Contents
What is restless leg syndrome (rls)
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, is a a neurological sensorimotor disease in which you have an uncontrollable urge to move your legs, usually due to leg discomfort 1. Restless legs syndrome typically happens in the evenings or nights while you’re sitting or lying down. Moving eases the unpleasant feeling temporarily.
Restless legs syndrome (RLS) can also cause an unpleasant crawling or creeping sensation in the feet, calves and thighs 2. The sensation is often worse in the evening or at night. Occasionally, the arms are affected too.
Restless legs syndrome, can begin at any age and generally worsens as you age. It can disrupt sleep — leading to daytime drowsiness — and make traveling difficult. The clinical course of RLS is generally chronic and often progressive.
Primary Features of RLS
- An urge to move, usually due to uncomfortable sensations that occur primarily in the legs
- The urge to move or unpleasant sensations are partially or totally relieved by movement
- The urge to move or unpleasant sensations increase or worsen during rest or inactivity
- Variability over the course of the day-night cycle, with symptoms worse in the evening and early in the night
- Your symptoms are not solely accounted for by another condition such as leg cramps, positional discomfort, leg swelling or arthritis. RLS often causes difficulty in falling or staying asleep, one of the chief complaints of the disease. Many people who have RLS also have periodic limb movements (PLMs) – jerking of the arms or legs that is often associated with sleep disruption.
Associated Features of RLS
- Periodic limb movements in sleep
- Sleep disturbance especially difficulty in sleep initiation
- Dyskinesias (rhythmic contractions of large muscle groups, often described as a rolling or writhing motion) while awake that occur almost exclusively at rest
- Positive family history
- Exclusion of potential underlying causes of restless leg syndrome
- Onset at any age with typically chronic and progressive course and occasional remissions
Some people with restless legs syndrome never seek medical attention because they worry they won’t be taken seriously. Some doctors wrongly attribute symptoms to nervousness, stress, insomnia or muscle cramps.
A chief complaint among people who have restless leg syndrome is difficulty in falling or staying asleep. Many individuals also have periodic limb movements in sleep. These movements occur every 20–30 seconds, on and off, throughout the night, causing partial awakenings that disrupt sleep. Sleep deprivation can seriously impact work, relationships, and health.
The symptoms of RLS cause significant distress or impairment in social, occupational, educational or other important areas of functioning by the impact on sleep, energy/vitality, daily activities, behavior, cognition or mood — due to the sleep disruption that they cause and the inability to keep still which causes difficulties in working, travelling and social activities.
But RLS or Willis-Ekbom disease has received attention and focus from the media and medical community in recent years, making more people aware of the condition. Up to 7-8% of the population has this neurological condition with 2–3% experiencing severe symptoms that affect their quality of life and require pharmaceutical treatment to manage their symptoms 3.
Restless leg syndrome is estimated to significantly affect two to three percent of adults. In the United States, 7.4 million adults are significantly affected by the disease.
While RLS is most often diagnosed in middle-aged individuals, the disease affects people of all ages. Patients can often trace symptoms back to their childhood and remember hearing things like “those are growing pains” or “quit wiggling so much.” This study 4 suggests that restless legs syndrome is common and troublesome in nearly 2 percent of children aged 8 to 17.
Clinical Course of Restless Leg Syndrome
- A. Chronic-persistent RLS: Symptoms when not treated would occur on average at least twice weekly for the past year.
- B. Intermittent RLS: symptoms when not treated would occur on average < 2/week for the past year, with at least 5 lifetime events.
If you think you may have restless legs syndrome/Willis-Ekbom disease, see your doctor.
Simple self-care steps and lifestyle changes may help you. To ease your symptoms, try:
- Cutting back on or eliminating caffeine, alcohol and tobacco. Caffeine use may intensify RLS symptoms. Caffeine-containing products, including chocolate and caffeinated beverages such as coffee, tea and soft drinks, should be avoided. Alcohol consumption also increases the span or intensity of symptoms for most individuals.
- Massaging your legs while soaking in a warm bath.
While a cure for RLS has not yet been discovered, many treatments, coping strategies and support resources are available to help individuals and families living with the disease. Medications also help many people with restless legs syndrome.
- Antihistamines (like Benadryl) found in many cold, allergy and over-the-counter sleep aids
- Antidizziness, antinausea medications like Meclizine, Compazine, Phenergan and Reglan
- Antidepressants such as Elavil, Prozac, Lexapro and Effexor
- Psychiatric medications such a haloperidol and phenothiazines that are used to treat bipolar disorders, schizophrenia and other serious disorders
Always be sure that your healthcare provider is aware of all the medicines you are taking, including herbal supplements and over-the-counter medications.
