Contents
What is Q fever
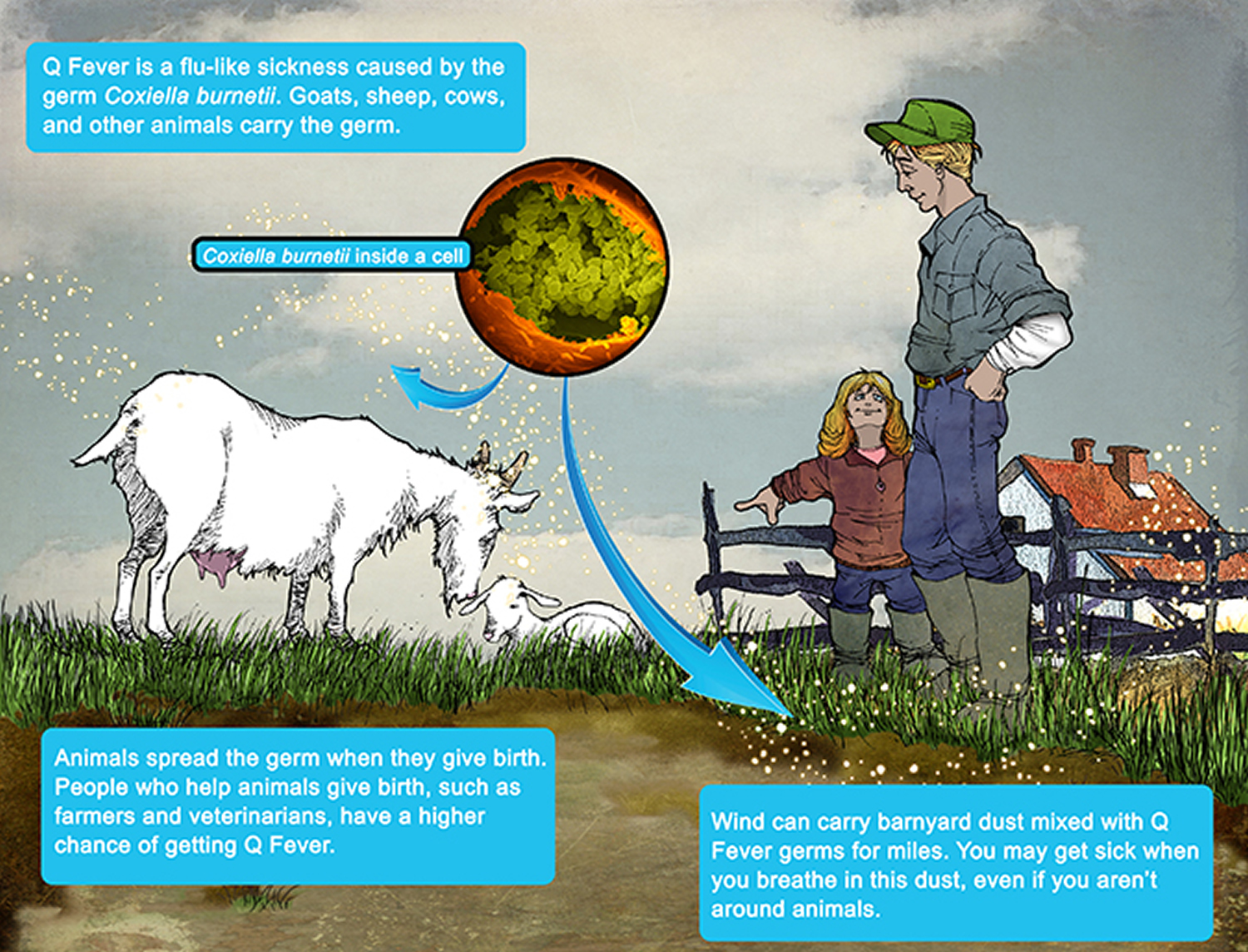
Q fever is an infection caused by Coxiella burnetii bacteria, which usually spreads to people from animals or their infected surroundings. As few as 1-10 Coxiella burnetii organisms may cause disease in a susceptible person. Vaccination is advised for people at high risk such as those who work with animals. However, the Q fever vaccine (available in Australia) is currently not available in the United States.
The Coxiella burnetii bacteria naturally infects some animals, such as goats, sheep, and cattle. However, infection has been confirmed in multiple vertebrate species, including wildlife, marine mammals, domestic mammals, birds, and reptiles 1. Coxiella burnetii bacteria have been isolated from approximately 40 species of ticks, and possible tickborne transmission of C. burnetii to humans has been reported 2. Any infected animal has the potential to transmit the pathogen via bacterial shedding in their body secretions. Human outbreaks and cases have been epidemiologically linked to exposure to multiple species including pigeons, dogs, and rabbits 3. Human cases and outbreaks linked to exposure to infected parturient cats also have been reported 4.
Coxiella burnetii bacteria are found and excreted in milk, urine, and feces of infected animals with the highest numbers shed during birthing in the amniotic fluids and the placenta. The Coxiella burnetii bacteria are extremely hardy and resistant to heat, drying, and many common disinfectants, which enable the bacteria to survive for long periods in the environment. Exposure usually occurs by inhalation of these organisms from air that is contaminated by excreta of infected animals. Other modes of transmission, including tick bites, ingestion of unpasteurized milk or dairy products, and person-to-person transmission, are rare. People are very susceptible to the disease, and very few organisms may be required to cause infection.
Direct contact (e.g. touching, being licked) with an animal is not required to become sick with Q fever. People may also get sick with Q fever by eating contaminated, unpasteurized dairy products. People can get infected by breathing in dust that has been contaminated by infected animal feces, urine, milk, and birth products. Rarely, Q fever has been spread through blood transfusion, from a pregnant woman to her fetus, or through sex. Some people never get sick; however, those who do usually develop flu-like symptoms including fever, chills, fatigue, and muscle pain.
For most people, it’s a mild infection similar to the flu and can be treated easily. But for a few people, Q fever can lead to serious health issues such as pneumonia and hepatitis.
Q fever can cause acute or chronic illness in humans. A few people develop chronic Q fever, which can resurface months or years later and can cause serious problems such as damage to the heart and other organs. Q fever can also cause serious problems for pregnant women.
Certain professions are at increased risk for exposure to Coxiella burnetii, including veterinarians, meat processing plant workers, dairy workers, livestock farmers, and researchers at facilities housing sheep and goats. People working in these areas may need to take extra precautions.
More cases of Q fever are reported in older people. Cases are also more likely to be male; however, jobs at high risk for Q fever exposure, such as ranching or livestock management, may be more commonly held by men. People who live or spend time near ranches and livestock facilities are at increased risk for Q fever infection. Studies have shown that people with a history of heart valve defects, endocarditis, or heart valve implants may increase the risk of chronic infection and severe disease.
Mild cases of Q fever clear up quickly with antibiotic treatment. But if Q fever recurs, you may need to take antibiotics for at least 18 months.
How Q fever is spread
Q fever is most often spread to humans by close contact with infected farm animals. The Coxiella burnetii bacteria can be spread by contact with:
- afterbirth (placenta)
- blood
- pee
- poo
- hides, fur and wool
The Coxiella burnetii bacteria in these products can be breathed in. You can also get Q fever from drinking unpasteurized milk (milk that hasn’t been heated to kill bacteria), but this is less likely.
Although Q fever is rare, people who work closely with animals are more at risk. For example farmers, vets, stablehands and abattoir workers.
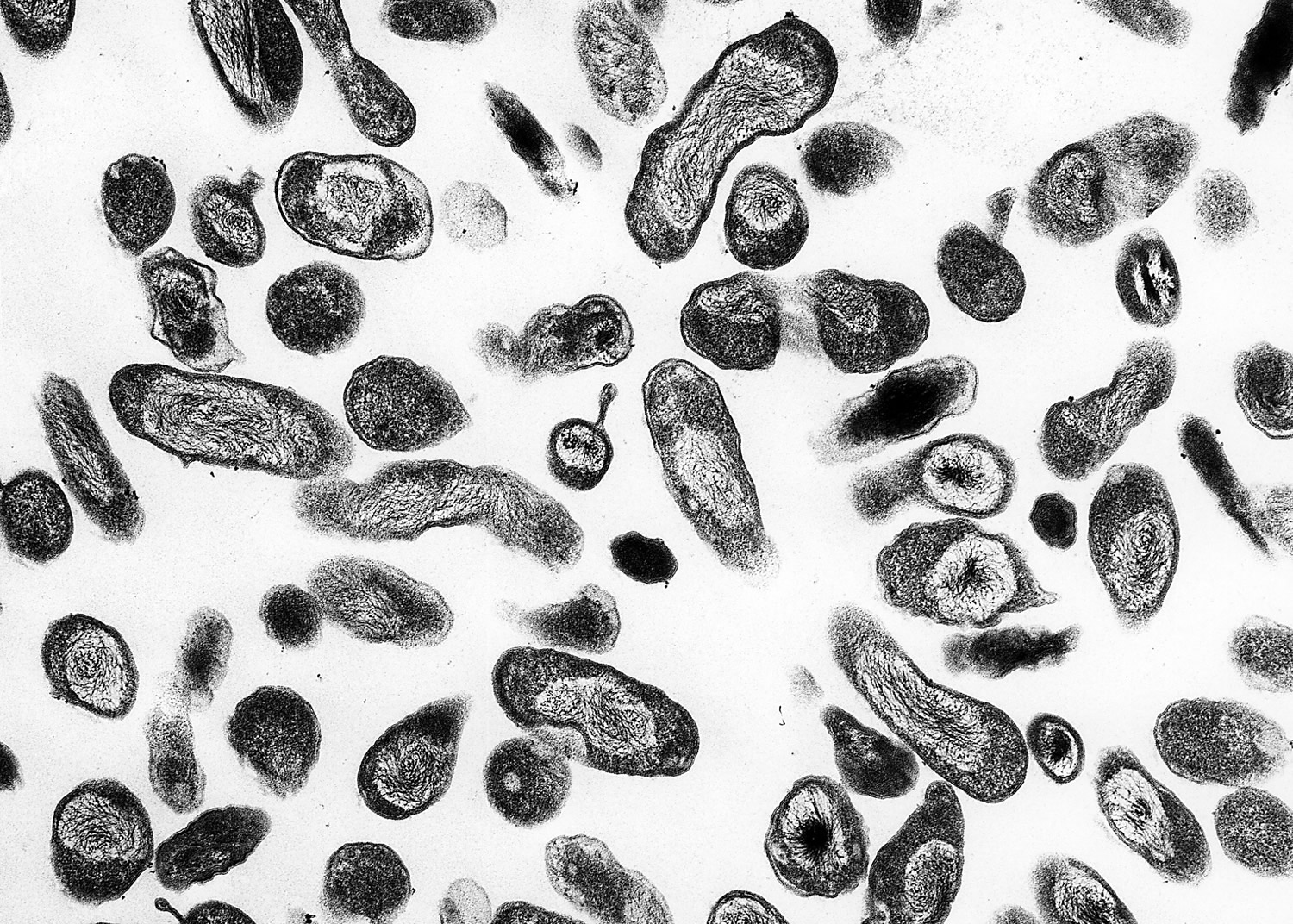
Figure 1. Coxiella burnetii bacteria
[Source 5]See a doctor if you think you have Q fever and:
- you’re pregnant – Q fever can cause miscarriage and if it spreads to your baby it can cause serious complications, especially if you catch it early in pregnancy
- your immune system is weakened, for example if you have had an organ transplant or you are having chemotherapy – the infection may affect your eyes or brain
- you have heart valve disease – where one or more of your heart valves are diseased or damaged
Q fever is usually harmless but in rare cases it can lead to serious problems.
