What is spinal cord compression ?
Acute spinal cord compression is a medical emergency and occurs as a result of compression of the spinal cord by bone fragments from a vertebral fracture, ruptured vertebral disc, an abscess, a tumor or metastases (see Figure 6) 1.
- Compression Fracture: A type of break in a bone caused by pressure and in which the bone collapses 2. Compression fractures usually occur in the spine (backbone) and in bones made weak by cancer or by osteoporosis (a decrease in bone mass and density).
- Spinal Cord Neoplasm (Tumor): An abnormal mass of tissue that results when cells divide more than they should or do not die when they should. Neoplasms may be benign (not cancer), or malignant (cancer).
Symptoms suggestive of acute spinal cord compression include an acute onset of back pain, dermatone of increased sensation, paralysis below the level of compression, urinary and fecal incontinence or retention. Lhermitte’s sign (intermittent electric shock-like sensation down the center of the back following flexion of the neck) and hyperreflexia may be present.
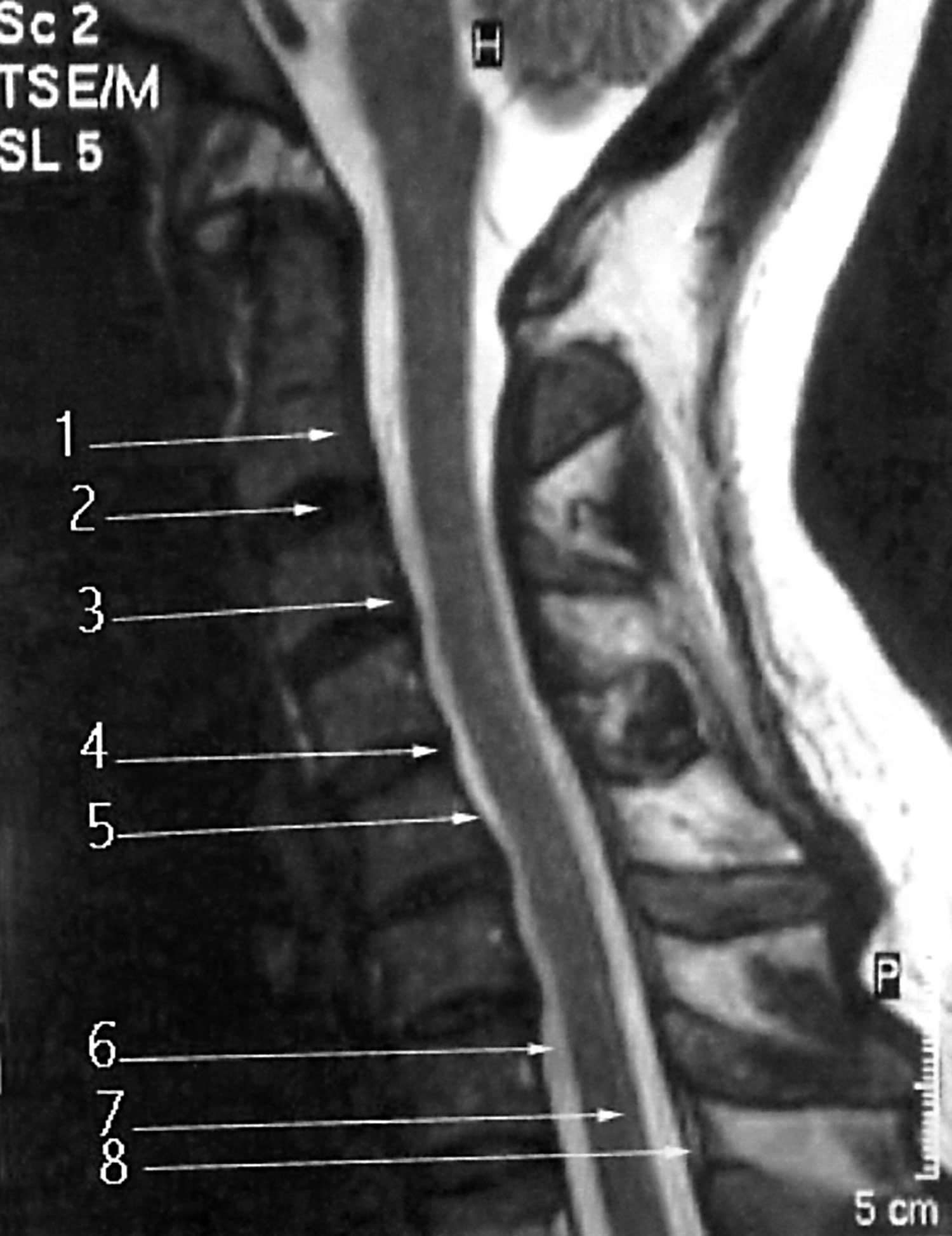
Urgent radiological investigations are required usually with MRI of the whole spine (Figure 6). The most common causes of cord compression are tumours such as lung cancer (non-small cell lung cancer), breast cancer, prostate cancer, renal cell carcinoma, thyroid carcinoma, lymphoma and multiple myeloma. Infective causes include abscesses and granulomas such as tuberculosis.
The median survival of patients with metastatic spinal cord compression is about 12 weeks, due to the advanced nature of the underlying malignant disease.
