Contents
What is a schwannoma
Schwannoma is a benign, slow‐growing, solitary tumor of the nerve sheath that covers nerves, called the Schwann cell 1. Schwannomas were first described by Verocay in 1908 2 and have since been given several names although schwannoma and neurilemmoma are the most common terms.
A schwannoma typically comes from a single bundle (fascicle) within the main nerve and displaces the rest of the nerve. When a schwannoma grows larger, more fascicles are affected, making removal more difficult. In general, a schwannoma grows slowly.
It is estimated that 25%–45% of all schwannoma variants occur in the head and neck, generally presenting in the fourth decade of life 3. The nerves most commonly involved in schwannomas of the head and neck are the vagus and the cervical sympathetic chain 4. The most common type of schwannoma is a vestibular schwannoma. It affects the nerve responsible for balance (also called the vestibular nerve).
It can cause inner ear deafness because the hearing and balance nerve run together, and as the tumor grows it damages the hearing nerve (cochlear nerve). Because of this doctors used to call them acoustic neuromas.
When schwannomas are cancerous they are called malignant schwannomas. They are also called malignant peripheral nerve sheath tumors or neurofibrosarcomas.
Schwannomas can start anywhere in the body.
The most common areas are:
- the major nerve of the leg (the sciatic nerve)
- the nerves at the top of the arm (the brachial plexus)
- the lower back (the network of nerves called the sacral plexus).
If you develop a schwannoma in an arm or leg, you may notice a painless lump. Schwannomas are rarely cancerous, but they can lead to nerve damage and loss of muscle control. See your doctor if you have any unusual lumps or numbness.
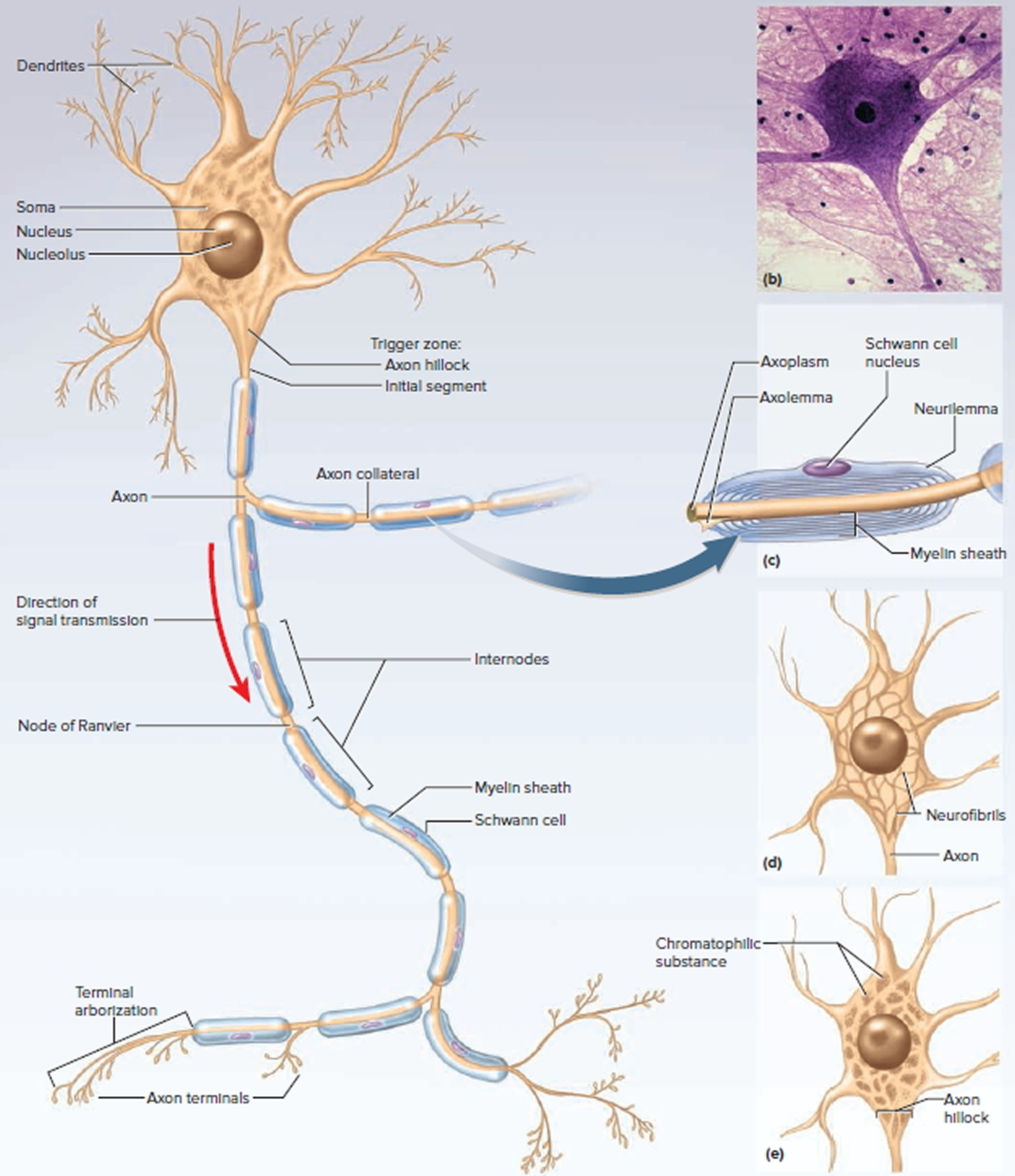
Figure 1. General structure of a neuron
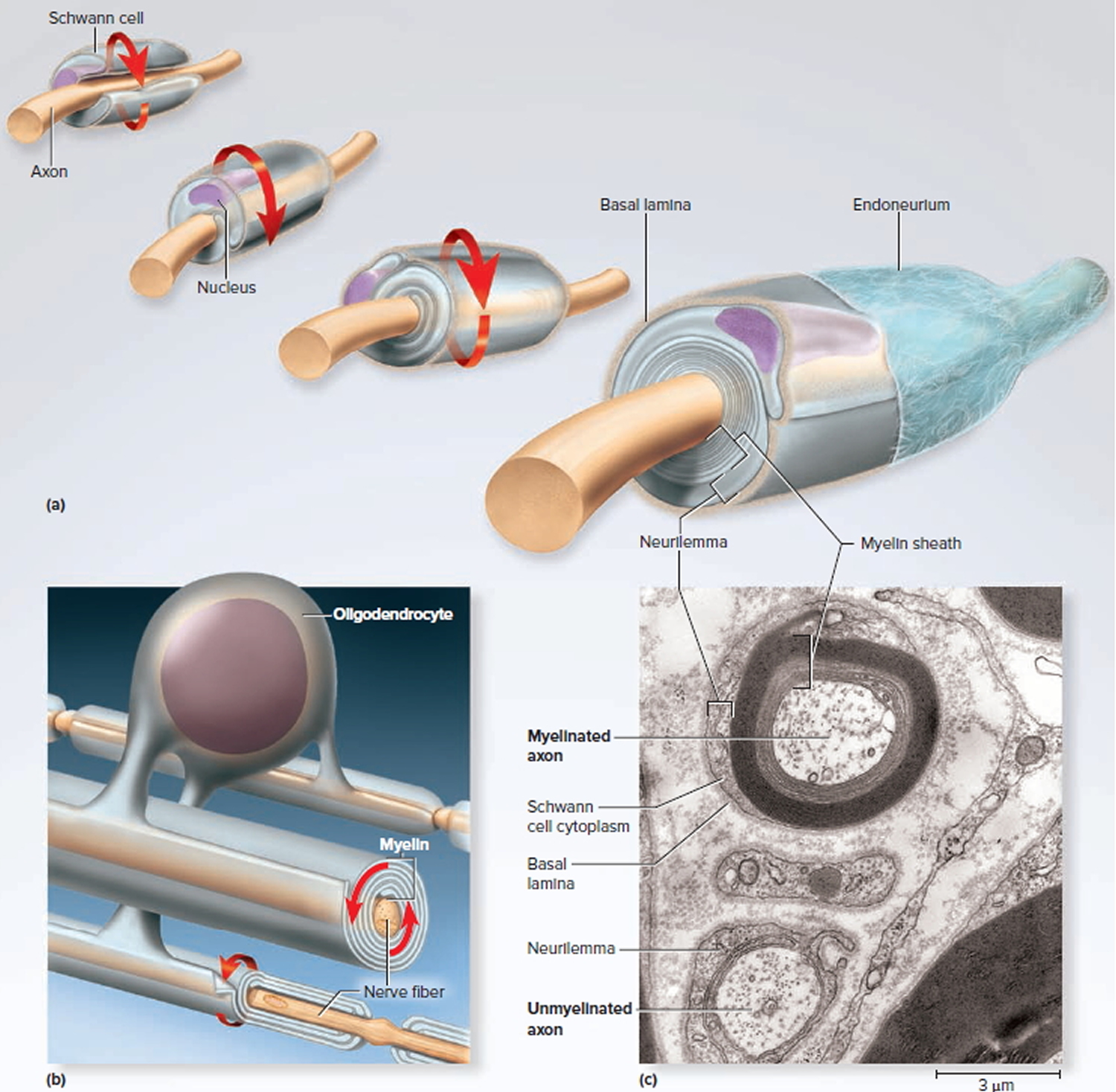
Figure 2. Myelination
Note: (a) A Schwann cell of the peripheral nervous system, wrapping repeatedly around an axon to form the multilayered myelin sheath.
