Why is my stomach growling
Stomach rumbling, stomach growling or gurgling noise is made by the movement of fluid and gas in the stomach and intestines. Bowel sounds show wide variations from person to person and even from the same person at different times 1. The interpretation of a person’s bowel sounds by different clinicians may also vary 2. In a study 3 on bowel sounds involving clinicians and 211 subjects (normal volunteers = 177, mechanical small bowel obstruction = 19, postoperative paralytic ileus= 15), found listening to bowel sounds with a stethoscope (auscultation) is not a useful in clinical practice when differentiating patients with normal versus pathologic bowel sounds. The researchers found the listener frequently arrives at an incorrect diagnosis 3. Another smaller study 4 on bowel sounds in the diagnosis of paralytic ileus (paralytic ileus is paralysis or the inability of the bowel to pass stool due to impaired peristalsis) and bowel obstruction (healthy volunteers = 10 and patients with radiologically or laparotomy confirmed small bowel obstruction = 9 and ileus = 7). Paralytic ileus is inevitable after abdominal surgery and lasts usually 3 to 5 days 5. In addition to surgery, other factors such as mechanical ventilation, increased intracranial or intra-abdominal pressure, sedation or sepsis may contribute to development of paralytic ileus 5. 20 physicians were then presented with 43 recordings in blinded fashion and were asked whether each was from a normal subject or from a subject with bowel obstruction or ileus. The results were the physicians only arrived at the correct diagnosis a median of 30 times out of 43 (69.8%). In other words bowel sounds is non-specific for diagnosing bowel obstruction and the clinical significance of abdominal bowel sounds is limited.
The intrinsic difficulty with the study of bowel sounds is that it is never possible to hear or record exactly the same pattern of bowel sounds with exactly same amplitude, frequency, duration and interval repeatedly and consistently as compared to the consistent sounds produced from the heart, which has a set rhythm and sound characteristics over time 1. The bowel sounds heard from the same patient will also differ at different times when the patient is re-examined. The wide range of physiological variations means that the clinical significance of bowel sounds is limited. There is no clear evidence that high-pitched bowel sounds have clinical significance or specificity 6. The recording of bowel sound yields only the sum of the motility of all areas of the alimentary track, so no statements are possible about the activity of any particular segment by comparison of sounds at different recording sites 7.
What is the stomach
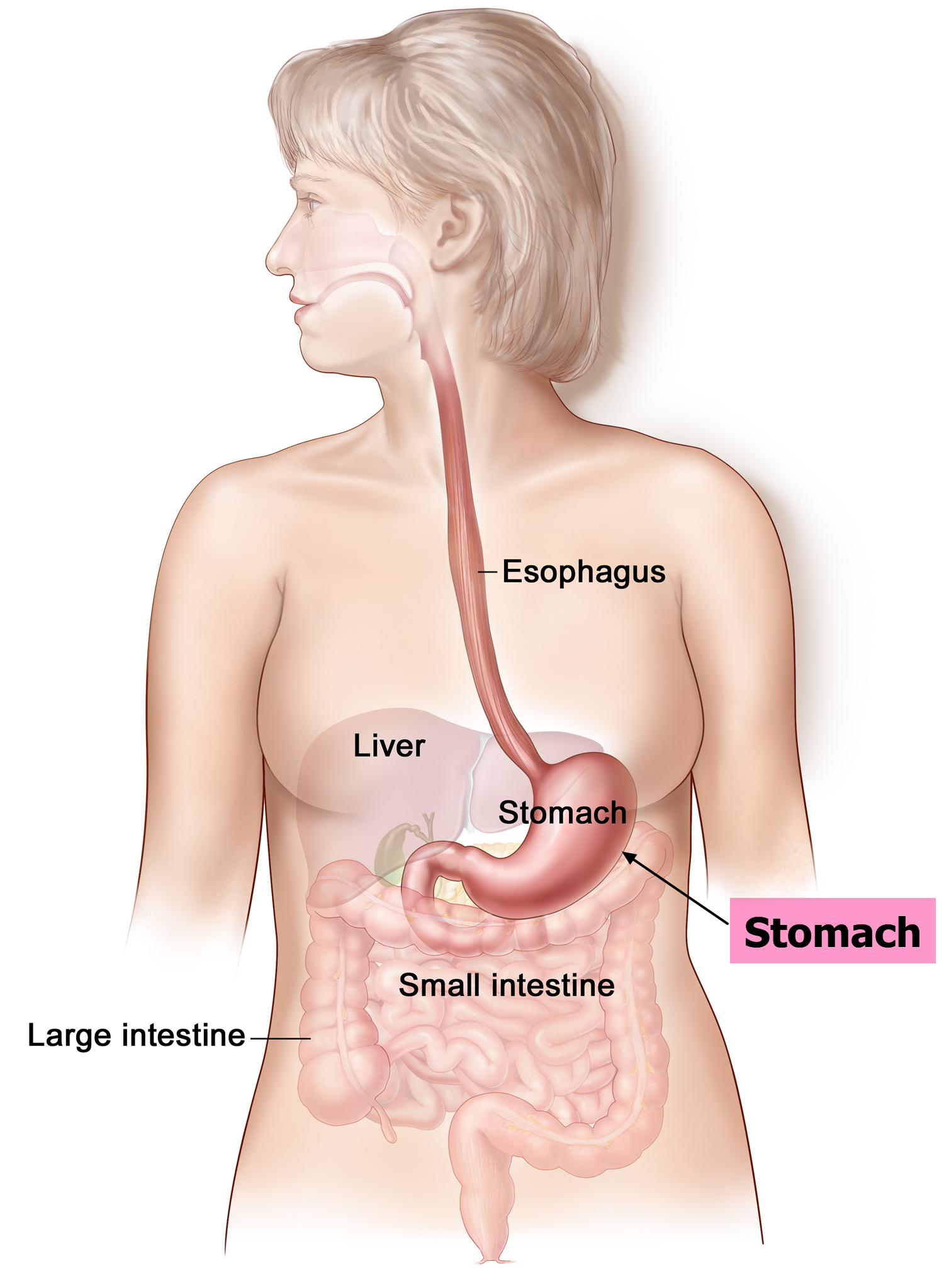
The stomach is a muscular J-shaped pouchlike hollow organ that hangs inferior to the diaphragm in the upper left portion of the abdominal cavity and has a capacity of about 1 liter or more (Figure 1) 8. The stomach’s shape and size vary from person to person, depending on things like people’s sex and build, but also on how much they eat.