Spinal cord Anatomy
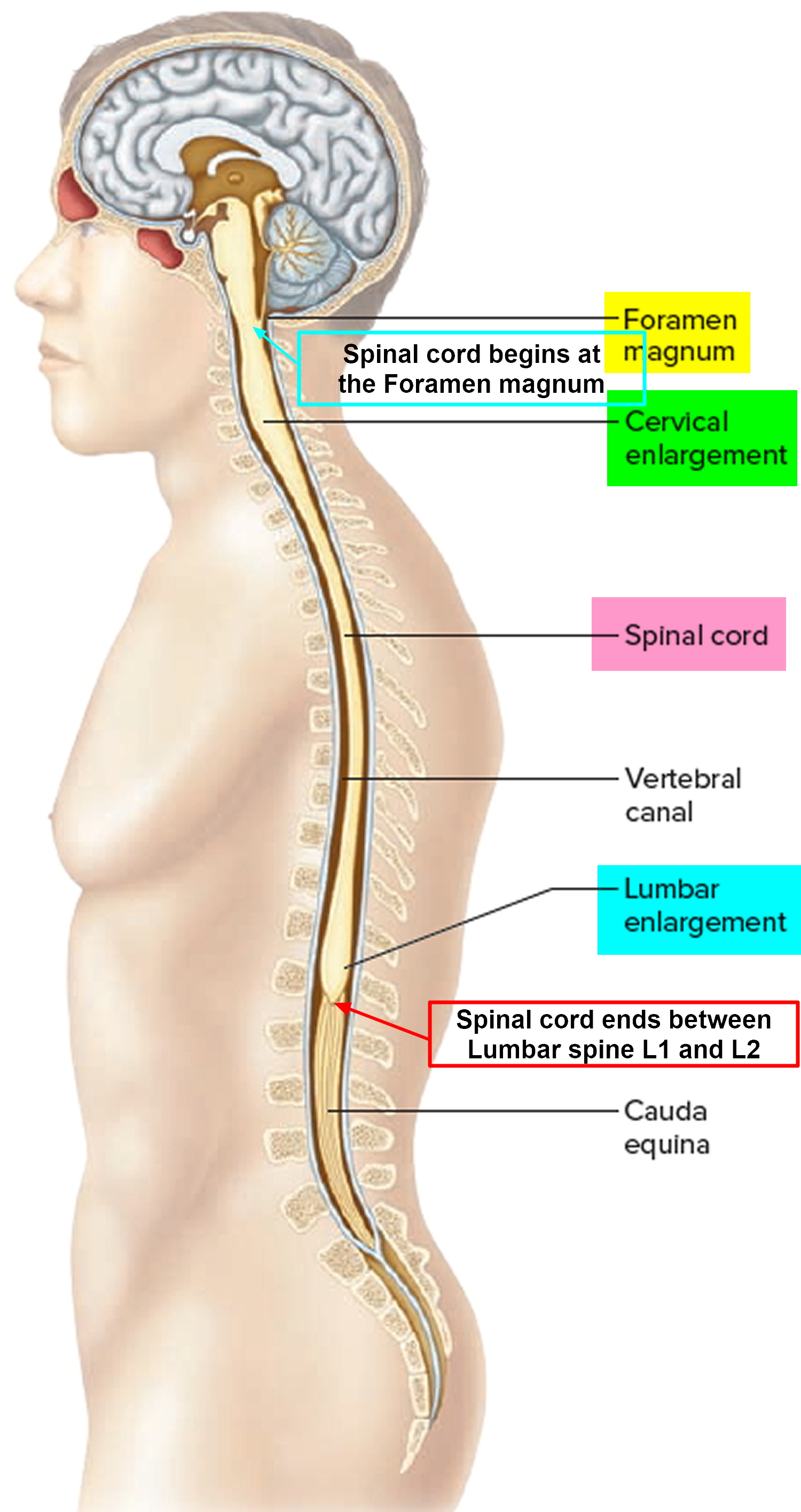
The spinal cord compression is a slender column of nervous tissue that passes downward from the brain into the vertebral canal. Although continuous with the brain, the spinal cord begins where nervous tissue leaves the cranial cavity at the level of the foramen magnum.
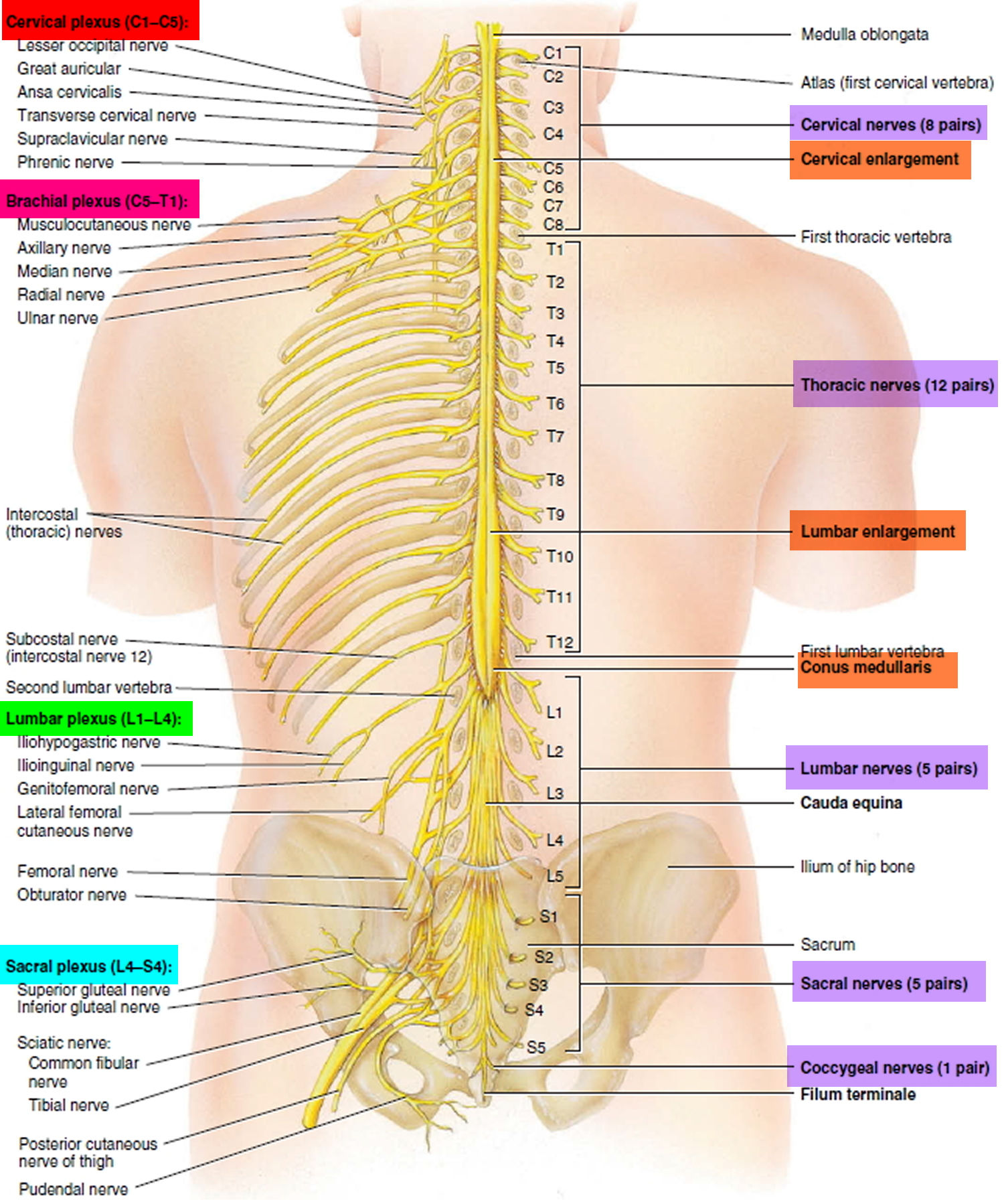
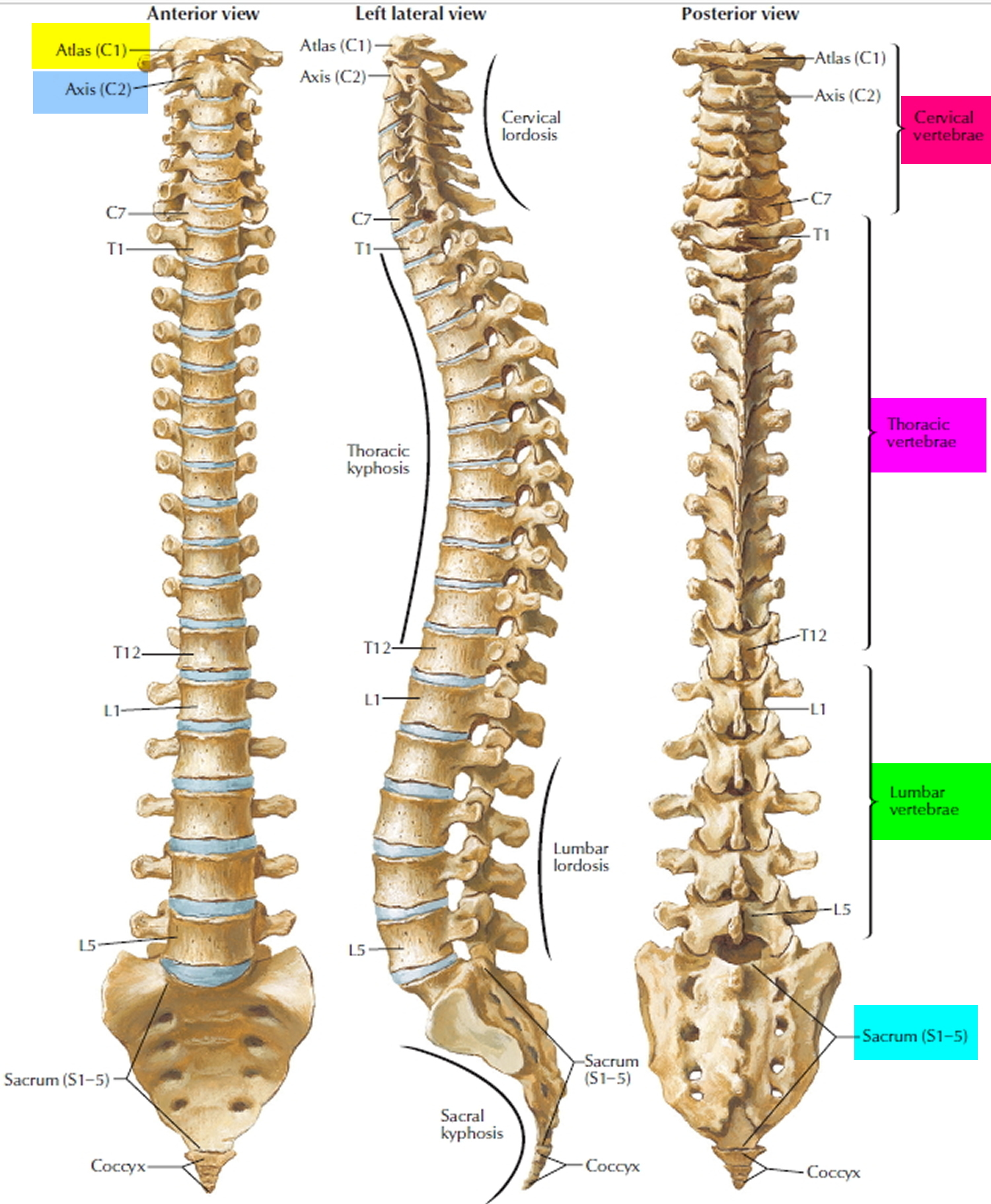
The spinal cord is not uniform in diameter along its length. In the neck region, a thickening in the spinal cord, called the cervical enlargement, occurs in the region associated with the origins of spinal nerves from the cervical spines to thoracic spine T1 giving rise to nerves to the upper limbs. A similar thickening in the lower back, the lumbosacral enlargement, occurs in the region associated with the origins of spinal nerves thoracic spine T 11 to Sacral S3 giving rise to nerves to the lower limbs. The spinal cord tapers to a point and ends near the intervertebral disc that separates the first (L1) and second lumbar (L2) vertebrae, adults, although it can end as high as thoracic vertebra T12 or as low as the disc between vertebrae lumbar vertebrae L2 and L3. From this point, nervous tissue, including axons of both motor and sensory neurons, extends downward to become spinal nerves at the remaining lumbar and sacral levels forming a structure called the cauda equina (horse’s tail).
