Contents
What is pyloric stenosis
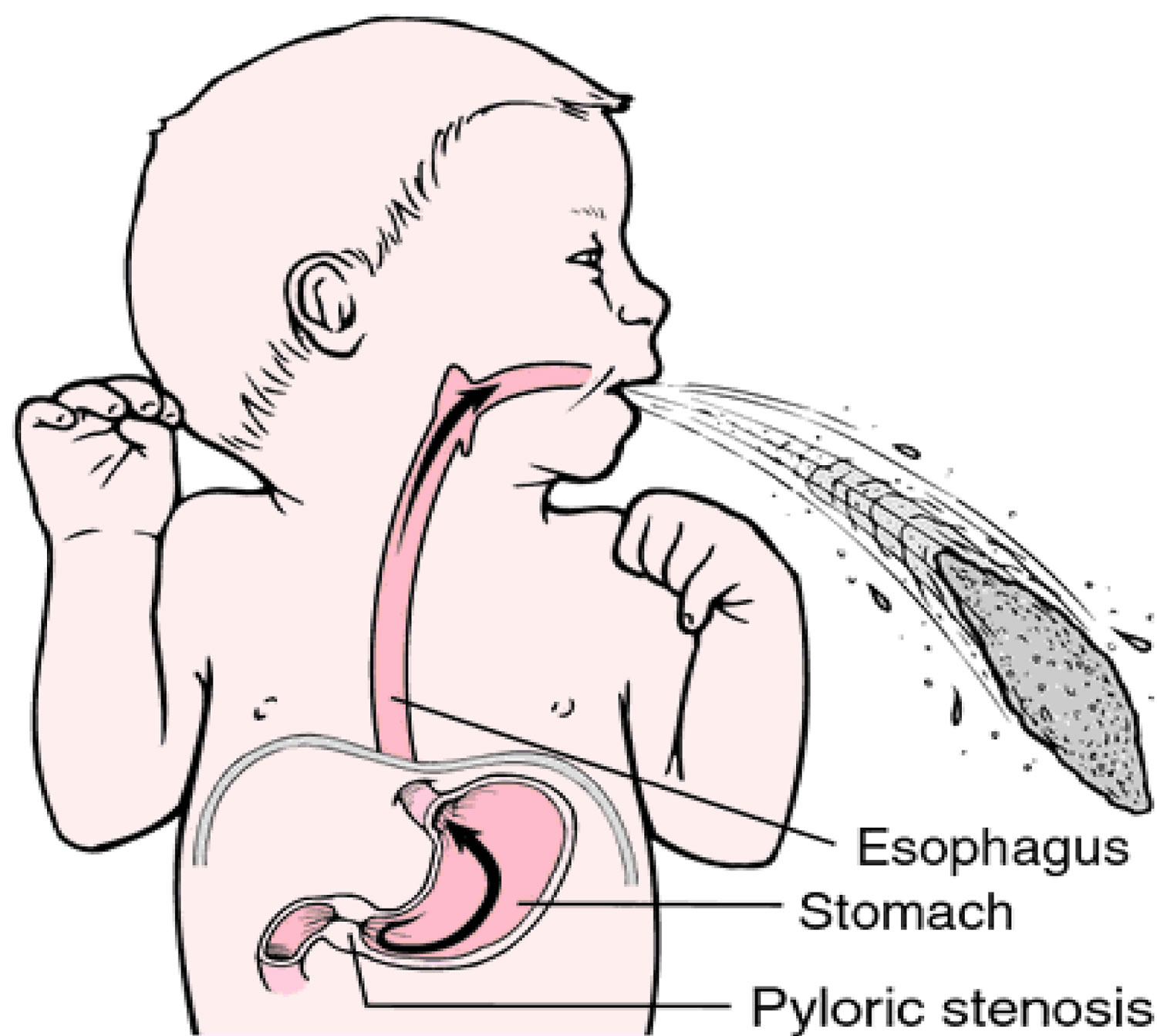
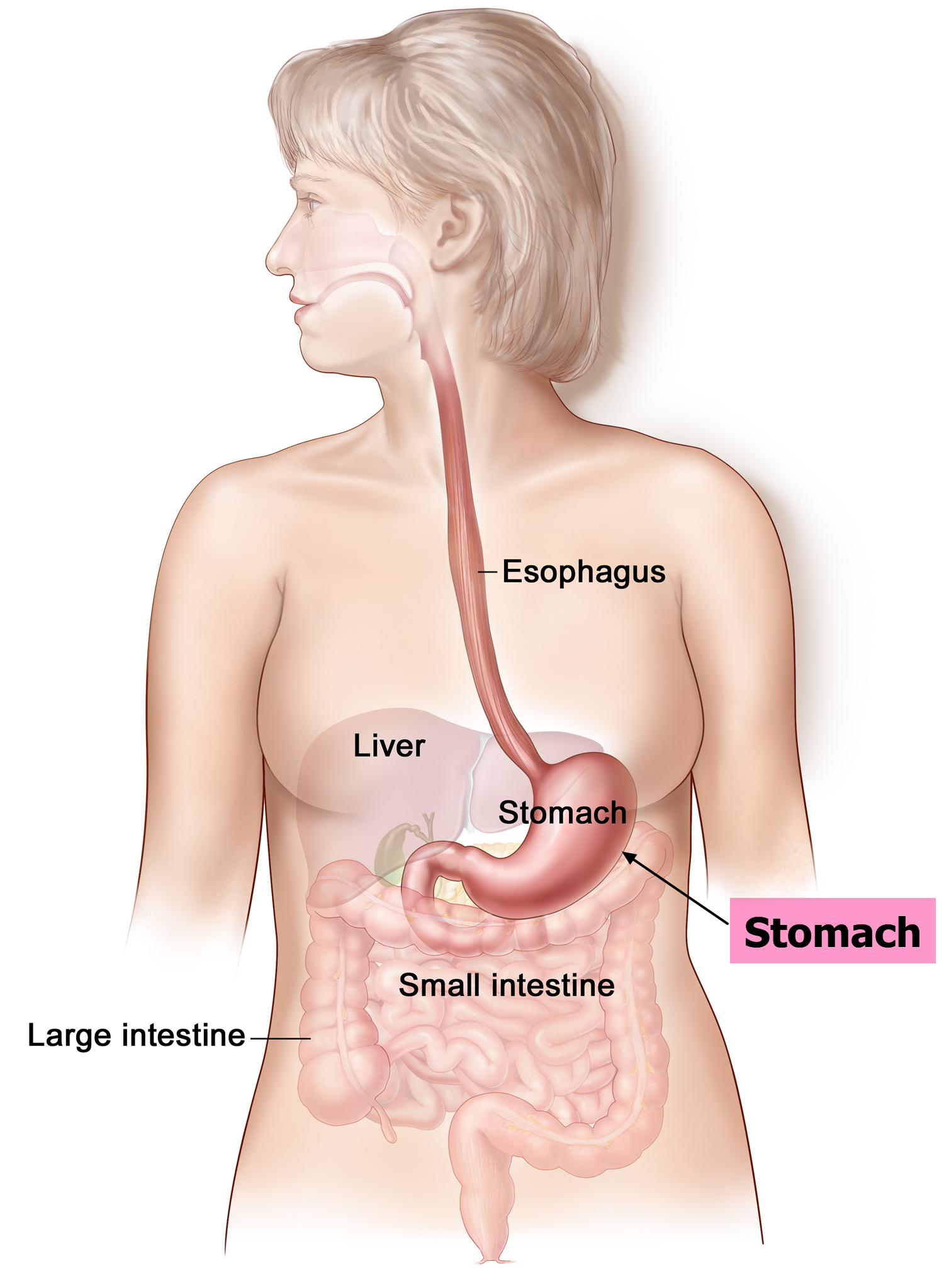
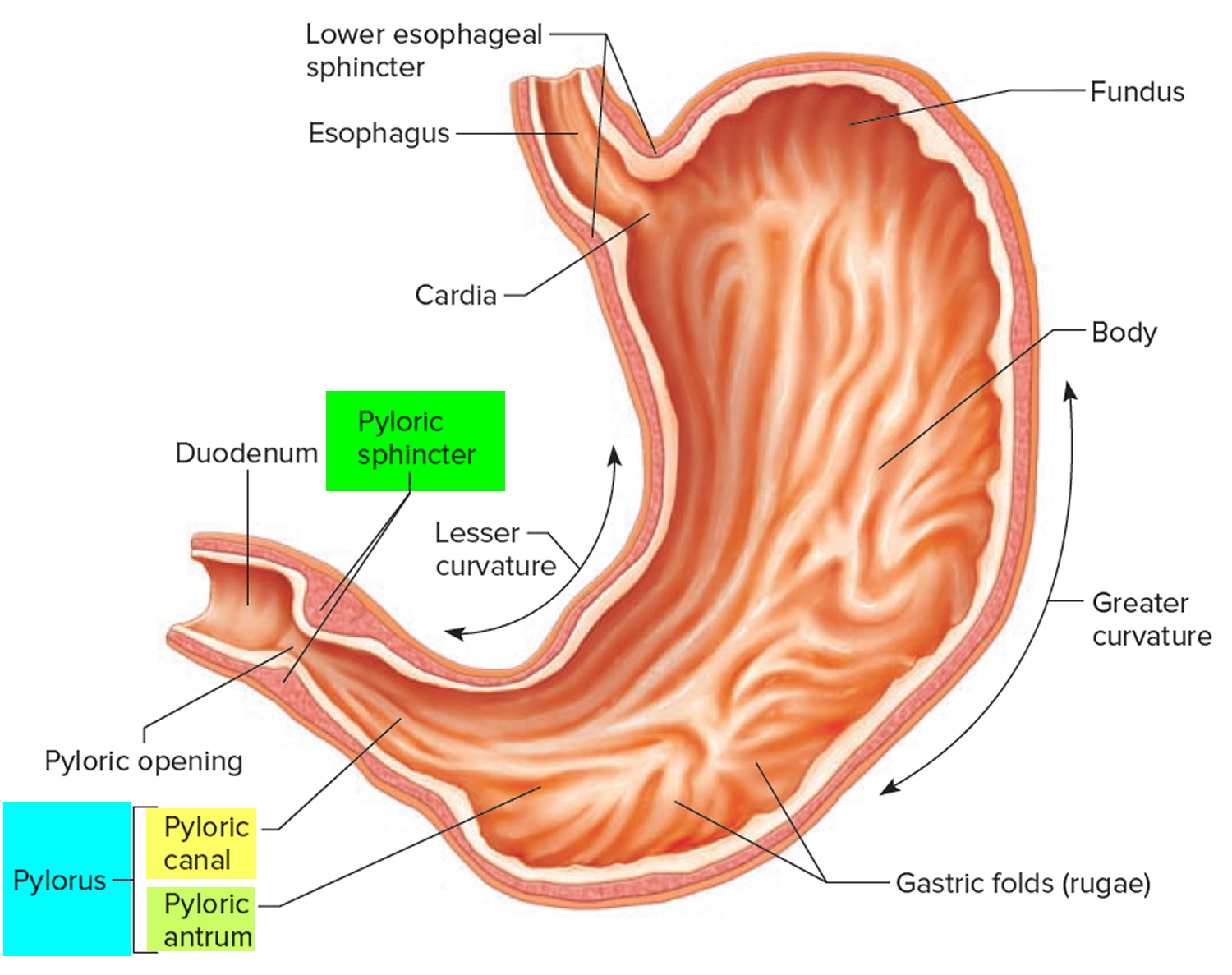
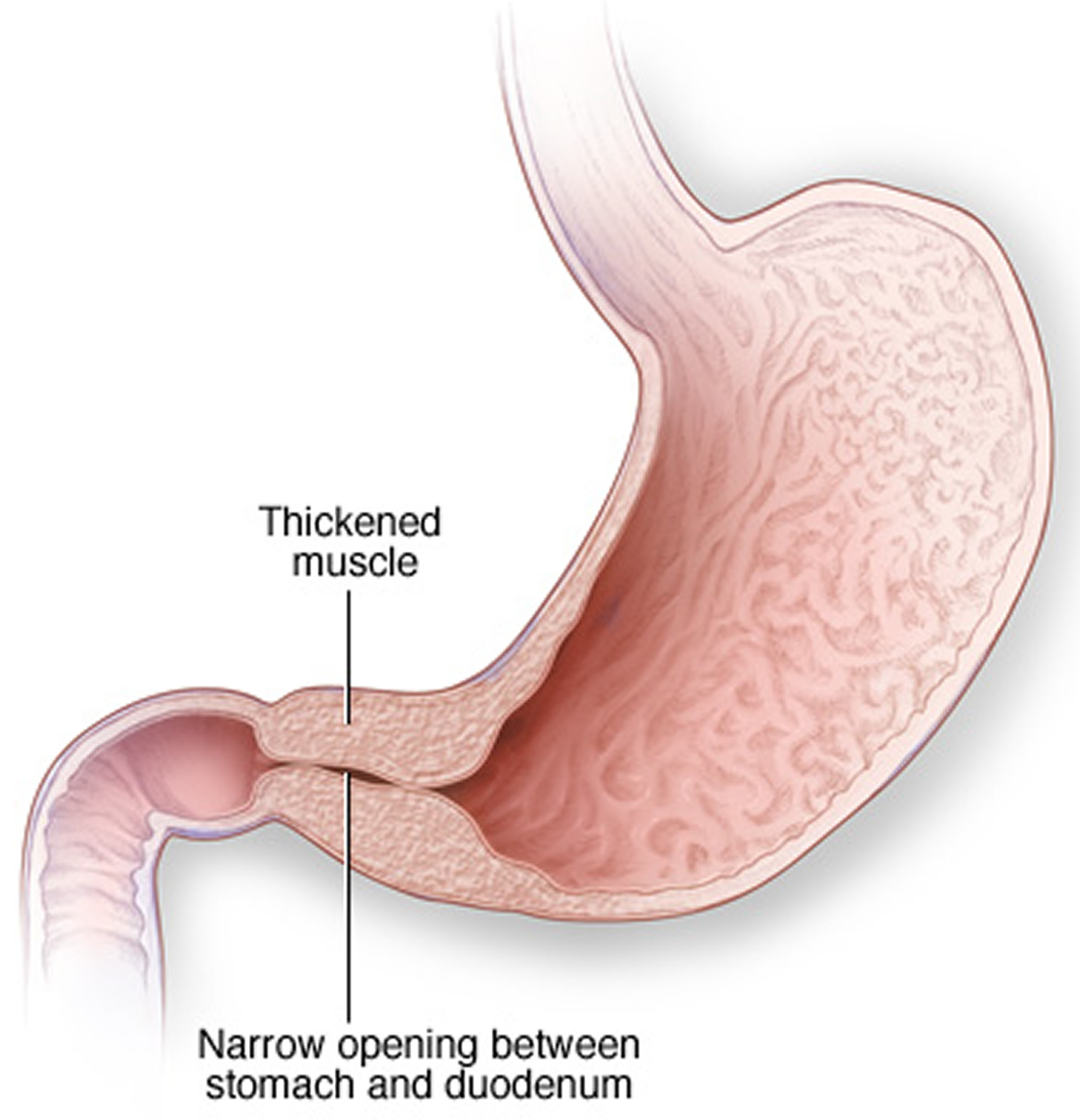
Pyloric stenosis (also called hypertrophic pyloric stenosis) is an uncommon condition in infants where there is a narrowing of the pylorus, the opening from the stomach into the small intestine (duodenum) that blocks food from entering the small intestine. Normally, a muscular valve (pylorus) between the stomach and small intestine holds food in the stomach until it is ready for the next stage in the digestive process (see Figures 1 and 2). In pyloric stenosis, the pylorus muscles thicken and become abnormally large, blocking food from reaching the small intestine (Figures 3 and 4).
The exact cause of the thickening is unknown. Genes may play a role, since children of parents who had pyloric stenosis are more likely to have this condition. Other risk factors include certain antibiotics, too much acid in the first part of the small intestine (duodenum), and certain diseases a baby is born with, such as diabetes.
