Contents
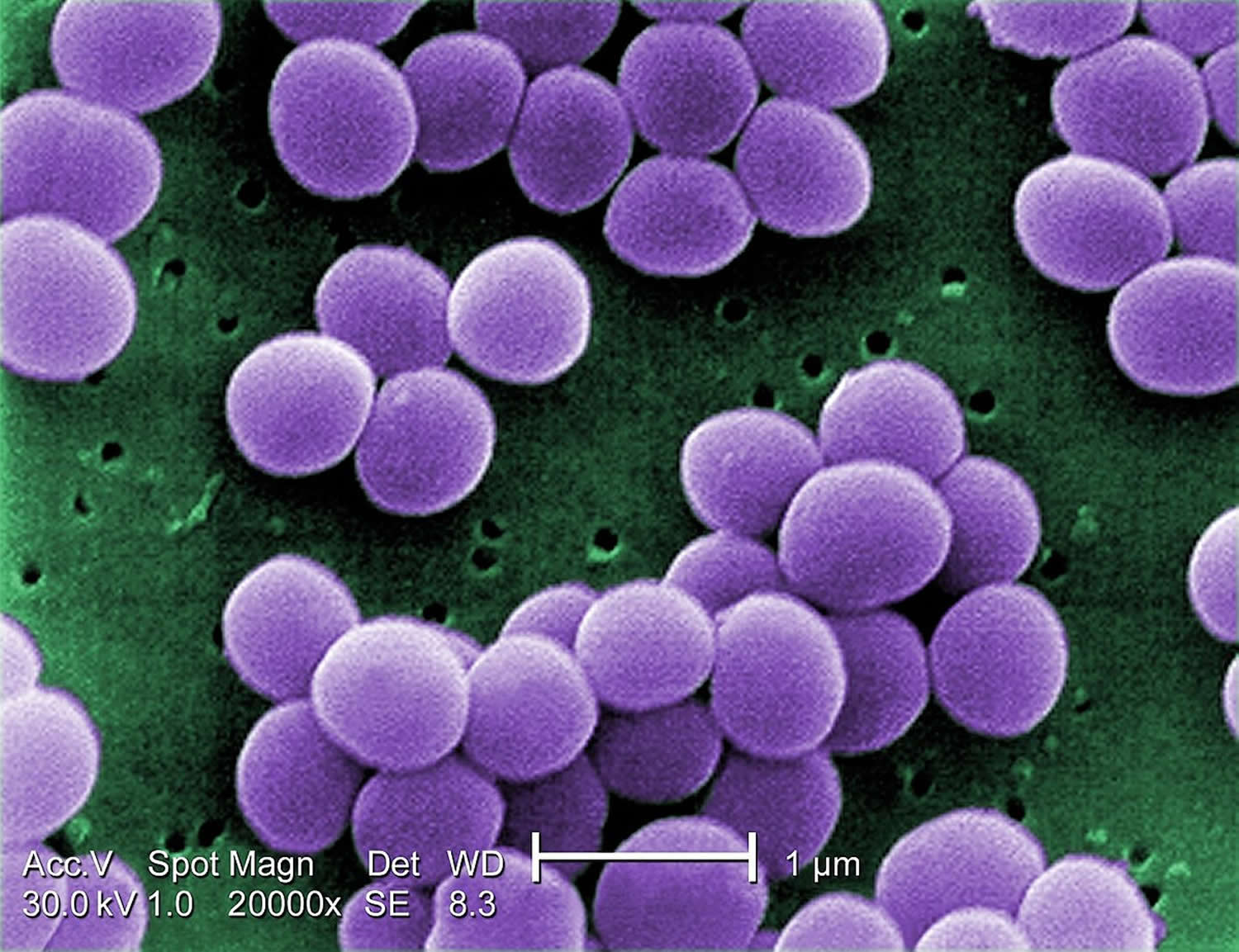
What is a staph infection
Staphylococcus aureus (staph) is both a commensal bacterium and a human pathogen. Staph is a type of bacteria that about 30% of people carry in their noses 1. Many healthy people carry these Staph bacteria on their skin and in their noses without getting sick. But when skin is punctured or broken, staph bacteria can enter the wound and cause infections, which can lead to other health problems. Most of the time, staph does not cause any harm; however, sometimes staph causes infections. Staph infection can be minor (such as pimples or boils) or serious (such as blood infections). Some staph infections may even kill you if the Staph bacteria invade deeper into your body, entering your bloodstream, joints, bones, lungs or heart. A growing number of otherwise healthy people are developing life-threatening staph infections. You can help prevent staph infections in your family by encouraging regular hand washing and daily bathing, and by keeping injured skin clean and covered.
Staph infections can range from minor skin problems to endocarditis, a life-threatening infection of the inner lining of your heart (endocardium). As a result, signs and symptoms of staph infections vary widely, depending on the location and severity of the infection.
Skin infections
Skin infections caused by staph bacteria include:
- Boils. The most common type of staph infection is the boil, a pocket of pus that develops in a hair follicle or oil gland. The skin over the infected area usually becomes red and swollen.
If a boil breaks open, it will probably drain pus. Boils occur most often under the arms or around the groin or buttocks.
- Impetigo. This contagious, often painful rash can be caused by staph bacteria. Impetigo usually features large blisters that may ooze fluid and develop a honey-colored crust.
- Cellulitis. Cellulitis — an infection of the deeper layers of skin — causes skin redness and swelling on the surface of your skin. Sores (ulcers) or areas of oozing discharge may develop, too.
Staphylococcal scalded skin syndrome. Toxins produced as a result of a staph infection may lead to staphylococcal scalded skin syndrome. Affecting mostly babies and children, this condition features fever, a rash and sometimes blisters. When the blisters break, the top layer of skin comes off — leaving a red, raw surface that looks like a burn.
Food poisoning
Staph bacteria are one of the most common causes of food poisoning. Symptoms come on quickly, usually within hours of eating a contaminated food. Symptoms usually disappear quickly, too, often lasting just half a day.
A staph infection in food usually doesn’t cause a fever. Signs and symptoms you can expect with this type of staph infection include:
- Nausea and vomiting
- Diarrhea
- Dehydration
- Low blood pressure
In healthcare settings, these Staph infections can be serious or fatal, including 2:
- Bacteremia or sepsis when bacteria spread to the bloodstream.
- Pneumonia, which predominantly affects people with underlying lung disease including those on mechanical ventilators.
- Endocarditis (infection of the heart valves), which can lead to heart failure or stroke.
- Osteomyelitis (bone infection), which can be caused by staph bacteria traveling in the bloodstream or put there by direct contact such as following trauma (puncture wound of foot or intravenous (IV) drug abuse).
Bacteremia
Also known as blood poisoning, bacteremia occurs when staph bacteria enter a person’s bloodstream. A fever and low blood pressure are signs of bacteremia. The bacteria can travel to locations deep within your body, to produce infections affecting:
- Internal organs, such as your brain, heart or lungs
- Bones and muscles
- Surgically implanted devices, such as artificial joints or cardiac pacemakers
Toxic shock syndrome
This life-threatening condition results from toxins produced by some strains of staph bacteria and has been linked to certain types of tampons, skin wounds and surgery. It usually develops suddenly with:
- A high fever
- Nausea and vomiting
- A rash on your palms and soles that resembles sunburn
- Confusion
- Muscle aches
- Diarrhea
- Abdominal pain
Septic arthritis
Septic arthritis is often caused by a staph infection. The bacteria often target the knees, shoulders, hips, and fingers or toes. Signs and symptoms may include:
- Joint swelling
- Severe pain in the affected joint
- Fever
Staph bacteria can also become resistant to certain antibiotics.
These drug-resistant staph infections include:
- Methicillin-resistant Staphylococcus aureus (MRSA),
- Vancomycin-intermediate Staphylococcus aureus (VISA), and
- Vancomycin-resistant Staphylococcus aureus (VRSA).
When to see a doctor
Go to the doctor if you or your child has:
- An area of red, irritated or painful skin
- Pus-filled blisters
- Fever
You may also want to consult your doctor if:
- Skin infections are being passed from one family member to another
- Two or more family members have skin infections at the same time.
Treatment for Staph Infection
Treatment of a staph infection may include:
- Antibiotics. Your doctor may perform tests to identify of the staph bacteria behind your infection, and to help choose the antibiotic that will work best. Antibiotics commonly prescribed to treat staph infections include certain cephalosporins, nafcillin or related antibiotics, sulfa drugs, or vancomycin.
Vancomycin increasingly is required to treat serious staph infections because so many strains of staph bacteria have become resistant to other traditional medicines. But vancomycin and some other antibiotics have to be given intravenously.
If you’re given an oral antibiotic, be sure to take it as directed, and to finish all of the medication prescribed by your doctor. Ask your doctor what signs and symptoms you should watch for that might indicate your infection is worsening.
- Wound drainage. If you have a skin infection, your doctor will likely make an incision into the sore to drain fluid that has collected there.
- Device removal. If your infection involves a device or prosthetic, prompt removal of the device is needed. For some devices, removal might require surgery.
How do you get a staph infection ?
Anyone can develop a staph infection, although certain groups of people are at greater risk, including people with chronic conditions such as diabetes, cancer, vascular disease, eczema, and lung disease. In a healthcare setting, the risk of more serious staph infection is higher because patients often have weakened immune systems or have undergone procedures such as surgery or have intravenous catheters.
Staph is usually spread through direct contact with another person, not through the air. Staph bacteria can spread through contaminated surfaces and from person to person. People can carry staph bacteria from one area of their body to another — or pass it to other people — via dirty hands or fingernails. That is why it is very important to wash your hands.
It’s also important to encourage kids to keep their skin clean with a daily bath or shower. If your child has a skin condition such as eczema (dermatitis) that makes regular bathing difficult, ask your doctor for advice.
Make sure to keep areas of injured skin — such as cuts, scrapes, and rashes caused by allergic reactions or poison ivy — clean and covered, and follow any directions given by your doctor, to prevent a staph infection.
If you do get a staph infection, and get an antibiotic (medicine), it is important to take your antibiotic until it is finished, even if you are feeling better. If you don’t, the staph germ may become resistant to the antibiotic.
Causes of Staph Infection
Many people carry staph bacteria and never develop staph infections. However, if you develop a staph infection, there’s a good chance that it’s from bacteria you’ve been carrying around for some time.
These bacteria can also be transmitted from person to person. Because staph bacteria are so hardy, they can live on inanimate objects such as pillowcases or towels long enough to transfer to the next person who touches them.
Staph bacteria are able to survive:
- Drying
- Extremes of temperature
- Stomach acid
- High levels of salt
Risk factors for Staph Infection
A variety of factors — including the status of your immune system to the types of sports you play — can increase your risk of developing staph infections.
Underlying health conditions
Certain disorders or the medications used to treat them can make you more susceptible to staph infections.