Figure 1. Spinal cord
Figure 2. Spinal cord segments
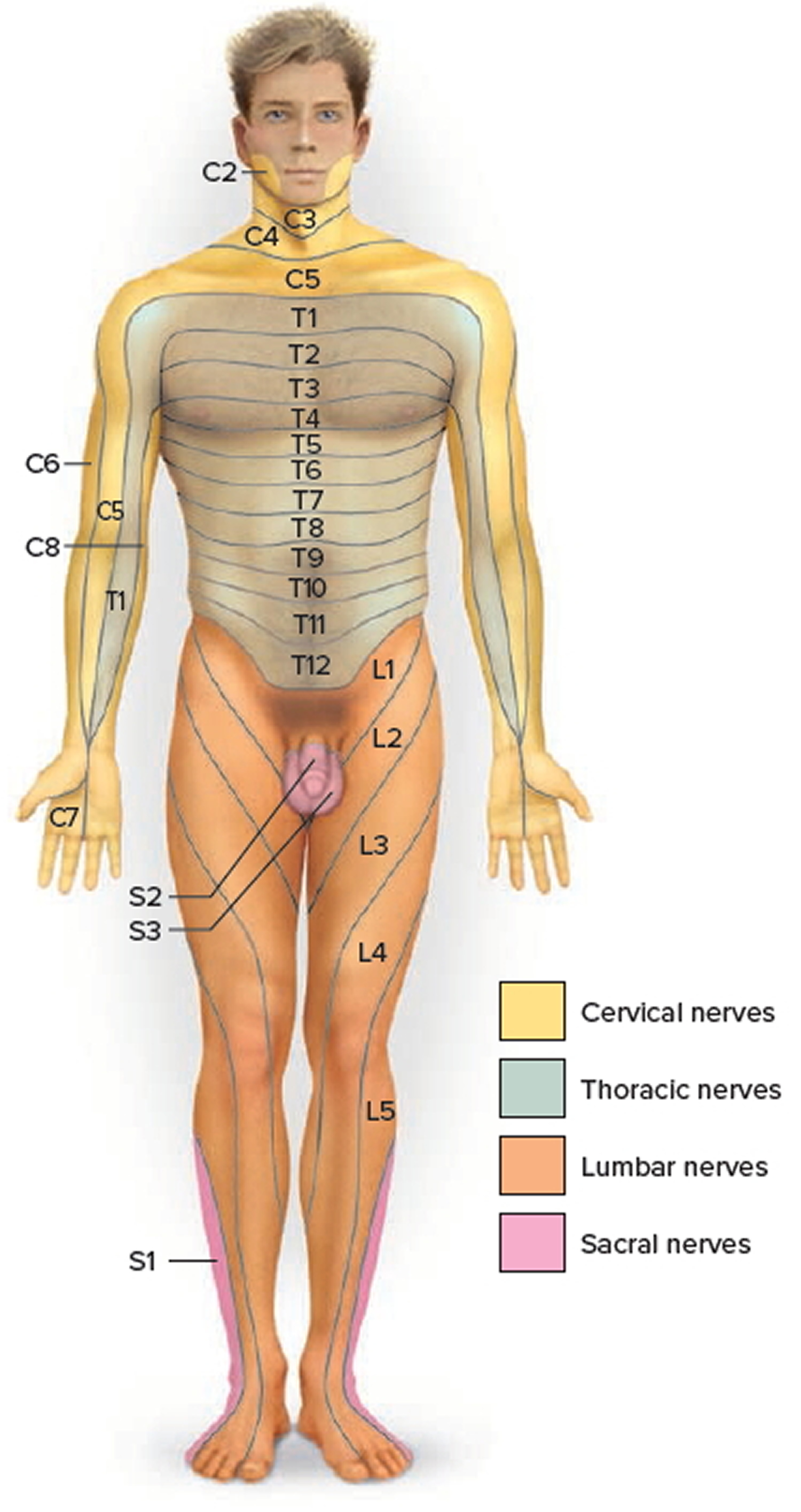
Figure 3. Dermatome (spinal nerves sensory innvervation)
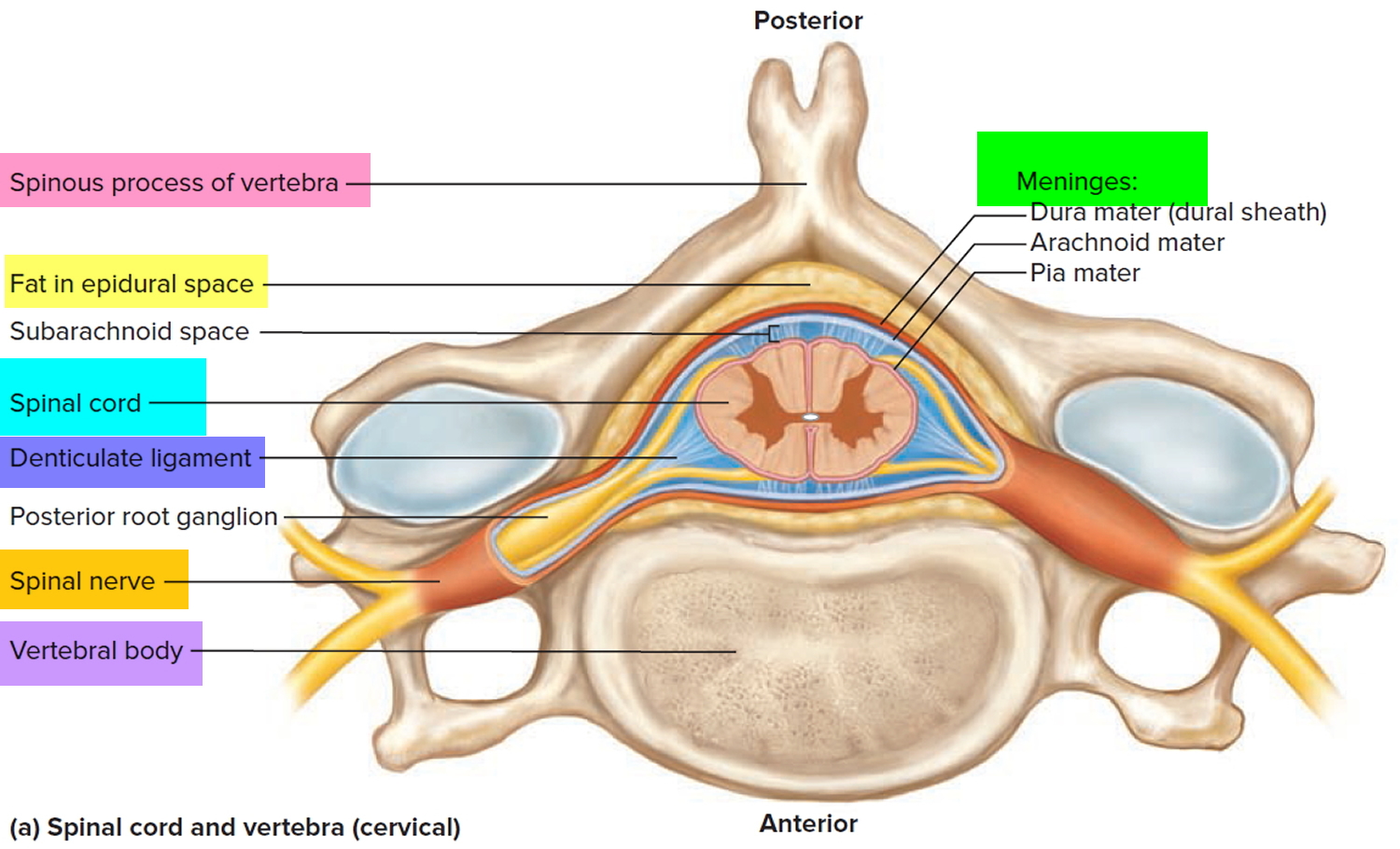
Figure 4. Spinal cord anatomy
Figure 5. Vertebral column
Figure 6. Spinal cord compression (MRI scan)
Note: The case above was due to a thyroid carcinoma bony metastasis to vertebral body T5 resulting in destruction of the body of the vertebra and subsequent posterior dislocation of T5, resulting in compression of the spinal cord.