Pregnancy and Restless Legs Syndrome
RLS during pregnancy poses a unique set of challenges 5. Symptoms of RLS may be difficult to differentiate from leg cramps – another common phenomenon in pregnancy – which also have the potential to disrupt sleep. But, unlike RLS, leg cramps involve painful and prolonged contraction and hardening of the muscle. RLS should also be differentiated from simple positional discomfort and leg edema 5. Restless legs syndrome can begin during pregnancy, or a woman already affected by RLS may notice that it becomes more severe during pregnancy.
Restless legs syndrome affects approximately one in five pregnant women in Western countries, less in some Asian countries 6. RLS symptoms are likely to occur or increase later in pregnancy, especially in the third trimester 7. For some women RLS is simply a nuisance. However, for others it can have major impact on sleep and daytime function. It is important to note that in the majority of cases, RLS symptoms resolve or improve significantly soon after delivery. About two-thirds of women with restless legs syndrome during pregnancy have “transient” RLS, with onset and resolution related to pregnancy 8. Predictors of developing RLS during pregnancy include a family history of RLS (8x risk), a history of RLS in a prior pregnancy (54x risk), a history of RLS in the past (13x risk), and low red blood cell count (2x risk) 9. Although “transient” RLS related to pregnancy has a good short-term prognosis, long-term there is triple the risk of developing chronic RLS compared to women who do not experience RLS during pregnancy 8. This and the strong family history of RLS in women who have RLS during pregnancy suggests a genetic predisposition that is unmasked due to pregnancy-related factors.
Factors specific to pregnancy that might account for the increased prevalence of restless legs syndrome in pregnant women have not been well delineated. Potential contributors include low mineral or vitamin levels (iron, folate), sleep deprivation (due to nocturnal discomfort caused by changing body habitus, decreased bladder capacity, or prolonged caffeine half-life), hormonal changes, and increased sensory input (such as caused by lower extremity edema, varicose veins, and nerve compression) 10. Very little research to date has been directed at the treatment of RLS in pregnancy. Most medications that have proven useful in treating RLS in the general population have been inadequately studied for safety in pregnancy, including pramipexole, ropinirole, rotigotine, and gabapentin enacarbil 5.
Before beginning or continuing treatment, women should discuss with their health care provider the risks and benefits of taking specific medications during pregnancy or while breastfeeding. In general, unless absolutely necessary, medications should be avoided during pregnancy unless the benefit clearly outweighs any concerns. To help address the need for treatment guidelines, an expert panel published recommendations in 2015 for the treatment of RLS during pregnancy and lactation 5.
Pregnant or lactating women with RLS should be encouraged to try behavioral approaches primarily, such as low-impact exercise and good sleep habits. Activities that maintain alertness seem to reduce RLS (such as knitting, engaging in intense discussions, or playing computer games). RLS typically subsides during the day, providing the opportunity for a morning or afternoon nap to obtain relief from fatigue after a sleepless night.
Prolonged immobility should be avoided and sleep apnea, if present, should be treated. The duration of caffeine is prolonged during pregnancy. It can aggravate RLS and interfere with sleep, even if taken earlier in the day.
Smoking and alcohol should be avoided. In addition to known harmful effects on the fetus, these have each been associated with increased sleep disturbance and increased RLS in pregnant women 11.
Medications that make RLS worse should also be avoided, including sedating antihistamines such as diphenhydramine (Benadryl). Many medications prescribed for nausea and vomiting of pregnancy can unmask or exacerbate RLS symptoms. In general, doxylamine, prochlorperazine, promethazine and metoclopramide should be avoided for nausea and vomiting of pregnancy. However, ondansetron does not appear to trigger RLS symptoms.
Oral iron is considered safe during pregnancy and lactation with potential benefits for both the mother and fetus. In addition, multiple lines of evidence implicate low iron stores as an aggravating factor for RLS 12. Importantly, it is not uncommon for women to require iron supplementation beyond that in prenatal vitamins during pregnancy, since there is heavy demand on iron stores during pregnancy and prenatal vitamins do not contain adequate iron to treat iron deficiency anemia or low iron stores 13.
For women with RLS during pregnancy or lactation, additional oral iron is recommended if serum ferritin is <75 mcg/L 5. The ferritin level reflects iron stores in the body and is measured by a simple blood test. For RLS it is best for ferritin to be in the “middle normal” range, above 75 mcg/L. Iron supplementation should be supervised by a medical professional to avoid the rare but very serious complication of iron overload. Also, iron should be stored out of the reach of children, because iron overdose in children can be fatal. Intravenous (IV) iron may be considered if oral iron fails and serum ferritin is <30 mcg/L 5.
If medication is felt to be needed for severe, refractory RLS, it should be chosen with care and in consultation with a health care provider, only after behavioral approaches and iron have failed. It should be used at the lowest dosage and frequency possible 5. The 2015 treatment guideline paper 5 includes a detailed discussion of the risks vs benefits of medications for refractory RLS, including clonazepam (Klonopin) or carbidopa/levodopa (Sinemet) during pregnancy, as well as gabapentin (Neurontin) or clonazepam (Klonopin) during lactation. Also, bupropion (Wellbutrin) for depression during pregnancy and lactation is discussed.