At the point where the esophagus leads into the stomach, the digestive tube is usually kept shut by muscles of the esophagus and diaphragm. When you swallow, these muscles relax and the lower end of the esophagus opens, allowing food to enter the stomach. If this mechanism does not work properly, acidic gastric juice might get into the esophagus, leading to heartburn or an inflammation (see Figure 2).
Thick folds (rugae) of mucosal and submucosal layers mark the stomach’s inner lining and disappear when the stomach wall is distended. The stomach receives food from the esophagus, mixes the food with gastric juice, initiates protein digestion, carries on limited absorption, and moves food into the small intestine.
Figure 1. Stomach
Small intestine
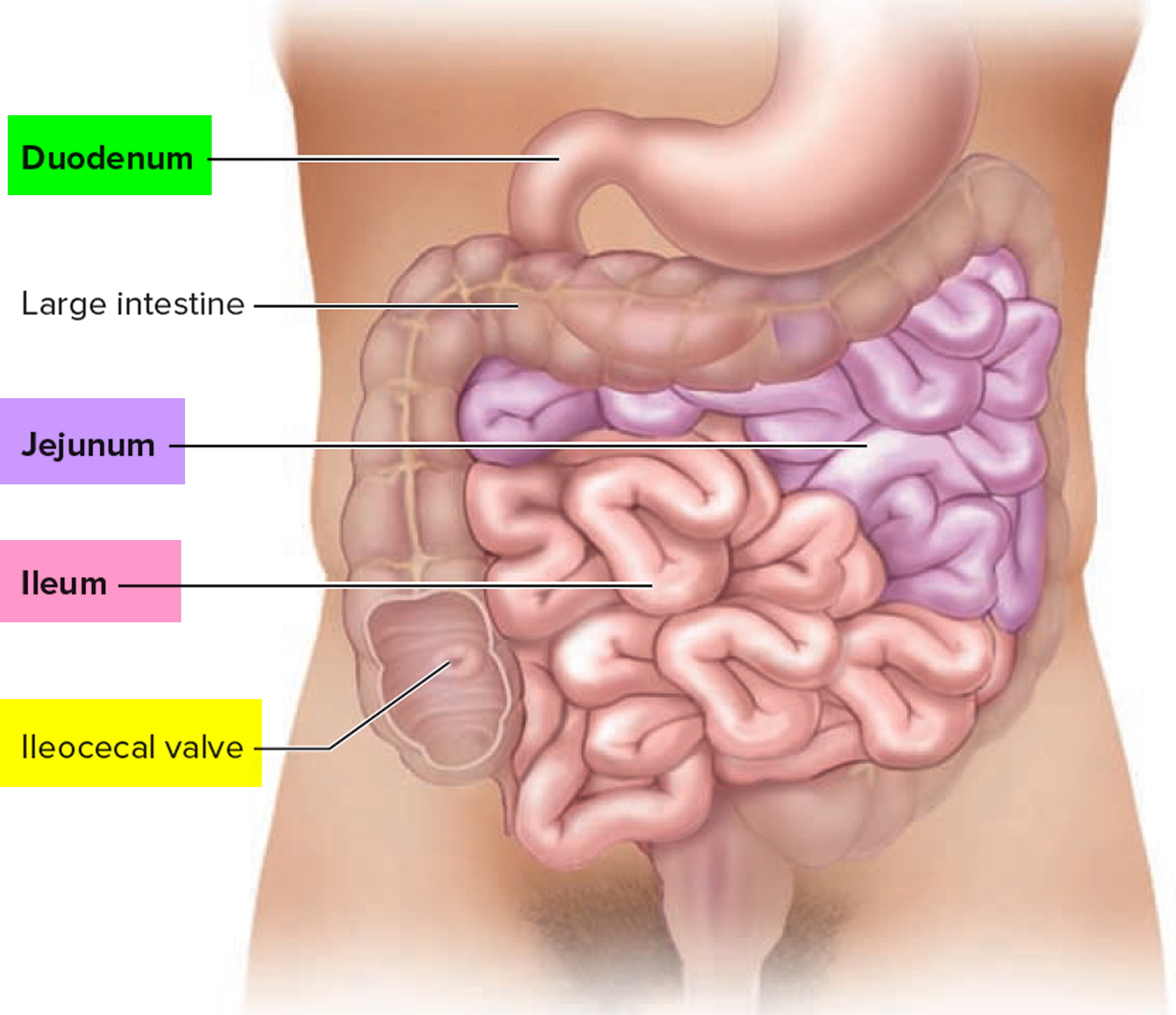
The small intestine is the longest part of the alimentary canal and it begins at the pyloric sphincter of the stomach, coils through the central and inferior part of the abdominal cavity, and eventually opens into the large intestine.
The term small intestine refers not to its length but to its diameter—about 2.5 cm (1 in.).
The small intestine is approximately 6 to 7 m long (range 3–7 m) with a narrowing diameter from beginning to end.
The small intestine consists of the duodenum, the jejunum, and the ileum.
The small intestine receives chyme from the stomach and secretions from the pancreas, liver, and gallbladder. It completes digestion of the nutrients in chyme, absorbs the products of digestion, and transports the residue to the large intestine.