Causes of spinal cord compression
Spinal cord compression is caused far more commonly by lesions outside the spinal cord (extramedullary) than by lesions within it (intramedullary) 3.
Spinal cord compression may be:
- Acute
- Subacute
- Chronic
Acute spinal cord compression
Acute spinal cord compression develops within minutes to hours 3. It is often due to trauma (e.g, vertebral crush fracture with displacement of fracture fragments, acute disk herniation, metastatic tumor, severe bone or ligamentous injury causing hematoma, vertebral subluxation or dislocation). It is occasionally due to abscess and rarely due to spontaneous epidural hematoma. Acute spinal cord compression may follow subacute and chronic compression, especially if the cause is abscess or tumor.
Subacute spinal cord compression
Subacute spinal cord compression develops over days to weeks 3. It is usually caused by a metastatic extramedullary tumor, a subdural or an epidural abscess or hematoma, or a cervical or, rarely, thoracic herniated disk.
Chronic spinal cord compression
Chronic compression develops over months to years 3. It is commonly caused by bony protrusions into the cervical, thoracic, or lumbar spinal canal (eg, due to osteophytes or spondylosis, especially when the spinal canal is narrow, as occurs in spinal stenosis). Compression can be aggravated by a herniated disk and hypertrophy of the ligamentum flavum. Less common causes include arteriovenous malformations and slow-growing extramedullary tumors.
Atlantoaxial subluxation and other craniocervical junction abnormalities may cause acute, subacute, or chronic spinal cord compression.
Lesions that compress the spinal cord may also compress nerve roots or, rarely, occlude the spinal cord’s blood supply, causing spinal cord infarction.
Cervical spinal cord compression
Cervical spinal cord compression in the elderly is most like be caused by cervical spondylotic myelopathy 4. Spondylosis refers to the degenerative changes that occur in the spine, including degeneration of the joints, intervertebral discs, ligaments and connective tissue of the cervical vertebrae.
There are three important pathophysiologic factors in the development of cervical spondylotic myelopathy 5:
- Static mechanical;
- Dynamic mechanical; and
- Spinal cord ischemia.
Static mechanical factors result in the reduction of spinal canal diameter and spinal cord compression. With aging, the intervertebral discs dry out resulting in loss of disc height.
This process puts greater stress on the articular cartilage of the vertebrae and their respective end plates. Osteophytic spurs develop at the margins of these end plates. Osteophytes stabilize adjacent vertebrae whose hypermobility is caused by the degeneration of the disc 6.
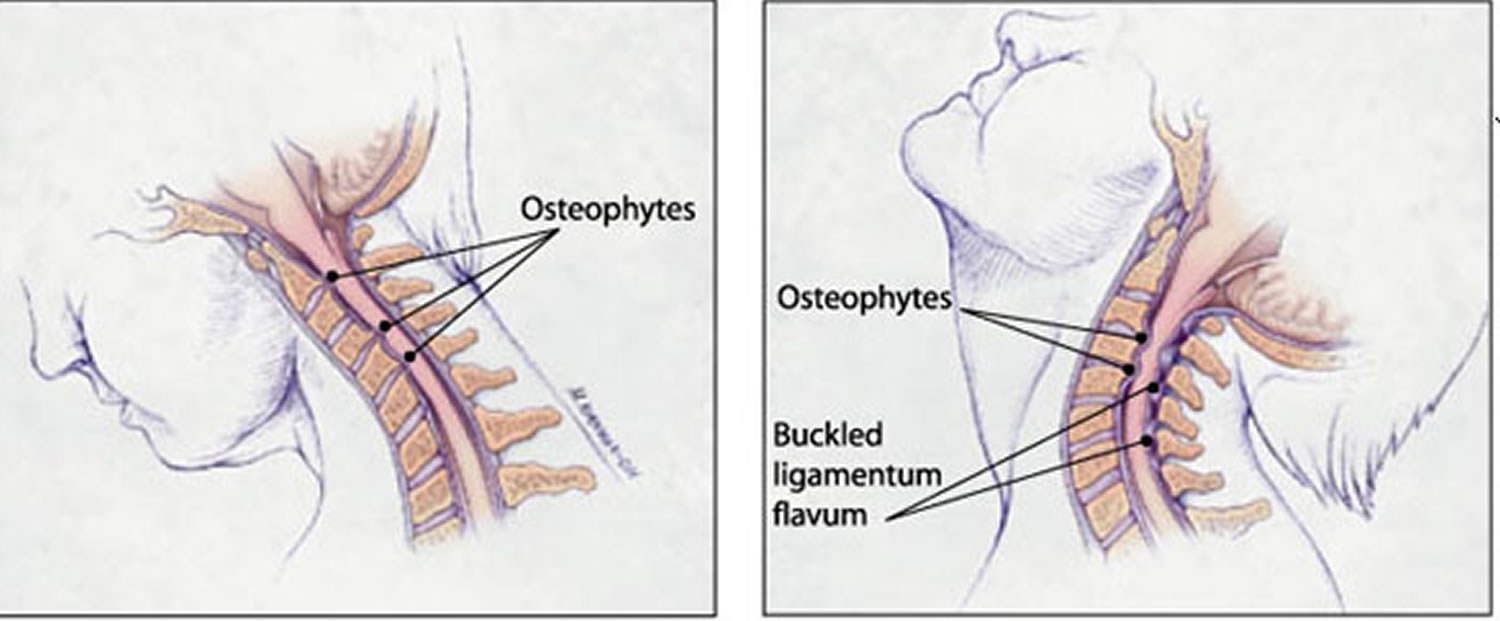
Osteophytic overgrowth ventrally and, in some cases, buckling of the ligamentum flavum dorsally can cause direct compression of the spinal cord resulting in myelopathy (clinically evident spinal cord dysfunction). Symptoms are believed to develop when the spinal cord has been reduced by at least 30 percent 7.
