For sporadic episodes of supraventricular tachycardia, you keep this portable ECG device available, attaching it to your body and pressing a button when you have symptoms. This lets your doctor check your heart rhythm at the time of your symptoms.
- Echocardiogram. In this noninvasive test, a hand-held device (transducer) placed on your chest uses sound waves to produce images of your heart’s size, structure and motion.
- Implantable loop recorder. This device detects abnormal heart rhythms and is implanted under the skin in the chest area.
If your doctor doesn’t find an arrhythmia during those tests, he or she may try to trigger your arrhythmia with other tests, which may include:
Stress test. For some people, supraventricular tachycardia is triggered or worsened by stress or exercise. During a stress test, you’ll be asked to exercise on a treadmill or stationary bicycle while your heart activity is monitored. If doctors are evaluating you to determine if coronary artery disease may be causing the arrhythmia, and you have difficulty exercising, then your doctor may use a drug to stimulate your heart in a way that’s similar to exercise.
Tilt table test. Your doctor may recommend this test if you’ve had fainting spells. Your heart rate and blood pressure are monitored as you lie flat on a table. The table is then tilted as if you were standing up. Your doctor observes how your heart and the nervous system that controls it respond to the change in angle.
Electrophysiological testing and mapping. In this test, doctors thread thin tubes (catheters) tipped with electrodes through your blood vessels to a variety of spots within your heart. Once in place, the electrodes can map the spread of electrical impulses through your heart.
In addition, your cardiologist can use the electrodes to stimulate your heart to beat at rates that may trigger — or halt — an arrhythmia. This allows your doctor to see the location of the arrhythmia and what may be causing it.
Supraventricular tachycardia treatment
Most people with supraventricular tachycardia do not require medical treatment. However, if you experience prolonged or frequent episodes, your doctor may recommend or try:
- Carotid sinus massage. Your doctor may try this type of massage that involves applying gentle pressure on the neck — where the carotid artery splits into two branches — to release certain chemicals that slow the heart rate. Don’t attempt to do this on your own as it may cause blood clots that could lead to a stroke, or heart or lung injury.
- Vagal maneuvers. You may be able to stop an episode of supraventricular tachycardia by using particular maneuvers that include holding your breath and straining, dunking your face in ice water, or coughing. These maneuvers affect the nervous system that controls your heartbeat (vagus nerves), often causing your heart rate to slow.
- Cardioversion. If you’re unable to stop an episode of supraventricular tachycardia on your own using vagal maneuvers, your doctor may use cardioversion, which can be conducted as a procedure or by using medications. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical impulses in your heart and can restore a normal rhythm.
- Medications. If you experience frequent episodes of supraventricular tachycardia, your doctor may prescribe medication to control your heart rate or restore a normal heart rhythm. It’s very important to take any anti-arrhythmic medication exactly as directed by your doctor in order to minimize complications.
- Catheter ablation. In this procedure, your doctor threads one or more catheters through your blood vessels to your heart. Electrodes at the catheter tips can use heat, extreme cold or radiofrequency energy to damage (ablate) a small spot of heart tissue and create an electrical block along the pathway that’s causing your arrhythmia.
In rare instances, treatment for supraventricular tachycardia may involve use of a small, implantable device called a pacemaker to emit electrical impulses that stimulate your heart to beat at a normal rate. The pacemaker is placed under the skin near the collarbone in a minor surgical procedure. An insulated wire extends from the device to the heart, where it’s permanently anchored.
Home remedies
Your doctor may suggest that, in addition to other treatments, you make lifestyle changes that will keep your heart as healthy as possible.
These lifestyle changes may include:
- Eat heart-healthy foods. Eat a healthy diet that’s low in salt and solid fats and rich in fruits, vegetables and whole grains.
- Exercise regularly. Exercise daily and increase your physical activity.
- Quit smoking. If you smoke and can’t quit on your own, talk to your doctor about strategies or programs to help you break a smoking habit.
- Maintain a healthy weight. Being overweight increases your risk of developing heart disease.
- Keep blood pressure and cholesterol levels under control. Make lifestyle changes and take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol.
- Drink alcohol in moderation. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger.
- Maintain follow-up care. Take your medications as prescribed and have regular follow-up appointments with your doctor. Tell your doctor if your symptoms worsen.
Alternative medicine
Research is ongoing regarding the effectiveness of several forms of complementary and alternative medical therapies for supraventricular tachycardia.
Some types of complementary and alternative therapies may be helpful to reduce stress, such as:
- Yoga
- Meditation
- Relaxation techniques
Some studies have shown that acupuncture may help reduce irregular heart rates in certain arrhythmias, but further research is needed.
The role of omega-3 fatty acids, a nutrient found mostly in fish, in the prevention and treatment of arrhythmias isn’t yet clear. But it appears as though this substance may be helpful in preventing and treating some arrhythmias.
Junctional tachycardia
Junctional tachycardia is a form of supraventricular tachycardia where the heart arrhythmias arising from the atrioventricular (AV) junction due to either as automatic tachycardia or as an escape mechanism when the sinus node is unable to work well 8. Junctional tachycardia can be contrasted to atrial tachycardia. It is a tachycardia associated with the generation of impulses in a focus in the region of the atrioventricular (AV) node due to an atrioventricular disassociation. In general, the atrioventricular (AV) junction’s intrinsic rate is 40-60 bpm so junctional tachycardia implies a rate >60 bpm. The precise anatomic site and nature of the pathways involved have not yet been established, and several attempts to provide a reasonable hypothesis based on anatomic or anisotropic models have been made 9. There has been considerable evidence that the right and left inferior extensions of the human atrioventricular (AV) node and the atrionodal inputs they facilitate may provide the anatomic substrate of the slow pathway, and a comprehensive model of the tachycardia circuit for all forms of junctional tachycardia based on the concept of atrionodal inputs has been proposed 9. Still, however, the circuit of junctional tachycardia remains elusive.
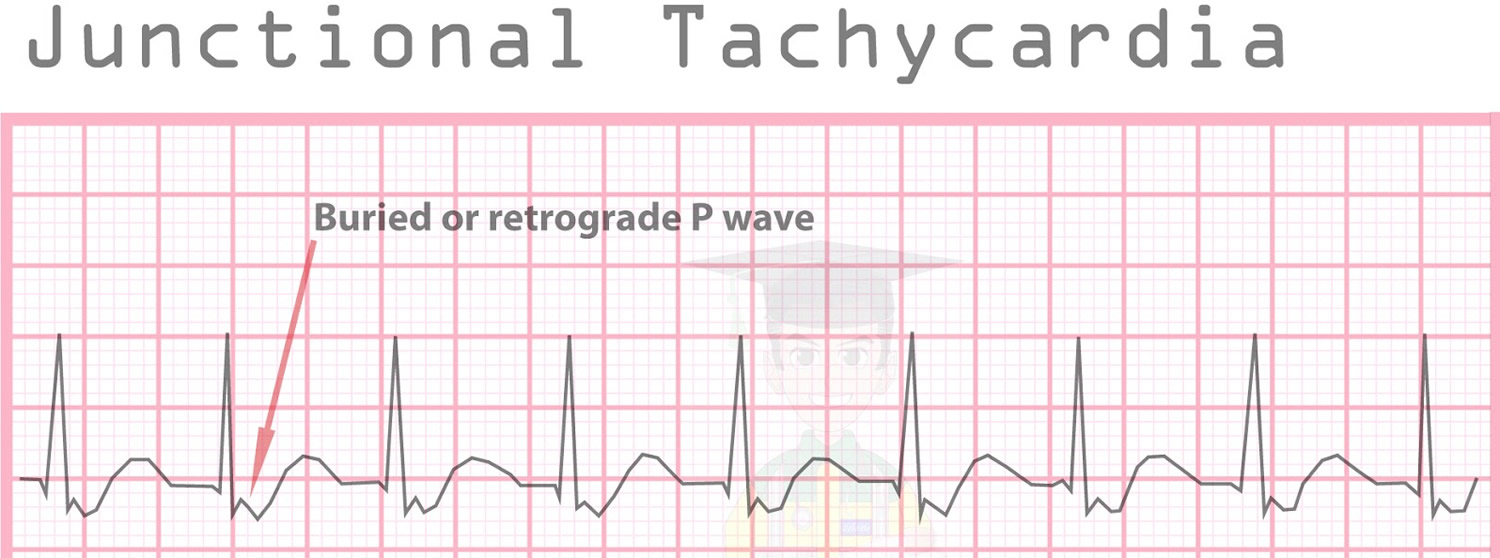
On an ECG, Junctional Tachycardia exhibits the following classic criteria:
- P Waves: The P Wave may be inverted in leads II, III and aVF or not visible
- Narrow QRS complexes (which is consistent with non-ventricular rhythms)
It can coexist with other superventricular tachycardias due to the disassociation between the SA node and the AV node. Junctional Tachycardia can appear similar to atrioventricular nodal reentrant tachycardia. One form is junctional ectopic tachycardia.
