Contents
What is a rapid strep test
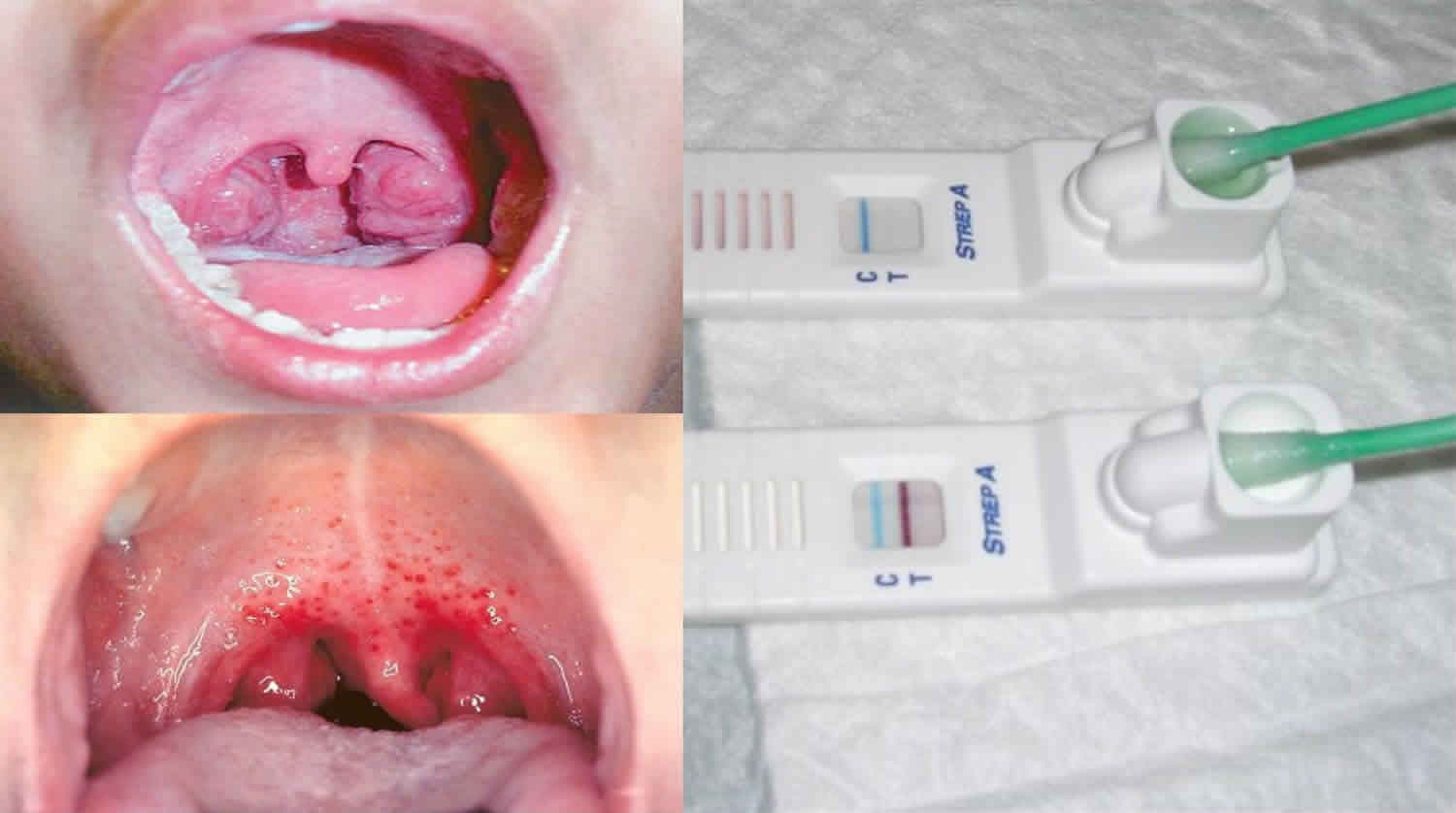
Rapid strep test also called rapid antigen test, is used to detect Group A Streptococcal infection provides important information for the antibiotic decision making for patients presenting with acute pharyngitis. Rapid strep tests should be reserved for patients with reasonable probability of Group A Streptococcal infection and negative results should be confirmed by culture tests in patients younger than 16 years of age, due to their higher risk of acute rheumatic fever 1. A rapid strep test is done in your doctor’s office during your visit. Rapid strep test involves sampling the Streptococcus pyogenes bacteria from the back of your throat and tonsils. Your doctor will insert a long, sterile cotton swab in your mouth and rub the back of your throat and tonsils to collect a bacteria sample. Swabbing is quick and painless. However, the procedure can make you gag. If your child is being swabbed for strep throat, encourage him or her to relax and sit still to make the procedure go smoothly. Most people react with little more than a cough after the procedure. The sample then undergoes rapid testing in the office while you wait for the results. The wait may take 7 to 15 minutes to find out if you test positive or negative for the strep infection. If the rapid strep test is negative for strep bacteria, your doctor will give you tips on how to ease the pain of a sore throat (see treatment). If the rapid strep test results are negative, but all physical signs and symptoms point to an infection, your doctor may send the sample to an outside lab for additional testing. It could take up to two days to get the results 2. If the rapid strep test is positive for the strep infection, your doctor will prescribe an antibiotic to kill the bacteria.