The myelin spirals outward away from the axon as it is laid down.
(b) An oligodendrocyte of the central nervous system (brain and spinal cord) wrapping around the axons of multiple neurons. Here, the myelin spirals inward toward the axon as it is laid down.
(c) A myelinated axon (top) and unmyelinated axon (bottom).
Vestibular schwannoma
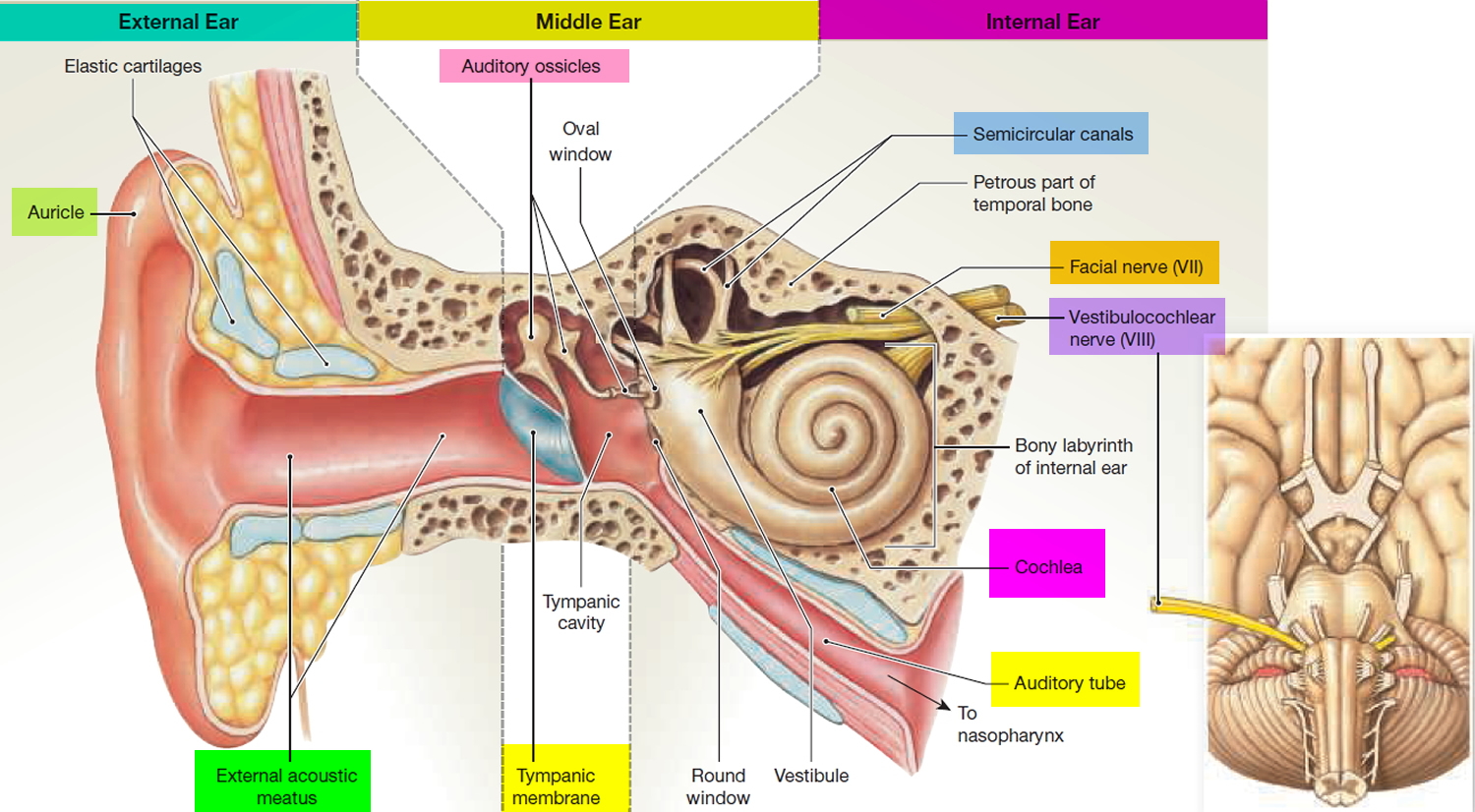
Vestubular schwannoma (acoustic schwannoma) starts in the Schwann cells (fatty cells) on the outside of the 8th cranial nerve (also known as the acoustic or vestibulocochlear nerve). Vestubular schwannomas are also called acoustic neuromas. Branches of the vestibular nerve directly influence your balance and hearing, and pressure from an acoustic neuroma can cause hearing loss, ringing in your ear and unsteadiness.
Acoustic neuroma usually arises from the Schwann cells covering this nerve and grows slowly or not at all. Rarely, it may grow rapidly and become large enough to press against the brain and interfere with vital functions.
It is estimated that the instances of acoustic schwannoma are between 1 to 3.5 in every 100,000.
Vestubular schwannomas are nearly always slow growing, do not spread, and are thought of as benign tumors. Often they have been there a long time by the time they are diagnosed.
Vestibular schwannomas are found most often in older people. Loss of hearing in one ear can be a sign of vestibular schwannoma.
Rarely, they are associated with a genetic condition called neurofibromatosis. People with neurofibromatosis are usually diagnosed at a much younger age and tumors might be on both sides of the brain (bilateral). Those affected might also develop another type of brain tumor called meningiomas.
Types of acoustic schwannoma
- Unilateral (one side) occurs spontaneously without any evidence of family history, accounts for 95% of vestubular schwannomas
- Bilateral (both sides) is most likely caused by a genetic condition called Neurofibromatosis Type 2 (NF2) which affects approximately 1 in every 40,000 people. Neurofibromatosis Type 2 will be suspected if a parent/sibling/child of the patient has Neurofibromatosis Type 2 and acoustic neuroma occurs before age 30 or if the patient has had a meningioma, glioma, or cataract.
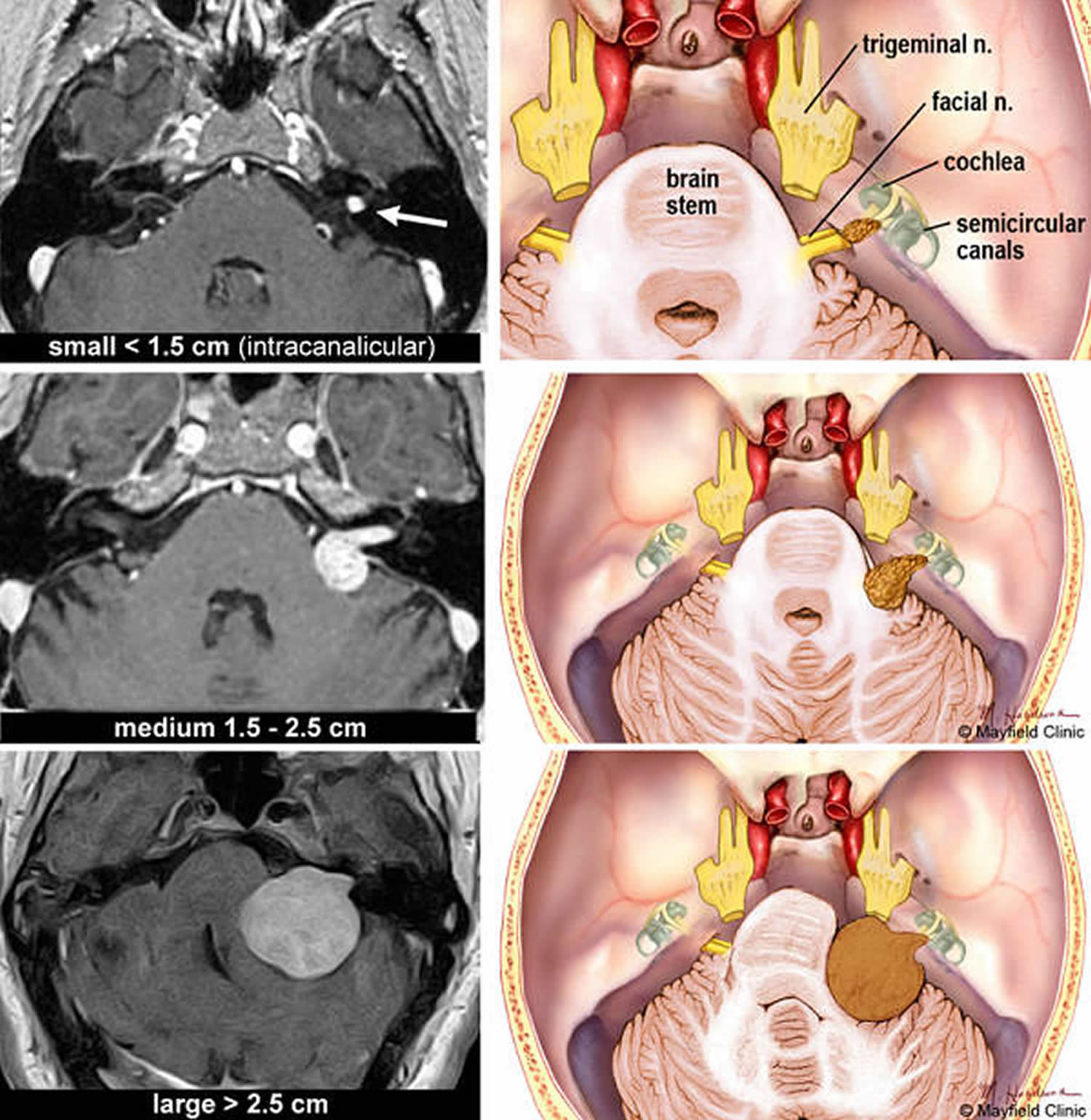
Treatment will depend on the size of your tumor.