People who may be more likely to get a staph infection include those with:
- Diabetes who use insulin
- HIV/AIDS
- Kidney failure requiring dialysis
- Weakened immune systems — either from a disease or medications that suppress the immune system
- Cancer, especially those who are undergoing chemotherapy or radiation
- Skin damage from conditions such as eczema, insect bites or minor trauma that opens the skin
- Respiratory illness, such as cystic fibrosis or emphysema
Current or recent hospitalization
Despite vigorous attempts to eradicate them, staph bacteria remain present in hospitals, where they attack the most vulnerable, including people with:
- Weakened immune systems
- Burns
- Surgical wounds
Invasive devices
Staph bacteria can travel along the medical tubing that connects the outside world with your internal organs. Examples include:
- Dialysis tubing
- Urinary catheters
- Feeding tubes
- Breathing tubes
- Intravascular catheters
Contact sports
Staph bacteria can spread easily through cuts, abrasions and skin-to-skin contact. Staph infections may also spread in the locker room through shared razors, towels, uniforms or equipment.
Unsanitary food preparation
Food handlers who don’t properly wash their hands can transfer staph from their skin to the food they’re preparing. Foods that are contaminated with staph look and taste normal.
Prevention of Staph Infection
These commonsense precautions can help lower your risk of developing staph infections:
- Wash your hands. Careful hand-washing is your best defense against germs. Wash your hands briskly for at least 20 seconds, then dry them with a disposable towel and use another towel to turn off the faucet. If your hands aren’t visibly dirty, you can use a hand sanitizer containing at least 60 percent alcohol.
- Keep wounds covered. Keep cuts and abrasions clean and covered with sterile, dry bandages until they heal. The pus from infected sores often contains staph bacteria, and keeping wounds covered will help keep the bacteria from spreading.
- Reduce tampon risks. Toxic shock syndrome is caused by staph bacteria. Since tampons left in for long periods can be a breeding ground for staph bacteria, you can reduce your chances of getting toxic shock syndrome by changing your tampon frequently, at least every four to eight hours. Use the lowest absorbency tampon you can, and try to alternate tampons with sanitary napkins whenever possible.
- Keep personal items personal. Avoid sharing personal items such as towels, sheets, razors, clothing and athletic equipment. Staph infections can spread on objects, as well as from person to person.
- Wash clothing and bedding in hot water. Staph bacteria can survive on clothing and bedding that isn’t properly washed. To get bacteria off clothing and sheets, wash them in hot water whenever possible.
- Also, use bleach on any bleach-safe materials. Drying in the dryer is better than air-drying, but staph bacteria may survive the clothes dryer.
- Take food safety precautions. Wash your hands before handling food. If food will be out for a while, make sure that hot foods stay hot — above 140 F (60 C) — and that cold foods stay at 40 F (4.4 C) or below. Refrigerate leftovers as soon as possible.
Complications of Staph Infections
If staph bacteria invade your bloodstream, you may develop a type of infection that affects your entire body. Called sepsis, this infection can lead to septic shock — a life-threatening episode with extremely low blood pressure. Staph bacteria can also cause toxic shock syndrome.
Skin and Soft Tissue Staph Infection Symptoms
Staph causes a variety of skin and soft tissue infections, ranging from the benign (e.g., impetigo and uncomplicated cellulitis) to the immediately life-threatening. It is the most common pathogen isolated from surgical site infections, cutaneous abscesses, and purulent cellulitis.
While Staph aureus has traditionally been the leading cause of skin and soft tissue infections, its importance has grown exponentially in the past 15 years with the emergence of a worldwide epidemic of community-associated meticillin-resistant Staphylococcus aureus (MRSA) skin and soft tissue infections 3. When community-associated-MRSA was first recognized in the United States in the late 1990s, molecular typing demonstrated that the predominant clone was USA400 4. Since 2000, USA400 has largely been supplanted by a single epidemic clone, USA300, which has been responsible for the rapid shift in epidemiology in the United States. King et al. 5 found that the USA300 clone was the cause of most community-onset Staph skin and soft tissue infections. Among 389 patients in a Georgia health system, 72% of all S. aureus Staph skin and soft tissue infections were caused by MRSA, and ∼85% of these were caused by USA300. Similar findings were seen concurrently in cohorts of patients presenting to emergency departments elsewhere in the United States 6. Increasing rates of Staph skin and soft tissue infections have also been noted in Australia and the United Kingdom. Notably, the increasing incidence of Staph skin and soft tissue infections in these regions cannot be attributed to USA300, which is an infrequent cause of staphylococcal infections in Europe 7 and Australia 8.
The primary defense against Staph infection is the neutrophil response. When Staph aureus enters the skin, neutrophils and macrophages migrate to the site of infection. Staph aureus evades this response in a multitude of ways, including blocking chemotaxis of leukocytes, sequestering host antibodies, hiding from detection via polysaccharide capsule or biofilm formation, and resisting destruction after ingestion by phagocytes.
With the rise in the number of Staph skin and soft tissue infections caused by community-associated-MRSA, there has been intense interest in understanding the enhanced pathogenicity of these strains. Multiple virulence factors appear to contribute, including Panton-Valentine leukocidin (PVL), alpha-hemolysin (also called alpha-toxin), phenol-soluble modulins (PSMs), the arginine catabolic mobile element (ACME), and a regulatory locus referred to as agr. Other candidate virulence determinants continue to be discovered. The sasX gene was found in the S. aureus clone most common in Asia. In addition to a putative role in nasal colonization and pleural infection, the presence of this gene was correlated with larger cutaneous abscesses than those in mice infected with sasX mutant strains 9.
Figure 1. Staph skin and soft tissue infections

Note: Staphylococcus aureus skin and soft tissue infections. Shown are abscess (top left), cellulitis surrounding a pustule (top right), embolic infarcts complicating infective endocarditis (bottom left), and impetigo complicating scabies infection (bottom right).
[Source 10]Folliculitis and Boils
Folliculitis is an infection of hair follicles, tiny pockets under the skin where hair shafts (strands) grow. In folliculitis, tiny white-headed pimples appear at the base of hair shafts, sometimes with a small red area around each pimple. This infection often happens in areas where there’s been friction or irritation, such as with shaving.
Folliculitis often clears up on its own with good skin care. But sometimes it goes on to become a boil (also called a furuncle). With a boil, the staph infection spreads deeper and wider, often affecting the subcutaneous tissue (deeper tissue under the skin) and oil-producing glands (called sebaceous glands).
In the first stage, which parents and kids often miss, the area of skin either begins to itch or becomes mildly painful. Next, the skin turns red and begins to swell over the infected area. Finally, the skin above the infection becomes very tender and a whitish “head” may appear. The head may break, and the boil may begin to drain pus, blood, or an amber-colored liquid. Boils can occur anywhere on the skin, especially under the arms or on the groin or buttocks in kids.
To help relieve pain from a boil, try warm-water soaks, a heating pad, or a hot-water bottle applied to the skin for about 20 minutes, three or four times a day. Make sure that the washcloths used for the soaks are washed after each use. Boils are occasionally treated with oral antibiotics and in some cases need to be surgically drained.
Impetigo
Impetigo is the most common bacterial skin infection of children 11. In general, impetigo presents as bullous or papular lesions that progress to crusted lesions, without accompanying systemic symptoms, on exposed areas of the body (usually the face or extremities). Recent studies of impetiginous lesions found recovery rates of 29 to 90% and 57 to 81% for Streptococcus pyogenes and S. aureus, respectively 12.
Figure 2. Impetigo

Cutaneous abscess and Nonpurulent cellulitis
While the hallmark of Staph skin and soft tissue infections is generally regarded as the cutaneous abscess 13, other manifestations of skin infection are also encountered clinically. Nonpurulent cellulitis may be caused by Staph infection in a minority of cases, although the lack of a diagnostic gold standard and variability introduced by different microbiological methods obscure the true microbiology of this condition 14. While Staph cellulitis most commonly involves the lower extremities, it may also involve other regions, including the upper extremities, abdominal wall, and face. It vies for primacy with streptococci as a cause of preseptal and orbital cellulitis (321,–323).
Figure 3. Staph cellulitis

Scalded Skin Syndrome
Scalded skin syndrome most often affects newborns and kids under age 5. The illness usually starts with a small staph skin infection, but the staph bacteria make a toxin that affects skin all over the body. The child has a fever, rash, and sometimes blisters. As blisters burst and the rash passes, the top layer of skin sheds and the skin surface becomes red and raw, like a burn.
Scalded skin syndrome is a serious illness that affects the body in the same way as serious burns. It needs to be treated in a hospital. After treatment, most kids make a full recovery.
Necrotizing fasciitis
Necrotizing fasciitis is another cutaneous syndrome caused by Staph infection. Necrotising fasciitis is a very serious bacterial infection of the soft tissue and fascia (a sheath of tissue covering the muscle) 15. The bacteria multiply and release toxins and enzymes that result in thrombosis (clotting) in the blood vessels. The result is destruction of the soft tissues and fascia. In a review of 843 patients with wound cultures positive for MRSA, 14 isolates were identified as being associated with necrotizing fasciitis or myositis. Coexisting conditions among those patients included injection drug use in 6/14 (43%) patients, previous MRSA infections in 3/14 (21%), diabetes mellitus in 3/14 (21%), and hepatitis C in 3/14 (21%) 16. In Taiwan, a review of 53 patients with necrotizing fasciitis revealed that 38% of infections were caused by Staph infection, 60% of which were caused by MRSA 17.
Figure 4. Necrotising fasciitis

Pyomyositis
Pyomyositis can occur with both MSSA (Methicillin-sensitive Staphylococcus aureus) and MRSA (Methicillin-resistant Staphylococcus aureus). Tropical pyomyositis is a rare condition characterized by primary muscle abscesses arising within large skeletal muscles. It has a tropical predilection, accounting for up to 1 to 4% of hospital admissions in some tropical countries, with Staph being responsible for an estimated 90% of these presentations 18. It is less common in temperate climates, where it occurs primarily in children and young adults 19 and has been reported in association with HIV 20.
Surgical site infections
Surgical site infections occur after 2 to 5% of all surgeries 21, although there is considerable heterogeneity depending on the type of procedure, population studied, comorbid illnesses, experience of the surgeon, setting, and antimicrobial prophylaxis utilized. According to 2009-2010 U.S. National Healthcare Safety Network data, Staph was the most common cause of surgical site infections overall, accounting for 30% of infections. Of these, 44% of isolates were methicillin resistant 22. In registrational trials of complicated Staph skin and soft tissue infections, even higher proportions of surgical site infections due to Staph have been found; for example, 49% of surgical site infections in ATLAS studies (telavancin versus vancomycin) were due to Staph aureus 23.