The small intestine the site of most enzymatic digestion and about 90 percent of all nutrients absorption and most of the rest occurs in the proximal portion of the large intestine. Its length alone provides a large surface area for digestion and absorption, and that area is further increased by circular folds, villi, and microvilli. Most digestive enzymes that operate within the small intestine are secreted not by the intestine, but by the pancreas. During digestion, the small intestine undergoes active segmentation movements, shuffling the chyme back and forth and thereby maximizing its contact with the nutrient-absorbing mucosa.
Peristalsis propels chyme through the small intestine in about 3–6 hours.
Figure 2. Small intestine
Large intestine
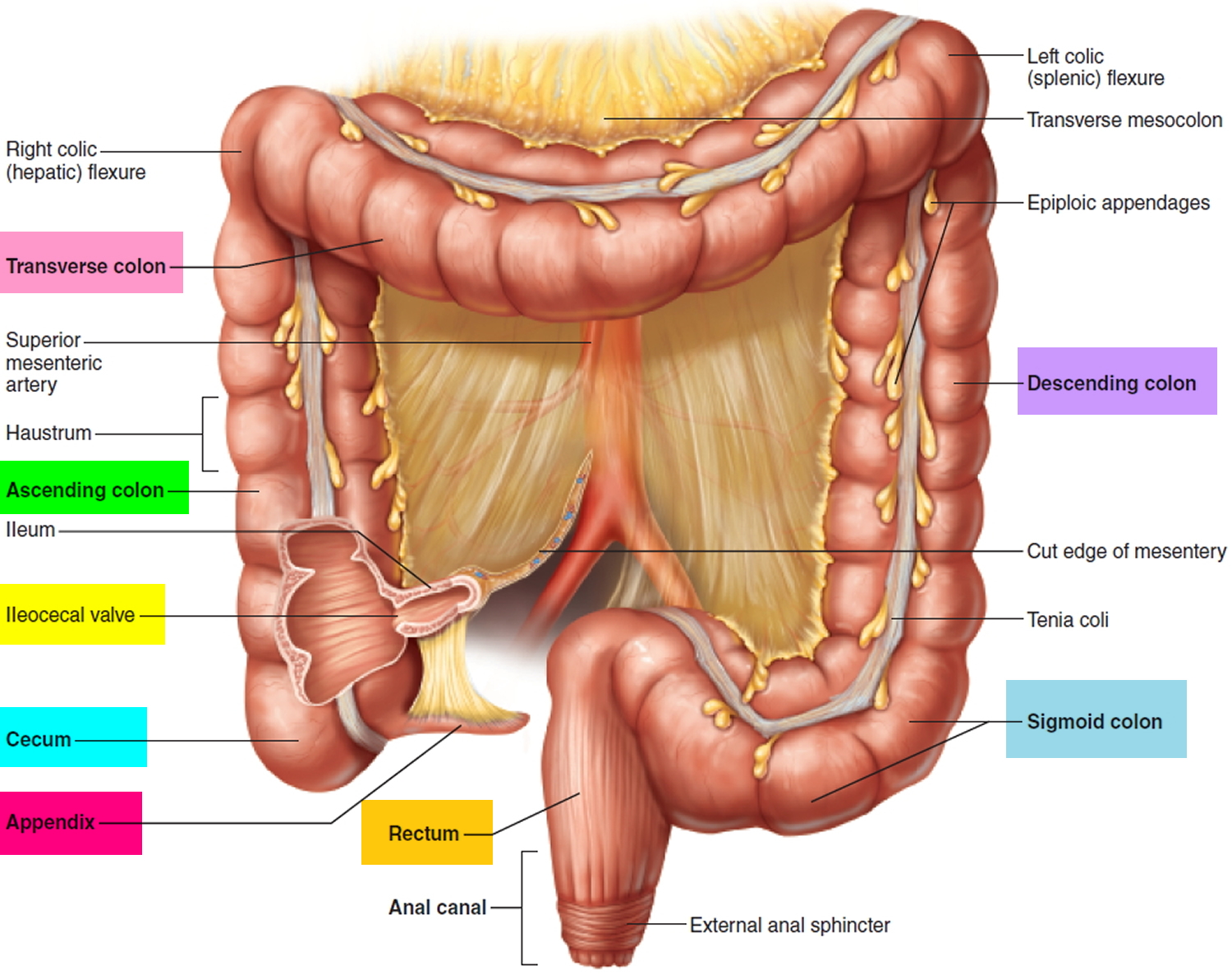
The large intestine extends from the distal end of the ileum to the anus, a distance of approximately 1.5 m in adults (5 ft) long and 6.5 cm (2.5 in.) in diameter. The large intestine is named for its relatively large diameter, not its length. The large intestine absorbs fluids and salts from the gut contents, thus forming feces. The large intestine consists of the cecum, appendix, colon, rectum, and anal canal.
Beginning in the right groin as the cecum, with its associated appendix, the large intestine continues upward as the ascending colon through the right flank and into the right hypochondrium. The ascending colon begins at the ileocecal valve and passes up the right side of the abdominal cavity. It makes a 90° turn at the right colic (hepatic) flexure, near the right lobe of the liver, and crosses the abdomen as the transverse colon to the left hypochondrium. At this position, just below the spleen, the large intestine bends downward, forming the left colic flexure (splenic flexure) and continues as the descending colon through the left flank and into the left groin. Ascending, transverse, and descending colons thus form a squarish, three-sided frame around the small intestine.
The cecum is a blind pouch in the lower right abdominal quadrant inferior to the ileocecal valve. Attached to its lower end is the appendix, a blind tube 2 to 7 cm long. The appendix is densely populated with lymphocytes and is a significant source of immune cells.