Pyloric stenosis occurs most often in infants younger than 6 months. It is more common in boys than in girls. Pyloric stenosis is relatively common and has a male predilection (male:female ratio of ~4:1), and is more commonly seen in Caucasians 1. While symptoms may start as early as 3 to 5 weeks after birth, it typically occurs between the 6 to 12 weeks of age. First born children are at higher risk and there may be a positive family history in some cases. If a parent had pyloric stenosis, then a baby has up to a 20% risk of developing it.
Incidence of hypertrophic pyloric stenosis is approximately 2-5 per 1,000 births per year in most white populations in United States. Hypertrophic pyloric stenosis is less common in India and among black and other Asian populations.
Clinical presentation of pyloric stenosis is typical with non-bilious projectile vomiting. Pyloric stenosis can lead to dehydration and weight loss. Babies with pyloric stenosis may seem to be hungry all the time. The hypertrophied pylorus can be palpated as an olive-sized mass in the right upper quadrant. A succussion splash may be audible, and although common, is only relevant if heard hours after the last meal 2.
Surgery cures pyloric stenosis.
See your baby’s doctor if your baby:
- Projectile vomits after feeding
- Seems less active or unusually irritable
- Urinates much less frequently or has noticeably fewer bowel movements
- Isn’t gaining weight or is losing weight
Figure 1. Stomach
Figure 2. Pylorus of the stomach
Figure 3. Hypertrophic pyloric stenosis – in pyloric stenosis, the pylorus muscles thicken, blocking food from entering the baby’s small intestine.
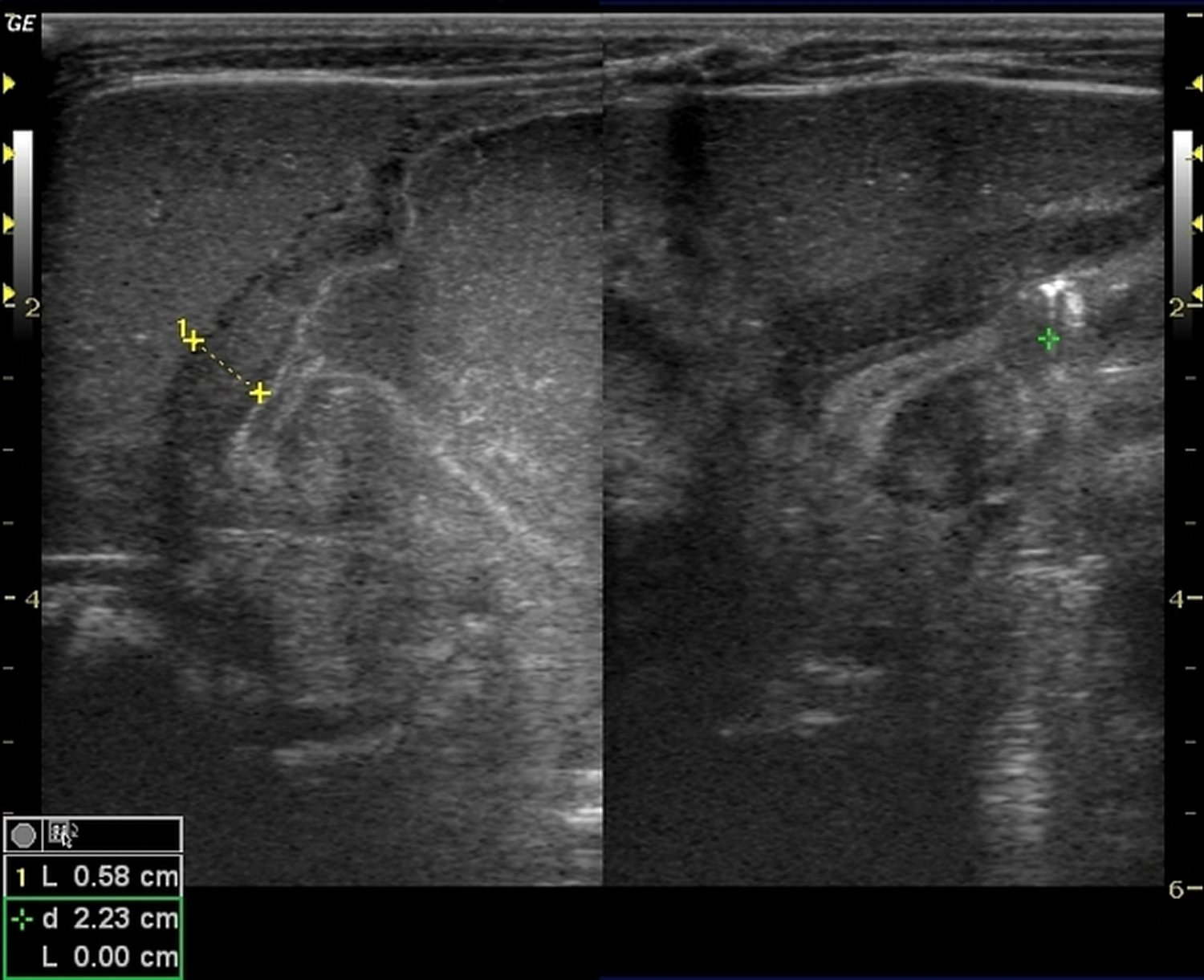
Figure 4. Pyloric stenosis ultrasound
Note: Abdominal ultrasound shows an elongated pyloric canal with increased pyloric muscle thickness. Redundant pyloric mucosa is seen projecting into the gastric antrum on longitudinal image (antral nipple).
