Contents
- What is sarcoidosis
- Sarcoidosis stages
- Prognosis of sarcoidosis
- Sarcoidosis symptoms and signs
- Lofgren’s Syndrome
- Common Signs and Symptoms
- Lung sarcoidosis
- Skin sarcoidosis may include the following:
- Swollen or Enlarged Lymph Nodes
- Eye sarcoidosis
- Cardiac sarcoidosis
- Brain and Nervous System Sarcoidosis
- Bones, Joints, and Muscles Sarcoidosis
- Spleen sarcoidosis
- Liver sarcoidosis
- Kidneys and Urinary Tract Sarcoidosis
- Salivary Glands Sarcoidosis
- Sinuses Sarcoidosis
- Other Signs and Symptoms of Sarcoidosis
- Sarcoidosis causes
- Diagnosis of sarcoidosis
- Sarcoidosis treatment
- Complications of sarcoidosis
- Living With Sarcoidosis
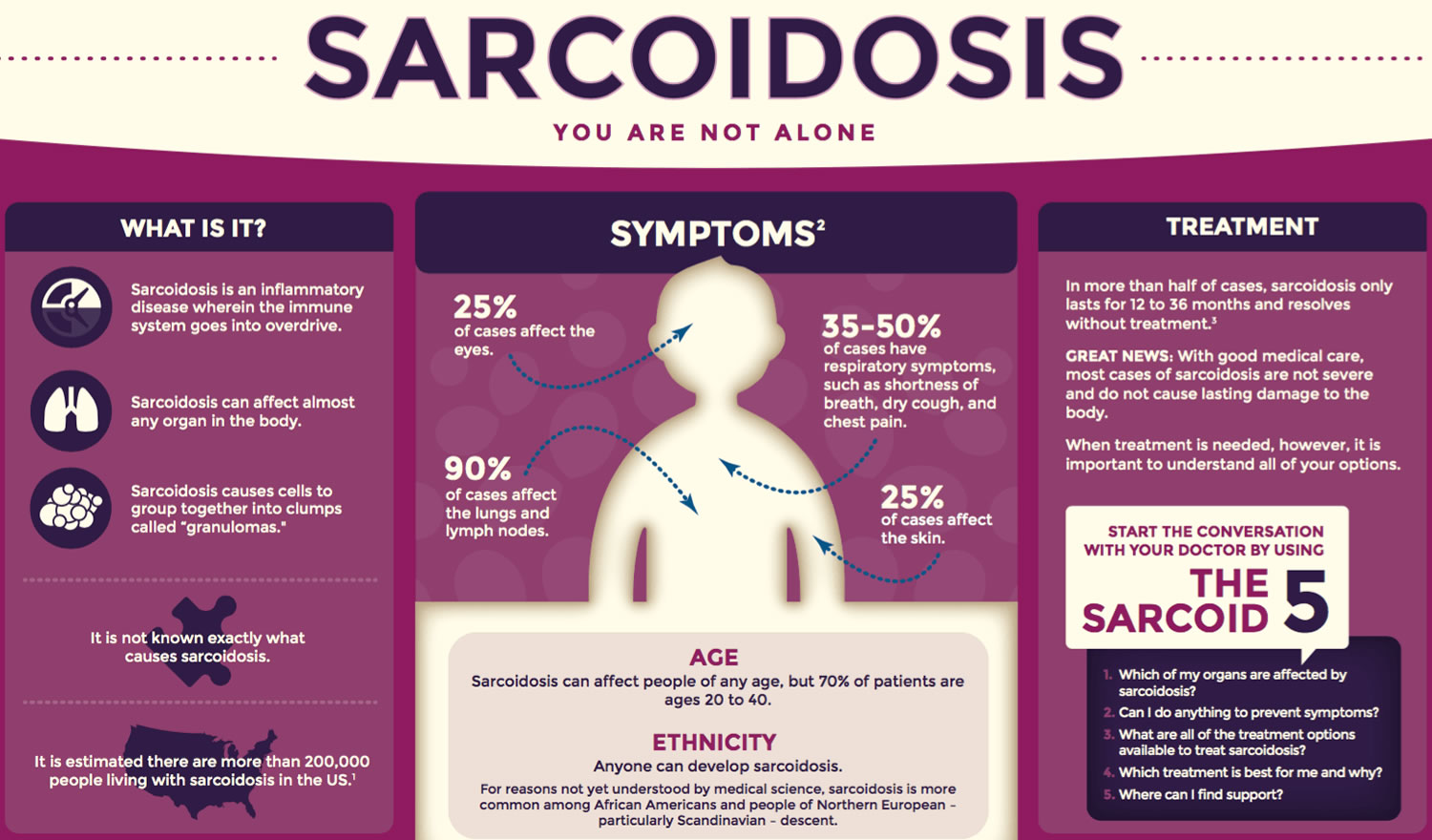
What is sarcoidosis
Sarcoidosis is a multisystem inflammatory disease of unknown cause that manifests by the formation of noncaseating granulomas, tiny clumps of inflammatory cells, in one or more organs of the body 1. When the immune system goes into overdrive and too many of these clumps form, they can interfere with an organ’s structure and function. When left unchecked, chronic inflammation can lead to fibrosis, which is permanent thickening or scarring of organ tissue.
The age-adjusted incidence of sarcoidosis is 11 cases per 100,000 population in whites but 34 cases per 100,000 population in African Americans.
This disorder can affect almost any organ in the body, including the heart, skin, liver, kidneys, brain, sinuses, eyes, muscles, bones, and other areas. Sarcoidosis most commonly targets the lungs and the intrathoracic lymph nodes, which are an important part of the immune system. When it affects the lungs, it is called pulmonary sarcoidosis. 90 percent or more of people diagnosed with the disease have lung involvement. Many people who have sarcoidosis have no signs or symptoms or mild ones 2.
Sarcoidosis affects people of all ages and races. However, it’s more common among African Americans and Northern Europeans. In the United States, the disease affects African Americans somewhat more often and more severely than Whites.
Studies have shown that sarcoidosis tends to vary amongst ethnic groups. For example, eye problems related to the disease are more common in Japanese people.
Lofgren’s syndrome, a type of sarcoidosis, is more common in people of European descent. Lofgren’s syndrome may involve fever, enlarged lymph nodes, arthritis (usually in the ankles), and/or erythema nodosum. Erythema nodosum is a rash of red or reddish-purple bumps on your ankles and shins. The rash may be warm and tender to the touch.
Sarcoidosis is somewhat more common in women than in men. The disease usually develops between the ages of 20 and 50. People who have a family history of sarcoidosis also are at higher risk for the disease.
Researchers have looked for a link between sarcoidosis and exposure to workplace and environmental factors. However, no clear link has been found.
Figure 1. Sarcoidosis
Treatment for sarcoidosis varies depending on which organs are affected. Your doctor may prescribe topical treatments and/or medicines to treat the disease. Not everyone who has sarcoidosis needs treatment.
Disease presentation and severity varies widely among patients. For educational purposes, not a clinical standard, the Foundation for Sarcoidosis Research recognizes three general categories in which patients may fall into:
Resolving Sarcoidosis
In many cases, inflammation can resolve itself without specific therapy and before causing serious damage to the body. Upon initial diagnosis, doctors will assess for danger (organ dysfunction) and the extent to which a patient’s quality of life is impaired. Fatigue and pain syndromes, for example, are common among sarcoidosis patients and can greatly affect quality of life. If the physician does see evidence of organ dysfunction and does not believe that the patient’s quality of life is affected enough to warrant treatment, ongoing monitoring may be warranted.