A particularly devastating surgical site infection is mediastinitis complicating median sternotomy for cardiac surgery. Staph aureus is the most common cause of postoperative mediastinitis 24. Fowler et al. 25 demonstrated that the presence of Staph becteremia in the postoperative period was highly predictive of a diagnosis of mediastinitis, with a likelihood ratio of 25, compared to blood cultures positive for other pathogens or negative blood cultures. These findings were subsequently independently validated 26. Thus, the presence of Staph becteremia following sternotomy mandates aggressive investigation to exclude the possibility of postoperative mediastinitis.
Treating Staph Skin Infections
You can treat most small staph skin infections by:
- washing the skin with an antibacterial cleanser
- using warm soaks (to keep the infection from spreading, use a towel only once when you soak or clean an area of infected skin, and then wash it)
- applying antibiotic ointment, if prescribed by your doctor
- covering the skin with a clean dressing or bandage
Your doctor may prescribe an oral antibiotic for your staph skin infection. If so, give the antibiotic on schedule for as many days as the doctor directs.
More serious staph infections might need to be treated in a hospital, and an abscess (or pocket of pus) that doesn’t respond to home care might need to be drained.
See the doctor whenever you have an area of red, irritated, or painful skin, especially if you see whitish pus-filled areas or you have a fever or feels sick. Also, see your doctor if skin infections seem to be passing from one family member to another or if two or more family members have skin infections at the same time.
Risk factors for Staph Bacteremia
Age is a powerful determinant of Staphylococcus aureus bacteremia incidence, with the highest rates of infection occurring at either extreme of life 27. Studies consistently demonstrate high rates in the first year of life, a low incidence through young adulthood, and a gradual rise in incidence with advancing age. For example, the incidence of Staph bacteremia is >100 per 100,000 person-years among subjects >70 years of age 28 but is only 4.7 per 100,000 person-years in younger, healthier U.S. military personnel 29. Male gender is consistently associated with increased Staph bacteremia incidence 30, with male-to-female ratios of ∼1.5. The basis for this increased risk is not understood.
The incidence of Staph bacteremia is also associated with ethnicity. In the United States, the incidence of invasive Methicillin-resistant Staphylococcus aureus (MRSA) in the black population (66.5 per 100,000 person-years) is over twice that in the white population (27.7 per 100,000 person-years) 31. In Australia, the incidence of Staph bacteremia in the indigenous population is 5.8 to 20 times that of nonindigenous Australians 32. Similarly, Maori and Pacific Island people have significantly higher rates of incidence of Staph bacteremia than do those of European ethnicity in New Zealand 33. Differences in markers of the socioeconomic status of indigenous compared to nonindigenous populations do not fully explain the disparity between these groups 32. The contribution of host genetic susceptibility to these ethnic differences has not yet been investigated.
The HIV-infected population has a significantly increased incidence of Staph bacteremia. Two studies reported incidences of Staph bacteremia in HIV-infected patients of 494 per 100,000 person-years 34 and 1,960 per 100,000 person-years 35, or 24 times that of the non-HIV-infected population 34. Although much of this increase results from high rates of injection drug use in the HIV-infected population, even the non-injection drug-using HIV-infected population exhibits higher rates of Staph bacteremia than those in the non-HIV-infected population 34. Among HIV-infected individuals, a low CD4 count was independently associated with Staph bacteremia. Also, compared to injection drug users, men who have sex with men were likely to have a low CD4 count and to have nosocomial Staph bacteremia 34. Thus, HIV-infected injection drug users tend to acquire community-onset Staph bacteremia as a consequence of injection drug use, whereas men who have sex with men have higher rates of nosocomial Staph bacteremia.
The high risk of Staph bacteremia in the overall injection drug user population can be inferred from a Dutch study that monitored 758 injection drug users for 1,640 person-years and determined that there were 10 confirmed episodes of Staph infective endocarditis 36. Based on these figures, the incidence of Staph bacteremia was at least 610 per 100,000 person-years. In the setting of injection of material into the bloodstream, additional factors contributing to the high incidence of Staph bacteremia include an increased prevalence of Staph colonization compared to that in the general population 37, frequent skin and soft tissue infections 38, and a drug-using environment that facilitates the person-to-person transmission of Staph 39.
Hemodialysis patients are also at a greatly increased risk of Staph bacteremia. The incidences of Staph bacteremia in hemodialysis-dependent patients were 3,064 per 100,000 person-years in Taiwan 40, 17,900 per 100,000 person-years in Ireland 41, and 4,045 to 5,015 per 100,000 person-years in the United States 42. The predominant risk factor for these patients is the presence of an intravascular access device and in particular the use of a cuffed, tunneled catheter (e.g., permacath) for dialysis 41. However, other host factors that result in an impairment of the host immune defense, including neutrophil dysfunction 43, iron overload 44, diabetes 45, and increased rates of colonization 45, may also increase the likelihood of invasive Staph infections. The infrequent vancomycin dosing strategy often used among hemodialysis-dependent patients may not maintain an adequate trough level in high-flux, large-pore-size artificial kidneys 46, increasing the risk for relapsing Staph bacteremia.
Staph Clinical Syndromes
Epidural Abscess
Epidural abscesses can be intracranial or spinal. Intracranial epidural abscesses are much less common than spinal epidural abscesses and usually follow surgery or trauma. Although a rare infection [∼1 in 20,000 hospitalized patients 47], spinal epidural abscess is the second most common infectious cause of medical malpractice in the United States 48. The incidence of epidural abscess appears to have increased over the past 30 years (765). This is likely to be in part due to the increasing availability of magnetic resonance imaging (MRI) (which is much more sensitive than previous modalities) and partly due to the increasing use of epidural catheters and electrodes for pain management. Staph aureus is the most common causative agent of spinal epidural abscess, accounting for 60 to 73% of all cases 49.
Pathophysiology and clinical manifestations of Staph Epidural Abscess
An epidural abscess may arise by hematogenous seeding from an episode of Staph becteremia, by contiguous spread from an adjacent focus (such as psoas abscess or vertebral osteomyelitis), or due to direct inoculation from trauma, spinal surgery, or the placement of epidural catheters 49. Although a spinal epidural abscess may occur anywhere from the cervical to the sacral spine, it is generally more likely to occur where the epidural space is larger. Thus, posterior epidural space involvement is more common than anterior epidural space involvement, and lumbar and lower thoracic epidural abscesses are more common than cervical epidural abscesses 50. Because the epidural space is a continuous vertical region, epidural abscesses generally spread over several vertebral levels and rarely may involve the entire spine. The most important potential consequence of spinal epidural abscesses is damage to the spinal cord and nerve roots, which can occur due to direct compression of the cord by an expanding collection of pus 51 or indirectly through arterial or venous ischemia. The major risk factors for Staph aureus spinal epidural abscess include diabetes mellitus 49, injection drug use 49, recent spinal surgery or trauma, and recent placement of epidural injections, catheters, or stimulating wires 52. Approximately 2.5% of patients with Staph bacteremia have epidural abscesses 53. Thus, any patient with Staph bacteremia who complains of new or changing back pain should undergo spinal imaging, preferably with MRI, to evaluate the possibility of an epidural abscess.
The classic clinical triad for epidural abscess is back pain, fever, and neurological signs; however, the complete triad is present in only a minority of patients at presentation 54. For this reason, the diagnosis of spinal epidural abscess is often not initially considered. For example, only 40% of admitting diagnoses included spinal epidural abscess as the suspected diagnosis for one series of 43 patients ultimately found to have epidural abscess 47. Darouiche et al. 47 described the following clinical staging system, which is useful for determining the timing and nature of management of spinal epidural abscesses: stage 1, back pain at the affected vertebral level; stage 2, nerve root pain radiating from the involved area; stage 3, objective motor and sensory loss and/or bladder and bowel dysfunction; and stage 4, paralysis. This staging system is important because once patients enter stages 2 and 3, their spinal cord is under threat, and urgent surgical decompression is required.
Management of spinal epidural abscess
In general, surgical decompression (laminectomy, debridement of infected or necrotic tissue, and drainage of pus) is required to achieve a successful outcome in cases of Staph aureus spinal epidural abscess. This is in conjunction with a long course of high-dose i.v. antibiotic therapy 49. Because of the possibility of permanent paralysis, spinal epidural abscess is a medical and surgical emergency. Once paralysis is established for >24 to 48 h, the damage is likely to be permanent. Thus, the key step is the early recognition of the possibility of spinal epidural abscess and rapid investigation to confirm the diagnosis. Most authors suggest that surgical decompression be performed urgently (within 24 h of diagnosis) in patients with Staph aureus spinal epidural abscess 47. However, it is increasingly being recognized that select patients may not require surgical intervention. Such patients include those in whom paralysis has been present for >48 h and those with early (clinical stage 1) infection with small abscesses, where a pathogen has been identified by blood culture or computed tomography (CT)-guided aspiration of the abscess 55. MSSA spinal epidural abscesses should be treated with ∼6 weeks of a high-dose i.v. antistaphylococcal β-lactam (e.g., 2 g nafcillin every 4 h [q4h] i.v.). For MRSA, treatment with vancomycin for a similar duration is advised, aiming for plasma levels of 15 to 20 mg/liter.
Meningitis
Staph aureus is an uncommon cause of bacterial meningitis, accounting for 4.9 to 6.4% of cases 56. Staph aureus meningitis may either arise by hematogenous spread from a non-CNS focus of infection or be secondary to neurosurgical intervention 57. Hematogenous Staph aureus meningitis is usually community acquired 58 and, compared with postsurgical S. aureus meningitis, typically affects older individuals (mean age of 59 years versus 40 years) 59 with severe medical comorbidities such as diabetes or chronic kidney disease 58. The initial source of hematogenous Staph aureus meningitis is generally infective endocarditis, pneumonia, or Staph skin and soft tissue infection 60. The mortality rate for hematogenous Staph aureus meningitis is higher (43 to 50%) than that occurring postsurgically (14 to 25%) 59. Among Staph aureus meningitis cases, methicillin resistance has been increasing in recent years 61. Specifically, Pintado et al. 62 conducted a retrospective, multicenter study examining MRSA meningitis in adults over a 25-year period (1981 to 2005). This group found that nearly half of MRSA meningitis cases arose in the last 5 years of the study. The 30-day mortality rate for these patients was 31%. Most MRSA meningitis cases are nosocomial and postsurgical 62.
Clinical manifestations and risk factors for Staph Meningitis
Because meningitis is a rare complication for patients with Staph bacteremia, occurring in 1.7% of 724 prospectively identified patients with Staph bacteremia, clinicians need to be alert to its possibility 53.
Staph aureus meningitis typically presents with one or more of the following signs or symptoms 62:
- persistent fever,
- headache,
- stiff neck, and
- vomiting.
Fever and change in consciousness are the two most common clinical symptoms 63. Patients with hematogenous Staph aureus meningitis typically have a greater degree of CSF leukocytosis than do postsurgical patients 59.