Figure 3. Large intestine
What causes stomach growling
Bowel sounds are generated by contractions of the alimentary tract, and mixing of gaseous, liquid and semisolid materials in the bowel lumen, with gas as the major component 9. The quality of bowel sounds varies according to the state of bowel activity 10. Bowel sounds are complex, and each sound comprises a mixture of tones and is often a sequence of closely connected sounds. Common descriptions of bowel sounds include gurgling or rattling or rustling noise heard in a normal person, rumbling explosions heard with gastroenteritis, succussion splash heard in gastric outlet obstruction, diminished, i.e., infrequent, and soft sounds, and prolonged tinkling or high-pitched metallic sounds that may be heard in bowel obstruction. Very diminished or absent bowel sounds may be caused by bowel obstruction, intestinal ischemia, paralytic ileus, and peritonitis.
Factors governing the quality of bowel sounds have been speculated to include dimensions of bowel segments, contents of the lumen and thickness of the intestinal wall 11. Nevertheless, because of the lack of knowledge on how they work or interact, these speculations have not been validated 12. The adult intestinal tract contains 100-200 ml of gas 13. The intraluminal gas, in the form of bubbles or bubble clusters, is a frequent finding in daily practice on ultrasonography (US), described as the ring-down artifact or the dirty shadowing 14. Gas bubbles responsible for these findings were found to be 1-7 mm in diameter 14. Moreover, intraluminal bubbles throughout the small bowel have been considered the major obstacle for clear visualization during capsule endoscopic examinations 15. A recent article confirmed the presence of vertically rising bubbles in human gastrointestinal tract on multidetector computed tomography scan 16. The accumulated evidence suggests that bubbles are constantly and actively present in the human gastrointestinal tract. The study by Sugrue et al 17 in 1994 compared characteristics of bowel sounds in controls (n = 63) and patients with acute appendicitis (n = 25), acute cholecystitis (n = 15), and bowel obstruction (n = 21). This study compared sound number, duration, interval, and amplitude but not frequency of bowel sounds. It was found that in bowel obstruction, the sound duration, interval, and amplitude all significantly increased when compared to control subjects.
However, in a more recent 2012 study 1 involving seventy-one patients, found no significant difference among the groups of patients with acute bowel obstruction, subacute bowel obstruction, and no bowel obstruction in the sound characteristics in terms of sound duration, sound-to-sound interval, dominant frequency and peak frequency when comparisons were made The results are summarized in Table 1. This study has shown objectively that bowel sound characteristics, in general, are not significantly different between patients with acute, subacute, or no intestinal obstruction using the commonly compared parameters, including sound duration, sound-to-sound interval, and dominant and peak frequencies 1. However, the obstructed large bowel has significantly longer sound duration (median 0.87 second vs 0.56 second) and higher dominant frequency (median 440 Hz vs 288 Hz) when compared to obstructed small bowel. The possible explanations for these differences are that movements within the colon usually involve less frequent peristalsis but larger volume shift with each peristalsis and, therefore, in the presence of an obstruction, a longer time elapses when fluid and gas are forced to pass through a tight stenosis. The higher sound frequency in large bowel obstruction can be explained by the fact that the majority of ileocecal valves are competent 18. In the event of large bowel obstruction, the pressure rises within the “closed loop” segment of the colon proximal to the point of obstruction. Progressive distension of the colon increases the tension on the colonic wall, as well as thinning of the wall; hence, vibration is produced at a higher frequency. In small bowel obstruction, the pressure within the obstructed segment of bowel is usually limited by reflux of the small bowel contents back into the stomach (except in the presence of certain uncommon situations causing a closed loop obstruction), hence the common presentation of vomiting in small bowel obstruction.
The point of “obstruction” in patients with pseudo-obstruction is often caused by a high resting anal sphincter tone, which impedes the evacuation of flatus and feces. This can be identified by digital rectal examination and the findings of a tight anus, which precludes easy entry of the examining finger. Upon entry of the finger, the rectum can be felt to be capacious and mainly gas and fluid filled.
Table 1. Sound characteristics of acute bowel obstruction vs subacute bowel obstruction vs no obstruction
| No obstruction (n = 20) | Subacute obstruction (n = 11) | Acute obstruction (n = 40) | |
| Sound duration (s) | 0.64 (0.20-1.57) | 0.63 (0.23-1.67) | 0.69 (0.19-2.10) |
| Sound-to-sound interval (s) | 0.72 (0.46-1.27) | 0.70 (0.47-1.67) | 0.75 (0.41-1.41) |
| Dominant frequency (Hz) | 325 (225-530) | 405 (218-565) | 315 (225-545) |
| Peak frequency (Hz) | 595 (378-713) | 655 (465-735) | 585 (530-706) |
Note: Data are presented as the median (inter-quartile range).