Remitting Sarcoidosis
Sarcoidosis can also go into remission, a period when the disease no longer causes symptoms or problems in the body. More than half of the people will experience remission within three years of their diagnosis, and two-thirds will go into remission within 10 years of diagnosis. Sarcoidosis symptoms can return after remission, but this is not common. Return of disease symptoms and activity after one or more years of remission occurs in less than five percent of patients.
Chronic Sarcoidosis
For some people, the disease can be ongoing, causing permanent damage to the body, organ failure, and even death. For pulmonary sarcoidosis patients, some cases result in permanent lung damage. These patients may require portable oxygen and/or a lung transplant. Medical treatment may ease symptoms, improve organ function, and limit damage to the body. However, treatments that work on some patients may not on others, and often the drugs used in treatments can cause other issues. More research is needed for additional treatment options.
Despite the best efforts of researchers for more than a century working to better understand the complexities of this disease, sarcoidosis remains difficult to diagnose with limited therapies. Many patients suffer for years before arriving at the correct diagnosis or discovering the best treatment plan, although we’re coming closer to understanding the mechanisms. Learn more about the possible mechanisms by which people develop sarcoidosis.
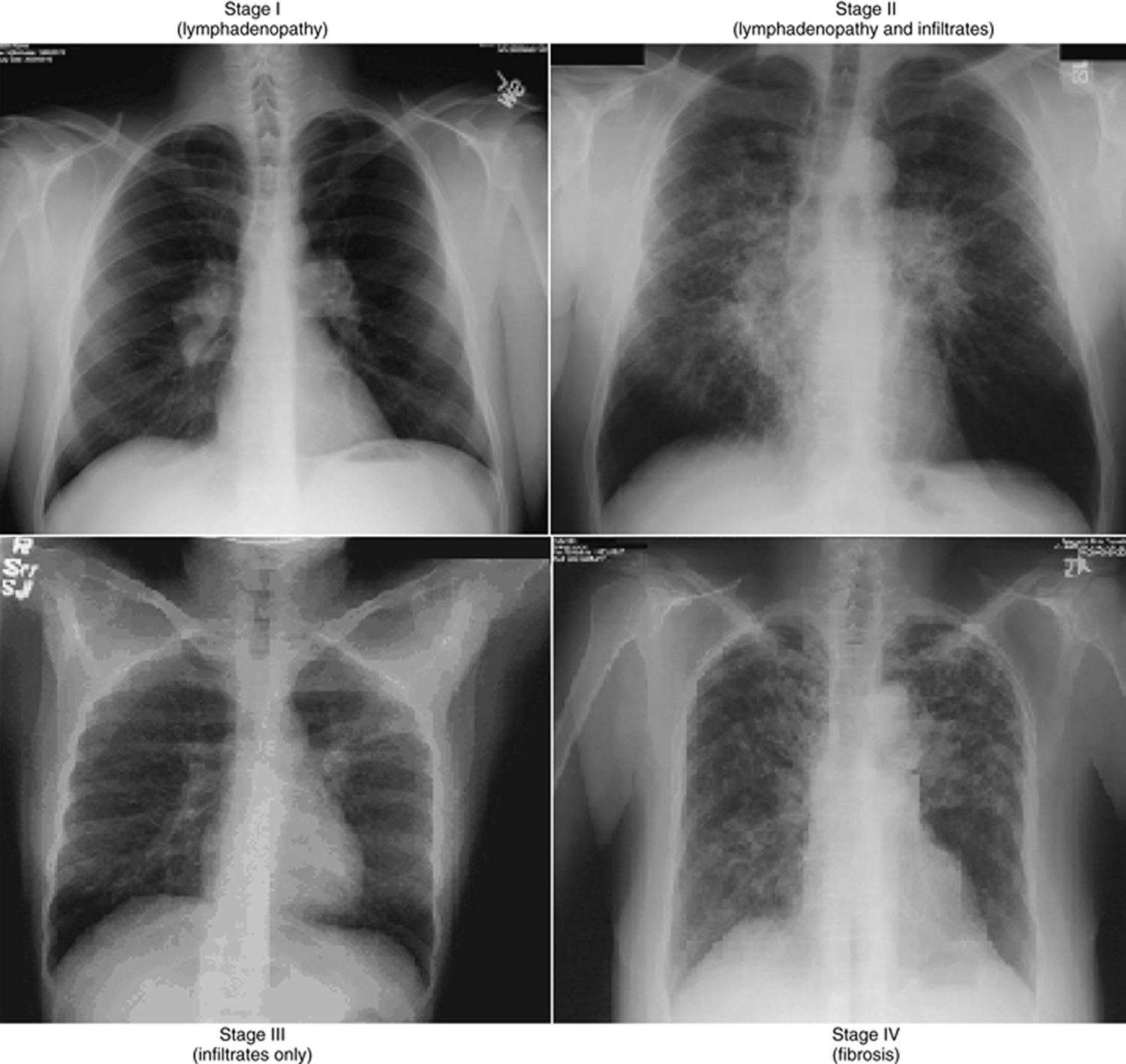
Sarcoidosis stages
It’s estimated that at least 90% of patients with sarcoidosis will experience lung involvement. Chest x-rays are often used to determine the nature of the disease. However, the results of this imaging can cause confusion for sarcoidosis patients- your doctor might tell you that the images indicate a certain “stage” of sarcoidosis. What does this mean? Is it like the stages of cancer? Being told you have “stage three” or “stage four” pulmonary sarcoidosis sounds bad- but what does it really mean?
Hopefully, your doctor gives you an accurate explanation of what the stages mean. The stages of sarcoidosis should not be viewed in the way that stages of cancer are- they do not indicate progression of the disease.
In sarcoidosis staging of pulmonary disease is based on the chest x-ray (see Figure 2) allows a general prediction of outcome. In sarcoidosis, staging is a way to indicate the location of granulomas- the lungs, the lymph nodes, or both- and the nature of the disease. If anything, the stages are an easy way for doctors to categorize their sarcoidosis patients, and should not be seen as an indication of severity.