Cord compression may occur anteriorly, secondary to midline disc prolapse, osteophyte or more rarely ossified posterior longitudinal ligament. The cord may be compressed posteriorly by a hypertrophied ligamentum flavum (Figure 8).
Spinal cord ischemia probably plays a role in the development of cervical spondylotic myelopathy, particularly in later stages 8, 9. Histopathologic changes in the spinal cord consistent with ischemia have been observed in patients with cervical spondylotic myelopathy. However, the precise mechanism for spinal cord ischemia is not completely understood. Other factors associated with the development of spondylosis include heavy labor, posture and genetic predisposition 10, 11. Also, 70 percent of patients with Down syndrome have an increased incidence of spondylosis by 50 years of age 12.
Cervical spondylotic myelopathy is the most common spinal cord disorder in persons more than 55 years of age in North America and perhaps in the world 4. As the number of older persons in the United States increases, the incidence of cervical spondylotic myelopathy will most likely increase. In a prospective study designed to more accurately define the incidence of cervical spondylotic myelopathy, 23.6 percent of 585 patients with tetraparesis or paraparesis admitted to a United Kingdom regional neuroscience center had cervical spondylotic myelopathy 13. The overall prevalence in this population is unknown.
Figure 8. Potential sites of cervical spinal cord compression (Normal Cervical Spine MRI scan)
Note: (1) C2 vertebral body. (2) Intervertebral disc. (3) Posterior body edge adjacent to disc space (site of potential osteophyte formation). (4) Posterior disc margin (site of potential disc prolapse). (5) Posterior longitudinal ligament (site of potential ossification and cord compression). (6) Cerebrospinal fluid in front of cord. (7) Spinal cord. (8) Ligamentum flavum (site of potential hypertrophy and cord compression).
Dynamic mechanical factors relate to the fact that the normal motion of the cervical spine may aggravate spinal cord damage precipitated by direct mechanical static compression. During flexion, the spinal cord lengthens, thus stretching over ventral osteophytic ridges. During extension, the ligamentum flavum may buckle into the spinal cord causing a reduction of available space for the spinal cord (Figure 9).
Figure 9. Dynamic mechanical factors in cervical spondylotic myelopathy
Note: (Left) During flexion, the spinal cord is stretched over ventral osteophytic ridges. (Right) During extension, the ligamentum flavum may buckle into the spinal cord reducing space for the cord.
[Source 4]Cervical spinal cord compression symptoms and signs
Patients with cervical spinal cord compression will generally have these symptoms: neck stiffness; unilateral or bilateral deep, aching neck, arm and shoulder pain; and possibly stiffness or clumsiness while walking. Cervical spinal cord compression usually develops insidiously. In the early stages of cervical spinal cord compression, complaints of neck stiffness are common because of the presence of advanced cervical spondylosis 14. Other common complaints include crepitus in the neck with movement; brachialgia, which is characterized as a stabbing pain in the pre- or postaxial border of the arm, elbow, wrist or fingers; a dull “achy” feeling in the arm; and numbness or tingling in the hands.
In patients with a disc herniation between the sixth and seventh vertebrae, pain radiates into the shoulder, upper arm, elbow, and index and middle fingers. It is typically unilateral. Numbness and weakness follow the same distribution.
The hallmark symptom of cervical spinal cord compression is weakness or stiffness in the legs 14, 15. Patients with cervical spinal cord compression may also present with unsteadiness of gait. Weakness or clumsiness of the hands in conjunction with the legs is also characteristic of cervical spinal cord compression. Symptoms may be asymmetric particularly in the legs. Loss of sphincter control or frank incontinence is rare; however, some patients may complain of slight hesitancy on urination.
Common symptoms:
- Clumsy or weak hands
- Leg weakness or stiffness
- Neck stiffness
- Pain in shoulders or arms
- Unsteady gait
Common signs:
- Atrophy of the hand musculature
- Hyperreflexia
- Lhermitte’s sign (intermittent electric shock-like sensation down the center of the back following flexion of the neck)
- Sensory loss.
Other conditions that can mimic cervical spinal cord compression on presentation are:
|
|
|
|
|
|
|
|
|
Cervical spinal cord compression diagnosis
The physical and neurologic examination is used to confirm the presence of spinal cord dysfunction. Flexion of the neck may cause a generalized “electric shock-like” sensation down the center of the back, referred to as Lhermitte’s sign. Atrophy of the hands, particularly the intrinsic musculature, may be present.
Sensory abnormalities have a variable pattern on examination. Loss of vibratory sense or proprioception in the extremities (especially the feet) can occur. Superficial sensory loss may be asymmetric and persons are variably affected. The sensory examination may be confounded by the presence of diabetes mellitus and a concurrent peripheral neuropathy.
A characteristic physical finding of cervical spinal cord compression is hyperreflexia. The biceps and supinator reflexes (C5 and C6) may be absent, with a brisk triceps reflex (C7). This pattern is almost pathognomonic of cord compression because of cervical spondylosis at the C5-C6 interspace 16. Ankle clonus and Babinski’s sign (pathologic extension of the great toe elicited by stroking the foot) in the feet may also be revealed. Hoffmann’s sign (a reflex contraction of the thumb and index finger after nipping the middle finger) is a subtle indicator of spinal cord dysfunction. A stiff or spastic gait is also characteristic of cervical spinal cord compression in its later stages.
When cervical spondylosis is isolated to the C6-7, C7-T1 spinal levels, the arm reflexes may be normal. A hyperactive pectoralis muscle reflex elicited by tapping the pectoralis tendon in the deltopectoral groove causing adduction and internal rotation of the shoulder is a sign of cord compression in the upper cervical spine (C2-3, C3-4 spinal levels) 17. The “dynamic” Hoffmann’s sign (when a typical Hoffmann’s sign is elicited after having the patient flex and extend the neck multiple times) may be an indicator of early cervical spinal cord compression 18. Hyperreflexia may be absent in cervical spinal cord compression patients who have concurrent diabetes, causing a peripheral neuropathy.