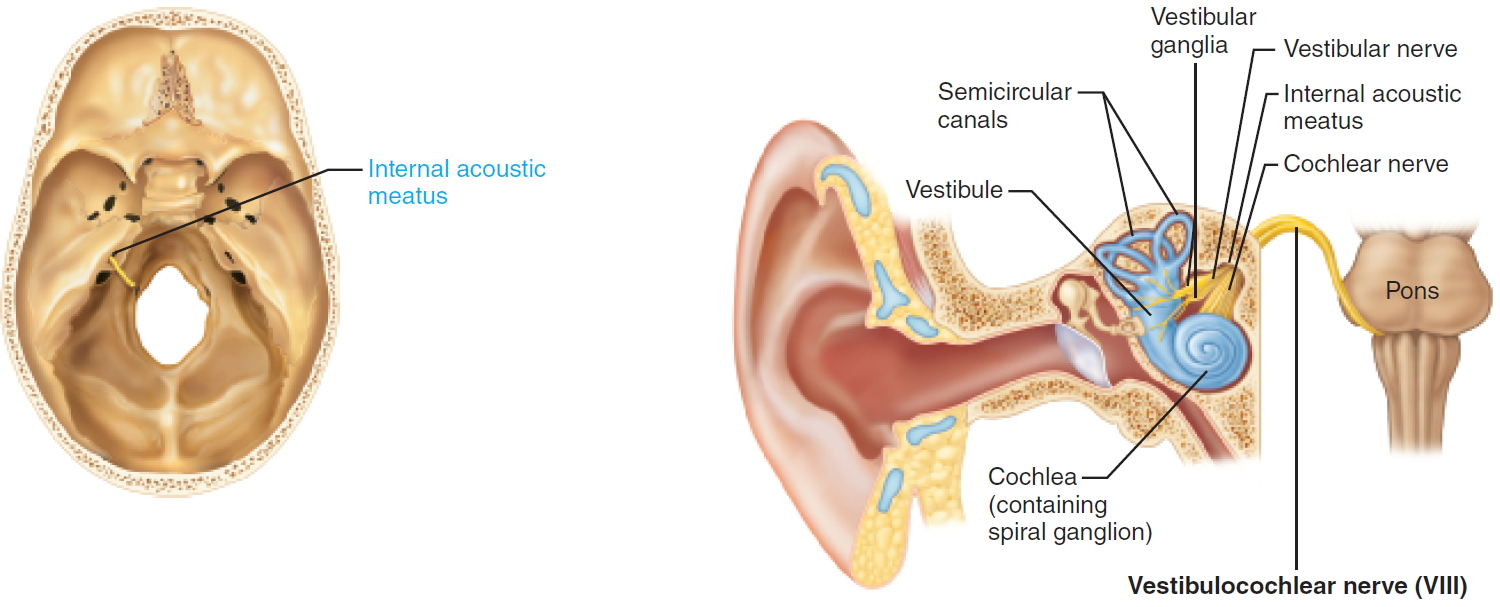
Figure 3. Vestibulocochlear nerve (Cranial nerve 8)
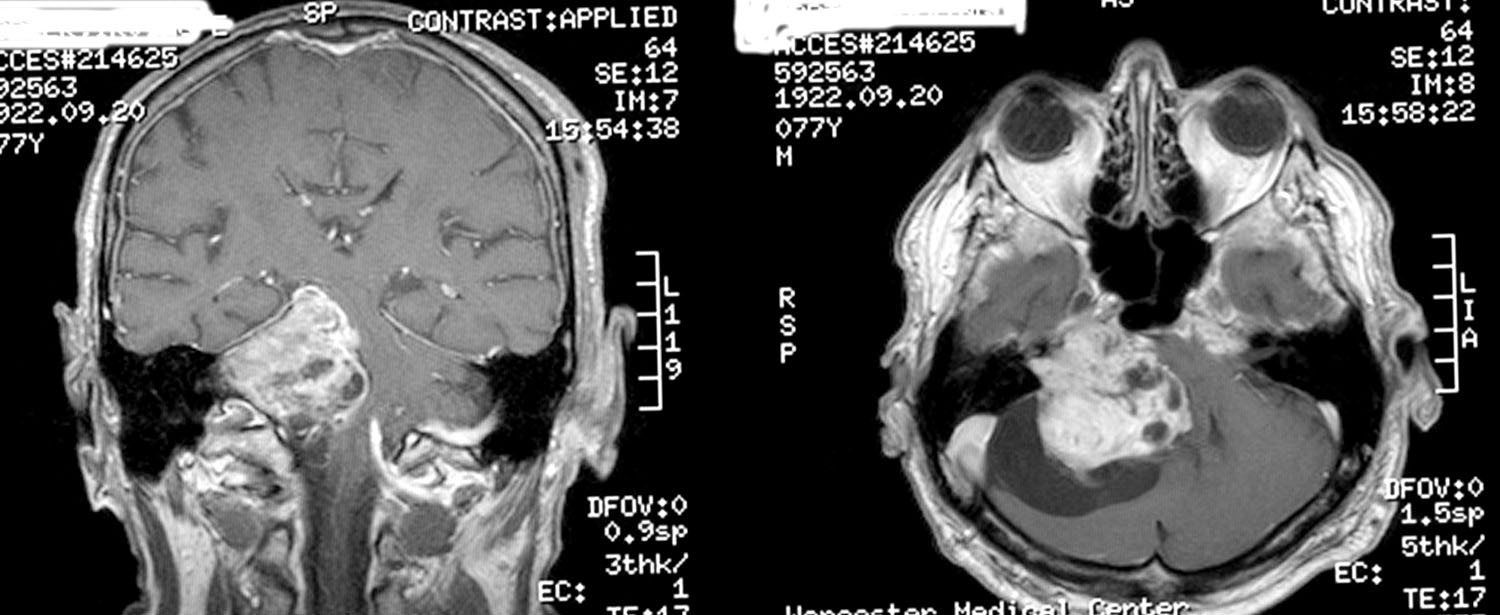
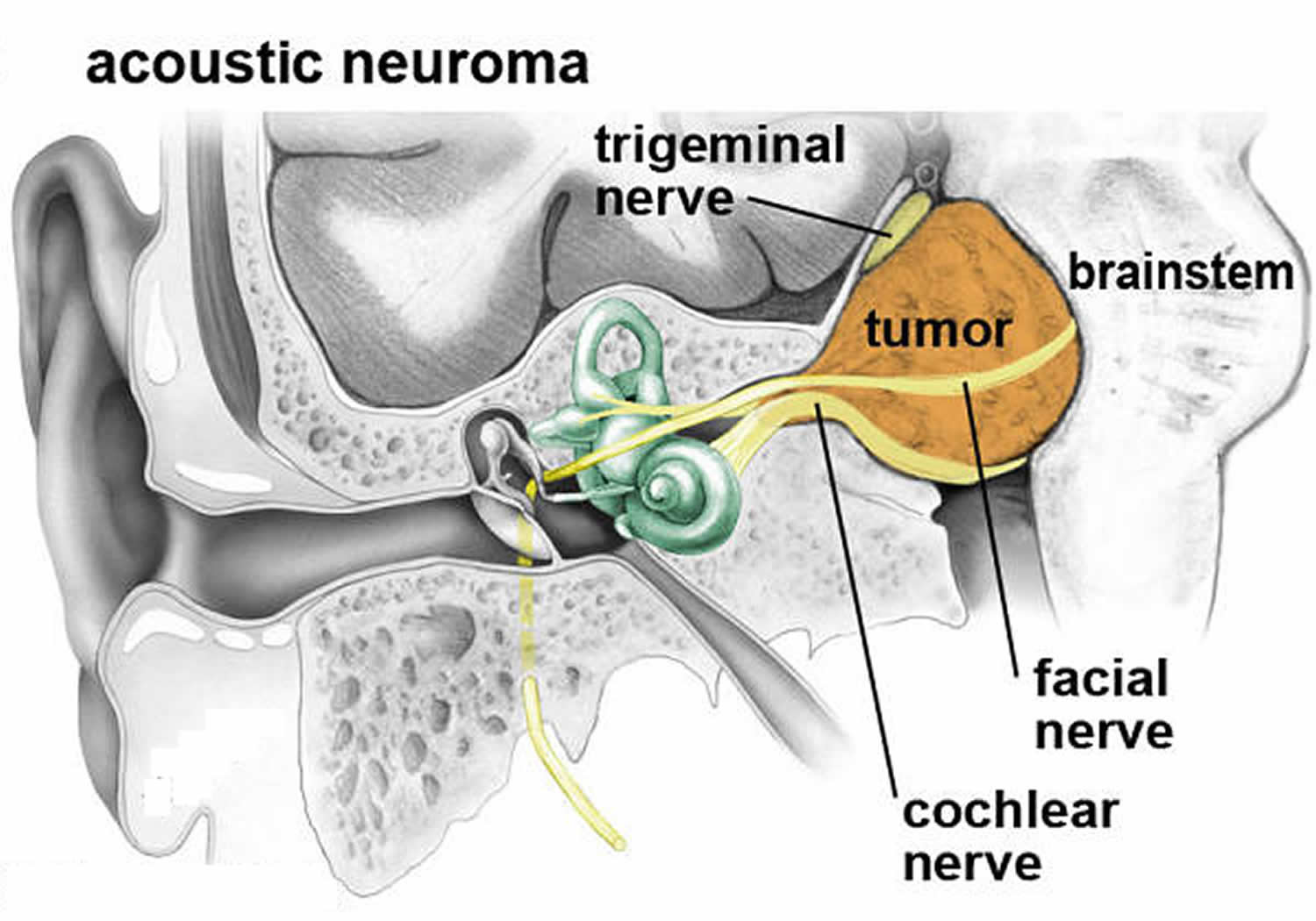
Figure 4. Vestubular schwannoma
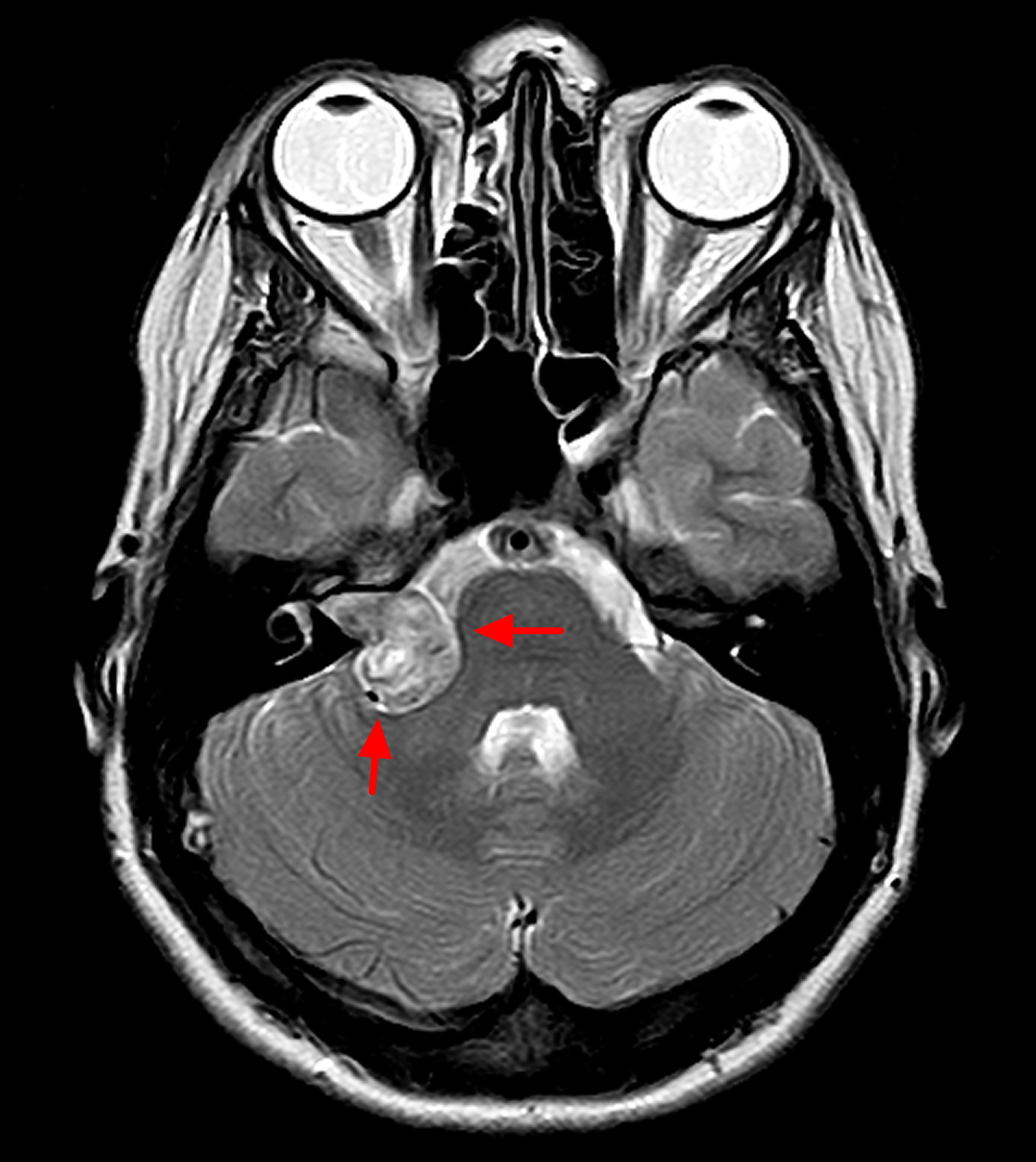
Figure 5. Vestubular schwannoma (there is a complex mass based within the right cerebellar-pontine angle, with widening of the right internal auditory canal, involvement of both cochlear and vestibular branches of cranial nerve VIII)
Vestubular schwannoma causes
The cause of vestubular schwannoma or acoustic neuroma is usually not known. A few people who have an vestubular schwannoma also have a rare inherited condition called neurofibromatosis type 2. In neurofibromatosis type 2, the acoustic neuromas appears to be a malfunctioning gene on chromosome 22. Normally, this gene produces a tumor suppressor protein that helps control the growth of Schwann cells covering the nerves. But for most people, there is no obvious cause.
Risk factors for vestubular schwannoma
The only confirmed risk factor for acoustic neuroma is having a parent with the rare genetic disorder neurofibromatosis type 2. But neurofibromatosis type 2 only accounts for about 5 percent of acoustic neuroma cases.
A hallmark characteristic of neurofibromatosis type 2 is the development of noncancerous tumors on the balance nerves on both sides of your head, as well as on other nerves.
Neurofibromatosis type 2 (NF2) is known as an autosomal dominant disorder, meaning that the mutation can be passed on by just one parent (dominant gene). Each child of an affected parent has a 50-50 chance of inheriting it.
Vestibular schwannoma symptoms
Usually vestubular schwannomas (acoustic neuromas) grow very slowly and the signs and symptoms of acoustic neuroma are often subtle and may take many years to develop. This means there may not be any symptoms in the early stages when the tumor is small.
Many people say they notice some loss of hearing and tinnitus, or ringing in the ears. Usually one ear is affected, but both ears can be involved if the person has neurofibromatosis type 2. Pressure from the tumor on adjacent nerves controlling facial muscles and sensation (facial and trigeminal nerves), nearby blood vessels, or brain structures may also cause problems.
Whether or not there are any other symptoms can depend on the size of the tumor and how hard it presses on the eighth cranial nerve. Some people with an vestubular schwannoma get:
- Hearing loss, usually gradual — although in some cases sudden — and occurring on only one side or more pronounced on one side
- Ringing (tinnitus) in the affected ear
- Dizziness or vertigo, which is a feeling that the space around you is spinning
- Loss of balance
- Headache
- Facial numbness or tingling.
In rare cases, an acoustic neuroma may grow large enough to compress the brainstem and become life-threatening.
Vestubular schwannoma complications
An acoustic neuroma may cause a variety of permanent complications, including:
- Hearing loss
- Facial numbness and weakness
- Difficulties with balance
- Ringing in the ear