Figure 4. Junctional tachycardia
Ventricular tachycardia
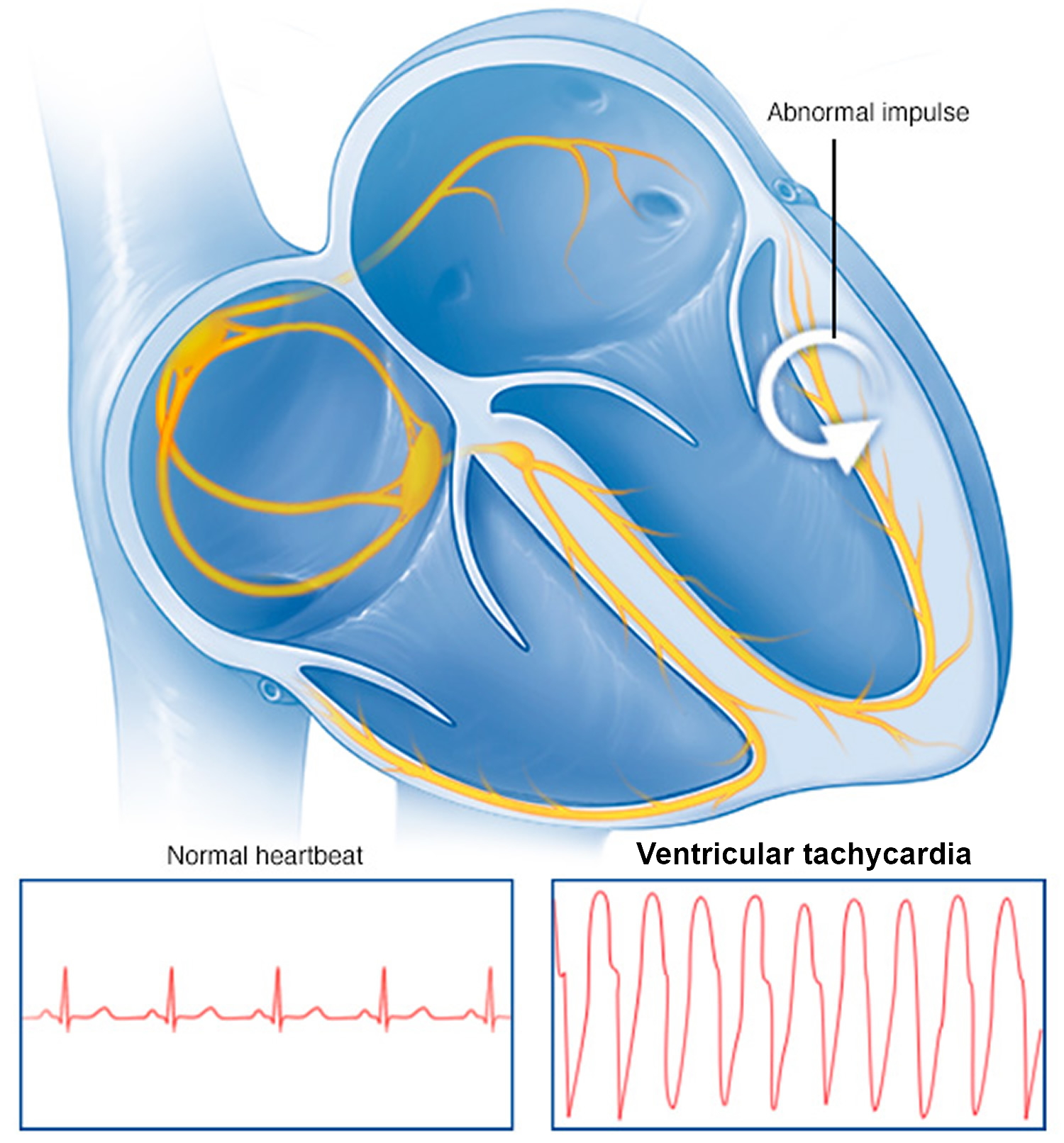
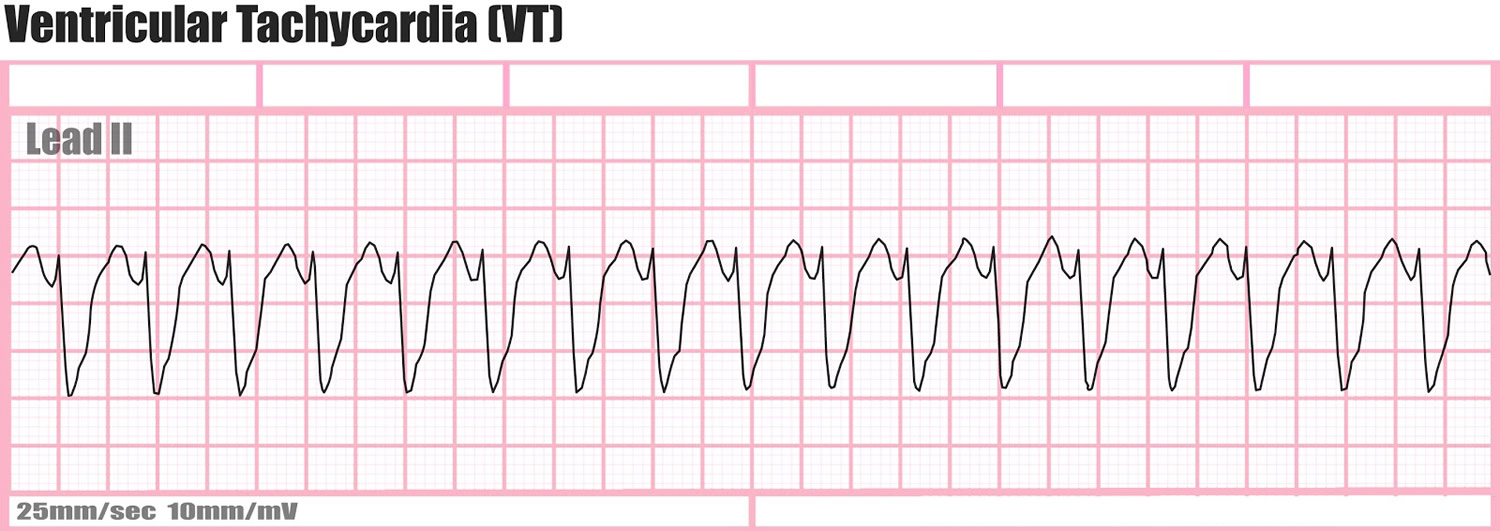
Ventricular tachycardia is is a potentially life-threatening fast heartbeat disorder (arrhythmia) caused by abnormal electrical signals in the lower chambers of the heart (ventricles). Ventricular tachycardia can be classified into monomorphic and polymorphic rhythms.
In ventricular tachycardia, abnormal electrical signals in the ventricles cause the heart to beat faster than normal, usually 100 or more beats a minute, out of sync with the upper chambers.
When that happens, your heart may not be able to pump enough blood to your body and lungs because the chambers are beating so fast or out of sync with each other that they don’t have time to fill properly.
Ventricular tachycardia may be brief, lasting for only a few seconds, and perhaps not cause any symptoms. Or it can last for much longer and cause symptoms such as dizziness, lightheadedness, palpitations or even loss of consciousness.
In some cases, ventricular tachycardia can cause your heart to stop (sudden cardiac arrest), which is a life-threatening medical emergency. This condition usually occurs in people with other heart conditions, such as those who have had a previous heart attack or other structural heart disease (cardiomyopathy).
Figure 5. Ventricular tachycardia
Ventricular tachycardia causes
Ventricular tachycardia is a pulse rate of more than 100 beats per minute, with at least 3 irregular heartbeats in a row.
The condition can develop as an early or late complication of a heart attack. It may also occur in people with:
- Cardiomyopathy
- Heart failure
- Heart surgery
- Myocarditis
- Valvular heart disease
- Abnormal electrical pathways in the heart present at birth (congenital heart conditions, including long QT syndrome)
- An inflammatory disease affecting skin or other tissues (sarcoidosis)
- Abuse of recreational drugs, such as cocaine
Ventricular tachycardia can occur without heart disease.
Scar tissue may form in the muscle of the ventricles days, months, or years after a heart attack. This can lead to ventricular tachycardia.
Ventricular tachycardia can also be caused by:
- Anti-arrhythmic drugs (used to treat an abnormal heart rhythm)
- Changes in blood chemistry (such as a low potassium level)
- Changes in pH (acid-base)
- Lack of oxygen to the heart due to tissue damage from heart disease
“Torsade de pointes” is a form of ventricular tachycardia. It is often due to congenital heart disease or the use of certain medicines.
In some cases, the exact cause of ventricular tachycardia can’t be determined (idiopathic ventricular tachycardia).
Risk factors for ventricular tachycardia
Any condition that puts a strain on the heart or damages heart tissue can increase your risk of ventricular tachycardia. Lifestyle changes or medical treatment may decrease the risk associated with the following factors:
- Heart disease (for example, prior heart attack, hypertrophic cardiomyopathy, inflammatory diseases of the heart or genetic conditions)
- Use of recreational drugs
- Severe electrolyte abnormalities
- Medication side effects
If you have a family history of ventricular tachycardia or other heart rhythm disorders, you may have an increased risk of ventricular tachycardia.
Ventricular tachycardia prevention
The most effective way to prevent ventricular tachycardia is to reduce your risk of developing heart disease. If you already have heart disease, monitor it and follow your treatment plan to lower your ventricular tachycardia risk.
In some cases, ventricular tachycardia may occur in the absence of heart disease (idiopathic ventricular tachycardia).
Prevent heart disease
Treat or eliminate risk factors that may lead to heart disease. Take the following steps:
- Exercise and eat a healthy diet. Live a heart-healthy lifestyle by exercising regularly and eating a healthy, low-fat diet that’s rich in fruits, vegetables and whole grains.
- Maintain a healthy weight. Being overweight increases your risk of developing heart disease.
- Keep blood pressure and cholesterol levels under control. Make lifestyle changes and take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol.
- Stop smoking. If you smoke and can’t quit on your own, talk to your doctor about strategies or programs to help you break a smoking habit.