Pyloric stenosis in adults
Idiopathic hypertrophic pyloric stenosis, in adults, is a rare disease 3. Pyloric stenosis in adults is a rare disease and presents in adult life as pyloric obstruction, without a history of vomiting in infancy or other gastrointestinal symptoms. Abdominal distention relieved by vomiting is usually the only physical sign. All patients experience weight loss 4. Diagnosis is made with barium contrast upper gastrointestinal series and upper endoscopy 5. Malignancy has to be ruled out. Optimal treatment should provide relief of obstruction, low recurrence and low operative morbidity, since adult idiopathic hypertrophic pyloric stenosis is a benign disease. Pyloromyotomy, pyloroplasty, gastrojejunostomy, endoscopic dilatation and gastrectomy have all been recommended for adult idiopathic hypertrophic pyloric stenosis 6.
Adult hypertrophic pyloric stenosis is classified into three types 5:
- The first type is the late stage of infantile hypertrophic pyloric stenosis, which is easily diagnosed from the history of symptoms during infancy.
- The second type is hypertrophic pyloric stenosis commencing in adult life but secondary to other disease in the upper gastrointestinal tract. This can be a hiatal hernia, duodenal ulcer, gastric ulcer, tumors or inflammatory diseases. This type is the most common and is recognized by a long-standing history of gastrointestinal complaints recently complicated by obstructive symptoms.
- Primary “idiopathic” hypertrophic pyloric stenosis presenting in adult life without any apparent cause is the third type. In this entity, there is no history of vomiting during infancy or other gastrointestinal symptoms. adult idiopathic hypertrophic pyloric stenosis is further divided into two groups.
- In one group, there are no complications from the stenosis.
- In the complicated variety, there is gastritis or peptic ulcer. The sequence of events can differentiate this type from the secondary type of hypertrophic pyloric stenosis 5
Diagnosis is based upon history, clinical and radiological findings and endoscopic appearance. The main symptom in every patient is postprandial upper abdominal distension. The discomfort is relieved by vomiting. Nausea and pain are minimal during vomiting. Anorexia and early satiety can be present. All patients experience weight loss. The absence of pain at the onset of symptoms is a significant diagnostic point. The duration of symptoms can range from 5 weeks to 16 years 5.
Several radiological signs have been described related to adult idiopathic hypertrophic pyloric stenosis. The length of a normal pyloric canal is no more than 1 cm. In adult idiopathic hypertrophic pyloric stenosis, the length may extend up to 4 cm. A convex indentation at the base of the duodenal bulb, known as Kirklin’s sign, is another indication of adult idiopathic hypertrophic pyloric stenosis. An eccentric or concentric narrowing of the pyloric region is the “string sign.” The “Twining’s” sign is a barium filling defect, which can project to either or both sides of the pylorus. It is located 4 to 6 cm proximal to the base of the duodenal bulb 5. Some or all these findings can distinguish adult idiopathic hypertrophic pyloric stenosis from other diseases. In contrast, there are reports that “typical” cases are rare, and the radiological picture is highly variable. Some patients with adult idiopathic hypertrophic pyloric stenosis have repeatedly normal radiographs. In addition, patients with pyloric carcinoma have had x-rays similar to those seen in adult idiopathic hypertrophic pyloric stenosis 7.
Endoscopically, the pylorus is fixed, markedly narrow and has a smooth border. Its appearance has been described as the “cervix sign,” or even as a “donut.” The pylorus fails to close completely even though the peristaltic waves appear to culminate in some degree of contraction in the pyloric area. The main advantage of endoscopy is that it can easily differentiate adult idiopathic hypertrophic pyloric stenosis from other diseases that cause gastric outlet obstruction 5. Biopsy should always be taken to exclude malignancy 6.
Surgical exploration has been advised to establish diagnosis and provide treatment. Gastrectomy, gastrojejunostomy, pyloromyotomy and pyloroplasty have been recommended for adult idiopathic hypertrophic pyloric stenosis. Full-thickness biopsy is proposed for the exclusion of malignancy 6. Most reports in the literature have advocated subtotal distal gastric resection. Pyloromyotomy is undesirable because of possible mucosal laceration and late diverticula. Pyloroplasty is considered technically difficult if the pylorus is grossly thickened and is reserved for the debilitated patient 8. Brahos and Meck have performed a double pyloroplasty in one patient. The closure was completed without tension, and a wide pyloric channel was produced 9. The benign nature of the disease prompted Levine et al 10 to suggest non-operative diagnosis and treatment. The authors have concluded that laparotomy is not required for the diagnosis and that gastroscopic findings are more important than radiographic findings. Dye et al treated a poor operative candidate with endoscopic dilatation. Examination with barium on the following day showed only a slightly wider pyloric channel. The patient subsequently was placed on a solid diet but had occasional vomiting 5. Endoscopic balloon dilatation performed for benign pyloric stenosis from other causes resulted in a high recurrent obstruction rate. In two separate studies, the authors suggested that endoscopic dilatation may palliate symptoms but should be reserved only for patients with high operative risk 11. The patient we are presenting had only temporary relief after two balloon dilatations.
The benign nature of the disease in adults mandates a surgical treatment that can be performed safely and effectively with low morbidity and mortality rate. It is reasonable to relieve the pyloric obstruction as directly and atraumatically as possible. A major operation like gastric resection seems unnecessary for a benign process. The diagnosis can be performed more safely with endoscopy, and pyloroplasty has less morbidity than gastrectomy. Laparoscopic pyloroplasty is a technically feasible operation requiring laparoscopic suturing skills. It can be safely performed in adult idiopathic hypertrophic pyloric stenosis. It provides treatment while preserving the benefits of a minimally invasive surgical technique in the debilitated patient. Laparoscopic pyloroplasty is safe, effective and offers decreased pain, hospital stay and postoperative disability. Larger studies and longer follow-up are required for its establishment as the treatment of choice.
