Contents
- What is rectal prolapse
- Rectal prolapse causes
- Rectal prolapse symptoms and signs
- Diagnosis of rectal prolapse
- Rectal prolapse vs Hemorrhoids
- Rectal prolapse treatment
- Transabdominal surgery for rectal prolapse
- Anterior rectopexy (Ripstein procedure)
- Posterior sling rectopexy (Wells procedure)
- Anterior resection without fixation
- Resection with sacral fixation
- Suture Rectopexy
- Laparoscopy surgery
- Perineal procedures
- Altemeier operation (perineal proctosigmoidectomy)
- Delorme Procedure
What is rectal prolapse
Rectal prolapse or procidentia occurs when the rectum falls and comes through the anal opening 1.
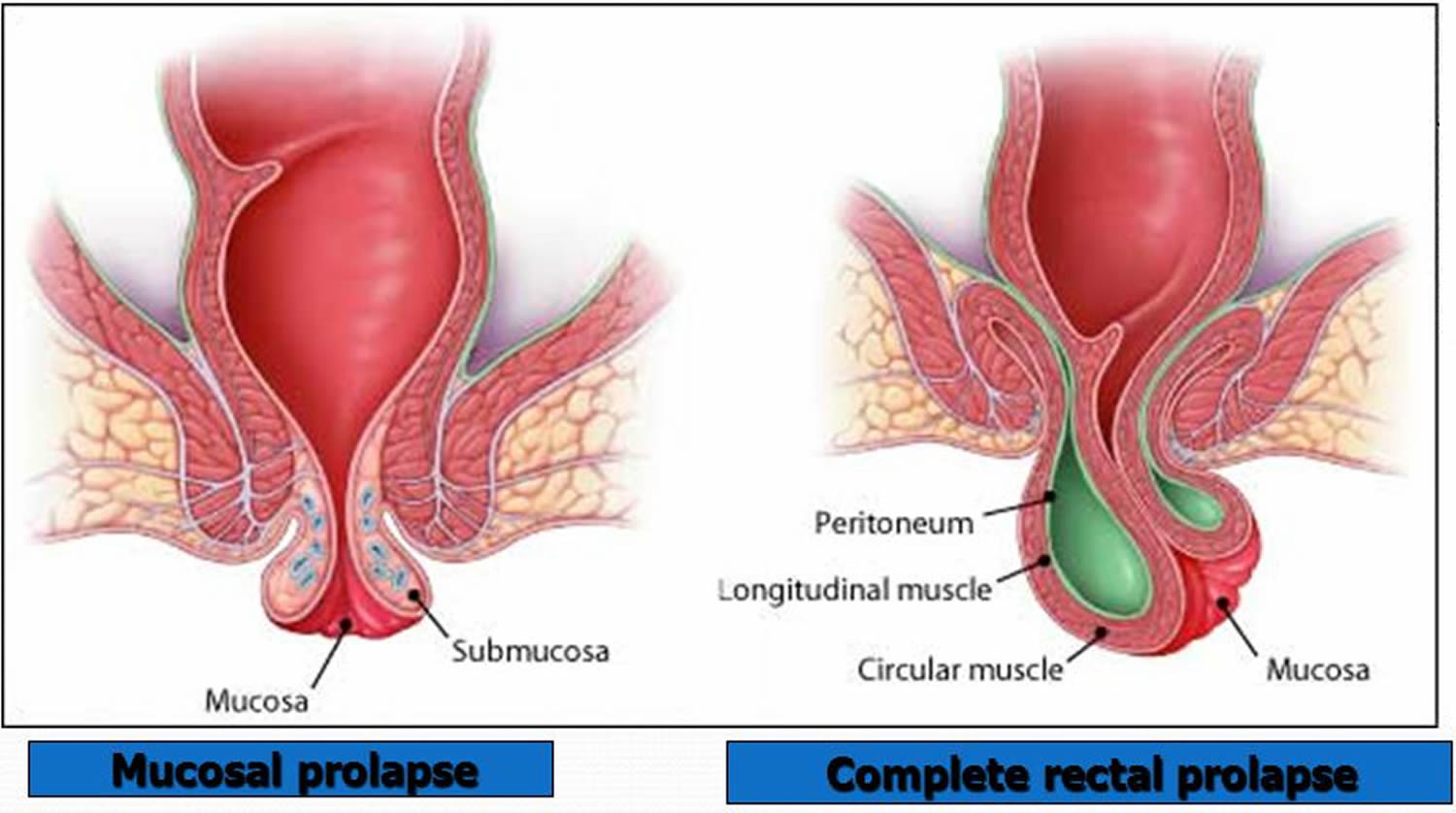
Rectal prolapse is a full thickness, circumferential intussusception (intussusception is the sliding of one part of the intestine into another) of the entire rectal wall through the anal canal resulting in part of the rectum remaining intermittently or occasionally permanently distal to the anus 2. The latter condition is known as third degree prolapse and the former state as second degree. Rectal prolapse is a relatively uncommon clinical entity and the primary cause of rectal prolapse is unclear 3.