Staging of sarcoidosis is as follows:
- Stage 0: Normal chest radiographic findings
- Stage I: Bilateral hilar lymphadenopathy
- Stage II: Bilateral hilar lymphadenopathy and infiltrates
- Stage III: Infiltrates alone
- Stage IV: Fibrosis
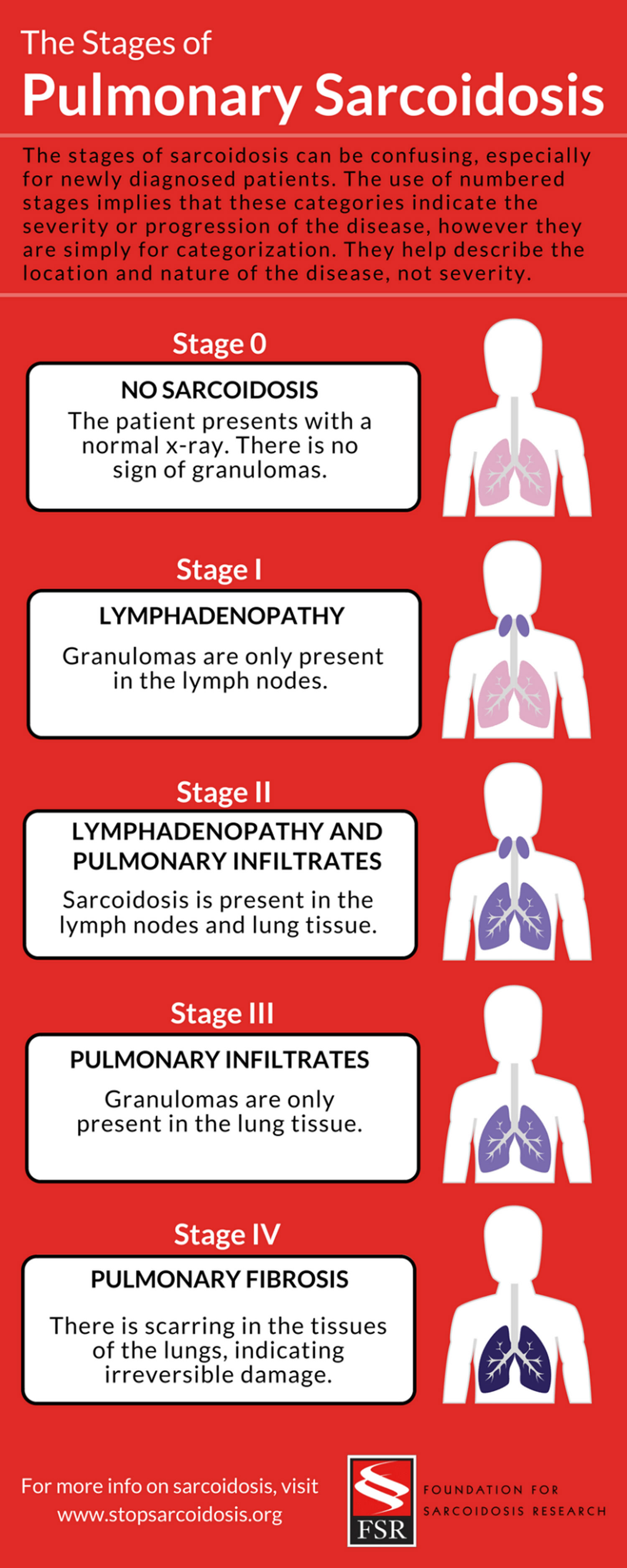
Stage one sarcoidosis indicates granulomas in the lymph nodes. Stage two indicates lymph node involvement in addition to granulomas in the lungs. At first, this might appear to be a progressive diagnosis compared to stage one. However, stage three sarcoidosis indicates granulomas present in the lungs, but not in the lymph nodes. This demonstrates how the stages are not a progression. A patient may even go between these stages- you might have stage two sarcoidosis, and then with treatment or time become stage one, or three, or go into remission altogether.
Stage four sarcoidosis is a little bit different than the other three. Stage four indicates scarring in the lungs- pulmonary fibrosis- which is irreversible. Because of this, stage four is the most severe presentation of sarcoidosis. This also contributes to the misconception that the stages of sarcoidosis follow a progression.
The stage of sarcoidosis does not indicate a level of severity- in fact, each “stage” can be at a different level of severity. An individual might have granulomas in their lungs but nowhere else (stage three) and be completely asymptomatic. This kind of sarcoidosis is often caught by accident on an x-ray for another injury or illness, and may not even require treatment. In another case, someone might have granulomas only present in their lymph nodes (stage one), but experience severe pain and swelling, or other complications.
Figure 2. Sarcoidosis Stages
Prognosis of sarcoidosis
The outlook for sarcoidosis varies. Many patients do not require therapy and their conditions spontaneously improve with few or no long-term problems 3. Markers for a poor prognosis include advanced chest radiography stage, extrapulmonary disease (predominantly cardiac and neurologic), and evidence of pulmonary hypertension 4. Multiple studies have demonstrated that the most important marker for prognosis is the initial chest radiography stage.
| Stage | Remission (%) | Asymptomatic at 5 y (%) | Chest Radiograph Clearing (%) | Mortality (%) |
| Stage I | 60-90 | 95 | 54 | 0 |
| Stage II | 40-70 | 58 | 31 | 11 |
| Stage III | 10-20 | 25 | 10 | 18 |
| Stage IV | 0 | N/A | 0 | N/A |
In one study of patients with radiographic stage IV sarcoidosis, during an average follow-up of 7 years, pulmonary hypertension was observed in 30% of cases. Long-term oxygen therapy was required in 12%. Survival was 84% at 10 yrs. Cause of death in 11% patients included refractory pulmonary hypertension, acute and chronic respiratory insufficiency, and heart sarcoidosis. Seventy-five percent of fatalities are directly attributable to respiratory causes 5.
- More than half of the people who have sarcoidosis have remission within 3 years of diagnosis. “Remission” means the disease isn’t active, but it can return.
- Two-thirds of people who have the disease have remission within 10 years of diagnosis. People who have Lofgren’s syndrome usually have remission. Relapse (return of the disease) 1 or more years after remission occurs in less than 5 percent of patients.
Sarcoidosis leads to organ damage in about one-third of the people diagnosed with the disease. Damage may occur over many years and involve more than one organ. Rarely, sarcoidosis can be fatal. Death usually is the result of problems with the lungs, heart, or brain.
Poor outcomes are more likely in people who have advanced disease and show little improvement from treatment.
Data regarding mortality from sarcoidosis are scant. In the United States, deaths tend to result from the complications of end-stage lung disease (eg, respiratory failure, right heart failure).
Functional impairment occurs in only 15-20% of patients and often resolves spontaneously. The overall mortality rate is less than 5% for untreated patients.
The likelihood of regression for pulmonary disease correlates with the extent of parenchymal disease, as noted by chest radiography stage.
According to a study by Swigris et al 6, the rate of sarcoidosis-related mortality in the United States appears to have increased significantly from 1988-2007, particularly in black females aged 55 years or older. This study also confirmed findings from prior reports, indicating that the underlying cause of death in most patients with sarcoidosis was the disease itself.
Certain people are at higher risk for poor outcomes from chronic (long-term) sarcoidosis. This includes people who have lung scarring, heart or brain complications, or lupus pernio. Lupus pernio is a serious skin condition that sarcoidosis may cause.
Research is ongoing for new and better treatments for sarcoidosis.
Sarcoidosis symptoms and signs
Signs and symptoms of sarcoidosis vary widely depending on the organs affected. While many people who have sarcoidosis have very few or no signs of the disease, others suffer debilitating effects that can interfere with daily life. It is important to discuss all symptoms with your physician so they can arrive at the correct diagnosis and develop the best treatment plan for your unique case.