Q Fever in the United States
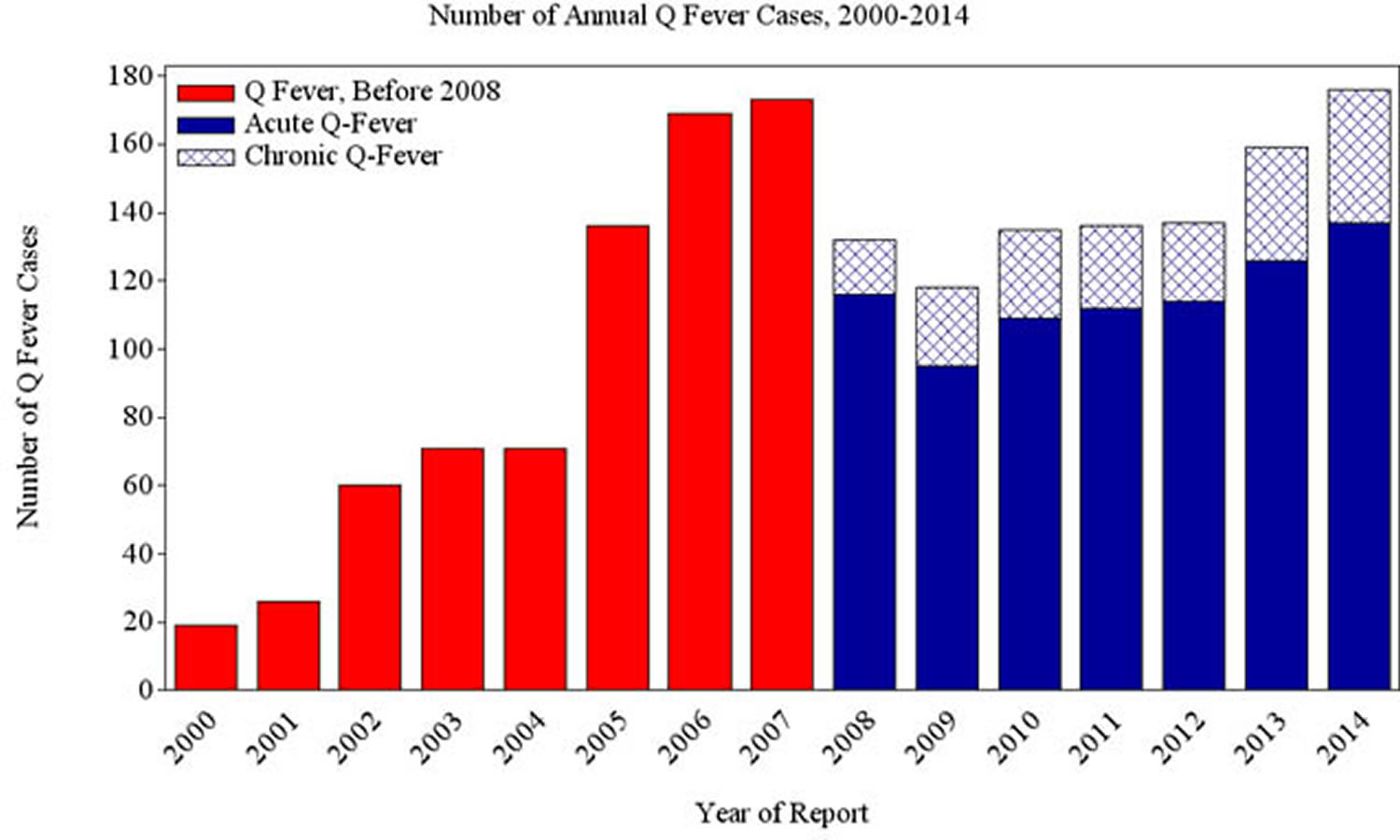
Q fever was made a nationally notifiable disease in the United States in 1999. Centers for Disease Control and Prevention (CDC) compiles the number of cases reported by state and local health departments and reports national trends. The number of Q fever cases reported to the Centers for Disease Control and Prevention has increased, from 19 cases reported in 2000, to 173 cases reported in 2007. In 2008, the Q fever case definition was changed to allow for the reporting of chronic and acute Q fever separately. During 2008–2013, the number of reported cases decreased slightly, relative to 2007, returning to high levels in 2014. In 2014 160 cases of Q fever were reported; of these, 137 were acute Q fever and 39 were chronic Q fever.
Figure 2. Number of U.S. Q Fever cases* reported to CDC, 2000 – 2014.
Note: *Numbers presented here may differ from numbers presented in the Morbidity and Mortality Weekly Report Annual Summary of Notifiable Diseases. Data presented here are based on year of illness onset rather than reporting year.
The graph displays the number of human cases of Q fever reported to CDC annually from 2000 through 2014. Cases of Q fever increased steadily from 19 cases in 2000 when the disease became nationally notifiable, to 173 in 2007. Cases decreased significantly in 2008–2013 relative to 2007, with total cases returning to high levels in 2014. Beginning in 2008, cases were differentiated as acute or chronic. Acute cases generally make up 75-90% of cases reported.
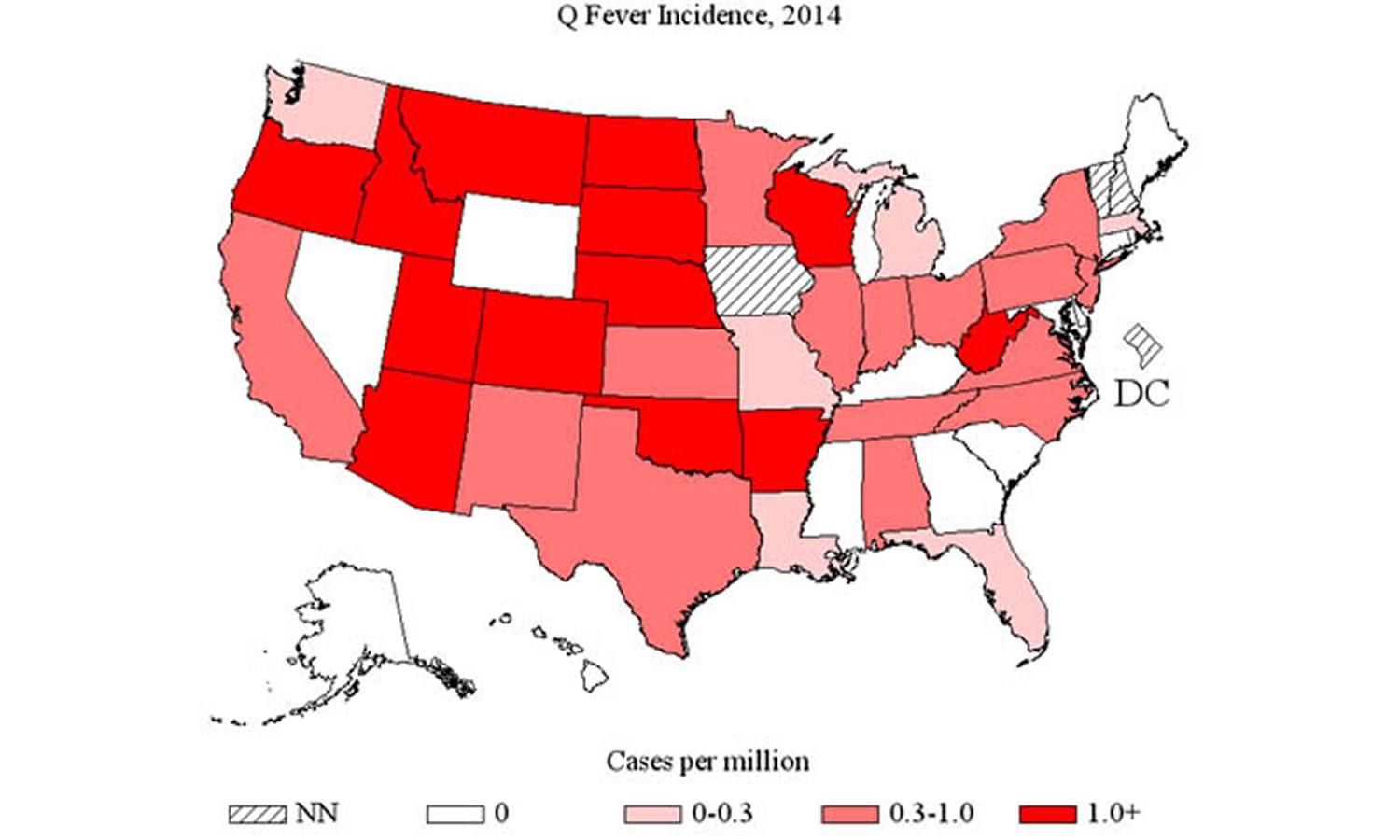
[Source 6]Figure 3. Geographic distribution of Q fever incidence in 2014
Note: This map shows the incidence (number of cases per million persons) of Q fever cases by state in 2014. Q fever was not notifiable in Iowa, New Hampshire, and Vermont, and the District of Columbia in 2014. The incidence rate was zero for Alaska, Connecticut, Delaware, Georgia, Hawaii, Kentucky, Maine, Maryland, Mississippi, Nevada, Rhode Island, South Carolina, and Wyoming. Incidence was greater than zero and less than 0.4 cases per million persons for Florida, Illinois, Indiana, Louisiana, Massachusetts, Michigan, Missouri, North Carolina, Ohio, Tennessee, and Washington. Annual incidence was at least 0.4 and less than 1.0 case per million persons in Alabama, California, Kansas, Minnesota, New Jersey, New Mexico, New York, Oklahoma, Pennsylvania, Texas, Virginia, and Wisconsin. The highest incidence rates, at least 1.0 case per million persons, were found in Arizona, Arkansas, Colorado, Idaho, Montana, Nebraska, North Dakota, Oregon, South Dakota, Utah, and West Virginia.