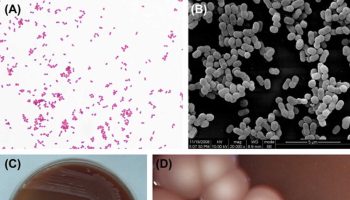
Group A Streptococcus also referred to as Group A beta-hemolytic Streptococcus or Streptococcus pyogenes is a gram positive bacteria which causes a variety of disease conditions and complications 3. These include conditions such as pharyngitis (throat infection) and skin infections, and more serious conditions such as glomerulonephritis, sepsis, rheumatic heart disease, toxic shock syndrome and necrotizing fasciitis 4. Pharyngitis is one of the common conditions that present at the primary health care facilities or emergency departments 5. Pharyngitis arises commonly from viral infection and less commonly from bacterial infection 6. It is estimated that Group A Streptococcus accounts for 20% to 40% of cases of pharyngitis in children and 5% to 15% in adults 6.
Strep throat will worsen if not treated or if you don’t finish all of your antibiotic medicine. Complications from untreated strep throat include kidney inflammation or rheumatic fever (an inflammatory disease that causes pain in the joints, a certain type of rash, or heart valve damage). Other things to consider include:
- If your symptoms don’t improve within 24 to 48 hours after starting your medicine, call your doctor.
- You can continue to spread the infection to others during the first 24 to 48 hours of antibiotic use. Adults and children with strep throat should stay home from work, school, and daycare during that time.
- Replace your or your child’s toothbrush after the first few days of starting antibiotics. The infection can survive on your toothbrush and re-infect you or another family member if toothbrushes are kept together.
- If you or your child has strep throat repeatedly, see your doctor. One of you may be a carrier. A carrier has strep in his or her throat, but shows no signs of illness. Treating the carrier can keep others in your family from getting the infection.
- If your rapid strep test comes back as positive for the infection, it could be a false positive. This type of result occurs more often when you have a fever and other strep throat symptoms.
- A rapid strep test will not find other causes of a sore throat.
Don’t share food, drink, or utensils with someone who has the strep throat infection. That’s good advice for any type of sore throat or cold symptoms.
How long does rapid strep test take?
Rapid strep test may take 5 to 15 minutes to find out if you test positive or negative for the strep infection.
How does a rapid strep test work?
All available rapid strep tests involve the detection of the Lancefield group A carbohydrate, a Group A streptococcus‐specific cell‐wall antigen. Different immunologic techniques are available for carbohydrate detection 7; from older to most recent:
- Enzyme immunoassay (EIA): the sample is placed at the end of a nitrocellulose strip and then migrates to an area where it forms an antigen‐antibody complex. These second‐generation tests are also known as immunochromatographic, sandwich or lateral‐flow assays. They are the most widespread and most used rapid strep tests in clinical practice.
- Optical immunoassay (OIA): the sample is placed on a silicon membrane in the presence of the reagent. The result is based on the change in optical properties of the inert membrane in the presence of an antigen‐antibody complex. These third‐generation tests seem to be more sensitive than enzyme immunoassays (EIAs) but their use is limited because of their high cost.
Alternative tests
Office culture
Another test for the diagnosis of Group A streptococcus in children with pharyngitis is a throat culture performed in the physician’s office (office culture). Office culture has the same disadvantage as a laboratory culture (a 48‐hour delay in obtaining results), with the major limitation being insufficient sensitivity (from 50% to 85%) 8. Office culture is almost completely abandoned and was not considered in this review.
Streptococcal antibody tests
Assessment of Group A streptococcus‐specific antibodies is the traditional reference test to differentiate true Group A streptococcus infection and Group A streptococcus carriage. The most commonly used Group A streptococcus‐specific antibody assays tests are for anti‐streptolysin O and anti‐DNase B antibodies. Increased antibody titre assessment diagnoses true Group A streptococcus infection better than a single absolute titer assessment 9. Streptococcal antibody tests are not used for the diagnosis of Group A streptococcus in children with pharyngitis because of the need for repeat blood samples. Moreover, the information about the kinetics of the immune response to Group A streptococcus in children with pharyngitis is very limited and the most recent data show that the interpretation of streptococcal antibody test results is not straightforward 9. Therefore, their use is usually limited to documenting recent Group A streptococcus infection in patients suspected of having Group A streptococcus non‐suppurative complications or to epidemiologic studies 9.