Up-to-date, evidence-based information on the safety and risk of drugs during pregnancy, is available at Motherisk (www.motherisk.org), www.perinatology.com, or the Centers for Disease Control and Prevention (CDC)(www.cdc.gov/ncbddd/meds/).
In summary, there is much research to be done on RLS including RLS in pregnancy. Women should be reassured that RLS is likely to resolve or improve significantly soon after delivery. Measures that promote restorative sleep, such as avoiding sleep deprivation, abstaining from caffeine, and partaking in regular moderate exercise should be encouraged. Where ferritin levels are found to be low, supplementation should be given to bring these levels into the mid-normal range. Rarely, in refractory cases, IV iron or medication may be considered 5.
What causes restless leg syndrome
Often, there’s no known cause for restless legs syndrome. Researchers suspect the condition may be due to an imbalance of the brain chemical dopamine, which sends messages to control muscle movement.
Heredity
Sometimes RLS runs in families, especially if the condition starts before age 50. Researchers have identified sites on the chromosomes where genes for restless legs syndrome may be present.
Restless leg syndrome pregnancy
Pregnancy or hormonal changes may temporarily worsen restless leg syndrome or Willis-Ekbom disease signs and symptoms. Some women get restless leg syndrome or Willis-Ekbom disease for the first time during pregnancy, especially during their last trimester. However, signs and symptoms usually disappear after delivery.
Risk factors for restless leg syndrome
Restless leg syndrome or Willis-Ekbom disease can develop at any age, even during childhood. The disorder is more common with increasing age and more common in women than in men.
Restless legs syndrome usually isn’t related to a serious underlying medical problem. However, restless leg syndrome or Willis-Ekbom disease sometimes accompanies other conditions, such as:
- Peripheral neuropathy. This damage to the nerves in your hands and feet is sometimes due to chronic diseases such as diabetes and alcoholism.
- Iron deficiency. Even without anemia, iron deficiency can cause or worsen RLS/WED. If you have a history of bleeding from your stomach or bowels, experience heavy menstrual periods or repeatedly donate blood, you may have iron deficiency.
- Kidney failure. If you have kidney failure, you may also have iron deficiency, often with anemia. When kidneys don’t function properly, iron stores in your blood can decrease. This, with other changes in body chemistry, may cause or worsen RLS/WED.
Complications of restless leg syndrome
Although restless leg syndrome or Willis-Ekbom disease doesn’t lead to other serious conditions, symptoms can range from barely bothersome to incapacitating. Many people with restless leg syndrome or Willis-Ekbom disease find it difficult to fall or stay asleep.
Severe restless leg syndrome or Willis-Ekbom disease can cause marked impairment in life quality and can result in depression. Insomnia may lead to excessive daytime drowsiness, but restless leg syndrome or Willis-Ekbom disease may prevent you from daytime napping.
Restless leg syndrome symptoms
The symptoms vary considerably in frequency from less than once a month or year to daily and severity from mildly annoying to disabling. Symptoms may also remit for various periods of time.
The compelling desire to move is what gives restless legs syndrome its name. Common characteristics of RLS signs and symptoms include:
- Sensation starts after being at rest. The sensation typically begins after you’ve been lying down or sitting for an extended time, such as in a car, airplane or movie theater.
- Relief by movement. The sensation of RLS or Willis-Ekbom disease lessens with movement, such as stretching, jiggling your legs, pacing or walking.
- Worsening of symptoms in the evening. Symptoms occur mainly at night.
- Nighttime leg twitching. RLS or Willis-Ekbom disease may be associated with another, more common condition called periodic limb movement of sleep, which causes your legs to twitch and kick, possibly throughout the night, while you sleep.
People typically describe restless legs syndrome symptoms as abnormal, unpleasant sensations in their legs or feet, usually on both sides of the body. Less commonly, the sensations affect the arms.
The sensations, which generally occur within the limb rather than on the skin, are described as:
- Crawling
- Creeping
- Pulling
- Throbbing
- Aching
- Itching
Sometimes the sensations seem to defy description. Affected people usually don’t describe the condition as a muscle cramp or numbness. They do, however, consistently describe the desire to move their legs.
It’s common for symptoms to fluctuate in severity. In some cases, symptoms disappear for periods of time, then recur.
Restless leg syndrome diagnosis
Your doctor will take your medical history and ask for a description of your symptoms. A diagnosis of restless leg syndrome or Willis-Ekbom disease is based on the following criteria, established by the International Restless Legs Syndrome Study Group 14:
Essential Diagnostic Criteria (all must be met)
- An urge to move the legs usually but not always accompanied by or felt to be caused by uncomfortable and unpleasant sensations in the legs.