[Source 6]Q fever hospitalization rates
Q fever infection, especially chronic Q fever, may be severe with complications requiring hospitalization that may include endocarditis (infection of the heart tissue), encephalitis (inflammation of the central nervous system), pneumonia (inflammation of the lungs), hepatitis (inflammation of the liver), and splenomegaly (enlargement of the spleen). Between 2002-2014 over 50% of cases required hospitalization. However, it is likely that mild Q fever infections which do not require hospitalization are more likely to be unrecognized and therefore may not be reported.
Q fever complications
A Q fever recurrence can affect your heart, liver, lungs and brain, giving rise to serious complications, such as:
- Endocarditis. An inflammation of the membrane inside your heart, endocarditis can severely damage your heart valves. Endocarditis is the most deadly of Q fever’s complications.
- Lung issues. Some people who have Q fever develop pneumonia. This can lead to acute respiratory distress, a medical emergency in which you’re not getting enough oxygen.
- Pregnancy problems. Chronic Q fever increases the risk of miscarriage, low birth weight, premature birth and stillbirth.
- Liver damage. Some people who have Q fever develop hepatitis, an inflammation of the liver that interferes with its function.
- Meningitis. Q fever can cause meningitis, an inflammation of the membrane surrounding your brain and spinal cord.
Treatment with doxycycline antibiotic will shorten the course of illness for acute Q fever. Although the majority of people with acute Q fever recover completely, a post-Q fever fatigue syndrome has been reported to occur in up to 20% of patients with acute Q fever. This syndrome is characterized by constant or recurring fatigue, night sweats, severe headaches, photophobia, pain in muscles and joints, mood changes, and difficulty sleeping. No consensus has been reached in the medical community on the pathogenesis or treatment of post Q fever fatigue syndrome.
- Chronic Q fever occurs in <5% of acutely infected patients. It may present within weeks after an acute infection or may manifest many years later. Anyone who was infected with Coxiella burnetii may be at risk for developing chronic Q fever, however, people with a history of valvular defects, arterial aneurisms, or vascular grafts are at increased risk. Women infected by Coxiella burnetii during pregnancy and those with immunosuppression have also been linked to the development of chronic Q fever.
Endocarditis is the most commonly identified manifestation of chronic Q fever and is fatal if untreated. Patients with endocarditis require early diagnosis and long-term antibiotic treatment (at least 18 months) for a successful outcome. Other forms of chronic Q fever include infections of vascular aneurysms, bone, liver, or reproductive organs.
Chronic Q fever
Chronic Q fever is rare, occurring in <5% of persons with acute infection, and might occur within a few months, years, or even decades after the initial acute infection 7. Chronic disease can occur after symptomatic or asymptomatic infections. Potential signs and symptoms include endocarditis, chronic hepatitis, chronic vascular infections, osteomyelitis, osteoarthritis, and chronic pulmonary infections 7. Although patients likely have lifelong immunity to reinfection, disease reappearance might occur and has been well documented 8.
The patients at highest risk for chronic Q fever are those with valvular heart disease, a vascular graft, or an arterial aneurysm. Acute infection in immunosuppressed persons and pregnant women also has been linked to later development of chronic disease 9. Since Q fever was categorized as a notifiable disease in the United States in 1999, CDC has received 49 reports of chronic Q fever, of which 24 manifested as endocarditis 10. Endoc arditis is the major form of chronic Q fever, comprising 60%–78% of all cases worldwide. Endocarditis is a severe condition that is invariably fatal due to heart failure if untreated and has a 10-year mortality rate of 19% in treated patients 11. The
second most common form of chronic Q fever is infection of aneurysms or vascular prostheses, followed by chronic Q fever infections after pregnancy 12. However, during the Q fever outbreak in the Netherlands, vascular infections were the most common form of chronic disease reported 13.
A clinical assessment of patients with acute Q fever should be performed to determine whether they are at high risk for subsequent chronic infection. Approximately 40% of persons with a known valvulopathy with an acute Q fever diagnosis subsequently develop infective endocarditis 14. Patients with endocarditis are predominantly men aged >40 years 11. Similar to other infective endocarditis etiologies, patients at highest risk for development of Q fever endocarditis after acute infection are those with a prosthetic valve, followed by patients with aortic bicuspid valves, mitral valve prolapse, and moderate mitral insufficiency 15.
The initial clinical signs and symptoms in patients with chronic Q fever often are nonspecific and highly variable. Features might include fatigue, fever, abdominal or chest pain, weight loss, night sweats, or hepatosplenomegaly 16. Arterial embolism, pulmonary embolism, or deep venous thrombosis also might occur 11. Valvular vegetations usually are small and are detected by echocardiogram in approximately 12% of cases. Cardiologists evaluating the echocardiogram should be made aware of the suspected diagnosis of chronic Q fever because the lesions, which often are subtle, might be missed 11. A transesophageal echocardiogram (TEE) is more sensitive than a transthoracic echocardiogram (TTE) in detecting valvular defects; TEEs should be performed in patients with
suspected endocarditis who have TTEs that are negative or not definitive 17. However, a negative echocardiogram, whether TTE or TEE, does not rule out a diagnosis of chronic Q fever endocarditis.
In a retrospective study of patients with Q fever endocarditis, the most common abnormality found by echocardiography in patients with chronic Q fever endocarditis was a newly discovered or worsening valvular insufficiency 11. Other echocardiographic findings included vegetations, valvular thickening, calcification, cardiac abscess, stenosis, prosthetic leakage or avulsion, or pericardial effusion. The mitral and aortic valves were most commonly affected. Patients often did not have a previous diagnosis of acute Q fever. The median onset time for endocarditis was 2.5 months (range: 1–66 months) after acute illness among those who received a diagnosis of acute Q fever 11.
Persons with arterial aneurysms or vascular grafts also are at risk for chronic Q fever, and C. burnetii vascular infection carries a high mortality rate even in treated patients 18. Treated patients have an estimated 3-year mortality rate of
25%, a rate much higher than patients with treated Q fever endocarditis, who have an estimated 3-year mortality rate of 7% 18. The majority of C. burnetii vascular infections reported in the literature are aortic infections, which complicate an aortic aneurysm or previously placed endovascular prosthesis 18. The infected aneurysm frequently is diagnosed during surgery because the aortic wall ruptures; death is most commonly caused by vascular rupture. Infections develop more slowly in grafts than in aneurysms. Patients might have culture-negative aortitis 19. Spondylodiscitis and vertebral involvement might occur and should prompt testing for Q fever in patients with aortic defects 18. Imaging techniques that might prove useful for diagnosis of vascular infections include computed tomography, magnetic resonance imaging, or duplex ultrasound. Fluorodeoxyglucose positron emission tomography combined with computed tomography has high sensitivity and specificity for diagnosis of low-grade vascular infections and can visualize other potential infectious foci that cannot be visualized by other imaging methods 16.
Chronic Q fever is rarely reported in children. Pediatric chronic Q fever manifests most frequently as chronic relapsing or multifocal osteomyelitis, blood-culture–negative endocarditis, or chronic hepatitis 20. Children with Q fever osteomyelitis often experience a prolonged course with recurrent episodes affecting multiple bones before diagnosis 21. Like adults, children who are immunocompromised or have underlying heart valve disease might be at higher risk
for chronic Q fever.
Summary of Chronic Q Fever
- Persons who are at high risk for development of chronic Q fever include persons with preexisting valvular heart disease, vascular grafts, or arterial aneurysms.
- Infection during pregnancy and immunosuppression (e.g., from chemotherapy) are both conditions that have been linked to chronic Q fever development.
- Endocarditis and infections of aneurysms or vascular prostheses are the most common forms of chronic Q fever and generally are fatal if untreated.
- Chronic Q fever is rarely reported in children.
- In contrast with adults, osteomyelitis is one of the most common findings in children with pediatric chronic Q fever.
Q fever causes
Q fever is caused by the bacterium Coxiella burnetii, commonly found in sheep, goats and cattle. The bacterium can also infect pets, including cats, dogs and rabbits.
These animals transmit the bacteria through their urine, feces, milk and birthing products — such as the placenta and amniotic fluid. When these substances dry, the bacteria in them become part of the barnyard dust that floats in the air. The infection is usually transmitted to humans through their lungs, when they inhale contaminated barnyard dust.
Risk factors for Q fever
Certain factors can increase your risk of being infected with Q fever bacteria, including:
- Occupation. Certain occupations place you at higher risk because you’re exposed to animals and animal products as part of your job. At-risk occupations include veterinary medicine, meat processing, livestock farming and animal research.
- Location. Simply being near a farm or farming facility may put you at higher risk of Q fever, because the bacteria can travel long distances, accompanying dust particles in the air.
- Your sex. Men are more likely to develop symptomatic acute Q fever.
- Time of year. Q fever can occur at any time of the year, but the number of infections usually peaks in April and May in the U.S.
Risk factors for chronic Q fever
The risk of eventually developing the more deadly form of Q fever is increased in people who have:
- Heart valve disease
- Blood vessel abnormalities
- Weakened immune systems
- Impaired kidney function
How to prevent Q fever
A Q fever vaccine has been developed in Australia for people who have high-risk occupations, but it’s not available in the United States. If you work with animals:
DO
- wash your hands regularly
- clean cuts or grazes immediately and cover them with a plaster or dressing
- wear protective clothing, such as waterproof gloves and goggles
- ensure all animal afterbirth (placenta) is cleaned up safely
DON’T
- help animals give birth if you’re pregnant
- touch anything that may have been in contact with animal blood, poo, pee or afterbirth – such as clothes, boots or gloves
- drink milk that hasn’t been heated yet to kill bacteria (unpasteurized)
- eat in areas where animals are kept
It’s especially important for pregnant women to avoid contact with sheep and lambs during the lambing season.
Don’t touch anything that might have come into contact with ewes or lambs, such as gloves or boots. Pregnant women who catch Q fever don’t usually have any symptoms, so it’s better to avoid any risk.
Why should pregnant women avoid sheep during the lambing season?