Some symptoms of an acoustic schwannoma can be difficult to live with and may affect your quality of life. For example, hearing impairment may have an impact on your job and communication may be more difficult. Severe dizziness and loss of balance may also affect your job and limit the activities you can do.
Speak to your doctor or specialist if your acoustic schwannoma is being monitored but you feel the symptoms are significantly affecting your daily life. There may be ways of easing your symptoms, such as using a hearing aid or painkilling medication, or you may need treatment to remove the tumor.
Large tumors may press on your brainstem, preventing the normal flow of fluid between your brain and spinal cord (cerebrospinal fluid). In this case, fluid can build up in your head (hydrocephalus), increasing the pressure inside your skull.
Recurrence
Occasionally, acoustic schwannomas return after being removed. The tumors reoccur in less than five in every 100 people who have surgery to remove them.
It’s likely that you’ll need to have magnetic resonance imaging (MRI) scans over a number of years, regardless of which treatment you have.
Hydrocephalus
One of the most serious complications of acoustic schwannoma is a condition called hydrocephalus.
Hydrocephalus occurs when an acoustic schwannoma is very large and presses on your brainstem (the lowest part of the brain that connects to the spinal cord).
This prevents the cerebrospinal fluid (CSF) from flowing between your brain and spinal cord. The blockage can cause pressure to build up inside your skull, which in turn puts pressure on the delicate tissues in your brain.
Hydrocephalus can be treated by draining away the excess CSF. It’s important that it’s treated quickly because in severe cases it can cause brain damage. In rare cases, hydrocephalus can be fatal.
Vestubular schwannoma diagnosis
Acoustic neuroma is often difficult to diagnose in the early stages because signs and symptoms may be subtle and develop gradually over time. Common symptoms such as hearing loss are also associated with many other middle and inner ear problems.
If your doctor suspects you have acoustic schwannoma, they might send you for tests such as hearing tests and magnetic resonance imaging, or MRI. An MRI allows your doctor to see if there’s a tumor, and its size and position if there is one.
- Hearing test (audiometry). In this test, conducted by a hearing specialist (audiologist), you hear sounds directed to one ear at a time. The audiologist presents a range of sounds of various tones and asks you to indicate each time you hear the sound. Each tone is repeated at faint levels to find out when you can barely hear. The audiologist may also present various words to determine your hearing ability.
- Imaging. Magnetic resonance imaging (MRI) is the preferred imaging test to confirm the presence of acoustic neuroma and can detect tumors as small as 1 to 2 millimeters in diameter. If MRI is unavailable or you can’t tolerate an MRI scan, computerized tomography (CT) may be used, but it may miss very small tumors.