- Rectal prolapse occurs most often in children under age 6 and in the elderly 4.
- In children, it can be found with cystic fibrosis and whipworm (trichuriasis) 4.
- In adults, it is usually found with constipation. It is also more common in people with autism, psychiatric disorders, and intellectual disability 4.
- Rectal prolapse is relatively uncommon in men; moreover they usually present when they are less than 50 years of age.
- Most patients are women > 60 years old 5.
- Rectal prolapse can sometimes be treated with stool softeners, suppositories and other medications. But surgery is usually needed to treat rectal prolapse.
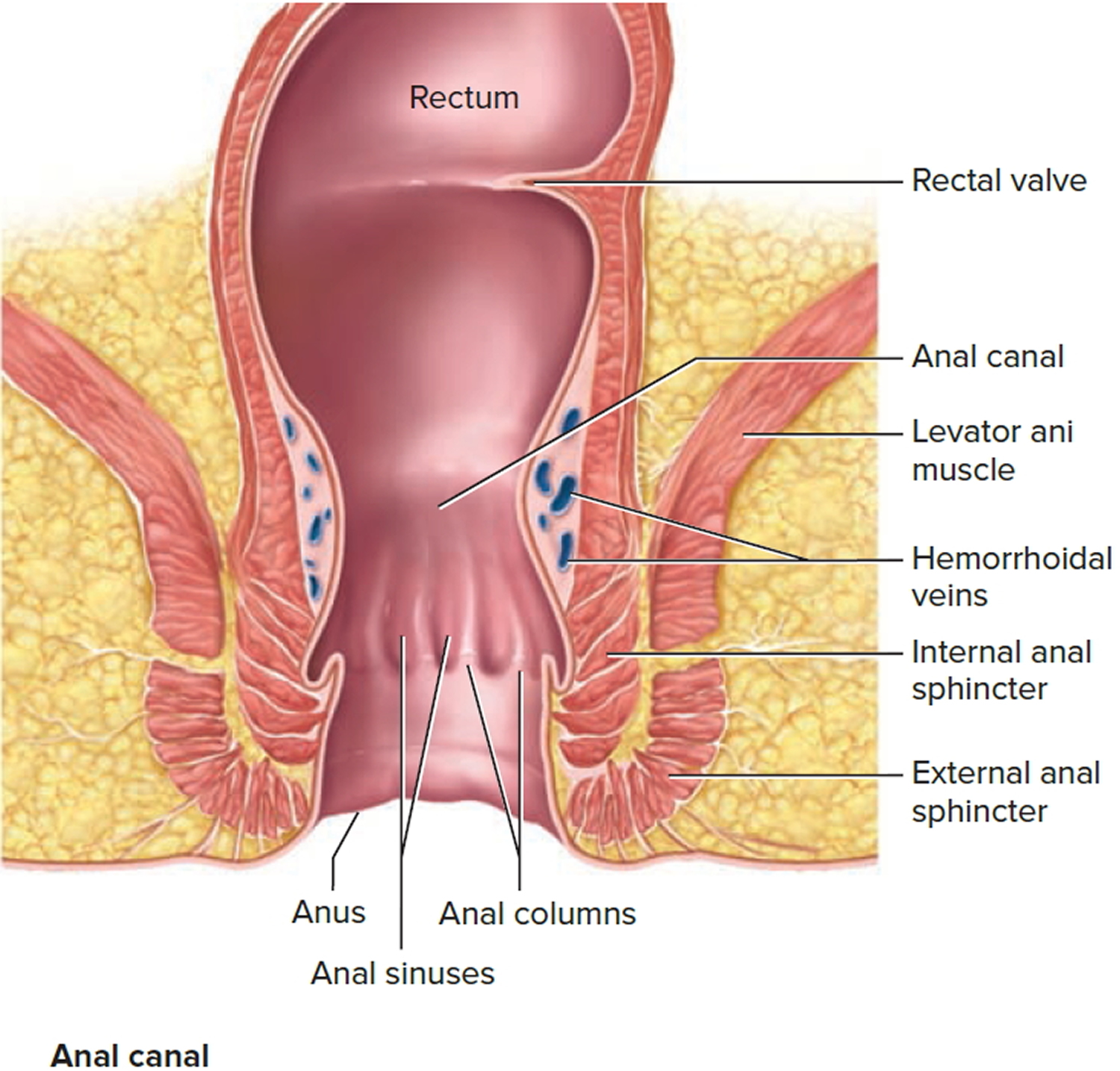
Figure 1. Rectum anatomy and Anus (anal canal)
Figure 2. Rectal prolapse
Rectal prolapse causes
Rectal prolapse is caused by either:
- Congenital (present at birth),
- Acquired.