Q fever infections in women that occur shortly before conception or during pregnancy might result in miscarriage, stillbirth, premature birth, intrauterine growth retardation, or low birthweight 22. Adverse pregnancy outcomes are likely to be caused by vasculitis or vascular thrombosis resulting in placental insufficiency, although direct infection of the fetus has been documented 23. Of the reports that describe outcomes of infected pregnant women, none have documented an increased risk for congenital malformations because of infection 23.
Women infected with Q fever during pregnancy are at high risk for developing chronic Q fever, possibly because of a failure to mount an appropriate immune response to acute infection or the ability of C. burnetii to use placental trophoblasts as a replicative niche 24. The earlier during pregnancy a woman is infected, the greater her risk for development of chronic disease 22. After a diagnosis of new onset acute infection, treatment throughout pregnancy is recommended to decrease the risk for an adverse birth outcome as well as the risk for future development of chronic Q fever 22. Chronic infection might be evidenced by increased phase I IgG C. burnetii titers that do not decrease after pregnancy and can lead to adverse outcomes during subsequent pregnancies 25.
To avoid the risk of infection, if you’re pregnant or think you might be pregnant:
- do not help deliver lambs (or calves or kids)
- do not milk ewes
- avoid contact with aborted (miscarried) or newborn lambs, and with the afterbirth, birthing fluids or contaminated materials, such as bedding
- ensure your partner washes thoroughly after contact with ewes that are lambing
- clothing worn during lambing should be washed separately from other washing
Farmers are responsible for minimizing the risk to pregnant women and members of their family, the public and professional staff who visit their farms.
Occupational Exposure and Prevention
Certain occupations are associated with increased risk for exposure to Coxiella burnetii, as might their associated institutions and businesses. Multiple Q fever outbreaks have been reported among workers in slaughterhouses, farms, animal research facilities, military units, and, rarely, hospitals and diagnostic laboratories (12,151–156). Employees in high-risk occupations should be educated about the risk for exposure and the clinical presentation of Q fever. Educational efforts should describe groups vulnerable to development of chronic Q fever, such as workers who have preexisting valvulopathy, a prosthetic heart valve, a vascular prosthesis, an aneurysm, are pregnant or might become pregnant, or are immunosuppressed, because these employees have a higher risk for a severe outcome or death if infected. Although protection for at-risk workers can be provided by Q fever vaccination, a licensed vaccine for humans is only commercially available in Australia (157). Therefore, most workers in high-risk occupations in the United States are not vaccinated.
Transmission of Coxiella burnetii to health-care personnel has been rarely reported (158,159). One obstetrician was infected through contact with the birth fluids of an infected parturient woman (48). Hospital personnel have become infected after autopsies of patients with Q fever, although the infection control precautions used, if any, are unknown (49,160).
Adherence to standard precautions is recommended to prevent Q fever infection in health-care personnel during routine care 26. During autopsies of patients who have died of Q fever, health-care personnel should use either a BSL-3 facility or use the barrier precautions of BSL-2 and the negative airflow and respiratory precautions of BSL-3 as recommended by the CDC Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories 27. During procedures that put health-care personnel at risk for infection from splashing of infected material, such the delivery of an infant from an infected woman, standard precautions including the use of a face mask and eye protection or a face shield are recommended. Care should be used when handling soiled laundry (e.g., bedding, towels, and personal clothing) of Q fever patients. Soiled laundry should not be shaken or otherwise handled in a way that might aerosolize infectious particles.
During any procedure that might generate aerosols of infectious materials (e.g., a procedure involving use of a surgical power instrument such as an oscillating bone saw) in a patient with suspected or confirmed Q fever, health-care personnel should also take the following precautions:
- Use a fit-tested N-95 (or comparable) respirator and eye protection (e.g., goggles or face shield).
- Contain and dispose of contaminated waste (e.g., dressings or birth products) in accordance with facility-specific guidelines for infectious waste.
- Place the patient in an airborne infection isolation room or a private room if one is not available during the procedure. The patient does not need to wear a face mask, because Q fever is not transmitted by sneezing or coughing.
- Handle used patient-care equipment in a way that prevents contamination of skin and clothing. Ensure that used equipment has been cleaned and reprocessed appropriately.
- Ensure that procedures are in place for cleaning and disinfecting environmental surfaces in the patient care environment.
Precautions used in addition to standard precautions are only recommended during an aerosol-generating procedure. Procedures that do not generate aerosols, such as drawing blood or giving physical examinations, do not pose a risk for transmission of Q fever. Transmission through coughing or sneezing is not a documented route of infection, and there is no evidence that Q fever is transmitted by any type of casual contact (e.g., hugging, shaking hands, kissing, or sharing food).
- The majority of occupationally related Q fever outbreaks in the United States have occurred among biomedical research facility workers exposed to infected pregnant ewes.
- Workplaces with employees at high risk for Coxiella burnetii exposure (e.g., laboratories that experiment with Coxiella burnetii and animal research facilities) should institute a Q fever medical surveillance and health education monitoring program. Engineering controls, administrative controls, and use of personal protective equipment are recommended when appropriate.
- Use of standard precautions by health-care providers is sufficient to prevent Q fever transmission during routine care. Additional precautions should be used during aerosol-generating procedures.
- Use of postexposure prophylaxis is not recommended for workers after a known or potential exposure; any acute febrile illness that occurs within 6 weeks of exposure warrants immediate treatment and medical evaluation.
Q fever signs and symptoms
Adults
About 5 out of 10 people infected with Coxiella burnetii will get sick. Illness typically develops 2-3 weeks after being exposed to the bacteria. Signs and symptoms of Q fever may include:
- Fever up to 105 °F (41 °C)
- Chills or sweats
- Fatigue (tiredness)
- Headache
- Muscle aches
- Nausea, vomiting, or diarrhea
- Chest pain
- Stomach pain
- Weight loss
- Swollen lymph glands
- Non-productive cough
- Sensitivity to light
Symptoms can be mild or severe. Symptoms of Q fever usually last up to 2 weeks.
People who develop severe disease may experience infection of the lungs (pneumonia) or liver (hepatitis).
Women who are infected during pregnancy may be at risk for miscarriage, stillbirth, pre-term delivery, or low infant birth weight.
Children
Children with Q fever are less likely to have symptoms than adults and might have a milder illness. Acute Q fever in symptomatic children typically is characterized by a febrile illness, often accompanied by headache, weakness, cough, and other nonspecific systemic symptoms. Illness frequently is self-limited, although a relapsing febrile illness lasting for several months has been documented in some children 28. Gastrointestinal symptoms such as diarrhea, vomiting, abdominal pain, and anorexia are reported in 50%–80% of pediatric cases 29. Skin rash is more common in children than adults, with a prevalence as high as 50% among children with diagnosed cases 29. Q fever pneumonia is usually moderate with mild cough; respiratory distress and chest pain might occur. Severe manifestations of acute disease are rare in children and include hepatitis, hemolytic uremic syndrome, myocarditis, pericarditis, encephalitis, meningitis, hemophagocytosis, lymphadenitis, acalculous cholecystitis, and rhabdomyolysis 30.
- Children with Q fever generally have a milder acute illness than adults.
- Children are more likely to have a rash than adults. Rash has been reported in up to 50% of children with acute Q fever.
Pregnant Women
Q fever infections in women that occur shortly before conception or during pregnancy might result in miscarriage, stillbirth, premature birth, intrauterine growth retardation, or low birthweight 22. Adverse pregnancy outcomes are likely to be caused by vasculitis or vascular thrombosis resulting in placental insufficiency, although direct infection of the fetus has been documented 23. Of the reports that describe outcomes of infected pregnant women, none have documented an increased risk for congenital malformations because of infection 22.
Pregnant women might be less likely to have symptoms of Q fever compared with other adults (e.g., a febrile illness), although they remain at risk for adverse pregnancy outcomes 31. As a result, if a pregnant woman with no history of clinical illness has only a single increased antibody titer, it is difficult for the health-care provider to determine whether the increase is from a previous or current infection. Serosurveys of pregnant women evaluating a possible association between a single, elevated C. burnetii antibody titer (which cannot differentiate between previous or current infection) and adverse pregnancy outcomes have reported mixed findings 32. A woman with a previous infection (>30 days before conception) with no evidence of progression to chronic disease does not require treatment during pregnancy. However, a Q fever infection during pregnancy requires antibiotic treatment (see Table 3 below), and health-care providers should consider several factors to determine the best treatment approach. Careful assessment of serologic results are useful because the phase II antibody response is increased in patients with an acute infection but decreases during convalescence as the phase I antibody response increases. Factors to consider before initiating treatment include whether the patient had contact with infected livestock, occupational animal contact, or an epidemiological link to another person with Q fever to guide treatment decisions.
The risk for adverse effects on the fetus and the risk that the mother will develop chronic Q fever are highest when an acute infection occurs during the first trimester 33. Untreated infection in the first trimester is more likely to result in miscarriage, whereas infection later in pregnancy is more likely to cause premature delivery 22. Women infected with acute Q fever during pregnancy, including those who were asymptomatic or experienced no adverse pregnancy outcomes, might be at risk for recrudescent infection during subsequent pregnancies 34. Therefore, pregnant women with a history of Q fever infection during a previous pregnancy should be monitored closely for recrudescent infection in all subsequent pregnancies.
Women of childbearing age who receive a diagnosis of acute Q fever should be aware of the potential risks to the fetus. These women should avoid pregnancy for at least 1 month after diagnosis and treatment and should receive a pregnancy test to determine whether long-term antibiotic treatment is needed.
Chronic Q fever
A very small percentage of people (less than 5 out of 100) who become infected with Coxiella burnetii bacteria develop a more serious infection called chronic Q fever. Chronic Q fever develops months or years following initial Q fever infection. People with chronic Q fever often develop an infection of one or more heart valves (called endocarditis). People with endocarditis may experience night sweats, fatigue, shortness of breath, weight loss, or swelling of their limbs. A healthcare provider will need to perform a series of tests to diagnose endocarditis.
Chronic Q fever is serious and can be deadly if not treated correctly. Chronic Q fever infection requires months of antibiotic treatment. Chronic Q fever is more likely to occur in people with heart valve disease, blood vessel abnormalities, or in people with weakened immune systems. Women infected during pregnancy may also be at risk for developing chronic Q fever.
- Persons who are at high risk for development of chronic Q fever include persons with preexisting valvular heart disease, vascular grafts, or arterial aneurysms.
- Infection during pregnancy and immunosuppression (e.g., from chemotherapy) are both conditions that have been linked to chronic Q fever development.
- Endocarditis and infections of aneurysms or vascular prostheses are the most common forms of chronic Q fever and generally are fatal if untreated.