- Sometimes the urge to move the legs is present without the uncomfortable sensations typically described as crawling, creeping, cramping, tingling or pulling and sometimes the arms or other parts of the body are involved in addition to the legs.
- For children, the description of these symptoms should be in the child s own words.
- The urge to move the legs and any accompanying unpleasant sensations begin or worsen during periods of rest or inactivity such as lying down or sitting.
- The urge to move the legs and any accompanying unpleasant sensations are partially or totally relieved by movement, such as walking or stretching, at least as long as the activity continues.
- When symptoms are very severe, relief by activity may not be noticeable but must have been previously present.
- The urge to move the legs and any accompanying unpleasant sensations during rest or inactivity only occur or are worse in the evening or night than during the day.
- When symptoms are very severe, the worsening in the evening or night may not be noticeable but must have been previously present.
- The occurrence of the above features are not solely accounted for as symptoms primary to another medical or a behavioral condition (e.g., myalgia, venous stasis, leg edema, arthritis, leg cramps, positional discomfort, habitual foot tapping).
- These conditions, often referred to as “RLS mimics”, have been commonly confused with RLS particularly in surveys because they produce symptoms that meet or at least come very close to meeting criteria 1-4. The list here gives some examples of this that have been noted as particularly significant in epidemiological studies and clinical practice. RLS may also occur with any of these conditions, but the RLS symptoms will then be more in degree, conditions of expression or character than those usually occurring as part of the other condition.
Your doctor may conduct a physical and a neurological exam. Blood tests, particularly for iron deficiency, may be ordered to exclude other possible causes for your symptoms.
In addition, your doctor may refer you to a sleep specialist. This may involve an overnight stay at a sleep clinic, where doctors can study your sleep if another sleep disorder such as sleep apnea is suspected. However, a diagnosis of restless leg syndrome or Willis-Ekbom disease usually doesn’t require a sleep study.
Restless leg syndrome treatment
Sometimes, treating an underlying condition, such as iron deficiency, greatly relieves symptoms of restless legs syndrome.
Your serum ferritin level should be measured. Ferritin is a blood cell protein that contains iron. A ferritin test helps your doctor understand how much iron your body is storing. If a ferritin test reveals that your blood ferritin level is lower than normal, it indicates your body’s iron stores are low and you have iron deficiency and, if the concentration is < 50‐75 μg/L, or if transferrin saturation is less than 20%, supplementation with orally administered iron is recommended unless poorly tolerated or contraindicated 15. Intravenous (IV) iron can also be considered. However, take iron supplements only with medical supervision and after your doctor has checked your blood-iron level.
If you have RLS without an associated condition, treatment focuses on lifestyle changes, and if those aren’t effective, medications.
A Task Force was established by the International Restless Legs Syndrome Study Group 14 in conjunction with the European Restless Legs Syndrome Study Group 16 and the RLS Foundation 17 to develop evidence-based and consensus-based recommendations for the prevention and treatment of long-term pharmacologic treatment of dopaminergic-induced augmentation in restless legs syndrome/Willis–Ekbom disease.
The Task Force made the following prevention and treatment recommendations:
As a means to prevent augmentation, medications such as α2δ ligands [alpha‐2‐delta ligands] (i.e. gabapentin, gabapentin enacarbil, pregabalin) may be considered for initial restless leg syndrome or Willis-Ekbom disease treatment; these drugs are effective and have little risk of augmentation compared to dopaminergic treatment. Alternatively, if dopaminergic drugs [i.e. Ropinirole (Requip), rotigotine (Neupro) and pramipexole (Mirapex)] are elected as initial treatment, then the daily dose should be as low as possible and not exceed that recommended for restless leg syndrome or Willis-Ekbom disease treatment. However, the physician should be aware that even low dose dopaminergics can cause augmentation. Patients with low iron stores should be given appropriate iron supplementation. Daily treatment by either medication should start only when symptoms have a significant impact on quality of life in terms of frequency and severity; intermittent treatment might be considered in intermediate cases.
Table 1. α2δ ligand suggested doses*
| Starting dose | Usual effective daily dose | ||
| <65 years | >65 years | ||
| α2δ ligands | |||
| Approved (USA, Japan as of 2015) | |||
| Gabapentin enacarbil | 600 mg | 300 mg | 600–1200 mg |
| Not approved | |||
| Pregabalin | 75 mg | 50 mg | 150–450 mg |
| Gabapentin* | 300 mg | 100 mg | 900–2400 mg |
*Long-term studies have not been performed with gabapentin in RLS/WED and absorption is variable, thereby complicating dosing.