Acoustic schwannoma treatment
Your acoustic neuroma treatment may vary, depending on the size and growth of the acoustic neuroma, your overall health, and if you’re experiencing symptoms. To treat acoustic neuroma, your doctor may suggest one or more of three potential treatment methods: monitoring, surgery or radiation therapy.
The options for treatment include:
- no treatment – just monitoring the tumor growth and related symptoms
- surgery – to cut out the tumor
- stereotactic treatment – this procedure sends focused radiation to the tumor to stop it from growing.
Which treatment you have depends on the size and location or the tumor, your symptoms, your age and general health, and what you want.
Even though acoustic neuromas are not cancerous, they can cause serious, permanent damage to nerves. If you have any of the symptoms listed above, see your doctor as soon as possible.
Monitoring
If you have an acoustic schwannoma that’s very small or growing very slowly, you may not need to have any immediate treatment. Instead, your condition will be carefully monitored.
Research suggests that up to three-quarters of acoustic schwannomas don’t appear to be growing, so monitoring the tumor is all that’s needed.
Simply monitoring an acoustic schwannoma is often the best option because the risks associated with surgery or radiosurgery (see below) outweigh the risk of the tumor having an adverse effect on your health.
Your doctor may recommend that you have regular imaging and hearing tests, usually every six to 12 months, to determine whether the tumor is growing and how quickly.
To help monitor your condition, you’ll need to have regular magnetic resonance imaging (MRI) scans (where a magnetic field and radio waves are used to create an image of the inside of your body). The MRI scan will be used to check the size and growth of your acoustic schwannoma.
Other treatments may be considered if the tumor shows any signs of growing or if there’s a risk of it significantly affecting your health.
You may need to have an MRI scan every one to two years, although this will depend on your general health and the size of your tumor.
Vestibular schwannoma surgery
You may need surgery to remove an acoustic neuroma. Your surgeon may use one of several techniques for removing an acoustic neuroma, depending on the size of your tumor, hearing status and other factors.
The goal of surgery is to remove the tumor, preserve the facial nerve to prevent facial paralysis and preserve hearing when possible.
Surgery for an acoustic neuroma is performed under general anesthesia and involves removing the tumor through the inner ear or through a window in your skull.
The entire tumor may not be able to be completely removed in certain cases. For example, if the tumor is too close to important parts of the brain or the facial nerve.
Sometimes, surgical removal of the tumor may worsen symptoms if the hearing, balance or facial nerves are damaged during the operation.
Complications may include:
- Leakage of cerebrospinal fluid (CSF) through the wound
- Hearing loss
- Facial weakness
- Facial numbness
- Ringing in the ear
- Balance problems
- Persistent headache
- Infection of the cerebrospinal fluid (meningitis)
- Stroke or brain bleeding
Microsurgery
Microsurgery can be used to remove an acoustic schwannoma. The surgery will be carried out under general anesthetic and the acoustic schwannoma will be removed through an incision made in your skull.
Small acoustic schwannomas can usually be completely removed. If you have a large tumor, a small part will occasionally be left behind to minimize the risk of damaging the facial nerve, which runs next to the acoustic nerve.
If a small part of the tumor remains, it can either be monitored with MRI scans or effectively treated using radiosurgery (see below).
- Hearing loss
After surgery to remove an acoustic schwannoma, hearing in the ear affected by the tumor is almost always lost.
You may wish to discuss the possibility of having a ‘bone anchored hearing aid’ with your ENT (ear, nose and throat) surgeon, which will help divert sound from your affected ear to your good ear.
- Facial nerve damage
Surgery can occasionally damage the facial nerve (cranial nerve 7). This is because the acoustic nerve is very close to the facial nerve and large tumors are often stuck to it. Your surgeon will try not to damage your facial nerve and with large tumors will sometimes leave a small part of the tumor on the facial nerve to try to preserve it.
If your facial nerve is damaged during surgery you may find that:
- your face droops on one side (facial palsy)
- you drool saliva on the weak side of your face
- you have difficulty closing your eye on the weak side of your face
- your speech is less clear
These symptoms may improve within six to 12 months of having surgery and be helped with physiotherapy. However, it’s important to be aware that some damage to your facial nerve may be permanent.
Facial nerve damage can also affect your eyes. For example, you may find it difficult to blink or close your eye completely on the side that was operated on. As a result, your eye may dry out and you may need to use artificial tears (eye lubricant).
In cases where the tumor is small, less than one in every 100 people’s facial nerve will be badly affected after treatment.
For large tumors, around three in 10 people will have permanent, severe facial nerve weakness after surgery if a complete tumor removal is attempted. This falls to around one person in over 100 if a small part of the tumor is left on the facial nerve to preserve it.
Any minor post-surgery facial nerve weakness is likely to be temporary, although it may take several months to recover.
Recovery from surgery
Following surgery, you’ll usually need to spend up to a week in hospital to recuperate.
You should be able to return to work after about two months. The length of time it takes you to recover may depend on the size and position of the tumor that was removed. The healthcare professionals treating you will be able to advise you further.
If your acoustic schwannoma was completely removed, you won’t usually need further treatment. However, you’ll continue to be monitored with MRI scans.
Radiation therapy
Stereotactic radiosurgery
Stereotactic radiosurgery delivers a very focused and precise dose of radiation to your acoustic schwannoma. Stereotactic means locating a point (in this case the position of the tumor in your brain) using three-dimensional co-ordinates.
During stereotactic radiosurgery, the maximum amount of radiation will be aimed at your tumor without the surrounding tissue being exposed. It may be given as a single dose or delivered over several sessions. It doesn’t get rid of your tumor but aims to stop it growing further. It can only be used on small tumors or the remains of a tumor after surgery on large tumors. It’s not usually used for large tumors.
Stereotactic radiosurgery is carried out under local anesthetic, which means you’ll be conscious throughout the procedure but your scalp will be numbed. A lightweight metal frame is usually attached to the scalp and a series of scans will accurately pinpoint the position of the tumor. It can then be treated using a precise beam of radiation.
Immediate side effects of stereotactic radiosurgery are rare, and you’ll usually only need to take a couple of days off work to have the treatment.
- Nerve damage
In some cases, stereotactic radiosurgery can cause nerve damage, although it may not be apparent until several weeks or months after treatment.
Symptoms of nerve damage can include:
- facial numbness (loss of feeling)
- facial paralysis (an inability to move part of your face)
- hearing loss
Facial paralysis affects around one in every 100 people who has stereotactic radiosurgery. It’s estimated that just under a third of people may experience hearing loss after stereotactic radiosurgery.
Stereotactic radiotherapy
Fractionated stereotactic radiotherapy delivers a small dose of radiation to the tumor over several sessions in an effort to curb the growth of the tumor without damaging surrounding brain tissue.
Proton beam therapy
This type of radiation therapy uses high-energy beams of positively charged particles called protons that are delivered to the affected area in targeted doses to treat tumors and minimize radiation exposure to the surrounding area.
Coping and support
Dealing with the possibility of hearing loss and facial paralysis and deciding which treatment would be best for you can be quite stressful. Here are some suggestions you may find helpful:
- Educate yourself about acoustic neuroma. The more you know, the better prepared you’ll be to make good choices about treatment. Besides talking to your doctor and your audiologist, you may want to talk to a counselor or social worker. Or you may find it helpful to talk to other people who’ve had an acoustic neuroma and learn more about their experiences during and after treatment.
- Maintain a strong support system. Family and friends can help you as you go through this difficult time. Sometimes, though, you may find the concern and understanding of other people with acoustic neuroma especially comforting.
Your doctor or a social worker may be able to put you in touch with a support group. Or you may find an in-person or online support group through the Acoustic Neuroma Association (https://www.anausa.org/).
Malignant schwannoma
Malignant schwannomas are also called malignant peripheral nerve sheath tumors or neurofibrosarcomas.
Malignant schwannomas are a rare type of cancerous tumor that are classed as a soft tissue sarcoma. Soft tissue is a term used to describe all the supporting tissues in the body, apart from the bones. So this includes muscle, nerves, tendons and deep skin tissue.
In over half of all cases they are linked to a condition called Neurofibromatosis type 1. Most of the other cases of malignant schwannoma occur as a one off.
Malignant schwannoma diagnosis
Your specialist will examine you and then you may need other tests which can include:
- blood tests
- ultrasound scan
- MRI scan
- CT scan
- X-ray
Malignant schwannoma treatment
These tumors can be difficult to treat. The main treatment is surgery, where the surgeon will try to remove as much of the tumor as possible and the surrounding tissue.
Radiotherapy might also be used before or after surgery to try to shrink the tumor or to reduce the risk of it coming back.
Malignant schwannomas don’t respond very well to chemotherapy. Chemotherapy may be used to try to shrink the tumor or to keep it at bay, but it is usually unlikely to cure it.
As malignant schwannomas are so rare there is not a lot of information about them. However people who seem to do best with treatment tend to:
- have tumors smaller than 5 cm across
- have had their tumors completely removed
- be younger
Malignant schwannoma that comes back
Usually, a schwannoma coming back in the same place means that it wasn’t completely removed the first time round. There may have been microscopic traces of it left behind. This is enough for it to grow into a new tumor. It might happen because your surgeon couldn’t remove any more than they did, due to its size or position in the body.
When malignant schwannoma comes back, it can be more difficult to treat. You might have surgery again if it is possible to remove the new tumor. You might be able to have radiotherapy again depending on the dose you had previosuly.