- Chronic Q fever is rarely reported in children.
- In contrast with adults, osteomyelitis is one of the most common findings in children with pediatric chronic Q fever.
Q fever diagnosis
The symptoms of Q fever are similar to many other diseases, often making diagnosis difficult. See your healthcare provider if you develop symptoms after spending time with or near animals—particularly sheep, goats, and cattle—or in areas where these animals may have been.
Information such as recent travel to rural or agricultural communities where infected livestock may be present, or employment in high-risk occupations, such as veterinarians or farmers, can be helpful in making the diagnosis.
Chronic Q fever is a risk for anyone with a history of acute Q fever, but are more frequent in persons with valvular disease, blood vessel abnormalities, immunosuppressed persons, and women who were pregnant when they became infected. Persons with these risk factors should be routinely monitored using serologic methods for the 2 years following diagnosis of acute Q fever to ensure rapid diagnosis and treatment of chronic Q fever.
To diagnose Q fever, your doctor will perform one or more blood tests, along with additional tests if chronic Q fever is suspected.
Lab tests
Your doctor may want to check your blood for antibodies to the Coxiella burnetii antigen and for evidence of liver damage.
Diagnostic tests based on the detection of antibodies will frequently appear negative in the first 7-15 days of illness. For this reason, healthcare providers must treat patients based on clinical suspicion alone and not wait for the return of confirmatory tests.
Detection of Coxiella burnetii DNA by polymerase chain reaction (PCR) can rapidly confirm an acute Q fever infection. Samples are ideally taken during the first 2 weeks of illness and before or shortly following doxycycline antibiotic administration. For definitive diagnosis in the early stages of illness it is recommended to use serologic tests in combination with polymerase chain reaction of whole blood or serum. Treatment should be initiated as soon as Q fever is suspected and should never be withheld pending the receipt of diagnostic test results.
Table 1. Types of Q fever diagnostic testing analyses, by phase of infection, type of sample, and interval since onset of symptoms
Phase of infection and type of sample | Interval since onset of symptoms | Type of analysis |
|---|---|---|
Acute | ||
Whole blood | Until day 14 (and before antibiotic therapy) | PCR |
Serum | Until day 21 for IFA Until day 14 for PCR (and before antibiotic therapy) | IFA for phase I and II IgG and IgM; PCR |
Convalescent | ||
Serum | 3–6 weeks after acute sample | IFA for phase I and II IgG and IgM |
Chronic | ||
Whole blood | >6 weeks after acute illness | PCR |
Serum | >6 weeks after acute illness | IFA for phase I and II IgG and IgM; PCR |
Heart valve and other tissues | 6 weeks to years | PCR, culture, IHC |
Abbreviations: IFA = immunofluorescent assay; IgG = immunoglobulin G; IgM = immunoglobulin M; IHC = immunohistochemistry; PCR = polymerase chain reaction. | ||
Imaging tests
- Chest X-ray. Q fever can cause pneumonia in some people. A chest X-ray can be used to see if your lungs look healthy.
- Echocardiography. If chronic Q fever is suspected, your doctor may do an echocardiogram to check for problems with your heart valves.
Laboratory Confirmation
Diagnosis of Acute Q fever
Chronic Q fever is confirmed by elevated phase I IgG antibody >1:1024 (and is typically higher than phase II IgG) and an identifiable persistent focus of infection (e.g., endocarditis). Whole blood, serum or tissue biopsies may be tested by polymerase chain reaction (PCR) for Coxiella burnetii. Polymerase chain reaction (PCR) of whole blood has low sensitivity in patients with chronic Q fever endocarditis, so serum antibody titers should also be tested. Polymerase chain reaction or immunohistochemistry of biopsy specimens from the site of active infection has also been used to diagnose chronic Q fever. These tests may be appropriate for endocarditis patients undergoing valve replacement surgery or patients with hepatitis.
Table 2. CDC surveillance case definition and case classification for acute and chronic Q fever
Acute Q fever | Chronic Q fever | |
|---|---|---|
Clinical evidence of infection | Fever and one or more of the following: rigors, severe retrobulbar headache, acute hepatitis, pneumonia, or elevated liver enzymes | Newly recognized culture-negative endocarditis (particularly in a patient with previous valvulopathy or compromised immune system), suspected infection of a vascular aneurysm or vascular prosthesis, or chronic hepatitis, osteomyelitis, osteoarthritis, or pneumonitis in the absence of other known etiology |
Laboratory criteria*,† | Laboratory confirmed (one or more of the following): | Laboratory confirmed (one or more of the following): |
• Fourfold change in IgG antibody titer to Coxiella burnetii phase II antigen by IFA between paired sera | • IgG titer ≥1:800§ to C. burnetii phase I antigen by IFA | |
• Detection of C. burnetii DNA in a clinical specimen by PCR | ||
• Detection of C. burnetii DNA in a clinical specimen by PCR | • Demonstration of C. burnetii in a clinical specimen by IHC | |
• Demonstration of C. burnetii in a clinical specimen by IHC | • Isolation of C. burnetii from a clinical specimen by culture | |
• Isolation of C. burnetii from a clinical specimen by culture | ||
Laboratory supportive (one or more of the following): | Laboratory supportive: | |
• Single IgG titer ≥1:128 to C. burnetii phase II antigen by IFA (phase I titers may be elevated as well) or | • IFA IgG titer ≥1:128 and <1:800§ to C. burnetii phase I antigen | |
• Elevated phase II IgG or IgM antibody reactive with C. burnetii antigen by ELISA, dot-ELISA, or latex agglutination | ||
Case classification | Confirmed acute Q fever: | Confirmed chronic Q fever: |
Laboratory-confirmation with clinical evidence of infection or an epidemiological link to a laboratory-confirmed case | Clinical evidence of infection with laboratory confirmation | |
Probable acute Q fever: | Probable chronic Q fever: | |
Clinical evidence of infection with laboratory-supportive results | Clinical evidence of infection with laboratory-supportive results | |
Abbreviations: ELISA = enzyme-linked immunosorbent assay; IFA = indirect immunofluorescence antibody assay; IgG = immunoglobulin G; IgM = immunoglobulin M; IHC = immunohistochemistry; PCR = polymerase chain reaction. * CDC prefers simultaneous testing of paired samples. IgM tests are not strongly supportive of serodiagnosis because the response might be persistent (making it unreliable as an indicator of recent infection) or nonspecific (resulting in false positives). ELISA tests are not quantitative and cannot be used to measure changes in antibody titer; thus, they can only be used for classification of probable cases. Performing laboratories determine the appropriate cutoff titers for ELISA. Serologic test results should be interpreted with caution because baseline antibodies acquired as a result of previous exposure to Q fever might exist, especially in patients with rural or farming backgrounds. † Patients with suspected chronic Q fever should be evaluated for titers both to phase I and phase II antigens. Serologic test results should be interpreted with caution because baseline antibodies acquired as a result of previous exposure to Q fever might exist, especially in patients with rural or farming backgrounds. § U.S. laboratories use a twofold dilution scheme that does not result in a titer equaling 800; in this document, a titer of 1024 is used as the replacement. | ||
Q fever treatment
Q fever is treated with the antibiotic doxycycline. How long you take the medicine depends on whether or not you have acute or chronic Q fever. For acute infections, antibiotic treatment lasts two to three weeks.
People who have chronic Q fever usually must take a combination of antibiotics for at least 18 months. Even after successful chronic Q fever treatment, you’ll need to go back for follow-up tests for years in case the infection returns.
Mild or nonsymptomatic cases of acute Q fever often get better with no treatment. However, if you have symptoms of Q fever or if you’re pregnant, antibiotic treatment is recommended. Your treatment plan may vary if you’re unable to take doxycycline.
If you have Q fever endocarditis, you may need surgery to replace damaged heart valves.
Acute Q Fever in Adults
The majority of acute Q fever cases resolve spontaneously within 2–3 weeks, even without treatment. Symptomatic patients with confirmed or suspected acute Q fever, including children with severe infections, should be treated with doxycycline (see Table 3). Doxycycline is the most effective treatment for Q fever. Treatment is most effective if given within the first 3 days of symptoms, shortens the illness, and reduces the risk for severe complications 13. Other antibiotic regimens that can be used if doxycycline is contraindicated because of allergies include moxifloxacin, clarithromycin, trimethoprim/sulfamethoxazole, and rifampin 22. Treatment for acute Q fever is not routinely recommended for asymptomatic persons or for those whose symptoms have resolved, although it might be considered in those at high risk for developing chronic Q fever. In one study of acute Q fever patients who were monitored over time for progression to chronic disease, those who eventually had chronic Q fever were more likely to have not received appropriate doxycycline treatment during their acute illness because their symptoms were mild or they were asymptomatic 13.
Patients with acute Q fever should undergo a careful clinical assessment to determine whether they might be at risk for progression to chronic Q fever because patients at high risk require closer observation during the convalescent period. A thorough clinical assessment should include review of possible immunosuppressive conditions, pregnancy testing when appropriate, and assessment for vascular and heart valve defects because certain valvular lesions might not be detectable by auscultation 35. A medical history and clinical examination alone might not be sufficient to identify patients with existing heart valve defects 36; health-care providers should use their clinical judgment to determine the most appropriate tools for assessment of risk.
Q fever antibiotics
Doxycycline is the recommended first-line treatment for non-pregnant adults with Q fever and is most effective at preventing severe complications if it is started within the first 3 days of symptoms. Treatment must be based on clinical suspicion and should alwfiays begin before laboratory results return. If the patient is treated within the first 3 days of the disease, fever generally subsides within 72 hours. Severely ill patients may require longer periods before their fever resolves.
Treatment is generally not recommended for patients who are asymptomatic or who have already recovered from their illness, but might be considered for those at high risk of developing chronic Q fever. There is no role for prophylactic antimicrobial agents in preventing Q fever after a known, naturally occurring exposure and prior to symptom onset; attempts at prophylaxis will likely extend the incubation period by several days but will not prevent infection from occurring.
Recommended Treatment and Dosage for Acute Q Fever
- Adults: Doxycycline, 100 mg every 12 hours for 14 days
- Pregnant women: trimethoprim/sulfamethoxazole, 160 mg/800 mg given twice a day throughout pregnancy, but not beyond 32 weeks gestation
- Children 8 years or older: doxycycline, 2.2 mg/kg body weight (up to 100mg) given twice a day for 14 days
- Children under 8 years with high risk criteria (i.e., those that are hospitalized, have severe illness, preexisting heart valvulopathy, immunocompromised, or delayed treatment for Q fever > 2 weeks): doxycycline, 2.2 mg/kg body weight (up to 100 mg) given twice a day for 14 days
- Children under 8 years with mild or uncomplicated illness: doxycycline, 2.2 mg/kg body weight (up to 100 mg) given twice a day for 5 days. If patient remains febrile past 5 days of treatment, treat with trimethoprim/sulfamethoxazole 4-20 mg/kg/24 hours (dose based on trimethoprim component) in equally divided doses every 12 hours (maximum: 320 mg trimethoprim per 24 hours).