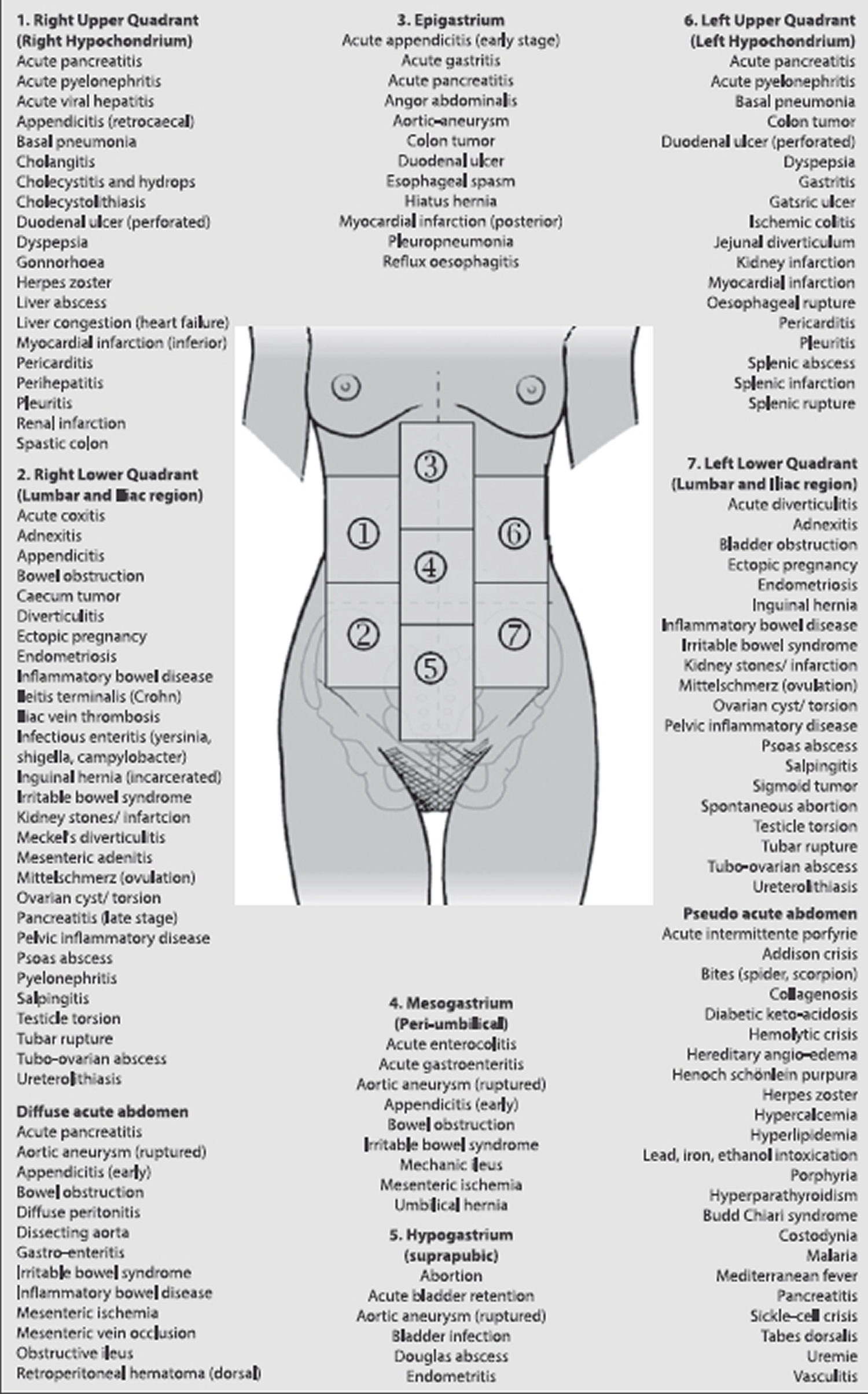
[Source 1]Figure 4. Differential diagnosis acute abdominal pain
[Source 19]The following definitions were used to compare bowel sounds between patients with acute bowel obstruction vs subacute obstruction vs no obstruction 20]
Acute bowel obstruction
Dilated bowel caliber (> 3 cm for small bowel, > 6 cm for large bowel) with symptoms of vomiting (for small bowel pathology) or no flatus/bowel motion for > 24 h (for large bowel pathology) and with CT/operative evidence of complete or high grade mechanical obstruction with a discrete transition point, collapsed distal segment, and little or no colonic gas present distal to the obstruction.
Although bowel dilatation is a common sign of obstruction at any level of the gastrointestinal tract, it may also appear without an obstruction (as in toxic megacolon or acute colonic pseudo-obstruction = Ogilvie’s syndrome). The most common predisposing conditions for Ogilvie’s syndrome are non-operative abdominal trauma, infections and cardiac diseases 21.
Subacute obstruction
Dilated bowel caliber (> 3 cm for small intestine, > 6 cm for large intestine), with or without symptoms as per acute obstruction, but no CT/operative evidence of complete or high-grade mechanical obstruction (a poorly defined transition zone, incomplete collapse of distal bowel segment, and moderate colonic gas distal to the obstruction).
Acute (complete) or subacute (partial) mechanical obstruction of the bowel may be caused by herniation, adhesions, volvulus, intussusception, foreign body, phytobezoar, strictures, cancer, or wall swelling (edema) due to inflammatory conditions. Partial obstruction allows some liquid contents and gas to pass through the point of obstruction, whereas complete obstruction impedes passage of all bowel contents.
No obstruction
No clinical/CT/operative/endoscopic evidence of mechanical obstruction and other diagnosis was observed during the clinical course of the patient. Diagnoses such as constipation colic, fecal impaction, paralytic ileus, chronic megacolon, and pseudo-obstruction will be classified under this category.
Lactose intolerance
If you have lactose intolerance, you have trouble digesting milk, cheese, and other dairy products. This condition is most common in people of Asian, American Indian, Hispanic, South American, or black heritage. Lactose intolerance is a condition in which you have digestive symptoms—such as bloating, diarrhea, and gas—after you consume foods or drinks that contain lactose. Lactose is a sugar that is naturally found in milk and milk products, like cheese or ice cream.
In people with lactose intolerance, they have trouble digesting milk because their body does not make enough lactase. Lactase is an enzyme that breaks down the natural sugar in milk. This sugar is called lactose.
In lactose intolerance, digestive symptoms are caused by lactose malabsorption. Lactose malabsorption is a condition in which your small intestine cannot digest, or break down, all the lactose you eat or drink. Experts estimate that about 68 percent of the world’s population has lactose malabsorption 22. Lactose malabsorption is more common in some parts of the world than in others. In Africa and Asia, most people have lactose malabsorption. In some regions, such as northern Europe, many people carry a gene that allows them to digest lactose after infancy, and lactose malabsorption is less common 23. In the United States, about 36 percent of people have lactose malabsorption 22.