- Drink in moderation. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. For some conditions it’s recommended that you completely avoid alcohol. Ask your doctor for advice specific to your condition. If you can’t control your alcohol consumption, talk to your doctor about a program to quit drinking and manage other behaviors related to alcohol abuse.
- Don’t use recreational drugs. Don’t use stimulants, such as cocaine. Talk to your doctor about an appropriate program for you if you need help ending recreational drug use.
- Use over-the-counter medications with caution. Some cold and cough medications contain stimulants that may trigger a rapid heartbeat. Ask your doctor which medications you need to avoid.
- Limit caffeine. If you drink caffeinated beverages, do so in moderation (no more than one to two beverages daily).
- Control stress. Avoid unnecessary stress and learn coping techniques to handle normal stress in a healthy way.
- Go to scheduled checkups. Have regular physical exams and report any signs or symptoms to your doctor.
Monitor and treat existing heart disease
If you already have heart disease, you can take steps to lower your risk of developing ventricular tachycardia or another arrhythmia:
- Follow the plan. Be sure you understand your treatment plan, and take all medications as prescribed.
- Report changes immediately. If your symptoms change or get worse or you develop new symptoms, tell your doctor immediately.
Ventricular tachycardia outlook (prognosis)
The outcome depends on the heart condition and symptoms.
Ventricular tachycardia possible complications
Complications of ventricular tachycardia vary in severity depending on such factors as the rate, and duration of a rapid heart rate, the frequency with which it happens, and the existence of other heart conditions. Possible complications include:
- Inability of the heart to pump enough blood (heart failure)
- Frequent fainting spells or unconsciousness
- Sudden death caused by cardiac arrest
Ventricular tachycardia symptoms
Brief episodes of ventricular tachycardia may not cause any symptoms in some people. Others may experience:
- Chest discomfort (angina)
- Fainting (syncope)
- Lightheadedness or dizziness
- Sensation of feeling the heart beat (palpitations)
- Shortness of breath
- Seizures
Symptoms may start and stop suddenly. In some cases, there are no symptoms.
Sustained or more serious episodes of ventricular tachycardia may cause:
- Loss of consciousness or fainting
- Cardiac arrest (sudden death)
Ventricular tachycardia diagnosis
To diagnose ventricular tachycardia, your doctor may review your symptoms and your family and medical history and conduct a physical examination.
Your doctor may order several tests to diagnose your condition, determine the cause and severity of your condition, and determine the most appropriate treatment.
In some cases, ventricular tachycardia may be a medical emergency and require an urgent diagnosis and prompt treatment.
Several heart tests also may be necessary to diagnose ventricular tachycardia.
The health care provider will look for:
- Absent pulse
- Loss of consciousness
- Normal or low blood pressure
- Rapid pulse
Tests that may be used to detect ventricular tachycardia include:
- Holter monitor
- ECG
- Intracardiac electrophysiology study (EPS)
- Rhythm monitoring with a loop recorder or device
You may also have blood chemistries and other tests.
Electrocardiogram (ECG)
An electrocardiogram, also called an ECG or EKG, is the most common tool used to diagnose ventricular tachycardia. It’s a painless test that detects and records your heart’s electrical activity using small sensors (electrodes) attached to your chest and arms.
An ECG records the timing and strength of electrical signals as they travel through your heart. Your doctor can look for patterns among these signals to determine what kind of tachycardia you have and how abnormalities in the heart may be contributing to a fast heart rate.
Your doctor may also ask you to use portable ECG devices at home to provide more information about your heart rate. These devices include:
- Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart’s activity for an entire 24-72 hour period, which provides your doctor with a prolonged look at your heart rhythms. Your doctor will likely ask you to keep a diary during the same 24 hours. You’ll describe any symptoms you experience and record the time they occur.
- Event monitor. This portable ECG device is intended to monitor your heart activity over a few weeks to a few months. You wear it all day, but it records only at certain times for a few minutes at a time. With many event monitors, you activate them by pushing a button when you experience symptoms of a fast heart rate. Other monitors automatically sense abnormal heart rhythms and then start recording. These monitors allow your doctor to look at your heart rhythm at the time of your symptoms.
- Transtelephonic monitor. This device provides continuous heart rhythm monitoring but must be worn continuously. It may or may not include wires.
- Implantable loop recorder. This is an implantable device that has no wires and can sit underneath your skin for up to three years to continuously monitor your heart rhythm.
Cardiac imaging
Imaging of the heart may be performed to determine if structural abnormalities are affecting blood flow and contributing to ventricular tachycardia.
Types of cardiac imaging used to evaluate ventricular tachycardia include:
- Echocardiogram (echo). An echocardiogram creates a moving picture of your heart using sound waves via a transducer placed on the chest that emits and detects these waves. An echo can identify abnormalities in the heart valves and heart muscle that contribute to poor blood flow.
- Magnetic resonance imaging (MRI). A cardiac MRI provides still or moving pictures of how the blood is flowing through the heart and detects irregularities. It is often used to evaluate potential causes of ventricular tachycardia.
- Computerized tomography (CT). CT scans combine several X-ray images to provide a more detailed cross-sectional view of the heart.
- Coronary angiogram. This may be used to study the flow of blood through your heart and blood vessels. Your doctor may use a coronary angiogram to reveal potential blockages or abnormalities. It uses a dye and special X-rays to show the inside of your coronary arteries.
- Chest X-ray. This painless test is used to take still pictures of your heart and lungs and can detect if your heart is enlarged.
Stress test
Your doctor may recommend a stress test to see how your heart functions while it is working hard during exercise or when medication is given to make the heart beat faster.
In an exercise stress test, electrodes are placed on your chest to monitor heart function while you exercise, usually by walking on a treadmill. Other heart tests may be performed in conjunction with a stress test.
Electrophysiological test
Your doctor may recommend an electrophysiological test to confirm the diagnosis or to pinpoint the location of problems in your heart’s circuitry.
During this test, a doctor inserts thin, flexible tubes (catheters) tipped with electrodes into an access point, usually your groin or neck, and guides them through your blood vessels to various spots in your heart.
Additional tests
Your doctor may order additional tests as needed to diagnose an underlying condition that is contributing to ventricular tachycardia and judge the condition of your heart.
Ventricular tachycardia treatment
The goals of ventricular tachycardia treatment are to restore your normal heart rhythm, regulate your heart rate and prevent future episodes.
Treatment of ventricular tachycardia depends largely on what is causing the arrhythmia and the type or severity of your ventricular tachycardia.
The two main types of ventricular tachycardia are those that resolve on their own within 30 seconds (nonsustained ventricular tachycardia) and those that last more than 30 seconds, interfere with normal blood flow or require medical intervention to resolve (sustained ventricular tachycardia).
If someone with ventricular tachycardia is in distress, they may require:
- CPR
- Cardioversion (electric shock)
- Medicines (such as lidocaine, procainamide, sotalol, or amiodarone) given through a vein
Urgent ventricular tachycardia treatment
Sustained ventricular tachycardia may sometimes lead to sudden death and often requires urgent medical intervention.
Immediate treatment usually involves restoring a normal heart rate by delivering a jolt of electricity to the heart via defibrillation or cardioversion but can also involve providing medications orally or intravenously.
Defibrillation may be performed using an automated external defibrillator by a bystander who recognizes the signs of cardiac arrest, or by medical professionals using paddles in a hospital setting. Cardioversion is performed in a hospital setting using a cardioversion machine that monitors your heart rhythm before and after shocks are delivered.
An injection of an anti-arrhythmic medication, such as lidocaine, may also be used to treat sustained ventricular tachycardia and restore a normal heart rhythm.
After an episode of ventricular tachycardia, steps are taken to prevent further episodes.
- Medicines taken by mouth may be needed for long-term treatment. However, these drugs may have severe side effects. They are being used less often as other treatments are developed.
- A procedure to destroy the heart tissue that is causing the abnormal heartbeat (called ablation) may be done.
- An implantable cardioverter defibrillator (ICD) may be used. It is a device that detects any life-threatening, rapid heartbeat. This abnormal heartbeat is called an arrhythmia. If it occurs, the implantable cardioverter defibrillator quickly sends an electrical shock to the heart to change the rhythm back to normal. This is called defibrillation.
Preventing episodes of a fast heart rate
People with nonsustained or sustained ventricular tachycardia may be treated in a variety of ways to prevent future episodes and related complications.
Treatments for ventricular tachycardia include:
- Catheter ablation. This procedure is often used when a discrete electrical pathway is responsible for an increased heart rate. In this procedure, a doctor inserts catheters into your groin or neck and guides them through the blood vessels to your heart. Electrodes at the catheter tips can use heat, extreme cold or radiofrequency energy to damage (ablate) the extra electrical pathway and prevent it from sending electrical signals.