Recommended Treatment and Dosage for Chronic Q Fever
Duration of treatment for chronic Q fever is based on serologic response and evidence of clinical improvement. Serologic monitoring of a patient with chronic Q fever should be done in consultation with an infectious disease specialist.
- Adults with endocarditis or vascular infection: doxycycline, 100 mg every 12 hours and hydroxychloroquine, 200 mg every 8 hours, for at least 18 months.
- Adults with non-cardiac organ disease: doxycycline, 100 mg every 12 hours and hydroxychloroquine, 200 mg every 8 hours.
- Postpartum women with titers elevated >12 months after delivery: doxycycline, 100 mg every 12 hours and hydroxychloroquine, 200 mg every 8 hours for 12 months.
- Pregnant women: no current recommendations. Consultation with an infectious disease and obstetric specialist is encouraged.
- Children: no current recommendations. Consultation with a pediatric infectious disease specialist is encouraged.
Doxycycline and Children
Short course therapy (e.g., <5 days) with doxycycline does not cause staining of permanent teeth, and most experts consider the benefit of doxycycline in treating Q fever greater than the potential risk of dental staining. Children with mild illness who are less than 8 years of age may be treated with a shorter dose (5 days) of doxycycline to minimize their exposure to the medication. Children with preexisting cardiac valve disease, or who are immunocompromised, or have delayed Q fever diagnosis and have experienced illness for 2 weeks without resolution of symptoms are considered to be at high risk for developing severe disease and should be treated with doxycycline for 2 weeks.
Other Treatments
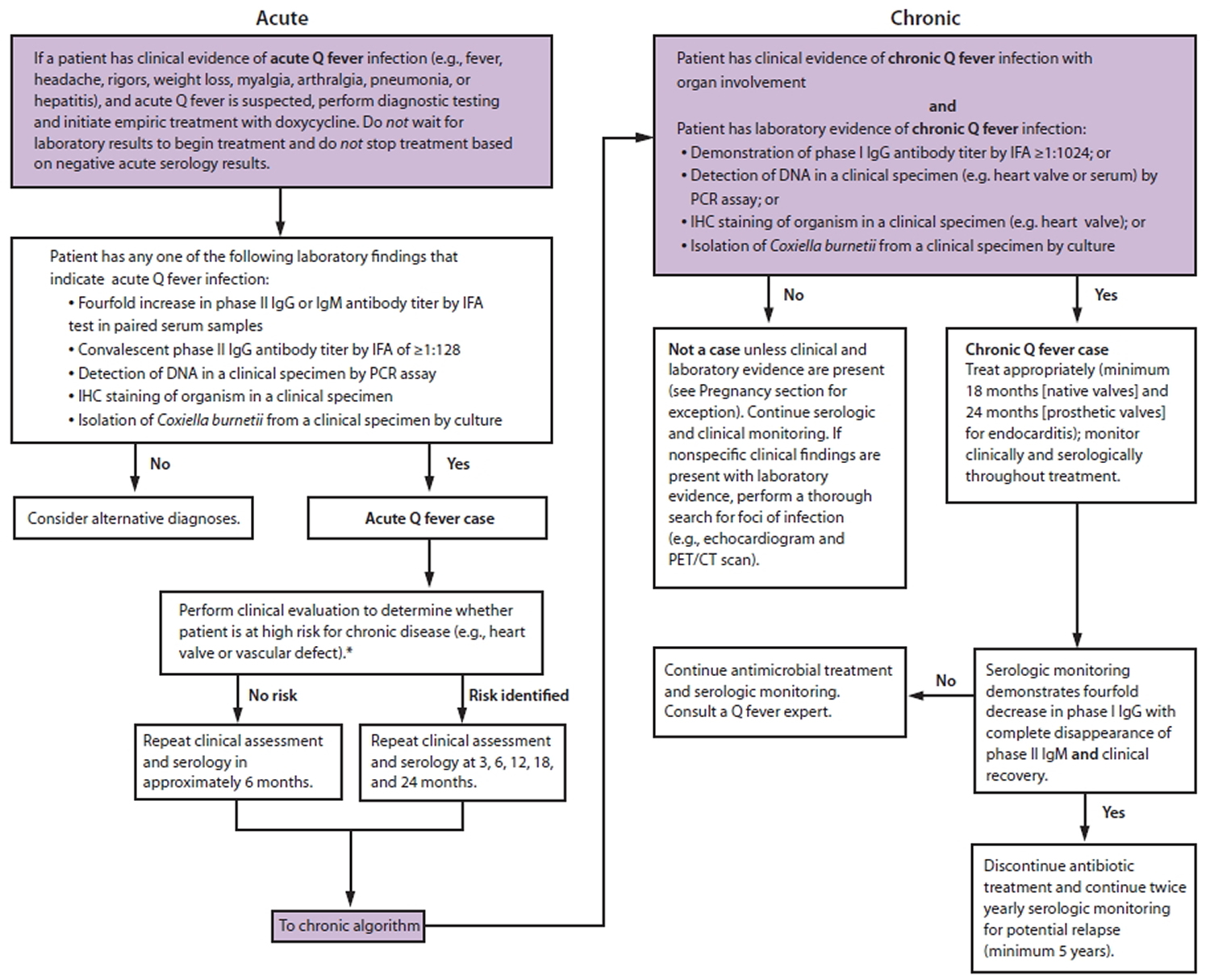
People with life-threatening allergies to doxycycline may need to consider alternate antibiotics such as moxifloxacin, clarithromycin, trimethoprim/sulfamethoxazole and rifampin. For more in-depth information about the treatment and management of Q fever see Figure 4 and Table 3 below.
Figure 4. Q fever treatment algorithm
Abbreviations: CT = computed tomography; IFA = immunofluorescent assay; IgG = immunoglobulin G; IgM = immunoglobulin M; IHC = immunohistochemistry; PCR = polymerase chain reaction; PET = positron emission tomography.
* This algorithm is intended for use as a general guide and does not replace the physician’s clinical judgment. It is intended to provide a management strategy for
patients under the care of a physician and is not intended for those who might be tested for Q fever as part of an occupational monitoring program. Women infected during pregnancy should be treated and monitored as described in the text of the report 37.
Table 3. Recommended antibiotics and dosages* for treatment of acute and chronic Q fever
Indication | Adults | Children¶ | Pregnant women |
|---|---|---|---|
Acute Q fever† | Doxycycline§ 100 mg twice a day for 14 days | ≥8 years: | Trimethoprim/sulfamethoxazole: 160 mg/800 mg twice a day throughout pregnancy but not beyond 32 weeks’ gestation†† |
<8 years with high risk criteria**: Doxycycline: 2.2 mg/kg per dose twice a day for 5 days (maximum: 100 mg per dose) If patient remains febrile past 5 days of treatment: trimethoprim/sulfamethoxazole 4–20 mg/kg/24 hours (dose based on trimethoprim component) in equally divided doses every 12 hours (maximum: 320 mg trimethoprim per 24 hours) | |||
<8 years with mild or uncomplicated illness: Doxycycline 2.2 mg/kg per dose twice a day for 5 days (maximum 100 mg per dose). If patient remains febrile past 5 days of treatment: trimethoprim/sulfamethoxazole 4–20 mg/kg twice a day for 14 days (maximum: 800 mg per dose) | |||
Chronic Q fever | |||
Endocarditis or vascular infection | Doxycycline§§ 100 mg twice a day and hydroxychloroquine¶¶ 200 mg three times a day ≥18 months | Recommend consultation*** | Recommend consultation††† |
Noncardiac organ disease§§§ | Doxycycline 100 mg twice a day and hydroxychloroquine 200 mg three times a day | Recommend consultation*** | Recommend consultation††† |
Postpartum¶¶¶ with serologic profile for chronic Q fever | Doxycycline 100 mg twice a day and hydroxychloroquine 200 mg three times a day for 12 months | — | — |
Post-Q fever fatigue syndrome**** | No current recommendations | No current recommendations | No current recommendations |
* All drug dosages are oral regimens. † Prophylactic treatment after a potential Q fever exposure is not recommended; treatment is not recommended for asymptomatic infections or after symptoms have resolved, although it might be considered in persons at high risk for development of chronic Q fever. § Patients may take doxycycline with food to avoid stomach upset but should have no dairy products within 2 hours (before or after) of taking medication. Doxycycline should not be taken with antacids or bismuth-containing products, and patients should avoid taking it immediately before going to bed or lying down. Doxycycline might cause photosensitivity and can decrease the efficacy of hormonal contraceptives. ¶ Doxycycline is the drug of choice for treatment of Q fever in adults and patients of any age with severe illness. Short courses (≤5 days) for treatment of rickettsial infections have not been shown to result in significant dental staining in children; however, whether a 2-week course will cause permanent tooth discoloration in children is unknown. Health-care providers should use their clinical judgment to determine appropriate therapy in children aged <8 years and may consider treatment with trimethoprim/sulfamethoxazole or a shorter duration of doxycycline (5 days) in children with a mild or uncomplicated illness. Trimethoprim/sulfamethoxazole is contraindicated in children aged <2 months. ** Children aged <8 years who are considered high risk and should therefore receive the full 14-day treatment with doxycycline include children who are hospitalized or have severe illness, children with preexisting heart valvulopathy, children who are immunocompromised, or children with delayed Q fever diagnosis who have experienced illness for >14 days without resolution of symptoms. †† Limited data are available on treatment of Q fever during pregnancy. Consultation with an expert in infectious diseases is recommended. Trimethoprim/sulfamethoxazole should be discontinued for the final 8 weeks of pregnancy because of the risk for hyperbilirubinemia. §§ Target serum levels for optimal efficacy during chronic Q fever treatment is ≥5 µg/mL. ¶¶ Take with food or milk. Should not be used by persons with glucose-6-phosphate dehydrogenase deficiency. Monitor for retinal toxicity. Target serum levels for optimal efficacy is 1.0+0.2 µg/mL. The safety of long-term treatment in children has not been evaluated. *** Limited data are available on treatment of chronic Q fever in children. Consultation with an expert in pediatric infectious diseases is recommended. ††† The safety of long-term doxycycline or hydroxychloroquine treatment in pregnant women and fetal risk has not been evaluated. Consultation with an expert in infectious diseases and obstetrics is recommended. §§§ Limited reports of treatment for chronic Q fever unrelated to endocarditis or vascular infection (e.g., osteoarticular infections or chronic hepatitis); duration of treatment is dependent on serologic response. Consultation with expert in infectious diseases is recommended. ¶¶¶ Women should only be treated postpartum if serologic titers remain elevated >12 months after delivery (immunoglobulin G phase I titer ≥1:1024). Women treated during pregnancy for acute Q fever should be monitored similarly to other patients who are at high risk for progression to chronic disease (e.g., serologic monitoring at 3, 6, 12, 18, and 24 months after delivery). **** Reports of treatment studies are rare. Although limited success has occurred with long-term or pulsed tetracycline-class antibiotics, evidence to guide patient management is weak. | |||
Acute and Chronic Q Fever in Pregnant Women
Treatment of pregnant women who received an acute Q fever diagnosis during pregnancy with trimethoprim/sulfamethoxazole throughout pregnancy has been shown to significantly decrease the risk for adverse consequences for the fetus 22. Up to 81% of untreated infected pregnant women might have adverse pregnancy outcomes 22.