Pyloric stenosis long term effects
Pyloric stenosis can lead to:
- Failure to grow and develop.
- Dehydration. Frequent vomiting can cause dehydration and a mineral (electrolyte) imbalance. Electrolytes help regulate many vital functions.
- Stomach irritation. Repeated vomiting can irritate your baby’s stomach and may cause mild bleeding.
- Jaundice. Rarely, a substance secreted by the liver (bilirubin) can build up, causing a yellowish discoloration of the skin and eyes.
Pyloric stenosis outlook (prognosis)
Surgery usually relieves all symptoms. As soon as several hours after surgery, the infant can start small, frequent feedings.
Pyloric stenosis causes
The causes of pyloric stenosis are unknown, but genetic and environmental factors might play a role. Pyloric stenosis usually isn’t present at birth and probably develops afterward.
Hypertrophic pyloric stenosis is the result of both hyperplasia and hypertrophy of the pyloric circular muscles fibers. The pathogenesis of this is not understood. There are four main theories 12:
- 1) Immunohistochemical abnormalities.
- 2) Genetic abnormalities.
- 3) An infectious cause.
- 4) The hyperacidity theory.
Risk factors for pyloric stenosis
Risk factors for pyloric stenosis include:
- Sex. Pyloric stenosis is seen more often in boys — especially firstborn children — than in girls.
- Race. Pyloric stenosis is more common in Caucasians of northern European ancestry, less common in African-Americans and rare in Asians.
- Premature birth. Pyloric stenosis is more common in babies born prematurely than in full-term babies.
- Family history. Studies found higher rates of this disorder among certain families. Pyloric stenosis develops in about 20 percent of male descendants and 10 percent of female descendants of mothers who had the condition.
- Smoking during pregnancy. This behavior can nearly double the risk of pyloric stenosis.
- Early antibiotic use. Babies given certain antibiotics in the first weeks of life — erythromycin to treat whooping cough, for example — have an increased risk of pyloric stenosis. In addition, babies born to mothers who took certain antibiotics in late pregnancy also may have an increased risk of pyloric stenosis.
- Bottle-feeding. Some studies suggest that bottle-feeding rather than breast-feeding can increase the risk of pyloric stenosis. Most people in these studies used formula rather than breast milk, so it isn’t clear whether the increased risk is related to formula or the mechanism of bottle-feeding.
Pyloric stenosis symptoms
Signs of pyloric stenosis usually appear within three to five weeks after birth. Pyloric stenosis is rare in babies older than age 3 months.
Signs and symptoms include:
- Vomiting after feeding. The baby may vomit forcefully (projectile vomiting), ejecting breast milk or formula up to several feet away (projectile vomiting). Vomiting might be mild at first and gradually become more severe as the pylorus opening narrows. The vomit may sometimes contain blood. Vomiting usually starts around 3 weeks of age, but may start any time between 1 week and 5 months of age.
- Persistent hunger. Babies who have pyloric stenosis often want to eat soon after vomiting.
- Stomach contractions. You may notice wave-like contractions (peristalsis) that ripple across your baby’s upper abdomen soon after feeding, but before vomiting. This is caused by stomach muscles trying to force food through the narrowed pylorus.
- Dehydration. Your baby might cry without tears or become lethargic. You might find yourself changing fewer wet diapers or diapers that aren’t as wet as you expect.
- Changes in bowel movements. Since pyloric stenosis prevents food from reaching the intestines, babies with this condition might be constipated.
- Failure to gain weight or weight loss. Pyloric stenosis can keep a baby from gaining weight, and sometimes can cause weight loss.
Other symptoms may include:
- Abdominal pain
- Burping
- Wave-like motion of the abdomen shortly after feeding and just before vomiting occurs.
Other conditions can cause similar problems. For instance:
- Gastroesophageal reflux usually begins before 8 weeks of age. Gastroesophageal reflux involves lots of spitting up (reflux) after feedings, which can look like vomiting. But most babies with gastroesophageal reflux don’t have projectile vomiting, and while they might have trouble gaining weight, they usually have normal poops.
- A milk protein allergy also can make a baby spit up or vomit, and have diarrhea. But these babies don’t have projectile vomiting.
- Gastroenteritis (inflammation in the digestive tract that can be caused by viral or bacterial infection) also can cause vomiting and dehydration. But babies with gastroenteritis usually also have diarrhea with loose, watery, or sometimes bloody stools. Diarrhea usually isn’t seen with pyloric stenosis.
Pyloric stenosis diagnosis
The condition is usually diagnosed before the baby is 6 months old. Your baby’s doctor will start with a physical examination. Sometimes, the doctor can feel an olive-shaped lump — the enlarged pyloric muscle — when examining the baby’s abdomen. The peristaltic waves in the baby’s abdomen are another telltale sign of pyloric stenosis.
A physical exam may reveal:
- Signs of dehydration, such as dry skin and mouth, less tearing when crying, and dry diapers
- Swollen belly
- Olive-shaped mass when feeling the upper belly, which is the abnormal pylorus
Your doctor might also recommend:
- Blood tests to check for dehydration or electrolyte imbalance or both
- Ultrasound to view the pylorus and confirm a diagnosis of pyloric stenosis
- X-rays of your baby’s digestive system, if results of the ultrasound aren’t clear
Plain radiograph
Abdominal x-ray findings are non-specific but may show a distended stomach with minimal distal intestinal bowel gas.