At the beginning of the 20th century Moschcowitz 6 described the anatomical basis for a rectal prolapse as a deficient pelvic floor through which the rectum herniates. This theory was that a redundant sigmoid colon lying within the deep pelvic sac, together with the resulting acute rectosigmoid junction, caused the patient to strain excessively to evacuate. Thus, the hypothesis continued, the eventual prolapse was the result of herniation through the weakened pelvic floor.
A latter concept suggested that rectal prolapse was actually a circumferential 2° or 3° intussusception 7. Complete circumferential intussusception usually starts 6–8 cm from the anal verge but can continue through the anal canal 8.
Predisposing and associated anatomical and functional factors:
Anatomical factors include:
- female sex,
- redundant rectosigmoid,
- deep pouch of Douglas,
- patulous anus (weak internal sphincter),
- diastasis of levator ani muscle (defects in pelvic floor),
- lack of fixation of rectum to sacrum.
Functional factors include:
- poor bowel habits (chronic constipation),
- neurologic disease including congenital anomaly,
- cauda equina lesion, spinal cord injury, and
- senility.
The majority of patients are women 9 and peak occurrence is in the sixth decade of life.
Rectal prolapse symptoms and signs
The most prominent symptom of rectal prolapse and procidentia is protrusion 5. It may only occur while straining or while walking or standing 5. Rectal bleeding can occur, and incontinence is frequent 5. Pain is uncommon unless incarceration or significant prolapse occurs.
Diagnosis of rectal prolapse
The patient will usually present with a protrusion (75%), and in about 70% of cases, coexisting fecal incontinence; almost 50% of patients have a history of constipation 9. The incontinence becomes more severe as the protrusion increases in degree. Dilatation of the canal by the mass results in further relaxation of the sphincter muscles and increased prolapse 10. Bleeding per rectum, discharge of mucus, or both, are common additional complaints. When an individual’s symptoms are suggestive of rectal prolapse, having the patient sit on the toilet and bear down to feign evacuation is often the only means by which the rectal prolapse can be visualized.
It is important to evaluate the tone and contractility of the sphincter mechanism. If sphincter tone is poor or if the anus is patulous, functional results after repair may be suboptimal. Alternatively, if the patient has relatively good sphincter tone and contractility, good bowel control can be ultimately anticipated. As occasionally a polyp or carcinoma of the rectum or sigmoid colon may be the “lead point” for an intussusception, an endoscopic examination should be performed. However ultimately, radiologic study of the rectum by means of defecography is most effective for identifying internal intussusception and other defecatory disorders.