Not everyone with lactose malabsorption has digestive symptoms after they consume lactose. Only people who have symptoms are lactose intolerant.
Most people with lactose intolerance can consume some amount of lactose without having symptoms. Different people can tolerate different amounts of lactose before having symptoms.
Lactose intolerance is different from a milk allergy. A milk allergy is an immune system disorder.
What is the difference between lactose intolerance and milk allergies?
Lactose intolerance and milk allergies are different conditions with different causes. Lactose intolerance is caused by problems digesting lactose, the natural sugar in milk. In contrast, milk allergies are caused by your immune system’s response to one or more proteins in milk and milk products.
A milk allergy most often appears in the first year of life, while lactose intolerance typically appears later 24. Lactose intolerance can cause uncomfortable symptoms, while a serious allergic reaction to milk can be life threatening.
What are the symptoms of lactose intolerance?
If you have lactose intolerance, you may have symptoms within a few hours after you have milk or milk products, or other foods that contain lactose.
Your symptoms may be mild or severe, depending on how much lactose you have.
The main problems caused by lactose intolerance in adults are:
- Stomach “growling” or rumbling sounds
- Gas
- Stomach cramps
- Pain in your abdomen
- Stomach bloating
- Diarrhea
- Nausea
- Vomiting
The condition is different in each person. Some people with this problem can safely drink small amounts of milk, especially if they eat food with it. Other people can’t drink any milk at all without having problems. The problems often start around two years of age, when the body naturally starts making less lactase.
Who is more likely to have lactose intolerance?
You are more likely to have lactose intolerance if you are from, or your family is from, a part of the world where lactose malabsorption is more common. In the United States, the following ethnic and racial groups are more likely to have lactose malabsorption:
- African Americans
- American Indians
- Asian Americans
- Hispanics/Latinos
Because these ethnic and racial groups are more likely to have lactose malabsorption, they are also more likely to have the symptoms of lactose intolerance.
Lactose intolerance is least common among people who are from, or whose families are from, Europe.
What causes lactose intolerance?
Lactose intolerance is caused by lactose malabsorption. If you have lactose malabsorption, your small intestine makes low levels of lactase—the enzyme that breaks down lactose—and can’t digest all the lactose you eat or drink.
The undigested lactose passes into your colon. Bacteria in your colon break down the lactose and create fluid and gas. In some people, this extra fluid and gas causes lactose intolerance symptoms.
In some cases, your genes are the reason for lactose intolerance. Genes play a role in the following conditions, and these conditions can lead to low levels of lactase in your small intestine and lactose malabsorption:
- Lactase nonpersistence. In people with lactase nonpersistence, the small intestine makes less lactase after infancy. Lactase levels get lower with age. Symptoms of lactose intolerance may not begin until later childhood, the teen years, or early adulthood. Lactase nonpersistence, also called primary lactase deficiency, is the most common cause of low lactase levels.
- Congenital lactase deficiency. In this rare condition, the small intestine makes little or no lactase, starting at birth.
Not all causes of lactose intolerance are genetic. The following can also lead to lactose intolerance:
- Injury to the small intestine. Infections, diseases, or other conditions that injure your small intestine, like Crohn’s disease or celiac disease, may cause it to make less lactase. Treatments—such as medicines, surgery, or radiation therapy —for other conditions may also injure your small intestine. Lactose intolerance caused by injury to the small intestine is called secondary lactose intolerance. If the cause of the injury is treated, you may be able to tolerate lactose again.
- Premature birth. In premature babies, or babies born too soon, the small intestine may not make enough lactase for a short time after birth. The small intestine usually makes more lactase as the baby gets older.
What are the complications of lactose intolerance?
Lactose intolerance may affect your health if it keeps you from getting enough nutrients, such as calcium and vitamin D. Milk and milk products, which contain lactose, are some of the main sources of calcium, vitamin D, and other nutrients.
You need calcium throughout your life to grow and have healthy bones. If you don’t get enough calcium, your bones may become weak and more likely to break. This condition is called osteoporosis . If you have lactose intolerance, you can change your diet to make sure you get enough calcium while also managing your symptoms.
How do doctors diagnose lactose intolerance?
To diagnose lactose intolerance, your doctor will ask about your symptoms, family and medical history, and eating habits.
Your doctor may perform a physical exam and tests to help diagnose lactose intolerance or to check for other health problems. Other conditions, such as irritable bowel syndrome, celiac disease, inflammatory bowel disease, or small bowel bacterial overgrowth can cause symptoms similar to those of lactose intolerance.
Your doctor may ask you to stop eating and drinking milk and milk products for a period of time to see if your symptoms go away. If your symptoms don’t go away, your doctor may order additional tests.
Physical exam
During a physical exam, your doctor may:
- check for bloating in your abdomen
- use a stethoscope to listen to sounds within your abdomen
- tap on your abdomen to check for tenderness or pain
Your doctor may order a hydrogen breath test to see how well your small intestine digests lactose.
Hydrogen breath test
Doctors use this test to diagnose lactose malabsorption and lactose intolerance. Normally, a small amount of hydrogen, a type of gas, is found in your breath. If you have lactose malabsorption, undigested lactose causes you to have high levels of hydrogen in your breath.
For this test, you will drink a liquid that contains a known amount of lactose. Every 30 minutes over a few hours, you will breathe into a balloon-type container that measures the amount of hydrogen in your breath. During this time, a health care professional will ask about your symptoms. If both your breath hydrogen levels rise and your symptoms get worse during the test, your doctor may diagnose lactose intolerance.
How is lactose intolerance treated?
In most cases, you can manage the symptoms of lactose intolerance by changing your diet to limit or avoid foods and drinks that contain lactose, such as milk and milk products.