Fluoroscopy
An upper gastrointestinal series (barium meal) excludes other, more serious causes of pathology, but the findings of a upper gastrointestinal series infer rather than directly visualize the hypertrophied muscle. On upper gastrointestinal fluoroscopy:
- delayed gastric emptying
- peristaltic waves (caterpillar sign)
- elongated pylorus with a narrow lumen (string sign) which may appear duplicated due to puckering of the mucosa (double-track sign)
- the pylorus indents the contrast-filled antrum (shoulder sign) or base of the duodenal bulb (mushroom sign)
- the entrance to the pylorus may be beak-shaped (beak sign)
Ultrasound
Ultrasound is the modality of choice in the right clinical setting because of its advantages over a barium meal are that it directly visualises the pyloric muscle and does not use ionising radiation. Unfortunately, it is incapable of excluding other diagnoses such as midgut volvulus. Easy ultrasound technique is to find gallbladder then turn the probe obliquely sagittal to the body in an attempt to find pylorus longitudinally.
The hypertrophied muscle is hypoechoic, and the central mucosa is hyperechoic.
Diagnostic measurements include (mnemonic “number pi”):
- pyloric muscle thickness, i.e. diameter of a single muscular wall on a transverse image: >3 mm (most accurate 3)
- length, i.e. longitudinal measurement: >15-17 mm
- pyloric volume: >1.5 cc
- pyloric transverse diameter: >13 mm
With the patient right side down the pylorus should be watched and should not be seen to open.
Described sonographic signs include:
- antral nipple sign
- cervix sign
- target sign
Pyloric stenosis treatment
Initial medical management is essential with rehydration and correction of electrolyte imbalances. This should be completed prior to surgical intervention.
Treatment is surgical with a pyloromyotomy in which the pyloric muscle is divided down to the submucosa. This can be performed both open and laparoscopically. The operation is curative and has very low morbidity 1.
Pyloric stenosis surgery
Surgery is needed to treat pyloric stenosis. The procedure (pyloromyotomy) is often scheduled on the same day as the diagnosis. If your baby is dehydrated or has an electrolyte imbalance, he or she will have fluid replacement before surgery.
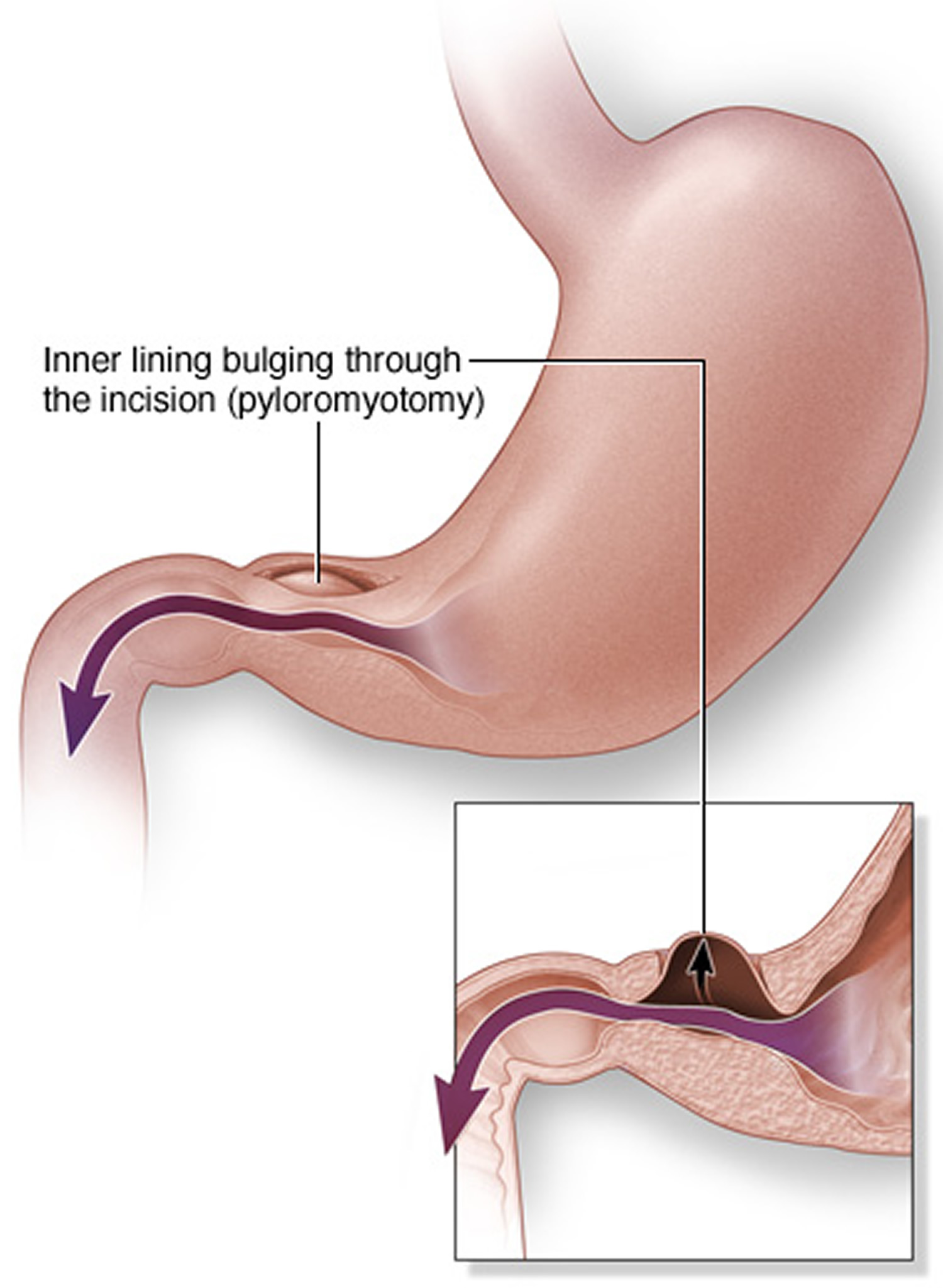
In pyloromyotomy, the surgeon cuts only through the outside layer of the thickened pylorus muscle, allowing the inner lining to bulge out. This opens a channel for food to pass through to the small intestine.