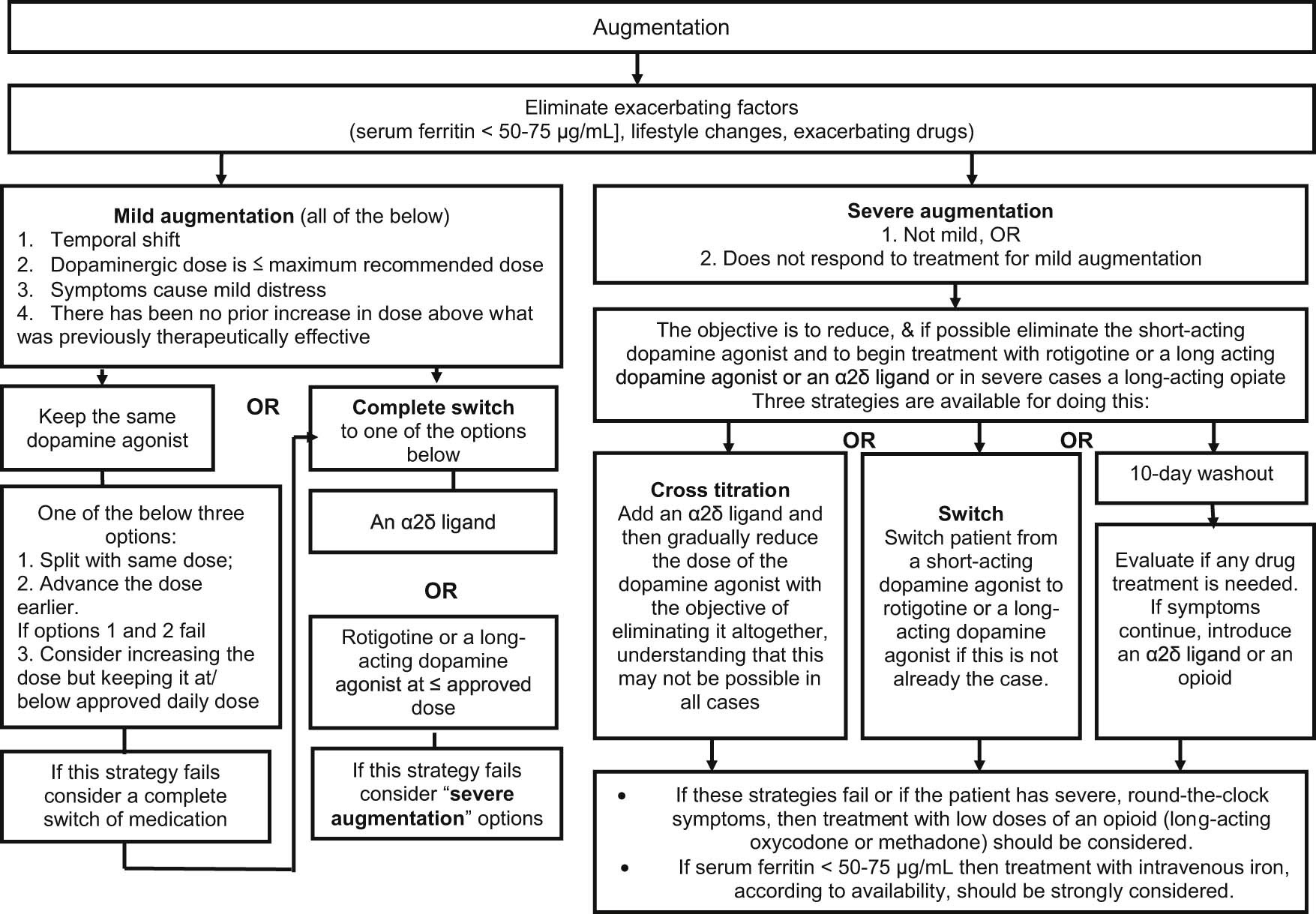
[Source 18]Treatment of existing augmentation should be initiated, where possible, with the elimination/correction of extrinsic exacerbating factors (iron levels, antidepressants, antihistamines, etc.). In cases of mild augmentation, dopamine agonist therapy can be continued by dividing or advancing the dose, or increasing the dose if there are breakthrough night-time symptoms. Alternatively, the patient can be switched to an α2δ ligand [alpha‐2‐delta ligand] (i.e. gabapentin, gabapentin enacarbil, pregabalin) or rotigotine. For severe augmentation the patient can be switched either to an α2δ ligand or rotigotine, noting that rotigotine may also produce augmentation at higher doses with long-term use. In more severe cases of augmentation an opioid may be considered, bypassing α2δ ligands and rotigotine.
Restless leg syndrome medication
Several prescription medications, most of which were developed to treat other diseases, are available to reduce the restlessness in your legs. These include:
- Medications that increase dopamine in the brain. These medications reduce motion in your legs by affecting the level of the chemical messenger dopamine in your brain. Ropinirole (Requip), rotigotine (Neupro) and pramipexole (Mirapex) are approved by the Food and Drug Administration for the treatment of moderate to severe restless leg syndrome or Willis-Ekbom disease. Short-term side effects of these medications are usually mild and include nausea, lightheadedness and fatigue. However, they can also cause impulse control disorders, such as compulsive gambling, and daytime sleepiness.