Some people may only need to limit the amount of lactose they eat or drink, while others may need to avoid lactose altogether. Using lactase products can help some people manage their symptoms.
Milk and milk products are an important source of calcium. Your goal should be to get 1,200 to 1,500 mg of calcium each day. Children, teenagers, women who are pregnant or breastfeeding, and women who have gone through menopause should take calcium supplements if they can’t drink enough milk or eat enough dairy products to get this much calcium.
Instead of drinking milk, eat foods that are high in calcium, like leafy greens (such as collards, kale, and mustard greens), oysters, sardines, canned salmon (if you eat the salmon bones), shrimp, broccoli, and brussels sprouts. You can buy orange juice with added calcium.
Ask your doctor if you should take calcium supplements. There are many kinds. The supplements with an oyster shell base are absorbed best. Check the amount of calcium on the product label. Some antacids have a lot of calcium in them. They make a good calcium supplement if you have to take antacids anyway.
If you can, eat and drink smaller servings of dairy products, but have them more often. The smaller the serving, the less likely it is that you’ll have problems.
Eat food when you drink milk. This slows the digestive process, and you have less chance of having problems.
You may not have any trouble eating yogurt if it includes an active culture. Check the label to see if active culture is included.
Ice cream, milk shakes, and aged (hard) cheeses are easier to digest than milk for most people with lactose intolerance, but these foods are high in fat. If your weight and cholesterol and triglyceride levels are normal, you can try them.
Look for lactose-reduced milk in your grocery store. It has about 70 percent less lactose than regular milk, but it costs a little more.
Lactase products
Lactase products are tablets or drops that contain lactase, the enzyme that breaks down lactose. You can take lactase tablets before you eat or drink milk products. You can also add lactase drops to milk before you drink it. The lactase breaks down the lactose in foods and drinks, lowering your chances of having lactose intolerance symptoms.
Check with your doctor before using lactase products. Some people, such as young children and pregnant and breastfeeding women, may not be able to use them.
Try adding lactase to regular milk. You can buy lactase at drug stores. Some people like the flavor of milk with added lactase because it tastes sweet.
How do doctors treat lactose intolerance?
Treatments depend on the cause of lactose intolerance. If your lactose intolerance is caused by lactase nonpersistence or congenital lactase deficiency, no treatments can increase the amount of lactase your small intestine makes. Your doctor or dietitian can help you change your diet to manage your symptoms.
If your lactose intolerance is caused by an injury to your small intestine, your doctor may be able to treat the cause of the injury. You may be able to tolerate lactose after treatment.
While some premature babies are lactose intolerant, the condition usually improves without treatment as the baby gets older.
How should I change my diet if I have lactose intolerance?
Talk with your doctor or a dietitian about changing your diet to manage lactose intolerance symptoms while making sure you get enough nutrients. If your child has lactose intolerance, help your child follow the dietary plan recommended by a doctor or dietitian.
To manage your symptoms, you may need to reduce the amount of lactose you eat or drink. Most people with lactose intolerance can have some lactose without getting symptoms.
Foods that contain lactose
You may not need to completely avoid foods and beverages that contain lactose—such as milk or milk products. If you avoid all milk and milk products, you may get less calcium and vitamin D than you need.
People with lactose intolerance can handle different amounts of lactose. Research suggests that many people could have 12 grams of lactose—the amount in about 1 cup of milk—without symptoms or with only mild symptoms 25.
You may be able to tolerate milk and milk products if you:
- drink small amounts of milk at a time and have it with meals
- add milk and milk products to your diet a little at a time and see how you feel
- try eating yogurt and hard cheeses, like cheddar or Swiss, which are lower in lactose than other milk products
- use lactase products to help digest the lactose in milk and milk products
Foods and drinks containing lactose
- Lactose is in all milk and milk products and may be found in other foods and drinks.
Milk and milk products may be added to boxed, canned, frozen, packaged, and prepared foods. If you have symptoms after consuming a small amount of lactose, you should be aware of the many products that may contain lactose, such as:
- bread and other baked goods, such as pancakes, biscuits, cookies, and cakes
- processed foods, including breakfast cereals, instant potatoes, soups, margarine, salad dressings, and flavored chips and other snack foods
- processed meats, such as bacon, sausage, hot dogs, and lunch meats
- milk-based meal replacement liquids and powders, smoothies, and protein powders and bars
- nondairy liquid and powdered coffee creamers, and nondairy whipped toppings
You can check the ingredient list on packaged foods to see if the product contains lactose. The following words mean that the product contains lactose:
- milk
- lactose
- whey
- curds
- milk by-products
- dry milk solids
- nonfat dry milk powder
A small amount of lactose may be found in some prescription and over-the-counter medicines. Talk with your doctor about the amount of lactose in medicines you take, especially if you typically cannot tolerate even small amounts of lactose.
Lactose-free and lactose-reduced milk and milk products
Using lactose-free and lactose-reduced milk and milk products may help you lower the amount of lactose in your diet. These products are available in many grocery stores and are just as healthy for you as regular milk and milk products.
Calcium and Vitamin D
If you are lactose intolerant, make sure you get enough calcium and vitamin D each day. Milk and milk products are the most common sources of calcium.
Many foods that do not contain lactose are also sources of calcium. Examples include:
- fish with soft bones, such as canned salmon or sardines
- broccoli and leafy green vegetables
- oranges
- almonds, Brazil nuts, and dried beans
- tofu
- products with labels that show they have added calcium, such as some cereals, fruit juices, and soy milk
Vitamin D helps your body absorb and use calcium. Be sure to eat foods that contain vitamin D, such as eggs and certain kinds of fish, such as salmon. Some ready-to-eat cereals and orange juice have added vitamin D. Some milk and milk products also have added vitamin D. If you can drink small amounts of milk or milk products without symptoms, choose products that have added vitamin D. Also, being outside in the sunlight helps your body make vitamin D.