The presentation in sarcoidosis varies with the extent and severity of organ involvement, as follows:
- Asymptomatic (incidentally detected on chest imaging): Approximately 5% of cases
- Systemic complaints of fever, anorexia (loss of appetite) and arthralgias (painful joints): 45% of cases
- Pulmonary complaints (dyspnea on exertion, chronic cough, wheezing, chest pain, and hemoptysis [rare]): 50% of cases
- Löfgren syndrome (fever, bilateral hilar lymphadenopathy, and polyarthralgias): Common in Scandinavian patients, but uncommon in African-American and Japanese patients. Lofgren’s syndrome is a classic set of signs and symptoms that is typical in some people who have sarcoidosis. Lofgren’s syndrome may cause fever, enlarged lymph nodes, arthritis (usually in the ankles) and/or erythema nodosum. Erythema nodosum is a rash of red or reddish-purple bumps on your ankles and shins. The rash may be warm and tender to the touch.This presentation is associated with an excellent prognosis.
Lofgren’s Syndrome
Lofgren’s syndrome is a classic set of signs and symptoms that occur in some people when they first have sarcoidosis. Signs and symptoms may include:
- Fever. This symptom only occurs in some people.
- Enlarged lymph nodes (which can be seen on a chest x ray).
- Arthritis, usually in the ankles. This symptom is more common in men than women.
- Erythema nodosum. This is a rash of red or reddish-purple bumps on your ankles and shins. The rash may be warm and tender to the touch. This symptom is more common in women than men.
Common Signs and Symptoms
In both adults and children, sarcoidosis most often affects the lungs. If granulomas (inflamed lumps) form in your lungs, you may wheeze, cough, feel short of breath, or have chest pain. Or, you may have no symptoms at all.
Some people who have sarcoidosis feel very tired, uneasy, or depressed. Night sweats and weight loss are common symptoms of the disease.
Common signs and symptoms in children are fatigue (tiredness), loss of appetite, weight loss, bone and joint pain, and anemia.
Children who are younger than 4 years old may have a distinct form of sarcoidosis. It may cause enlarged lymph nodes in the chest (which can be seen on chest x-ray pictures), skin lesions, and eye swelling or redness.
Lung sarcoidosis
The lungs are the most commonly affected organ in sarcoidosis. Ninety percent or more of people with sarcoidosis have lung involvement, whether they have symptoms or not. Symptoms specific to sarcoidosis affecting the lungs include:
- Dry coughing
- Trouble breathing, wheezing, or pain with breathing
- Chest pain, tightness, or discomfort
- Coughing up blood (which is rare), especially in the early stages of sarcoidosis.
There are many problems that can be caused by sarcoidosis affecting the lungs, usually only in the most serious cases. Those problems include:
- Pulmonary Fibrosis: scarring that occurs in the lungs as a result of untreated or unyielding inflammation/granuloma formation. As scar tissue builds up in the walls of air sacs in the lungs, it can make it hard for oxygen to get into your blood over time, leading to reduced oxygen levels in the blood and shortness of breath. Pulmonary fibrosis belongs to a larger group of lung diseases called “interstitial lung diseases,” another way in which your doctor might refer to your condition.
- Fibrocystic disease: an advanced form of lung disease in which scars block airways in one or both lungs
- Pulmonary hypertension: a condition in which scar tissue narrows or blocks arteries in the lungs, causing high blood pressure. The high blood pressure, also known as hypertension, forces the heart to work harder to pump blood through the vessels. Over time, heart muscle builds up and weakens, hindering its ability to deliver oxygen to lungs and other parts of the body.
- Bronchiectasis: condition in which the walls of the bronchi, or airways in the lungs, thicken due to chronic inflammation/granuloma formation. Overtime, bronchi become unable to clear out mucus. The mucus then builds up, creating an environment where bacteria will grow. Over time, the airways become inflamed, stretched out, and scarred, making it harder for the lungs to move air through them.
- Aspergilloma: a clump of fungus that forms in healed lung scars and enlarged airways, and can cause bleeding in the lungs.
Skin sarcoidosis may include the following:
Roughly a quarter of people with sarcoidosis will develop skin problems related to the disease. Sarcoidosis can cause lumps, ulcers (sores), or areas of discolored skin. Often, these skin problems can indicate the seriousness of the case of sarcoidosis.
- Erythema nodosum, which causes raised, red, and tender bumps to form on the skin, usually on the front of the legs. Nearby joints are often swollen and painful. These areas may itch, but they don’t hurt. Erythema nodosum usually goes away on its own in six to eight weeks, even without treatment. Often, the presence of erythema nodosum is a good sign, indicating the type of sarcoidosis that also goes away on its own after a few months or years.
- A lower-extremity panniculitis with painful, erythematous nodules (often with Löfgren syndrome)
- Lupus pernio (the most specific associated cutaneous lesion). Lupus pernio, which is an uncommon serious skin condition that causes hard, reddish-purplish bumps to form on the cheeks, nose, nasal passages, lips, eyelids, fingers and/or ears. These bumps do not go away on their own and often come back when treatment is stopped. They are usually associated with chronic sarcoidosis. In some cases, the sores are disfiguring and can damage underlying cartilage and bone.
- Violaceous rash on the cheeks or nose (common)
- Maculopapular plaques (uncommon)
Other bumps on or under the skin, rashes, sores, scaling, and/or changes in old scars or tattoos that do not go away and are rarely painful or itchy. These skin problems are associated with the kind of sarcoidosis that lasts a long time.
Figure 3. Lupus pernio (cutaneous sarcoidosis)