Table 2. Suggested initial dose and maximum recommended dose for dopamine agonists
| Initial dose | Max. recommended dose | |
|---|---|---|
| Pramipexole | 0.125 mg/day | 0.75 mg/day |
| Ropinirole | 0.25 mg/day | 4 mg/day |
| Rotigotine | 1 mg/day | 3 mg/day |
- Drugs affecting calcium channels. Certain medications, such as gabapentin (Neurontin) and pregabalin (Lyrica), work for some people with restless leg syndrome or Willis-Ekbom disease.
- Opioids. Narcotic medications can relieve mild to severe symptoms, but they may be addicting if used in high doses. Some examples of these medications include codeine, oxycodone (Oxycontin, Roxicodone), combined oxycodone and acetaminophen (Percocet, Roxicet), and combined hydrocodone and acetaminophen (Norco).
- Muscle relaxants and sleep medications. This class of medications, known as benzodiazepines, helps you sleep better at night, but they don’t eliminate the leg sensations, and they may cause daytime drowsiness. Commonly used sedatives for restless leg syndrome or Willis-Ekbom disease include clonazepam (Klonopin), eszopiclone (Lunesta), temazepam (Restoril), zaleplon (Sonata) and zolpidem (Ambien).
It may take several trials for you and your doctor to find the right medication or combination of medications that work best for you.
Table 3. Factors that affect selection of an agent for initial treatment in patients with restless legs syndrome/Willis–Ekbom disease
| Factor that impacts the choice of agent | Treatment choice |
|---|---|
| Time of day (daytime symptoms) | Preferably a long-acting agent Twice-a-day dosing of a short-acting agent |
| Sleep disturbance disproportionate to other symptoms of RLS/WED, eg, severe insomnia | α2δ ligand |
| Comorbid insomnia | α2δ ligand |
| Pregnancy risk | Avoid both DAs and α2δ ligands Consider the use of iron |
| Impaired renal function | Select a drug that is not renally excreted or reduce dose of renally excreted drugs |
| Increased risk of falls | Dopamine-receptor agonist |
| Painful restless legs | α2δ ligand |
| Comorbid pain syndrome | α2δ ligand |
| History of impulse control disorder | α2δ ligand |
| History of alcohol or substance abuse | Dopamine-receptor agonist or α2δ ligand |
| Very severe symptoms of RLS/WED | Dopamine-receptor agonist |
| Excess weight, metabolic syndrome | Dopamine-receptor agonist |
| Availability or cost of drug | Dopamine-receptor agonist or α2δ ligand |
| Comorbid depression | Dopamine-receptor agonist |
| Comorbid generalized anxiety disorder | α2δ ligand |
| Higher potential for drug interactions | Select drug that is not hepatically metabolized |
| Symptomatic PLMS | Dopamine-receptor agonist |
Table 4. Common adverse at 52 weeks
| Event | Pregabalin 300 mg | Pramipexole 0.25 mg | Pramipexole 0.5 mg |
|---|---|---|---|
| Serious adverse events, no. | 11 | 20 | 12 |
| Patients with serious adverse events, no.(%) | 9(4.9) | 12(6.7) | 9(5.0) |
| Patients with adverse events, no.(%) | 155(85.2) | 142(79.8) | 140(77.8) |
| Discontinuations due to adverse events, no.(%) | 50(27.5) | 33(18.5) | 43(23.9) |
| Suicidal ideation, no. | 6 | 3 | 2 |
| Common adverse events, no.(%) appearing in >8% of patients | |||
| Dizziness | 39(21.4%) | 15(8.4%) | 17(9.4%) |
| Somnolence | 32(17.6%) | 12(6.7%) | 14(7.8%) |
| Fatigue | 23(12.6%) | 19(10.7%) | 22(12.2%) |
| Headache | 22(12.1%) | 30(16.9%) | 35(19.4%) |
| Nasopharyngitis | 19(10.4%) | 20(11.2%) | 17(9.4%) |
| Weight gain | 16(8.8%) | 12(6.7%) | 12(6.7%) |
| Constipation | 14(7.7%) | 3(1.7%) | 2(1.1%) |
| Nausea | 11(6.0%) | 18(10.1%) | 26(14.4%) |
| Back pain | 10(5.5%) | 16(9.0%) | 13(7.2%) |
| Influenza | 9(4.9%) | 13(7.3%) | 3(1.7%) |
| Vomiting | 3(1.6%) | 4(2.2%) | 10(5.6%) |
| Diarrhea | 7(3.8%) | 9(5.1%) | 10(5.6%) |
Caution about medications
Sometimes dopamine medications that have worked for a while to relieve your RLS become ineffective. Or you notice your symptoms returning earlier in the day. This is called augmentation. Your doctor may substitute another medication to combat the problem.
