Contents
What is Salter Harris fracture
Salter-Harris fracture also called growth plate fracture or physeal fracture, refers to fractures through a growth plate (physis) and are therefore specifically applied to bone fractures in children 1. Salter-Harris fracture classification system used to grade fractures according to the involvement of the growth plate (physis), metaphysis, and epiphysis is important as it has implications for both prognosis and treatment 2.
Salter-Harris fractures are common among children and comprise 15% to 30% of all bony injuries. Harris-Salter fractures are described exclusively in children and do not occur in the well-developed bones of adults.
In general, upper extremity injuries are more common than lower-extremity injuries.
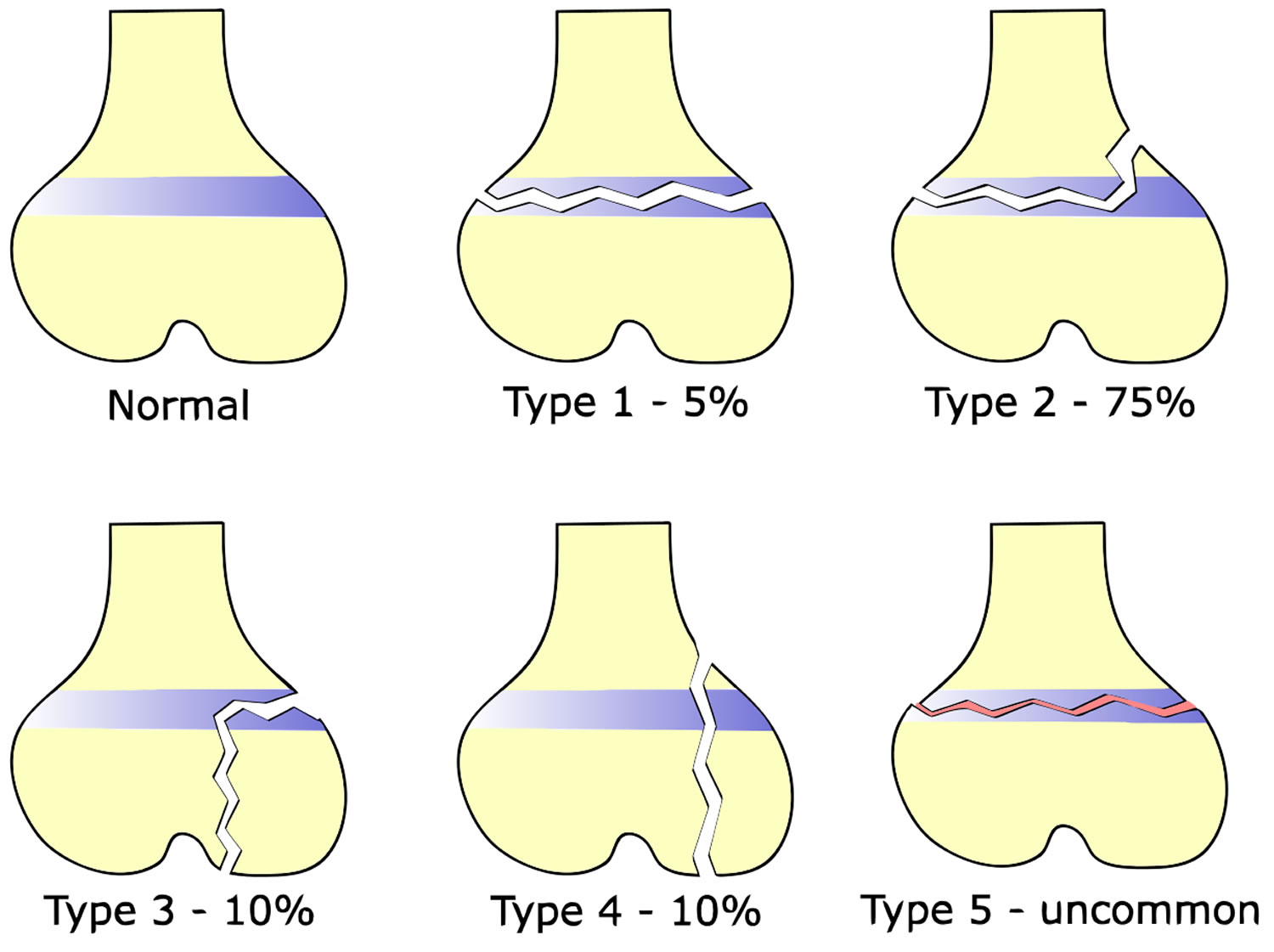
Of the five most common Salter-Harris fracture types, type II is the most common (75%) followed by types III (10%), IV (10%), type I (5%), and lastly, type V which is very rare 1.