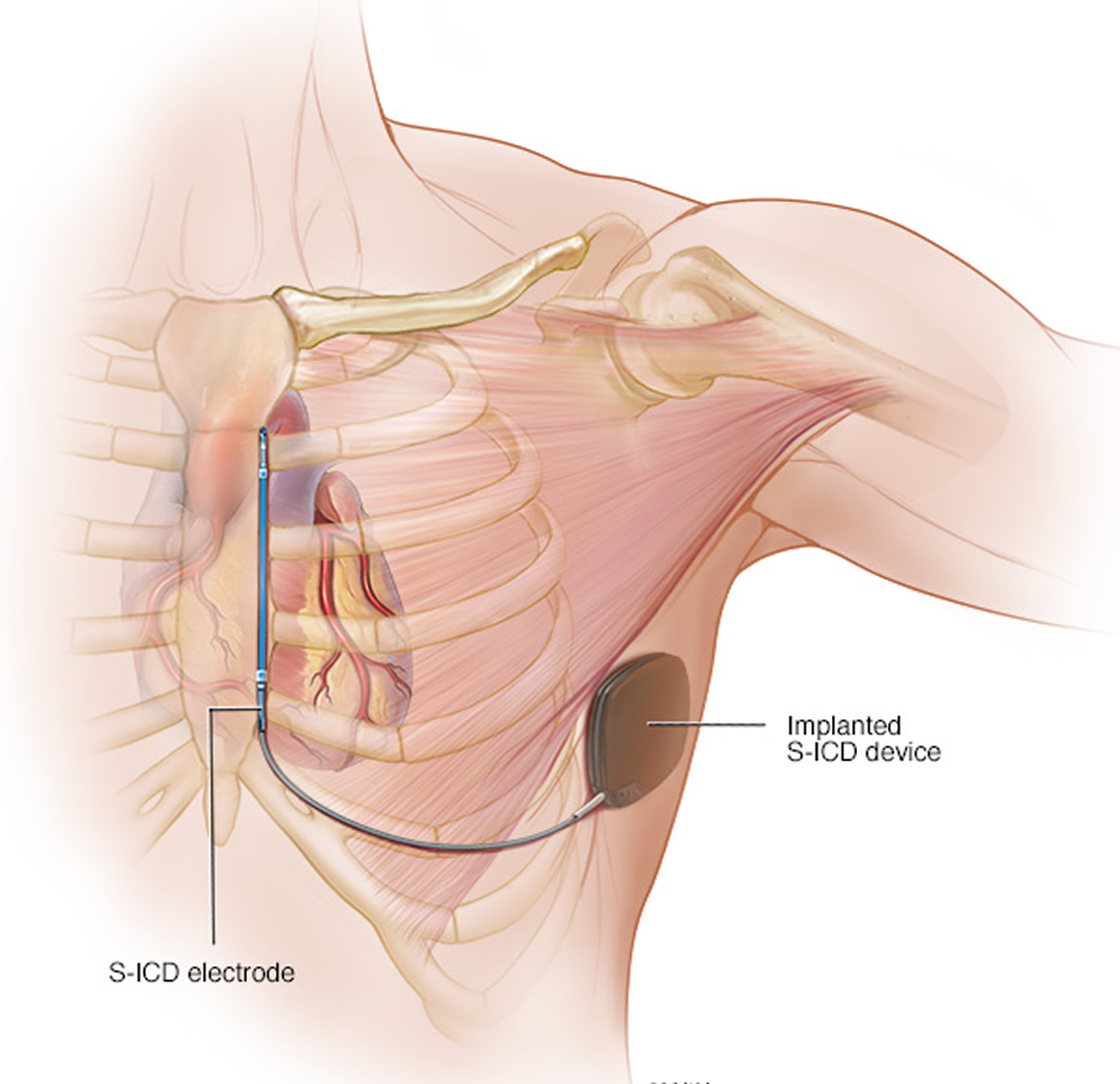
- Medications. Anti-arrhythmic medications may prevent a fast heart rate when taken regularly.
- Implantable cardioverter-defibrillator. If you’re at risk of having a life-threatening ventricular tachycardia episode, your doctor may recommend an implantable cardioverter-defibrillator (implantable cardioverter-defibrillator). The device, about the size of a pager, is surgically implanted in your chest. The implantable cardioverter-defibrillator continuously monitors your heartbeat, detects an increase in heart rate and delivers precisely calibrated electrical shocks, if needed, to restore a normal heart rhythm. A new type of implantable cardioverter-defibrillator called a subcutaneous implantable cardioverter-defibrillator (S-implantable cardioverter-defibrillator) is less invasive but larger in size than an implantable cardioverter-defibrillator. Your doctor implants the S-implantable cardioverter-defibrillator under the skin at the side of the chest below the armpit. It’s attached to an electrode that runs along your breastbone. You may be a candidate for an S-implantable cardioverter-defibrillator if you have structural defects in your heart that prevent advancing wires to the heart through your blood vessels, or if you have other reasons for wanting to avoid traditional implantable cardioverter-defibrillators.
- Surgery. Open-heart surgery may be needed in some cases to treat a process contributing to ventricular tachycardia (for example, if there are blockages in blood vessels). Surgery is usually used only when other treatment options don’t work or when surgery is needed to treat another heart disorder.
Treating an underlying disease
If another medical condition is contributing to ventricular tachycardia, such as some form of heart disease, treating the underlying problem may prevent or minimize ventricular tachycardia episodes.
Figure 7. Subcutaneous implantable cardioverter-defibrillator
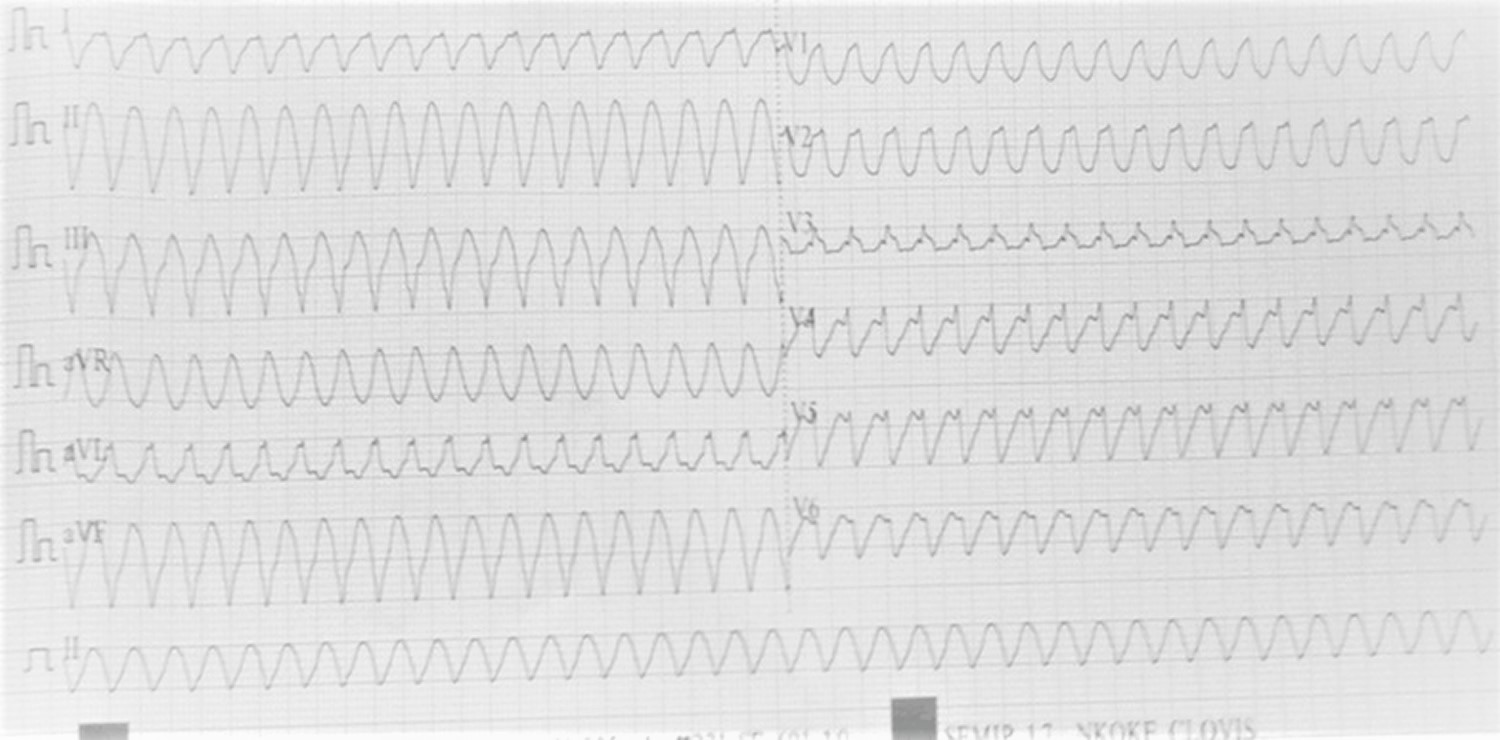
Monomorphic ventricular tachycardia
Monomorphic ventricular tachycardia means that the appearance of all the QRS complexes remain identical from beat to beat matching each other in each lead of a surface electrocardiogram (ECG) 10. Myocadial scar-related monomorphic ventricular tachycardia is the most common type and a frequent cause of death in patients having survived a heart attack or myocardial infarction, especially if they have weak heart muscle.