The major predisposing factors for postsurgical meningitis are (i) the presence of an intrathecal device or ventriculoperitoneal shunt 58, (ii) recent neurosurgery, and (iii) a CSF leak 58. Of note, Staph aureus is the second leading cause of bacterial meningitis among patients with a ventriculoperitoneal shunt 64. Intravenous drug use is an important risk factor for hematogenous Staph aureus meningitis, being present in 52% of patients in a recent series of 21 cases of hematogenous Staph aureus meningitis from a single center in the United States 58 but in only 12.5% of 96 cases from a nationwide Danish study 65.
Risk factors for mortality among patients with Staph aureus meningitis include a hematogenous compared with a postsurgical source [e.g., 56% mortality for a hematogenous source versus 18% for a postsurgical source within a national Danish study 66], increasing age and number of comorbidities, the presence of septic shock and concurrent infective endocariditis 63.
Management of Staph Meningitis
The IDSA recommends high-dose i.v. nafcillin or oxacillin to treat MSSA (Methicillin-resistant Staphylococcus aureus) meningitis and vancomycin for MRSA (Methicillin-resistant Staphylococcus aureus) meningitis 67. Vancomycin has poor penetration into the CSF of ∼1% through uninflamed and 5% through inflamed meninges 63, and in practice, it can be difficult to achieve therapeutic levels within the CSF. This is even more of an issue when the vancomycin MIC (minimum inhibitory concentration) of an MRSA isolate approaches or exceeds 2 μg/ml. In such dire settings, consideration can be given to unproven adjunctive therapies such as the intrathecal administration of vancomycin 68 or the addition of antibiotics such as linezolid (CSF penetration, 66%), TMP-SMX (CSF penetration, ∼50%), or daptomycin (CSF penetration, 6%).
Toxic Shock Syndrome
Staph aureus toxic shock syndrome was first described in 1978 by Todd et al. 69, who reported the illness in a group of 7 children. Shortly thereafter, Staph aureus toxic shock syndrome became linked with superabsorbent tampons in menstruating women in the 1980s 70, reaching an annual infection rate of 13.7 per 100,000 menstruating women 71. After the removal of highly absorbent tampons from the market, the annual incidences of S. aureus TSS declined to 1 per 100,000 menstruating women and 0.3 per nonmenstruating persons 72. The incidence of Staph aureus toxic shock syndrome has remained stable since that time, with the current annual incidences reported to be 0.69 per 100,000 menstruating women and 0.32 per 100,000 total population 73. Currently, the numbers of menstrual and nonmenstrual cases of staphylococcal toxic shock syndrome are similar, and the most common foci of infection in nonmenstrual cases are Staph skin and soft tissue infections 73. Nonmenstrual cases have been associated with a higher mortality rate than menstrual cases 74.
Clinical manifestations and diagnosis of toxic shock syndrome
Staph aureus toxic shock syndrome is a superantigen-mediated process. Some strains of Staph aureus secrete an exotoxin called toxic shock syndrome toxin 1 (TSST-1) 75. TSST-1 cross-links the T-cell receptor with major histocompatibility complex class II (MHC-II) on antigen-presenting cells, triggering large-scale T-cell activation and massive cytokine release 76. This leads to an overwhelming systemic inflammatory response syndrome and is manifested by septic shock with organ failure. The CDC reported diagnostic criteria for staphylococcal toxic shock syndrome 77.
A confirmed case must meet all of the following criteria:
- (i) a fever of >38.9°C,
- (ii) shock (systolic blood pressure of <90 mm Hg despite adequate fluid resuscitation),
- (iii) a diffuse macular erythematous rash (typically followed 1 to 2 weeks later by desquamation), and
- (iv) specific abnormalities involving at least three organ systems:
- The organ system involvements that can be included are as follows:
- (i) gastrointestinal, with vomiting or diarrhea;
- (ii) musculoskeletal, with severe myalgia or creatinine kinase levels >2 times the upper limit of normal;
- (iii) renal, with serum creatinine levels >2 times the upper limit of normal;
- (iv) hepatic, with bilirubin or transaminase levels >2 times the upper limit of normal;
- (v) hematologic, with platelet counts of <100,000 platelets/μl; and
- (vi) CNS, with delirium without focal signs.
- The organ system involvements that can be included are as follows:
Management of toxic shock syndrome
The key aspects of treatment of Staph aureus toxic shock syndrome include identifying and removing the source of Staph aureus toxin production (e.g., tampon or surgical wound) and supportive care 78. In the setting of postoperative Staph aureus toxic shock syndrome, the involved surgical wound often appears normal 74. However, this benign appearance in no way reduces the need for surgical debridement in patients with wound-associated Staph aureus toxic shock syndrome. Antibiotics, in contrast, play a secondary role in the management of toxic shock syndrome. Because it can block the production of exotoxins by the bacterial ribosome, clindamycin or linezolid is often added to standard antibiotic therapy 79. Intravenous immunoglobulin may also be effective, although clinical evidence of benefit is not well established, and there is less evidence supporting the use of i.v. immunoglobulin to treat staphylococcal toxic shock syndrome than for streptococcal toxic shock syndrome. Nonetheless, it is recommended that i.v. immunoglobulin be considered for patients who have had no clinical response to aggressive supportive therapy within 6 h 80.
Osteoarticular Infections
Staph aureus is the most common pathogen in all three major classes of osteoarticular infection, namely, osteomyelitis 81, native joint septic arthritis 82, and prosthetic joint infection 83. As staphylococcal osteoarticular infections in children are common and have distinctive clinical and management issues compared to those in adults, we include an in-depth discussion of this important subpopulation.
Osteomyelitis
Osteomyelitis is an infection of bone resulting in its inflammatory destruction, bone necrosis, and new bone formation. The Waldvogel classification system 84 describes three types of osteomyelitis: hematogenous osteomyelitis, contiguous-focus osteomyelitis (from adjacent structures such as joint spaces or soft tissues or from trauma or surgery with direct implantation of organisms), and osteomyelitis with vascular insufficiency (most commonly in patients with diabetes or peripheral vascular disease and generally involving the foot). Staph aureus is the predominant cause of osteomyelitis in all of these categories and is identified in 30 to 60% of cases. Hematogenous osteomyelitis generally involves the ends of long bones in children and adolescents and the axial skeleton in older adults (408), partly due to the blood supply to vertebrae in adults being more extensive than that to the long bones. This section principally focuses on hematogenous osteomyelitis that most commonly manifests as vertebral osteomyelitis in adults and long bone osteomyelitis in children, where Staph aureus is typically the key pathogen.
Clinical manifestations and outcomes of Osteomyelitis
Vertebral osteomyelitis generally involves the endplates of two adjacent vertebrae and the intervening disc space. The most common route of spread is hematogenous seeding to the vertebral endplates, and from here, the infection spreads directly into the disc space. Hence, the term “discitis” is a misnomer, since disc space infection is secondary. The exception is where infection has been directly introduced to the disc space (e.g., following a surgical microdiscectomy). The hallmark of vertebral osteomyelitis is back pain, being present in 85 to 100% of patients. Localized vertebral percussion tenderness is present in >80% of cases, but fever is present in anywhere from 18 to 83% of cases in various case series. A significant minority of patients have signs of nerve compression (such as limb weakness) at presentation, and one-quarter of patients with vertebral osteomyelitis will ultimately develop paralysis or significant neurologic dysfunction 85. Among 133 consecutive patients with SAB and concomitant vertebral osteomyelitis, the most frequent primary foci or portals of entry of infection were the skin (21%) and urinary tract (10%). However, 71/133 patients (53%) had no identified primary focus 86. Comparisons between vertebral osteomyelitis caused by MRSA and that caused by MSSA have found that patients with infections due to MRSA have more comorbidities and are more likely to have had recent nonspinal surgery (390). Lumbar vertebrae are most frequently affected, followed by thoracic and then cervical regions. Notably, the diagnosis of vertebral osteomyelitis is frequently delayed, with an interval of >1 month from symptom onset to diagnosis for the majority of patients 85. Delayed diagnosis has been associated with poorer longer-term outcomes, including death, chronic pain, and residual disability 85.
The peripheral WBC (white blood cell) count is raised in a variable proportion of patients with osteomyelitis, but the erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) level are raised in 95 to 100% of patients with acute osteomyelitis. A systematic review of 14 studies of vertebral osteomyelitis found that the reported yield from blood cultures for a microbiological diagnosis was 58% (range, 30 to 78%) 87. Therefore, in the appropriate clinical and radiological settings, positive blood cultures can eliminate the need for diagnostic biopsy or aspiration of infected bone for culture. However, bone biopsy for culture and histology should be pursued if blood cultures are negative, as it provides a higher diagnostic yield (77%; range, 47 to 100%) 87. Where possible, the biopsy specimen is best obtained prior to antibiotic treatment. Several investigators have found that the microbiological yield from biopsy specimens of patients on antibiotics is ∼50% lower than that from biopsy specimens obtained prior to antibiotic treatment 88. Where an initial percutaneous biopsy specimen is negative, there may be value in obtaining a second percutaneous biopsy specimen. Gras et al. 89 examined a cohort of 136 patients with vertebral osteomyelitis who were all blood culture negative and who had not received antibiotics in the previous 2 weeks. Performance of a second biopsy after an initial negative result led to a microbiological diagnosis in 80% (74/93) of cases, versus 44% (60/136) with only one biopsy specimen. While significantly more invasive, open surgical biopsy is also more likely to yield a diagnosis than needle biopsy. For example, in a series of 70 patients from Missouri, an open biopsy had a 93% diagnostic yield, compared with 48% for radiologically guided needle biopsy 90. In summary, a microbiological diagnosis should be sought to guide subsequent therapy. One suggested approach to the diagnosis of vertebral osteomyelitis begins with blood cultures, followed by an initial percutaneous biopsy, a second percutaneous biopsy if the initial biopsy specimen is sterile, and an open biopsy if clinically indicated 91.
The short-term mortality rates for osteomyelitis are substantial, at 2.8 to 7.7% for nonvertebral osteomyelitis 92 and 6 to 16% for vertebral osteomyelitis 85. Furthermore, health care costs 93 and rates of long-term functional impairment 85 are also high. Akiyama et al. 94 found that for vertebral osteomyelitis, higher mortality rates were significantly associated with older age (patients aged 60 to 69, 70 to 79, and ≥80 years), compared with those aged ≤59 years), hemodialysis use, diabetes, liver cirrhosis, malignancy, and infective endocarditis .