Males are more likely to be affected because they have an increased tendency to engage in high-risk activities. Girls are affected at a younger age (11 to 12 years) than boys (12 to 14 years).
Most of these Salter-Harris fractures occur during the time of a child’s growth spurt when their bone’s growth plates are the weakest. Active children are the most likely to encounter injuries involving the growth plate as the ligaments and joint capsules surrounding the growth plate tend to be much stronger and more stable. They are thereby able to sustain greater external loads to the joint, relative to the growth plate itself 3.
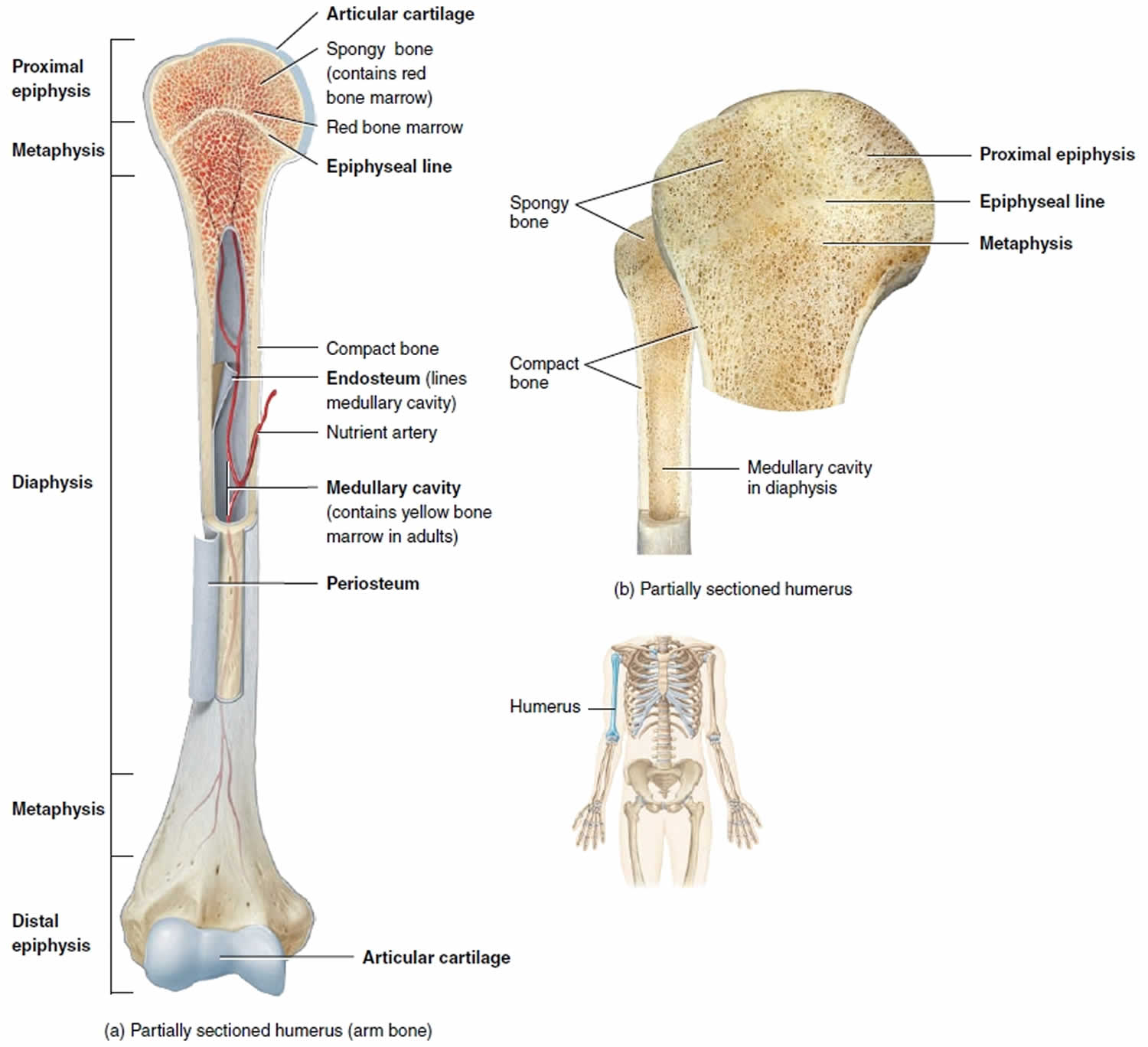
Long bone anatomy
Most long bones in the body contain at least two growth plates (one at each end), a hyaline cartilage plate located between the epiphysis and metaphysis near both ends of a long bone. Once a child or adolescent completes his or her growth spurt, the plate will eventually ossify and form an epiphyseal line. Examples of long bones include the femur (thighbone), the radius and ulna in the forearm, as well as the metacarpal bones in the hands.