Figure 8. Monomorphic ventricular tachycardia
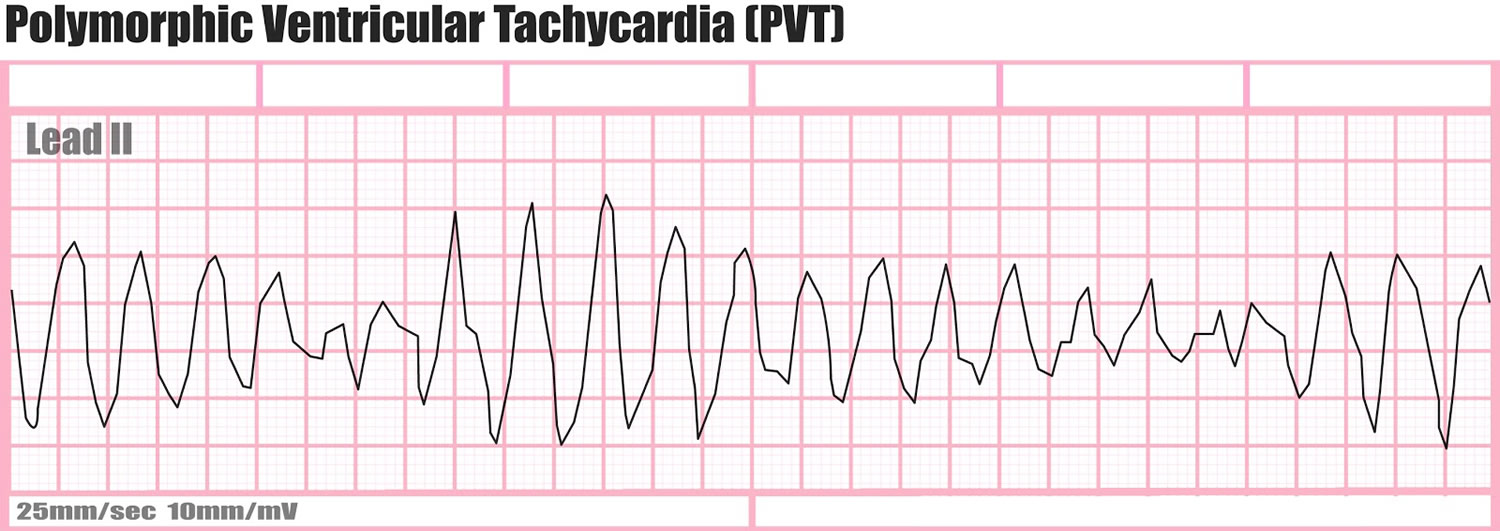
Polymorphic ventricular tachycardia
Polymorphic ventricular tachycardia, on the other hand, has beat-to-beat variations in morphology. This may appear as a cyclical progressive change in cardiac axis, previously referred to by its French name torsades de pointes (“twisting of the spikes”). However, at the current time, the term torsades de pointes is reserved for polymorphic VT occurring in the context of a prolonged resting QT interval.
Figure 9. Polymorphic ventricular tachycardia
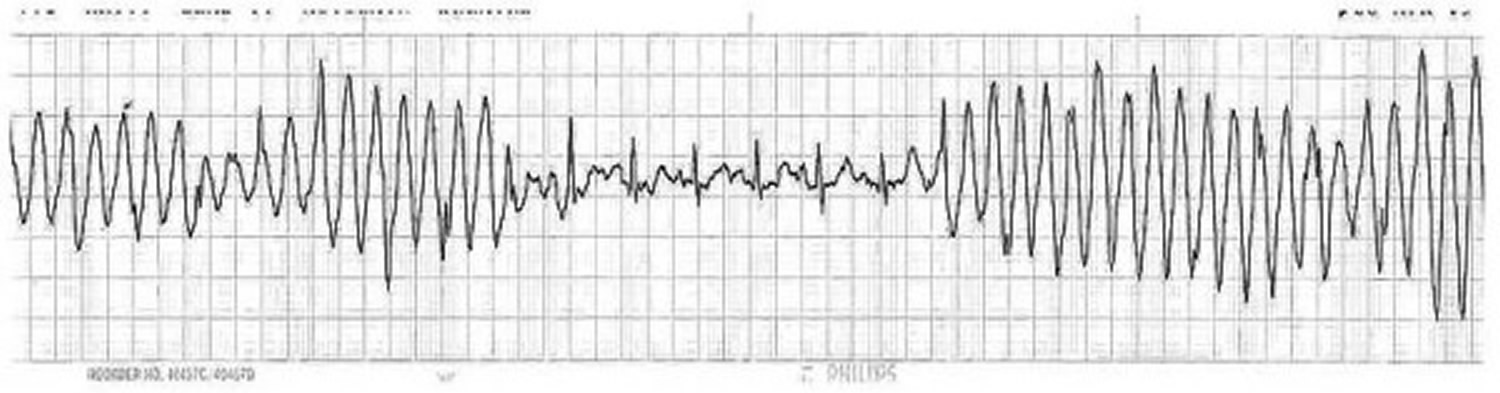
Wide complex tachycardia
A wide complex tachycardia is defined as a cardiac rhythm with a rate >100 beats per minute and a QRS width >120 milliseconds (ms) 11.
Ventricular tachycardia accounts for 80% of wide complex tachycardia 12. In such patients, a history of structural heart disease, particularly of coronary artery disease or prior myocardial infarction, strongly suggests a diagnosis of ventricular tachycardia.
Supraventricular tachycardia (SVT) with aberrancy accounts for a relatively small number of patients with wide complex tachycardia 11. Supraventricular tachycardia (SVT) typically originates in atrial tissue and/or AV junction and utilizes the normal atrioventricular (AV) conduction system for ventricular activation. Aberrance occurs when there is delay or block in the His-Purkinje system during antegrade conduction of impulses over the normal AV fascicles. Essentially, all types of supraventricular tachycardia with aberrant conduction can present as a wide complex tachycardia. Atrial tachycardias, atrioventricular nodal reentrant tachycardias, orthodromic reciprocating tachycardias are some of the common supraventricular tachycardias which can be associated with aberrance. Termination of wide complex tachycardia by adenosine, digoxin, calcium-channel blockers, beta-blockers or vagal maneuvers is suggests supraventricular tachycardia. Grubb, however, showed that ventricular tachycardia too could be terminated with carotid sinus stimulation 13.
In ventricular fibrillation multiple foci take over from the ventricles and produce a disorganized, chaotic rhythm. The patient is considered pulse-less, with no blood pressure, requiring immediate intervention. Ventricular fibrillation is secondary to coronary artery disease, myocardial ischemia, myocardial infarction, cardiomyopathy, cardiac trauma, drug toxicity, hypoxia, and electrolyte imbalance.
Preexcited tachycardias are conducted antegradely over an accessory pathway. Evidence for the presence of an accessory pathway can be manifest of the surface electrocardiogram (EKG) which can show intermittent or continuous presence of a delta wave associated with a short PR interval. The delta wave represents the part of the ventricular myocardium that is depolarized through the accessory pathway.
Table 1. Selected differential diagnosis of wide complex tachycardia
| Condition | Characteristics |
|---|---|
| Ventricular tachycardia (VT) | Presence of AV dissociation with more ventricular than atrial events, QRS duration more than 140 ms, fusion beats, capture beats |
| Supraventricular tachycardia with aberrancy A) with aberrancy in the His-Purkinje system | QRS duration of not more than 140 ms 14 |
| EKG artifacts | Hemodynamically stable, normal QRS complexes, “precipitating” cause viz. movements |
| Pre-excitation tachycardia | Presence of “delta wave”, short PR interval |
| Ventricular fibrillation | No apparent rate, fibrillatory waves, absent pulse, unrecordable BP |
Figure 10. Wide complex tachycardia ECG
Postural orthostatic tachycardia syndrome
Postural orthostatic tachycardia syndrome is one of a group of disorders that have orthostatic intolerance as their primary symptom. Orthostatic intolerance describes a condition in which an excessively reduced volume of blood returns to the heart after an individual stands up from a lying down position. The primary symptom of orthostatic intolerance is lightheadedness or fainting. In postural orthostatic tachycardia syndrome, the lightheadedness or fainting is also accompanied by a rapid increase in heartbeat of more than 30 beats per minute, or a heart rate that exceeds 120 beats per minute, within 10 minutes of rising. Patients usually also complain of palpitations, fatigue, exercise intolerance, nausea, diminished concentration, tremulousness, syncope (fainting), and near syncope (faintness) 16. The faintness or lightheadedness of postural orthostatic tachycardia syndrome are relieved by lying down again. Anyone at any age can develop postural orthostatic tachycardia syndrome, but the majority of individuals affected (between 75 and 80 percent) are women between the ages of 15 to 50 years of age. Some women report an increase in episodes of postural orthostatic tachycardia syndrome right before their menstrual periods. postural orthostatic tachycardia syndrome often begins after a pregnancy, major surgery, trauma, or a viral illness. Postural orthostatic tachycardia syndrome may make individuals unable to exercise because the activity brings on fainting spells or dizziness.
Symptoms may be of such severity that normal activities of life, such as bathing, housework, and even eating can be significantly limited. Postural orthostatic tachycardia syndrome patients have been reported to suffer from a degree of functional impairment similar to that seen in conditions such as chronic obstructive pulmonary disease (COPD) and congestive heart failure, yet these patients are all-too-frequently misdiagnosed as having severe anxiety or panic disorder 17.
Although it is difficult to determine the true prevalence of postural orthostatic tachycardia syndrome, current estimates suggest that at least 500 000 patients are affected by the disorder in the United States alone and millions more around the world 18. Of this total, 25% are disabled and unable to work 19. It should be noted that many patients with orthostatic intolerance due to postural orthostatic tachycardia syndrome will not demonstrate orthostatic hypotension (defined as fall of >20/10 mm Hg on standing). Instead, they may display no change, a small decline, or even a modest increase in blood pressure 20. Some investigators have noted that focusing on heart rate overlooks a number of other autonomic symptoms that may be present, such as disturbances in sweating, thermoregulation and bowel and bladder function. It should also be remembered that other orthostatic intolerance syndromes exist in addition to postural orthostatic tachycardia syndrome, in which symptoms occur in the absence of dramatic heart rate increases.
Doctors aren’t sure yet what causes the reduced return of blood to the heart that occurs in orthostatic intolerance, or why the heart begins to beat so rapidly in postural orthostatic tachycardia syndrome. Current thinking is that there are a number of mechanisms. Some individuals have peripheral denervation (neuropathic postural orthostatic tachycardia syndrome); some have symptoms that are due to sustained or parosyxmal overactivity of the sympathetic nervous system (hyperadrenergic postural orthostatic tachycardia syndrome); and many individuals with postural orthostatic tachycardia syndrome have significant deconditioning.