Rectal prolapse vs Hemorrhoids
Hemorrhoids
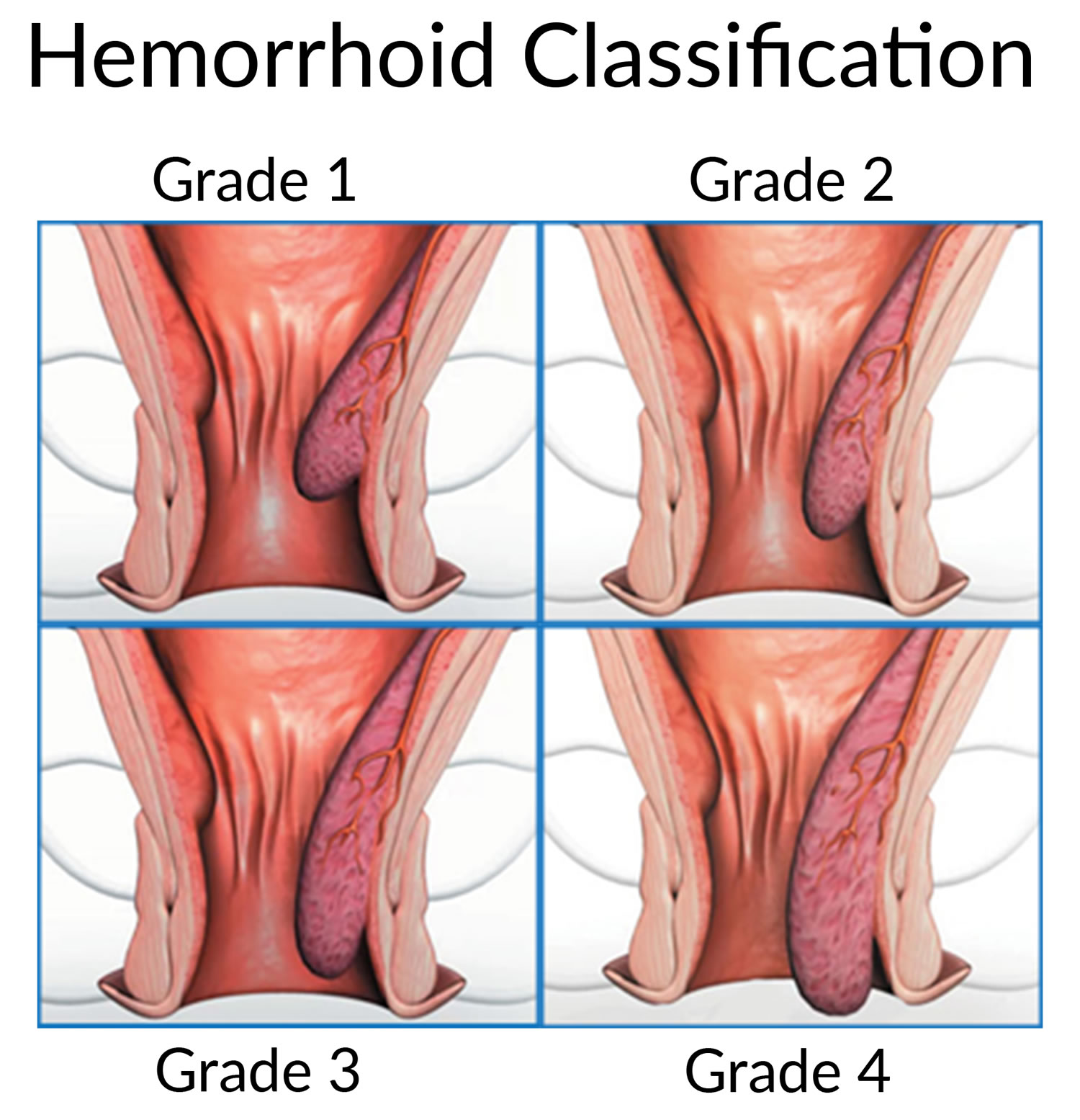
Hemorrhoids, also called piles, are swollen and inflamed veins around your anus or in your lower rectum 11.
Hemorrhoids are the most common cause of minor rectal bleeding, and are typically not associated with pain.
To tell the difference between rectal prolapse or a hemorrhoid is that a protruding mass of hemorrhoidal tissue tends to be lobular as compared to the circular lining in rectal prolapse. Specifically the folds between the mucosal layers in hemorrhoidal prolapse are radial whereas in rectal prolapse they are circumferential. It is important to distinguish full thickness prolapse from mucosal prolapse because treatment of the two conditions is very different.
Hemorrhoids are very common in both men and women and affect about 1 in 20 Americans 12. About half of adults older than age 50 have hemorrhoids 13.
The most common symptom of hemorrhoids inside the anus is bright red blood covering the stool, on toilet paper or in the toilet bowl 12. Symptoms usually go away within a few days 12.
- However, if you have rectal bleeding you should see a doctor. You need to make sure bleeding is not from a more serious condition such as colorectal or anal cancer.