Growth plates are located between the widened part of the shaft of the bone (the metaphysis) and the end of the bone (the epiphysis). The long bones of the body do not grow from the center outward. Instead, growth occurs at each end of the bone around the growth plate. When a child is fully grown, the growth plates harden into solid bone.
In the physis, four zones are described from the epiphysis toward the metaphysis: (1) resting cells, (2) proliferating cells, (3) hypertrophic/maturing cells, and (4) provisional calcification.
The zone of hypertrophic/maturing cells is involved when fractures occur. In the event of a fracture, the blood supply which enters the bone through the epiphysis may become compromised.
Physeal fractures tend to occur through the zone of provisional calcification. They may even cross several zones depending on the type of injury or the external force that is applied (e.g., shear vs. compression vs. tension forces).
The physis or growth plate is a weak part of cartilage present in the developing bone. The physis closes in children at varying ages.
Figure 1. Long bone anatomy
Salter Harris fracture types
Salter-Harris classification includes types I through V, with the higher numbers indicating a higher risk for growth abnormalities 4.
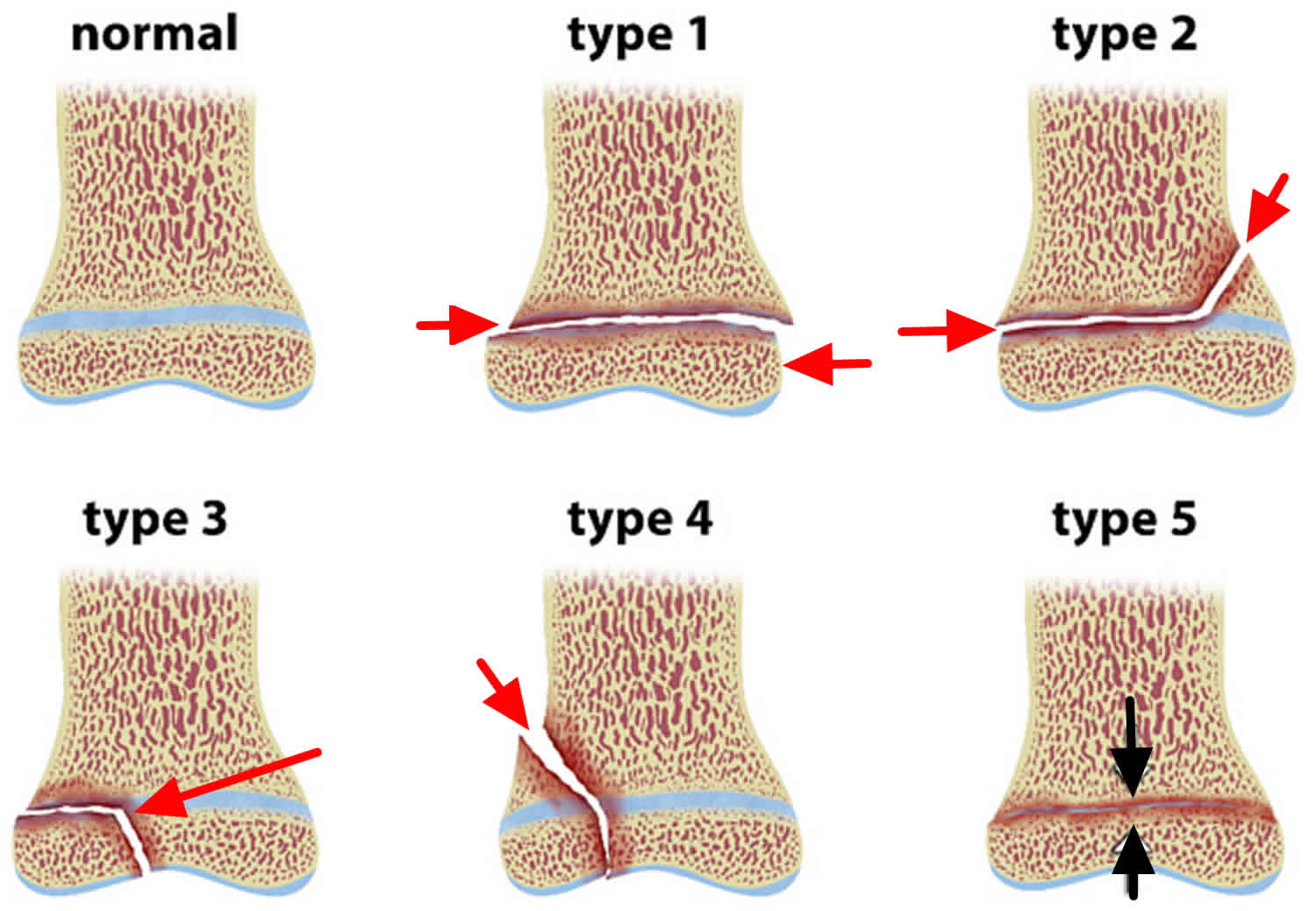
Figure 2. Salter Harris fracture types
Salter Harris fracture fracture type 1
In Salter Harris fracture type 1 the fracture line extends “through the physis” or within the growth plate. Type I fractures are due to the longitudinal force applied through the physis and split the epiphysis from the metaphysis. Beware that a normal radiograph cannot exclude a physis injury in a symptomatic pediatric patient. A radiograph may be normal due to lack of bony involvement, and mild to moderate soft tissue swelling may be noted. Look for the widening of the physis or displacement of the epiphysis, which may suggest a fracture. Diagnosis is based on clinical findings such as the presence of focal tenderness or a swelling surrounding the growth plate. An example is Slipped Capital Femoral Epiphysis (SCFE).