Postural orthostatic tachycardia syndrome may follow a relapsing-remitting course, in which symptoms come and go, for years. In most cases (approximately 80 percent), an individual with postural orthostatic tachycardia syndrome improves to some degree and becomes functional, although some residual symptoms are common.
Quality-of-Life and Disability
Some patients have fairly mild symptoms and can continue with normal work, school, social and recreational activities. For others, symptoms may be so severe that normal life activities, such as bathing, housework, eating, sitting upright, walking or standing can be significantly limited. Physicians with expertise in treating postural orthostatic tachycardia syndrome have compared the functional impairment seen in postural orthostatic tachycardia syndrome patients to the impairment seen in chronic obstructive pulmonary disease (COPD) or congestive heart failure. Approximately 25% of postural orthostatic tachycardia syndrome patients are disabled and unable to work. Researchers found that quality-of-life in postural orthostatic tachycardia syndrome patients is comparable to patients on dialysis for kidney failure 21.
Postural orthostatic tachycardia syndrome diagnostic criteria
The current diagnostic criteria for postural orthostatic tachycardia syndrome is a heart rate increase of 30 beats per minute or more, or over 120 beats per minute, within the first 10 minutes of standing, in the absence of orthostatic hypotension and not associated with other chronic debilitating conditions such as prolonged bed rest or the use of medications known to diminish vascular or autonomic tone 18, 17. In children and adolescents, a revised standard of a 40 beats per minute or more increase has recently been adopted 22. Postural orthostatic tachycardia syndrome is often diagnosed by a Tilt Table Test, but if such testing is not available, postural orthostatic tachycardia syndrome can be diagnosed with bedside measurements of heart rate and blood pressure taken in the supine (laying down) and standing up position at 2, 5 and 10 minute intervals. Doctors may perform more detailed tests to evaluate the autonomic nervous system in postural orthostatic tachycardia syndrome patients, such as Quantitative Sudomotor Axon Reflex Test (QSART, sometimes called Q-Sweat), Thermoregulatory Sweat Test (TST), skin biopsies looking at the small fiber nerves, gastric motility studies and more.
Is postural orthostatic tachycardia syndrome caused by anxiety?
While some of the physical symptoms of postural orthostatic tachycardia syndrome overlap with the symptoms of anxiety, such as tachycardia and palpitations, postural orthostatic tachycardia syndrome is not caused by anxiety. Postural orthostatic tachycardia syndrome patients are often misdiagnosed as having anxiety or panic disorder, but their symptoms are real and can severely limit a person’s ability to function. Research has shown that postural orthostatic tachycardia syndrome patients are similarly or even less likely to suffer from anxiety or panic disorder than the general public. Research surveys that evaluate mental health show similar results between postural orthostatic tachycardia syndrome patients and national norms.
Postural orthostatic tachycardia syndrome classifications
Postural orthostatic tachycardia syndrome researchers have classified postural orthostatic tachycardia syndrome in various ways. Dr. Blair Grubb has described postural orthostatic tachycardia syndrome as “primary” or “secondary” 18. “Primary” refers to postural orthostatic tachycardia syndrome with no other identifiable medical condition (also known as “idiopathic” postural orthostatic tachycardia syndrome). Postural orthostatic tachycardia syndrome is a heterogeneous (meaning it has many causes) group of disorders with similar clinical manifestations. Postural orthostatic tachycardia syndrome itself is not a disease; it is simply a cluster of symptoms that are frequently seen together. This is why the it’s called a “postural orthostatic tachycardia syndrome.” Since postural orthostatic tachycardia syndrome is not a disease, it is fair to say that postural orthostatic tachycardia syndrome is caused by something else. However, figuring out what is causing the symptoms of postural orthostatic tachycardia syndrome in each patient can be very difficult, and in many cases, patients and their doctors will not be able to determine the precise underlying cause. When doctors cannot pinpoint the underlying cause of a patient’s postural orthostatic tachycardia syndrome, it may be called Primary or Idiopathic postural orthostatic tachycardia syndrome 18. Idiopathic simply means “of an unknown origin.”
“Secondary” refers to postural orthostatic tachycardia syndrome with the presence of another medical condition known to cause or contribute towards postural orthostatic tachycardia syndrome symptoms 18. Dr. Julian Stewart has described “high flow” and “low flow” postural orthostatic tachycardia syndrome, based upon the flow of blood in the patients lower limbs 23.
Other researchers have described postural orthostatic tachycardia syndrome based on some of its more prominent characteristics: hypovolemic postural orthostatic tachycardia syndrome, which is associated with low blood volume; partial dysautonomic or neuropathic postural orthostatic tachycardia syndrome which is associated with a partial autonomic neuropathy; and hyperandrenergic postural orthostatic tachycardia syndrome which is associated with elevated levels of norepinephrine 22. These are not distinct medical conditions and many postural orthostatic tachycardia syndrome patients have two or three of the different characteristics present. For example, one patient can have neuropathy, low blood volume and elevated norepineprhine.
Postural orthostatic tachycardia syndrome causes
While researchers are still working to identify the root causes and pathology of postural orthostatic tachycardia syndrome, there are several underlying diseases and conditions that are known to cause or be associated with postural orthostatic tachycardia syndrome or postural orthostatic tachycardia syndrome like symptoms in some patients. This is a partial list:
- Amyloidosis 18;
- Autoimmune Diseases such as Autoimmune Autonomic Ganglionopathy, Sjogren’s Syndrome, Lupus, Sarcoidosis, Antiphospholipid Syndrome 18;
- Chiari Malformation 24;
- Deconditioning 22;
- Delta Storage Pool Deficiency 25;
- Diabetes and pre-diabetes
- Ehlers Danlos Syndrome – a collagen protein disorder than can lead to joint hypermobility and “stretchy” veins 26;
- Genetic Disorders/Abnormalities 27;
- Infections such as Mononucleosis, Epstein Barr Virus, Lyme Disease, extra-pulmonary Mycoplasma pneumonia and Hepatitis C 28;
- Multiple Sclerosis 29;
- Mitochondrial Diseases 30;
- Mast Cell Activation Disorders 27;
- Paraneoplastic Syndrome – rare small tumors of the lung, ovary, breast and pancreas that produce antibodies 18;
- Toxicity from alcoholism, chemotherapy and heavy metal poisoning 18;
- Traumas, pregnancy or surgery 18;
- Vaccinations 31;
- Vitamin Deficiencies/Anemia 32;
Postural orthostatic tachycardia syndrome signs and symptoms
While the diagnostic criteria focus on the abnormal heart rate increase upon standing, postural orthostatic tachycardia syndrome usually presents with symptoms much more complex than a simple increase in heart rate. It is fairly common for postural orthostatic tachycardia syndrome patients to have a drop in blood pressure upon standing, but some postural orthostatic tachycardia syndrome patients have no change or even an increase in blood pressure upon standing.1 postural orthostatic tachycardia syndrome patients often have hypovolemia (low blood volume) and high levels of plasma norepinephrine while standing, reflecting increased sympathetic nervous system activation 27. Approxiamtely 50% of postural orthostatic tachycardia syndrome patients have a small fiber neuropathy that impacts their sudomotor nerves. Many postural orthostatic tachycardia syndrome patients also experience fatigue, headaches, lightheadedness, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, chest pain and shortness of breath 22. Patients can develop a reddish purple color in the legs upon standing, believed to be caused by blood pooling or poor circulation. The color change subsides upon returning to a reclined position.
Postural orthostatic tachycardia syndrome treatment
Therapies for postural orthostatic tachycardia syndrome are targeted at relieving low blood volume or regulating circulatory problems that could be causing the disorder. No single treatment has been found to be effect for all. The most common treatments for postural orthostatic tachycardia syndrome include increasing fluid intake to 2-3 liters per day; adding extra salt to the diet; wearing compression stockings; raising the head of the bed (to conserve blood volume); reclined exercises such as rowing, recumbent bicycling and swimming; a healthy diet; avoiding substances and situations that worsen orthostatic symptoms; and finally, the addition of medications meant to improve symptoms. Many different medications are used to treat postural orthostatic tachycardia syndrome, such as Fludrocortisone, Beta Blockers, Midodrine, Clonidine, Pyridostigmine, Benzodiazepines, SSRIs, SNRIs, Erythropoietin and Octreotide. If an underlying cause of the postural orthostatic tachycardia syndrome symptoms can be identified, treating the underlying cause is very important as well.
Postural orthostatic tachycardia syndrome prognosis
Currently, there is no cure for postural orthostatic tachycardia syndrome, however researchers believe that some patients will see an improvement in symptoms over time. Detailed long term follow up studies on the course of postural orthostatic tachycardia syndrome are sparse. With proper lifestyle adjustments, exercise, diet and medical treatments, many patients see an improvement in their quality of life. If an underlying cause can be identified, and if that cause is treatable, the postural orthostatic tachycardia syndrome symptoms may subside. While the prognosis is good for most patients, researchers have noted that some patients will not improve and may actually worsen over time.
The longest follow-up study done to date comes from Mayo Clinic. Mayo Clinic did a survey 33 of their pediatric postural orthostatic tachycardia syndrome patients seen between 2003 and 2010. Of those who responded to the survey, 18.2% reported a complete resolution of their postural orthostatic tachycardia syndrome symptoms, while 52.8% reported persistent but improved symptoms. Male patients were twice as likely to report recovery. The average survey respondent had been diagnosed for about 5 years. Both patients who fully recovered and those who did not had mental health scores similar to the national norm.