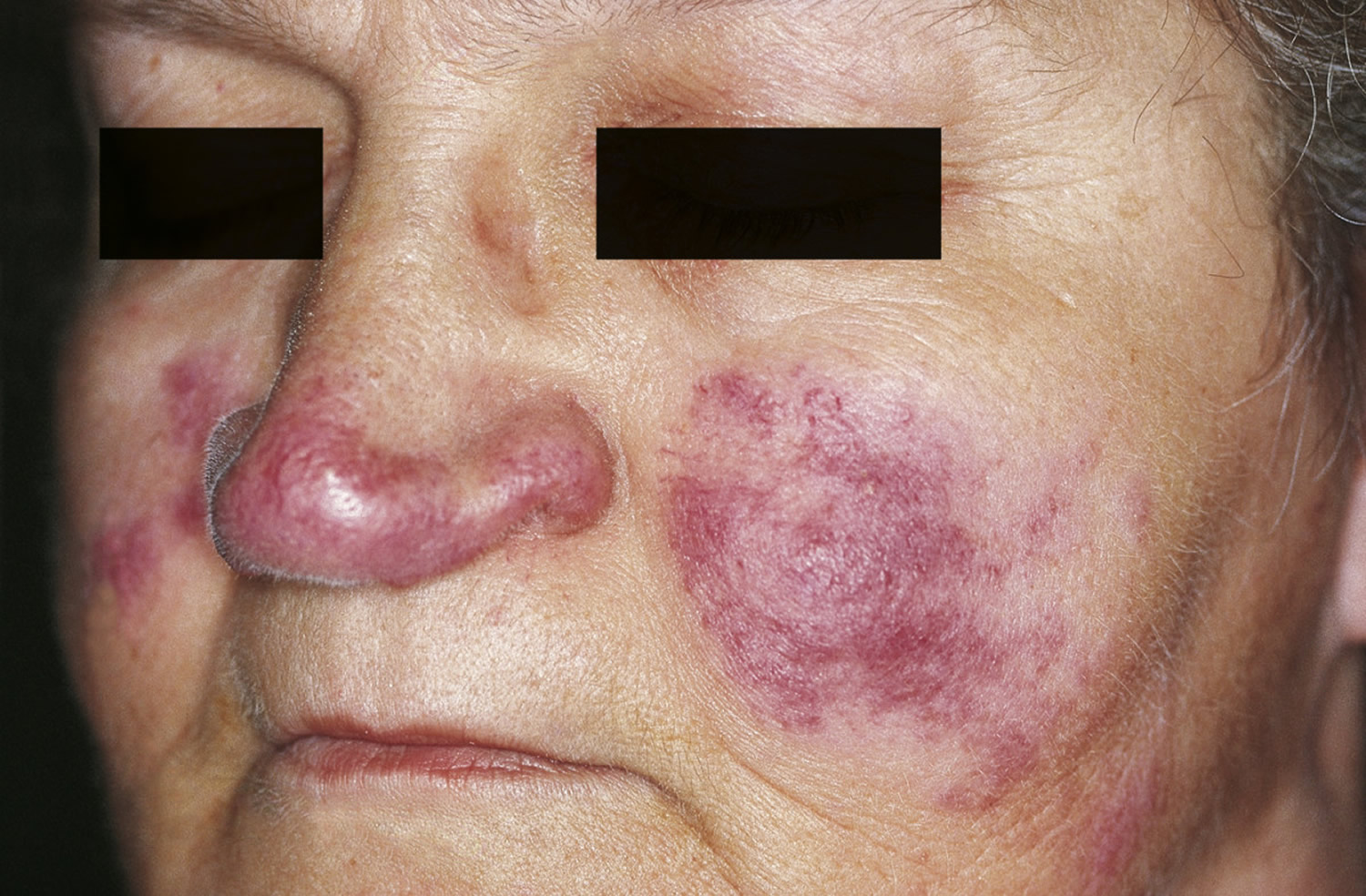
Figure 4. Erythema nodosum of sarcoidosis

Swollen or Enlarged Lymph Nodes
Sarcoidosis affects the lymph nodes in up to 90 percent of people with the disease. Sarcoidosis can cause enlarged lymph nodes that feel tender. Lymph nodes are glands found throughout the body that make and store white blood cells. When sarcoidosis inflammation targets these glands, they become enlarged. Swollen lymph nodes can be uncomfortable, but they rarely cause medical problems unless they press on organs or blood vessels.
Sarcoidosis usually affects the lymph nodes in your neck and chest. However, the disease also may affect the lymph nodes under your chin, in your armpits, or in your groin.
Most commonly, it is the lymph glands in the chest that are affected, but this can be hard to detect without an x-ray. Some of the other places affected by enlarged lymph nodes (they appear as swollen lumps) include:
- Neck
- Under the chin
- Armpit
- Groin
Unlike during a cold or the flu, swollen lymph nodes in these areas are not usually tender when associated with sarcoidosis.
Eye sarcoidosis
Sarcoidosis affects the eyes in a quarter or more of people with the disease. In many cases, these problems go away on their own within a year. Many eye problems are treatable with various options.
Eye symptoms can include:
- Burning, itching, and/or pain
- Dryness
- Tearing
- Red eyes
- Vision problems, such as seeing black spots or having blurred vision
- Sensitivity to light
- Small, pale yellow bumps on the eye
Eye problems caused by sarcoidosis might include:
- Uveitis (the most common eye problem), which is inflammation of the middle membrane – or the uvea – of the eye.
- Conjunctival lesions and scleral plaques
- Dry eye syndrome (also called keratoconjunctivitis), which occurs when the tear ducts are blocked by inflammation.
- Tear gland enlargement (also called lacrimal gland enlargement), which occurs when the tear glands are swollen by inflammation and granulomas.
- Glaucoma, cataracts, and blindness, which are rare but serious problems that can occur if uveitis goes untreated.
Cardiac sarcoidosis
Researchers estimate that sarcoidosis of the heart, or cardiac sarcoidosis, affects more than 10 percent of people with sarcoidosis in the United States, and perhaps as many as 25 percent. Because heart problems can be very serious, everyone who has sarcoidosis should be screened for cardiac sarcoidosis.
Some people with heart involvement might notice symptoms, but many people will feel no obvious effect, even in late-stage disease.
Heart symptoms might include:
- Irregular heartbeats, which can feel like palpitations and/or skipped beats
- Shortness of breath, coughing, chest tightness, and/or wheezing (although these symptoms can also be associated with lung problems)
- Swelling in the legs, which usually occurs only in late-stage sarcoidosis of
the heart - Feeling lightheaded or fainting
The problems caused by cardiac sarcoidosis can include:
- Arrhythmias, which are abnormal heartbeats or rhythms.
- Heart blocks, which are the blockage of electrical impulses that regulate the heart rate, impairing blood flow to the rest of the body.
- Heart failure, which occurs when the heart is unable to pump enough blood through the body, causing blood and fluid to back up in the lungs and elsewhere.
- Pericarditis, which although rare, can cause inflammation of the covering of the heart, as well as chest pain.
- Heart valve problems, which can prevent blood from flowing through the heart correctly.
- Heart attacks, which can occur when a blockage prevents blood and oxygen from reaching part of the heart.
Brain and Nervous System Sarcoidosis
Sarcoidosis affects the brain and nervous system in up to 15 percent of cases. Although it can affect almost any part of the nervous system, the cranial nerves, which are important nerves at the base of the brain, are commonly involved.
Brain and nervous system symptoms can include:
- Facial palsy (also called Bell’s palsy), which causes drooping and/or paralysis on one side of the face (the most common nervous system symptom)
- Headaches
- Eye pain and redness
- Blurry or double vision
- Blindness
- Weakness, numbness, tingling, and/or pain in the face, arms, and/or legs
- Arm and/or leg paralysis
- Seizures
- Behavior and mood changes, irritability, memory loss, and hallucinations (which are rare)
The problems caused by sarcoidosis of the nervous system can include:
- Nerve inflammation and/or damage, which results in many of the symptoms described above, depending on which nerves are affected. For example, facial palsy is a result of damage to a nerve or nerves at the base of the brain.
- Peripheral neuropathy, which is a condition that impairs the nerves’ ability to transmit messages between the brain and spinal cord and the rest of the body. It can cause the weakness and numbness described previously.
- Masses of granulomas in the meninges, or more rarely, in the brain, which cause the headaches, vision problems, and muscle weakness described previously. These masses can also cause meningitis, hydrocephalus, neuroendocrine disorders, and coma (see below).
- Meningitis, which is inflammation of the meninges, the membranes that surround your brain and spinal cord.
- Hydrocephalus, which is excess cerebrospinal fluid in the skull. It might occur with or after meningitis.
- Neuroendocrine disorders, which affect how the nervous and endocrine systems interact (the endocrine system makes and secretes hormones). When sarcoidosis damages an area at the base of the brain called the hypothalamus, it can lead to neuroendocrine disorders, such as hypopituitarism (an underactive pituitary gland).
- Coma, although this is rare.
Bones, Joints, and Muscles Sarcoidosis
Sarcoidosis affects the bones and joints in up to a third of people who have the disease. Granulomas can even form in the bone marrow, a problem that occurs in up to 10 percent of cases. Muscle symptoms are somewhat less common than bone symptoms.