The two types of hemorrhoids are 11:
- External hemorrhoids, which form under the skin around the anus.
- Internal hemorrhoids, which form in the lining of the anus and lower rectum.
The exact cause of bleeding from hemorrhoids is not known, but it often seems to be related to constipation, diarrhea, sitting or standing for long periods, obesity heavy lifting and pregnancy.
Figure 3. Hemorrhoids
You are more likely to get hemorrhoids if you:
- strain during bowel movements
- sit on the toilet for long periods of time
- have chronic constipation or diarrhea
- eat foods that are low in fiber
- are older than age 50
- are pregnant
- often lift heavy objects
Complications of hemorrhoids can include the following:
- blood clots in an external hemorrhoid
- skin tags—extra skin left behind when a blood clot in an external hemorrhoid dissolves
- infection of a sore on an external hemorrhoid
- strangulated hemorrhoid—when the muscles around your anus cut off the blood supply to an internal hemorrhoid that has fallen through your anal opening
- anemia
How are hemorrhoids treated ?
Medical treatment of hemorrhoids includes treatment of any underlying constipation, taking warm baths and applying an over-the-counter cream or suppository that may contain hydrocortisone. If medical treatment fails there are a number of ways to reduce the size or eliminate internal hemorrhoids. Each method varies in its success rate, risks and recovery time. Your doctor will discuss these options with you. Rubber band ligation is the most common outpatient procedure for hemorrhoids in the United States. It involves placing rubber bands around the base of an internal hemorrhoid to cut off its blood supply. This causes the hemorrhoid to shrink, and in a few days both the hemorrhoid and the rubber band fall off during a bowel movement. Possible complications include pain, bleeding and infection. After band ligation, your doctor may prescribe medications, including pain medication and stool softeners, before sending you home. Contact your doctor immediately if you notice severe pain, fever or significant rectal bleeding. Laser or infrared coagulation and sclerotherapy (injection of medicine directly into the hemorrhoids) are also officebased treatment procedures, although they are less common. Surgery to remove hemorrhoids may be required in severe cases or if symptoms persist despite rubber band ligation, coagulation or sclerotherapy.
Rectal prolapse treatment
Management of rectal prolapse is surgical; over 100 different procedures have been described 2. The existence of so many surgical options is attestation to the lack of uniform success associated with any one single procedure 2. Since no procedure is a panacea, the operation selected should be matched to the physiologic condition of the patient.
Transabdominal surgery for rectal prolapse
Transabdominal repairs involve rectal fixation, rectal resection or a combination of resection and fixation 2. Attachment of the rectum to the sacrum can be performed using foreign material or sutures although the lateral rectal attachments can be achieved to the sacral periosteum without foreign material.
The primary advantages of a transabdominal procedure are the lower recurrence rates and the associated improvements in incontinence as well as the preservation of a rectal reservoir. Disadvantages are that they are a more invasive procedures and do have an associated risk of postoperative sexual dysfunction in males 2.
Anterior rectopexy (Ripstein procedure)
The rectum is completely mobilized posteriorly 2. A loose sung of mesh is wrapped around the anterior wall of the rectum and sutured to the sacrum.
Results: Recurrence varies form 0 to 10% 14, 15. Sling complications are noted in as many as 16.5% of patients with a 4% reoperation rate.
Posterior sling rectopexy (Wells procedure)
After posterior rectal mobilization and fixation of a mesh to the sacral hollow, the mesh is wrapped around the lateral aspects while the anterior rectal wall is left free to prevent stricture.
Results: Recurrence rates for anterior and posterior rectopexy are similar. However the rate of stricture and therefore postoperative constipation may be lower after posterior than after anterior rectopexy.
Anterior resection without fixation
After anterior resection the rectum becomes secondarily scarred and therefore adherent to the sacrum.
Advantages: removal of the redundant colon may prevent volvulus and torsion and may ameliorate some bowel complaints, especially constipation.
Disadvantages: Risk for anastomotic leak.
Results: Recurrence rate 9% 16. Deterioration of continence has been reported in 10–20% of patients 17.
Resection with sacral fixation
Fixation of the distal rectal segment to the sacrum with redundant sigmoid extirpation.
Results: Initial reports stated recurrence rates of 2–9% 18, 19, 20. Bowel control is more likely to be improved when compared to other methods. The procedure is comparable to rectopexy with respect to operative morbidity but postoperative constipation is less likely 21. Division of the lateral ligaments decrease recurrence rates but increase the incidence of postoperative constipation.