Management of osteomyelitis
The management of vertebral osteomyelitis caused by Staph aureus requires prolonged courses of antibiotics. Jensen et al. 86 found that among 114 patients with bacteremic Staph aureus osteomyelitis, recurrence was more likely in patients receiving <8 weeks of antibiotic therapy than in those receiving ≥8 weeks of therapy. Park et al. 95 determined that for 62 patients with vertebral osteomyelitis due to MRSA, patients receiving <8 weeks of antibiotic treatment were 4.8 times more likely to relapse than those receiving ≥8 weeks of therapy. There was no such association for 77 patients with MSSA infections 95. In contrast, Roblot et al. 96 determined that for 120 patients, outcomes were similar for 36 patients treated at one center with a median of 6 weeks of total therapy and for 84 patients treated at another center with a median of 10 weeks total therapy. These data and other observational data have led to recommendations that range from 6 weeks 96 to 12 weeks 91 of antibiotic treatment. Most recently, Bernard et al. 97 compared antibiotic treatments for 6 weeks and 12 weeks for patients with pyogenic vertebral osteomyelitis. In an open-label, noninferiority clinical trial design powered to achieve an absolute margin of 10%, 359 patients from 71 French medical care centers were randomly assigned to either of the treatment durations. Of these infections, 145 (41%) were due to S. aureus, 95% (n = 137) of which were due to MSSA. The primary endpoint was defined as the proportion of patients who were classified as being cured at 1 year by a masked independent validation committee. In an intention-to-treat analysis, 6 weeks of antibiotic treatment was noninferior to 12 weeks of antibiotic treatment, suggesting that the standard duration of antibiotic treatment for patients with this infection could be reduced to 6 weeks 97 . Where clinical improvement is slow, undrained or unremoved foci exist, the CRP level is slow to normalize, or infection is due to MRSA, we consider it prudent to extend antibiotic therapy to at least 8 weeks. For patients responding well to initial i.v. therapy, observational data suggest that a switch to oral therapy after 2 weeks may be safe. Results reported by Bernard et al. 97 are also supportive in that the overall rate of treatment success in their randomized clinical trial was 91% with a median duration of 14 days of i.v. therapy.
Osteoarticular Infections in Children
The incidence of osteoarticular infections in children ranges from 7 to 22 per 100,000 person-years based on studies from Europe 98. These infections are more common in males than in females (with incidences in French children of 24 per 100,000 person-years for boys and 19 per 100,000 person-years for girls) and in toddlers than in other age groups 99. Some ethnic groups may be at higher risk, with Maori and Pacific Islander populations being overrepresented in a study involving 813 cases of acute osteomyelitis in New Zealand 100. In the United States, community associated-MRSA has become considerably more prominent as a cause of acute osteoarticular infections since 2000. In a study of 158 cases in Tennessee, the proportion of osteoarticular infections due to community associatedA-MRSA rose from 4% to 40% from 2000 to 2004 101. Similarly, the proportion of cases of acute osteomyelitis due to CA-MRSA was 6% in 1999 to 2001 compared to 31% in 2001 to 2003 in Dallas, TX 102. In Houston, TX, between 2001 and 2010, 195 of 376 (52%) cases of Staph aureus osteomyelitis were due to MRSA 103.
Clinical manifestations and outcomes of Acute osteomyelitis
Acute hematogenous osteomyelitis in children presents with fever and malaise, local pain, and point tenderness and most commonly involves the metaphysis of the tibia or the femur, resulting in limping or an inability to walk 104. The pain is often poorly localized but becomes more focal over time. The hallmark of the pain is its constant nature. Overlying redness and swelling are often present, which may create diagnostic confusion. For diagnostic purposes, CRP analysis is highly sensitive and thus has value in excluding the diagnosis of acute osteoarticular infection. In a prospective study of 265 osteoarticular infections in children, using a cutoff of 20 mg/liter, CRP analysis had a sensitivity of 95% for the diagnosis of acute osteomyelitis; and the combination of CRP and ESR (with a cutoff 20 mm/h) analyses provided a sensitivity of 98% 105. Additionally, CRP analysis can be used to monitor the response to antibiotic treatment 105. Peltola and Paakkonen provide an excellent diagnostic algorithm for acute osteomyelitis in children 104.
With regard to acute osteomyelitis caused by Staph aureus, Ju et al. 106 found four clinical parameters that could predict the probability of acute osteomyelitis in children due to MRSA compared to MSSA: temperature of >38°C, hematocrit level of <34%, white blood cell count of >12,000 cells/μl, and CRP level of >13 mg/liter. However, this study suffers from having only 11 patients with MRSA and a lack of genotyping data and from its single-center design 106. An attempt to validate this clinical prediction algorithm among 58 patients (MRSA, n = 16; MSSA, n = 42) in Phoenix, AZ, found the algorithm to have a poor predictive value 107. Without genotyping data, it seems likely that the study by Ju et al. and previous studies that also compared cases of acute osteomyelitis due to MRSA versus MSSA found discriminators between USA300 and other Staph aureus clones rather than between MRSA and MSSA per se.
With the emergence of community associated-MRSA, deep venous thrombosis (DVT) adjacent to the site of osteomyelitis has been described by several groups 108. Deep venous thrombosis (DVT) with acute osteomyelitis has been associated with MRSA, PVL-positive strains of Staph aureus and USA300 in particular 109. Compared to patients with acute osteomyelitis but no DVT, those with DVT were consistently unwell, likely to be bacteremic, and likely to have pulmonary involvement (presumably due to septic pulmonary emboli), and MRSA was overrepresented. Thus, a high index of suspicion for DVT is required for children with acute osteomyelitis who are critically unwell or who have pulmonary involvement, and Doppler ultrasound screening near the site of infection should be considered 110.
Nonetheless, most large series suggest that for acute osteomyelitis in children, outcomes are generally favorable. Only 1 child out of 1,000 with osteomyelitis died in a case series from France 99, and of 131 prospectively monitored cases in Finland, only 2 children developed mild sequelae (varus deformity of tibia and ankle pain during exercise) 111. The mean length of hospital stay was 8.6 days in the French series 99.
Management of Acute osteomyelitis in Children
Empirical treatment for acute osteomyelitis in children is dictated by the local antibiogram of Stph aureus. Where the prevalence of MRSA is <10% among community Staph aureus strains, an antistaphylococcal penicillin or cephalosporin is recommended; where the prevalence of community associated-MRSA is >10% and the rate of clindamycin resistance is <10%, clindamycin is recommended; and where both the prevalence of community associated-MRSA and the rate of clindamycin resistance are >10%, vancomycin should be used 104. If the child is severely ill and has suspected acute osteomyelitis or septic arthritis, it is prudent to treat the child with both vancomycin and an antistaphylococcal β-lactam until bacterial susceptibilities are known 103.
For pediatric acute osteomyelitis caused by MSSA, an early switch to oral therapy appears safe. A prospective study of 70 children with either septic arthritis or osteomyelitis demonstrated that an algorithmic approach resulted in 59% of children converting to oral therapy after 3 days of i.v. therapy and 86% converting to oral therapy after 5 days. All 70 children had good outcomes at 1 year of follow-up 112. Similarly, Peltola et al. switched 131 patients to oral therapy after a median of 3 to 4 days of i.v. therapy, with excellent outcomes 113. An early switch to oral therapy is particularly important for children, as the risk for central line-related complications is high. Ruebner et al. 114 found that of 75 patients who received >2 weeks of treatment for acute osteomyelitis through a central venous catheter, 41% developed at least one central venous catheter-related complication.
A prospective, quasirandomized, controlled, open-label trial involving 252 children with osteoarticular infections (82/252 with osteomyelitis and 189/252 with Staph aureus [all MSSA]; the proportion of cases of osteomyelitis with MSSA was not reported) in Finland determined that oral clindamycin or a first-generation cephalosporin was equally efficacious as follow-up therapy 115. The same investigators also determined in an randomized control trial involving 131 children with acute osteomyelitis (117 with S. aureus, all MSSA) that 20 days of total therapy resulted in outcomes equivalent to those with 30 days of total therapy 111. In children with septic arthritis, a separate Finnish study (517) found that a duration of 10 days of total antibiotic therapy was equivalent to 30 days of therapy. Of 130 cases, only 1 developed a late-onset infection following completion of therapy, and this case was in the 30-day arm of the study. A systematic review 116 noted that the above-mentioned randomized clinical trials are only of moderate quality, principally due to a lack of blinding, and concluded that the recommendations of treatment for acute osteomyelitis of 3 to 4 days of i.v. therapy followed by oral antibiotics for a total treatment duration of 3 weeks should be regarded as being supported by only weak evidence (grade 2B).
Given the severity of osteoarticular infections caused by community associated-MRSA and their conspicuous absence in the Finnish studies, it is unknown whether abbreviated i.v. and subsequent oral therapies can effectively treat acute osteomyelitis due to MRSA. This point is acknowledged by Peltola and Paakkonen 104 and also in IDSA guidelines for MRSA infections 117. Both reports suggest that acute osteomyelitis due to MRSA should be treated with a minimum of 4 to 6 weeks of total therapy. Additionally, it is recommended that infants <3 months of age receive a longer course of i.v. therapy due to concerns over the absorption and efficacy of oral antibiotics 116.
Only 12% of 130 patients with septic arthritis in a Finnish study 118 required a surgical procedure, and in a separate trial, 62/131 (47%) cases of acute osteomyelitis received resectional surgery to the bone cortex 111. However, higher rates of surgery have been noted in the United States. For example, Tuason et al. found that of 57 cases of acute osteomyelitis, 41 (72%) children required surgery, 12 of whom underwent ≥2 surgeries 119. Additional concerns are that hip septic arthritis in children can result in ischemic necrosis of the femoral head and that sequelae of septic arthritis may be more common than for osteomyelitis. An Australian study including 44 children, in whom S. aureus was the causative organism in 76% of cases, found that 10% of children at 12 months had residual joint dysfunction 120. Thus, careful clinical assessment and monitoring are mandatory. For patients with extensive disease or where levels of inflammatory markers are not being reduced as expected, ongoing reassessment of the need for surgical intervention is advised.
Adjunctive dexamethasone appears to be a promising intervention to accelerate recovery and decrease residual morbidity in children with native joint septic arthritis. Odio et al. 121 randomized 123 children with septic arthritis (67% of whom had infections due to Staph aureus) to receive 4 days of adjunctive i.v. dexamethasone in addition to antibiotics. They found that a significantly lower proportion of patients in the dexamethasone group had residual joint dysfunction after 12 months of follow-up (2% versus 26%). Harel et al. 122 randomized 49 children to receive 4 days of dexamethasone or placebo for septic arthritis and found more rapid resolution of fever and pain and a shorter duration of i.v. antibiotics in the dexamethasone group. However, it is unclear if these results apply to S. aureus infections, as 65% of patients had no pathogen isolated from joint fluid, and for the remainder of the patients, the most common pathogen was Kingella kingae. More rapid early recovery with dexamethasone was also recently found in a double-blind, nonrandomized, prospective clinical trial enrolling 60 children in Pakistan 123.