Salter Harris fracture type 2
Salter Harris fracture type 2 is a “fracture of the physis, extending to the metaphysis” away from the joint space. Salter Harris type II fractures are the most common and occur when a piece of the metaphysis remains attached to the epiphysis.
A corner sign means the small corner of metaphysis may be visible as corner sign which is also called Thurston-Holland fragment. Beware that these involve the metaphysis. Be careful in using the terms proximal and distal to describe the extension, because the position of the physis is relative to the metaphysis and is not fixed.
If the proximal end of the bone is involved, the physis is proximal to the metaphysis, so this extends distally from the physis into the metaphysis. If it involves the distal end of the bone, the physis is distal to the metaphysis, so the this extends proximally from the physis into the metaphysis.
Salter Harris fracture type 3
Salter Harris fracture type 3 is an intra-articular fracture extending from the physis (growth plate) into the epiphysis (toward the joint space). If the fracture extends the complete length of the physis, this type of fracture may form two epiphyseal segments. Since epiphysis is involved, damage to the articular cartilage can occur. An example is a Tillaux fracture of the ankle which is a fracture of the anterolateral aspect of the growth plate and epiphysis.
Salter Harris fracture type 4
Salter Harris fracture type 4 is also an intra-articular fracture, in which the fracture passes through the epiphysis, physis, and metaphysis. As Salter Harris fracture type 4 involves the epiphysis, the articular cartilage may be damaged. An example is a Triplane fracture at the ankle which has the following three components:
- Vertical component through the epiphysis
- Horizontal component through the growth plate
- Oblique component through the metaphysis.