Musculoskeletal symptoms might include:
- Early-onset arthritis, which causes joint pain, stiffness, and/or swelling that usually occurs in the first six months of the disease, begins suddenly in one or both of the ankles and/or feet, and sometimes involves the knees, toes, fingers, wrists, and/or elbow joints. It often accompanies erythema nodosum (described previously in SKIN), and it usually goes away on its own in a few weeks or months.
- Late-onset arthritis, which usually occurs six months or more after sarcoidosis develops, is less painful and affects fewer joints than early-onset arthritis (usually the knees and/or ankles, or sometimes the fingers or toes). It is often associated with chronic skin symptoms (described previously in SKIN) rather than erythema nodosum. This type of arthritis can last for a long time, a lifetime, or it may come and go. It usually does not go away for good without treatment like early-onset arthritis does. It can cause permanent joint damage and should be treated even when it is not painful.
- Bone cysts (which are rare)
- Muscle aches or muscle pain (also called myalgia)
- Muscle weakness
Problems caused by musculoskeletal sarcoidosis can include:
- Permanent bone and joint damage, which occurs from the formation of granulomas and cysts on the bones or from chronic arthritis. Such damage is rare, but when it does occur, it often affects the hands.
- Bone thinning (also called low bone density or osteopenia), which occurs when microscopic holes develop in the bones, making them weaker and more prone to fracture.
- Chronic myopathy, which is a general term for muscle weakness or muscle disease that lasts a long time or a lifetime. It is uncommon, but when it does occur, it is more likely to affect women.
Spleen sarcoidosis
The spleen is a large organ on the left side of the body under the ribs that produces and filters red blood cells and some types of white blood cells. Along with the lymph nodes, the spleen is part of the lymphatic system, which regulates blood cells and plays a role in immunity.
Sarcoidosis of the spleen does not usually cause symptoms, but possible symptoms may include:
- Pain on the upper left side under the ribs
- A sensation of pressure in the same area
- Feeling tired
Some of the problems sarcoidosis might cause when it affects the spleen include:
- Spleen enlargement (also called splenomegaly), which occurs when inflammation and the formation of granulomas cause the spleen to swell.
- Anemia, which occurs when blood does not contain enough healthy red blood cells to carry sufficient oxygen to the body’s tissues, and can cause fatigue.
- Leukopenia, which occurs when there are not enough white blood cells circulating through the body, and makes the body prone to infections.
- Thrombocytopenia, which occurs when the body does not have enough of the circulating blood platelets necessary for blood clotting.
Liver sarcoidosis
Between 50 and 80 percent of people with sarcoidosis develop granulomas in the liver. However, the disease rarely causes serious liver problems, and most people do not even realize when their liver is affected.
Liver symptoms may include:
- Fever
- Feeling tired or fatigued
- Itchy skin
- Jaundice, which causes skin and eyes to look somewhat yellow
- Pain on the upper right side under the ribs
The liver problems caused by sarcoidosis might include:
- Liver enlargement (also called hepatomegaly), which occurs when inflammation and granulomas on the liver cause it to swell.
- Abnormal liver enzyme levels, which is a common problem, but not usually a serious one.
- Portal hypertension, which is a rare complication defined as high blood pressure in the main blood vessel that carries blood to the liver. When pressure on this vein prevents normal blood flow, the blood must return to the heart through other blood vessels. These blood vessels become swollen and fragile due to the extra load.
- Cirrhosis, which is a rare condition that occurs when inflammation and granulomas scar the liver.
Kidneys and Urinary Tract Sarcoidosis
Sarcoidosis rarely attacks the kidneys directly. However, sarcoidosis can cause the body to overproduce vitamin D, which in turn causes the body to absorb too much calcium and can lead to kidney stones. Although they are uncommon in sarcoidosis, kidney stones can be painful when they break loose from the kidney and pass into the bladder, so patients are advised to be checked for excess calcium before kidney stones have the chance to develop.
Kidney and urinary tract symptoms include:
- Pain in the back or side, just under the ribs, which can be caused by large kidney stones.
- An increased urge to urinate, which is also caused by kidney stones.
Kidney problems caused by sarcoidosis might include:
- Too much calcium in the blood (also called hypercalcemia), which occurs in roughly 10 percent of people with sarcoidosis.
- Too much calcium in the urine (also called hypercalciuria), which occurs in roughly a third of people with sarcoidosis.
- Kidney stones, which are fairly uncommon.
- Loss of kidney function or kidney failure, which is often due to excessively high calcium levels in the blood or urine.
Salivary Glands Sarcoidosis
Sarcoidosis causes enlargement of the salivary glands in some people. This inflammation is sometimes painful and can cause dryness in the mouth. It can also make the cheeks look swollen. These symptoms are not serious, and they are usually treatable.
Sinuses Sarcoidosis
Sarcoidosis can also cause inflammation of the sinuses (called sinusitis). Symptoms include a runny nose, stuffiness, and sinus pain or headache. The sinusitis associated with sarcoidosis is often chronic and can be very troublesome, although it is rarely serious. Medication can relieve some of the symptoms.
Other Signs and Symptoms of Sarcoidosis
Because sarcoidosis can affect any organ in the body, a wide variety of symptoms can be seen, including:
- Fatigue
- Unexplained weight loss
- Night sweats
- Overall feeling of sickness
- Irregular heart beat
- Swollen legs
- Headaches
- Visual problems
- Weakness or numbness of an arm, leg, or part of the face
- Discoloration of the nose, cheeks, lips, and ears
- Scaly-appearing skin rash
- Joint pain
- Muscle swelling and soreness
- Arthritis
- Burning, itching, tearing, or pain in the eyes
- Red eyes
- Sensitivity to light
- Blurred vision
Note that this is not an all-encompassing list. There are many more signs and symptoms that can be seen in patients depending on the organs involved.
Sarcoidosis causes
The cause of sarcoidosis is unknown. More than one factor may play a role in causing the disease.
Some researchers think that sarcoidosis develops if your immune system responds to a trigger, such as bacteria, viruses, dust, or chemicals.
Normally, your immune system defends your body against foreign or harmful substances. For example, it sends special cells to protect organs that are in danger.
These cells release chemicals that recruit other cells to isolate and destroy the harmful substance. Inflammation occurs during this process. Once the harmful substance is gone, the cells and the inflammation go away.
In people who have sarcoidosis, the inflammation doesn’t go away. Instead, some of the immune system cells cluster to form lumps called granulomas in various organs in your body.
Genetics also may play a role in sarcoidosis. Researchers believe that sarcoidosis occurs if:
- You have a certain gene or genes that raise your risk for the disease
—And—
- You’re exposed to something that triggers your immune system
Triggers may vary depending on your genetic makeup. Certain genes may influence which organs are affected and the severity of your symptoms.
Researchers continue to try to pinpoint the genes that are linked to sarcoidosis.
What are the Risk Factors of sarcoidosis ?
Once thought rare, sarcoidosis is now known to be common and affects people worldwide. The disease can affect people of any age, race and gender. However, it is most common among adults between the ages of 20 and 40 and in certain ethnic groups. Disease severity can vary by race or ethnicity:
In the United States, it is most common in African Americans and people of European “particularly Scandinavian” descent.
Among African Americans, the most affected U.S. group, the estimated lifetime risk of developing sarcoidosis might be as high as 2 percent.