- The role of nasal carriage in Staphylococcus aureus infections. Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, Nouwen JL. Lancet Infect Dis. 2005 Dec; 5(12):751-62. https://www.ncbi.nlm.nih.gov/pubmed/16310147/[↩]
- Staphylococcus aureus in Healthcare Settings. https://www.cdc.gov/HAI/organisms/staph.html[↩]
- Community-associated meticillin-resistant Staphylococcus aureus. DeLeo FR, Otto M, Kreiswirth BN, Chambers HF. Lancet. 2010 May 1; 375(9725):1557-68.[↩]
- Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. David MZ, Daum RS. Clin Microbiol Rev. 2010 Jul; 23(3):616-87.[↩]
- Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. King MD, Humphrey BJ, Wang YF, Kourbatova EV, Ray SM, Blumberg HM. Ann Intern Med. 2006 Mar 7; 144(5):309-17.[↩]
- Methicillin-resistant S. aureus infections among patients in the emergency department. Moran GJ, Krishnadasan A, Gorwitz RJ, Fosheim GE, McDougal LK, Carey RB, Talan DA, EMERGEncy ID Net Study Group.. N Engl J Med. 2006 Aug 17; 355(7):666-74.[↩]
- Molecular epidemiology of community-associated meticillin-resistant Staphylococcus aureus in Europe. Otter JA, French GL. Lancet Infect Dis. 2010 Apr; 10(4):227-39.[↩]
- Methicillin-resistant Staphylococcus aureus in the Australian community: an evolving epidemic. Nimmo GR, Coombs GW, Pearson JC, O’Brien FG, Christiansen KJ, Turnidge JD, Gosbell IB, Collignon P, McLaws ML. Med J Aust. 2006 Apr 17; 184(8):384-8.[↩]
- MRSA epidemic linked to a quickly spreading colonization and virulence determinant. Li M, Du X, Villaruz AE, Diep BA, Wang D, Song Y, Tian Y, Hu J, Yu F, Lu Y, Otto M. Nat Med. 2012 May; 18(5):816-9.[↩]
- Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clinical Microbiology Reviews. 2015;28(3):603-661. doi:10.1128/CMR.00134-14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4451395/[↩]
- Bangert S, Levy M, Hebert AA. 2012. Bacterial resistance and impetigo treatment trends: a review. Pediatr Dermatol 29:243–248. doi:10.1111/j.1525-1470.2011.01700.x.[↩]
- McDonald M, Dougall A, Holt D, Huygens F, Oppedisano F, Giffard PM, Inman-Bamber J, Stephens AJ, Towers R, Carapetis JR, Currie BJ. 2006. Use of a single-nucleotide polymorphism genotyping system to demonstrate the unique epidemiology of methicillin-resistant Staphylococcus aureus in remote aboriginal communities. J Clin Microbiol 44:3720–3727. doi:10.1128/JCM.00836-06.[↩]
- Liu C, Graber CJ, Karr M, Diep BA, Basuino L, Schwartz BS, Enright MC, O’Hanlon SJ, Thomas JC, Perdreau-Remington F, Gordon S, Gunthorpe H, Jacobs R, Jensen P, Leoung G, Rumack JS, Chambers HF. 2008. A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004-2005. Clin Infect Dis 46:1637–1646. doi:10.1086/587893[↩]
- Chambers HF. 2013. Cellulitis, by any other name. Clin Infect Dis 56:1763–1764. doi:10.1093/cid/cit126.[↩]
- Necrotising fasciitis. https://www.dermnetnz.org/topics/necrotising-fasciitis/[↩]
- Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS, Tang AW, Phung TO, Spellberg B. 2005. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med 352:1445–1453. doi:10.1056/NEJMoa042683.[↩]
- Lee YT, Lin JC, Wang NC, Peng MY, Chang FY. 2007. Necrotizing fasciitis in a medical center in northern Taiwan: emergence of methicillin-resistant Staphylococcus aureus in the community. J Microbiol Immunol Infect 40:335–341.[↩]
- Chauhan S, Jain S, Varma S, Chauhan SS. 2004. Tropical pyomyositis (myositis tropicans): current perspective. Postgrad Med J 80:267–270. doi:10.1136/pgmj.2003.009274.[↩]
- Pannaraj PS, Hulten KG, Gonzalez BE, Mason EO Jr, Kaplan SL. 2006. Infective pyomyositis and myositis in children in the era of community-acquired, methicillin-resistant Staphylococcus aureus infection. Clin Infect Dis 43:953–960. doi:10.1086/507637.[↩]
- Al-Tawfiq JA, Sarosi GA, Cushing HE. 2000. Pyomyositis in the acquired immunodeficiency syndrome. South Med J 93:330–334.[↩]
- Lewis SS, Moehring RW, Chen LF, Sexton DJ, Anderson DJ. 2013. Assessing the relative burden of hospital-acquired infections in a network of community hospitals. Infect Control Hosp Epidemiol 34:1229–1230. doi:10.1086/673443.[↩]
- Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, Kallen A, Limbago B, Fridkin S, National Healthcare Safety Network Team, Participating NHSN Facilities . 2013. Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol 34:1–14. doi:10.1086/668770.[↩]
- Wilson SE, O’Riordan W, Hopkins A, Friedland HD, Barriere SL, Kitt MM, ATLAS Investigators. 2009. Telavancin versus vancomycin for the treatment of complicated skin and skin-structure infections associated with surgical procedures. Am J Surg 197:791–796. doi:10.1016/j.amjsurg.2008.05.012.[↩]
- Steingrimsson S, Gottfredsson M, Kristinsson KG, Gudbjartsson T. 2008. Deep sternal wound infections following open heart surgery in Iceland: a population-based study. Scand Cardiovasc J 42:208–213. doi:10.1080/14017430801919557.[↩]
- Fowler VG Jr, Kaye KS, Simel DL, Cabell CH, McClachlan D, Smith PK, Levin S, Sexton DJ, Reller LB, Corey GR, Oddone EZ. 2003. Staphylococcus aureus bacteremia after median sternotomy: clinical utility of blood culture results in the identification of postoperative mediastinitis. Circulation 108:73–78. doi:10.1161/01.CIR.0000079105.65762.DB.[↩]
- Nakamura T, Daimon T, Mouri N, Masuda H, Sawa Y. 2014. Staphylococcus aureus and repeat bacteremia in febrile patients as early signs of sternal wound infection after cardiac surgery. J Cardiothorac Surg 9:80. doi:10.1186/1749-8090-9-80.[↩]
- Population-based survey of invasive bacterial diseases, Greenland, 1995-2004. Meyer A, Ladefoged K, Poulsen P, Koch A. Emerg Infect Dis. 2008 Jan; 14(1):76-9.[↩]
- The changing epidemiology of Staphylococcus aureus bloodstream infection: a multinational population-based surveillance study. Laupland KB, Lyytikäinen O, Søgaard M, Kennedy KJ, Knudsen JD, Ostergaard C, Galbraith JC, Valiquette L, Jacobsson G, Collignon P, Schønheyder HC, International Bacteremia Surveillance Collaborative. Clin Microbiol Infect. 2013 May; 19(5):465-71.[↩]
- Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US military health system, 2005-2010. Landrum ML, Neumann C, Cook C, Chukwuma U, Ellis MW, Hospenthal DR, Murray CK. JAMA. 2012 Jul 4; 308(1):50-9.[↩]
- Secular changes in incidence and mortality associated with Staphylococcus aureus bacteraemia in Quebec, Canada, 1991-2005. Allard C, Carignan A, Bergevin M, Boulais I, Tremblay V, Robichaud P, Duperval R, Pepin J Clin Microbiol Infect. 2008 May; 14(5):421-8.[↩]
- Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE, McDougal LK, Carey RB, Fridkin SK, Active Bacterial Core Surveillance MRSA Investigators . 2007. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763–1771. doi:10.1001/jama.298.15.1763.[↩]
- Tong SY, van Hal SJ, Einsiedel L, Currie BJ, Turnidge JD. 2012. Impact of ethnicity and socio-economic status on Staphylococcus aureus bacteremia incidence and mortality: a heavy burden in indigenous Australians. BMC Infect Dis 12:249. doi:10.1186/1471-2334-12-249.[↩][↩]
- Hill PC, Wong CG, Voss LM, Taylor SL, Pottumarthy S, Drinkovic D, Morris AJ. 2001. Prospective study of 125 cases of Staphylococcus aureus bacteremia in children in New Zealand. Pediatr Infect Dis J 20:868–873. doi:10.1097/00006454-200109000-00009.[↩]
- Larsen MV, Harboe ZB, Ladelund S, Skov R, Gerstoft J, Pedersen C, Larsen CS, Obel N, Kronborg G, Benfield T. 2012. Major but differential decline in the incidence of Staphylococcus aureus bacteraemia in HIV-infected individuals from 1995 to 2007: a nationwide cohort study. HIV Med 13:45–53. doi:10.1111/j.1468-1293.2011.00937.x.[↩][↩][↩][↩]
- Burkey MD, Wilson LE, Moore RD, Lucas GM, Francis J, Gebo KA. 2008. The incidence of and risk factors for MRSA bacteraemia in an HIV-infected cohort in the HAART era. HIV Med 9:858–862. doi:10.1111/j.1468-1293.2008.00629.x.[↩]
- Spijkerman IJ, van Ameijden EJ, Mientjes GH, Coutinho RA, van den Hoek A. 1996. Human immunodeficiency virus infection and other risk factors for skin abscesses and endocarditis among injection drug users. J Clin Epidemiol 49:1149–1154. doi:10.1016/0895-4356(96)00180-1.[↩]
- Tuazon CU, Sheagren JN. 1974. Increased rate of carriage of Staphylococcus aureus among narcotic addicts. J Infect Dis 129:725–727. doi:10.1093/infdis/129.6.725.[↩]
- Palepu A, Tyndall MW, Leon H, Muller J, O’Shaughnessy MV, Schechter MT, Anis AH. 2001. Hospital utilization and costs in a cohort of injection drug users. CMAJ 165:415–420.[↩]
- Craven DE, Rixinger AI, Goularte TA, McCabe WR. 1986. Methicillin-resistant Staphylococcus aureus bacteremia linked to intravenous drug abusers using a “shooting gallery.” Am J Med 80:770–776.[↩]
- Wang IK, Chang YC, Liang CC, Chuang FR, Chang CT, Lin HH, Lin CC, Yen TH, Lin PC, Chou CY, Huang CC, Tsai WC, Chen JH. 2012. Bacteremia in hemodialysis and peritoneal dialysis patients. Intern Med 51:1015–1021. doi:10.2169/internalmedicine.51.7111.[↩]