Salter Harris types 3 and 4 fractures each carry a risk for growth retardation, altered joint mechanics, and functional impairment. They therefore both require urgent orthopedic evaluation.
Salter Harris fracture type 5
Salter Harris fracture type 5 is due to a crush or compression injury of the growth plate. Beware that it can be radiographically occult, and thus the radiograph may appear normal. One should consider the possibility of Salter Harris fracture type 5 in a symptomatic child with a normal radiograph in an appropriate setting.
In Salter Harris fracture type 5, the force is transmitted through the epiphysis and physis, potentially resulting in disruption of the germinal matrix, hypertrophic region, and vascular supply. Though Salter Harris type 5 fractures are very rare, they may be seen in cases of electric shock, frostbite, and irradiation. These typically result in a poor prognosis in so far as this fracture pattern tends to result in severe injury, involving bone growth arrest.
Salter Harris fracture cause
Salter Harris fractures are often caused by a single event, such as a fall or car accident. They can also occur gradually as a result of repetitive stress on the bone, which may occur when a child overtrains in a sports activity.
All children who are still growing are at risk for Salter Harris fractures, but there are certain factors that may make them more likely to occur:
- Salter Harris fractures occur twice as often in boys as in girls, because girls finish growing earlier than boys.
- One-third of all Salter Harris fractures occur during participation in competitive sports such as football, basketball, or gymnastics.
- About 20% of all Salter Harris fractures occur during participation in recreational activities such as biking, sledding, skiing, or skateboarding.
- The incidence of Salter Harris fractures peaks in adolescence.
Salter Harris fracture symptoms
A Salter Harris fracture usually causes persistent or severe pain. Other common symptoms include:
- Visible deformity, such as a crooked appearance of the limb
- An inability to move or put pressure on the limb
- Swelling, warmth, and tenderness in the area around the end of the bone, near the joint
The most common presentation of a Salter-Harris fracture is localized joint pain following a traumatic event (e.g., collision, crush injury, or fall). The patient may present with swelling around the joint in addition to focal (or point) tenderness over the physis. If the injury occurs in the upper extremity, the patient may complain of reduced (or limited) range of motion. If the injury involves a lower extremity, the patient may be unable to bear weight on the affected side. It is important to note that symptoms may mimic ligamentous injury, and there potentially may be findings on ligamentous laxity tests. Therefore, one must be cautious to avoid misdiagnosing symptoms as related to joint tissues alone.
Salter Harris fracture complications
Although most Salter-Harris fractures heal without any lasting effect, complications can occur.
Rarely, a bony bridge will form across the fracture line, stunting the growth of the bone or causing the bone to curve. If this occurs, your doctor may perform a procedure to remove the bony bar and insert fat or other materials to prevent it from reforming.
In other cases, a Salter-Harris fracture may actually stimulate growth so that the injured bone ends up longer than its opposite, uninjured limb. If this occurs, surgery can help achieve a more even length.
Salter Harris fracture diagnosis
Because a child’s bones heal quickly, a potential growth plate injury should be examined by a doctor as quickly as possible, ideally within 5 to 7 days. It is important that the bone receives the proper treatment before it begins to heal.
After discussing your child’s symptoms and medical history, your doctor will perform a careful physical examination of the injured area.
Your doctor will likely order an x-ray to determine whether a growth plate fracture has occurred. X-rays provide clear images of dense structures, such as bone. If greater detail is needed, your doctor may order other diagnostic imaging tests that can better show the soft tissues, or a cross-sectional view of the injured area. These types of scans include magnetic resonance imaging (MRI) scans and computed tomography (CT) scans.
Though many acute Salter-Harris fractures may not initially be visible on a plain radiograph, there may be evidence of physeal widening, in other words, a potential clue to the presence of displacement. Two views, anteroposterior and lateral, may be necessary to delineate the fracture type properly; in addition to comparing the injured extremity with the opposite, unaffected extremity.
Computerized tomography (CT) scan with multiplanar reconstruction can be obtained if it is necessary to determine the exact orientation of severely comminuted epiphyseal or metaphyseal fractures. This may be helpful to define the exact measurements of fracture diastasis which is important when an articular cartilage is involved, for example in weight-bearing zones).