Suture Rectopexy
Perhaps the simplest abdominal approach is rectopexy. The rectum is mobilized distally down to the levator ani muscles. The mesentery of the rectum and the muscularis are secured to the sacral fascia or bone.
Results: Recurrence rates are reported in 2–5% 22, 23. However a redundant sigmoid colon may at least theoretically cause the onset of or exacerbate preexisting constipation.
Laparoscopy surgery
Sutured rectopexy, mesh rectopexy, and anterior resection or resection rectopexy are all technically feasible laparoscopic approaches. So far controlled trials have not been performed and long-term recurrence data are not yet available. Small series suggest that morbidity and short term recurrence rates are similar to these reported by laparotomy.
Perineal procedures
Perineal procedures are associated with a higher recurrence rate than abdominal procedures. In addition postoperative incontinence may be exacerbated 24. However the benefits are related to avoiding a laparotomy and include a very low morbidity and negligible disability. These operations can be done under general, regional or occasionally local anesthesia.
Altemeier operation (perineal proctosigmoidectomy)
Perineal resection of the full thickness of the prolapsed segment with coloanal anastomosis.
Results: Recurrence rates can reach up to 50%. Additional plication of the levator ani muscles seems to be associated with a lower incidence of recurrence and better functional outcome 25, 26. The addition of a colonic J pouch has been attempted but no results have been reported to date.
Delorme Procedure
Unlike the perineal rectosigmoidectomy the dissection is within the submucosal layer. The mucosa and the submucosa are excised and the denuded muscularis is longitudinally pleated prior to effecting the anastomosis.
Results: Recurrence varies from 7 to 22% 27, 28.
Summary of rectal prolapse surgery
Surgical approaches to rectal prolapse will continue to be controversial unless a convincing control led trial demonstrates superiority of a single technique 2.
The treatment of choice is an abdominal procedure (preferably resection rectopexy) due to the fact that the recurrence rates are lower and continence is more likely to be restored than after other operations. Although perineal operations may have higher recurrence rates they are also much less invasive. These latter surgeries are well chosen for the elderly patients with comorbidities in whom an abdominal approach carries a prohibitively high operative risk. One must match the operation to the patient, balancing morbidity, function and recurrence.
- Rectal prolapse. Medline Plus. https://medlineplus.gov/ency/article/001132.htm[↩]
- Hamel CT, Wexner SD. Rectal prolapse. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001. Available from: https://www.ncbi.nlm.nih.gov/books/NBK6929/[↩][↩][↩][↩][↩][↩][↩]
- Boutsis C., Ellis H. The Ivalon-sponge wrap operation for rectal prolapse: An experience with 26 patients. Dis Colon Rectum. 1974;17:21–37. https://www.ncbi.nlm.nih.gov/pubmed/4589828[↩]
- Rectal prolapse. Medline Plus. https://wwwqa.nlm.nih.gov/medlineplus/275/ency/article/001132.htm[↩][↩][↩]
- Rectal Prolapse and Procidentia. Merck Manual. http://www.merckmanuals.com/professional/gastrointestinal-disorders/anorectal-disorders/rectal-prolapse-and-procidentia[↩][↩][↩][↩]
- Moschcowitz A V. The pathogenesis , anatomy and cure of prolapse of the rectum. Surg Gynecol Obstet. (1912);15:7–12.[↩]
- Monro A (1811) The morbid anatomy of the human gullet, stomach, and intestines. Archibald Constable & Co, Edinburgh: p 363.[↩]
- Broden G, Dolk A, Holmstrom B. Recovery of the internal anal sphincter following rectopexy: a possible explanation for continence improvement. Int J Colorectal Dis. (1988);3(1):23–28. https://www.ncbi.nlm.nih.gov/pubmed/3361220[↩]