The disease is slightly more common in women than in men.
The disease manifests differently in different groups of people. While the lungs and lymph nodes are affected in almost everyone who has sarcoidosis, African Americans and people of Japanese descent are more likely to have eye involvement than Caucasians. On the other hand, skin lumps are most likely to affect people of Northern European descent, and those with a Japanese background seem prone to sarcoidosis-related heart problems.
Research also shows that risk appears to be elevated to some extent if someone in his or her close family has sarcoidosis, although researchers have not yet found a gene or genes linked to the development of sarcoidosis.
Diagnosis of sarcoidosis
Sarcoidosis is a diagnosis of exclusion, meaning that doctors will oftentimes have to rule out other possible diseases before confirming that your symptoms are caused by sarcoidosis. There is no objective test which can easily diagnose sarcoidosis. Numerous exams and tests are required to confirm your diagnosis and help your doctor decide on the best treatment options.
Your doctor will diagnose sarcoidosis based on your medical history, a physical exam, and test results. He or she will look for granulomas (inflamed lumps) in your organs. Your doctor also will try to rule out other possible causes of your symptoms.
Medical History
Your doctor may ask you detailed questions about your medical history. For example, he or she may ask whether you:
- Have a family history of sarcoidosis.
- Have had any jobs that may have raised your risk for the disease.
- Have ever been exposed to inhaled beryllium metal. (This type of metal is used to make aircrafts and weapons.)
- Have had contact with organic dust from birds or hay.
Exposure to beryllium metal and organic dust can cause inflamed lumps in your lungs that look like the granulomas from sarcoidosis. However, these lumps are signs of other conditions.
Physical Exam
Your doctor will check you for signs and symptoms of sarcoidosis. Signs and symptoms may include red bumps on your skin; swollen lymph nodes; an enlarged liver, spleen, or salivary glands; or redness in your eyes. Your doctor also will check for other causes of your symptoms.
Your doctor may listen to your lungs and heart. Abnormal breathing or heartbeat sounds could be a sign that sarcoidosis is affecting your lungs or heart.
Diagnostic Tests
You may have tests to confirm a diagnosis and to find out how sarcoidosis is affecting you. Tests include a chest x ray, lung function tests, biopsy, and other tests to assess organ damage.
Chest X Ray
A chest x ray is a painless test that creates pictures of the structures inside your chest, such as your heart and lungs. The test may show granulomas or enlarged lymph nodes in your chest. About 95 percent of people who have sarcoidosis have abnormal chest x rays.
Lung Function Tests
Lung function tests measure how much air you can breathe in and out, how fast you can breathe air out, and how well your lungs deliver oxygen to your blood. These tests can show whether sarcoidosis is affecting your lungs.
Biopsy
Your doctor may do a biopsy to confirm a diagnosis or rule out other causes of your symptoms. A biopsy involves taking a small sample of tissue from one of your affected organs.
Usually, doctors try to biopsy the organs that are easiest to access. Examples include the skin, tear glands, or the lymph nodes that are just under the skin.
If this isn’t possible, your doctor may use a positron emission tomography (PET) scan to pinpoint areas for biopsy. For this test, a small amount of radioactive substance is injected into a vein, usually in your arm.
The substance, which releases energy, travels through the blood and collects in organs or tissues. Special cameras detect the energy and convert it into three-dimensional (3D) pictures.
If lung function tests or a chest x ray shows signs of sarcoidosis in your lungs, your doctor may do a bronchoscopy to get a small sample of lung tissue.
During this procedure, a thin, flexible tube is passed through your nose (or sometimes your mouth), down your throat, and into the airways to reach your lung tissue. Medication will be used to numb your throat before the procedure, and you will be given medication to help you relax.
Other Tests To Assess Organ Damage
You also may have other tests to assess organ damage and find out whether you need treatment. For example, your doctor may recommend blood tests and/or an EKG (electrocardiogram).
Blood tests: Many people with sarcoidosis make excess amounts of vitamin D and/or a chemical called angiotensin-converting enzyme. Blood tests can be used to detect high levels of these substances. However, other conditions also cause elevated levels of vitamin D and angiotensin-converting enzymes, so these tests cannot be used to diagnose sarcoidosis. Blood tests can also be used to check blood levels and to look for evidence of liver or kidney damage.
MRI (magnetic resonance imaging): Like x-rays and CT scans, MRI tests provide a glimpse inside the body. MRIs can be used to look for signs of sarcoidosis in the brain, spinal cord, heart, bones, and other organs.
Nuclear imaging: These tests use radioactive dye to help clinicians see blood flow through various body organs. The dye is injected into your veins before the scan. After a period of time, your body is scanned with a special camera that can detect the radiation from the dye. Nuclear imaging tests are sometimes used to help diagnose sarcoidosis of the heart.
Heart rhythm monitoring: Your health care provider may use electrocardiography (often called ECG or EKG) to get information about the functioning of your heart. Up to 50 percent of people with sarcoidosis will have an abnormal EKG, so additional testing might be needed to see whether the changes are worrisome.
Echocardiogram: An echocardiogram is an ultrasound of the heart. It uses ultrasound waves to look at the heart. (Pregnancy ultrasounds use the same technology to provide a look at the fetus.) Your health care provider might order an echocardiogram to see how the heart is pumping blood.
If you’re diagnosed with sarcoidosis, you should see an ophthalmologist (eye specialist), even if you don’t have eye symptoms. In sarcoidosis, eye damage can occur without symptoms.
Sarcoidosis treatment
Not everyone who has sarcoidosis needs treatment. Sometimes the disease goes away on its own. Whether you need treatment and what type of treatment you need depend on your signs and symptoms, which organs are affected, and whether those organs are working well.
If the disease affects certain organs—such as your eyes, heart, or brain—you’ll need treatment even if you don’t have any symptoms.
In either case, whether you have symptoms or not, you should see your doctor for ongoing care. He or she will want to check to make sure that the disease isn’t damaging your organs. For example, you may need routine lung function tests to make sure that your lungs are working well.
If the disease isn’t worsening, your doctor may watch you closely to see whether the disease goes away on its own. If the disease does start to get worse, your doctor can prescribe treatment.
The goals of treatment include:
- Relieving symptoms
- Improving organ function
- Controlling inflammation and reducing the size of granulomas (inflamed lumps)
- Preventing pulmonary fibrosis (lung scarring) if your lungs are affected
Your doctor may prescribe topical treatments and/or medicines to treat the disease.
Medications
Prednisone
Prednisone, a type of steroid, is the main treatment for sarcoidosis. This medicine reduces inflammation. In most people, prednisone relieves symptoms within a couple of months.
Although most people need to take prednisone for 12 months or longer, your doctor may lower the dose within a few months after you start the medicine.
Long-term use of prednisone, especially at high doses, can cause serious side effects. Work with your doctor to decide whether the benefits of this medicine outweigh the risks. If your doctor prescribes this treatment, he or she will find the lowest dose that controls your disease.
When you stop taking prednisone, you should cut back slowly (as your doctor advises). This will help prevent flareups of sarcoidosis. Cutting back slowly also allows your body to adjust to not having the medicine.
If a relapse or flareup occurs after you stop taking prednisone, you may need a second round of treatment. If you remain stable for more than 1 year after stopping this treatment, the risk of relapse is low.