Imaging and Diagnostic Studies
Magnetic resonance imaging (MRI) of the cervical spine is the procedure of choice during the initial screening process of patients with suspected cervical spinal cord compression 19. MRI is noninvasive and provides images of the spine and spinal cord in several planes (Figure 3). In addition to giving an assessment of the degree of spinal canal stenosis, an MRI can identify intrinsic spinal cord lesions that can also present with myelopathy (e.g., tumors). High signal changes seen in the spinal cord of patients with cervical spinal cord compression may indicate myelomalacia or permanent spinal cord damage.
Computed tomography (CT) is complementary to MRI. CT scan may give a more accurate assessment of the amount of canal compromise because it is superior to MRI in evaluating bone (osteophytes) 20. Myelography or the intrathecal injection of a contrast agent is used in conjunction with CT scan. Since the advent of MRI, the use of myelography has decreased; however, it still provides useful information in some instances for surgical planning. Plain radiographs alone are of little use as an initial diagnostic procedure.
Figure 10. Magnetic resonance imaging showing narrowing of the spinal canal as a result of anterior herniated discs/osteophytes and posterior buckling of hypertrophied ligamentum flavum
Treatment for cervical spinal cord compression
Evaluating the efficacy of any particular treatment strategy for cervical spinal cord compression is difficult because reports show that as many as 18 percent of patients with cervical spinal cord compression will improve spontaneously, 40 percent will stabilize and approximately 40 percent will deteriorate if no treatment is given 21. Unfortunately, the current understanding of cervical spinal cord compression does not allow physicians to predict the course of a patient. Also, the literature regarding various treatment strategies (surgical and nonsurgical) for cervical spinal cord compression is flawed because of a lack of prospective controlled studies.
NONSURGICAL TREATMENT
In patients who are mildly affected by cervical spinal cord compression, a “careful watching” approach can be taken. A variety of nonsurgical strategies have been used with variable success for the treatment of cervical spinal cord compression. These include cervical traction, cervical immobilization (collar or neck brace), skull traction and physical therapy. Cervical immobilization is the most commonly used treatment in the United States. Some studies demonstrate the benefits of wearing a brace, while other studies show that immobilization does not improve the patient’s condition 22. It has also been reported that symptomatic patients may deteriorate neurologically during bracing, causing many to advocate earlier surgical intervention 23. A nonsurgical approach is usually inadvisable.
SURGICAL TREATMENT
Once frank myelopathy occurs, surgical intervention is necessary. The primary goal of surgery is to decompress the spinal cord, thus giving the neural elements more room. Traditionally, cervical laminectomy, a posterior approach, has been used for surgical treatment of cervical spinal cord compression. However, over the past 20 years, it has been increasingly recognized that laminectomy is not appropriate for all patients. Further neurologic deterioration after laminectomy is attributed to a development of latent instability of the spine with development of kyphotic spinal deformities and to the inability of posterior approaches to directly address anterior vector compression secondary to osteophytic overgrowth.
For this reason, anterior approaches to the spine have been increasingly used 24. Through an anterior cervical approach, one can directly address and remove osteophytes and disc material for decompression of the spinal cord. Also, with the addition of interposition bone grafts and, in some cases, cervical plates (instrumentation) to promote spinal fusion, the development of instability of the neck can be prevented. A variety of factors must be considered when deciding whether to use an anterior or posterior approach, but the primary goal of both approaches is to provide adequate space for the spinal cord.
Many surgical series show “improvement,” or at least stabilization of symptoms with posterior and anterior approaches. After reviewing the surgical literature, one investigator found that the rate of successful outcome after surgery was at best 50 percent with the potential for significant postsurgical morbidity 24. The older surgical literature has been criticized because of the uncertainty of whether nonspondylotic myelopathy conditions (e.g., multiple sclerosis, ALS) had been sufficiently excluded before surgery 24.
A variety of factors determine success after surgery. Factors that may portend a less than satisfactory surgical outcome include severe preoperative neurologic deficits, abnormal signal changes within the spinal cord and/or spinal cord atrophy seen on MRI, and severity of cord compression seen on radiographic studies 25, 26, 27.
Spinal cord compression symptoms and signs
Acute or advanced spinal cord compression causes 3:
- Segmental deficits,
- Paraparesis or quadriparesis,
- Hyporeflexia (when acute) followed by hyperreflexia,
- Extensor plantar responses,
- Loss of sphincter tone (with bowel and bladder dysfunction), and
- Sensory deficits.
Subacute or chronic compression 3:
- May begin with local back pain, often radiating down the distribution of a nerve root (radicular pain), and sometimes hyperreflexia and loss of sensation.
- Sensory loss may begin in the sacral segments.
- Complete loss of function may follow suddenly and unpredictably, possibly resulting from secondary spinal cord infarction.
Spinal percussion tenderness is prominent if the cause is metastatic carcinoma, abscess, or hematoma.
Intramedullary lesions tend to cause poorly localized burning pain rather than radicular pain and to spare sensation in sacral dermatomes. These lesions usually result in spastic paresis.
Spinal cord compression Diagnosis
- MRI or CT myelography
Spinal cord compression is suggested by spinal or radicular pain (radicular pain is a type of pain that radiates into the lower extremity directly along the course of a spinal nerve root – see Figure 3) with reflex, motor, or sensory deficits, particularly at a segmental level.
MRI is done immediately if available. If MRI is unavailable, CT myelography is done; a small amount of iohexol (a nonionic, low osmolar radiopaque dye) is introduced via a lumbar puncture and allowed to run cranially to check for complete cerebrospinal fluid (CSF) block. If a block is detected, a radiopaque dye is introduced via a cervical puncture to determine the rostral (front end or nose end) extension of the block. If traumatic bone abnormalities (e.g, fracture, dislocation, subluxation) that require immediate spinal immobilization are suspected, plain spinal x-rays can be done. However, CT detects bone abnormalities better.
Spinal cord compression treatment
- Relief of compression
Treatment of spinal cord compression is directed at relieving pressure on the cord. Incomplete or very recent complete loss of function may be reversible, but complete loss of function rarely is; thus, for acute compression, diagnosis and treatment must occur immediately.