- Fitzgerald SF, O’Gorman J, Morris-Downes MM, Crowley RK, Donlon S, Bajwa R, Smyth EG, Fitzpatrick F, Conlon PJ, Humphreys H. 2011. A 12-year review of Staphylococcus aureus bloodstream infections in haemodialysis patients: more work to be done. J Hosp Infect 79:218–221. doi:10.1016/j.jhin.2011.06.015.[↩][↩]
- Kallen AJ, Mu Y, Bulens S, Reingold A, Petit S, Gershman K, Ray SM, Harrison LH, Lynfield R, Dumyati G, Townes JM, Schaffner W, Patel PR, Fridkin SK. 2010. Health care-associated invasive MRSA infections, 2005-2008. JAMA 304:641–648. doi:10.1001/jama.2010.1115.[↩]
- Vanholder R, Ringoir S, Dhondt A, Hakim R. 1991. Phagocytosis in uremic and hemodialysis patients: a prospective and cross sectional study. Kidney Int 39:320–327. doi:10.1038/ki.1991.40.[↩]
- Boelaert JR, Daneels RF, Schurgers ML, Matthys EG, Gordts BZ, Van Landuyt HW. 1990. Iron overload in haemodialysis patients increases the risk of bacteraemia: a prospective study. Nephrol Dial Transplant 5:130–134. doi:10.1093/ndt/5.2.130.[↩]
- Zimakoff J, Bangsgaard Pedersen F, Bergen L, Baago-Nielsen J, Daldorph B, Espersen F, Gahrn Hansen B, Hoiby N, Jepsen OB, Joffe P, Kolmos HJ, Klausen M, Kristoffersen K, Ladefoged J, Olesen-Larsen S, Rosdahl VT, Scheibel J, Storm B, Tofte-Jensen P. 1996. Staphylococcus aureus carriage and infections among patients in four haemo- and peritoneal-dialysis centres in Denmark. The Danish Study Group of Peritonitis in Dialysis (DASPID). J Hosp Infect 33:289–300.[↩][↩]
- Jeremiah CJ, Wills C, Bayly A, Perry GJ, Davis JS, Tong SY, Currie BJ. 2014. Vancomycin dosing nomogram for haemodialysis patients. Nephrology 19:513–514. doi:10.1111/nep.12270.[↩]
- Darouiche RO, Hamill RJ, Greenberg SB, Weathers SW, Musher DM. 1992. Bacterial spinal epidural abscess. Review of 43 cases and literature survey. Medicine (Baltimore) 71:369–385.[↩][↩][↩][↩]
- Bryan CS. 2002. Infectious diseases in primary care, p 111–152. WB Saunders, Philadelphia, PA.[↩]
- Reihsaus E, Waldbaur H, Seeling W. 2000. Spinal epidural abscess: a meta-analysis of 915 patients. Neurosurg Rev 23:175–204; discussion 205. doi:10.1007/PL00011954.[↩][↩][↩][↩][↩]
- Chen WC, Wang JL, Wang JT, Chen YC, Chang SC. 2008. Spinal epidural abscess due to Staphylococcus aureus: clinical manifestations and outcomes. J Microbiol Immunol Infect 41:215–221.[↩]
- Feldenzer JA, McKeever PE, Schaberg DR, Campbell JA, Hoff JT. 1988. The pathogenesis of spinal epidural abscess: microangiographic studies in an experimental model. J Neurosurg 69:110–114. doi:10.3171/jns.1988.69.1.0110.[↩]
- Sillevis Smitt P, Tsafka A, van den Bent M, de Bruin H, Hendriks W, Vecht C, Teng-van de Zande F. 1999. Spinal epidural abscess complicating chronic epidural analgesia in 11 cancer patients: clinical findings and magnetic resonance imaging. J Neurol 246:815–820. doi:10.1007/s004150050460.[↩]
- Fowler VG Jr, Olsen MK, Corey GR, Woods CW, Cabell CH, Reller LB, Cheng AC, Dudley T, Oddone EZ. 2003. Clinical identifiers of complicated Staphylococcus aureus bacteremia. Arch Intern Med 163:2066–2072. doi:10.1001/archinte.163.17.2066.[↩][↩]
- Davis DP, Wold RM, Patel RJ, Tran AJ, Tokhi RN, Chan TC, Vilke GM. 2004. The clinical presentation and impact of diagnostic delays on emergency department patients with spinal epidural abscess. J Emerg Med 26:285–291. doi:10.1016/j.jemermed.2003.11.013.[↩]
- Wheeler D, Keiser P, Rigamonti D, Keay S. 1992. Medical management of spinal epidural abscesses: case report and review. Clin Infect Dis 15:22–27. doi:10.1093/clinids/15.1.22.[↩]
- Pizon AF, Bonner MR, Wang HE, Kaplan RM. 2006. Ten years of clinical experience with adult meningitis at an urban academic medical center. J Emerg Med 30:367–370. doi:10.1016/j.jemermed.2005.07.010.[↩]
- Teh BW, Slavin MA. 2012. Staphylococcus aureus meningitis: barriers to treatment. Leuk Lymphoma 53:1443–1444. doi:10.3109/10428194.2012.668685.[↩]
- Aguilar J, Urday-Cornejo V, Donabedian S, Perri M, Tibbetts R, Zervos M. 2010. Staphylococcus aureus meningitis: case series and literature review. Medicine (Baltimore) 89:117–125. doi:10.1097/MD.0b013e3181d5453d.[↩][↩][↩][↩][↩]
- Pintado V, Meseguer MA, Fortun J, Cobo J, Navas E, Quereda C, Corral I, Moreno S. 2002. Clinical study of 44 cases of Staphylococcus aureus meningitis. Eur J Clin Microbiol Infect Dis 21:864–868. doi:10.1007/s10096-002-0814-1.[↩][↩][↩]
- Lerche A, Rasmussen N, Wandall JH, Bohr VA. 1995. Staphylococcus aureus meningitis: a review of 28 consecutive community-acquired cases. Scand J Infect Dis 27:569–573. doi:10.3109/00365549509047069.[↩]
- Lu CH, Chang WN. 2000. Adults with meningitis caused by oxacillin-resistant Staphylococcus aureus. Clin Infect Dis 31:723–727. doi:10.1086/314034.[↩]
- Pintado V, Pazos R, Jimenez-Mejias ME, Rodriguez-Guardado A, Gil A, Garcia-Lechuz JM, Cabellos C, Chaves F, Domingo P, Ramos A, Perez-Cecilia E, Domingo D. 2012. Methicillin-resistant Staphylococcus aureus meningitis in adults: a multicenter study of 86 cases. Medicine (Baltimore) 91:10–17. doi:10.1097/MD.0b013e318243442b.[↩][↩][↩]
- Huang WC, Lee CH, Liu JW. 2010. Clinical characteristics and risk factors for mortality in patients with meningitis caused by Staphylococcus aureus and vancomycin minimal inhibitory concentrations against these isolates. J Microbiol Immunol Infect 43:470–477. doi:10.1016/S1684-1182(10)60073-4.[↩][↩][↩]
- Givner LB, Kaplan SL. 1993. Meningitis due to Staphylococcus aureus in children. Clin Infect Dis 16:766–771. doi:10.1093/clind/16.6.766.[↩]
- Pedersen M, Benfield TL, Skinhoej P, Jensen AG. 2006. Haematogenous Staphylococcus aureus meningitis. A 10-year nationwide study of 96 consecutive cases. BMC Infect Dis 6:49. doi:10.1186/1471-2334-6-49.[↩]
- Jensen AG, Espersen F, Skinhoj P, Rosdahl VT, Frimodt-Moller N. 1993. Staphylococcus aureus meningitis. A review of 104 nationwide, consecutive cases. Arch Intern Med 153:1902–1908.[↩]
- Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM, Whitley RJ. 2004. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 39:1267–1284. doi:10.1086/425368.[↩]
- Goto K, Ohi T, Namba A, Uemura N, Kitaguchi H. 2011. Successful treatment of methicillin-resistant Staphylococcus aureus meningitis by intrathecal injection of vancomycin. Brain Nerve 63:417–421.[↩]
- Todd J, Fishaut M, Kapral F, Welch T. 1978. Toxic-shock syndrome associated with phage-group-I staphylococci. Lancet ii:1116–1118.[↩]
- Herzer CM. 2001. Toxic shock syndrome: broadening the differential diagnosis. J Am Board Fam Pract 14:131–136.[↩]
- Osterholm MT, Forfang JC. 1982. Toxic-shock syndrome in Minnesota: results of an active-passive surveillance system. J Infect Dis 145:458–464. doi:10.1093/infdis/145.4.458.[↩]
- DeVries AS, Lesher L, Schlievert PM, Rogers T, Villaume LG, Danila R, Lynfield R. 2011. Staphylococcal toxic shock syndrome 2000-2006: epidemiology, clinical features, and molecular characteristics. PLoS One 6:e22997. doi:10.1371/journal.pone.0022997.[↩]
- toxic shock syndrome[↩][↩]
- Descloux E, Perpoint T, Ferry T, Lina G, Bes M, Vandenesch F, Mohammedi I, Etienne J. 2008. One in five mortality in non-menstrual toxic shock syndrome versus no mortality in menstrual cases in a balanced French series of 55 cases. Eur J Clin Microbiol Infect Dis 27:37–43. doi:10.1007/s10096-007-0405-2.[↩][↩]
- Musser JM, Schlievert PM, Chow AW, Ewan P, Kreiswirth BN, Rosdahl VT, Naidu AS, Witte W, Selander RK. 1990. A single clone of Staphylococcus aureus causes the majority of cases of toxic shock syndrome. Proc Natl Acad Sci U S A 87:225–229. doi:10.1073/pnas.87.1.225.[↩]
- Fraser J, Arcus V, Kong P, Baker E, Proft T. 2000. Superantigens—powerful modifiers of the immune system. Mol Med Today 6:125–132. doi:10.1016/S1357-4310(99)01657-3.[↩]
- Centers for Disease Control and Prevention. 1997. Case definitions for infectious conditions under public health surveillance. MMWR Recommend Rep 46(RR-10):1–55[↩]
- Low DE. 2013. Toxic shock syndrome: major advances in pathogenesis, but not treatment. Crit Care Clin 29:651–675. doi:10.1016/j.ccc.2013.03.012.[↩]
- Successful treatment of staphylococcal toxic shock syndrome with linezolid: a case report and in vitro evaluation of the production of toxic shock syndrome toxin type 1 in the presence of antibiotics. Stevens DL, Wallace RJ, Hamilton SM, Bryant AE. Clin Infect Dis. 2006 Mar 1; 42(5):729-30.[↩]
- Lappin E, Ferguson AJ. 2009. Gram-positive toxic shock syndromes. Lancet Infect Dis 9:281–290. doi:10.1016/S1473-3099(09)70066-0.[↩]
- The microbiology of chronic osteomyelitis: prevalence of resistance to common empirical anti-microbial regimens. Sheehy SH, Atkins BA, Bejon P, Byren I, Wyllie D, Athanasou NA, Berendt AR, McNally MA. J Infect. 2010 May; 60(5):338-43.[↩]