Trigeminal schwannoma
Trigeminal schwannomas are rare tumors, accounting for between 0.07% and 0.36% of all intracranial tumors and 0.8% and 8% of intracranial schwannomas 5. The trigeminal nerve is the second most common intracranial site of occurrence after vestibular nerve origin 5. Trigeminal schwannoma is more common in females 6 and usually involves patients of fourth and fifth decades 7. Trigeminal schwannoma in childhood is extremely rare, even rarer is their occurrence in childhood, in the absence of neurofibromatosis, only five such cases have been described in literature. All literature that describes surgical approaches for these tumors is mostly confined to adults 5. The rarity of these tumors in childhood and their multi-compartmental extensions pose a unique challenge that needs to be understood. Several authors have described staged surgery for such childhood tumors 8.
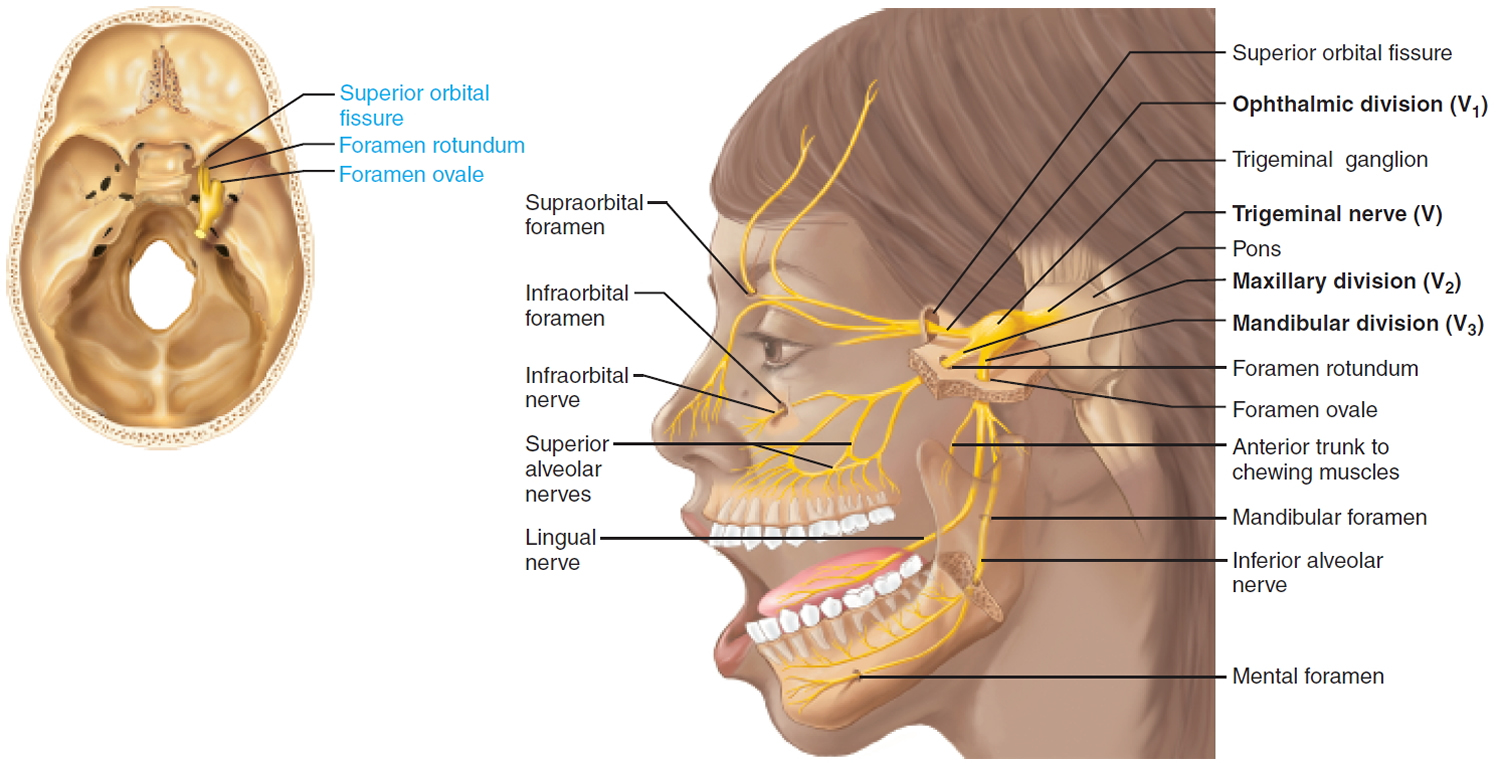
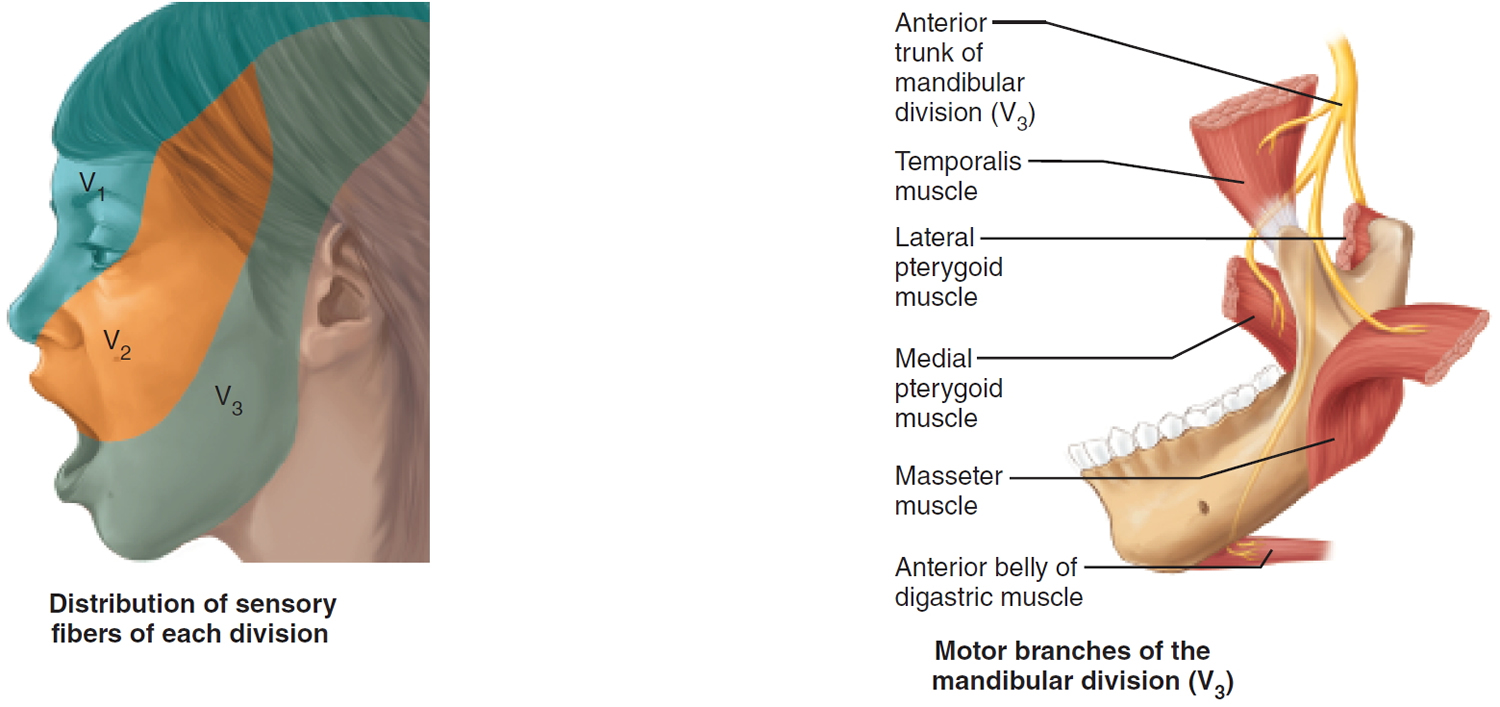
Figure 6. Trigeminal nerve (Cranial nerve 5)
In 1955, Jefferson categorized Trigeminal schwannomas into the following 3 types 8:
- Type A, tumors of the gasserian ganglion in the middle cranial fossa;
- Type B, tumors of the roots of the trigeminal nerve in the posterior fossa; and
- Type C, the so-called hourglass tumors occupying both the middle and posterior fossae.
- Some authors added a fourth classification, type D, for tumors with an extra cranial extension.
Growth from the root of cranial nerve V in the posterior fossa involves cerebellopontine angle whereas growth occurs epidurally into orbit and infratemporal fossa if there is involvement of extracranial branches. The tumor may extend into the orbit through the superior orbital fissure, in the infratemporal fossa through the foramen ovale or foramen rotundum and in the cavernous sinus through the lateral wall, and in the cerebellopontine angle through the trigeminal pore. There are so many different classifications for trigeminal schwannomas 9. Tumors of the neurogenic origin are rare in orbit and account for 1% of all the orbital tumors 10. Orbital schwannoma may be associated with Neurofibromatosis Type 1 in 1.5% of the patients. As these tumors are slow growing and subtle in nature, patients usually present with large tumor at the time of diagnosis. Variable location of these tumors can cause variable symptoms and signs. Trigeminal nerve-related complaints are the initial one in majority of the patients 11. Facial hypoesthesia is the most common complaint and presents in 60% of the patients 12. There may be involvement of motor part of trigeminal nerve. Corneal reflex may be diminished or absent.