Other Medicines
Other medicines, besides prednisone, also are used to treat sarcoidosis. Examples include:
- Hydroxychloroquine or chloroquine (known as antimalarial medicines). These medicines work best for treating sarcoidosis that affects the skin or brain. Your doctor also may prescribe an antimalarial if you have a high level of calcium in your blood due to sarcoidosis.
- Medicines that suppress the immune system, such as methotrexate, azathioprine, or leflunomide. These medicines work best for treating sarcoidosis that affects your lungs, eyes, skin, or joints.
Your doctor may prescribe these medicines if your sarcoidosis worsens while you’re taking prednisone or if you can’t handle prednisone’s side effects.
If you have Lofgren’s syndrome with pain or fever, your doctor may prescribe nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen.
If you’re wheezing and coughing, you may need inhaled medicine to help open your airways. You take inhaled medicine using an inhaler. This device allows the medicine to go straight to your lungs.
Anti-tumor necrosis factor drugs, originally developed to treat arthritis, are being studied to treat sarcoidosis.
Ongoing Research
Researchers continue to look for new and better treatments for sarcoidosis. They’re currently studying treatments aimed at the immune system. Researchers also are studying antibiotics as a possible treatment for sarcoidosis that affects the skin.
Complications of sarcoidosis
There are a few complications that can result from ongoing inflammation, including those directly related to the formation of granulomas within endocrine glands. They include:
- Hypercalcaemia (too much calcium in the blood) and Hypercalciuria (too much calcium in urine) – The incidence of hypercalcaemia is estimated to be 10% in sarcoidosis patients, with no association with a specific demographic. The severity depends on many factors, including disease activity, sunlight, and diet variations. Hypercalciuria on the other hand is estimated to be three times more common and seen more often in men than women. If left untreated, elevated levels of calcium in the blood or urine can cause potentially severe complications including bone loss, osteoporosis (week or brittle bones, especially with long-term treatment with steroids), and long-term kidney and pancreas complications. While the mechanism is not fully understood, treatment for high levels of calcium in the blood or urine include corticosteroids (first-line treatment), ketoconazole, chloroquine, hydroxcloroquine, and other drugs, including diuretics. Ongoing monitoring of calcium levels is needed to ensure the condition does not worsen and to ensure any side effects of medications do not cause further complications.
- Suppressed Parathyroid Hormone (PTH) – PTH is released by four small glands in the neck when vitamin D metabolites and low levels of calcium are detected in the blood. It is responsible for controlling the levels of ionized calcium and fluid in the blood. Elevated levels of calcium in the blood blocks the release of PTH. Since sarcoidosis patients commonly have high levels of calcium in the blood and therefore suppressed release of PTH, physicians should be suspicious that their patient also suffers from hyperthyroidism when PTH levels are high.
- Vitamin D Dysregulation – Patients who suffer from sarcoidosis often have elevated levels of vitamin D in their blood, believed to be part of the immune response in the condition. However, there are two forms of vitamin D, the active and inactive forms. In doing routine blood work, many physicians will notice that the levels of the active form of vitamin D are low in sarcoidosis patients. To address this perceived issue, patients are often prescribed a supplement to increase the levels of the active form in their system resulting in kidney stones. In order to appropriately determine if a supplement is needed, the physician needs to run more extensive blood work, measuring both the active and inactive forms of vitamin D. Studies have shown that in the majority of cases, no supplementation is required.
Complications in Sarcoidosis Affecting the Eyes
- Cataract Formation – A well recognized complication of uveitis with an estimated 14-30% of patients affected, cateract occurs either as a result of inflammation or treatment with steroids. In general, cataract surgery is the recommended treatment with good outcomes, provided that inflammation is controlled after surgery and there is no permanent damage due to structural abnormalities or glaucoma.
- Glaucoma – Describing increased pressure within the eyeball due to damage of the optic nerve, this condition can result in gradual loss of sight or total blindness. Treatment with corticosteroids is often to blame. It is recommended that sarcoidosis patients have regular appointment with an ophthalmologist (twice a year) to ensure that sarcoidosis affecting the eye and systemic treatments do not cause complications.
Living With Sarcoidosis
Sarcoidosis has no cure, but you can take steps to manage the disease. Get ongoing care and follow a healthy lifestyle. Talk with your doctor if you’re pregnant or planning a pregnancy.
Ongoing Care
Ongoing care is important, even if you don’t take medicine for your sarcoidosis. New symptoms can occur at any time. Also, the disease can slowly worsen without your noticing.
How often you need to see your doctor will depend on the severity of your symptoms, which organs are affected, which treatments you’re using, and whether you have any side effects from treatment. Even if you don’t have symptoms, you should see your doctor for ongoing care.
Your doctor may recommend routine tests, such as lung function tests and eye exams. He or she will want to check to make sure that the disease isn’t damaging your organs.
Discuss with your doctor how often you need to have followup visits. You may have some followup visits with your primary care doctor and others with one or more specialists.
Make sure to take all of your medicines as your doctor prescribes.
Lifestyle Changes
Making lifestyle changes can help you manage your health. For example, follow a healthy diet and be as physically active as you can. A healthy diet includes a variety of fruits, vegetables, and whole grains.
It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, trans fat, cholesterol, sodium (salt), and added sugar.
If you smoke, quit. Talk with your doctor about programs and products that can help you quit. Also, try to avoid other lung irritants, such as dust, chemicals, and secondhand smoke.
If you have trouble quitting smoking on your own, consider joining a support group. Many hospitals, workplaces, and community groups offer classes to help people quit smoking.
Emotional Issues
Living with sarcoidosis may cause fear, anxiety, depression, and stress. Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to living with sarcoidosis. You can see how other people who have the same symptoms have coped with them. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve stress and anxiety. Let your loved ones know how you feel and what they can do to help you.
Pregnancy
Many women who have sarcoidosis give birth to healthy babies. Women who have severe sarcoidosis, especially if they’re older, may have trouble becoming pregnant. Sometimes sarcoidosis may get worse after the baby is delivered.
If you have sarcoidosis and are pregnant or planning a pregnancy, talk with your doctor about the risks involved. Also, if you become pregnant, it’s important to get good prenatal care and regular sarcoidosis checkups during and after pregnancy.
Some sarcoidosis medicines are considered safe to use during pregnancy; others are not recommended.
- What is Sarcoidosis? https://www.stopsarcoidosis.org/what-is-sarcoidosis/[↩]
- Sarcoidosis. https://www.nhlbi.nih.gov/health/health-topics/topics/sarc[↩]
- What Is Sarcoidosis? https://www.nhlbi.nih.gov/health/health-topics/topics/sarc[↩]
- Sarcoidosis. https://emedicine.medscape.com/article/301914-overview[↩][↩]
- Nardi A, Brillet PY, Letoumelin P, Girard F, Brauner M, Uzunhan Y, et al. Stage IV sarcoidosis: comparison of survival with the general population and causes of death. Eur Respir J. 2011 Dec. 38(6):1368-73.[↩]
- Swigris JJ, Olson AL, Huie TJ, Fernandez-Perez ER, Solomon J, Sprunger D. Sarcoidosis-related mortality in the United States from 1988 to 2007. Am J Respir Crit Care Med. 2011 Jun 1. 183(11):1524-30.[↩]