Tachycardia causes
Tachycardia is caused by something that disrupts the normal electrical impulses that control the rate of your heart’s pumping action. Many things can cause or contribute to problems with the heart’s electrical system. These include:
- Damage to heart tissues from heart disease
- Abnormal electrical pathways in the heart present at birth (congenital heart conditions, including long QT syndrome)
- Disease or congenital abnormality of the heart
- Anemia
- Exercise
- Sudden stress, such as fright
- High or low blood pressure
- Smoking
- Fever
- Drinking too much alcohol
- Drinking too many caffeinated beverages
- Medication side effects
- Abuse of recreational drugs, such as cocaine
- Imbalance of electrolytes, mineral-related substances necessary for conducting electrical impulses
- Overactive thyroid (hyperthyroidism)
In some cases, the exact cause of tachycardia can’t be determined.
Risk factors for tachycardia
Any condition that puts a strain on the heart or damages heart tissue can increase your risk of tachycardia. Lifestyle changes or medical treatment may decrease the risk associated with the following factors:
- Heart disease
- High blood pressure
- Sleep apnea
- Overactive or underactive thyroid
- Smoking
- Diabetes
- Heavy alcohol use
- Heavy caffeine use
- Use of recreational drugs
- Psychological stress or anxiety
- Anemia
Other factors that may increase the risk of tachycardia include:
- Older age. Aging-related wear on the heart makes you more likely to develop tachycardia.
- Family. If you have a family history of tachycardia or other heart rhythm disorders, you may have an increased risk of tachycardia.
Tachycardia prevention
The most effective way to prevent tachycardia is to maintain a healthy heart and reduce your risk of developing heart disease. If you already have heart disease, monitor it and follow your treatment plan to lower your tachycardia risk.
Prevent heart disease
Treat or eliminate risk factors that may lead to heart disease. Take the following steps:
- Exercise and eat a healthy diet. Live a heart-healthy lifestyle by exercising regularly and eating a healthy, low-fat diet that’s rich in fruits, vegetables and whole grains.
- Maintain a healthy weight. Being overweight increases your risk of developing heart disease.
- Keep blood pressure and cholesterol levels under control. Make lifestyle changes and take medications as prescribed to correct high blood pressure (hypertension) or high cholesterol.
- Stop smoking. If you smoke and can’t quit on your own, talk to your doctor about strategies or programs to help you break a smoking habit.
- Drink in moderation. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women of all ages and men older than age 65, and up to two drinks a day for men age 65 and younger. For some conditions it’s recommended that you completely avoid alcohol.
- Ask your doctor for advice specific to your condition.
- Don’t use recreational drugs. Don’t use stimulants, such as cocaine. Talk to your doctor about an appropriate program for you if you need help ending recreational drug use.
- Use over-the-counter medications with caution. Some cold and cough medications contain stimulants that may trigger a rapid heartbeat. Ask your doctor which medications you need to avoid.
- Limit caffeine. If you drink caffeinated beverages, do so in moderation (no more than one to two beverages daily).
- Control stress. Avoid unnecessary stress and learn coping techniques to handle normal stress in a healthy way.
- Go to scheduled checkups. Have regular physical exams and report any signs or symptoms to your doctor.
Monitor and treat existing heart disease
If you already have heart disease, you can take steps to lower your risk of developing tachycardia or another arrhythmia:
- Follow the plan. Be sure you understand your treatment plan, and take all medications as prescribed.
- Report changes immediately. If your symptoms change or get worse or you develop new symptoms, tell your doctor immediately.
Tachycardia diagnosis
If you notice your heart racing or beating irregularly, you should see your doctor.
To diagnose your condition and determine the specific type of tachycardia, your doctor will evaluate your symptoms, conduct a thorough physical examination, and ask you about your health habits and medical history.
Several heart tests also may be necessary to diagnose tachycardia.
Electrocardiogram (ECG)
An electrocardiogram, also called an ECG or EKG, is the most common tool used to diagnose tachycardia. It’s a painless test that detects and records your heart’s electrical activity using small sensors (electrodes) attached to your chest and arms.
An ECG records the timing and strength of electrical signals as they travel through your heart. Your doctor can look for patterns among these signals to determine what kind of tachycardia you have and how abnormalities in the heart may be contributing to a fast heart rate.
Your doctor may also ask you to use portable ECG devices at home to provide more information about your heart rate. These devices include:
Holter monitor. This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It records your heart’s activity for an entire 24-hour period, which provides your doctor with a prolonged look at your heart rhythms.
Your doctor will likely ask you to keep a diary during the same 24 hours. You’ll describe any symptoms you experience and record the time they occur.
Event monitor. This portable ECG device is intended to monitor your heart activity over a few weeks to a few months. You wear it all day, but it records only at certain times for a few minutes at a time.
With many event monitors, you activate them by pushing a button when you experience symptoms of a fast heart rate. Other monitors automatically sense abnormal heart rhythms and then start recording. These monitors allow your doctor to look at your heart rhythm at the time of your symptoms.
Electrophysiological test
Your doctor may recommend an electrophysiological test to confirm the diagnosis or to pinpoint the location of problems in your heart’s circuitry.
During this test, a doctor inserts thin, flexible tubes (catheters) tipped with electrodes into your groin, arm or neck and guides them through your blood vessels to various spots in your heart. Once in place, the electrodes can precisely map the spread of electrical impulses during each beat and identify abnormalities in your circuitry.
Cardiac imaging
Imaging of the heart may be performed to determine if structural abnormalities are affecting blood flow and contributing to tachycardia.
Types of cardiac imaging used to diagnose tachycardia include:
- Echocardiogram (echo). An echocardiogram creates a moving picture of your heart using sound waves. An echo can identify areas of poor blood flow, abnormal heart valves and heart muscle that’s not working normally.
- Magnetic resonance imaging (MRI). A cardiac MRI can provide still or moving pictures of how the blood is flowing through the heart and detect irregularities.
- Computerized tomography (CT). CT scans combine several X-ray images to provide a more detailed cross-sectional view of the heart.
- Coronary angiogram. To study the flow of blood through your heart and blood vessels, your doctor may use a coronary angiogram to reveal potential blockages or abnormalities. It uses a dye and special X-rays to show the inside of your coronary arteries.
- Chest X-ray. This test is used to take still pictures of your heart and lungs and can detect if your heart is enlarged.
Stress Test
Your doctor may recommend a stress test to see how your heart functions while it is working hard during exercise or when medication is given to make it beat fast.
In an exercise stress test, electrodes are placed on your chest to monitor heart function while you exercise, usually by walking on a treadmill. Other heart tests may also be performed in conjunction with a stress test.
Tilt table test
This test is sometimes used to help your doctor better understand how your tachycardia contributes to fainting spells. Under careful monitoring, you’ll receive a medication that causes a tachycardia episode.
You lie flat on a special table, and then the table is tilted as if you were standing up. Your doctor observes how your heart and nervous system respond to these changes in position.
Additional tests
Your doctor may order additional tests as needed to diagnose an underlying condition that is contributing to tachycardia and judge the condition of your heart.
Tachycardia treatment
Treatments for tachycardia are designed to address the cause of the condition as well as slow a fast heart rate when it occurs, prevent future episodes and minimize complications.
Stopping a fast heart rate
A fast heartbeat may correct itself, and you may be able to slow your heart rate using simple physical movements. However, you may need medication or other medical treatment to slow down your heartbeat.
Ways to slow your heartbeat include:
Vagal maneuvers. Your doctor may ask you to perform an action, called a vagal maneuver, during an episode of a fast heartbeat.
Vagal maneuvers affect the vagus nerve, which helps regulate your heartbeat. The maneuvers include coughing, bearing down as if you’re having a bowel movement and putting an ice pack on your face.
Medications. If vagal maneuvers don’t stop the fast heartbeat, you may need an injection of an anti-arrhythmic medication to restore a normal heart rate. An injection of this drug is administered at a hospital.
Your doctor also may prescribe a pill version of an anti-arrhythmic drug to take if you have an episode of a fast heartbeat that doesn’t respond to vagal maneuvers.
Cardioversion. In this procedure, a shock is delivered to your heart through paddles, an automated external defibrillator (AED) or patches on your chest. The current affects the electrical impulses in your heart and restores a normal rhythm. It’s generally used when emergency care is needed or when maneuvers and medications aren’t effective.
Preventing episodes of a fast heart rate
With the following treatments, it may be possible to prevent or manage episodes of tachycardia.
Catheter ablation. This procedure is often used when an extra electrical pathway is responsible for an increased heart rate.
In this procedure, a doctor inserts catheters into your groin, arm or neck and guides them through the blood vessels to your heart. Electrodes at the catheter tips can use extreme cold or radiofrequency energy to damage (ablate) the extra electrical pathway and prevent it from sending electrical signals.
Catheter ablation does not require surgery to access the heart, but it may also be performed in conjunction with other heart valve or artery repair surgeries.
Medications. Pill versions of anti-arrhythmic medications may prevent a fast heart rate when taken regularly.
Other types of drugs, such as calcium channel blockers and beta blockers, may be prescribed either as an alternative to or in combination with anti-arrhythmic medications.
Pacemaker. Some types of tachycardias may be treated with a pacemaker. A pacemaker is a small device that’s surgically implanted under your skin. When the device senses an abnormal heartbeat, it emits an electrical pulse that helps the heart resume a normal beat.
Implantable cardioverter. If you’re at risk of having a life-threatening tachycardia episode, your doctor may recommend an implantable cardioverter-defibrillator (ICD).