Figure 1. Augmentation treatment algorithm
[Source 18]Most drugs prescribed to treat RLS aren’t recommended during pregnancy. Instead, your doctor may recommend self-care techniques to relieve symptoms. However, if the sensations are particularly bothersome during your last trimester, your doctor may approve the use of certain drugs.
Some medications may worsen symptoms of RLS. These include some antidepressants, some antipsychotic medications, some anti-nausea drugs and some cold and allergy medications. Your doctor may recommend that you avoid these medications, if possible. However, if you need to take these medications, talk to your doctor about adding drugs that to help manage your RLS.
Adjusting daily treatment of RLS to prevent augmentation
If a patient is already being treated with a dopaminergic agent, the lowest possible cumulative daily dopaminergic dose should be used to control the majority of bothersome RLS symptoms, and the total daily dose should not exceed maximum recommended levels (pramipexole, 0.5–0.75 mg; ropinirole, 4 mg; rotigotine, 3 mg). However, even low-dose dopaminergic treatments have a risk of augmentation 19. Physicians should explain to patients that the goal of treatment is not to completely eradicate symptoms but to ensure they do not interfere with quality of life. If symptoms become bothersome, the dose can be increased cautiously, but this will increase the risk of developing augmentation. A non-dopaminergic agent can be added if concerns about dose of the dopaminergic drug occur. These therapeutic decisions should also be based on other factors related to patient characteristics such as age, previous episodes of augmentation, and vulnerability to class-related side effects.
Intermittent (non-daily) treatment of RLS to prevent augmentation
The daily treatment of RLS should be deferred as long as possible until symptoms occur almost daily. However, a number of factors make this goal difficult to achieve. First, in patients with intermittent RLS the emergence of symptoms is often unpredictable. Second, many patients find that it is more effective to take medication prior to onset of symptoms, preventing their occurrence, rather than waiting until after symptom onset. Nevertheless, the goal of intermittent dosing should be pursued, especially if symptoms are infrequent (<1–2 per week), or as preventive medications before predictable conditions of immobility (eg, long car or plane trips, medical procedures). Levodopa may be used for intermittent treatment at most two to three times a week, but should not be used for daily treatment, given the high risk of augmentation with this medication.
Using longer acting dopamine agonists
As mentioned above, longer-acting dopaminergic agonists may cause less augmentation than shorter-acting dopamine agonists. As with all other dopamine agonists, the dose of longer-acting dopamine agonists should never be increased above recommended levels (rotigotine, 3 mg) for the treatment of RLS.
Fluctuating RLS symptoms
Longitudinal studies demonstrate that RLS symptom intensity fluctuates and that some patients appear to go into spontaneous remission. Therefore, in patients with a history of notable fluctuating RLS symptoms, the clinician may consider it appropriate to intermittently attempt to reduce the dose or even discontinue the drug in order to ensure that the patient is being treated with the lowest effective dose. If implemented, the patient should be made aware that withdrawal symptoms may be severe and may occur for several days or even weeks after dose reduction and this has to be distinguished from the requirement for continued medication treatment or a true worsening of RLS symptoms.
Switching to an alternate dopaminergic agent
Switching from one dopamine agonist to another is generally not considered useful for preventing (or treating) augmentation, except for switching from levodopa to a longer-acting formulation of a approved dopamine agonist. Physicians may wish to consider long-acting formulations of dopamine agonists as an alternative to reduce the risk of augmentation, although there is no evidence that this will ultimately delay or prevent augmentation. Table 5 provides the suggested initial dose for switching dopamine agonists.
Table 5. Suggested initial dose for switching dopamine agonists
| Rotigotine | Pramipexole ER* | |
|---|---|---|
| Pramipexole | ||
| 0.25 mg | 2 mg | 0.375 mg |
| 0.50 mg (or higher) | 3 mg | 0.75 mg |
| Ropinirole | ||
| 0.5–1.0 mg | 2 mg | 0.375 mg |
| 2 mg or higher | 3 mg | 0.75 mg |
*The incidence rate of augmentation has not been assessed with pramipexole extended release.
[Source 18]Home remedies for restless legs syndrome
Making simple lifestyle changes can help alleviate symptoms of RLS.
- Try baths and massages. Soaking in a warm bath and massaging your legs can relax your muscles.
- Apply warm or cool packs. Use of heat or cold, or alternating use of the two, may lessen your limb sensations.
- Try relaxation techniques, such as meditation or yoga. Stress can aggravate RLS/WED. Learn to relax, especially before bedtime.
- Establish good sleep hygiene. Fatigue tends to worsen symptoms of RLS/WED, so it’s important that you practice good sleep hygiene. Ideally, have a cool, quiet, comfortable sleeping environment; go to bed and rise at the same time daily; and get adequate sleep. Some people with RLS/WED find that going to bed later and rising later in the day helps in getting enough sleep.