- Jurgeleit H C, Corman M L, Coller J A, Veidenheimer M C. Symposium: Procidentia of the rectum: teflon sling repair of rectal prolapse, Lahey Clinic experience. Dis Colon Rectum. (1975);18(6):464–467. https://www.ncbi.nlm.nih.gov/pubmed/1181148[↩][↩]
- Schuster M M. The riddle of the sphincters. Gastroenterology. (1975);69(1):249–262. https://www.ncbi.nlm.nih.gov/pubmed/1097292[↩]
- Definition & Facts of Hemorrhoids. The National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/definition-facts[↩][↩]
- Hemorrhoids. Medline Plus. https://medlineplus.gov/hemorrhoids.html[↩][↩][↩]
- Fox A, Tietze PH, Ramakrishnan K. Anorectal conditions: hemorrhoids. FP Essentials. 2014;419:11–19.[↩]
- Morgan C N, Porter N H, Klugman D J. Ivalon (polyvinyl alcohol) sponge in the repair of complete rectal prolapse. Br J Surg. (1972);59(11):841–846. https://www.ncbi.nlm.nih.gov/pubmed/4637084[↩]
- Gordon P H, Hoexter B. Complications of the Ripstein procedure. Dis Colon Rectum. (1978);21(4):277–280. https://www.ncbi.nlm.nih.gov/pubmed/657938[↩]
- Schlinkert R T, Beart R W Jr, Wolff B G, Pemberton J H. Anterior resection for complete rectal prolapse. Dis Colon Rectum 1985. (1985);28(6):409–412. https://www.ncbi.nlm.nih.gov/pubmed/4006636[↩]
- Cirocco W C, Brown A C. Anterior resection for the treatment of rectal prolapse: a 20-year experience. Am Surg. (1993);59(4):265–269. https://www.ncbi.nlm.nih.gov/pubmed/8489090[↩]
- Watts J D, Rothenberger D A, Buls J G. The management of procidentia: 30 years of experience. Dis Colon Rectum. (1985);28:96. https://www.ncbi.nlm.nih.gov/pubmed/3971814[↩]
- Madoff R D, Williams J G, Wong W D, Rothenberger D A, Goldberg S M. Long-term functional results of colon resection and rectopexy for overt rectal prolapse. Am J Gastroenterol. (1992);87(1):101–104. https://www.ncbi.nlm.nih.gov/pubmed/1728105[↩]
- Husa A, Sainio P, von Smitten K. Abdominal rectopexy and sigmoid resection (Frykman-Goldberg Operation) for rectal prolapse. Acta Chir Scand. (1988);154(3):221–224. https://www.ncbi.nlm.nih.gov/pubmed/3376679[↩]
- Sayfan J, Pinho M, Alexander-Williams J, Keighley M R. Sutured posterior abdominal rectopexy with sigmoidectomy compared with Marlex rectopexy for rectal prolapse. Br J Surg. (1990);77(2):143–145. https://www.ncbi.nlm.nih.gov/pubmed/2317672[↩]
- Blatchford G J, Perry R E, Thorson A G, Christensen M A. Rectopexy without resection for rectal prolapse. Am J Surg. (1989);158(6):574–576. https://www.ncbi.nlm.nih.gov/pubmed/2589593[↩]
- Ejerblad S, Krause U. Repair of rectal prolapse by rectosacral suture fixation. Acta Chir Scand. (1954);154(2):103–105. https://www.ncbi.nlm.nih.gov/pubmed/3281400[↩]
- Bartolo D C. Rectal prolapse. Br J Surg. (1996);83(1):3–5. https://www.ncbi.nlm.nih.gov/pubmed/8653355[↩]
- Ramanujam P S, Venkatesh K S, Fietz M J. Perineal excision of rectal procidentia in elderly high-risk patients. A ten-year experience. Dis Colon Rectum. (1994);37(10):1027–1030. https://www.ncbi.nlm.nih.gov/pubmed/7924710[↩]
- Agachan F, Pfeifer J, Joo J S, Nogueras J J, Weiss E G, Wexner S D. Results of perineal procedures for the treatment of rectal prolapse. Am Surg. (1997);63(1):9–12. https://www.ncbi.nlm.nih.gov/pubmed/8985063[↩]
- Lechaux J P, Lechaux D, Perez M. Results of Delorme’s procedure for rectal prolapse. Advantages of a modified technique. Dis Colon Rectum. (1995);38(3):301–307. https://www.ncbi.nlm.nih.gov/pubmed/7882798[↩]
- Senapati A, Nicholls R J, Thomson J P, Phillips R K. Results of Delorme’s procedure for rectal prolapse. Dis Colon Rectum. (1994);37(5):456–460. https://www.ncbi.nlm.nih.gov/pubmed/8181407[↩]