Pyloromyotomy is often done using minimally invasive surgery. A slender viewing instrument (laparoscope) is inserted through a small incision near the baby’s navel. Recovery from a laparoscopic procedure is usually quicker than recovery from traditional surgery, and the procedure leaves a smaller scar.
Figure 5. Pyloric stenosis surgery (Pyloromyotomy)
After pyloric stenosis surgery:
- Your baby might be given intravenous fluids for a few hours or until he or she can eat. You can probably start feeding your baby again within 12 to 24 hours.
- Your baby might want to feed more often.
- Some vomiting may continue for a few days after surgery.
Most babies return to normal feedings fairly quickly, usually 3 to 4 hours after the surgery. Because of swelling at the surgery site, a baby may still vomit small amounts for a day or so. If there are no complications, most babies who have had pyloromyotomy can return to a normal feeding schedule and go home within 24 to 48 hours of the surgery.
If you’re breastfeeding, you might worry about continuing while your baby is hospitalized. The hospital staff should be able to provide a breast pump and help you use it so that you can continue to express milk until your baby can feed regularly.
After a successful pyloromyotomy, your baby won’t need to follow any special feeding schedules. Your doctor will probably want to examine your child at a follow-up appointment to make sure the surgical site is healing properly and that your baby is feeding well and maintaining or gaining weight.
Pyloric stenosis should not happen again after a pyloromyotomy. If your baby still has symptoms weeks after the surgery, there might be another medical problem, such as gastritis or gastroesophageal reflux, so let your doctor know right away.
Potential complications from pyloric stenosis surgery include bleeding and infection. However, complications aren’t common, and the results of surgery are generally excellent.
- Fischer JE, Bland KI. Mastery of surgery. Lippincott Williams & Wilkins. (2007) ISBN:078177165X.[↩][↩]
- Howe CT, Spence MP. Pyloric stenosis in adults. Postgrad Med J. 1960;36 : 743-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2482055/pdf/postmedj00481-0045.pdf[↩]
- Danikas D, Geis WP, Ginalis EM, Gorcey SA, Stratoulias C. Laparoscopic Pyloroplasty in Idiopathic Hypertrophic Pyloric Stenosis in an Adult. JSLS : Journal of the Society of Laparoendoscopic Surgeons. 2000;4(2):173-175. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3015380/[↩]
- Du Plessis DJ. Primary hypertrophic pyloric stenosis in the adult. Br J Surg. 1966;53:485–492 https://www.ncbi.nlm.nih.gov/pubmed/5936976[↩]
- Dye TE, Vidals VG, Lockhart CE, Snider WR. Adult hypertrophic pyloric stenosis. Am Surg. 1979;45:478–484 https://www.ncbi.nlm.nih.gov/pubmed/464395[↩][↩][↩][↩][↩][↩][↩]
- Simson JN, Thomas AJ, Stoker TA. Adult hypertrophic pyloric stenosis and gastric carcinoma. Br J Surg. 1986;73:379–380 https://www.ncbi.nlm.nih.gov/pubmed/3708291[↩][↩][↩]
- Caldwell JH, Cerilli GJ. Adult hypertrophic pyloric stenosis. Report of an unusual case detected by saline load test. Am J Gastroenterol. 1977;67:261–264 https://www.ncbi.nlm.nih.gov/pubmed/868847[↩]
- MacDonald JA. Adult hypertrophic pyloric stenosis. Br J Surg. 1973;60:73–75 https://www.ncbi.nlm.nih.gov/pubmed/4685929[↩]
- Brahos GJ, Mack E. Adult hypertrophic pyloric stenosis managed by double pyloroplasty. JAMA. 1980;243:1928–1929 https://www.ncbi.nlm.nih.gov/pubmed/7365976[↩]
- Levine SM, Brodmerkel G, Burke EL. Idiopathic adult hypertrophic pyloric stenosis. Non-operative diagnosis and management. Gastrointest Endosc. 1969;16:26–29 https://www.ncbi.nlm.nih.gov/pubmed/5798911[↩]
- Lau JY, Chung SC, Sung JJ, et al. Through the scope balloon dilation for pyloric stenosis: long-term results. Gastrointest Endosc. 1996;43:98–101 https://www.ncbi.nlm.nih.gov/pubmed/8635729[↩]
- Rogers I. Open Journal of Pediatrics. 2012;02 (02): . doi:10.4236/ojped.2012.22017 http://file.scirp.org/Html/2-1330082_19844.htm[↩]