- Adult native septic arthritis: a review of 10 years of experience and lessons for empirical antibiotic therapy. Clerc O, Prod’hom G, Greub G, Zanetti G, Senn L. J Antimicrob Chemother. 2011 May; 66(5):1168-73.[↩]
- Early onset prosthetic hip and knee joint infection: treatment and outcomes in Victoria, Australia. Peel TN, Cheng AC, Choong PF, Buising KL. J Hosp Infect. 2012 Dec; 82(4):248-53.[↩]
- Osteomyelitis: a review of clinical features, therapeutic considerations and unusual aspects. Waldvogel FA, Medoff G, Swartz MN. N Engl J Med. 1970 Jan 22; 282(4):198-206.[↩]
- Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. McHenry MC, Easley KA, Locker GA. Clin Infect Dis. 2002 May 15; 34(10):1342-50.[↩][↩][↩][↩][↩]
- Bacteremic Staphylococcus aureus spondylitis. Jensen AG, Espersen F, Skinhøj P, Frimodt-Møller N. Arch Intern Med. 1998 Mar 9; 158(5):509-17.[↩][↩]
- Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A. Semin Arthritis Rheum. 2009 Aug; 39(1):10-7.[↩][↩]
- Therapeutic impact of percutaneous spinal biopsy in spinal infection. Rankine JJ, Barron DA, Robinson P, Millner PA, Dickson RA. Postgrad Med J. 2004 Oct; 80(948):607-9.[↩]
- Microbiological diagnosis of vertebral osteomyelitis: relevance of second percutaneous biopsy following initial negative biopsy and limited yield of post-biopsy blood cultures. Gras G, Buzele R, Parienti JJ, Debiais F, Dinh A, Dupon M, Roblot F, Mulleman D, Marcelli C, Michon J, Bernard L. Eur J Clin Microbiol Infect Dis. 2014 Mar; 33(3):371-5.[↩]
- The epidemiology of hematogenous vertebral osteomyelitis: a cohort study in a tertiary care hospital. Bhavan KP, Marschall J, Olsen MA, Fraser VJ, Wright NM, Warren DK. BMC Infect Dis. 2010 Jun 7; 10():158.[↩]
- Suggestions for managing pyogenic (non-tuberculous) discitis in adults. Grados F, Lescure FX, Senneville E, Flipo RM, Schmit JL, Fardellone P. Joint Bone Spine. 2007 Mar; 74(2):133-9.[↩][↩]
- Outcomes of osteomyelitis among patients treated with outpatient parenteral antimicrobial therapy. Tice AD, Hoaglund PA, Shoultz DA. Am J Med. 2003 Jun 15; 114(9):723-8.[↩]
- Cost analysis of debridement and retention for management of prosthetic joint infection. Peel TN, Dowsey MM, Buising KL, Liew D, Choong PF. Clin Microbiol Infect. 2013 Feb; 19(2):181-6.[↩]
- Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the Japanese diagnosis procedure combination database. Akiyama T, Chikuda H, Yasunaga H, Horiguchi H, Fushimi K, Saita K. BMJ Open. 2013 Mar 25; 3(3).[↩]
- Clinical characteristics and therapeutic outcomes of hematogenous vertebral osteomyelitis caused by methicillin-resistant Staphylococcus aureus. Park KH, Chong YP, Kim SH, Lee SO, Choi SH, Lee MS, Jeong JY, Woo JH, Kim YS. J Infect. 2013 Dec; 67(6):556-64.[↩][↩]
- Optimal duration of antibiotic therapy in vertebral osteomyelitis. Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, Bastides F, Le Moal G, Godet C, Mulleman D, Azaïs I, Becq-Giraudon B, Choutet P. Semin Arthritis Rheum. 2007 Apr; 36(5):269-77.[↩][↩]
- Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Dénes E, Debard A, Chirouze C, Fèvre K, Dupon M, Aegerter P, Mulleman D, Duration of Treatment for Spondylodiscitis (DTS) study group. Lancet. 2015 Mar 7; 385(9971):875-82.[↩][↩][↩]
- Mitha A, Boutry N, Nectoux E, Petyt C, Lagree M, Happiette L, Martinot A., Hospital Network for Evaluating the Management of Infectious Diseases in Children, Dubos F, editor. 2015. Community-acquired bone and joint infections in children: a 1-year prospective epidemiological study. Arch Dis Child 100:126–129. doi:10.1136/archdischild-2013-305860.[↩]
- Paediatric bone and joint infections are more common in boys and toddlers: a national epidemiology study. Grammatico-Guillon L, Maakaroun Vermesse Z, Baron S, Gettner S, Rusch E, Bernard L. Acta Paediatr. 2013 Mar; 102(3):e120-5.[↩][↩][↩]
- Pediatric Acute Hematogenous Osteomyelitis. Street M, Puna R, Huang M, Crawford H. J Pediatr Orthop. 2015 Sep; 35(6):634-9.[↩]
- Changing patterns of acute hematogenous osteomyelitis and septic arthritis: emergence of community-associated methicillin-resistant Staphylococcus aureus. Arnold SR, Elias D, Buckingham SC, Thomas ED, Novais E, Arkader A, Howard C. J Pediatr Orthop. 2006 Nov-Dec; 26(6):703-8.[↩]
- Changing trends in acute osteomyelitis in children: impact of methicillin-resistant Staphylococcus aureus infections. Saavedra-Lozano J, Mejías A, Ahmad N, Peromingo E, Ardura MI, Guillen S, Syed A, Cavuoti D, Ramilo O. J Pediatr Orthop. 2008 Jul-Aug; 28(5):569-75.[↩]
- Recent lessons for the management of bone and joint infections. Kaplan SL. J Infect. 2014 Jan; 68 Suppl 1():S51-6.[↩][↩]
- Acute osteomyelitis in children. Peltola H, Pääkkönen M. N Engl J Med. 2014 Jan 23; 370(4):352-60.[↩][↩][↩][↩]
- Sensitivity of erythrocyte sedimentation rate and C-reactive protein in childhood bone and joint infections. Pääkkönen M, Kallio MJ, Kallio PE, Peltola H. Clin Orthop Relat Res. 2010 Mar; 468(3):861-6.[↩][↩]
- Differentiating between methicillin-resistant and methicillin-sensitive Staphylococcus aureus osteomyelitis in children: an evidence-based clinical prediction algorithm. Ju KL, Zurakowski D, Kocher MS. J Bone Joint Surg Am. 2011 Sep 21; 93(18):1693-701.[↩][↩]
- Independent analysis of a clinical predictive algorithm to identify methicillin-resistant Staphylococcus aureus osteomyelitis in children. Wade Shrader M, Nowlin M, Segal LS. J Pediatr Orthop. 2013 Oct-Nov; 33(7):759-62.[↩]
- Deep venous thrombosis associated with osteomyelitis in children. Hollmig ST, Copley LA, Browne RH, Grande LM, Wilson PL. J Bone Joint Surg Am. 2007 Jul; 89(7):1517-23.[↩]
- Venous thrombosis associated with staphylococcal osteomyelitis in children. Gonzalez BE, Teruya J, Mahoney DH Jr, Hulten KG, Edwards R, Lamberth LB, Hammerman WA, Mason EO Jr, Kaplan SL. Pediatrics. 2006 May; 117(5):1673-9.[↩]
- When should DVT be suspected in children with osteomyelitis? Altobelli MG, Quinonez RA. Hosp Pediatr. 2012 Jul; 2(3):167-72.[↩]
- Short- versus long-term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture-positive cases. Peltola H, Pääkkönen M, Kallio P, Kallio MJ, Osteomyelitis-Septic Arthritis Study Group. Pediatr Infect Dis J. 2010 Dec; 29(12):1123-8.[↩][↩][↩]
- Prospective evaluation of a shortened regimen of treatment for acute osteomyelitis and septic arthritis in children. Jagodzinski NA, Kanwar R, Graham K, Bache CE. J Pediatr Orthop. 2009 Jul-Aug; 29(5):518-25.[↩]
- Short- versus long-term antimicrobial treatment for acute hematogenous osteomyelitis of childhood: prospective, randomized trial on 131 culture-positive cases. Peltola H, Pääkkönen M, Kallio P, Kallio MJ, Osteomyelitis-Septic Arthritis Study Group.. Pediatr Infect Dis J. 2010 Dec; 29(12):1123-8.[↩]
- Complications of central venous catheters used for the treatment of acute hematogenous osteomyelitis. Ruebner R, Keren R, Coffin S, Chu J, Horn D, Zaoutis TE. Pediatrics. 2006 Apr; 117(4):1210-5.[↩]
- Clindamycin vs. first-generation cephalosporins for acute osteoarticular infections of childhood–a prospective quasi-randomized controlled trial. Peltola H, Pääkkönen M, Kallio P, Kallio MJ, OM-SA Study Group. Clin Microbiol Infect. 2012 Jun; 18(6):582-9.[↩]
- Systematic review of duration and choice of systemic antibiotic therapy for acute haematogenous bacterial osteomyelitis in children. Howard-Jones AR, Isaacs D. J Paediatr Child Health. 2013 Sep; 49(9):760-8.[↩][↩]
- Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, J Rybak M, Talan DA, Chambers HF, Infectious Diseases Society of America. Clin Infect Dis. 2011 Feb 1; 52(3):e18-55.[↩]
- Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Peltola H, Pääkkönen M, Kallio P, Kallio MJ, Osteomyelitis-Septic Arthritis (OM-SA) Study Group. Clin Infect Dis. 2009 May 1; 48(9):1201-10.[↩]
- Clinical and laboratory parameters associated with multiple surgeries in children with acute hematogenous osteomyelitis. Tuason DA, Gheen T, Sun D, Huang R, Copley L. J Pediatr Orthop. 2014 Jul-Aug; 34(5):565-70.[↩]
- Twelve-month outcome following septic arthritis in children. Howard-Jones AR, Isaacs D, Gibbons PJ. J Pediatr Orthop B. 2013 Sep; 22(5):486-90.[↩]
- Double blind, randomized, placebo-controlled study of dexamethasone therapy for hematogenous septic arthritis in children. Odio CM, Ramirez T, Arias G, Abdelnour A, Hidalgo I, Herrera ML, Bolaños W, Alpízar J, Alvarez P. Pediatr Infect Dis J. 2003 Oct; 22(10):883-8.[↩]
- Dexamethasone therapy for septic arthritis in children: results of a randomized double-blind placebo-controlled study. Harel L, Prais D, Bar-On E, Livni G, Hoffer V, Uziel Y, Amir J. J Pediatr Orthop. 2011 Mar; 31(2):211-5.[↩]
- The effect of intravenous dexamethasone in the treatment of septic arthritis. Arti H, Mousapour A, Alavi SM. Pak J Med Sci. 2014 Sep; 30(5):955-7.[↩]