Clinical scoring systems
Clinical scoring systems have been developed to diagnose Group A streptococcus on clinical grounds. The most popular of these scores are the Centor score 10 and the McIsaac score 11. The scores are based on assessing simple clinical criteria (history of fever, cough, tonsillar swelling or exudate, tender cervical adenopathy and age). Their use is recommended in adults but might be inappropriate in children; several authors have reported a lack of diagnostic accuracy in this population 12.
Rapid molecular biology assays
Rapid molecular biology assays for Group A streptococcus in children with pharyngitis have been recently developed (Group A Streptococcus Direct Test; GenProbe Inc., San Diego, CA; and LightCycler Strep‐A assay; Roche Applied Science, Indianapolis, IN) 13. These techniques, based on DNA‐rRNA hybridisation or polymerase chain reaction (PCR), are highly sensitive but are not currently used widely because of their cost, the need for highly specialised equipment and personnel, and the two‐hour delay in results 7.
Rapid strep test accuracy
In studies in which all participants underwent both rapid strep test and throat culture (105 test evaluations; 58,244 participants; median prevalence of participants with Group A streptococcus was 29.5%), rapid strep test had a summary sensitivity of 85.6% and a summary specificity of 95.4% 14. From systematic reviews and observational studies the sensitivity values ranged between 82% and 100% for molecular assays and between 55% and 94% for immunoassays 15. Specificities for the two test types were 91% to 99% for molecular assays and 81% to 100% for immunoassays 15. There was substantial heterogeneity in sensitivity across studies; specificity was more stable. There was no evidence of a trade‐off between sensitivity and specificity. Heterogeneity in accuracy was not explained by study‐level characteristics such as whether an enrichment broth was used before plating, mean age and clinical severity of participants, and Group A streptococcus prevalence. The sensitivity of rapid strep test – enzyme immunoassays (EIA) and optical immunoassays (OIA) tests was comparable (summary sensitivity 85.4% versus 86.2%) 14. Sensitivity analyses showed that summary estimates of sensitivity and specificity were stable in low risk of bias studies 14.
In a population of 1000 children with a Group A streptococcus prevalence of 30%, 43 patients with Group A streptococcus will be missed. Whether or not rapid strep test can be used as a stand‐alone test to rule out Group A streptococcus will depend mainly on the epidemiological context 14. The sensitivity of rapid strep test – enzyme immunoassays (EIA) and optical immunoassays (OIA) tests seems comparable. Rapid strep test specificity is sufficiently high to ensure against unnecessary use of antibiotics. Based on these results, you would expect that amongst 100 children with strep throat, 86 would be correctly detected with the rapid test while 14 would be missed and not receive antibiotic treatment 14. Of 100 children with non‐streptococcal sore throat, 95 would be correctly classified as such with the rapid test while 5 would be misdiagnosed as having strep throat and receive unnecessary antibiotics.
Rapid strep test sensitivity
Rapid strep test had a summary sensitivity of 85.6% 14. The high specificity of rapid antigen detection tests implies that positive results may not require throat culture confirmation and could be used as a basis to prescribe antibiotics in children with pharyngitis.
Rapid strep test false positive
Interpretation considering a cohort of 1000 participants and the rapid strep test to have sensitivity 85.6% and specificity 95.8%, assuming various prevalence rates of Group A Streptococcal infection cases 15.
Prevalence: 20%
Consequence in a cohort of 1000 participants:
- Of the 200 participants with positive culture test for Group A Streptococcal infection, 171 will be identified (true positive) and 29 will be missed (false negative).
- Of the 800 participants without G A Strep, 763 will be not be treated (true negative) and 37 may receive unnecessary treatment with antibiotic (false positive).
Prevalence: 30%
Consequence in a cohort of 1000 participants:
- Of the 300 participants with positive culture test for Group A Streptococcal infection, 257 will be identified (true positive) and 43 will be missed (false negative).
- Of the 700 participants without Group A Streptococcal infection, 668 will be not be treated (true negative) and 32 may receive unnecessary treatment with antibiotic (false positive).
Prevalence: 40%
Consequence in a cohort of 1000 participants:
- Of the 400 participants with positive culture test for Group A Streptococcal infection, 342 will be identified (true positive) and 58 will be missed (false negative).
- Of the 600 participants without Group A Streptococcal infection, 572 will be not be treated (true negative) and 28 may receive unnecessary treatment with antibiotic (false positive).