Talk with your doctor or dietitian about whether you are getting the nutrients you need. For safety reasons, also talk with your doctor before using dietary supplements or any other complementary or alternative medicines or practices. Also talk with your doctor about sun exposure and sun safety.
- Ching SS, Tan YK. Spectral analysis of bowel sounds in intestinal obstruction using an electronic stethoscope. World Journal of Gastroenterology : WJG. 2012;18(33):4585-4592. doi:10.3748/wjg.v18.i33.4585. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3435785/[↩][↩][↩][↩][↩]
- Physicians’ abdominal auscultation. A multi-rater agreement study. Gade J, Kruse P, Andersen OT, Pedersen SB, Boesby S. Scand J Gastroenterol. 1998 Jul; 33(7):773-7. https://www.ncbi.nlm.nih.gov/pubmed/9712245/[↩]
- Usefulness of bowel sound auscultation: a prospective evaluation. J Surg Educ. 2014 Sep-Oct;71(5):768-73. doi: 10.1016/j.jsurg.2014.02.003. Epub 2014 Apr 24. https://www.jsurged.org/article/S1931-7204(14)00052-X/fulltext[↩][↩]
- How Useful Are Bowel Sounds in Assessing the Abdomen? Dig Surg 2010;27:422–426 https://www.karger.com/Article/Abstract/319372[↩]
- Fruhwald S, Holzer P, Metzler H: Gastrointestinal motility in acute illness. Wien Klin Wochenschr 2008; 120: 6−17. doi: 10.1007/s00508-007-0920-2.[↩][↩]
- Moll van Charante EP, de Jongh TO. [Auscultation of the abdomen] Ned Tijdschr Geneeskd. 2011;155:A2657. https://www.ncbi.nlm.nih.gov/pubmed/21342596[↩]
- Connell AM. The assessment of intestinal motility. Proc R Soc Med. 1966;59 Suppl:6–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1900637/pdf/procrsmed00174-0010.pdf[↩]
- How does the stomach work ? National Center for Biotechnology Information, U.S. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072488/[↩]
- Hardwick, A.J. and Walton, A.J. Forced oscillation of a bubble in a liquid. Eur. J. Phys. 15: 325-328, 1994.[↩]
- Arnbjörnsson E. Normal and pathological bowel sound patterns. Ann Chir Gynaecol. 1986;75:314–318. Arnbjörnsson E. Normal and pathological bowel sound patterns. Ann Chir Gynaecol. 1986;75:314–318. https://www.ncbi.nlm.nih.gov/pubmed/3579191[↩]
- Watson, W.C. and Knox, E.C. Phonoenterography: the recording and analysis of bowel sounds. Gut 8: 88-94, 1967.[↩]
- Madsen, D., Sebolt, T., Cullen, L. Folkedahl, B., Mueller, T., Richardson, C. and Titler, M. Listening to bowel sounds: An evidence-based practice project. Am. J. Nurs. 105: 40-49, 2005.[↩]
- Serra, J., Azpiroz, F. and Malagelada, J.R. Intestinal gas dynamics and tolerance in humans. Gastroenterology 115: 542-550, 1998.[↩]
- Avruch, L. and Cooperberg, P.L. The ring-down artifact. J. Ultrasound. Med. 4: 21-28, 1985.[↩][↩]
- Leighton, J.A. and Shiff, A.D. Capsule endoscopy: ways to avoid missing lesions and to optimize diagnostic yield. Tech. Gastrointest. Endosc. 8: 169-174, 2006.[↩]
- Liu, F., Cuevas, C., Moss, A.A., Kolokythas, O., Dubinsky, T.J. and Kinahan, P.E. Gas bubble motion artifact in MDCT. Am. J. Roentgenol. 190: 294-299, 2008.[↩]
- Sugrue M, Redfern M. Computerized phonoenterography: the clinical investigation of a new system. J Clin Gastroenterol. 1994;18:139–144. https://www.ncbi.nlm.nih.gov/pubmed/8189010[↩]
- Gazet JC. The surgical significance of the ileo-caecal junction. Ann R Coll Surg Engl. 1968;43:19–38. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2312254/pdf/annrcse00254-0026.pdf[↩]
- Malbrain MLNG, De Waele J: PACT module: abdominal problems. ESICM PACT 2007.[↩]
- Suri S, Gupta S, Sudhakar PJ, Venkataramu NK, Sood B, Wig JD. Comparative evaluation of plain films, ultrasound and CT in the diagnosis of intestinal obstruction. Acta Radiol. 1999;40:422–428. https://www.ncbi.nlm.nih.gov/pubmed/10394872[↩]
- Saunders MD: Acute colonic pseudo-obstruction. Gastrointest Endosc Clin N Am 2007; 17: 341−360, vi-vii.[↩]
- Storhaug CL, Fosse SK, Fadnes LT. Country, regional, and global estimates for lactose malabsorption in adults: a systematic review and meta-analysis. The Lancet. Gastroenterology & Hepatology. 2017;2(10):738–746.[↩][↩]
- Misselwitz B, Fox M. What is normal and abnormal in lactose digestion? The Lancet. Gastroenterology & Hepatology. 2017;2(10):696–697.[↩]
- Bayless TM, Brown E, Paige DM. Lactase non-persistence and lactose intolerance. Current Gastroenterology Reports. 2017;19(5):23.[↩]
- Dalal SR, Chang EB. Chapter 65: Disorders of epithelial transport, metabolism, and digestion in the small intestine. In: Podolsky DK, Camilleri M, Fitz JG, Kalloo AN, Shanahan F, Wang TC, eds. Yamada’s Textbook of Gastroenterology. 6th ed. West Sussex: John Wiley & Sons; 2016;1276–1293.[↩]