The pager-sized device is surgically implanted in your chest. The ICD continuously monitors your heartbeat, detects an increase in heart rate and delivers precisely calibrated electrical shocks, if needed, to restore a normal heart rhythm.
Surgery. Open-heart surgery may be needed in some cases to destroy an extra electrical pathway causing tachycardia.
In another type of surgery, called the maze procedure, a surgeon makes small incisions in heart tissue to create a pattern or maze of scar tissue. Because scar tissue doesn’t conduct electricity, it interferes with stray electrical impulses that cause some types of tachycardia.
Surgery is usually used only when other treatment options don’t work or when surgery is needed to treat another heart disorder.
Preventing blood clots
Some people with tachycardia have an increased risk of developing a blood clot that could cause a stroke or heart attack. Your doctor may prescribe a blood-thinning medication to help lower your risk.
Treating an underlying disease
If another medical condition is contributing to tachycardia, such as some form of heart disease or hyperthyroidism, treating the underlying problem may prevent or minimize tachycardia episodes.
- Sheldon RS, Grubb B P, Olshansky B, et al. 2015 Heart Rhythm Society Expert Consensus Statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015;12:e41–63. DOI: 10.1016/j.hrthm.2015.03.029. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5267948/[↩]
- Is sinus node modification appropriate for inappropriate sinus tachycardia with features of postural orthostatic tachycardia syndrome? Pacing Clin Electrophysiol, 24 (2001), pp. 217-230[↩]
- Still AM, Raatikainen P, Ylitalo A, et al. Prevalence, characteristics and natural course of inappropriate sinus tachycardia. Europace. 2005;7:104–12.[↩]
- Nwazue C, Paranjape SY, Black BK, et al. Postural tachycardia syndrome and inappropriate sinus tachycardiad: role of autonomic modulation and sinus node automaticity. J Am Heart Assoc. 2014;3:e000700. DOI: 10.1161/JAHA.113.000700.[↩][↩]
- Morillo CA, Klein GJ, Thakur RK, et al. Mechanism of ‘inappropriate’ sinus tachycardia. Role of sympathovagal balance. Circulation. 1994;90:873–7.[↩]
- Morillo CA, Klein GJ, Thakur RK, et al. Mechanism of ‘inappropriate’ sinus tachycardia. Role of sympathovagal balance. Circulation. 1994;90:873–7[↩]
- Cappato R, Castelvecchio S, Ricci C, et al. Clinical efficacy of ivabradine in patients with inappropriate sinus tachycardia: a prospective, randomized, placebo-controlled, double-blind, crossover evaluation. J Am Coll Cardiol. 2012;60:1323–9. DOI: 10.1016/j.jacc.2012.06.031.[↩]
- Katritsis DG, Camm AJ. Atrioventricular nodal reentrant tachycardia. Circulation 2010;122:831-40. http://circ.ahajournals.org/content/122/8/831.long[↩]
- Katritsis DG, Becker A. The circuit of atrioventricular nodal reentrant tachycardia: a proposal. Heart Rhythm. 2007; 4: 1354–1360.[↩][↩]
- Ventricular arrhythmias and sudden cardiac death. Lancet. 2012 Oct 27;380(9852):1520-9. doi: 10.1016/S0140-6736(12)61413-5. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)61413-5/fulltext[↩]
- B Garner J, M Miller J. Wide Complex Tachycardia – Ventricular Tachycardia or Not Ventricular Tachycardia, That Remains the Question. Arrhythmia & Electrophysiology Review. 2013;2(1):23-29. doi:10.15420/aer.2013.2.1.23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4711501/[↩][↩]
- Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosed and outcome after emergency therapy. Ann Intern Med. 1986;104:766–771. http://annals.org/aim/article-abstract/700488/wide-complex-tachycardia-misdiagnosis-outcome-after-emergent-therapy?volume=104&issue=6&page=766[↩]
- Grubb BP. Termination of ventricular tachycardia by carotid sinus stimulation. Int J Cardiol. 1989;23:397–399. doi: 10.1016/0167-5273(89)90201-5. https://www.ncbi.nlm.nih.gov/pubmed/2737783[↩]
- Drew B, Scheinman M. ECG criteria to distinguish between aberrantly conducted supraventricular tachycardia and ventricular tachycardia. Pacing Clinical Electrophysiol. 1995;18:2194–2208. doi: 10.1111/j.1540-8159.1995.tb04647.x. https://www.ncbi.nlm.nih.gov/pubmed/8771133[↩]
- Mukerji S, Aloka F, Khasnis A. Asymptomatic wide complex tachycardia: a case report. Cases Journal. 2009;2:47. doi:10.1186/1757-1626-2-47. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2630301/[↩]
- Karas B, Grubb BP, Boehm K, Kip K. The postural tachycardia syndrome: a potentially treatable cause of chronic fatigue, exercise intolerance and cognitive impairment. Pacing Clin Electrophysiology. 2000; 22: 344–351.[↩]
- Grubb BP, Row P, Calkins H. Postural tachycardia, orthostatic intolerance and the chronic fatigue syndrome. In: Grubb BP, Olshansky B, eds. Syncope: Mechanisms and Management 2nd Ed. Malden, Mass: Blackwell/Future Press; 2005: 225–244.[↩][↩]
- Postural Tachycardia Syndrome. Blair P. Grubb, Circulation. 2008; 117: 2814-2817. http://circ.ahajournals.org/content/117/21/2814.full[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Goldstein D, Robertson D, Esler M, Straus S, Eisenhofer G. Dysautonomias: clinical disorders of the autonomic nervous System. Ann Intern Med. 2002; 137: 753–763.[↩]
- Low P, Opfer-Gehrking T, Textor S, Benarroch E, Shen W, Schondorf R, Suarez G, Rummans T. Postural tachycardia syndrome (POTS). Neurology. 1995; 45: 519–525. http://n.neurology.org/content/45/3/519[↩]
- Estimation of sleep disturbances using wrist actigraphy in patients with postural tachycardia syndrome. Bagai K1, Wakwe CI, Malow B, Black BK, Biaggioni I, Paranjape SY, Orozco C, Raj SR. Auton Neurosci. Oct 2013; 177(2): 260?265. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3700681/[↩]
- Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Autonomic Neuroscience: Basic and Clinical 161 (2011) 46-48. http://www.autonomicneuroscience.com/article/S1566-0702(11)00035-X/fulltext[↩][↩][↩][↩]
- Increased plasma angiotensin II in postural tachycardia syndrome (POTS) is related to reduced blood flow and blood volume. Stewart JM, Glover JL, Medow MS. Clin Sci (Lond). 2006 Feb;110(2):255-63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4511483/[↩]
- Orthostatic intolerance and syncope associated with Chiari type I malformation. Prilipko, O. et al. J Neurol Neurosurg Psychiatry 2005;76:1034-1036. http://jnnp.bmj.com/content/76/7/1034.full[↩]
- Platelet Delta Granule and Serotonin Concentrations Are Decreased in Patients with Postural Orthostatic Tachycardia Syndrome Presented at the 51st Annual Meeting of the American Society of Hematology, December 6, 2009.[↩]
- Dysautonomia in the joint hypermobility syndrome. Gazit Y, Nahir AM, Grahame R, Jacob G. Am J Med. 2003 Jul;115(1):33-40. https://www.ncbi.nlm.nih.gov/pubmed/12867232[↩]
- The Postural Tachycardia Syndrome (POTS): Pathophysiology, Diagnosis & Management. Satish R Raj, MD MSCI, Indian Pacing Electrophysiol J. 2006 April-Jun; 6(2): 84-99. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1501099/[↩][↩][↩]
- Postural Orthostatic Tachycardia Syndrome Associated With Mycoplasma pneumoniae. Kasmani, Rahil MD, MRCP; Elkambergy, Hossam MD; Okoli, Kelechi MD, MRCP; Infectious Diseases in Clinical Practice: September 2009 – Volume 17 – Issue 5 – pp 342-343. https://journals.lww.com/infectdis/Abstract/2009/09000/Postural_Orthostatic_Tachycardia_Syndrome.16.aspx[↩]
- Autonomic dysfunction presenting as postural orthostatic tachycardia syndrome in patients with multiple sclerosis. Kanjwal K, Karabin B, Kanjwal Y, Grubb BP. Int J Med Sci, 2010 Mar 11;7:62-7.[↩]
- Autonomic dysfunction presenting as orthostatic intolerance in patients suffering from mitochondrial cytopathy. Kanjwal K, Karabin B, Kanjwal Y, Grubb BP. Clin Cardiol. 2010 Oct;33(10):626-9.[↩]
- Postural tachycardia syndrome after vaccination with Gardasil. Blitshteyn, Svetlana. European Journal of Neurology; 2010; Letter to the Editor http://www.dysautonomiaclinic.com/articles/Gardasil_and_POTS.pdf [↩]
- Iron insufficiency and hypovitaminosis D in adolescents with chronic fatigue and orthostatic intolerance. Antiel RM, Caudill JS, Burkhardt BE, Brands CK, Fischer PR. South Med J. 2011 Aug;104(8):609-11. https://www.ncbi.nlm.nih.gov/pubmed/21886073[↩]
- Long-term outcomes of adolescent-onset postural orthostatic tachycardia syndrome. S.J. Kizilbash, S.P. Ahrens, R. Bhatia, J.M. Killian, S. A. Kimmes, E.E. Knoebel, P. Muppa, A.L. Weaver, P.R. Fischer. Clin. Auton. Res. October 2013. Abstract presented at the 24th International Symposium on the Autonomic Nervous System.[↩]