MRI Scan may show the following findings:
- Widening and increased T2-weighted signal within the fractured physis
- Bone marrow edema in the vicinity of fracture
- Metaphyseal fracture line (Salter-Harris II)
- Epiphyseal fracture line (Salter-Harris III)
- Periosteal disruption.
Ultrasound may be useful in infants as cartilage has not ossified in young infants.
Salter Harris fracture treatment
Treatment for Salter Harris fractures depends on several factors, including:
- Which bone is injured
- The type of fracture
- How much the broken ends of the bone are out of alignment (displaced)
- The age and health of the child
- Any associated injuries
Salter Harris type 1 and 2 fractures can be treated with closed reduction and casting or splinting. The reduction should be performed carefully to avoid damage to or grating of the physis on any metaphyseal bone fragments 5.
Salter Harris type 3 and 4 fractures usually require open reduction and an internal fixation (avoiding crossing the physis).
Beware that Salter Harris type 5 fracture diagnosis may be delayed unless there is a high degree of clinical suspicion. Often the diagnosis is not made at the initial presentation. An emergent orthopedic consultation should be obtained if the fracture is recognized in the emergency department. As these fractures involve the germinal matrix, they have a potential for growth arrest.
In all cases, a reexamination is necessary for seven to ten days to monitor and maintain proper reduction and healing and determine whether any complications, such as growth arrest, will occur. If clinically indicated, an additional follow-up radiograph at six months and 12 months may be obtained to reassess for any growth arrest.
Nonsurgical treatment
Many Salter Harris type 1 and 2 fractures can heal successfully when treated with immobilization: a cast is applied to the injured area and the child limits some types of activity.
Doctors most often use cast immobilization when the broken fragments of bone are not significantly out of place. A cast will protect the bones and hold them in proper position while they heal.
Surgical treatment
If the bone fragments are displaced and the fracture is unstable, surgery may be necessary. The most common operation used to treat fractures is called open reduction and internal fixation.
During the procedure, the bone fragments are first repositioned into their normal alignment (called a reduction). The bones are then fixed into place with special implants like screws or wires, or by attaching metal plates to the outer surface of the bone.
A cast is often applied to protect and immobilize the injured area while it heals.
Salter Harris fracture recovery time
A child’s bones heal quickly, but a Salter Harris fracture can still take several weeks to heal. If cast immobilization is used, the length of time the cast is worn will vary depending on the severity of the Salter Harris fracture.
After the bone heals, your doctor may recommend specific exercises to strengthen the muscles that support the injured area of bone and improve the range of motion of the joint.
Salter Harris fracture long-term outcomes
Salter Harris fractures must be watched carefully to ensure proper long-term results. Regular follow-up visits to the doctor should continue for at least a year after the fracture to make sure that the growth plate is growing appropriately.
More complicated fractures, as well as fractures to the thighbone (femur) and shinbone (tibia), may require follow-up visits until the child reaches skeletal maturity.
- Levine RH, Foris LA, Waseem M. Salter Harris Fractures. [Updated 2019 May 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430688[↩][↩]
- Sheffer BW, Villarreal ED, Ochsner MG, Sawyer JR, Spence DD, Kelly DM. Concurrent Ipsilateral Tibial Shaft and Distal Tibial Fractures in Pediatric Patients: Risk Factors, Frequency, and Risk of Missed Diagnosis. J Pediatr Orthop. 2019 Apr 08[↩]
- Rickert KD, Hosseinzadeh P, Edmonds EW. What’s New in Pediatric Orthopaedic Trauma: The Lower Extremity. J Pediatr Orthop. 2018 Sep;38(8):e434-e439[↩]
- Asad WA, Younis MHS, Ahmed AF, Ibrahim T. Open versus closed treatment of distal tibia physeal fractures: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2018 Apr;28(3):503-509[↩]
- D’Angelo F, Solarino G, Tanas D, Zani A, Cherubino P, Moretti B. Outcome of distal tibia physeal fractures: a review of cases as related to risk factors. Injury. 2017 Oct;48 Suppl 3:S7-S11[↩]