If compression is due to a tumor, IV (intravenous) dexamethasone 100 mg is given immediately to reduce the peri-lesion oedema and hence relieved the compressive pressure off the cord, followed by 25 mg q 6 h and immediate surgery or radiation therapy.
Emergency radiotherapy (20Gy/5 fractions, 30Gy/10 fractions, or 8Gy/1 fraction) is the mainstay of treatment for malignant spinal cord compression in centres where radiotherapy is available. If this is not available, then decompressive surgery is the main stay of therapy in order to prevent permanent neurological damage to the cord and permanent paralysis. Surgery is also indicated if permanent paralysis has occurred for pain controlled. Post-operative radiation is delivered within 2-3 weeks of surgical decompression as adjuvant therapy for the tumour.
Surgery is indicated in the following cases:
- Neurologic deficits worsen despite nonsurgical treatment.
- A biopsy is needed.
- The spine is unstable.
- Tumors recur after radiation therapy.
- An abscess or a compressive subdural or epidural hematoma is suspected.
Summary
Spinal cord compression is usually secondary to an extrinsic mass.
Manifestations may include back and radicular pain (early) and segmental sensory and/or motor deficits, altered reflexes, extensor plantar responses, and loss of sphincter tone (with bowel and bladder dysfunction).
Do MRI or CT myelography immediately.
To relieve pressure on the cord, do surgery or give corticosteroids as soon as possible.
- Spinal Cord Compression. National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0030152/[↩]
- Compression Fracture. National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0028123/[↩]
- Spinal Cord Compression. Merck Manual. https://www.merckmanuals.com/professional/neurologic-disorders/spinal-cord-disorders/spinal-cord-compression[↩][↩][↩][↩][↩][↩]
- Cervical Spondylotic Myelopathy: A Common Cause of Spinal Cord Dysfunction in Older Persons. Am Fam Physician. 2000 Sep 1;62(5):1064-1070. http://www.aafp.org/afp/2000/0901/p1064.html[↩][↩][↩]
- Fehlings MG, Skaf G. A review of the pathophysiology of cervical spondylotic myelopathy with insights for potential novel mechanisms drawn from traumatic spinal cord injury. Spine. 1998;23:2730–7.[↩]
- Wilkinson M. The morbid anatomy of cervical spondylosis and myelopathy. Brain. 1960;83:589–616.[↩]
- Penning L, Wilmink JT, van Woerden HH, Knole E. CT myelographic findings in degenerative disorders of the cervical spine: clinical significance. AJR Am J Roentgenol. 1986;146:793–801.[↩]
- Brain WR. Discussion on rupture of the intervertebral disc in the cervical region. Proc R Soc Med. 1948;41:509–11.[↩]
- Mair WG, Druckman R. The pathology of spinal cord lesions and their relationship to the clinical features in protrusion of cervical intervertebral discs: a report of four cases. Brain. 1953;76:70–91.[↩]
- Alexander JT. Natural history and nonoperative management of cervical spondylosis. In: Menezes AH, Sonntag VK, eds. Principles of spinal surgery. New York: McGraw-Hill Companies, Health Professions Division, 1996:547–57.[↩]
- Yoo K, Origitano TC. Familial cervical spondylosis. Case Report. J Neurosurg. 1998;89:139–41.[↩]
- Olive PM, Whitecloud TS 3d, Bennett JT. Lower cervical spondylosis and myelopathy in adults with Down’s syndrome. Spine. 1988;13:781–4.[↩]
- Moore AP, Blumhardt LD. A prospective survey of the causes of nontraumatic spastic parapesis and a tetraparapesis in 585 patients. Spinal Cord. 1997;35:361–7.[↩]
- Adams RD, Victor M. Diseases of the spinal cord, peripheral nerve and muscle. In: Adams RD, Victor M, eds. Principles of neurology. 5th ed. New York:McGraw-Hill, Health Professions Division, 1993:1100–1.[↩][↩]
- Brain NR, Northfield D, Wilkinson M. The neurological manifestations of cervical spondylosis. Brain. 1952;75:187–225.[↩]
- Patten J. Neurological differential diagnosis. 2d ed. New York: Springer, 1996.[↩]
- Watson JC, Broaddus WC, Smith MM, Kubal WS. Hyperactive pectoralis reflex as an indicator of upper cervical spinal cord compression. Report of 15 cases. J Neurosurg. 1997;86:159–61.[↩]
- Denno JJ, Meadows GR. Early diagnosis of cervical spondylotic myelopathy. A useful clinical sign. Spine. 1991;16:1353–5.[↩]
- Al-Mefty O, Harkey LH, Middleton TH, Smith RR, Fox JL. Myelopathic cervical spondylotic lesions demonstrated by magnetic resonance imaging. J Neurosurg. 1988;68:217–22.[↩]
- Freeman TB, Martinez CR. Radiological evaluation of cervical spondylotic disease: limitation of magnetic resonance imaging for diagnosis and preoperative assessment. Perspect Neurol Surg. 1992;3:34–6.[↩]
- Kumar VG, Rea GL, Mervis LJ, McGregor JM. Cervical spondylotic myelopathy: functional and radiographic long-term outcome after laminectomy and posterior fusion. Neurosurgery. 1999;44:771–8.[↩]
- Roberts AH. Myelopathy due to cervical spondylosis treated by collar immobilization. Neurology. 1966;16:951–4.[↩]
- Zeidman SM, Ducker TB. Cervical disk diseases: part 1. Treatment options and outcomes. Nuerosurgy Quarterly. 1992;2:116–43.[↩]
- Saunders RL. Corpectomy for cervical spondylotic myelopathy. In: Menezes AH, Sonntag VK, eds. Principles of spinal surgery. New York: McGraw-Hill Companies, Health Professions Division, 1996: 559–69.[↩][↩][↩]
- Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery. 1998;43:43–50.[↩]
- Bucciero A, Vizioli L, Tedeschi G. Cord diameters and their significance in prognostication and decisions about management of cervical spondylotic myelopathy. J Neurosurg Sci. 1993;37:223–8.[↩]
- Chiles BW 3d, Leonard MA, Choudhri HF, Cooper PR. Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery. 1999;44:762–70.[↩]