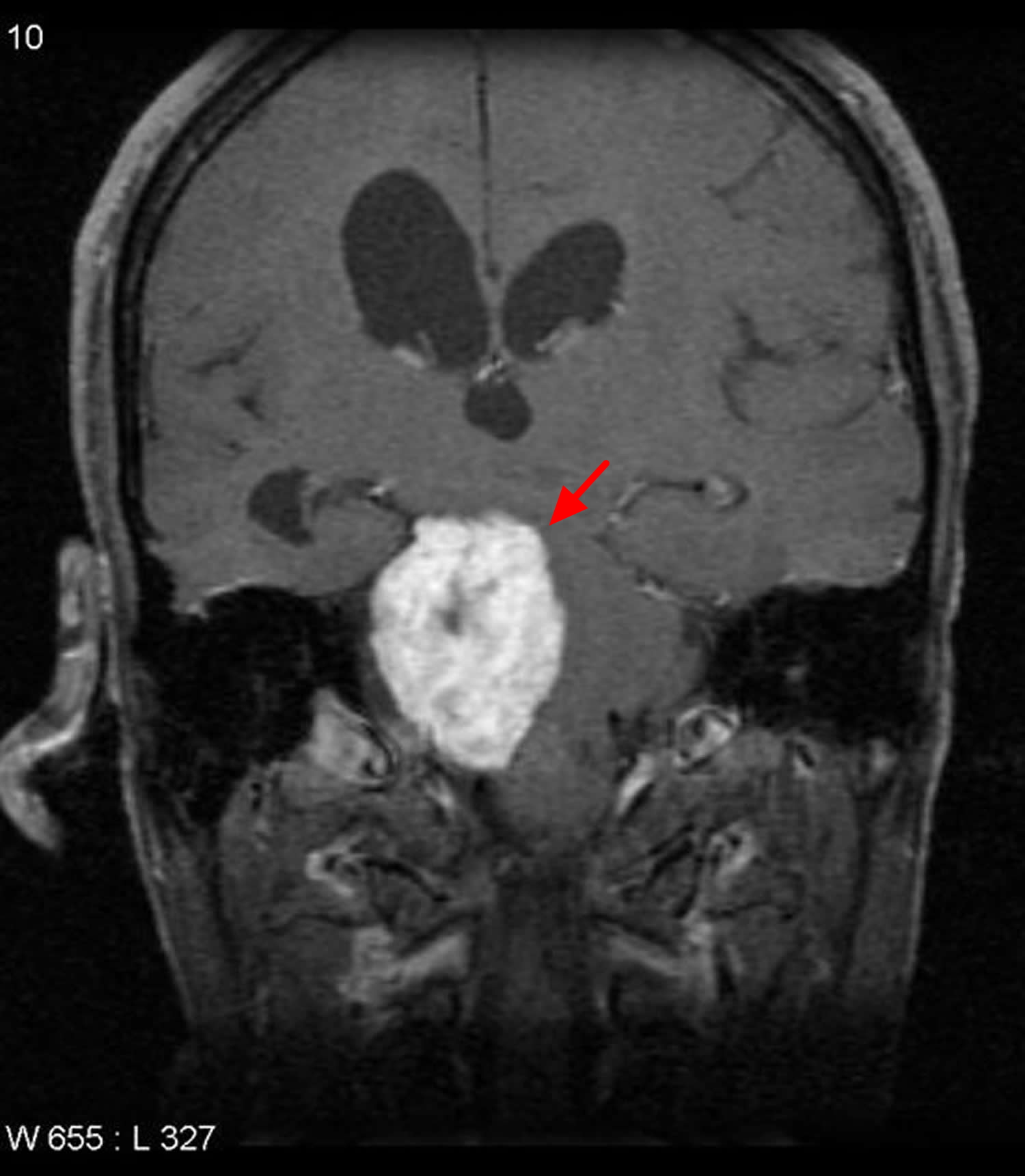
Figure 7. Trigeminal schwannoma
Note: The mass has a dumbbell configuration, with a component in Meckle’s cave (red arrow) and a larger one in the cerebellopontine angle (blue arrow). The fourth ventricle is markedly distorted (yellow arrow), as is the basilar artery (green arrow).
About 24% of the orbital schwannoma arise from first division of trigeminal nerve and rest may be from supra- or infra-orbital nerve. These patients usually present with slowly progressive proptosis, diplopia, decrease extraocular movement, and sometimes with vision loss if the tumor directly compresses the optic nerve or secondarily due to raised intracranial pressure 13.
Gadolinium-enhanced MRI of brain with orbit is the imaging modality of choice to diagnose trigeminal schwannoma. Schwannomas appear as well-circumscribed, heterogeneously enhancing masses that may be iso- or hypo-intense on T1-weighted images and hyperintense on T2-weighted images. Intratumoral hemorrhage may be seen but cystic changes are rare. Computed tomography scan is good to evaluate the accompanied bony changes such as erosion of petrous bone and widening of cranial foramen.
Because trigeminal schwannomas are benign and well-circumscribed tumors with only rare cases demonstrating invasion, complete surgical resection remains the definitive treatment. Selection of the surgical approach is dictated mainly by the location of the tumor. Radiotherapy is indicated in postoperative residual tumor. Incomplete excision of tumor may result in postoperative recurrence.
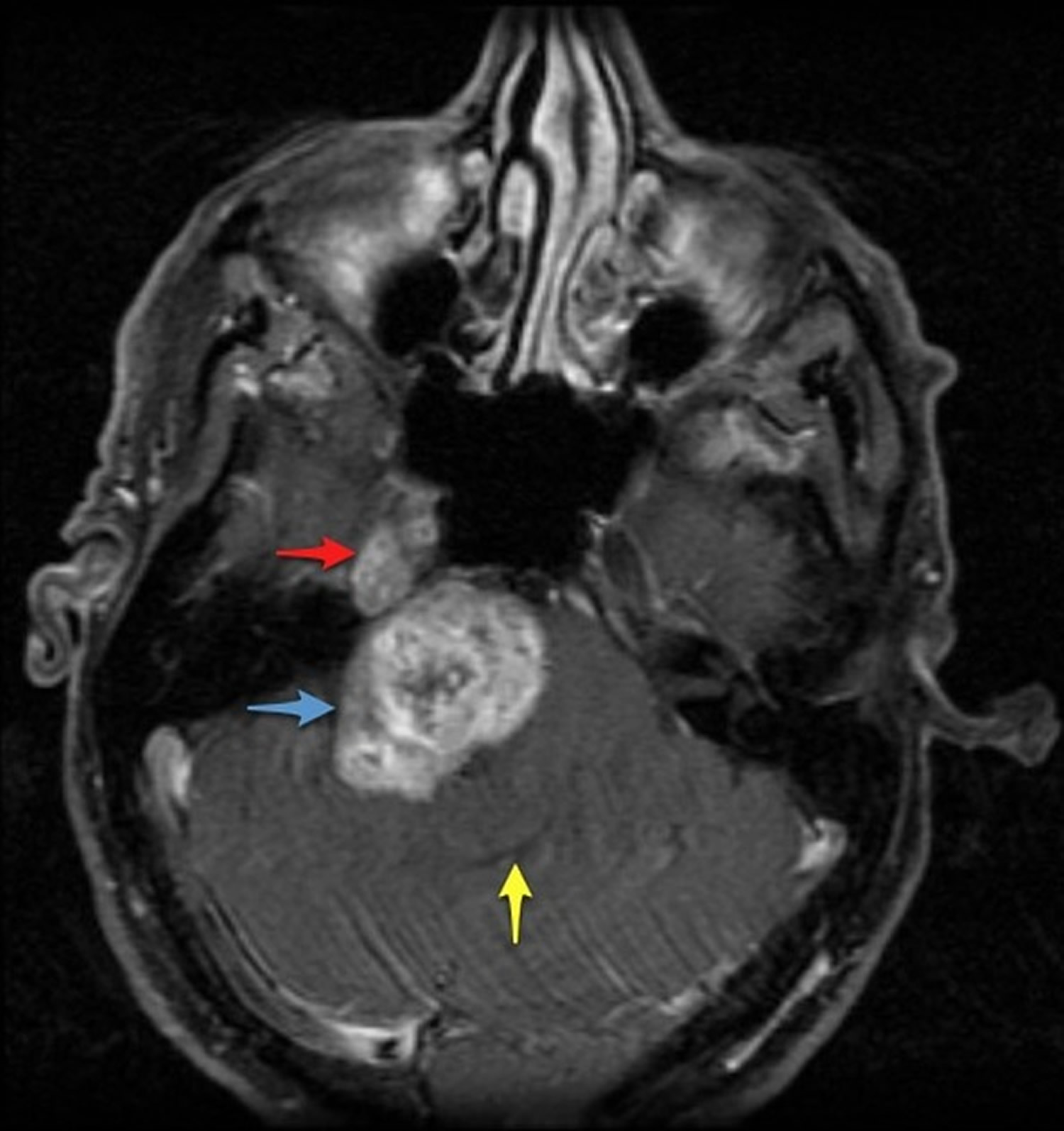
Schwannoma spine
Spinal schwannomas are schwannomas arising from nerves within the spinal canal. They are the most common intradural extramedullary spinal tumors, representing 30% of such lesions in adults 14. Spinal schwannomas are most frequently seen in the cervical and lumbar regions, far more frequently than in the thoracic spine 15. Most spinal schwannomas are solitary and sporadic. However, there is an association with neurofibromatosis type 2 (NF2). In patients with NF2, almost all spinal nerve root tumors are schwannomas or mixed tumors.