- Exercise. Getting moderate, regular exercise may relieve symptoms of RLS/WED, but overdoing it or working out too late in the day may intensify symptoms.
- Avoid caffeine. Sometimes cutting back on caffeine may help restless legs. Try to avoid caffeine-containing products, including chocolate and caffeinated beverages, such as coffee, tea and soft drinks, for a few weeks to see if this helps.
Coping and support
RLS is generally a lifelong condition. Living with restless leg syndrome involves developing coping strategies that work for you, such as:
- Tell others about your condition. Sharing information about RLS will help your family members, friends and co-workers better understand when they see you pacing the halls, standing at the back of the theater, or walking to the water cooler many times throughout the day.
- Don’t resist your need for movement. If you attempt to suppress the urge to move, you may find that your symptoms worsen.
- Keep a sleep diary. Keep track of the medications and strategies that help or hinder your battle with restless leg syndrome , and share this information with your doctor.
- Stretch and massage. Begin and end your day with stretching exercises or gentle massage.
- Seek help. Support groups bring together family members and people with restless leg syndrome . By participating in a group, your insights not only can help you but also may help someone else.
- Restless legs syndrome Diagnostic Criteria. http://irlssg.org/diagnostic-criteria/[↩]
- Restless legs syndrome. https://www.nhs.uk/conditions/restless-legs-syndrome/[↩]
- Symptoms & Diagnosis. https://www.rls.org/understanding-rls/symptoms-diagnosis[↩]
- https://news.illinois.edu/view/6367/206571[↩]
- Picchietti DL, Hensley JG, Bainbridge JL, Lee KA, Manconi M, McGregor JA, et al. Consensus Clinical Practice Guidelines for the Diagnosis and Treatment of Restless Legs Syndrome/Willis-Ekbom Disease During Pregnancy and Lactation. Sleep Med Rev 2015;22:64-77. Review.[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Shang X, Yang J, Guo Y, Ma S, Jia Z, Xue R. Restless legs syndrome among pregnant women in China: prevalence and risk factors. Sleep and Breathing. 2014 Dec 02. doi:10.1007/s11325-014-1089-3.[↩]
- Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA. Sleep disturbances in pregnancy. Obstet Gynecol. 2010;115:77-83.[↩]
- Cesnik E, Casetta I, Turri M, Govoni V, Granieri E, Strambi LF, Manconi M. Transient RLS during pregnancy is a risk factor for the chronic idiopathic form. Neurology 75(23), 2117-20, 2010.[↩][↩]
- Sikandar R, Khealani BA, Wasay M. Predictors of restless legs syndrome in pregnancy: a hospital based cross sectional survey from Pakistan. Sleep Med 10(6), 676-8, 2009.[↩]
- Manconi M, Ulfberg J, Berger K, Ghorayeb I, Wesström J, Fulda S, et al. When gender matters: Restless legs syndrome. Report of the “RLS and woman” workshop endorsed by the European RLS Study Group. Sleep Medicine Reviews. 2012;16:297-307.[↩]
- Kaneita Y, Ohida T, Takemura S, et al. Relation of smoking and drinking to sleep disturbance among Japanese pregnant women. Prev Med. 2005;41(5-6):877-882.[↩]
- Earley CJ, Connor J, Garcia-Borreguero D, Jenner P, Winkelman J, Zee PC, et al. Altered Brain iron homeostasis and dopaminergic function in Restless Legs Syndrome (Willis–Ekbom Disease). Sleep Medicine. 2014;15:1288-301.[↩]
- Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr 72(1 Suppl), 257S-64S, 2000.[↩]
- International Restless Legs Syndrome Study Group. http://irlssg.org/[↩][↩]
- http://irlssg.org/wp-content/uploads/2015/05/Summary-of-recommendations-RLS-Augmentation-13Aug2015.pdf[↩]
- European Restless Legs Syndrome Study Group. http://www.eurlssg.org/[↩]
- RLS Foundation. https://www.rls.org/[↩]
- Guidelines for the first-line treatment of restless legs syndrome/Willis–Ekbom disease, prevention and treatment of dopaminergic augmentation: a combined task force of the IRLSSG, EURLSSG, and the RLS-foundation. Garcia-Borreguero, Diego et al. Sleep Medicine , Volume 21 , 1 – 11. http://www.sleep-journal.com/article/S1389-9457(16)00056-3/fulltext[↩][↩][↩][↩][↩][↩]
- Allen, R.P., Chen, C., Garcia-Borreguero, D. et al. Comparison of pregabalin with pramipexole for restless legs syndrome. N Engl J Med. 2014; 370: 621–631 http://www.nejm.org/doi/full/10.1056/NEJMoa1303646[↩]