Although approximately 40% of pregnant women who receive long-term trimethoprim/sulfamethoxazole treatment might still experience adverse outcomes, complications are more likely to be limited to intrauterine growth retardation and premature delivery instead of stillbirth or miscarriage 22. Long-term trimethoprim/sulfamethoxazole treatment during pregnancy has decreased the risk for conversion to chronic Q fever in the mother and prevented adverse pregnancy events in subsequent pregnancies 22.
Doxycycline is classified as a category D drug because of demonstrated concerns about the effects of tetracyclines on the bone structure and dentitia of the developing fetus (see drug categories for pregnancy at http://chemm.nlm.nih.gov/pregnancycategories.htmExternal Web Site Icon). An effective alternative, trimethoprim/sulfamethoxazole, has been used as a treatment in pregnant women who received an acute Q fever diagnosis, although the drug is classified as a category C drug. The use of trimethoprim/sulfamethoxazole during pregnancy might increase the risk for congenital abnormalities (primarily including urinary tract and cardiovascular abnormalities) because of antifolate effects 38, and concomitant use of folic acid is recommended. Research to assess the potential fetal risk from trimethoprim/sulfamethoxazole during pregnancy has been inconclusive 39.
Because pregnant women with acute Q fever are considered to be at high risk for chronic Q fever infection or recrudescent infections activated during subsequent pregnancies, patients should be monitored after delivery for postpartum progression to chronic disease and during subsequent pregnancies. Although rare, the development of Q fever endocarditis in a pregnant woman presents a difficult clinical dilemma because the safety of the treatment of choice (doxycycline and hydroxychloroquine) has not been evaluated during pregnancy. Health-care providers who are treating chronic Q fever endocarditis during pregnancy should consult with an expert in infectious diseases.
Women who are treated for acute Q fever during pregnancy should be monitored similarly to other patients at high risk for progression to chronic disease (e.g., serologic monitoring at 3, 6, 12, 18, and 24 months after delivery). Women should be advised of potential risks to the fetus should they become pregnant during the monitoring or treatment period. In one study, seven women treated for chronic Q fever with doxycycline and hydroxychloroquine for at least 1 year had normal subsequent pregnancies with no recurrent miscarriages 25. Q fever serologic testing should be resumed for women previously treated during pregnancy who become pregnant again during this 2-year period; reinitiation of long-term trimethoprim/sulfamethoxazole is indicated when IgG titers demonstrate a fourfold rise indicating a recrudescent infection, even if other signs or a definite nidus of infection cannot be identified. In these women, the nidus of infection is assumed to be the reproductive system, and the only clinical sign might be an adverse pregnancy event in a subsequent pregnancy.
Acute and Chronic Q Fever in Children
Doxycycline is the drug of choice for treatment of acute Q fever in children and is recommended for patients aged ≥8 years and for severe infections in children of any age. The pediatric doxycycline dose for treatment of acute Q fever is 2.2 mg/kg twice per day for 2 weeks (maximum 100 mg per dose). The clinical benefit of using doxycycline to treat Q fever in children aged <8 years who meet the criteria for being considered high risk is greater than the potential risk for dental staining. Children aged <8 years who are considered high risk and should therefore receive the full 2-week treatment with doxycycline include children who are hospitalized or have severe illness, children with preexisting heart valvulopathy, children who are immunocompromised, or children with delayed Q fever diagnosis who have experienced illness for >2 weeks without resolution of symptoms.
Although short courses (≤5 days) of doxycycline for the treatment of rickettsial infections such as Rocky Mountain spotted fever have not resulted in significant dental staining in children, the possible long-term dental effects of 2 weeks of doxycycline in children aged <8 years have not been well studied 40. Because acute Q fever is frequently a mild or self-limiting illness with a low risk for death or a poor prognosis, health-care providers should use their clinical judgment to determine whether a 2-week course of doxycycline treatment should be used to treat Q fever infections in children aged <8 years who have a mild or uncomplicated illness. For these patients, health-care providers might consider a 5-day course of doxycycline, which does not cause dental staining. Children with continued mild symptoms after a short course of doxycycline can be treated with 14 days of trimethoprim/sulfamethoxazole.
Limited data are available on treatment of chronic Q fever in children; therefore, consultation with an expert in pediatric infectious diseases is recommended. The safety of long-term hydroxychloroquine treatment in children has not been determined, and evaluation for retinal toxicity might be limited because of difficulties in evaluation of color vision. Alternative long-term treatments that might be considered in children with chronic Q fever include use of a fluoroquinolone (e.g., moxifloxacin or levofloxacin) with rifampin or trimethoprim/sulfamethoxazole with doxycycline.
Chronic Q Fever in Adults
Management of chronic Q fever is evaluated through both serologic and clinical monitoring. Using the same laboratory and testing procedures for serologic monitoring is important because variations among laboratories might give an inaccurate appearance of significant titer decreases or increases.
Patients who are healthy and have no identified risk factor for chronic illness should receive a clinical and serologic evaluation approximately 6 months after diagnosis of acute infection to identify potential progression to chronic disease. Phase I and phase II IgG and IgM antibodies should be measured to endpoint by IFA and compared with previous titers. Patients with a phase I IgG antibody titer ≥1:1024 should be carefully assessed for clinical evidence of progression to chronic Q fever infection. If a patient has no serologic or clinical evidence of progression to chronic infection, serologic monitoring can either be discontinued or continued less frequently if deemed appropriate by the health-care provider. However, patients should be advised to seek medical care immediately should symptoms of chronic Q fever occur at any time throughout their lives.
Patients with cardiovascular risk factors for chronic disease (e.g., heart valve defect, vascular graft, or aneurysm) at the time of acute infection should be serologically monitored and receive a physical examination at intervals of 3, 6, 12, 18, and 24 months. Women infected during pregnancy should be serologically and clinically monitored at the same intervals (3, 6, 12, 18, and 24 months) after delivery. If there is no evidence of an increase in phase I IgG titers ≥1:1024 after 2 years and no evidence of clinical progression to chronic infection, serologic monitoring may be discontinued or continued less frequently if deemed appropriate by the health-care provider. However, patients should be advised to seek medical care immediately should symptoms occur at any time throughout their lives, because those with valvular defects or vascular abnormalities remain at high risk for chronic Q fever for life. In addition, patients who have been infected with acute Q fever and develop valvular disease later in life from any cause are at risk for a recrudescent infection that can result in chronic Q fever endocarditis.
It is not uncommon for patients with an acute Q fever infection to develop serologic profiles of chronic Q fever that eventually regress. Clinical evidence of chronic Q fever must accompany increased phase I IgG antibody titers to confirm a chronic diagnosis, and treatment should not be given based on increased titers alone. In all monitored patients, diagnosis of chronic Q fever is based on a rising or elevated phase I IgG titer (typically ≥1:1024) and an identifiable nidus of infection (e.g., endocarditis, vascular infection, and osteomyelitis). Any symptomatic patient with serologic evidence of chronic Q fever (phase I IgG antibody titer ≥1:1024) should be given a thorough clinical assessment to identify potential organ infection. The phase I IgG antibody titer might be higher than the phase II IgG titer; however, this is not a diagnostic criterion because patients with chronic Q fever might retain extremely high phase II IgG titers that equal or exceed phase I IgG titers 41.
Adults who receive a diagnosis of chronic Q fever should receive a treatment regimen of doxycycline and hydroxychloroquine (100 mg of doxycycline twice daily with 200 mg of hydroxychloroquine three times daily); duration of treatment might vary by the site of infection (Table 3) 7. A combination regimen is necessary to eradicate the organism because hydroxychloroquine raises the pH in the acidified phagosomal compartment and, in combination with doxycycline, has been shown to have in vitro bactericidal activity against C. burnetii. Because of potential retinal toxicity from long-term use of hydroxychloroquine, a baseline ophthalmic examination should be performed before treatment and every 6 months thereafter. Both doxycycline and hydroxychloroquine can cause photohypersensitivity, and hypersensitivity to sunlight is a potential complication with acute and chronic treatment regimens. Hydroxychloroquine is contraindicated in persons with glucose-6-phosphate dehydrogenase deficiency and persons with retinal or visual field deficits.
During treatment for chronic Q fever, patients should receive monthly serologic testing for C. burnetii phase I and II IgG and IgM antibodies and monthly clinical evaluations. If an appropriate treatment response is not achieved, monthly monitoring for hydroxychloroquine plasma levels (which should be maintained at 0.8–1.2 µg/mL) and doxycycline plasma levels (which should be maintained at ≥5 µg/mL) should also be performed during the treatment 42. Treatment should continue for at least 18 months for native valve infections and at least 24 months for prosthetic valve infections 11.
Although treatment of vascular infections, such as infected aneurysms or grafts, is less clearly defined because of the smaller patient group, duration of antibiotic therapy reported in recovered patients is similar (18–24 months) 18. Early surgical intervention improves patient survival and might be necessary to remove an infected graft if the patient does not respond to antibiotic therapy 19. Treatment and management of rarer manifestations of chronic disease (e.g., osteoarticular infections) depends on clinical and serologic response, and consultation with an infectious disease physician is recommended.