Rapid strep test false negative
Interpretation considering a cohort of 1000 participants and the rapid strep test to have sensitivity 85.6% and specificity 95.8%, assuming various prevalence rates of Group A Streptococcal infection cases 15.
Prevalence: 20%
Consequence in a cohort of 1000 participants:
- Of the 200 participants with positive culture test for Group A Streptococcal infection, 171 will be identified (true positive) and 29 will be missed (false negative).
- Of the 800 participants without G A Strep, 763 will be not be treated (true negative) and 37 may receive unnecessary treatment with antibiotic (false positive).
Prevalence: 30%
Consequence in a cohort of 1000 participants:
- Of the 300 participants with positive culture test for Group A Streptococcal infection, 257 will be identified (true positive) and 43 will be missed (false negative).
- Of the 700 participants without Group A Streptococcal infection, 668 will be not be treated (true negative) and 32 may receive unnecessary treatment with antibiotic (false positive).
Prevalence: 40%
Consequence in a cohort of 1000 participants:
- Of the 400 participants with positive culture test for Group A Streptococcal infection, 342 will be identified (true positive) and 58 will be missed (false negative).
- Of the 600 participants without Group A Streptococcal infection, 572 will be not be treated (true negative) and 28 may receive unnecessary treatment with antibiotic (false positive).
- Banerjee S, Ford C. Clinical Decision Rules and Strategies for the Diagnosis of Group A Streptococcal Infection: A Review of Clinical Utility and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2018 May 23. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532209[↩]
- Lean WL, Arnup S, Danchin M, Steer AC. Rapid diagnostic tests for group A streptococcal pharyngitis: A meta-analysis. Pediatrics [Internet]. 2014 Oct;134(4):771–81 http://pediatrics.aappublications.org/content/134/4/771.long[↩]
- Group A Streptococcal (GAS) Infections. https://emedicine.medscape.com/article/228936-overview[↩]
- Abraham T, Sistla S. Identification of Streptococcus pyogenes – Phenotypic Tests vs Molecular Assay (spy1258PCR): A Comparative Study. J Clin Diagn Res. 2016;10(7):DC01–DC3. doi:10.7860/JCDR/2016/20053.8093 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5020175[↩]
- Lean WL, Arnup S, Danchin M, Steer AC. Rapid diagnostic tests for group A streptococcal pharyngitis: A meta-analysis. Pediatrics [Internet]. 2014 Oct;134(4):771–81 https://pediatrics.aappublications.org/content/134/4/771.long[↩]
- Cohen JF, Bertille N, Cohen R, Chalumeau M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database Syst Rev. 2016 Jul 4;7:CD010502[↩][↩]
- Gerber MA, Shulman ST. Rapid diagnosis of pharyngitis caused by group A streptococci. Clinical Microbiology Reviews 2004;17(3):571‐80.[↩][↩]
- Tanz RR, Shulman ST. Chronic pharyngeal carriage of group A streptococci. Pediatric Infectious Disease Journal 2007;26(2):175‐6.[↩]
- Johnson DR, Kurlan R, Leckman J, Kaplan EL. The human immune response to streptococcal extracellular antigens: clinical, diagnostic, and potential pathogenetic implications. Clinical Infectious Diseases 2010;50(4):481‐90.[↩][↩][↩]
- Centor RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Medical Decision Making 1981;1(3):239‐46.[↩]
- McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. Canadian Medical Association Journal 1998;158(1):75‐83.[↩]
- Cohen JF, Cohen R, Levy C, Thollot F, Benani M, Bidet P, et al. Selective testing strategies for diagnosing group A streptococcal infection in children with pharyngitis: a systematic review and prospective multicentre external validation study. CMAJ 2015;187(1):23‐32.[↩]
- Uhl JR, Adamson SC, Vetter EA, Schleck CD, Harmsen WS, Iverson LK. Comparison of LightCycler PCR, rapid antigen immunoassay, and culture for detection of group A streptococci from throat swabs. Journal of Clinical Microbiology 2003;41:242‐9.[↩]
- Cohen JF, Bertille N, Cohen R, Chalumeau M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database of Systematic Reviews 2016, Issue 7. Art. No.: CD010502. DOI: 10.1002/14651858.CD010502.pub2 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010502.pub2/full[↩][↩][↩][↩][↩][↩]
- Rapid Tests for the Diagnosis of Group A Streptococcal Infection: A Review of Diagnostic Test Accuracy, Clinical Utility, Safety, and Cost-Effectiveness. https://www.cadth.ca/sites/default/files/pdf/htis/2018/RD0046-Group%20A%20Strep%20Rapid%20Tests%20Final.pdf[↩][↩][↩][↩]