The incidence of spinal schwannoma is 0.3–0.5/100,000 individuals annually 15. Its prevalence is similar in males and females, and it is usually diagnosed during the fourth and fifth decades of life 16.
On imaging, they are usually characterized as solid and well-defined lesions with low T1 and high T2 MRI signals, and showing contrast enhancement. The signal intensity can be heterogeneous due associated haemorrhage, intrinsic vascular changes (thrombosis, sinusoidal dilatation), cyst formation and fatty degeneration.
The initial symptoms are varied in accordance with the level of the tumor. Patients commonly present with pain and the pain is localized in one (tumor) place, sometimes spread in both sides, mostly temporarily, but constantly in the same place and hurt as a knife 17. At the beginning the root pain is attributed to the disturbance of nerve conductivity because of the direct or indirect irritation of nerve root or root compression by the tumor 14. Later on when compression increases to spinal cord, spinal tracts gets damaged and myelopathy develops 18. However, motor weakness rarely occurs as an initial symptom in the lumbosacral region. Motor weakness of the lower extremity may not be obvious until the later stage, as in patients with lumbar canal stenosis.
Currently, the standard treatment is gross total resection of the tumor with as much preservation of neurovascular structures as possible 19. Although total resection of spinal nerve sheath tumors has been considered to be feasible 18, some cases have resected incompletely 20. There may be two obstacles to total resection : one is adhesion to the spinal cord because of hemorrhage, inflammation, or subpial localization; the other is critical structures attached to extradural components outside the spinal canal in the cervical region, such as the vertebral artery.
Figure 8. Spinal schwannoma
Schwannoma symptoms
The symptoms and signs of a schwannoma develop from direct effects on the main nerve or from the tumor pressing on nearby nerves, blood vessels or tissues. As the schwannoma tumor grows, it may be more likely to cause signs and symptoms, although tumor size doesn’t always determine effects.
Signs and symptoms of peripheral nerve tumors vary depending on the location of the tumors and which tissues are affected. They include:
- Swelling or a lump under your skin
- Pain, tingling or numbness
- Weakness or loss of function in the affected area
- Dizziness or loss of balance
Schwannoma diagnosis
To diagnose a schwannoma, your doctor may ask you about signs and symptoms, discuss your medical history, and perform both a general physical and neurological exam. If signs suggest that you could have a schwannoma or other nerve tumor, your doctor may recommend one or more of these diagnostic tests:
- Magnetic resonance imaging (MRI). This scan uses a magnet and radio waves to produce a detailed, 3-D view of your nerves and surrounding tissue.
- Computerized tomography (CT). A CT scanner rotates around your body to record a series of images. A computer uses the images to make a detailed view of your growth so that your doctor can evaluate how it may be affecting you.
- Electromyogram (EMG). For this test, your doctor places small needles in your muscles so an electromyography instrument can record the electrical activity in your muscle as you try to move it.
- Nerve conduction study. You’re likely to have this test along with your EMG. It measures how quickly your nerves carry electrical signals to your muscles.
- Tumor biopsy. If imaging tests identify a nerve tumor, your doctor may remove and analyze a small sample of cells (biopsy) from your tumor. Depending on the tumor’s size and location, you may need local or general anesthesia during the biopsy.
- Nerve biopsy. If you have a condition such as progressive peripheral neuropathy or enlarged nerves that mimic nerve tumors, your doctor may take a nerve biopsy.
Schwannoma treatment
Schwannoma treatment depends on where the abnormal growth is located and whether it is causing pain or growing quickly. Treatment options include:
- Monitoring. Your doctor may suggest observing your condition over time. Observation may include regular checkups and a CT or MRI scan every few months to see if your tumor is growing.
- Surgery. An experienced peripheral nerve surgeon can remove the tumor if it is causing pain or growing quickly. Schwannoma surgery is done under general anesthesia. Depending on the location of the tumor, some patients can go home the day of surgery. Others may need to stay in the hospital for one or two days. Even after successful removal of the tumor during surgery, a tumor may recur.
- Radiation therapy. Radiation therapy is used to help control the tumor growth and improve your symptoms. It may be used in combination with surgery.
- Stereotactic radiosurgery. If the tumor is near vital nerves or blood vessels, a technique called stereotactic body radiation therapy may be used to limit damage to healthy tissue. With this technique, doctors deliver radiation precisely to a tumor without making an incision.
- Agrawal A, Singh V, Rohilla S, Sharma B. Trigeminal schwannoma. National Journal of Maxillofacial Surgery. 2017;8(2):149-152. doi:10.4103/njms.NJMS_82_14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5773990/[↩]
- Daly J. F., and Roesler H. K.. 1963. Neurilemmoma of the cervical sympathetic chain. Archives of Otolaryngology. Head Neck Surg. 77:262. https://www.ncbi.nlm.nih.gov/pubmed/14024784[↩]
- Plexiform and other unusual variants of palisaded encapsulated neuroma. Argenyi ZB, Cooper PH, Santa Cruz D. J Cutan Pathol. 1993 Feb; 20(1):34-9. https://www.ncbi.nlm.nih.gov/pubmed/8468415/[↩]
- Ancient cervical vagal neurilemmoma: a case report. Saydam L, Kizilay A, Kalcioglu T, Gurer I. Am J Otolaryngol. 2000 Jan-Feb; 21(1):61-4. https://www.ncbi.nlm.nih.gov/pubmed/10668680/[↩]
- Chen LF, Yang Y, Yu XG, Gui QP, Bu B, Xu BN, et al. Operative management of trigeminal neuromas: An analysis of a surgical experience with 55 cases. Acta Neurochir (Wien) 2014;156:1105–14. https://www.ncbi.nlm.nih.gov/pubmed/24633987[↩][↩][↩]
- VandeVyver V, Lemmerling M, Van Hecke W, Verstraete K. MRI findings of the normal and diseased trigeminal nerve ganglion and branches: A pictorial review. JBR BTR. 2007;90:272–7. https://www.ncbi.nlm.nih.gov/pubmed/17966244[↩]
- McCormick PC, Bello JA, Post KD. Trigeminal schwannoma. Surgical series of 14 cases with review of the literature. J Neurosurg. 1988;69:850–60. https://www.ncbi.nlm.nih.gov/pubmed/3057125[↩]
- Verstappen CC, Beems T, Erasmus CE, van Lindert EJ. Dumbbell trigeminal schwannoma in a child: Complete removal by a one-stage pterional surgical approach. Childs Nerv Syst. 2005;21:1008–11. https://www.ncbi.nlm.nih.gov/pubmed/15770515[↩][↩]
- Yoshida K, Kawase T. Trigeminal neurinomas extending into multiple fossae: Surgical methods and review of the literature. J Neurosurg. 1999;91:202–11 https://www.ncbi.nlm.nih.gov/pubmed/10433308[↩]
- Khetan VD. Giant subperiosteal orbital schwannoma with luxated globe. J Clin Ophthalmol Res. 2013;1:159–62.[↩]
- Al-Mefty O, Ayoubi S, Gaber E. Trigeminal schwannomas: Removal of dumbbell-shaped tumors through the expanded Meckel cave and outcomes of cranial nerve function. J Neurosurg. 2002;96:453–63. https://www.ncbi.nlm.nih.gov/pubmed/11883829[↩]
- Jefferson G. The trigeminal neurinomas with some remarks on malignant invasion of the gasserian ganglion. Clin Neurosurg. 1953;1:11–54 https://www.ncbi.nlm.nih.gov/pubmed/14379464[↩]
- Ghosh S, Das D, Varshney R, Nandy S. Orbital extension of trigeminal schwannoma. J Neurosci Rural Pract. 2015;6:102–4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4244767/[↩]
- Celli P, Trillo G, Ferrante L. Spinal extradural schwannoma. J Neurosurg Spine. 2005;2:447–456. https://www.ncbi.nlm.nih.gov/pubmed/15871485[↩][↩]
- Long-term outcome after removal of spinal schwannoma: a clinicopathological study of 187 cases. Seppälä MT, Haltia MJ, Sankila RJ, Jääskeläinen JE, Heiskanen O. J Neurosurg. 1995 Oct; 83(4):621-6. https://www.ncbi.nlm.nih.gov/pubmed/7674010/[↩][↩]
- Clinical characteristics of spinal nerve sheath tumors: analysis of 149 cases. Jinnai T, Koyama T. Neurosurgery. 2005 Mar; 56(3):510-5; discussion 510-5. https://www.ncbi.nlm.nih.gov/pubmed/15730576/[↩]
- Jeon JH, Hwang HS, Jeong JH, Park SH, Moon JG, Kim CH. Spinal Schwannoma; Analysis of 40 Cases. Journal of Korean Neurosurgical Society. 2008;43(3):135-138. doi:10.3340/jkns.2008.43.3.135. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2588243/[↩]
- Subaciute J. [Early diagnosis of spinal cord schwannoma : the significance of the pain syndrome] Medicina (Kaunas) 2002;38:1086–1088 https://www.ncbi.nlm.nih.gov/pubmed/12532722[↩][↩]
- Yu NH, Lee SE, Jahng TA, Chung CK. Giant invasive spinal schwannoma: its clinical features and surgical management. Neurosurgery (2012) 71:58–66.10.1227/NEU.0b013e31824f4f96 https://www.ncbi.nlm.nih.gov/pubmed/22353794[↩]
- Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas : retrospective analysis and long-term outcome of 179 consecutively operated cases and review of the literature. Surg Neurol. 2004;61:34–43. discussion 44 https://www.ncbi.nlm.nih.gov/pubmed/14706374[↩]