The definition of a cured case of chronic fever on the basis of serologic testing previously was defined as phase I IgG ≤1:200, although other researchers have recommended a phase I IgG cutoff of <1:800 to determine treatment duration 43. Because these specific titer dilutions are not available from commercial laboratories in the United States, they are more difficult to interpret in the United States. Rather than rely on indiscriminate application of predetermined cutoff titers, health-care providers should use serologic testing as a tool to ensure that the phase I IgG is decreasing during treatment in conjunction with recovery from clinical symptoms. A patient who has been treated appropriately for ≥18 months and has recovered from clinical symptoms but whose phase I IgG remains ≥1:1024 might not benefit from continued treatment. One study found that a favorable prognostic indicator for treated endocarditis patients who had no progression of clinical disease yet who were not considered cured on the basis of serologic testing was a fourfold decrease in phase I IgG and IgA and the complete disappearance of phase II IgM 11. Twice yearly serologic monitoring of treated patients should continue for a minimum of 5 years after treatment, and lifelong serologic monitoring might be warranted in patients with severe valvular defects 11.
Treatment of chronic Q fever is challenging. Because of the highly variable clinical nature both of acute and chronic Q fever, clinical judgment remains the most crucial factor in the treatment and management.
Summary of Q Fever Treatment and Management
- Because of the delay in seroconversion often necessary to confirm diagnosis, antibiotic treatment should never be withheld pending laboratory tests or discontinued on the basis of a negative acute specimen. In contrast, treatment of chronic Q fever should be initiated only after diagnostic confirmation.
- Treatment for acute or chronic Q fever should only be provided for patients with clinically compatible cases and not based on elevated serologic titers alone.
- Doxycycline is the drug of choice, and 2 weeks of treatment is recommended for adults, children aged ≥8 years, and for severe infections in patients of any age.
- Children aged <8 years with uncomplicated illness may be treated with trimethoprim/sulfamethoxazole or a shorter duration (5 days) of doxycycline.
- Women who are pregnant when acute Q fever is diagnosed should be treated with trimethoprim/sulfamethoxazole throughout the duration of pregnancy.
- Serologic monitoring is recommended after an acute Q fever infection to assess possible progression to chronic infection. The recommended schedule for monitoring is based on the patient’s risk for chronic infection.
- Babudieri B. Q fever: a zoonosis. Adv Vet Sci 1959;5:81.[↩]
- Thompson HDD, Dasch GQ. Fever. In: Goodman J, ed. Tick-borne diseases of humans. Washington, DC: ASM Press; 2005:328–42.[↩]
- Stein A, Raoult D. Pigeon pneumonia in Provence: a bird-borne Q fever outbreak. Clin Infect Dis 1999;29:617–20.[↩]
- Pinsky RL, Fishbein DB, Greene CR, Gensheimer KF. An outbreak of cat-associated Q fever in the United States. J Infect Dis 1991;164:202–4.[↩]
- Coxiella burnetii bacteria.https://phil.cdc.gov/Details.aspx?pid=18158[↩]
- Q Fever Epidemiology and Statistics. https://www.cdc.gov/qfever/stats/[↩][↩]
- Maurin M, Raoult DQ. Fever. Clin Microbiol Rev 1999;12:518–53.[↩][↩][↩]
- Williams JC. Infectivity, virulence, and pathogenicity of Coxiella burnetii for various hosts. In: Williams JC, Thompson HA, eds. Q fever: the biology of Coxiella burnetii. Boca Raton, FL: CRC Press, Inc; 1991:21–72.[↩]
- Fournier PE, Casalta JP, Piquet P, Tournigand P, Branchereau A, Raoult D. Coxiella burnetii infection of aneurysms or vascular grafts: report of seven cases and review. Clin Infect Dis 1998;26:116–21.[↩]
- Diagnosis and Management of Q Fever — United States, 2013: Recommendations from CDC and the Q Fever Working Group. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr6203a1.htm[↩][↩][↩][↩][↩]
- Million M, Thuny F, Richet H, Raoult D. Long-term outcome of Q fever endocarditis: a 26-year personal survey. Lancet Infect Dis 2010;10:527–35.[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Raoult D, Marrie T, Mege J. Natural history and pathophysiology of Q fever. Lancet Infect Dis 2005;5:219–26.[↩]
- Kampschreur LM, Dekker S, Hagenaars JC, et al. Identification of risk factors for chronic Q fever, the Netherlands. Emerg Infect Dis 2012;18:563–70.[↩][↩][↩]
- Fenollar F, Fournier P-E, Carrieri MP, Habib G, Messana T, Raoult D. Risk factors and prevention of Q fever endocarditis. Clin Infect Dis 2001;33:312–6.[↩]
- Raoult D, Million M, Thuny F, Carrieri P. Chronic Q fever detection in the Netherlands. Clin Infect Dis 2011;53:1170–1.[↩]
- Wegdam-Blans MC, Kampschreur LM, Delsing CE, et al. Chronic Q fever: review of the literature and a proposal of new diagnostic criteria. J Infect 2012;64:247–59.[↩][↩]
- Shively BK, Gurule FT, Roldan CA, Leggett JH, Schiller NB. Diagnostic value of transesophageal compared with transthoracic echocardiography in infective endocarditis. J Am Coll Cardiol 1991;18:391–7.[↩]
- Botelho-Nevers E, Fournier PE, Richet H, et al. Coxiella burnetii infection of aortic aneurysms or vascular grafts: report of 30 new cases and evaluation of outcome. Eur J Clin Microbiol Infect Dis 2007;26:635–40.[↩][↩][↩][↩][↩]
- Wegdam-Blans MC, Ter Woorst JF, Klompenhouwer EG, Teijink JA. David procedure during a reoperation for ongoing chronic Q fever infection of an ascending aortic prosthesis. Eur J Cardiothorac Surg 2012;42:e19–20.[↩][↩]
- McQuiston JH. Coxiella burnetii (Q fever). In: Long SS, ed. Principles and practices of pediatric infectious diseases. 3rd ed. Philadelphia, PA: Churchill Livingstone; 2009:885–7.[↩]
- Nourse C, Allworth A, Jones A, et al. Three cases of Q fever osteomyelitis in children and a review of the literature. Clin Infect Dis 2004;39:e61–6.[↩]
- Carcopino X, Raoult D, Bretelle F, Boubli L, Stein A. Managing Q fever during pregnancy: the benefits of long-term cotrimoxazole therapy. Clin Infect Dis 2007;45:548–55.[↩][↩][↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Stein A, Raoult D. Q Fever during pregnancy: a public health problem in southern France. Clin Infect Dis 1998;27:592–6.[↩][↩][↩]
- Ben Amara A, Ghigo E, Le Priol Y, et al. Coxiella burnetii, the agent of Q fever, replicates within trophoblasts and induces a unique transcriptional response. PLoS ONE 2010;5:e15315.[↩]
- Raoult D, Fenollar F, Stein A. Q fever during pregnancy: diagnosis, treatment, and follow-up. Arch Intern Med 2002;162:701–4.[↩][↩]
- Siegel JRE, Jackson M, Chiarello L; Healthcare Infection Control Practices Advisory Committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings; 2007 Available at http://www.cdc.gov/ncidod/dhqp/pdf/isolation2007.pdf[↩]
- Guidelines for Safe Work Practices in Human and Animal Medical Diagnostic Laboratories.https://www.cdc.gov/mmwr/preview/mmwrhtml/su6101a1.htm[↩]
- Richardus JH, Dumas A, Huisman J, Schapp G. Q fever in infancy: a review of 18 cases. Pediatr Infect Dis 1985;4:369–73.[↩]
- Terheggen U, Leggat PA. Clinical manifestations of Q fever in adults and children. Travel Med Infect Dis 2007;5:159–64.[↩][↩]
- Maltezou HC, Kallergi C, Kavazarakis E, Stabouli S, Kafetzis DA. Hemolytic-uremic syndrome associated with Coxiella burnetii infection. Pediatr Infect Dis J 2001;20:811–3.[↩]
- Tissot-Dupont H, Vaillant V, Rey S, Raoult D. Role of sex, age, previous valve lesion, and pregnancy in the clinical expression and outcome of Q fever after a large outbreak. Clin Infect Dis 2007;44:232–7.[↩]
- van der Hoek W, Meekelenkamp JC, Leenders AC, Wijers N, Notermans DW, Hukkelhoven CW. Antibodies against Coxiella burnetii and pregnancy outcome during the 2007–2008 Q fever outbreaks in the Netherlands. BMC Infect Dis 2011;11:44.[↩]
- Carcopino X, Raoult D, Bretelle F, Boubli L, Stein A. Q fever during pregnancy. Ann N Y Acad Sci 2009;1166:79–89.[↩]
- Syrucek L, Sobeslavsky O, Gutvirth I. Isolation of Coxiella burnetii from human placentas. J Hyg Epidemiol Microbiol Immunol 1958;2:29–35.[↩]
- Fenollar F, Thuny F, Xeridat B, Lepidi H, Raoult D. Endocarditis after acute Q fever in patients with previously undiagnosed valvulopathies. Clin Infect Dis 2006;42:818–21.[↩]
- Healy B, Llewelyn M, Westmoreland D, Lloyd G, Brown N. The value of follow-up after acute Q fever infection. J Infect 2006;52:e109–12.[↩]
- Diagnosis and Management of Q Fever — United States, 2013: Recommendations from CDC and the Q Fever Working Group. https://www.cdc.gov/mmwr/pdf/rr/rr6203.pdf[↩]
- Czeizel AE, Rockenbauer M, Sørensen HT, Olsen J. The teratogenic risk of trimethoprim-sulfonamides: a population based case-control study. Reprod Toxicol 2001;15:637–46.[↩]
- Forna F, McConnell M, Kitabire F, et al. Systematic review of the safety of trimethoprim-sulfamethoxazole for prophylaxis in HIV-infected pregnant women: implications for resource-limited settings. AIDS Rev 2006;8:24–36.[↩]
- American Academy of Pediatrics. Rocky Mountain spotted fever. In: Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. Red book 2009: Report of the Committee on Infectious Diseases. 28th ed. Elk Grove, IL: American Academy of Pediatrics; 2009:573–75.[↩]
- Fenollar F, Fournier PE, Raoult D. Molecular detection of Coxiella burnetii in the sera of patients with Q fever endocarditis or vascular infection. J Clin Microbiol 2004;42:4919–24.[↩]
- Rolain JM, Mallet MN, Raoult D. Correlation between serum doxycycline concentrations and serologic evolution in patients with Coxiella burnetii endocarditis. J Infect Dis 2003;188:1322–5.[↩]
- Parker NR, Barralet JH, Bell AM. Q fever. Lancet 2006;367:679–88.[↩]